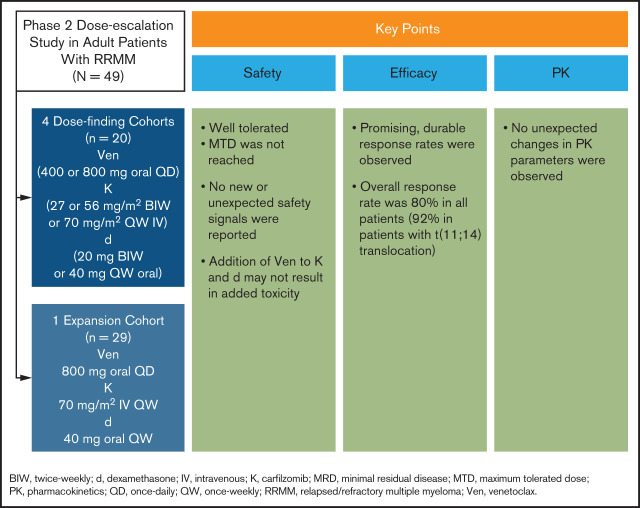
Key Points
Venetoclax combined with carfilzomib and dexamethasone is well tolerated, and no new or unexpected safety signals have been reported.
Venetoclax in combination with carfilzomib and dexamethasone shows antimyeloma activity and durable response rates in patients with RRMM.
Visual Abstract
Abstract
Proteins in the antiapoptotic B-cell lymphoma 2 (BCL-2) family play a role in the pathophysiology of multiple myeloma (MM). Venetoclax is a highly selective, potent, oral BCL-2 inhibitor that induces apoptosis of MM cells, and its efficacy may be potentiated through combination with agents that increase BCL-2 dependency or have complementary mechanisms of action. The safety, tolerability, pharmacokinetics, and antitumor activity of venetoclax in combination with carfilzomib and dexamethasone (VenKd) in adults with relapsed/refractory MM (RRMM) were investigated in this phase 2 dose-escalation study. Oral venetoclax (400 or 800 mg) was administered daily in combination with intravenous carfilzomib (27, 56, or 70 mg/m2) and oral dexamethasone (20 or 40 mg) in 4 dose-finding cohorts. The expansion cohort received venetoclax 800 mg, carfilzomib 70 mg/m2, and dexamethasone 40 mg. Forty-nine patients received treatment. Median prior lines of therapy was 1 (range, 1-3), and median time in the study was 27 months. The most common treatment-emergent adverse events were diarrhea (65%), fatigue (47%), nausea (47%), and lymphopenia (35%). Serious adverse events occurred in 26 (53%) patients. Of 3 treatment-emergent deaths, 1 was considered treatment related. The overall response rate was 80% in all patients, 92% in patients with t(11;14) (n = 13), and 75% in patients without (n = 36). The rate of complete response or better was 41%. Median progression-free survival was 22.8 months. Treatment with VenKd was well tolerated and showed promising response rates in this RRMM patient population, with greater responses observed in patients with t(11;14). This trial is registered at www.clinicaltrials.gov as #NCT02899052.
Introduction
Outcomes for patients with multiple myeloma (MM) have improved over the past decade.1,2 However, MM remains incurable and invariably relapses.3,4 In the relapsed/refractory (RR) setting, MM becomes increasingly aggressive, and remission durations often decrease with each subsequent regimen.1,5-7
Several therapeutic agents with unique mechanisms of action have recently been approved for RRMM, including new proteasome inhibitors (PIs; ie, carfilzomib, ixazomib), immunomodulatory (IMiD)/cereblon-binding drugs (ie, pomalidomide), monoclonal antibodies (ie, daratumumab, isatuximab, elotuzumab, and belantamab mafodotin), and a selective inhibitor of nuclear export (ie, selinexor).1,4,8
Dysregulation of the intrinsic apoptotic pathway contributes to hematologic malignancy pathogenesis.9 Members of the B-cell lymphoma 2 (BCL-2) protein family function as key regulators of the intrinsic apoptosis pathway.10 Antiapoptotic BCL-2 family proteins, including BCL-2, myeloid cell leukemia 1 (MCL-1), and BCL-XL, contribute to development and progression of MM.11 Venetoclax is a highly selective, potent, oral BCL-2 inhibitor that restores apoptosis by direct, high-affinity binding to its prosurvival target, BCL-2.12 Venetoclax, as a monotherapy and in combination studies, has demonstrated meaningful clinical activity in RRMM.13,14 Therapeutic approaches that combine venetoclax with agents that increase BCL-2 dependency or have complementary mechanisms of action may further potentiate therapeutic efficacy in MM.
Notably, the proapoptotic, BH3-only protein NOXA promotes apoptosis through direct binding to MCL-1, triggering its proteasomal degradation.15 PIs, including bortezomib and the second-generation inhibitor carfilzomib, have demonstrated significant activity in RRMM.1,16 Through a potential class effect, PIs upregulate NOXA expression, inducing apoptosis of MM cells.17-19 Furthermore, carfilzomib and the glucocorticoid dexamethasone indirectly promote BCL-2 dependency in MM cells by shifting binding of the proapoptotic protein BIM to BCL-2.18 Dexamethasone additionally decreases BCL-XL expression.18
Given promising early clinical data to support the combination of venetoclax with PIs, this phase 2 study was initiated to investigate outcomes of venetoclax in combination with carfilzomib and dexamethasone (VenKd) in adults with RRMM.
Methods
Study design
This open-label, multicenter, phase 2, dose-escalation study in adults with RRMM was conducted at 10 sites. Patients were enrolled from February 2017 through February 2019 to receive VenKd in 1 of 4 dose-finding cohorts and 1 expansion cohort (supplemental Figure 1). The protocol and amendments were approved by the institutional review boards of the participating centers; all patients provided written informed consent. This study was conducted in compliance with the International Conference on Harmonization Good Clinical Practice guidelines and the Declaration of Helsinki.
Patients
Patients ≥18 years of age with RRMM were eligible. They had received 1 to 3 lines of prior therapy, had an Eastern Cooperative Oncology Group (ECOG) performance status ≤2, and had measurable disease. Patients were not eligible if they were refractory to any BCL-2 family inhibitor, had grade ≥3 peripheral neuropathy, or had significant cardiovascular disease. Patients could be refractory to PIs but could not have had prior treatment with carfilzomib. Additional eligibility criteria are in supplemental Methods.
Procedures
Patients received treatment at 1 of 4 dose-finding levels with oral venetoclax daily (400 or 800 mg), intravenous carfilzomib (27 or 56 mg/m2 on days 1, 2, 8, 9, 15, and 16 administered over 10-30 minutes, or 70 mg/m2 on days 1, 8, and 15 administered as a 30-minute infusion or per institutional guidelines), and oral dexamethasone (40 mg on days 1, 8, 15, and 22 or 20 mg on days 1, 2, 8, 9, 15, 16, 22, and 23) in 28-day cycles (supplemental Table 1). Venetoclax dose ramp-up was not performed. Carfilzomib was administered at 20 mg/m2 during the first week and was increased to the target dose in cycle 1 on day 8. Intravenous administration of dexamethasone was permitted; patients ≥75 years of age could receive 20 mg dexamethasone. Treatment continued until disease progression or unacceptable toxicity.
Patients who completed ≥80% of venetoclax and carfilzomib doses in cycle 1 or experienced a dose-limiting toxicity (DLT) were evaluable for dose-escalation decisions, which were guided by Bayesian optimal interval design. DLTs for dose escalation decisions were assessed during the first cycle (28 days) and could have been attributable to venetoclax, carfilzomib, or dexamethasone (supplemental Methods). Adverse events (AEs) that occurred after cycle 1 were evaluated by the investigator and could be considered dose limiting. Patients who did not complete ≥80% of venetoclax and carfilzomib doses in cycle 1 and did not experience a DLT were evaluated for safety.
Tumor lysis syndrome prophylaxis with oral and intravenous hydration was initiated in all patients ≥72 hours before the first dose of venetoclax and carfilzomib. Given the BELLINI study (www.clinicaltrials.gov, #NCT02755597) findings,20 the protocol was amended in March 2019 to implement antibiotic prophylaxis for prevention of grade ≥3 or serious infections: trimethoprim/sulfamethoxazole (160/800 mg) or equivalent while receiving treatment and levofloxacin (500 mg daily, adjusted for renal function) or equivalent for the first 90 days in the study and after development of grade 4 neutropenia. All patients received antiviral prophylaxis for prevention of herpes zoster. Patients who remained in the study beyond cycle 18 could receive venetoclax monotherapy or continue a combination regimen.
Assessments
Primary outcomes included safety, tolerability, and preliminary efficacy. Safety assessments included the number of patients with DLTs, AEs, and changes in laboratory results. Treatment-emergent AEs (TEAEs) were summarized per the Medical Dictionary for Regulatory Activities, version 22.1 (http://meddra.org); AEs and laboratory values were graded per National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.03 (https://ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm). Preliminary efficacy was assessed through overall response rate (ORR; ie, partial response or better) and the rate of very good partial response (VGPR) or better in all patients and those with t(11;14). The presence of t(11;14) was determined a priori.
Secondary outcomes included pharmacokinetics (PKs) and secondary efficacy assessments: progression-free survival (PFS), time to progression (TTP), duration of response (DOR), and minimal residual disease (MRD) in all patients and in those with high BCL-2 expression. BCL-2 protein expression was determined by immunohistochemical analysis of bone marrow (BM) core biopsy specimens, with high expression defined as ≥50% of tumor cells having a cytoplasmic intensity score of ≥2+ on a 0-to-3 scale. BCL2 gene expression was determined by quantitative polymerase chain reaction in BM aspirates after CD138 enrichment, with high expression (BCL2high) defined by the bootstrapping and aggregating thresholds from trees analysis used in the BELLINI study.20 Fluorescence in situ hybridization analysis was performed on CD138-enriched BM aspirates to assess t(11;14) and known prognostic cytogenetic markers in MM. MRD was assessed in BM aspirates by next-generation sequencing (supplemental Methods). Patients with missing or unevaluable MRD status were considered MRD+ according to international harmonization.21
Blood samples for PK assays were collected at specified time points (supplemental Methods). Plasma concentrations were determined by using liquid–liquid extraction and liquid chromatography with tandem mass spectrometric detection.22
Statistical analyses
The data cutoff date was 14 February 2020. Safety, PK, and efficacy analyses included all patients who received ≥1 dose of any of the study drugs. Patients were required to have ≥1 postdose PK result for inclusion in PK analyses. Continuous demographic data were summarized, and frequencies and percentages were computed for categorical data. Plasma concentrations and PK parameter values of venetoclax and carfilzomib were tabulated for each patient and dose combination, and summary statistics were computed for each sampling time and parameter. PK parameters were estimated using the noncompartmental methods in Phoenix WinNonlin, version 6.4 (Certara USA, Inc, Princeton, NJ).
TEAEs were defined as those with onset on or after the first dose of study drug until 30 days after the last date of venetoclax administration. Serious AEs were defined as AEs that were life-threatening; resulted in death, congenital abnormality, or persistent or significant disability or incapacity; or required medical or surgical intervention to prevent serious outcome. Clinical responses were defined according to International Myeloma Working Group criteria,23,24 per investigator assessment, and confirmed by consecutive assessment. The ORR, ≥VGPR rate, and CR or better (≥CR) rate were calculated; the 95% confidence interval (CI) was calculated by the Clopper-Pearson method. Time-to-event end points, PFS, and DOR were censored at last adequate disease assessment for patients without events. Time-to-event end points were analyzed using Kaplan-Meier product-limit methodology, and median time-to-event and corresponding 95% CIs were estimated.
For exploratory subgroup analyses, the rates of ORR, ≥VGPR, ≥CR, and MRD negativity (<10−5) were compared between biomarker subgroups. P-values were calculated with a 2-sample proportion test with Yates continuity correction, and 95% CIs were calculated using the Clopper-Pearson method. HR and 95% CIs of PFS and DOR were estimated with a Cox proportional hazards model that included biomarker subgroups including t(11;14) vs non-t(11;14), BCL2high vs BCL2low gene expression, MRD-positive vs MRD-negative, and PI refractory vs IMiD refractory vs double refractory. Median survival time and corresponding 95% CIs for each subgroup were estimated by using the Kaplan-Meier product-limit method.
Results
Patients
A total of 49 patients were enrolled, including 20 patients in the 4 dose-finding cohorts and 29 in the expansion cohort (supplemental Figure 1). Most patients received carfilzomib 70 mg/m2 (n = 35; 71%), with fewer patients treated with 56 mg/m2 (n = 7; 14%) or 27 mg/m2 (n = 7; 14%). The majority of patients received 800 mg venetoclax (n = 45; 92%); only 4 (8%) patients received 400 mg venetoclax. The median age was 66 years (range, 37-79), 39 (80%) patients were White, 29 (59%) had ECOG performance status of 1 or 2, 30 (61%) had International Staging System (ISS) stage II or III disease, and all had received a median of 1 (range, 1-3) prior line of therapy (Table 1). Most patients had prior exposure to a PI (n = 47; 96%), IMiD (n = 44; 90%), or both (n = 42; 86%). One patient had prior exposure to an anti-CD38 monoclonal antibody. Forty-two (86%) patients were refractory to the last prior therapy, with 28 (57%), 35 (71%), and 22 (45%) patients refractory to a PI, IMiD, or both, respectively. Thirteen (27%) patients had high-risk cytogenetic status, defined as the presence of t(4;14), t(14;16), or del(17p). The t(11;14) translocation was detected in 13 (27%) patients, and baseline disease characteristics were generally similar, irrespective of t(11;14) status, although fewer patients with t(11;14) had ISS stage II or III disease vs those without t(11;14) (38% vs 69%). Baseline BM core biopsy samples from 28 patients were evaluable for BCL-2 protein expression; 26 (93%) had high protein expression (≥50% tumor cells with ≥2+ staining intensity). Baseline BM aspirate samples from 39 patients were evaluable for determining BCL2 gene expression. A broad range of BCL2 gene expression (range 2−ΔCt, 0.0-2.3) was observed, which generally correlated with BCL-2 protein expression (supplemental Figure 2).
Table 1.
Patient demographics and baseline disease characteristics
| Characteristic | All patients, N = 49 | t(11;14), n = 13 | Non-t(11;14), n = 36 |
|---|---|---|---|
| Median age (range), y | 66 (37-79) | 63 (47-75) | 68 (37-79) |
| Race, n (%) | |||
| White | 39 (80) | 10 (77) | 29 (81) |
| Black or African American | 10 (20) | 3 (23) | 7 (19) |
| ECOG performance status, n (%) | |||
| 0 | 15 (31) | 4 (31) | 11 (31) |
| 1-2 | 29 (59) | 7 (54) | 22 (61) |
| Missing | 5 (10) | 2 (15) | 3 (8) |
| ISS stage, n (%) | |||
| I | 18 (37) | 8 (62) | 10 (28) |
| II | 15 (31) | 1 (8) | 14 (39) |
| III | 15 (31) | 4 (31) | 11 (31) |
| Unknown | 1 (2) | 0 | 1 (3) |
| Cytogenetic status, n (%) | |||
| High-risk* | 13 (27) | 4 (31) | 9 (25) |
| Standard risk† | 29 (59) | 9 (69) | 20 (56) |
| Unknown | 7 (14) | 0 (0) | 7 (19) |
| Cytogenetic abnormalities, n (%) | |||
| t(11;14) | 13 (27) | 13 (100) | 0 |
| t(4;14) | 2 (4) | 0 | 2 (6) |
| t(14;16) | 2 (4) | 0 | 2 (6) |
| del(17p) | 10 (20) | 4 (31) | 6 (17) |
| 1q21 gain (≥3 copies) | 21 (43) | 5 (39) | 16 (44) |
| Hyperdiploid | 11 (22) | 2 (15) | 9 (25) |
| Median time from diagnosis to treatment (range), months | 37.4 (2.4-195.6) | 37.7 (4.9-126.7) | 34.7 (2.4-195.6) |
| Median no. of prior lines of therapy (range) | 1 (1-3) | 1 (1-2) | 1 (1-3) |
| Refractory to last prior therapy, n (%) | 42 (86) | 9 (69) | 33 (92) |
| Prior stem cell transplantation, n (%) | 25 (51) | 3 (23) | 22 (61) |
| Prior exposure to PI, n (%) | 47 (96) | 12 (92) | 35 (97) |
| Refractory to PI | 28 (57) | 9 (69) | 19 (53) |
| Prior exposure to IMiD, n (%) | 44 (90) | 10 (77) | 34 (94) |
| Refractory to IMiD | 35 (71) | 9 (69) | 26 (72) |
| Prior exposure to PI+IMiD, n (%) | 42 (86) | 9 (69) | 33 (92) |
| Double refractory | 22 (45) | 6 (46) | 16 (44) |
| BCL-2 expression (IHC), n/n (%) ‡ | |||
| High | 26/28 (93) | 7/7 (100) | 19/21 (90) |
| Low | 2/28 (7) | 0 | 2/21 (10) |
| BCL2 expression (qPCR), n/n (%) § | |||
| High | 22/39 (56) | 8/9 (89) | 14/30 (47) |
| Low | 17/39 (44) | 1/9 (11) | 16/30 (53) |
IHC, immunohistochemistry; IMiD, immunomodulatory drug; qPCR, quantitative polymerase chain reaction.
t(4;14), t(14;16), or del(17p).
No high-risk cytogenetics present.
Baseline BM core biopsy samples from 28 patients were evaluable for BCL-2 protein expression by IHC. High expression was defined as ≥50% of tumor cells with a cytoplasmic intensity score of ≥2+ on a 0 to 3+ intensity scale. Percentages exclude patients with missing data.
Baseline BM aspirate samples from 39 patients were evaluable for BCL2 gene expression by qPCR. High expression was defined as previously described.20 Percentages exclude patients with missing data.
Patients’ median time on study was 27.0 months (range, 11.4-36.5; supplemental Table 2). As of the data cutoff, study treatment was ongoing in 13 (27%) patients. Of 36 patients who withdrew, the primary reasons for discontinuation were progressive disease (n = 18; 37%), withdrawal of consent (6; 12%), an AE (4; 8%), physician’s decision (3; 6%), death (3; 6%), lack of efficacy (1; 2%), and other (1; 2%). The median duration of venetoclax and carfilzomib exposure was 9.2 months (range, 0.3-36.5) and 8.6 months (range, 0.5-18.0), respectively. Dose reductions and interruptions are summarized in supplemental Table 3.
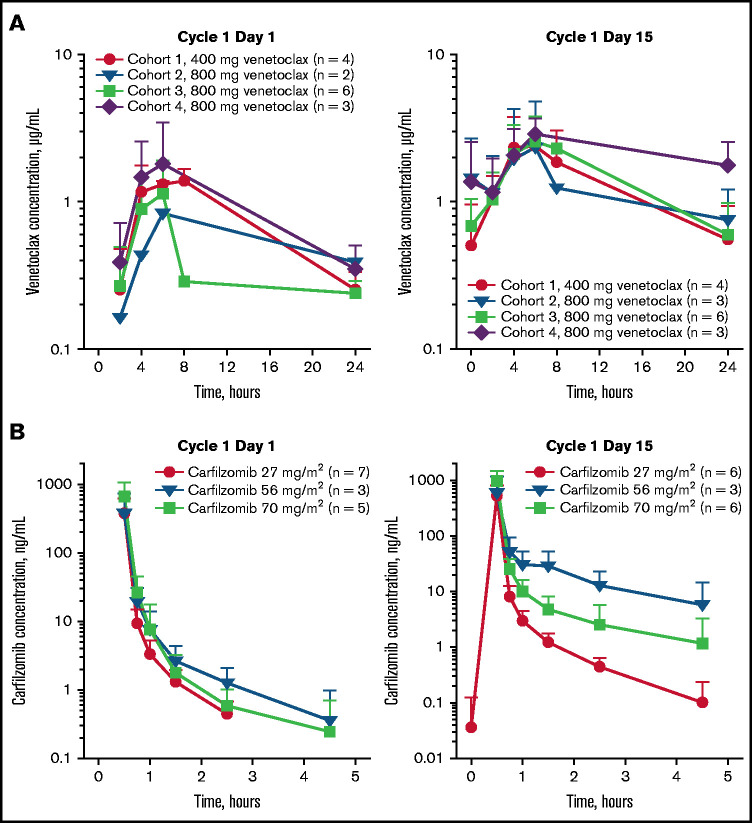
PK
Venetoclax and carfilzomib PK profiles are shown in Figure 1. PK parameters are summarized by dose cohort in Table 2. Peak venetoclax concentrations were attained 4 to 6 hours after the dose was administered, whereas carfilzomib concentrations peaked at 0.4 to 1.3 hours after. Venetoclax half-life could not be estimated because of the limited sampling after the time to maximum observed plasma concentration was reached. Carfilzomib half-life was <1 hour. Venetoclax exposures when coadministered with carfilzomib were comparable to venetoclax exposures when coadministered with bortezomib.14,25 Carfilzomib exposure at the 27 mg/m2 dose in combination with venetoclax was similar to those in previous reports, but exposure was lower than previously described at the 70 mg/m2 dose.26,27
Figure 1.
Plasma concentration-time profiles. Venetoclax (A) and carfilzomib (B).
Table 2.
Venetoclax and carfilzomib PK parameters in the plasma
| Cohort 1 | Cohort 2 | Cohort 3 | Cohort 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Venetoclax 400 mg+ | Venetoclax 800 mg+ | Venetoclax 800 mg+ | Venetoclax 800 mg+ | |||||
| carfilzomib 27 mg/m2+ | carfilzomib 27 mg/m2+ | carfilzomib 70 mg/m2+ | carfilzomib 56 mg/m2+ | |||||
| dexamethasone 40 mg | dexamethasone 40 mg | dexamethasone 40 mg | dexamethasone 40 mg | |||||
| C1D1, n = 4 | C1D15, n = 4 | C1D1, n = 2* | C1D15, n = 3 | C1D1, n = 6 | C1D15, n = 6 | C1D1, n = 3 | C1D15, n = 3 | |
| Venetoclax PK parameters | ||||||||
| Tmax, h† | 6.0 (4.0, 8.0) | 4.0 (4.0, 6.0) | 6.0, 24.0 | 6.0 (6.0, 8.0) | 6.0 (6.0, 6.0) | 6.0 (6.0, 8.0) | 6.0 (4.0, 6.0) | 6.0 (4.0, 6.0) |
| Cmax, µg/mL | 1.57 (1.58, 9) | 2.18 (2.47, 57) | 0.505, 1.23 | 2.05 (2.59, 86) | 0.915 (1.13, 68) | 2.29 (2.69, 51) | 1.42 (1.85, 88) | 2.85 (2.94, 28) |
| AUC24, µg × h per mL | 19.9 (19.9, 9) | 30.2 (33.1, 54) | 9.34, 16.7 | 31.7 (39.9, 86) | 14.2 (15.2, 44)‡ | 33.0 (39.3, 49) | 20.8 (24.9, 77) | 50.9 (52.5, 30) |
| Carfilzomib PK parameters | n = 4 | n = 3 | n = 3 | n = 3 | n = 5 | n = 6 | n = 3 | n = 3 |
| Tmax, h† | 0.58 (0.57, 0.70) | 0.57 (0.55, 0.62) | 0.58 (0.52, 0.58) | 0.67 (0.58, 0.70) | 0.55 (0.52, 0.75) | 0.55 (0.27, 0.92) | 0.52 (0.50, 0.53) | 0.50 (0.50, 0.53) |
| Cmax, ng/mL | 135 (384, 87) | 501 (574, 67) | 351 (368, 34) | 455 (483, 42) | 519 (661, 62) | 852 (982, 50) | 263 (377, 95) | 429 (600, 97) |
| AUCinf, ng × h per mL | 72.1 (166, 85) | 212 (241, 65) | 146 (155, 37) | 209 (224, 47) | 241 (294, 61) | 381 (401, 29) | 121 (160, 84) | 247 (314, 89) |
| t1/2, h§ | 0.67 (0.3) | 0.75 (0.4) | 0.55 (0.1) | 0.63 (0.1) | 0.58 (0.2) | 0.98 (0.3) | 0.70 (0.6) | 0.83 (0.5) |
Data are reported as geometric mean (arithmetic mean, %CV) unless otherwise specified.
AUC24, area under the plasma concentration-time curve over a 24-hour dose interval; AUCinf, AUC from time 0 to infinity; C1D1: cycle 1, day 1; C1D15: cycle 1, day 15; Cmax, maximum observed plasma concentration; CV, coefficient of variation; t1/2, terminal elimination half-life; Tmax, time to Cmax.
n = 2; presented as individual values.
Median (minimum, maximum).
n = 4.
Harmonic mean (pseudo standard deviation).
Safety
No patients in any dose-finding cohort experienced DLTs. The study doses of carfilzomib 70 mg/m2 on days 1, 8, and 15; venetoclax 800 mg daily; and dexamethasone 40 mg on days 1, 8, 15, and 22 were selected for further evaluation in an expansion cohort of 29 patients. This carfilzomib dose regimen was selected, in part, based on findings from the CHAMPION-1 study27 and to provide convenience of administration.
All patients experienced ≥1 TEAE (Table 3). The most common nonhematologic TEAEs were diarrhea (65%), fatigue (47%), and nausea (47%); the most prevalent hematologic TEAEs were lymphopenia (35%) and thrombocytopenia (31%). Grade 3 or 4 TEAEs were observed in 45 (92%) patients (Table 3). The most common grade 3 and 4 nonhematologic TEAEs were hypertension (16%) and pneumonia (12%); the most prevalent hematologic TEAEs were lymphopenia (31%), leukopenia (12%), and neutropenia (12%). Serious TEAEs occurred in 26 (53%) patients; of those, pneumonia (7; 14%), influenza (3; 6%), acute kidney injury (2; 4%), congestive cardiac failure (2; 4%), and hypoxia (2; 4%) occurred in ≥1 patient. The most common any-grade infections included upper respiratory tract infection (39%), sinusitis (20%), pneumonia (18%), and influenza (16%; supplemental Table 4). Pneumonia (12%) and influenza (6%) were among the most common grade 3 and 4 infections. Of the 4 (8%) patients who withdrew from the study because of TEAEs, only 1 had an infection (influenza). Other reasons included diverticulitis, non-ST–elevated myocardial infarction with unstable angina, and decreased ejection fraction (n = 1 each). Grade 3 and 4 cardiac disorders occurred in 4 (8%) patients, and the only event reported in ≥1 patient was congestive cardiac failure (2; 4%). No grade 5 cardiovascular TEAEs occurred. One patient with t(11;14) and 60% BM infiltration at screening experienced clinical tumor lysis syndrome on cycle 1 day 2 after treatment with venetoclax 800 mg and carfilzomib 20 mg/m2. The patient was hospitalized and received hydration and allopurinol. Elevations in aspartate aminotransferase, lactate dehydrogenase, uric acid, and creatinine normalized, and treatment resumed 4 days later.
Table 3.
Summary of TEAEs
| TEAE by preferred term* | All patients n (%) (N = 49) | |
|---|---|---|
| Any grade | Grade ≥3 | |
| Any TEAE | 49 (100) | 45 (92) |
| Nonhematologic TEAEs | ||
| Diarrhea | 32 (65) | 5 (10) |
| Fatigue | 23 (47) | 3 (6) |
| Nausea | 23 (47) | 2 (4) |
| Upper respiratory tract infection | 19 (39) | 0 |
| Dyspnea | 17 (35) | 3 (6) |
| Insomnia | 17 (35) | 5 (10) |
| Cough | 16 (33) | 0 |
| Vomiting | 14 (29) | 3 (6) |
| Hypertension | 13 (27) | 8 (16) |
| Dyspepsia | 12 (24) | 0 |
| Edema peripheral | 12 (24) | 0 |
| Headache | 10 (20) | 0 |
| Hypocalcemia | 10 (20) | 0 |
| Hypokalemia | 10 (20) | 1 (2) |
| Sinusitis | 10 (20) | 0 |
| Abdominal pain | 9 (18) | 0 |
| Hypophosphatemia | 9 (18) | 5 (10) |
| Pneumonia | 9 (18) | 6 (12) |
| Hyperglycemia | 8 (16) | 3 (6) |
| Hypomagnesemia | 8 (16) | 0 |
| Influenza | 8 (16) | 3 (6) |
| Hematologic TEAEs | ||
| Lymphopenia† | 17 (35) | 15 (31) |
| Thrombocytopenia‡ | 15 (31) | 4 (8) |
| Neutropenia§ | 11 (22) | 6 (12) |
| Leukopenia|| | 11 (22) | 6 (12) |
| Anemia | 9 (18) | 4 (8) |
TEAEs presented are those occurring in ≥15% of patients for any grade or in ≥10% of patients for grades 3 and 4.
Includes decreased lymphocyte count.
Includes decreased platelet count.
Includes decreased neutrophil count.
||Includes decreased white blood cell count.
Five deaths occurred (supplemental Results). Two grade 5 infections occurred: non–treatment-emergent pulmonary aspergillosis in a patient with t(11;14) and treatment-emergent influenza B in a patient without t(11;14). Two additional treatment-emergent deaths were reported: 1 of respiratory arrest and 1 of unexplained cause, with reasonable possibility of being carfilzomib-related. Last, a patient died of non–treatment-emergent disease progression that occurred ≥30 days after the last dose of the study treatment.
Efficacy
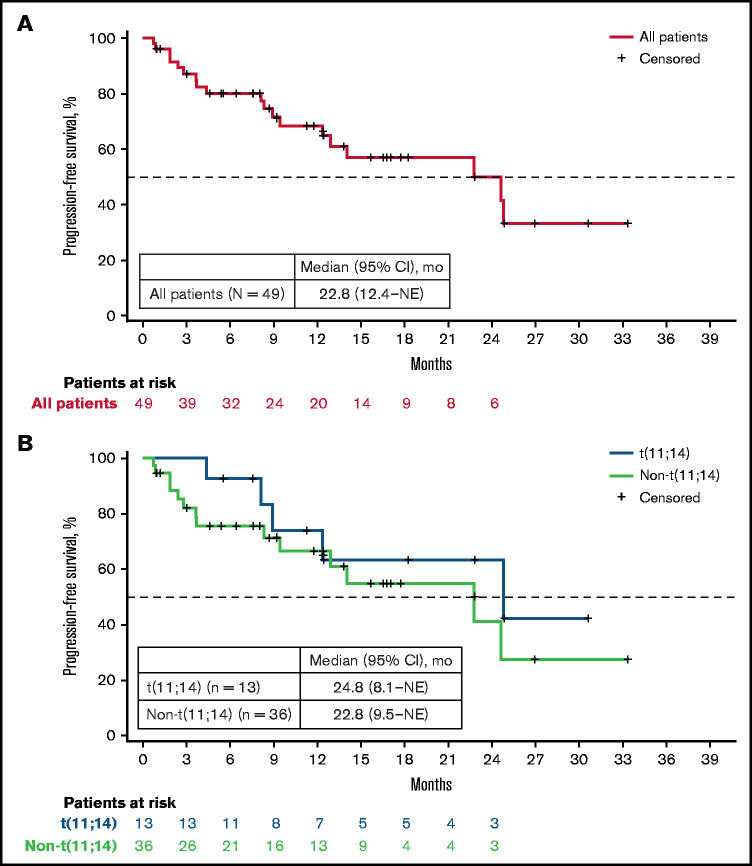
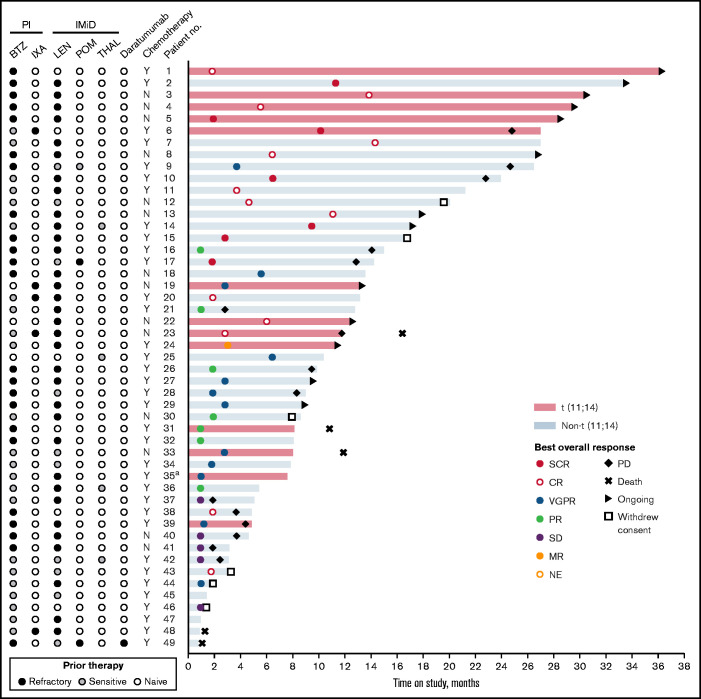
The ORR (≥PR) was 80% (95% CI, 66-90), the ≥VGPR rate was 65% (95% CI, 50-78), the ≥CR rate was 41% (95% CI, 27-56), and the MRD negativity (<10−5) rate was 12% among all patients (Table 4). With a median follow-up of 27 months (range, 11.4-36.5), 19 patients experienced PFS events including 14 with disease progression and 5 deaths. Median PFS was 22.8 months (95% CI, 12.4-not estimable [NE]) for all patients (Figure 2A), with the estimated 2-year PFS rate of 50% (95% CI, 29-68). A trend toward improved PFS was observed among patients who became MRD negative vs those who did not (hazards ratio [HR], 0.21; 95% CI, 0.03-1.62; P = .101). Median time to first response was 1.8 months (range, 0.9-14.3). Median TTP was 24.6 months (95% CI, 12.9-NE), with estimated 2-year TTP rate of 56% (95% CI, 33-74). Median DOR was 19.7 months (95% CI, 13.1-NE; Table 4; supplemental Figure 3). Best response, time on study, and status (ie, refractory, sensitive, and naïve) to prior therapy (ie, PIs, IMiDs, daratumumab, and chemotherapy) are shown for all patients in Figure 3.
Table 4.
Response rates and MRD negativity rates in all patients and key patient subgroups
| Characteristic | All patients (N = 49) | t(11;14) (n = 13) | Non-t(11;14) (n = 36) | BCL2 gene expression | Prior therapy | |||
|---|---|---|---|---|---|---|---|---|
| High (n = 22) | Low (n = 17) | PI refractory (n = 28) | IMiD refractory (n = 35) | PI and IMiD refractory (n = 22) | ||||
| ORR (≥PR) | 39 (80) | 12 (92) | 27 (75) | 19 (86) | 11 (65) | 24 (86) | 29 (81) | 18 (82) |
| ≥VGPR | 32 (65) | 11 (85) | 21 (58) | 17 (77) | 8 (47) | 20 (71) | 23 (64) | 15 (68) |
| ≥CR | 20 (41) | 7 (54) | 13 (36) | 9 (41) | 8 (47) | 13 (46) | 15 (42) | 10 (45) |
| Best overall response | ||||||||
| sCR | 7 (14) | 2 (15) | 5 (14) | 2 (9) | 5 (29) | 5 (18) | 6 (17) | 4 (18) |
| CR | 13 (27) | 5 (38) | 8 (22) | 7 (32) | 3 (18) | 8 (29) | 9 (25) | 6 (27) |
| VGPR | 12 (24) | 4 (31) | 8 (22) | 8 (36) | 0 | 7 (25) | 8 (22) | 5 (23) |
| PR | 7 (14) | 1 (8) | 6 (17) | 2 (9) | 3 (18) | 4 (14) | 6 (17) | 3 (14) |
| MR | 1 (2) | 1 (8) | 0 | 0 | 0 | 0 | 1 (3) | 0 |
| SD | 5 (10) | 0 | 5 (14) | 2 (9) | 3 (18) | 2 (7) | 3 (8) | 2 (9) |
| PD | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Not evaluable | 4 (8) | 0 | 4 (11) | 1 (5) | 3 (18) | 2 (7) | 3 (8) | 2 (9) |
| MRD | ||||||||
| <10−4 | 9 (18) | 4 (31) | 5 (14) | 7 (32) | 2 (12) | 6 (21) | 7 (20) | 5 (23) |
| <10−5 | 6 (12) | 2 (15) | 4 (11) | 4 (18) | 2 (12) | 3 (11) | 4 (11) | 2 (9) |
| <10−6 | 2 (4) | 1 (8) | 1 (3) | 2 (9) | 0 | 1 (4) | 1 (3) | 1 (5) |
| Median DOR (95% CI), mo | 19.7 (13.1-NE) | NR (9.6-NE) | 16.4 (9.2-NE) | 23.8 (19.8-NE) | 16.4 (13.2-NE) | 19.7 (9.2-NE) | 16.4 (9.6-NE) | NR (9.2-NE) |
Data are expressed as the number (percentage of study group), unless otherwise specified.
BCL2, B-cell lymphoma 2 gene; MR, minimal response; NR, not reached; PD, progressive disease; PR, partial response; sCR, stringent CR; SD, stable disease.
Figure 2.
Progression-free survival. All patients (A) and patients by t(11;14) status (B).
Figure 3.
Prior therapy status, best response, and time in the study for all patients. Refractory: patients who were exposed to the indicated therapy and progressed while receiving treatment or within 60 days after stopping treatment. Sensitive: patients who were exposed to the indicated therapy but did not progress while receiving therapy or who discontinued therapy because of toxicity. Naïve: patients who did not have prior exposure to the indicated therapy. aPatient 35 was also refractory to nivolumab and elotuzumab. BTZ, bortezomib; IXA, ixazomib; K, carfilzomib; LEN, lenalidomide; MR, minimal response; N, no; No., number; PD, progressive disease; POM, pomalidomide; PR, partial response; sCR, stringent complete response; SD, stable disease; THAL, thalidomide; Y, yes.
Patients with t(11;14) and without achieved ORRs of 92% (95% CI, 62-100) and 75% (95% CI, 58-87), respectively, ≥VGPR rates of 85% (95% CI, 54-97) and 58% (95% CI, 41-74), ≥CR rates of 54% (95% CI, 26-80) and 36% (95% CI, 21-54), and MRD negativity (<10−5) rates of 15% (95% CI, 2.7-46.3) and 11% (95% CI, 3.6-27.0; Table 4). Generally, greater ORRs were observed in patients with t(11;14) vs without, irrespective of ISS stage, although the limited sample size precludes meaningful conclusions (supplemental Table 5). In patients with t(11;14) and those without, median PFS was 24.8 months (95% CI, 8.1-NE) and 22.8 months (95% CI, 9.5-NE), respectively (Figure 2A). The median time to first response was 1.9 months (range, 1.0-13.8) in patients with t(11;14) and 1.7 months (range, 0.9-14.3) in patients without. Median TTP was not reached (95% CI, 12.4-NE) in the t(11;14) subgroup but was 22.8 months (95% CI, 9.5-NE) in the non-t(11;14) subgroup, with estimated 2-year TTP rates of 79% (95% CI, 37-95) and 44% (95% CI, 15-69), respectively. Median DOR was not reached in patients with t(11;14) and was 16.4 months (95% CI, 9.2-NE) in patients without (Table 4; supplemental Figure 3). Of the 5 t(11;14) patients who remained on study for >24 months, all achieved a best response of ≥CR and 4 had ongoing responses as of data cutoff (Figure 3).
BCL2 gene expression was defined as high in 22 patients. Higher ORR, ≥VGPR rate, and MRD negativity rate were observed in BCL2high patients compared with those of BCL2low patients (Table 4). In BCL2high and BCL2low patients, median PFS was 24.7 months (95% CI, 9.0-NE) and 22.8 months (95% CI, 3.7-NE), respectively. Furthermore, 27 patients had t(11;14) or BCL2high gene expression (n = 1 with t(11;14) only; n = 4 with t(11;14) who were not evaluable for BCL2; n = 14 with BCL2high only; n = 8 with both t(11;14) and BCL2high). In this combined subgroup, ORR was 85% (95% CI, 65.4-95.1), ≥VGPR rate was 78% (95% CI, 57.3-90.6), ≥CR rate was 41% (95% CI, 23.0-61.0), and MRD negativity (<10−5) rate was 15% (95% CI, 4.9-34.6). The median PFS was 24.7 months (95% CI, 12.4-NE).
Patients who were PI, IMiD, or double refractory achieved comparable ORRs, ≥VGPR rates, ≥CR rates, and MRD negativity (<10−5) rates (Table 4).
Discussion
Therapeutic advances in RRMM have been paralleled by advances in molecular technologies that have increased understanding of MM initiation and progression.28 Clinical heterogeneity in MM can be attributed, in part, to the molecular variation evidenced among patients, which results in variable outcomes.29,30 Consequently, patient outcomes may be enhanced through biomarker-driven, personalized treatment strategies.28,30 In MM, BCL-2 dependency varies between patients.31,32 Patients with t(11;14) are characterized by greater BCL-2 expression vs other subgroups, resulting in increased BCL-2 dependency and therefore sensitivity to venetoclax.31-33 Preferential BCL-2 dependency and BCL-2 family member expression among patients with MM may represent an avenue for personalized medicine. Therapeutic efficacy of venetoclax in RRMM may be potentiated though treatment strategies that combine venetoclax with other agents that increase BCL-2 dependency. One combinatorial approach was investigated in this phase 2 study with the triplet combination of VenKd for adults with RRMM.
To our knowledge, ours is the first study to date to use this combination. No unexpected changes in PK parameters were observed, and the maximum tolerated dose was not reached. This regimen was well tolerated, and no new or unexpected safety signals were reported. In the BELLINI study, a randomized, double-blind, phase 3 study of venetoclax plus bortezomib/dexamethasone vs placebo plus bortezomib/dexamethasone, higher rates of death and infection-related death were observed in the venetoclax with bortezomib/dexamethasone arm, and increased mortality was observed in patients without t(11;14) and with low BCL2 expression.20 Given the BELLINI findings, antibiotic prophylaxis was implemented in our study in March 2019, at which time enrollment for dose-escalation had ended and was ongoing for expansion. Notably, rates of infection in this study (supplemental Table 4) were similar to those observed in patients treated with venetoclax monotherapy.13 No differences were noted with respect to treatment-emergent deaths in patients, based on t(11;14) status or BCL2 expression.
The safety profile observed in this study was generally consistent with that observed in clinical studies of patients with RRMM treated with carfilzomib monotherapy, in combination with dexamethasone, and the triplet combination of carfilzomib, dexamethasone, and daratumumab.16,26,27,34-37 Similar rates of infection were observed in this study compared with those of carfilzomib combination therapies.16,27,34,35 The safety profile of carfilzomib differs from that of its first-generation predecessor, bortezomib, particularly with respect to cardiovascular AEs.36,38 Rates of grade ≥3 cardiac failure were similar in this study vs carfilzomib combination studies.16,27,34,39 Although rates of cytopenia were higher vs carfilzomib combination studies,16,27,34,35 this finding was not unexpected, given the venetoclax AE profile.13,20 Collectively, these findings suggest that, apart from the expected slight increase in cytopenias given the venetoclax profile, the addition of venetoclax to carfilzomib and dexamethasone may not result in added toxicity.
The study combination demonstrated promising, durable response rates, including MRD negativity, in a refractory patient population. Nearly all patients had received prior treatment with PI, IMiD, or both, and 57%, 71%, and 45% of patients, respectively, were refractory to these agents. Only 1 patient had prior exposure to daratumumab, which was not unexpected. Patients who were PI, IMiD, or double refractory achieved ORR, ≥VGPR rates, and ≥CR rates that were similar to those observed in all patients. Further, the sensitivity of MM cells to venetoclax has been shown to correlate closely with the presence of the t(11;14) translocation,40 which increases the dependency of malignant cells on BCL-2 for survival.13,40 In previous venetoclax monotherapy and combination therapy studies, improved responses to venetoclax were observed in patients with t(11;14) RRMM.13,14,20 Accordingly, in this study, patients with t(11;14) received the most benefit (although the sample size of this subgroup was limited), and of note, a greater proportion of patients with t(11;14) harbored concurrent high-risk cytogenetic abnormalities, including del(17p). Recently, Black or African American patients with t(11;14) MM were shown to have inferior outcomes vs White patients with t(11;14) MM.41-43 Notably, Black patients with MM are less likely to receive triplet therapies or frontline stem cell transplantation,43 the latter of which improves survival in patients with t(11;14).42 The limited number of Black or African American patients enrolled in this study, of which only 3 had t(11;14), precludes assessment of outcomes by race and supports the observed underrepresentation of racial minorities in cancer trials in general.44,45
Further, patients with high vs low BCL2 gene expression and patients with t(11;14) and/or BCL2high gene expression vs all patients showed greater benefit in ORR and ≥VGPR rate. These findings are supported by the BELLINI study, where patients with t(11;14) and/or BCL2high gene expression had a more favorable risk-benefit profile compared with patients with non-t(11;14) and BCL2low gene expression.20 Collectively, these data suggest that a biomarker-driven approach may be appropriate for venetoclax in MM.
Although this study was limited by lack of a randomized design and notwithstanding limitations inherent with cross-trial comparisons, the observed responses compare favorably with those reported in clinical studies of pomalidomide with bortezomib, carfilzomib with dexamethasone, or the triplet combination of carfilzomib, dexamethasone, and daratumumab.16,20,27,34,35,46 The patient population in this study was generally similar to that treated with pomalidomide, bortezomib, and dexamethasone in OPTIMISMM, a randomized phase 3 study, with a few exceptions.46 Specifically, more patients with ISS stage II or III disease were enrolled in this study than in OPTIMISMM (61% vs 47%), had been exposed to fewer prior lines of therapy (median 1 vs 2), and had substantially more PI refractory patients (57% vs 13%).46 Whereas ORRs were similar in this study vs OPTIMISMM (80% vs 82%), a greater proportion of patients achieved ≥CR (41% vs 16%) and PFS was doubled (22.8 months vs 11.2 months), despite enrollment of ∽4 times greater PI-refractory patients in our study.46 Responses also compare favorably with those of randomized clinical studies of carfilzomib combination therapies that included patients refractory to PIs or IMiDs.16,27,34,35 ORR was similar in this study vs carfilzomib combination studies16,27,34,35 (80% vs 63% to 84%), but ≥CR rate (41% vs 7% to 29%) and median PFS were greater (22.8 months vs 11.2-18.7 months). Notably, because this was a dose-escalation study, some patients may have received suboptimal doses of carfilzomib and venetoclax. Nevertheless, the durable responses reported herein warrant further investigation in prospective clinical studies.
In summary, the combination of VenKd was well tolerated and had promising efficacy in patients with RRMM, many of whom had prior exposure to PIs and/or IMiDs, irrespective of t(11;14) status. These findings support the use of venetoclax in novel combinations for RRMM. The strong preliminary responses observed in patients with t(11;14) highlight the utility of venetoclax as a biomarker-driven treatment of this patient population. To further evaluate study combination in this key patient subgroup, the study plans to call for enrollment of ∽65 patients with t(11;14) in an expansion cohort. Patients will be randomly assigned to VenKd vs carfilzomib and dexamethasone. The expansion cohort may deepen understanding of the utility of venetoclax as a biomarker-driven therapy in patients with t(11;14) RRMM.
Supplementary Material
The full-text version of this article contains a data supplement.
Acknowledgments
The authors thank the patients and their families, study coordinators, and support staff. Venetoclax is being developed in a collaboration between AbbVie and Genentech. AbbVie and Genentech sponsored the study and participated in the design, study conduct, collection, analysis, and interpretation of the data, and the writing, review, and approval of the publication. No honoraria or payments were made for authorship. Venetoclax is a BCL-2 inhibitor that is FDA approved for some indications. MM is not an approved indication for treatment with venetoclax.
Medical writing support was provided by Ashley Skorusa and Grace Lewis of Bio Connections, LLC, funded by AbbVie.
Authorship
Contribution: L.J.C., W.-J.H., A.H.S., A.A.M., W.M., J.A.R., O.F.B., S.K.K., and E.A.S. contributed to the conception and design of the study; L.J.C., F.E.D., T.K., A.J., J.L.K., W.-J.H., S.K.K., and E.A.S. contributed to the provision of study materials or patients; L.J.C., A.J., W.-J.H., A.A.M., W.M., J.A.R., and O.F.B. collected and assembled the data; and all authors analyzed and interpreted the data, contributed to writing of the manuscript, and provided final approval of the manuscript.
Conflict-of-interest disclosure: L.J.C. has received honoraria from Amgen, Celgene, and Sanofi and research funding from AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Janssen, and Karyopharm Therapeutics. F.E.D. has received honoraria from Adaptive Biotechnologies; has served in a consultancy or advisory role for Amgen, Bristol-Myers Squibb, Celgene, Janssen, Oncopeptides, Roche, Sanofi, and Takeda; has received travel support from Bristol-Myers Squibb, Celgene, Janssen, Roche, and Takeda; and has received research funding from Bristol-Myers Squibb, Celgene, and Janssen. G.P.M. has stock or other ownership in EI Dupont, Johnson & Johnson, Novartis, and Pfizer. T.K. has received honoraria from Amgen and Celgene and research funding from AbbVie, Amgen, Janssen, and Prothena. A.J. has served in a consultancy/advisory role with honoraria for AbbVie, Amgen, Bristol-Myers Squibb/Celgene, GSK, Janssen, Juno, and Karyopharm. J.L.K. has received honoraria from Tecnofarma; served in a consultancy or advisory role for Amgen, Bristol-Myers Squibb, Celgene, Janssen, Karyopharm Therapeutics, Sanofi, Takeda, Tecnofarma, and TG Therapeutics; has received travel support from Amgen, Bristol-Myers Squibb, Celgene, Janssen, Sanofi, and Takeda; and has received research funding from AbbVie/Genentech, Amgen, Bristol-Myers Squibb, Celgene, Fortis Therapeutics, Janssen, Merck, and Sutro Biopharma. W.-J.H. and M.D. report employment with Genentech/Roche; have stock or other ownership in Roche; and have received travel support from Genentech/Roche. A.H.S., J.A.R., X.Y., A.A.M., W.M., and O.F.B report employment with AbbVie and may hold stock or other options. S.K.K. has served in a consultancy or advisory role for AbbVie, Adaptive Biotechnologies, Amgen, Bluebird Bio, Celgene, Genecentrix, Genentech/Roche, Janssen Oncology, Kite Pharma, Merck, Molecular Partners, Oncopeptides, and Takeda; and has received research funding from AbbVie, Carsgen Therapeutics Ltd, Celgene, Janssen Oncology, Kite Pharma, MedImmune, Merck, Novartis, Roche/Genentech, Sanofi, Takeda, and TeneoBio. E.A.S. has served in consultancy or advisory roles for Amgen, Celgene, Janssen, Novartis, Sanofi, Takeda, and Teva, and has received research funding from AbbVie/Genentech. N.B. declares no competing financial interests.
Correspondence: Luciano J. Costa, University of Alabama at Birmingham, 1720 University Blvd, Birmingham, AL 35294, e-mail: ljcosta@uabmc.edu.
References
- 1.Naymagon L, Abdul-Hay M.. Novel agents in the treatment of multiple myeloma: a review about the future. J Hematol Oncol. 2016;9(1):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moreau P, Attal M, Facon T.. Frontline therapy of multiple myeloma. Blood. 2015;125(20):3076-3084. [DOI] [PubMed] [Google Scholar]
- 3.Ravi P, Kumar SK, Cerhan JR, et al. Defining cure in multiple myeloma: a comparative study of outcomes of young individuals with myeloma and curable hematologic malignancies. Blood Cancer J. 2018;8(3):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chim CS, Kumar SK, Orlowski RZ, et al. Management of relapsed and refractory multiple myeloma: novel agents, antibodies, immunotherapies and beyond [published correction appears in Leukemia. 2019;33(4):1058–1059]. Leukemia. 2018;32(2):252-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar SK, Lee JH, Lahuerta JJ, et al. ; International Myeloma Working Group . Risk of progression and survival in multiple myeloma relapsing after therapy with IMiDs and bortezomib: a multicenter international myeloma working group study [published correction appears in Leukemia. 2012 May;26(5):1153.]. Leukemia. 2012;26(1):149-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Egan JB, Shi CX, Tembe W, et al. Whole-genome sequencing of multiple myeloma from diagnosis to plasma cell leukemia reveals genomic initiating events, evolution, and clonal tides. Blood. 2012;120(5):1060-1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bolli N, Avet-Loiseau H, Wedge DC, et al. Heterogeneity of genomic evolution and mutational profiles in multiple myeloma. Nat Commun. 2014;5(1):2997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lonial S, Lee HC, Badros A, et al. Belantamab mafodotin for relapsed or refractory multiple myeloma (DREAMM-2): a two-arm, randomised, open-label, phase 2 study. Lancet Oncol. 2020;21(2):207-221. [DOI] [PubMed] [Google Scholar]
- 9.Valentin R, Grabow S, Davids MS.. The rise of apoptosis: targeting apoptosis in hematologic malignancies. Blood. 2018;132(12):1248-1264. [DOI] [PubMed] [Google Scholar]
- 10.Kale J, Osterlund EJ, Andrews DW.. BCL-2 family proteins: changing partners in the dance towards death. Cell Death Differ. 2018;25(1):65-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Touzeau C, Maciag P, Amiot M, Moreau P.. Targeting Bcl-2 for the treatment of multiple myeloma. Leukemia. 2018;32(9):1899-1907. [DOI] [PubMed] [Google Scholar]
- 12.Souers AJ, Leverson JD, Boghaert ER, et al. ABT-199, a potent and selective BCL-2 inhibitor, achieves antitumor activity while sparing platelets. Nat Med. 2013;19(2):202-208. [DOI] [PubMed] [Google Scholar]
- 13.Kumar S, Kaufman JL, Gasparetto C, et al. Efficacy of venetoclax as targeted therapy for relapsed/refractory t(11;14) multiple myeloma. Blood. 2017;130(22):2401-2409. [DOI] [PubMed] [Google Scholar]
- 14.Moreau P, Chanan-Khan A, Roberts AW, et al. Promising efficacy and acceptable safety of venetoclax plus bortezomib and dexamethasone in relapsed/refractory MM. Blood. 2017;130(22):2392-2400. [DOI] [PubMed] [Google Scholar]
- 15.Willis SN, Chen L, Dewson G, et al. Proapoptotic Bak is sequestered by Mcl-1 and Bcl-xL, but not Bcl-2, until displaced by BH3-only proteins. Genes Dev. 2005;19(11):1294-1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dimopoulos MA, Moreau P, Palumbo A, et al. ; ENDEAVOR Investigators . Carfilzomib and dexamethasone versus bortezomib and dexamethasone for patients with relapsed or refractory multiple myeloma (ENDEAVOR): a randomised, phase 3, open-label, multicentre study. Lancet Oncol. 2016;17(1):27-38. [DOI] [PubMed] [Google Scholar]
- 17.Ponder KG, Matulis SM, Hitosugi S, et al. Dual inhibition of Mcl-1 by the combination of carfilzomib and TG02 in multiple myeloma. Cancer Biol Ther. 2016;17(7):769-777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matulis SM, Gupta VA, Nooka AK, et al. Dexamethasone treatment promotes Bcl-2 dependence in multiple myeloma resulting in sensitivity to venetoclax. Leukemia. 2016;30(5):1086-1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qin JZ, Ziffra J, Stennett L, et al. Proteasome inhibitors trigger NOXA-mediated apoptosis in melanoma and myeloma cells. Cancer Res. 2005;65(14):6282-6293. [DOI] [PubMed] [Google Scholar]
- 20.Kumar SK, Harrison SJ, Cavo M, et al. Venetoclax or placebo in combination with bortezomib and dexamethasone in patients with relapsed or refractory multiple myeloma (BELLINI): a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2020;21(12):1630-1642. [DOI] [PubMed] [Google Scholar]
- 21.Costa LJ, Derman BA, Bal S, et al. International harmonization in performing and reporting minimal residual disease assessment in multiple myeloma trials. Leukemia. 2021;35(1):18-30. [DOI] [PubMed] [Google Scholar]
- 22.Liu H, Michmerhuizen MJ, Lao Y, et al. Metabolism and disposition of a novel B-cell lymphoma-2 inhibitor venetoclax in humans and characterization of its unusual metabolites. Drug Metab Dispos. 2017;45(3):294-305. [DOI] [PubMed] [Google Scholar]
- 23.Rajkumar SV, Harousseau JL, Durie B, et al. ; International Myeloma Workshop Consensus Panel 1 . Consensus recommendations for the uniform reporting of clinical trials: report of the International Myeloma Workshop Consensus Panel 1. Blood. 2011;117(18):4691-4695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Durie BG, Harousseau JL, Miguel JS, et al. ; International Myeloma Working Group . International uniform response criteria for multiple myeloma [published correction appears in Leukemia. 2006;20(12):2220]. Leukemia. 2006;20(9):1467-1473. [DOI] [PubMed] [Google Scholar]
- 25.Freise KJ, Jones AK, Verdugo ME, Menon RM, Maciag PC, Salem AH.. Moving beyond maximum tolerated dose for targeted oncology drugs: Use of Clinical Utility Index to optimize venetoclax dosage in multiple myeloma patients. Clin Pharmacol Ther. 2017;102(6):970-976. [DOI] [PubMed] [Google Scholar]
- 26.Papadopoulos KP, Siegel DS, Vesole DH, et al. Phase I study of 30-minute infusion of carfilzomib as single agent or in combination with low-dose dexamethasone in patients with relapsed and/or refractory multiple myeloma. J Clin Oncol. 2015;33(7):732-739. [DOI] [PubMed] [Google Scholar]
- 27.Berenson JR, Cartmell A, Bessudo A, et al. CHAMPION-1: a phase 1/2 study of once-weekly carfilzomib and dexamethasone for relapsed or refractory multiple myeloma. Blood. 2016;127(26):3360-3368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pawlyn C, Davies FE.. Toward personalized treatment in multiple myeloma based on molecular characteristics. Blood. 2019;133(7):660-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Mel S, Lim SH, Tung ML, Chng WJ.. Implications of heterogeneity in multiple myeloma. BioMed Res Int. 2014;2014:232546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lohr JG, Stojanov P, Carter SL, et al. ; Multiple Myeloma Research Consortium . Widespread genetic heterogeneity in multiple myeloma: implications for targeted therapy. Cancer Cell. 2014;25(1):91-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Touzeau C, Ryan J, Guerriero J, et al. BH3 profiling identifies heterogeneous dependency on Bcl-2 family members in multiple myeloma and predicts sensitivity to BH3 mimetics. Leukemia. 2016;30(3):761-764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu J, Ross J, Peale FV Jr, et al. A favorable BCL-2 family expression profile may explain the increased susceptibility of the t(11;14) multiple myeloma subgroup to single agent venetoclax [abstract]. Blood. 2016;128(22). Abstract 5613. [Google Scholar]
- 33.Punnoose EA, Leverson JD, Peale F, et al. Expression profile of BCL-2, BCL-XL, and MCL-1 predicts pharmacological response to the BCL-2 selective antagonist venetoclax in multiple myeloma models. Mol Cancer Ther. 2016;15(5):1132-1144. [DOI] [PubMed] [Google Scholar]
- 34.Usmani SZ, Quach H, Mateos M-V, et al. Carfilzomib, dexamethasone, and daratumumab versus carfilzomib and dexamethasone for patients with relapsed or refractory multiple myeloma (CANDOR): results from the randomized, multicentre, open-label, phase 3 study. Lancet. 2020;396(10245):186–197. [DOI] [PubMed] [Google Scholar]
- 35.Moreau P, Mateos MV, Berenson JR, et al. Once weekly versus twice weekly carfilzomib dosing in patients with relapsed and refractory multiple myeloma (A.R.R.O.W.): interim analysis results of a randomised, phase 3 study. Lancet Oncol. 2018;19(7):953-964. [DOI] [PubMed] [Google Scholar]
- 36.Siegel D, Martin T, Nooka A, et al. Integrated safety profile of single-agent carfilzomib: experience from 526 patients enrolled in 4 phase II clinical studies. Haematologica. 2013;98(11):1753-1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lendvai N, Hilden P, Devlin S, et al. A phase 2 single-center study of carfilzomib 56 mg/m2 with or without low-dose dexamethasone in relapsed multiple myeloma. Blood. 2014;124(6):899-906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Groen K, van de Donk N, Stege C, Zweegman S, Nijhof IS.. Carfilzomib for relapsed and refractory multiple myeloma. Cancer Manag Res. 2019;11:2663-2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cornell RF, Ky B, Weiss BM, et al. Prospective study of cardiac events during proteasome inhibitor therapy for relapsed multiple myeloma. J Clin Oncol. 2019;37(22):1946-1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Touzeau C, Dousset C, Le Gouill S, et al. The Bcl-2 specific BH3 mimetic ABT-199: a promising targeted therapy for t(11;14) multiple myeloma. Leukemia. 2014;28(1):210-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gasparetto C, Abonour R, Jagannath S, et al. Impact of t(11;14) on outcomes in African American (AA) and non-AA (NAA) patients (Pts) with newly diagnosed multiple myeloma (NDMM): Connect MM registry [abstract]. J Clin Oncol. 2017;35(15_suppl). Abstract 8023. [Google Scholar]
- 42.Badar T, Hari P, Dávila O, et al. African Americans with translocation t(11;14) have superior survival after autologous hematopoietic cell transplantation for multiple myeloma in comparison with Whites in the United States. Cancer. 2020;127(1):82-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Derman BA, Jasielec J, Langerman SS, Zhang W, Jakubowiak AJ, Chiu BC.. Racial differences in treatment and outcomes in multiple myeloma: a multiple myeloma research foundation analysis. Blood Cancer J. 2020;10(8):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Murthy VH, Krumholz HM, Gross CP.. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004;291(22):2720-2726. [DOI] [PubMed] [Google Scholar]
- 45.Nazha B, Mishra M, Pentz R, Owonikoko TK.. Enrollment of Racial Minorities in Clinical Trials: Old Problem Assumes New Urgency in the Age of Immunotherapy. Am Soc Clin Oncol Educ Book. 2019;39(39):3-10. [DOI] [PubMed] [Google Scholar]
- 46.Richardson PG, Oriol A, Beksac M, et al. ; OPTIMISMM trial investigators . Pomalidomide, bortezomib, and dexamethasone for patients with relapsed or refractory multiple myeloma previously treated with lenalidomide (OPTIMISMM): a randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(6):781-794. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.