Key Points
Platelets exposed to cold temperature generate contractile forces in growing thrombi under shear stress and in a static single-cell assay.
Cold exposure reduces GPVI levels in mouse and human platelets and decreases the response to GPVI agonists before and after transfusion.
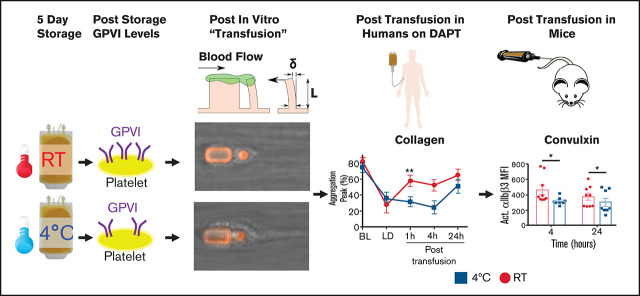
Visual Abstract
Abstract
Platelets are currently stored at room temperature before transfusion to maximize circulation time. This approach has numerous downsides, including limited storage duration, bacterial growth risk, and increased costs. Cold storage could alleviate these problems. However, the functional consequences of cold exposure for platelets are poorly understood. In the present study, we compared the function of cold-stored platelets (CSP) with that of room temperature–stored platelets (RSP) in vitro, in vivo, and posttransfusion. CSP formed larger aggregates under in vitro shear while generating similar contractile forces compared with RSP. We found significantly reduced glycoprotein VI (GPVI) levels after cold exposure of 5 to 7 days. After transfusion into humans, CSP were mostly equivalent to RSP, yet aggregated significantly less to the GPVI agonist collagen. In a mouse model of platelet transfusion, we found a significantly lower response to the GPVI-dependent agonist convulxin and significantly lower GPVI levels on the surface of transfused platelets after cold storage. In summary, our data support an immediate but short-lived benefit of cold storage and highlight the need for thorough investigations of CSP. This trial was registered at www.clinicaltrials.gov as #NCT03787927.
Introduction
Platelets are transfused to prevent and treat bleeding. Standard platelet storage is limited to 5 to 7 days at room temperature (RT; 20-24°C) to limit the risk of sepsis.1,2 As a consequence, they require additional labor and costs resulting from bacterial testing,3 logistical issues with maintaining an adequate supply, and shortages.
Cold-stored platelets (CSP; 1-6°C) were the standard of care in the 1960s and 1970s but were abandoned because the circulation time is severely shortened.4 Nevertheless, storage of platelets at 4°C has potential advantages like prolonged storage times, bacterial growth prevention, and easier transport and storage. Despite the short circulation time, CSP could be beneficial for actively bleeding trauma or surgery patients, improving the availability of RT-stored platelets (RSP) for hematology and oncology patients. Numerous studies of CSP have shown better in vitro function than RSP in a wide range of assays.5-13 These studies have mostly been performed in stored concomitant plasma and thus have neglected the substantial dilution that occurs upon transfusion into humans. This dilution factor likely renders the concomitant plasma irrelevant for stored platelet function in vivo. Cold exposure also elicits specific changes in the platelet cytoskeleton, such as actin filament barbed-end capping, actin polymerization, and de novo nucleation.14 Increased cytosolic calcium and microtubule disintegration accompany the cytoskeletal changes.15 Combined, these phenomena mimic responses to agonists and could prime cold-exposed platelets for immediate activation at sites of vascular injury. However, persistent preactivation could also cause desensitization and loss of efficacy. Therefore, it is unclear whether CSP can contribute to thrombus contraction under physiologic flow or generate forces on a single-cell level.16 Previous studies have examined platelet clot retraction in plasma and whole blood, making it challenging to dissect individual platelet and plasma protein contributions.17-19 Few studies have investigated CSP function after transfusion into humans.20 These studies were predominantly published in the 1970s, and the data are inconclusive.11,20-26 Given the unclear effect transfusion has on stored platelets and the limited posttransfusion human data available, further in vivo investigation of RSP and CSP is urgently needed. If CSP prove effective, a practical application is implementing a dual blood bank inventory, freeing up RSP for prophylactic transfusions and allocating CSP for therapeutic transfusions in actively bleeding patients. Whether CSP have a role in prophylactic transfusions requires additional basic and clinical investigations.
This study addresses the effects of different storage temperatures in state-of-the-art assays while controlling extracellular testing conditions. Furthermore, we evaluate the function of RSP and CSP after transfusion into humans in dual antiplatelet therapy and in untreated mice. Our findings highlight the need for posttransfusion and in vivo data on this product.
Methods
Platelet block and post assay
We collected whole blood and removed platelets by centrifugation. Platelet-poor plasma derived from fresh whole blood was used to dilute the red blood cell–rich sample fraction to yield thrombocytopenic blood. Apheresis platelet-rich plasma (PRP; fresh, RT stored, and cold stored) was added to yield a final target hematocrit of 40% and platelet count of 3 × 1011/L.
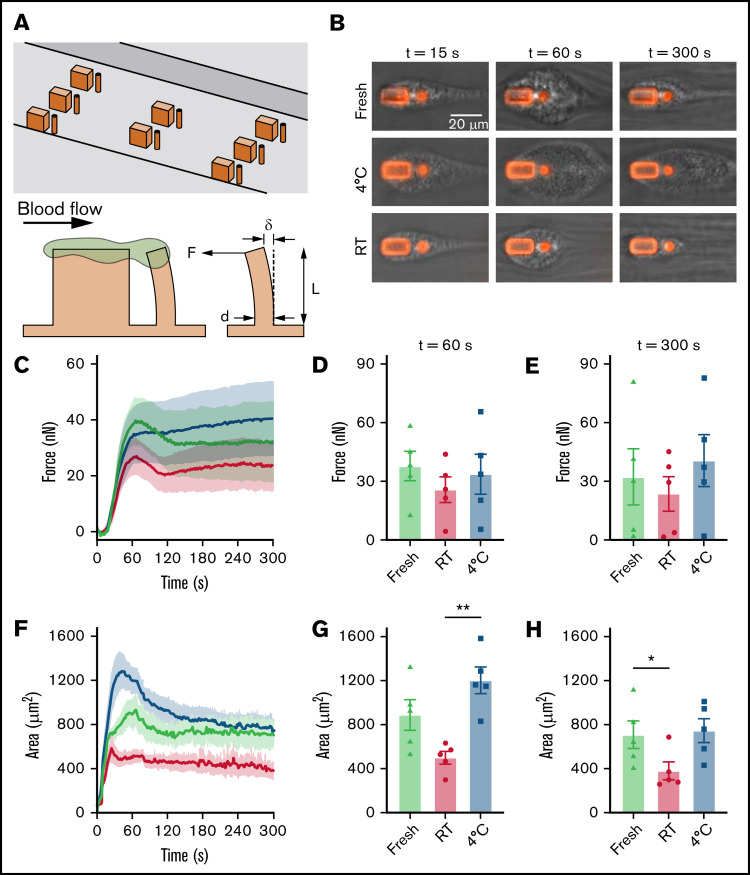
Reconstituted blood was perfused through a microfluidic channel made with polydimethylsiloxane (PDMS; Sylgard 184) with embedded microscale blocks and microposts (Figure 2A) to monitor platelet aggregation and their production of contractile forces.16 Before testing, the microchannels were incubated with rat tail collagen type 1 (200 μg/mL; BD Bioscience) in 0.1 M of acetic acid to support the adhesion and activation of platelets. For testing, a blood sample was flowed through the microfluidic device at a shear rate of 16 000 s−1 using a syringe pump (Harvard Apparatus). Platelets within the blood sample attached initially to the blocks and then aggregated to form platelet-rich plugs that bridged the 9-μm gap with each post. After 15 seconds of flow, the shear rate decreased to 500 s−1 to reduce the aggregation rate and avoid occluding the microchannel with platelets.
Figure 2.
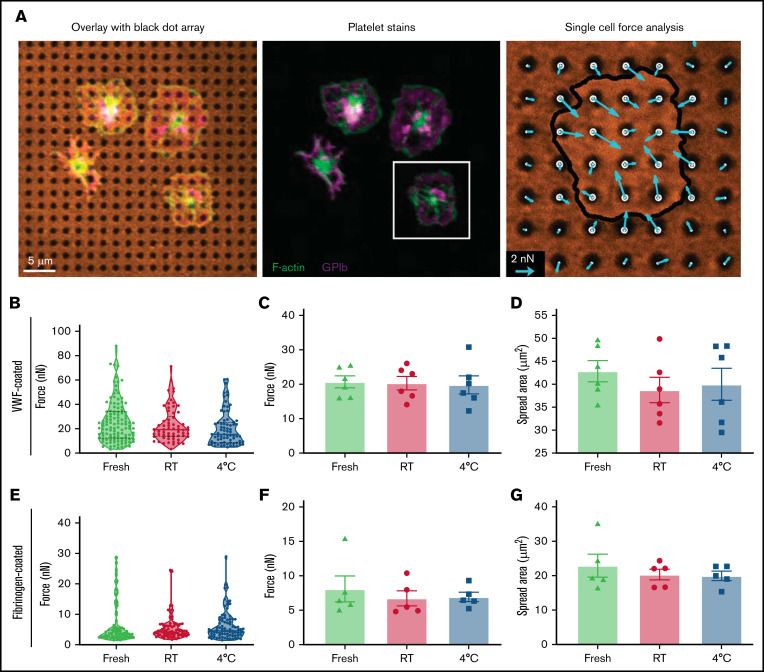
Single-platelet contraction force and spread area. Apheresis platelets were washed and seeded onto flexible PDMS substrates that were printed with an array of black dots to measure traction forces and spread area of individual platelets. (A) Platelets were fixed, stained, and imaged to visualize F-actin (green), GPIb (purple), and the array of black dots (orange). The magnitude and direction of platelet traction forces (blue arrows) were calculated from the displacement of the dots. (B) Traction forces were measured for fresh (green), RT-stored (red), and 4°C-stored (blue) platelets that were seeded onto black dot substrates coated with VWF. Violin plots show data from a representative donor for whom 252 platelets were measured (fresh, n = 117; RT stored, n = 73; 4°C stored, n = 62). (C) Average traction forces per platelet were measured for 6 donors, and no statistically significant difference was observed between fresh (green triangles), RT-stored (red circles), and 4°C-stored (blue squares) platelets. (D) Average spread area of platelets on VWF-coated black dots was measured for each donor, and no significant difference was observed between the conditions. (E) Traction forces were measured for fresh (green), RT-stored (red), and 4°C-stored (blue) platelets on fibrinogen-coated black dots. Violin plots show data from a representative donor for whom 242 platelets were measured (fresh, n = 81; RT stored, n = 84; 4°C stored, n = 77). (F-G) Average traction forces (F) and average spread area (G) of platelets on fibrinogen-coated black dots were measured for 5 donors, and no significant difference was observed between conditions.
The size of the aggregates and deflection of the post as a result of platelet forces were recorded every 2 seconds over 5 minutes using phase and fluorescent timelapse images obtained on a Nikon Eclipse Ti-E inverted microscope with a 40× objective. The images were then quantified postexperiment using custom MATLAB scripts. The force that aggregated platelets produced was calculated using Hooke’s law (data supplement). On day 5 of storage, this protocol was repeated with fresh thrombocytopenic whole blood derived from the same donor and PRP from apheresis platelets stored at room temperature or 4°C.
Single-platelet contractile force assay
We used a microcontact-printed, reference-free traction force microscopy approach (Kevin M. Beussman and M.Y.M., manuscript in preparation). Specifically, a PDMS stamp for microcontact printing was created by casting Sylgard 184 (prepared at a 10:1 ratio) against a silicon master with an array of circular features arranged in an orthogonal lattice. A solution of 2.5 μg/mL of Alexa-Fluor 594–conjugated bovine serum albumin (BSA) was pipetted onto the surface of the PDMS stamps and allowed to adsorb for 1 hour. The stamp was then brought into contact with a polyvinyl alcohol film to transfer the fluorescent bovine serum albumin pattern onto the film. Subsequently, the polyvinyl alcohol film was applied to the surface of a PDMS substrate made with 95% Sylgard 527 (prepared at a 1:1 ratio) and 5% Sylgard 184 (prepared at a 10:1 ratio), which produced substrates with a stiffness of 12 kPa.27 The process of microcontact printing resulted in a flexible substrate with a contiguous fluorescent coating containing an orthogonal array of circular regions that were 1 μm in diameter and 2 μm in spacing and lacked fluorescence (termed black dots). The substrates with black dots were treated with 5 μg/mL of von Willebrand factor (VWF; Haematological Technologies) or 5 mg/mL of fibrinogen (Sigma Aldrich) for 1 hour at RT to promote platelet adhesion.
Platelets were obtained, stored, and washed (described in detail in the data supplement). Platelets were further diluted in Tyrode’s buffer and seeded at 2.5 × 1010/L onto VWF-coated black dots and at 5 × 1010/L onto fibrinogen-coated black dots to ensure there was separation between the platelets. After 10 minutes of incubation to allow for platelet adhesion, the black dots were gently rinsed with phosphate-buffered saline to remove the unbound platelets. The substrates were then submerged into fresh Tyrode’s buffer for 30 minutes to allow the platelets to spread and generate traction forces. Platelets on the black dots were fixed with 4% paraformaldehyde for 20 minutes and permeabilized with 0.1% Triton X-100 for 20 minutes. Platelet glycoprotein Ib (GPIb) was labeled with a CD42b monoclonal antibody, clone SZ2 (Life Technologies), and a goat anti-mouse immunoglobulin G secondary antibody (Life Technologies). Platelet F-actin was labeled with phalloidin (Life Technologies). Black dots were mounted on glass coverslips using Fluoromount-G mounting medium (Invitrogen) and imaged with confocal microscopy using a Nikon A1R confocal microscope with a 60× oil objective. Single-platelet traction forces were calculated from black dot displacement using regularized Fourier transform traction cytometry. Single-platelet forces were measured in 6 donors treated with VWF and 5 donors treated with fibrinogen. For each donor, each black dot treatment (VWF and fibrinogen), and each condition (fresh, cold stored, and RT stored), an average of 88 platelets were measured for a total of 2905 platelets included in this study.
Healthy human participant research
The Western Institutional Review Board–Copernicus Institutional Review Board Group approved our research, and all human participants provided written informed consent. We conducted the study following the Declaration of Helsinki. All authors had access to primary clinical trial data.
Healthy human participant demographics and recruitment
Fourteen participants were enrolled in the study. Six had to end their participation early for different reasons (supplemental Figure 1). Eight had evaluable data for platelet transfusions. One participant did not complete the RT storage arm because of quality control failure (supplemental Figure 1). Overall, the mean age was 28 years (interquartile range, 24-32 years), 2 participants were female (25%), the mean height was 173 cm (standard deviation [SD], ±9.3 cm), the mean weight was 70.6 kg (SD, ±4.7 kg), and the mean body mass index was 23.8 kg/m2 (SD, ±2.6 kg/m2).
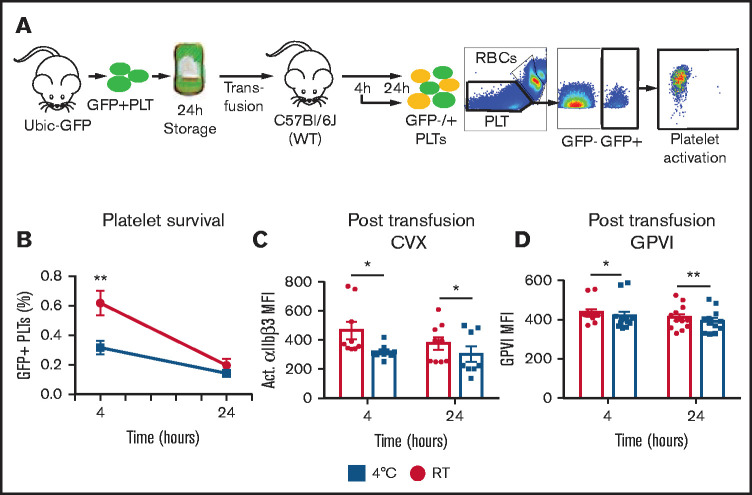
In vivo survival and function of transfused mouse platelets
We collected green fluorescent protein (GFP)–positive whole blood from UbiC-GFP mice in acid citrate dextrose solution A via retroorbital bleeding. PRP was isolated from whole blood and stored at RT or 4°C for 24 hours before transfusion. After platelet concentrations were adjusted to 2 × 1011 platelets per L, we transfused GFP+ platelets into wild-type recipients via tail-vein injection. After transfusion, blood samples were collected from each recipient at 4 and 24 hours. These samples were gated for GFP+ platelets. The transfused platelet population was identified as GFP+ and the endogenous population as GFP−. GPVI levels were evaluated by JAQ-1 antibody binding with an immunoglobulin G–phycoerythrin secondary antibody. The samples were analyzed for activation of mouse αIIbβ3 using Jon/A-phycoerythrin antibody to measure the activation level. We acquired all posttransfusion recovery data, and functional test data were obtained by flow cytometry.
Statistical analysis
Results are reported as mean ± standard error of the mean. Statistical significance was assessed by either paired 2-tailed Student t test or analysis of variance with Tukey correction, as appropriate. A P value ≤.05 was considered significant. The analyses were performed with Prism (GraphPad, La Jolla, CA).
Results
Poststorage platelet in vitro function
Exposure of platelets to cold induces actin assembly and initiates shape change, resembling the activation response to agonists like thrombin, adenosine 5′-diphosphate (ADP), and collagen.14 To test if these changes affect thrombus formation and clot retraction in flowing blood, we used a microfluidic collagen-coated block and post assay to quantify aggregation and contractile force generation within a growing thrombus (Figure 1A; supplemental Videos 1-3).16 In this assay, platelets in a small sample of blood are stimulated to attach and aggregate to form a platelet-rich plug by a local gradient in the shear rate caused by the block and post. Within a few seconds, a plug is typically large enough to bridge the gap between the block and post, and thus, the contractile force produced by the platelets can be measured by how far the post is deflected toward the block. We stored platelets collected by apheresis for 5 days at RT, as per current clinical practice, or at 4°C, as previously described,28 and added them to freshly drawn red blood cells and plasma to reconstitute a whole-blood sample. CSP reconstituted in fresh platelet–depleted blood samples adhered readily to the block and post and generated contractile forces that were statistically comparable to those of samples with freshly drawn PRP or RSP (Figure 1B-E). CSP formed significantly larger aggregates than RSP at the early time point (60 seconds; Figure 1B,F-G). However, after 300 seconds, the size of the CSP aggregates decreased, and they were statistically similar to RSP. RSP samples formed consistently smaller aggregates over time than those from fresh blood samples, and the difference between RSP and fresh samples was significant at 300 seconds (Figure 1H). CSP formed larger aggregates after 60 seconds, but this did not increase force generation, suggesting individual CSP were generating lower forces. To further evaluate this possibility, we used a novel single-platelet force assay that measures single-platelet contractile traction forces by quantifying the deformation of dots in a fluorescent array coated with either VWF or fibrinogen (Figure 2A). Similar to what we observed in measuring force generation by aggregates formed under flow, individual platelets treated with VWF or fibrinogen were statistically similar among freshly drawn platelets, RSP, and CSP (Figure 2B-C,E-F). These results indicate that the contractile function of platelets might be independent of the storage condition. We noted that traction forces for freshly drawn platelets, RSP, and CSP were more than twofold higher with VWF coating vs fibrinogen coating. On the basis of these results, we concluded that CSP have a higher propensity for shear-induced aggregation than RSP, and CSP can generate contractile forces similar to those of freshly drawn platelets and RSP.
Figure 1.
Platelet aggregate force and area in response to shear flow. Reconstituted whole-blood samples with fresh (green triangle), RT-stored (red circles), or 4°C-stored (blue squares) apheresis platelets were perfused through a microfluidic device to measure the force and area of platelet aggregates formed under shear flow. (A) Each microfluidic channel contains multiple sets of block and post force sensors. While under flow, platelets attach and aggregate to form a plug-like structure (green) that encapsulates the block and post. Aggregated platelets are able to produce contractile forces (F) that pull the flexible post toward the rigid block. Force is calculated from displacement of the tip of the post (δ) using Hooke’s law: F = k δ, where k = 3π E d4/64 L3, and E is the modulus of elasticity, d is the diameter, and L is the length of the post. (B) Representative images of platelet aggregate area 15, 60, and 300 seconds after blood enters the channel. (C) Mean force of the platelet aggregates over time (n = 5; shaded regions represent standard error of the mean [SEM]). (D) Force of the platelet aggregates at 60 seconds (n = 5; shown as mean ± SEM). (E) Force of the platelet aggregates at 300 seconds (n = 5; shown as mean ± SEM). (F) Mean area of the platelet aggregates over time (n = 5; shaded regions represent SEM). (G) Area of the platelet aggregates at 60 seconds (n = 5; shown as mean ± SEM). (H) Area of the platelet aggregates at 300 seconds (n = 5; shown as mean ± SEM). *P = .0103 for fresh and RT (H) , **P = .0032 for 4°C and RT (G).
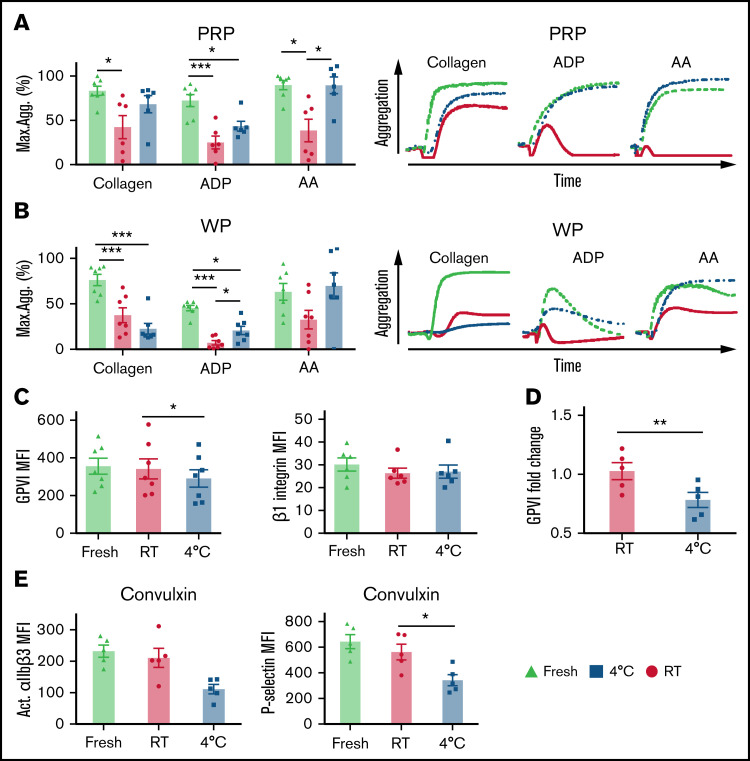
Because we observed larger aggregates under flow with a collagen-coated block and post, we tested the ability of CSP and RSP to aggregate in response to collagen. We observed a trend toward increased aggregation when CSP in concomitant plasma were stimulated with collagen (Figure 2A), in agreement with previously published data.6,28,29 However, testing platelets in their stored plasma disregards the large degree of dilution that platelets undergo upon transfusion into the entire blood volume of the recipient. Surprisingly, when testing washed platelets stimulated with collagen, the trend toward better aggregation with CSP compared with RSP was reversed, and there was a clear trend toward more aggregation with RSP (Figure 3B). This reversal was not seen when we stimulated platelets with ADP and arachidonic acid (Figure 3A-B). Collagen is known to activate platelets mainly through GPVI and αIIβ1. Therefore, we tested for expression levels of both receptors before and after storage. We found a significant reduction in GPVI levels after storage in CSP vs RSP, whereas αIIβ1 integrin levels remained unchanged (Figure 3C). Next, we tested for GPVI levels by liquid chromatography–mass spectrometry on platelets obtained from a separate cohort to confirm these findings. Indeed, we found significantly lower GPVI levels in CSP than in RSP (Figure 3D). To evaluate functional differences in this cohort, we diluted platelets with separately stored plasma from the same donors. We tested for activated αIIbβ3 integrin and P-selectin expression by flow cytometry after adding the GPVI-activating snake venom convulxin. Similar to our aggregometry findings with washed platelets, we found lower integrin activation and α-granule secretion in CSP than in RSP (Figure 3E).
Figure 3.
Platelet storage temperature and response to agonists in PRP and washed platelets (WPs). We obtained human platelets by apheresis and used platelets either fresh (green triangles) or stored for 5 days at either 4°C (blue squares) or 22°C (RT; red circles). Aggregation was induced by stimulation with 5 μg/mL of collagen, 20 μM of ADP, or 0.5 mM of arachidonic acid (AA; shown as maximum aggregation; mean ± standard error of the mean [SEM]; n = 6-7). (A) PRP: collagen, ADP, and AA (left) and representative aggregation traces (right). (B) WPs: collagen, ADP, and AA (left) and representative aggregation traces (right). (C) GPVI levels on platelets determined by flow cytometry with fluorochrome-conjugated anti-GPVI antibody (n = 7; left), And β1 integrin levels on platelets determined by flow cytometry with fluorochrome-conjugated β1 antibody (n = 7; right). (D) Separate cohort of healthy volunteers, whose platelets were stored for 7 days at RT or 4°C under the same conditions as described for the original cohort. GPVI levels were determined using liquid chromatography–tandem mass spectrometry. Results are shown as fold change from baseline (fresh; n = 5). (E) PRP was diluted with separately stored plasma and stimulated with 100 ng/mL of convulxin. We stained with antibodies against activated integrin (PAC-1) and P-selectin (anti-CD62P; shown as change in mean fluorescence intensity [MFI] ± SEM from unstimulated; n = 5). *P < .5, **P < .01, ***P < .001. ns, not significant.
Another critical aspect of platelet function is the ability to promote coagulation in a growing thrombus. Regardless of temperature, storage led to a trend for more thrombin generation and a shorter time to peak thrombin concentration than fresh platelets (supplemental Figure 4), likely because of increased phosphatidylserine exposure.28 When replacing the stored supernatant plasma with separately stored 4°C plasma, CSP generated more thrombin than RSP.
CSP function in humans
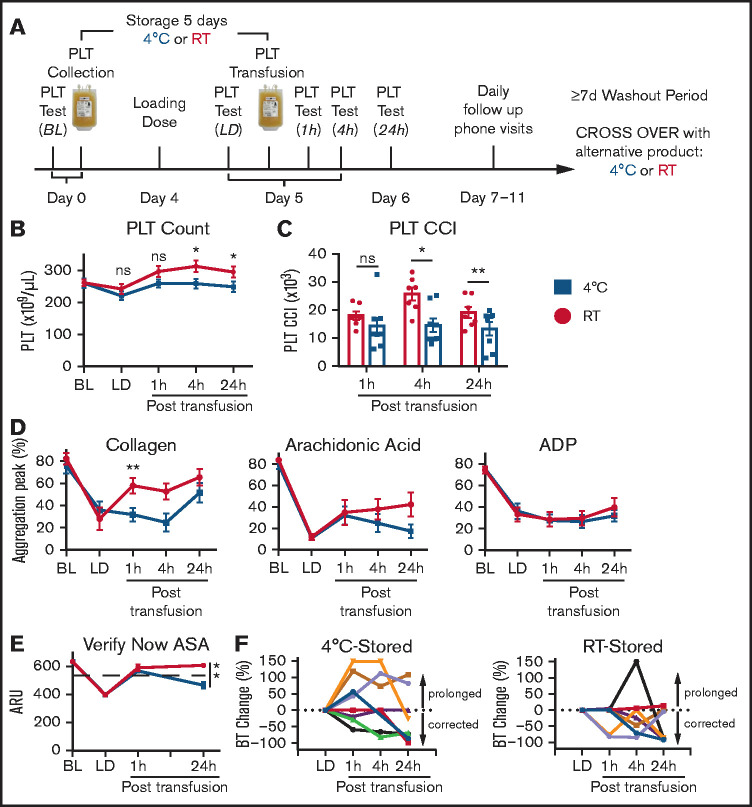
To test if the loss of GPVI during cold storage led to measurable differences after transfusion in humans, we included 8 healthy human volunteers in a randomized crossover study (described in detail in “Methods”). In brief, we collected apheresis platelets for autologous transfusion. Platelets were stored at either 4°C (CSP) or 22°C (RSP), based on randomization. After 4 days of platelet storage, participants received a loading dose of acetylsalicylic acid (ASA) and clopidogrel and 12 to 24 hours later were transfused the entire unit of stored platelets. We assessed the efficacy of transfusion with platelet function tests at baseline, immediately before transfusion (after antiplatelet drug dosing), and 3 times after transfusion. A washout period of at least 7 days between the first and second rounds ensured clearance of previously transfused platelets and antiplatelet therapy; then, an identical experiment was performed with autologous platelets stored under the alternative condition (supplemental Figure 1; Figure 4A).
Figure 4.
Posttransfusion and in vivo platelet (PLT) function in healthy humans. (A) Time course of the healthy human crossover study, including baseline (BL) PLT test; PLT function 24 hours after loading dose (LD) with 325 mg of ASA and 600 mg of clopidogrel; and 1-, 4-, and 24-hour PLT function tests posttransfusion. (B) Absolute PLT counts at different time points of the study from individuals during RT-stored PLT transfusion round (red circles) and 4°C-stored PLT transfusion round (blue squares; n = 7-8; shown as mean ± standard error of the mean [SEM]). (C) Corrected count increments at posttransfusion time points (n = 7-8; shown as mean ± SEM). (D) PLTs were washed before assessment by light transmission aggregometry. Platelets were stimulated with 20 μg/mL of collagen, 20 mM of ADP, and 0.5 mM of arachidonic acid (n = 7-8; shown as mean ± SEM of maximum aggregation). (E) PLT reactivity tested by Verify NOW for ASA (aspirin reaction units [ARUs]; n = 7-8; shown as mean ± SEM). (F) Individual responses of participants to autologous transfusion, after LD (normalized to 0) and at 1, 4, and 24 hours posttransfusion (shown as percentage change from bleeding LD value; negative values indicate shortening of bleeding time [BT; ie, correction of prolonged BT], and positive values indicate prolongation of bleeding time [ie, worsening of prolonged BT]). Responses after transfusion of cold-stored autologous units (4°C stored; n = 8; left), and responses after transfusion of RT-stored autologous units (RT stored; n = 7; right). *P = .0110 (4-hour time point) and P = .0154 (24-hour time point) (B) and P = .015 (4-hour time point) and P = .0098 (24-hour time point) (C), **P = .0088 (D) and P = .0018 (E). CCI, corrected count increment; ns, not significant.
Platelet transfusion parameters
Platelet counts decreased in all participants after platelet collection (Figure 4B). The absolute platelet counts and the corrected count increments were significantly lower in the CSP transfusion arm after 4 and 24 hours (Figure 4B-C). More information about the transfusion sequence and number of transfused platelets is provided in supplemental Figure 2.
Platelet function testing after transfusion
Because our primary concern was that reduced GPVI levels would lead to reduced response to collagen after transfusion, we isolated and washed platelets from the transfusion recipients. We adjusted the platelet counts and stimulated with collagen. Indeed, we found significantly more aggregation after transfusion of RSP vs CSP, confirming that the loss of GPVI had measurable effects on platelet function after transfusion (Figure 4D). We tested with pathway-specific agonists to gather further information about CSP function in volunteers receiving dual antiplatelet therapy. Arachidonic acid showed an increase in aggregation 1 hour after transfusion of both products compared with post–loading dose levels and a trend toward a reduced aggregation response in the cold-stored group at the 4- and 24-hour time points (Figure 4D). No significant differences between CSP and RSP or evidence of reversal of clopidogrel were seen after stimulation with ADP (Figure 4D; supplemental Figure 3D). To confirm these findings in whole blood, we use the αIIbβ3 integrin activation–based point-of-care assay Verify NOW. One hour after transfusion, we observed reversal of ASA with both CSP and RSP (Figure 4E). After 24 hours, ASA reaction units were significantly lower in the cold-stored group, suggesting the reappearance of ASA inhibition (Figure 4E). We found a trend toward better platelet function after transfusion with RSP in other assays, including a shorter bleeding time at the 1-hour posttransfusion time point, but none of these findings were statistically significant (supplemental Figure 3A-E). Because bleeding time varies among individuals, we normalized the values after the loading dose (Figure 4F) and calculated the change as a percentage for posttransfusion time points. A majority of participants who received RSP showed improvement or no change. In contrast, 50% of CSP recipients showed further bleeding time prolongation (Figure 4F).
Evaluation of mouse platelet GPVI expression and function after transfusion
Our human data suggest that GPVI levels of stored platelets remain reduced after transfusion, without recovery of function or receptor level normalization. However, the study in humans did not allow us to distinguish between transfused (stored) and endogenous platelets. To investigate this further in a living organism without dual antiplatelet therapy, we used a mouse model to track transfused platelets. We obtained and stored platelets from UBiC-GFP mice that have GFP fused to ubiquitin. After transfusion of GFP+ platelets into WT C57BL6/J mice, we obtained blood samples to assess GFP+ platelets and their survival (Figure 5A-B). We tested platelet function by flow cytometry with an activation-specific antibody to αIIbβ3 after stimulation with the GPVI agonist convulxin. Similar to our findings in humans, the αIIbβ3 integrin activation was lower in CSP than RSP posttransfusion (Figure 5C). Consistent with these findings, GPVI levels of CSP were significantly lower than those of RSP after transfusion (Figure 5D).
Figure 5.
Stored platelet (PLT) posttransfusion function in mice. (A) Outline of the mouse PLT transfusion model (details provided in “Methods”). (B) PLT in vivo survival after storage for 24 hours at either RT (red circles) or 4°C (blue squares; n = 9). (C) αIIbβ3 integrin activation in whole blood 4 and 24 hours after PLT transfusion with either 24-hour RT- (red circles) or 4°C-stored (blue squares) PLTs after stimulation with 100 nM of convulxin (n = 9; shown as mean fluorescence intensity [MFI] ± standard error of the mean [SEM] of Jon/A antibody binding). (D) GPVI expression 4 and 24 hours after transfusion of either 24-hour RT- (red circles) or 4°C-stored (blue squares) PLTs (n = 9; shown as MFI ± SEM of JAQ-1 with goat anti-rat immunoglobulin G–phycoerythrin secondary antibody). *P = .032 (4 hours) (C) and P = .038 (4 hours) (D), **P = .001 (4 hours: RT vs 4°C) (B), P = .012 (24 hours) (C), and P = .008 (24 hours) (D). CVX, convulxin; RBC, red blood cell; WT, wild type.
Discussion
Our study is the first to identify CSP as force-generating contributors in growing thrombi under flow and on a single-cell level. Using clot retraction assays, other groups have examined the function of CSP and reported contradictory results.8,30-32 Plasma factors like thrombin or fibrin generation likely obfuscated the contribution of platelets in these studies. Also, conventional clot retraction assays do not take adhesion or thrombus growth under flow into account. Interestingly, in our assay, the thrombus size was significantly larger with CSP than with RSP, but we did not observe more force generation. This finding could indicate that cold-induced αIIbβ3 preactivation effectively mediates larger, shear-resistant, fibrinogen-dependent platelet-to-platelet aggregates instead of passive agglutination. However, it is unclear why this was not followed by increased thrombus contraction strength. An advantage of our study is that we tested platelets with minimal storage-related plasma factors and on a single-platelet level. However, the spread of data, especially for fresh platelet and CSP force generation, is remarkable and highlights the need to better understand donor-to-donor variability.
Our crossover study in healthy humans shows that CSP show an immediate ASA-reversing effect after transfusion into healthy humans. Although the impact of RSP lasted >24 hours, the inhibition reappeared 24 hours after CSP transfusion. This reappearance of inhibition with CSP indicates that endogenous platelet production (48 hours after antiplatelet drug dosing) was not sufficient to overcome the effect of dual antiplatelet therapy and therefore also serves as an internal no-transfusion control. We doubt the lower platelet count in the recipient after CSP transfusion per se was responsible for this effect, because we observed this phenomenon in whole blood and washed platelets with adjusted platelet counts. A pilot trial in patients undergoing cardiac surgery did not find significant chest tube output differences between RSP and CSP (both stored in platelet additive solution E [PAS-E] instead of 100% plasma).26 Storing CSP in PAS-E only led to a small and nonsignificant reduction in GPVI levels.33 Taken together with our study results, this may suggest that PAS-E is a preferable storage solution for CSP, although more studies in humans are needed to investigate this further. One previous study tested 100% plasma-stored CSP in healthy human participants receiving aspirin and clopidogrel. The authors stored platelets for a shorter period (72 hours) and used bleeding time as the only readout.34 Unsurprisingly, and very similar to our absolute bleeding time results, they did not observe any significant differences between CSP and RSP. In our study, 50% of the CSP recipients showed a bleeding time prolongation after transfusion, which could hint at a possible disadvantage of this product. Besides apparent efficacy in overcoming some antiplatelet therapy effects, none of our different posttransfusion assays showed any advantage of CSP relative to RSP at any time point after transfusion. These results contradict our and others’ previously published in vitro results.5-13
In fact, our data show detrimental effects of cold storage. GPVI receptor levels on CSP were reduced, and we observed diminished responses to GPVI agonists pre- and posttransfusion in humans and mice. Our group and others recently observed more collagen-induced aggregation with CSP than RSP with concomitant plasma. It is unclear how the stored plasma supernatant improves GPVI function in CSP. There are reports that GPVI expression levels vary by approximately ∼1.5-fold among healthy human donors.35 GPVI function is preserved even at much lower levels than those observed in our study.35 However, the authors tested fresh and otherwise functional platelets at optimized conditions. The loss of GPVI in our study has to be seen in the platelet storage lesion context. Other unfavorable storage-related factors lead to dysfunctional platelets, and any loss of GPVI is likely exacerbated.35,36 In our human study, the participants’ endogenous platelet population was rendered dysfunctional by dual antiplatelet therapy. Thus, the antiplatelet therapy reduced the ability of the endogenous platelets to overcome the combined effect of storage lesion and loss of GPVI in transfused platelets. Nevertheless, our findings are relevant, because CSP are intended to be transfused into actively bleeding patient populations with known endogenous platelet defects, like surgery patients after cardiopulmonary bypass and trauma patients.37 We were able to reproduce our findings of decreased GPVI-mediated platelet function with CSP in a mouse transfusion model without antiplatelet therapy using the more potent agonist convulxin to stimulate platelets after transfusion. Beyond αIIbβ3 integrin activation, CSP generated more thrombin than RSP, likely mediated by phosphatidylserine-positive procoagulant CSP and microparticles. When procoagulant CSP interact with vascular injury sites, they could promote coagulation locally. Evidence supporting this mechanism has been reported by other groups.8,13 This provides a possible alternative mechanism for how CSP could compensate for platelet receptor deficiencies in actively bleeding patients.
In the contractile force flow assay with a collagen-coated block and post, we did not observe significantly different forces between RSP and CSP, even though we replaced most storage plasma with fresh plasma. The presence of VWF and its ability to adhere to collagen and platelets likely helped to overcome the effect of low GPVI levels on CSP in this assay. Whether the same is true in actively bleeding humans remains to be investigated. This mechanistic difference could explain the lack of force increase in CSP, despite larger aggregates, although this warrants further investigation. It is currently unclear how platelets lose GPVI from their membranes during cold storage. Previous studies have shown that it can be cleaved by ADAM 10/17 or taken up by endocytosis.38-40 One study observed cleavage of GPVI during RT storage.41 Enzymatic activity is likely reduced at 4°C, making cleavage as the primary mechanism unlikely. In a previous study, we saw more microparticles in CSP than RSP.28 This suggests that loss of GPVI by membrane microvesicles may be responsible for the findings in the current study. Although we show GPVI levels are essential for CSP function, we make no claim that loss of GPVI affected platelet clearance. Other groups have identified different CSP clearance mechanisms.42-44
In summary, our study is the first to provide a thorough assessment of the contractile function and the pre- and posttransfusion functions of CSP compared with the current clinical standard. Importantly, clinical trials are required to test the efficacy of CSP in actively bleeding patients.
Supplementary Material
The full-text version of this article contains a data supplement.
Acknowledgments
The authors thank Renetta Stevens and Tena Petersen for administrative support.
This study was funded by the National Institutes of Health (1R01HL153072-01), the American Society of Hematology Scholar Award, and the National Blood Foundation (Early Career Award) (M.S.). The bleeding time templates were a gift provided by Dr. Sherrill Slichter and were originally manufactured by the University of Washington Medical Center workshop.
Authorship
Contribution: J.M. recruited participants, performed apheresis collections, performed experiments, analyzed data, and helped write the manuscript; S.L.B., A.M.O., M.Y.M., C.U., D.B., J.R.F., L.F., and K.H. performed experiments, analyzed data, and helped write the manuscript; J.C. and B.O. recruited participants, performed apheresis collections, and performed platelet transfusions; Y.W. and Y.S. performed experiments; X.F., J.-F.D., and N.J.S. designed experiments, analyzed data, and helped write the manuscript; and M.S. designed the study, reviewed and analyzed data, and wrote a first draft of the manuscript.
Conflict-of-interest disclosure: N.J.S. is a cofounder and board member of and has equity in Stasys Medical Corporation and is a scientific advisor for and has equity in Nanosurface Biomedical, Inc. M.S. has received research funding from Cerus. The remaining authors declare no competing financial interests.
Correspondence: Moritz Stolla, Bloodworks Northwest Research Institute, 1551 Eastlake Ave, Suite 100, Seattle, WA 98102; e-mail: mstolla@bloodworksnw.org.
References
- 1.US Food and Drug Administration. Fatalities reported to FDA following blood collection and transfusion: annual summary for fiscal year 2017. https://www.fda.gov/media/124796/download. Accessed 19 September 2019.
- 2.Dumont LJ, Kleinman S, Murphy JR, et al. Screening of single-donor apheresis platelets for bacterial contamination: the PASSPORT study results. Transfusion. 2010;50(3):589-599. [DOI] [PubMed] [Google Scholar]
- 3.US Food and Drug Administration. Bacterial risk control strategies for blood collection establishments and transfusion services to enhance the safety and availability of platelets for transfusion. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/bacterial-risk-control-strategies-blood-collection-establishments-and-transfusion-services-enhance. Accessed 18 September 2019.
- 4.Murphy S, Gardner FH. Effect of storage temperature on maintenance of platelet viability—deleterious effect of refrigerated storage. N Engl J Med. 1969;280(20):1094-1098. [DOI] [PubMed] [Google Scholar]
- 5.Getz TM, Montgomery RK, Bynum JA, Aden JK, Pidcoke HF, Cap AP. Storage of platelets at 4°C in platelet additive solutions prevents aggregate formation and preserves platelet functional responses. Transfusion. 2016;56(6):1320-1328. [DOI] [PubMed] [Google Scholar]
- 6.Reddoch KM, Pidcoke HF, Montgomery RK, et al. Hemostatic function of apheresis platelets stored at 4°C and 22°C. Shock. 2014;41(suppl 1):54-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pidcoke HF, Cap AP. Refrigerated platelets for the treatment of acute bleeding: a review of the literature and reexamination of current standards: reply. Shock. 2015;43(3):298-299. [DOI] [PubMed] [Google Scholar]
- 8.Nair PM, Pidcoke HF, Cap AP, Ramasubramanian AK. Effect of cold storage on shear-induced platelet aggregation and clot strength. J Trauma Acute Care Surg. 2014;77(3 suppl 2):S88-S93. [DOI] [PubMed] [Google Scholar]
- 9.Montgomery RK, Reddoch KM, Evani SJ, Cap AP, Ramasubramanian AK. Enhanced shear-induced platelet aggregation due to low-temperature storage. Transfusion. 2013;53(7):1520-1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reddoch KM, Montgomery RK, Rodriguez AC, et al. Endothelium-derived inhibitors efficiently attenuate the aggregation and adhesion responses of refrigerated platelets. Shock. 2016;45(2):220-227. [DOI] [PubMed] [Google Scholar]
- 11.Becker GA, Tuccelli M, Kunicki T, Chalos MK, Aster RH. Studies of platelet concentrates stored at 22 C and 4 C. Transfusion. 1973;13(2):61-68. [DOI] [PubMed] [Google Scholar]
- 12.Johnson L, Tan S, Wood B, Davis A, Marks DC. Refrigeration and cryopreservation of platelets differentially affect platelet metabolism and function: a comparison with conventional platelet storage conditions. Transfusion. 2016;56(7):1807-1818. [DOI] [PubMed] [Google Scholar]
- 13.Six KR, Devloo R, Compernolle V, Feys HB. Impact of cold storage on platelets treated with Intercept pathogen inactivation. Transfusion. 2019;59(8):2662-2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffmeister KM, Falet H, Toker A, Barkalow KL, Stossel TP, Hartwig JH. Mechanisms of cold-induced platelet actin assembly. J Biol Chem. 2001;276(27):24751-24759. [DOI] [PubMed] [Google Scholar]
- 15.Winokur R, Hartwig JH. Mechanism of shape change in chilled human platelets. Blood. 1995;85(7):1796-1804. [PubMed] [Google Scholar]
- 16.Ting LH, Feghhi S, Taparia N, et al. Contractile forces in platelet aggregates under microfluidic shear gradients reflect platelet inhibition and bleeding risk. Nat Commun. 2019;10(1):1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carr ME Jr, Zekert SL. Measurement of platelet-mediated force development during plasma clot formation. Am J Med Sci. 1991;302(1):13-18. [DOI] [PubMed] [Google Scholar]
- 18.Jen CJ, McIntire LV. The structural properties and contractile force of a clot. Cell Motil. 1982;2(5):445-455. [DOI] [PubMed] [Google Scholar]
- 19.Cohen I, De Vries A. Platelet contractile regulation in an isometric system. Nature. 1973;246(5427):36-37. [DOI] [PubMed] [Google Scholar]
- 20.Mack JP, Miles J, Stolla M. Cold-stored platelets: review of studies in humans. Transfus Med Rev. 2020;34(4):221-226. [DOI] [PubMed] [Google Scholar]
- 21.Filip DJ, Aster RH. Relative hemostatic effectiveness of human platelets stored at 4 degrees and 22 degrees C. J Lab Clin Med. 1978;91(4):618-624. [PubMed] [Google Scholar]
- 22.Slichter SJ, Harker LA. Preparation and storage of platelet concentrates. II. Storage variables influencing platelet viability and function. Br J Haematol. 1976;34(3):403-419. [DOI] [PubMed] [Google Scholar]
- 23.Apelseth TK, Kristoffersen EK, Kvalheim VL, et al. Transfusion with cold stored platelets in patients undergoing complex cardiothoracic surgery with cardiopulmonary bypass circulation: effect on bleeding and thromboembolic risk. Transfusion. 2017;57:3A-4A.28097696 [Google Scholar]
- 24.Strandenes GK, Kristoffersen EK, Bjerkvig CK, et al. Cold stored apheresis platelets in treatment of postoperative bleeding in cardiothoracic surgery. Transfusion. 2016;56(suppl 4):16A. [Google Scholar]
- 25.Valeri CR. Circulation and hemostatic effectiveness of platelets stored at 4 C or 22 C: studies in aspirin-treated normal volunteers. Transfusion. 1976;16(1):20-23. [DOI] [PubMed] [Google Scholar]
- 26.Strandenes G, Sivertsen J, Bjerkvig CK, et al. A pilot trial of platelets stored cold versus at room temperature for complex cardiothoracic surgery. Anesthesiology. 2020;133(6):1173-1183. [DOI] [PubMed] [Google Scholar]
- 27.Rodriguez ML, Beussman KM, Chun KS, et al. Substrate stiffness, cell anisotropy, and cell-cell contact contribute to enhanced structural and calcium handling properties of human embryonic stem cell-derived cardiomyocytes. ACS Biomater Sci Eng. 2019;5(8):3876-3888. [DOI] [PubMed] [Google Scholar]
- 28.Stolla M, Bailey SL, Fang L, et al. Effects of storage time prolongation on in vivo and in vitro characteristics of 4°C-stored platelets. Transfusion. 2020;60(3):613-621. [DOI] [PubMed] [Google Scholar]
- 29.Meledeo MA, Campbell JE, Rodriguez AC, Valenciana MV, Cap AP. Both acute delivery of and storage with magnesium sulfate promote cold-stored platelet aggregation and coagulation function. J Trauma Acute Care Surg. 2015;79(4 suppl 2):S139-S145. [DOI] [PubMed] [Google Scholar]
- 30.Agey A, Reddoch-Cardenas K, McIntosh C, et al. Effects of intercept pathogen reduction treatment on extended cold storage of apheresis platelets. Transfusion. 2021;61(1):167-177. [DOI] [PubMed] [Google Scholar]
- 31.Reid TJ, LaRussa VF, Esteban G, et al. Cooling and freezing damage platelet membrane integrity. Cryobiology. 1999;38(3):209-224. [DOI] [PubMed] [Google Scholar]
- 32.Reid TJ, Esteban G, Clear M, Gorogias M. Platelet membrane integrity during storage and activation. Transfusion. 1999;39(6):616-624. [DOI] [PubMed] [Google Scholar]
- 33.Wood B, Padula MP, Marks DC, Johnson L. Refrigerated storage of platelets initiates changes in platelet surface marker expression and localization of intracellular proteins. Transfusion. 2016;56(10):2548-2559. [DOI] [PubMed] [Google Scholar]
- 34.Cohn SM, Jimenez JC, Khoury L, Perez JM, Panzo M. Inability to reverse aspirin and clopidogrel-induced platelet dysfunction with platelet infusion. Cureus. 2019;11(1):e3889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Best D, Senis YA, Jarvis GE, et al. GPVI levels in platelets: relationship to platelet function at high shear. Blood. 2003;102(8):2811-2818. [DOI] [PubMed] [Google Scholar]
- 36.Ng MSY, Tung JP, Fraser JF. Platelet storage lesions: what more do we know now [published online ahead of print 17 April 2018]? Transfus Med Rev. doi: 10.1016/j.tmrv.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 37.Cap AP. Platelet storage: a license to chill! Transfusion. 2016;56(1):13-16. [DOI] [PubMed] [Google Scholar]
- 38.Takayama H, Hosaka Y, Nakayama K, et al. A novel antiplatelet antibody therapy that induces cAMP-dependent endocytosis of the GPVI/Fc receptor gamma-chain complex. J Clin Invest. 2008;118(5):1785-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bender M, Hofmann S, Stegner D, et al. Differentially regulated GPVI ectodomain shedding by multiple platelet-expressed proteinases. Blood. 2010;116(17):3347-3355. [DOI] [PubMed] [Google Scholar]
- 40.Montague SJ, Hicks SM, Lee CS, et al. Fibrin exposure triggers αIIbβ3-independent platelet aggregate formation, ADAM10 activity and glycoprotein VI shedding in a charge-dependent manner. J Thromb Haemost. 2020;18(6):1447-1458. [DOI] [PubMed] [Google Scholar]
- 41.Hosseini E, Ghasemzadeh M, Nassaji F, Jamaat ZP. GPVI modulation during platelet activation and storage: its expression levels and ectodomain shedding compared to markers of platelet storage lesion. Platelets. 2017;28(5):498-508. [DOI] [PubMed] [Google Scholar]
- 42.Hoffmeister KM, Felbinger TW, Falet H, et al. The clearance mechanism of chilled blood platelets. Cell. 2003;112(1):87-97. [DOI] [PubMed] [Google Scholar]
- 43.Sørensen AL, Rumjantseva V, Nayeb-Hashemi S, et al. Role of sialic acid for platelet life span: exposure of beta-galactose results in the rapid clearance of platelets from the circulation by asialoglycoprotein receptor-expressing liver macrophages and hepatocytes. Blood. 2009;114(8):1645-1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen W, Druzak SA, Wang Y, et al. Refrigeration-induced binding of von Willebrand factor facilitates fast clearance of refrigerated platelets. Arterioscler Thromb Vasc Biol. 2017;37(12):2271-2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.