Abstract
Aims
Retirement is a major life transition that may improve or worsen mental health, including depression. Existing studies provide contradictory results. We conducted a systematic review with meta-analysis to quantitatively pool available evidence on the association of retirement and depressive symptoms.
Methods
We applied PRISMA guidelines to conduct a systematic review and meta-analysis to retrieve, quantitatively pool and critically evaluate the association between retirement and both incident and prevalent depression and to understand better the potential role of individual and contextual-level determinants. Relevant original studies were identified by searching PubMed, Embase, PsycINFO and the Cochrane Library, through 4 March 2021. Subgroup and sensitivity meta-analyses were conducted by gender, study design (longitudinal v. cross-sectional studies), study quality score (QS) and considering studies using validated scales to diagnose depression. Heterogeneity between studies was evaluated with I2 statistics.
Results
Forty-one original studies met our a priori defined inclusion criteria. Meta-analysis on more than half a million subjects (n = 557 111) from 60 datasets suggested a protective effect of retirement on the risk of depression [effect size (ES) = 0.83, 95% confidence interval (CI) = 0.74–0.93], although with high statistical heterogeneity between risk estimates (χ2 = 895.19, df = 59, I2 = 93.41%, p-value < 0.0001). Funnel plot asymmetry and trim and fill method suggested a minor potential publication bias. Results were consistent, confirm their robustness and suggest stronger protective effects when progressively restricting the included studies based on quality criteria: (i) studies with the highest QS [55 datasets, 407 086 subjects, ES = 0.81, 95% CI = 0.71–0.91], (ii) studies with a high QS and using validated assessment tools to diagnose depression (44 datasets, 239 453 subjects, ES = 0.76, 95% CI = 0.65–0.88) and (iii) studies of high quality, using a validated tool and with a longitudinal design (24 datasets, 162 004 subjects, ES = 0.76, 95% CI = 0.64–0.90). We observed a progressive reduction in funnel plot asymmetry. About gender, no statistically significant difference was found (females ES = 0.79, 95% CI = 0.61–1.02 v. men ES = 0.87, 95% CI = 0.68–1.11).
Conclusions
Pooled data suggested that retirement reduces by nearly 20% the risk of depression; such estimates got stronger when limiting the analysis to longitudinal and high-quality studies, even if results are affected by high heterogeneity.
As retirement seems to have an independent and protective effect on mental health and depressive symptoms, greater flexibility in retirement timing should be granted to older workers to reduce their mental burden and avoid the development of severe depression. Retirement may also be identified as a target moment for preventive interventions, particularly primary and secondary prevention, to promote health and wellbeing in older ages, boosting the observed impact.
Keywords: depression, epidemiology, prevention, retirement, social factors, systematic review and meta-analysis
Introduction
Globally, the proportion of older adults (>60 years) is estimated to almost double between 2015 and 2050, from about 12% to 22% (United Nations, 2015). As the world population ages, it is critical to promote and support healthy ageing processes to improve societal wellbeing and limit its clinical and economic burden (Dietz et al., 1987). The prevalence of late-life depression is 7% among the general older population (Mccall and Kintziger, 2013) and accounts for 5.7% of years lived with disability in those over 60 years old (Killinger, 2012). Depressive symptoms are often overlooked and untreated in older populations, are associated with psychosocial and cognitive decline (Nelson, 2001), and result from a complex interaction between psychological, biological and social factors (Alexopoulos, 2019). One significant determinant that could play a role is transitioning into retirement, whose timing, decision and consequences could be influenced by depressive symptoms, such as loneliness and hopelessness, acting as moderators (Gum et al., 2017; Segel-Karpas et al., 2018). Retirement is a major life transition that results in social and psychological transformations (Bosse et al., 1991), which pose both threats and opportunities for mental health. On the one hand, as a potentially stressful life event, retirement can have adverse repercussions on individual physical and psychological wellbeing (Portnoi, 1981). People lose access to social networks, lifestyles and daily routines, as well as potential stimulation, activity and purposes. Conversely, retirement may reduce work-related exposures and improve physical and mental health through complex mechanisms. These could include an increase in social support and in the time available for leisure and healthy activities, and disconnection from work-related stressors (Van Der Heide et al., 2013; Eibich, 2015). These positive health effects were particularly observed among retirees from strenuous jobs (Belloni et al., 2016; Blake and Garrouste, 2019; Ardito et al., 2020; Carrino et al., 2020; Fleischmann et al., 2020). Therefore, as we reported in previous research (Vigezzi et al., 2021), health behaviours changes (e.g. changes in smoke habit, alcohol consumption, physical activity, time use, social interactions) appeared to be among the most relevant mediators of retirement consequences on olders’ health, affecting life years after the withdrawal from work (Lang et al., 2007; Vahtera et al., 2009; Celidoni and Rebba, 2017). Nonetheless, current findings are inconclusive. As it has been previously conceptualised (Van Solinge, 2007), health consequences of retiring are influenced by the employment history, the job characteristics (Ardito et al., 2020) and the transition to retirement itself, as well as by the availability of socioeconomic resources at the time of retirement and, last but not least, by individuals’ characteristics and appraisal of stress-generating life events (Van Solinge, 2007; Augner, 2018). As a result of such a complex conceptual model, no conclusive evidence exists on the harm-benefit health balance of retirement. In particular, both older and more recent studies have shown contradictory results on the impact of retirement on mental health outcomes (Bossé et al., 1987; Salokangas and Joukamaa, 1991; Gall et al., 1997; Drentea, 2002; Mein et al., 2003; Buxton et al., 2005; Gill et al., 2006; Mojon-Azzi et al., 2007; Van Solinge, 2007; Alavinia and Burdorf, 2008; Vahtera et al., 2009; Jokela et al., 2010; Westerlund et al., 2010).
Here we performed a systematic review and meta-analysis to identify the overall association of retirement with depression. As a second aim, we sought to identify potential modifying individual- and contextual-level factors.
Methods
We followed the Prepared Items for Systematic Reviews and Meta-Analysis (PRISMA) (Liberati et al., 2009; Page et al., 2021) and the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines (Stroup et al., 2000).
Search methods and inclusion criteria
Studies identified searching the electronic databases PubMed/Medline, Embase, PsycINFO and the Cochrane Library through 4 March 2021 were included. The search strategy was first developed in Medline and then adapted for use in the other databases (online Supplementary Table 1). Briefly, we used a combination of free text and exploded MeSH headings, identifying: (i) the concept of ‘retirement/transition to retirement’ and (ii) ‘depression/depressive symptoms’. Further studies were retrieved from manual reference listing of relevant articles and consultation with experts in the field. Details on inclusion and exclusion criteria are reported in Table 1, according to the Population, Exposure, Comparison, Outcomes and Study design (PECOS) framework (Brown et al., 2006; Higgins and Green, 2013). Our inclusion criteria were limited to those studies: reporting original data from quantitative analysis, providing effect sizes (ESs) of the association between retirement (exposure of interest) and depression (outcome of interest); natural experiments (Stuckler, 2017; Ronchetti et al., 2020), observational studies with prospective, retrospective and cross-sectional designs; and written in English. An extensive definition of retirement and retirement status was used: depending on study design, both retired status and transition to retirement were included as exposure of interest; we considered all retirement types, apart from retirement only for disability, which was excluded. Depression-related outcomes of interest included: depressive symptoms, Diagnostic and Statistical Manual of Mental Disorders (DSM), or International Classification of Diseases scale (ICD)-based diagnosis as major depressive disorder and persistent depressive disorder. We excluded opinion papers (i.e. editorials, narrative reviews, commentaries and letters to the Editor) not providing original data. Systematic reviews were also excluded but screened to retrieve relevant original studies. The review's protocol was drafted and approved by authors before conduction (not archived on public databases).
Table 1.
A priori defined inclusion and exclusion criteria according to the Population (P), Exposure (E), Comparison (C), Outcomes (O) and Study design (S) (PECOS) framework
| Search strategy | Details |
|---|---|
| Inclusion criteria | P: general adult population (male and female) |
| E: retirement | |
| C: still employed | |
| O: depressive symptoms | |
| S: original data (all study designs) | |
| Exclusion criteria | E: disability retirement |
| O: other mental health outcomes (including anxiety symptoms, post-traumatic stress symptoms) | |
| S: no original data (opinion papers, review articles, commentaries, letters, protocols, studies without quantitative data) | |
| Language filter | English |
| Time filter | From inception through 4 March 2021 |
| Database | PubMed/Medline; EMBASE, PsycINFO, Cochrane |
Study selection, data extraction and quality appraisal
Identified studies were independently reviewed for eligibility by two authors (V.G. and G.P.V.) in a two-step process; a first screening was performed based on title and abstract. Then, full texts were retrieved for a second screening. At both stages, disagreements among reviewers were resolved by consensus and by consulting a third senior author (A.O.) when disagreement persisted. Data were independently extracted by two authors (V.G. and G.P.V.), supervised by a third author (A.O.), using an ad-hoc developed data extraction spreadsheet. The data extraction spreadsheet was piloted on ten randomly selected papers and modified accordingly. Data extraction included: full reference details, country of study conduction, study design, study setting, study population details, sample size, exposure details, outcomes of interest, including validated assessment tools for depression, and quantitative results, including ESs and corresponding confidence intervals (CIs). Corresponding authors were contacted by e-mail in case of incomplete data. Quality appraisal of included studies was carried out applying the 14-item scoring system developed by Shim et al. for population-based studies on retirement as a risk factor (Shim et al., 2013). As determined by consensus following the review methodology literature, we consider of high quality the studies with at least ⩾75% of the highest score.
Data pooling and meta-analysis
We performed descriptive analysis to report and pool the characteristics of included studies using ranges and average values. With regard to the pre-specified outcomes of interest, we would expect variability between studies, e.g. by study design and population. We, therefore, applied random-effects meta-analyses to acquire estimates of the association between retiring and risk of depression/depressive symptoms, rather than to assume a single true value in a fixed-effects approach (Higgins and Green, 2013). Moreover, a random effect model is highly recommended when high heterogeneity is expected or detected. Pooled ESs were calculated as odd ratios (ORs) (Ter Hoeve et al., 2020). When the included studies reported ESs as regression beta coefficients with corresponding standard errors (s.e.s), we mathematically converted them into ORs with corresponding CIs (Bland and Altman, 2000; Hailpern and Visintainer, 2003). We also included studies that reported ESs as χ2 or ρ correlation coefficients with corresponding total sample sizes or as mean differences with sample sizes and corresponding correlations. Heterogeneity was assessed using the I2 statistic (see online Supplementary Table 3 for details) and visual inspection of funnel plots. We performed sensitivity analyses progressively limiting meta-analysis to: (i) high-quality studies; (ii) high-quality studies using validated scales to diagnose depression; (iii) high-quality longitudinal studies using validated scales to diagnose depression. Moreover, we conducted a subgroup meta-analysis by gender strata and study design.
We assessed publication bias with funnel plot visual inspection (Higgins et al., 2011) and the Begg and Mazumdar (1994) and Egger et al. (1997) tests. A ‘trim and fill’ method was used if publication bias was detected (Duval and Tweedie, 2000; Gianfredi et al., 2020) to estimate potential missing studies which contribute to the funnel plot's asymmetry (Sutton et al., 2000). This method assumes that the most extreme ES studies have not been reported, biasing the overall ES estimates (Shi and Lin, 2019). Meta-analyses were conducted using ProMeta3® (Internovi, Milan, Italy) software.
Results
Characteristics of included studies
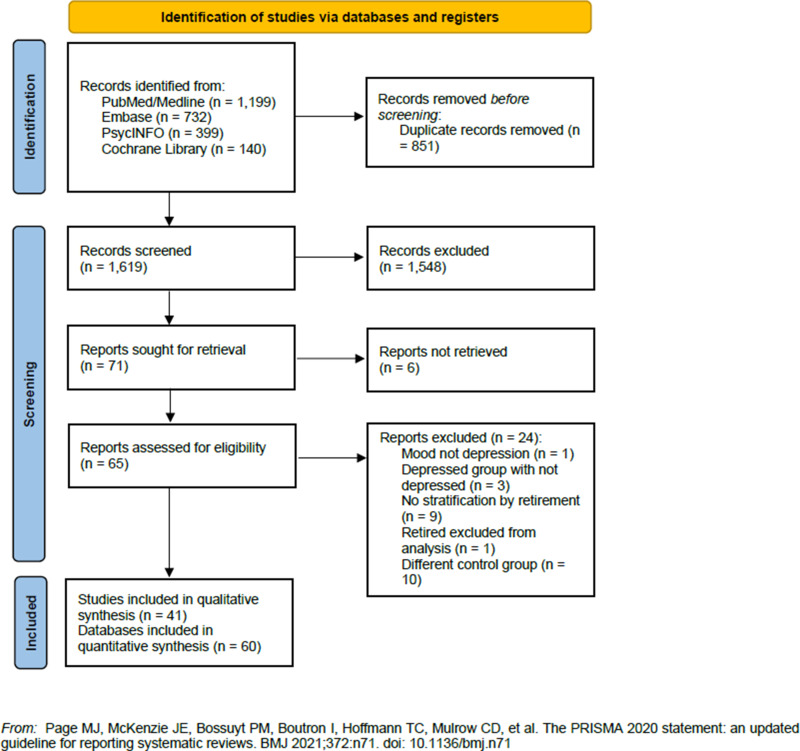
We identified 2470 studies by searching the selected databases and listing references of relevant articles. After removing duplicates, 1619 records were retrieved. Papers were screened and selected, as illustrated in Fig. 1 (1548 records were excluded after first screening; six reports were not retrieved in full text; 24 were excluded with reasons), resulting in 41 papers meeting our inclusion criteria (Farakhan et al., 1984; Borson et al., 1986; Herzog et al., 1991; Pahkala et al., 1992; Midanik et al., 1995; Reitzes et al., 1996; Fernandez et al., 1998; Kim and Moen, 2002; Buxton et al., 2005; Tuohy et al., 2005; Butterworth et al., 2006; Mojon-Azzi et al., 2007; Alavinia and Burdorf, 2008; Schwingel et al., 2009; Coursolle et al., 2010; Behncke, 2012; Calvo et al., 2013; Choi et al., 2013; Gayman et al., 2013; Leinonen et al., 2013; Airagnes et al., 2015, 2016; Bretanha et al., 2015; Olesen et al., 2015; Belloni et al., 2016; Calvó-Perxas et al., 2016; Mosca and Barrett, 2016; Park and Kang, 2016; Rhee et al., 2016; Heller-Sahlgren, 2017; Shiba et al., 2017; Arias-De La Torre et al., 2018; Augner, 2018; Fernández-Niño et al., 2018; Sheppard and Wallace, 2018; Van Den Bogaard and Henkens, 2018; Anxo et al., 2019; Kolodziej and García-Gómez, 2019; Noh et al., 2019; Matta et al., 2020; Han, 2021). Characteristics of included studies are reported in Table 2. Studies were published between 1984 and 2021, with almost one third (n = 12, 29.3%) published in the last 5 years. The majority of the studies (n = 21, 51.2%) were conducted in Europe (United Kingdom, n = 3; France, n = 3; Finland, n = 2; Sweden, n = 1; Spain, n = 1; Switzerland, n = 1; Denmark, n = 1; Ireland, n = 1; Scotland, n = 1; multi-centric European studies, n = 5) and in the USA (n = 13, 31.7%). Four studies were conducted in Asia, one in Brazil, one in Australia; four were multi-centre studies conducted at the global and European level.
Fig. 1.
Flow diagram of the studies selection process.
Table 2.
Descriptive characteristics of the included studies stratified by study design and listed in alphabetical order and by study design
| Author Year (reference) |
Country of study implementation | Study design | Study period | Study population | Sample size (n.) Gender Age |
Attrition | Type of retirement | Diagnosis of depression | Validated tool for depression | Effect size (CI95%) | Adjustment | QS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cross-sectional study design | ||||||||||||
| Alavinia and Burdorf (2008) | Austria, Greece, Denmark, France, Germany, Italy, the Netherlands, Spain, Sweden, Switzerland | Cross-sectional | 2004 | SHARE study | 11 462, F M, 50–64 y |
61.8% | Statutory and early retirement | EURO-D | Yes | Moderately depressed: OR = 1.28 (1.08–1.52), p < 0.05 |
Self-perceived health, sex, age, education, BMI, marital status, smoking, drinking, physical activity | 15 |
| Heavily depressed: OR = 2.60 (1.37–4.94), p < 0.05 | ||||||||||||
| Anxo et al. (2019) | Sweden | Cross-sectional | 2014–2015 | Combination of Swedish register data and LISA study | 3901, F (45%) M (55%), 66–76 y |
3878 | Prolonged v. statutory retirement | Depression index | No | β = −0.029 (s.e. = 0.034) | Age, sex, migration status, education, marital status, life expectancy, previous labour market experience, income, previous health | 12 |
| Arias-de la Torre et al. (2018) | Spain | Cross-sectional | 2014–2015 | European Health Interview Survey | 21 546 F (53.2%) M (46.8%), ⩾18 y |
1296 | n.a. | PHQ-8 | Yes | F: OR = 1.91 (1.31–2.82) |
Gender, age, marital status, country of birth, educational level, residence area, employment status, occupational social class |
14 |
| M: OR = 1.68 (0.93–3.03) | ||||||||||||
| Augner (2018) | Austria, Germany, Sweden, Spain, Italy, France, Denmark, Greece, Switzerland, Belgium, Israel, Czech Republic, Poland, Portugal, Slovenia Estonia, Croatia, Luxembourg | Cross-sectional | 2014–2015 | SHARE | 13 447, F (54.2%) M (45.8%), 60–69 y |
n.a. | Statutory and early retirement | EURO-D | Yes | OR = 0.79 (0.71–0.88)a | Sex, country | 12 |
| Behncke (2012) | UK | Cross-sectional | n.a. | ELSA | Employed: 1247, F (50%) M (50%), mean age 55 y |
839 | n.a. | CES-D | Yes | βATET = 0.047 (s.e. = 1.22) | Socioeconomic status, sex, age, education, job characteristics, health indicators (subjective and objective health measures, proxy for genetic predisposition, underlying health state) | 15 |
| Retired: 192, F (54%) M (46%), mean age 60.20 y | ||||||||||||
| Belloni et al. (2016) | Austria, Belgium, Denmark, France, Germany, Italy, the Netherlands, Spain, Sweden, Switzerland | Cross-sectional | 2004–2013 | SHARE | 21 960, F (48%) M (52%), 55–70 y |
n.a. | Statutory and early retirement | EURO-D | Yes | F: βFE = −0.240 (s.e. = 0.082), p < 0.01; blue collar F (n = 1691) βFE = −0.0530 (s.e. = 0.784); white collar F (n = 8064) βFE = 0.158 (s.e. = 0.285) | Age, marital status, number of grandchildren, household income, health index, regional unemployment rate, waves | 14 |
| M: βFE = −0.203 (S.E. = 0.062), p < 0.01; blue collar M (n = 3399) βFE = −0.0534 (S.E. = 0.413); white collar M (n = 7212) βFE = 0.0892 (S.E. = 0.373) | ||||||||||||
| Borson et al. (1986) | USA | Cross-sectional | December 1978 | Subjects admitted at The MCCU of the Seattle Veterans Administration Medical Center | 404, F (3.5%) M (96.5%), >60 y |
513 | Disability pension excluded | ZSDS | Yes | Depressed among retired v. non-retired: χ2 = 1.6, p = 0.197 | Age, sex, marital status, years of education, household income, type of residence, household composition | 14 |
| Bretanha et al. (2015) | Brazil | Cross-sectional | 2008 | Subjects living in the 20 basic health units of the urban zone of Bagé, Rio Grande do Sul | 1514, F (62.8%) M (37.2%), >60 y |
199 | n.a. | GDS-15 | Yes | OR = 0.77 (0.61–0.97), p = 0.026 | Sex, age, skin colour, schooling, marital status, economic status | 12 |
| Butterworth et al. (2006) | Australia | Cross-sectional | 1997 | National Survey MHWB | 4189, F (54%) M (46%), 45–74 y |
6452 | ‘Not in the labour force’ as retirement | CIDI version 2.1, meeting the ICD-10 | Yes | F 45–54 retired: OR = 1.20 (0.80–1.80); F 55–64 retired: OR = 0.46 (0.29–0.73); F 65–74 retired: OR = 0.27 (0.17–0.44) |
Age group, labour force status, interaction between age and labour force status, main source of income, home ownership, physical health, living situation, partnered, socio-economic status | 16 |
| M 45–54 retired: OR = 2.86 (1.37–6.00); M 55–64 retired: OR = 0.67 (0.35–1.29); M 65–74 retired: OR = 0.42 (0.20–0.85) | ||||||||||||
| Buxton et al. (2005) | UK | Cross-sectional | 2000 | 2000 Psychiatric Morbidity Survey of Great Britain | 1875, F (51%) M (49%), 50–64 y |
n.a. | Early retirement | CIS-R | Yes | F: OR = 2.6 (0.9–7.4); | Age, tenure, mental health, physical health | 15 |
| M: OR = 4.3 (1.7–11.0) | ||||||||||||
| Choi et al. (2013) | Denmark, Sweden, Austria, France, Germany, Switzerland, Belgium, the Netherland, Spain, Italy, Greece, Israel, Czech Republic, Poland and Ireland | Cross-sectional | 2004–2007 | SHARE | 7238, F (48.3%) M (51.7%) ⩾60 y |
8857 | Inclusive definition: unemployed, long term sick, disabled, inactive, statutory retirement v. paid work | EURO-D | Yes | OR = 1.41 (0.79–2.44)a, p = 0.24 | Age, sex, marital status, education, economic status, country | 14 |
| Farakhan et al. (1984) | USA | Cross-sectional | n.a. | Elderly black persons | 30, F (76%), M (24%) 52–97 y |
n.a. | n.a. | DACL | Yes | Data not extractable: reduced risk of depression | n.a. | 6 |
| Fernández-Niño et al. (2018) | China, Ghana, India, Mexico, Russian Federation and South Africa | Cross-sectional | 2007–2009 | SAGE study | 18 148, F (54%) M (46%), 64–75 y |
3262 | Retirement with a pension (retirement without a pension and not working due to disability excluded) | World Mental Health Survey version of the Composite International Diagnostic Interview based on ICD-10 (MDE) | Yes | China: F OR = 1.60 (0.73–3.53), p = 0.24; M OR = 0.23 (0.08–0.70), p = 0.01 |
Sex, age, marital status, education, belonging to a religious minority, self-report of having some type of health care service, physical disability, multimorbidity, accidents/injuries, living alone, participation in social religious activities, participation in non-religious social activities, horizontal trust, household wealth and country effect | 15 |
| China F 3854 M 3671 | ||||||||||||
| Ghana F 1469 M 1374 |
Ghana: F OR = 3.26 (0.84–12.6), p = 0.09; M OR = 0.25 (0.07–0.95), p = 0.04 |
|||||||||||
| India F 1870 M 2101 |
India: F OR = 0.05 (0.01–0.51), p = 0.01: M OR = 0.49 (0.16–1.52), p = 0.22, |
|||||||||||
| Mexico F 1145 M 736 |
Mexico: F OR = 0.39 (0.04–3.50), p = 0.40; M not estimable |
|||||||||||
| Russia F 1923 M 1122 |
Russia: F OR = 0.89 (0.39–2.01), p = 0.77; M OR = 1.43 (0.27–7.54), p = 0.67 |
|||||||||||
| South Africa F 1264 M 881 |
South Africa: F OR = 0.19 (0.04–0.97), p = 0.05; M OR = 0.89 (0.09–8.82), p = 0.03 |
|||||||||||
| Heller-Sahlgren (2017) | Austria, Belgium, Denmark, France, Germany, Italy, the Netherlands, Spain, Sweden, Switzerland | Cross-sectional | 2004–2012 | SHARE | 4704, F M, ⩾50 y |
3862 | Retired but excluding all non-workers in the non-retired category | EURO-D | Yes | EURO-D: βFEIV = 1.69 (s.e. = 0.67), p < 0.05 | Sex, education, occupational physical burden, occupational psychosocial burden | 15 |
| Clinical depression: βFEIV = 0.37 (S.E. = 0.15), p < 0.05 | ||||||||||||
| Herzog et al. (1991) | USA | Cross-sectional | May-October 1986 | ACL Survey | 1332, F M, 55–64 y 510, >65 y 822 | 2285 | Retirement for non-health reasons | CES-D | Yes | 55–64y: βOLS = −0.14 | Gender, race, educational attainment, marital status, current or former occupation, age | 15 |
| >65y: βOLS = 0.12 n.s. | ||||||||||||
| Kolodziej and García-Gómez (2019) | Austria, Belgium, Denmark, France, Germany, Italy, Greece, the Netherlands, Spain, Sweden, Switzerland | Cross-sectional | 2004–2013 | SHARE | 37 333, F (46.3%) M (53.6%), 55–69 y |
n.a. | Self-reported retirement status or self-reported permanent absence from the labour force or not having performed any paid work in the past month | EURO-D | Yes | βOLS = 0.456 (s.e. = 0.020), p < 0.01 | Gender, age at the time of the interview, age squared, number of children, education, marital status, area of residence, seasonal dummies, country dummies | 15 |
| F: βIV = −1.314 (S.E. = 0.341), p < 0.01; M: βIV = −0.894 (S.E. = 0.439), p < 0.05 | ||||||||||||
| White collar: βIV = −0.671 (S.E. = 0.371), p < 0.1; blue collar: βIV = −1.792 (S.E. = 0.459), p < 0.01 | ||||||||||||
| Midanik et al. (1995) | USA | Cross-sectional | 1985–1987 | Northern California Kaiser Permanente Medical Care Program | 595, F (43%) M (57%), 55–75 y |
400 | n.a. | CES-D | Yes | F: RR = 0.5 (0.2–1.2) |
Age, gender, marital status, education, baseline mental health | 14 |
| M: RR = 1.0 (0.4–2.4) | ||||||||||||
| Total: RR = 0.7 (0.4–1.3) | ||||||||||||
| Mojon-Azzi et al. (2007) | Switzerland | Cross-sectional | 1999–2003 | Swiss Household Panel | 557, F (45%) M (55%), 55–75 y |
811 | Retired due to old age and retired for other reasons, such as disability or severe illness | Frequency of negative feelings such as depression or anxiety (from 0 = never to 10 = always) | No | OR = 1.1 (0.9–1.3) | Sex, general health at baseline, highest level of education achieved, occupation class, years from official retirement | 15 |
| Pahkala et al. (1992) | Finland | Cross-sectional | 1984 | Subjects born in 1923 or earlier and living in a semi-industrialised community in the western part of central Finland | 594, F M, ⩾60 y |
771 | n.a. | ZSDS | Yes | Data not extractable: increased proportion of dysthymic men had retired |
Education, occupation, marital status, living conditions, living partners, hobbies, visiting contacts, social participation, appreciation, intimacy of relationships | 12 |
| Sheppard and Wallace (2018) | USA | Cross-sectional | 2016 | Women who had retired part-time or full time from working outside of the home or a home-based business | 80, F, 55–81 y |
n.a. | Forced or voluntary, part- or full-time retirement for < or = 10 years. | Questions regarding depression | No | ρ = −0.116 (for the length of retirement) | n.a. | 11 |
| Tuohy et al. (2005) | Scotland | Cross-sectional | n.a. | Retired police officers | 1334, M, mean age 61 y, range 34–94 y |
2669 | Early and statutory retirement | HADS | Yes |
ρ = −0.09 (for the retirement age), p < 0.001 β = −0.031 n.s. |
Anxiety scores, present age, retirement age, retirement type, postretirement work | 14 |
| Prospective cohort studies | ||||||||||||
| Airagnes et al. (2015) | France | Longitudinal 15 y | 1993–2008 | GAZEL study | 9755, F (20.6%) M (79.4%), mean age 55.4 ± 2.4 y |
10 733 | n.a. | CES-D | Yes | β = −0.378, p < 0.001 | Age, gender, occupational grade, history of sickness absences for depression, alcohol consumption, Type A personality (competitiveness, sense of urgency, and irritability) | 18 |
| Airagnes et al. (2016) | France | Longitudinal 25 y | 1989–2004 | GAZEL study | 9242, F (23.7%) M (76.3%), mean age: F 57.0 ± 3.9 y; M 59.4 ± 2.7 y |
11 383 | n.a. | CES-D | Yes | F: β = −0.480, p < 0.001 |
Age, marital status, occupational status, alcohol consumption, self-rated health, CES-D score before retirement, adverse childhood life events | 18 |
| M: β = −0.183, p = 0.005 | ||||||||||||
| Calvo et al. (2013) | USA | Longitudinal 18 y | 1992–2010 | HRS survey | 6624, F (47.3%) M (56.7%), mean age 64.01 ± 6.48 y |
3129 | Statutory and early retirement | Reduced CES-D | Yes | For emotional health: short-term model: βFEIV = −1.54 (s.e. = 0.20), p < 0.001; long-term model: βFEIV = −1.26 (s.e. = 0.15), p < 0.001 | Changes to Social Security's full retirement age and unexpected early retirement window offers, age, interaction between retirement and age, wealth, income, marital status, gender, race, education, blue/white collar | 18 |
| Calvó-Perxas et al. (2016) | Austria, Germany, Sweden, the Netherlands, Spain, Italy, France, Denmark, Switzerland, Belgium, Czech Republic, Slovenia, Estonia | Longitudinal 2 y | 2011–2013 | SHARE | 22 280, F (58.2%) M (41.8%), mean age 64.2 y |
15 932 | n.a. | EURO-D | Yes | Incident depression after 2 y of retirement: F OR = 1.02 (0.83–1.27); M OR = 1.03 (0.73–1.43) |
Age, marital status, employment, education level, number of comorbidities, BMI, BADL, anxiety | 16 |
| Persistent depression after 2 y of retirement: F OR = 1.08 (0.84–1.39); M OR = 0.82 (0.54–1.24) | ||||||||||||
| Coursolle et al. (2010) | USA | Longitudinal, 11 y | 1993–2004 | Wisconsin Longitudinal Study | 2666, F (45%), M (55%), 64–65 y in 2004 |
7651 | Self-reported full and partial retirement | CES-D | Yes | For full retirement: total: βFE = −0.97 (s.e. = 0.31), p < 0.01; F βFE = −0.16 (s.e. = 0.51), n.s.; M βFE = −1.53 (s.e. = 0.39), p < 0.001 |
Gender, wages, assets, physical health, educational attainment, family characteristics and relationships, employment characteristics, work-family conflict | 19 |
| For partial retirement: total: βFE = −0.61 (s.e. = 0.35), n.s.; F βFE = −0.39 (s.e. = 0.60), n.s.; M βFE = −0.86 (s.e. = 0.43), p < 0.05 | ||||||||||||
| Fernandez et al. (1998) | USA | Longitudinal 2 y | 1992–1994 | Mature men and women residing in a North Carolina metropolitan area | 749, F M, 58–64 y |
582 | Retirement from full-time employment (working less than 35 h a week included) | CES-D | Yes | White men β = −0.82, p < 0.05 |
n.a. | 15 |
| African American men β = 2.70, p < 0.05 | ||||||||||||
| Gayman et al. (2013) | USA | Longitudinal 14 y | 1994–2008 | HRS survey | 3264, F M 51–61 y in 1992 |
9390 | Self-reported retirement, excluding disability | CES-D | Yes | Depressed between retired: Whites χ2 diff. = 5.49, p = 0.02 |
Race, gender, education, age, disability exit, death in the study period | 18 |
| Whites = 2765 | ||||||||||||
| Blacks = 499 | Blacks χ2 diff. = 0.01, p = 0.92 |
|||||||||||
| Han (2021) | USA | Longitudinal 18 y | 1998–2016 | RAND HRS | 9347, F 49.74% M 50.26%, >51 y | n.a. | Retirement as not working or self-identified as completely retired | CES-D | Yes | Retired for non-health reasons: βREWB = −0.382 (s.e. = 0.119), p < 0.01 | Self-rated health, labour force status, transition, age, gender, race, education, occupation type, marital status, household income, household wealth, health insurance coverage, household size | 17 |
| Retired due to poor health: βREWB = 1.790 (S.E. = 0.117) | ||||||||||||
| Continued retirement: βREWB = 0.385 (S.E. = 0.053), p < 0.001 | ||||||||||||
| Kim and Moen (2002) | USA | Longitudinal 5 y | 1994–1999 | Cornell Retirement and Well-Being Study | 458, F (38%) M (62%), 50–72 y |
304 | Long-term retirees v. newly retired v. not-yet retired individuals | CES-D | Yes | F: long-term retired (n = 91) βOLS = 0.19 (s.e. = 2.94); newly retired (n = 33) βOLS = −2.09 (s.e. = 3.14) |
Income adequacy, subjective health, marital quality, marital conflict, personal control, age, psychological well-being, interaction between psychological well-being and retirement transition, spouse's employment status, interaction between retirement status and spouse's employment status | 15 |
| M: long-term retired (n = 181) βOLS = −1.55 (S.E. = 1.55); newly retired (n = 47) βOLS = −1.67 (S.E. = 1.92) | ||||||||||||
| Leinonen et al. (2013) | Finland | Longitudinal 11 y | 1997–2007 | data from administrative register data from various sources linked together by Statistics Finland | 19 877, F M, 57–68 y |
n.a. | Disability and old-age retirement | ICD-10 | Yes | Mean DDD/3-months period 0.01 (−0.01–0.03); antidepressant drugs use instead of depression | Calendar year, age at retirement, gender, occupational social class, living arrangements | 18 |
| Matta et al. (2020) | France | Longitudinal 21 y | 1989–2014 | GAZEL study | 17 655, F M, 55.2 y mean age at retirement | 1839 | Official retirement (retirement due to illness excluded) | CES-D | Yes | βME = −1.704 (s.e. = 0.13), p < 0.05 | Gender, marital status, occupational status, alcohol occupation, smoking status, time, retirement, interaction between time and retirement, BMI, interactions between BMI and retirement, time and double interaction with retirement and time | 18 |
| Mosca and Barrett (2016) | Ireland | Longitudinal 4 y | 2009–2013 | TILDA | 2373, F M, >50 y |
4537 | Voluntary and involuntary full retirement | CES-D | Yes | Retired due to own ill health: βOLS = 2.584 (s.e. = 1.85), p < 0.10 | Death of a close relative or a friend, stop participating in a group, changes in functional capacity, chronic illness, self-reported health and vision, changes in income | 16 |
| Retired involuntary: βOLS = 2.212 (S.E. = 1.71), p < 0.10 | ||||||||||||
| Retired voluntarily: βOLS = 0.674 (S.E. = 1.56), n.s. | ||||||||||||
| Noh et al. (2019) | Korea | Longitudinal 2 y | 2010–2012 | Korea Longitudinal Study of Aging | 7134, F M, ⩾45 y |
8272 | Retired v. currently working or currently not working but looking for a job | CES-D10 | Yes | Total: βOLS = 0.12 (s.e. = 0.19), 95% CI −0.26–0.50 | Age, gender, education, marital status, self-rated health status, urbanity, CES-D10 score in 2010 | 17 |
| F: βOLS = −0.56 (S.E. = 0.29), 95% CI −1.12–0.01 | ||||||||||||
| M: βOLS = 0.90 (S.E. = 0.26), p < 0.001, 95% CI 0.40–1.41 | ||||||||||||
| Olesen et al. (2015) | Denmark | Longitudinal 6 y | 2000–2006 | Danish national registers/administrative data 2000–2006 | 245 082, F (49%) M (51%), n.a. |
7134 | Statutory old-age retirement (disability pension excluded) | Hospital treatment for depression (ICD-10) | No | Total: OR = 1.15 (95% CI 0.98–1.35) | Sex, cohabitation, disposable income, level of education, area of residence | 19 |
| F: OR = 1.23 (95% CI 0.98–1.54) | ||||||||||||
| M: OR = 1.07 (95% CI 0.86–1.34) | ||||||||||||
| Park and Kang (2016) | Korea | Longitudinal 6 y | 2006–2012 | Korea Longitudinal Study of Aging | 5937, F (50%) M (50%), mean age 59.60 ± 10.02 y |
4317 | Voluntary and involuntary retirement | CES-D10 | Yes | F: voluntary retirement HR = 1.361 (1.051–1.762); involuntary retirement HR = 1.584 (1.216–2.062) |
Age, property, household income, perceived health status, medical disability | 19 |
| M: voluntary retirement HR = 1.255 (0.987–1.596); involuntary retirement HR = 1.310 (1.063–1.613) | ||||||||||||
| Reitzes et al. (1996) | USA | Longitudinal 2 y | 1992–1994 | Carolina Health and Transitions Study | 757, F (52%) M (48%), range 58–64 y |
69 | n.a. | CES-D | Yes |
β = −0.132 (s.e. = −1.655), p < 0.001 |
Poor health, age, race, marital status, gender, income, education, occupation, worker commitment, worker identity, depression in 1992 | 16 |
| Rhee et al. (2016) | USA | Longitudinal 4 y | 2006–2010 | RAND HRS survey with Participant Lifestyle Questionnaire | 1195, F (48%) M (52%), >50 y, mean age 61.89 y |
828 | Multicategorical model: transition to voluntary and involuntary retirement | CES-D | Yes | Transition to involuntary retirement: β = 0.09 (s.e. = 0.07) |
Control over financial situation, positive family relationships, negative family relationships, social integration | 18 |
| Transition to voluntary retirement: β = −0.04 (S.E. = 0.04) | ||||||||||||
| Schwingel et al. (2009) | Singapore | Cross-sectional | 2004–2007 | Singapore Longitudinal Ageing Studies | 2716, F M, ⩾55 y; retired = 1360, workers = 201 |
92 | Retired and non-volunteering v. still working and retired and volunteering v. still working | GDS-15 | Yes | Retired and not volunteering: mean = 3.17 (s.e. = 0.11), p = 0.012; retired and volunteering: mean = 2.68 (s.e. = 0.18), p = 0.71; still working: mean = 2.76 (s.e. = 0.18) |
Age (<62 or ⩾62), education, gender, social network and support, general health status, physical functioning | 19 |
| Longitudinal 2 y | 1754, F M, ⩾55 y |
1054 | Retired and not volunteering: baseline mean = 1.91 ± 2.72, follow-up mean = 1.16 ± 2.09, p = 0.03; retired and volunteering: baseline mean = 1.27 ± 2.07, follow-up mean = 0.65 ± 1.37; still working: baseline mean = 1.39 ± 2.04, follow-up mean = 0.58 ± 0.99, p = 0.58 |
Age (<62 or ⩾62), education, gender, social network and support, general health status, physical functioning, interval between baseline and follow-up | ||||||||
| Shiba et al. (2017) | Japan | Longitudinal 3 y | 2010–2013 | Japan Gerontological Evaluation Study | 62 437, F (46%) M (54%), ⩾65 y, mean age 72.9 y |
n.a. | Still at work v. retired v. long-term retired | GDS-15 | Yes | F: retired β = 0.28 (95% CI 0.12–0.44); long-term retired β = 0.05 (95% CI −0.03–0.14) | Changes in social contacts and social support, occupational class, social participation, household income, marital status, instrumental activities of daily living, incidence of serious illnesses, family caregiving | 17 |
| M: retired β = 0.33 (95% CI 0.21–0.45);long-term retired β = 0.10 (95% CI 0.02–0.18) | ||||||||||||
| van den Bogaard and Henkens (2018) | 20 European countries and Israel | Longitudinal 2 y | 2011–2013 | SHARE | 9092, F M, range 50–70 y |
6040 | Voluntary retirement | EURO-D | Yes | βOLS = −0.10 (s.e. = 0.03), p < 0.01 | Physical and psychological job demand, gender, partner T1, educational level, work hours T1, household income T1, age, country, physical and mental health score T1, interaction between health situation T1 and retirement | 19 |
ρ, Pearson correlation; ACL, Americans' Changing Lives; ATET, Average Treatment Effect on the Treated; BALD, Basic Activities of Daily Living; BMI, Body Mass Index; BDI, Beck Depression Inventor; CES-D, Center for Epidemiologic Studies Depression Scale; CIS-R, Clinical Interview Schedule-Revised; CCRC, Continuing Care Retirement Community; CI, Confidence Interval; CIDI, Composite International Diagnostic Interview version 2.1; DACL, Depression Adjective Check List; DDD, Defined Daily Dose; ELSA, English Longitudinal Study of Ageing; EURO-D, Euro Depression-scale; F, Female; FE, Fixed Effects; FEIV, Fixed Effects Instrumental Variables; GAZEL, Gaz et Electricité; GDS, Geriatric Depression Scale; HADS, The Hospital Anxiety and Depression Scale; HR, hazard ratio; HRS, Health and Retirement Study; ICD, International Classification of Diseases scale; IV, Instrumental Variables; LISA, Longitudinal Integration Database for Health Insurance and Labour Market Studies; M, Male; MCCU, Medical Comprehensive Care Unit; MHWB, National Survey of Mental Health and Well-Being; n.a., not available; n.s., not significant; OLS, Ordinary Least Squares; OR, Odd Ratio; PHQ, Patient Health Questionnaire; QS, Quality Score; RR, relative risk; SAGE, Study on Global Ageing and Adult Health; s.e., Standard Error; SHARE, Survey on Health and Ageing in Europe; TILDA, The Irish Longitudinal Study on Ageing; UK, United Kingdom; USA, United States of America; y, years; ZSDS, Zung Self-rating Depression Scale.
Odds ratios and corresponding confidence intervals were calculated as the reverse odds ratios for the association between depression and employment compared to retired people.
Nineteen (46.3%) studies were longitudinal studies; their follow-up time ranged from 2 to 25 years, with most of them (n = 12, 60.0%) having less than 10 years of follow-up. Most of the longitudinal analyses were derived from the Survey on Health and Ageing and Retirement in Europe (SHARE, n = 8), followed by the Health and Retirement Study (HRS, n = 4) and the Gaz et Electricité cohort study (GAZEL, n = 3). Twenty-one studies (51.2%) had a cross-sectional study design, while only one study reported both cross-sectional and longitudinal data (Schwingel et al., 2009). Overall, sample sizes of included studies ranged from 30 (Farakhan et al., 1984) to 245 082 subjects (Olesen et al., 2015) (mean: 14 423 subjects, median: 4189 subjects); longitudinal studies sample sizes ranged between 458 and 245 082 subjects (mean: 21 884 subjects, median: 7134 subjects). The majority of included study populations’ age ranged between 45 and 80 years (n = 38, 92.7%). One study included only males (Tuohy et al., 2005) and one only females (Sheppard and Wallace, 2018). Details on study populations are reported in Table 2, which also reports information on the type of retirement, available for 76% of studies, and outcomes assessment.
More than ninety per cent of included studies used validated tools to diagnose depression-related outcomes, including the Center for Epidemiologic Studies Depression scale (CES-D) in 17 studies (41.5%), the Euro Depression-scale (EURO-D) in eight studies (19.5%), the Geriatric Depression Scale (GDS) in three studies (7.1%) and the Zung Self-rating Depression Scale (ZSDS) in two studies (4.9%). The International Classification of Diseases-10 (ICD-10) was used to identify depression-related conditions in three studies (7.1%). The Patient Health Questionnaire-8 (PHQ-8), the Hospital Anxiety and Depression Scale (HADS), the Composite International Diagnostic Interview (CIDI), the Depression Adjective Check List (DACL) and the Clinical Interview Schedule-Revised (CIS-R) were used in only one study each (Table 2). Three studies (7.1%) used non validated tools to identify depression-related outcomes (Mojon-Azzi et al., 2007; Sheppard and Wallace, 2018; Anxo et al., 2019). Included studies’ quality score (QS) is also reported in Table 2. The mean QS was 15.5/20. The lowest QS was 6 (Farakhan et al., 1984), whereas the highest was 19 (Schwingel et al., 2009; Olesen et al., 2015; Park and Kang, 2016; Van Den Bogaard and Henkens, 2018). Question 7 [Is retirement a main effect, co-variable, confounder, or interaction in the study?] (n = 15) and Question 13 [Was the loss to follow-up appropriately addressed and/or adequately described in the study?] (n = 11) reported the lowest scores (for details on quality appraisal, see online Supplementary Table 2).
Retirement and depression: qualitative reporting
Overall, more than one third (n = 15, 36.6%) of included studies reported a statistically significant negative association between retirement and depression (i.e. retirement decreased the risk of depression) (Farakhan et al., 1984; Tuohy et al., 2005; Butterworth et al., 2006; Schwingel et al., 2009; Coursolle et al., 2010; Calvo et al., 2013; Airagnes et al., 2015, 2016; Bretanha et al., 2015; Belloni et al., 2016; Augner, 2018; Van Den Bogaard and Henkens, 2018; Kolodziej and García-Gómez, 2019; Matta et al., 2020; Han, 2021), 14.6% (n = 6) reported a positive association (Pahkala et al., 1992; Alavinia and Burdorf, 2008; Park and Kang, 2016; Heller-Sahlgren, 2017; Shiba et al., 2017; Arias-De La Torre et al., 2018), while 48.8% (n = 20 studies) did not report statistically significant associations between retirement and depression (Borson et al., 1986; Herzog et al., 1991; Midanik et al., 1995; Reitzes et al., 1996; Fernandez et al., 1998; Kim and Moen, 2002; Buxton et al., 2005; Mojon-Azzi et al., 2007; Behncke, 2012; Choi et al., 2013; Gayman et al., 2013; Leinonen et al., 2013; Olesen et al., 2015; Calvó-Perxas et al., 2016; Mosca and Barrett, 2016; Rhee et al., 2016; Fernández-Niño et al., 2018; Sheppard and Wallace, 2018; Anxo et al., 2019; Noh et al., 2019). The reported ESs included: β coefficients (β) (n = 19), ORs (n = 11), χ2 (n = 3), relative risks (RRs) (n = 1), hazard ratios (HRs) (n = 1) and mean differences (n = 2). Almost all included studies reported adjusted effect estimates (i.e. accounting for age, gender, education, health and marital status; details on multivariate models’ adjustments are reported in Table 2). Two studies reported separate data based on the severity of depression (Alavinia and Burdorf, 2008; Heller-Sahlgren, 2017); two studies reported separate data for short-term (incident) and long-term (persistent) depression (Calvo et al., 2013; Calvó-Perxas et al., 2016); two studies reported separate data by age group (Herzog et al., 1991; Butterworth et al., 2006). Some studies differentiated the analysis by type of retirement, distinguishing between full and partial retirement (Coursolle et al., 2010), retirement for health and non-health reasons (Han, 2021), long-term and new retirement (Kim and Moen, 2002; Shiba et al., 2017), voluntary and involuntary retirement (Mosca and Barrett, 2016; Park and Kang, 2016; Rhee et al., 2016), or considered retirement jointly with volunteering (Schwingel et al., 2009). One study reported separate data for cross-sectional and longitudinal analysis (Schwingel et al., 2009), as reported above.
Fourteen studies reported separate data for men and women (Midanik et al., 1995; Kim and Moen, 2002; Buxton et al., 2005; Butterworth et al., 2006; Coursolle et al., 2010; Olesen et al., 2015; Airagnes et al., 2016; Belloni et al., 2016; Calvó-Perxas et al., 2016; Park and Kang, 2016; Shiba et al., 2017; Arias-De La Torre et al., 2018; Fernández-Niño et al., 2018; Kolodziej and García-Gómez, 2019); two studies reported separate data based on ethnicity (Gayman et al., 2013; Fernandez et al., 1998); one study reported independent results based on the country (Fernández-Niño et al., 2018), so they were considered separately. Among included studies, data from two studies were not extractable (Farakhan et al., 1984; Pahkala et al., 1992). Three studies did not report ESs and CIs (Herzog et al., 1991; Fernandez et al., 1998) or outcomes comparable to other works (Leinonen et al., 2013) and were not included in the quantitative analysis.
Retirement and depression: quantitative reporting and meta-analysis
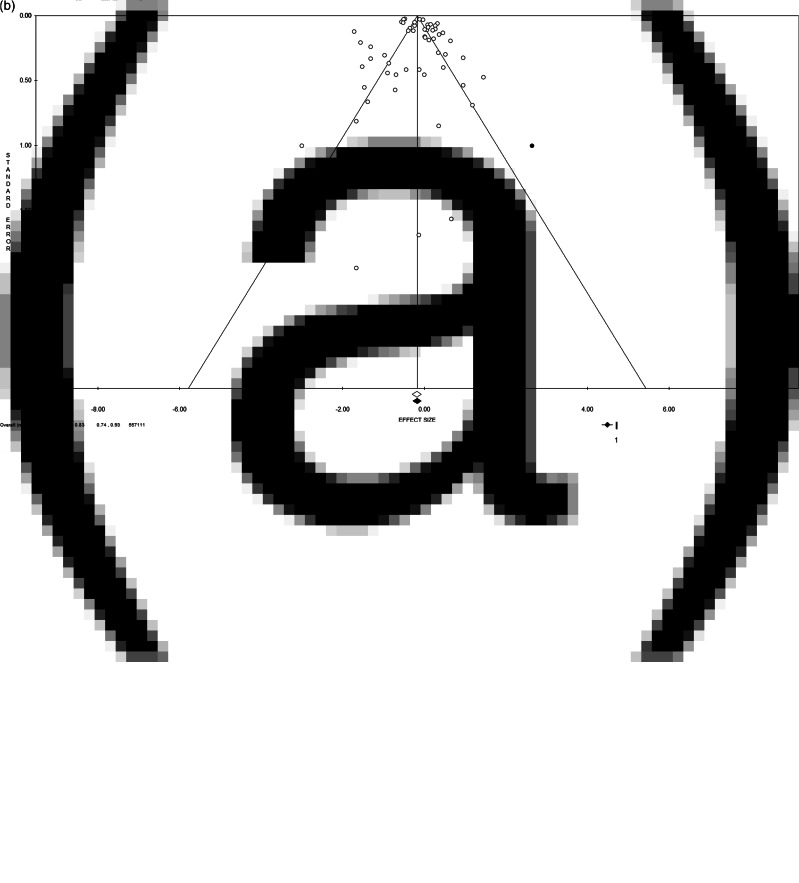
Quantitative pooling of effect estimates was conducted on a total of 557 111 subjects from 60 different databases. Overall, the pooled ES for the risk of depression when retired is 0.83 (95% CI = 0.74–0.93, p-value = 0.001, Fig. 2a), with high statistical heterogeneity (χ2 = 895.19, df = 59, I2 = 93.41, p-value < 0.001). The funnel plot resulted slightly asymmetrical at visual inspection, showing a low potential for publication bias, not confirmed by Egger's linear regression test (Intercept 0.53, t = 0.78, p-value = 0.439). Moreover, the ES change after the trim and fill method was minor [0.84 (95% CI = 0.75–0.94)], and two studies were trimmed in the lower right quarter of the funnel plot (Fig. 2b), suggesting few studies of poor quality could be missing.
Fig. 2.
(a) Forest plot and (b) funnel plot (after trim and fill method) of the meta-analysis assessing the association between retirement and depression. ES, effect size; CI, confidence interval.
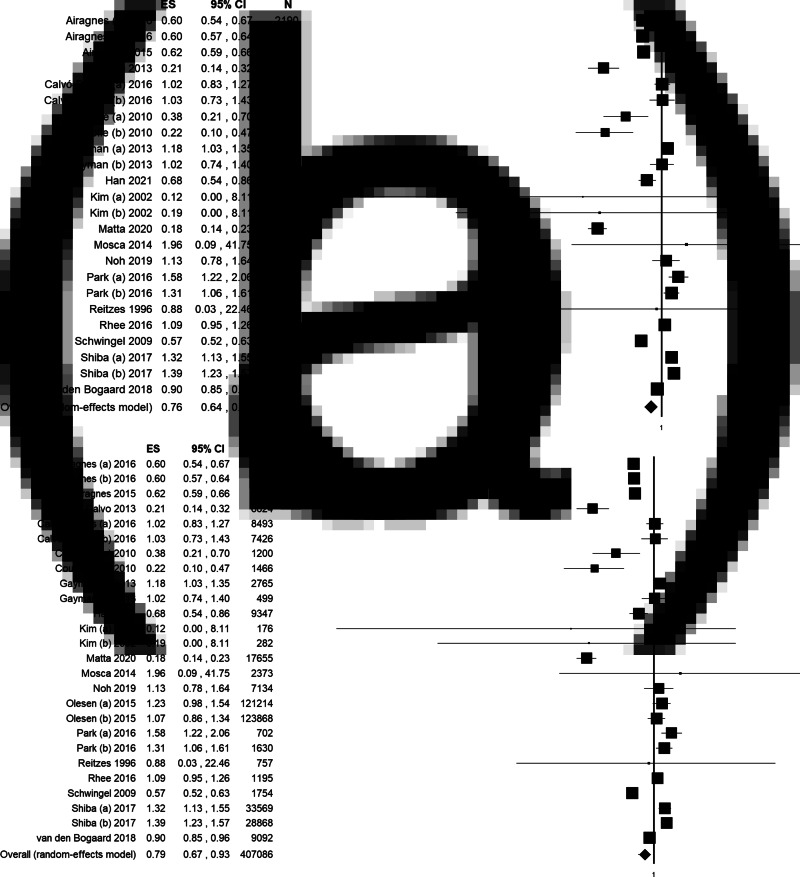
Results of the sensitivity and subgroup analyses are summarised in Table 3. We performed a sensitivity analysis, progressively increasing the quality of included studies in order to test our overall results’ consistency. First, we limited the analysis to studies of the highest quality (QS equal or higher than 15): 47 datasets and 485 092 subjects were included in the meta-analysis, reporting a consistent statistically significant association between retirement and decreased risk of depression (ES = 0.79, 95% CI = 0.68–0.91, p-value = 0.001, online Supplementary Fig. 1a). Then, we limited the analysis to studies with high QS and using validated assessment tools to diagnose depression. In this analysis, 44 datasets were included, for a total of 239 453 subjects, strengthening the significant association between retirement and decreased risk of depression (ES = 0.76, 95% CI = 0.65–0.88, p-value < 0.001, online Supplementary Fig. 1b). Finally, only studies (i) with a QS equal or higher than 15, (ii) using validated assessment tools to diagnose depression and (iii) with a longitudinal study design were included. We report a statistically significant association between retirement and depression (ES = 0.76, 95% CI = 0.64–0.90, p-value = 0.001, Fig. 3a) based on 24 datasets and 162 004 subjects. High statistical heterogeneity and slight visual asymmetry of the funnel plot were observed at each step of the analysis (Table 3), with the exception of the last one restricted to longitudinal studies of the highest quality, when estimated ES did not change with the trim and fill method.
Table 3.
Results of overall, sensitivity and subgroup analyses
| Type of analysis | N. of included datasets | ES | 95% CI, p-value |
N. of participants | χ2; df | I2 | p-value | Intercepta | t-valuea | p-valuea |
|---|---|---|---|---|---|---|---|---|---|---|
| Overall | 60 | 0.83 | (0.74; 0.93), 0.001 |
557 111 | 895.19; 59 | 93.41 | <0.001 | 0.53 | 0.78 | 0.439 |
| Sensitivity analysis | ||||||||||
| QS ⩾15 | 47 | 0.79 | (0.68; 0.91), 0.001 |
485 092 | 808.42; 46 | 94.31 | <0.0001 | 0.52 | 0.65 | 0.520 |
| QS ⩾15 + validated tool to diagnose depression | 44 | 0.76 | (0.65; 0.88), 0.0001 | 239 453 | 763.78; 43 | 94.37 | <0.0001 | 0.33 | 0.41 | 0.687 |
| QS ⩾15+ validated tool to diagnose depression + longitudinal design | 24 | 0.76 | (0.64; 0.90), 0.001 | 162 004 | 652.18; 23 | 96.47 | <0.001 | 0.85 | 0.52 | 0.607 |
| Subgroup analysis by study design | ||||||||||
| Longitudinal | 26 | 0.79 | (0.67; 0.93), 0.004 |
407 086 | 681.14; 25 | 96.33 | <0.001 | 1.18 | 0.76 | 0.455 |
| Cross-sectional | 33 | 0.89 | (0.76; 1.04), 0.136 |
139 484 | 161.43; 32 | 80.18 | <0.001 | −0.24 | −0.48 | 0.638 |
| Subgroup analysis by gender | ||||||||||
| Women | 21 | 0.79 | (0.61; 1.02), 0.074 |
219 655 | 189.48; 20 | 89.44 | <0.001 | −0.25 | −0.25 | 0.805 |
| Men | 20 | 0.87 | (0.68; 1.11), 0.258 |
223 840 | 252.80; 19 | 92.48 | <0.001 | 0.99 | 0.93 | 0.366 |
df, degree of freedom; ES, Effect Size; N., number; QS, quality score
Egger's linear regression test.
Fig. 3.
Forest plot of subgroups meta-analysis assessing the association between retirement and depression limited to: (a) studies with a quality score (QS) equal or higher than 15, using validated diagnostic tools and with a longitudinal study design; (b) longitudinal studies. ES, effect size; CI, confidence interval.
These results appeared to be dragged by longitudinal studies as, when considering data from longitudinal studies only (26 datasets, 407 086 subjects), a statistically significant association between retirement and depression was equally found (ES = 0.79, 95% CI = 0.67–0.93, p-value = 0.004), with high statistical heterogeneity (χ2 = 681.14, df = 25, I2 = 96.33, p-value < 0.001), but no publication bias, as confirmed by funnel visual inspection and Egger's test (Intercept 1.18, t = 0.76, p-value = 0.455, Table 3, Fig. 3b). On the contrary, no statistically significant association resulted when quantitative pooling was limited to cross-sectional studies (33 datasets, 139 484 subjects) (Table 3, online Supplementary Fig. 2a). In this case, publication bias was suggested by funnel plot visual inspection.
Gender-strata meta-analyses are reported in online Supplementary Fig. 2b and 2c. When only considering women, the analysis included 21 datasets and a total of 219 655 subjects, reporting no statistically significant association between retirement and depression (pooled ES = 0.79, 95% CI = 0.61–1.02, p-value = 0.074) and high heterogeneity (Table 3). About men, the analysis included 20 datasets, for a total of 223 840 participants, reporting a pooled ES of 0.87 (95% CI = 0.68–1.11, p-value = 0.258) and high heterogeneity between studies (Table 3). In both cases, evidence of publication bias was suggested by funnel plot.
Discussion
Pooled data from 41 original studies and more than half a million subjects suggested that retirement or transition to retirement reduce by nearly 20% the risk of depression or depressive symptoms; such estimates remain consistent when limiting the analysis to longitudinal and high-quality studies.
Before interpreting our findings further, we must account for the considerable heterogeneity among the included studies, which might limit the generalisability of pooled effect estimates. To overcome this and test the results level of strength, we first applied a random-effect model. Secondly, we conducted sensitivity and stratified meta-analyses by study design and QS. The reasons behind the high level of heterogeneity among the included studies are to be explored in light of, on one side, the wide variety of studies’ designs, settings and populations, definitions and methodological quality and, on the other side, of the complex, multi-determinant and multi-mediator relationship between the process of retirement and mental health and wellbeing (Pesaran et al., 1999; Rabe-Hesketh and Skrondal, 2008; Behncke, 2012; Oksanen and Virtanen, 2012; Insler, 2014; Eibich, 2015). We could not retrieve further evidence on the reasons: even excluding one dataset at a time in the meta-analysis to identify potential outliers, heterogeneity persisted (online Supplementary Table 3). However, sensitivity analyses confirmed the results’ consistency.
Despite half of the retrieved studies being cross-sectional, which did not allow us to explore causality, they accounted for less than one-third of included subjects. Another limitation to consider is that duration of retirement was not reported in most studies, so we could not differentiate among the potential risk of depression for short- or long-term exposure to retirement. A subgroup analysis considering the work before retiring was not possible since only two included studies stratified results for this variable (Belloni et al., 2016; Kolodziej and García-Gómez, 2019). Lastly, even if most of the analysed data came from administrative databases or surveys designed for other purposes, some studies had small sample sizes with poor precision in effect estimates.
To the best of our knowledge, this is the first systematic review and meta-analysis pooling all original studies investigating the association of retirement with prevalent and incident depression. We used a comprehensive range of databases and search terms to maximise the number of studies retrieved and minimise the chance of publication bias. Besides, further studies were retrieved from the reference listing of relevant articles. Such a comprehensive and rigorous summary of the available evidence offers several meaningful insights, valuable to plan, implement and evaluate public health and preventive strategies, public policies, as well as future avenues of research.
Despite the well-known assumption that considers retirement as a potentially stressful life event (Kremer, 1985; Ekerdt, 1987; Salokangas and Joukamaa, 1991), one of our review's critical findings is that retiring does not necessarily harm an individual's mental health but possibly decrease the risk of depression, as a balance of contextual and individual-level variables impact on such association. In conceptual frameworks proposed in the ageing research literature (Van Solinge, 2007), these variables were categorised into: (i) characteristics of the retirement transition, (ii) characteristics of the job, (iii) access to resources, (iv) individual appraisal and (v) gender.
Characteristics of the transition refer to the type and conditions of retirement, which were available in 76% of included studies. For instance, we report different impacts on depression between voluntary and involuntary retirement, with the more considerable impact of the latter (Mosca and Barrett, 2016), suggesting elements of desirability and degree of control might play a role in the association (Van Solinge, 2007).
There is extensive literature on how employment characteristics influence health after retirement (Hernberg, 2001; Robroek et al., 2013; De Wind et al., 2014, 2015; Soh et al., 2016; Ardito et al., 2020). As emerges from original data, among job characteristics, employment history, time pressure, workload and physical demand may impact the risk of mental health disorders’ onset after retirement (Thoits, 1983; Shultz et al., 1998).
With reference to resources, access to social and financial resources around retirement might compensate and mitigate the impact of lifestyle changes and the psychological consequences of retiring. We reviewed data where the risk of depression at retirement is differentially distributed by household socioeconomic status (Arias-De La Torre et al., 2018), marital and family relations (Park and Kang, 2016), social engagement (Sabbath et al., 2015; Shiba et al., 2017): as the studies suggest, reliable financial resources, social networks and marriage can mitigate negative health repercussions of retirement (Deeg and Bath, 2003).
Concerning individual appraisal, personality characteristics influence the meaning assigned to retirement and the ability to cope with this change. Negative expectations and fears about retirement are more likely related to adverse repercussions on individuals’ wellbeing (Barnes-Farrell, 2003). Moreover, having confidence in coping with changes determines fewer difficulties in adjusting to retirement (Van Solinge and Henkens, 2005).
Regarding gender, differences in primary role between women and men, at home and work, respectively, could explain differences in adapting to the event and in health outcomes by gender (Moen, 1996), but need to be further explored.
Overall and sensitivity analyses results are consistent with other reviews on the topic. Van Der Heide et al. (2013) focused on mental health and antidepressant use in longitudinal studies. They registered an improvement in mental health shortly after retirement, possibly linked to work pressure reduction, even if with gender differences. Schaap et al. (2018) analysed the health effects of an exit from work across different socioeconomic groups. They found out that, despite significant heterogeneity, withdrawal from work had more positive effects among employees with a higher socioeconomic status than with a lower position. On the contrary, a systematic review was previously conducted on the effects of working or volunteering beyond statutory retirement ages on mental health by Maimaris et al. (2010); they suggested that, through the mechanism of maintaining a productive societal role with a continued income and social support, working beyond retirement age might be beneficial for mental health. Nevertheless, the benefits were not universal, but they varied greatly by lifestyles, self-esteem and socioeconomic status.
Implications for public health policies and practice
Regarding public health and preventive strategies, we demonstrated that, besides other factors influencing the risk of late-life depression, transition to retirement, as a life event that almost the entire population experience at some point (Clark and Oswald, 1994), has an independent effect in itself. The transition is differentially distributed by contextual and individual-level characteristics and, as such, could be identified as a target point for mental health prevention, including both primary and secondary interventions. We claim that primary prevention interventions, aimed at promoting healthy lifestyles and supporting social roles, could be effectively directed towards subjects who do not benefit from retirement flexibility and its protective effect on short- and long-term risk of late-life depression (Smit et al., 2006; Barnett et al., 2012; Lindwall et al., 2017). As life-course transitions tend to bring along lifestyle changes, synchronising them with public health interventions might be a successful approach (Ben-Shlomo and Kuh, 2002; Werkman et al., 2010; Heaven et al., 2013, 2016). Along the same lines, secondary prevention, including early depressive symptoms detection, could be effectively targeted to older workers still employed, with particular reference to interventions implemented at the primary care level (Okereke et al., 2013; Costantini et al., 2021).
About public policies, our data complement the accumulating evidence on the impact of pension reforms on health and mental health (Eibich, 2015; Carrino et al., 2020), suggesting that older workers should be granted greater flexibility in the timing of retirement in order to reduce their mental burden and avoid the development of severe depression. As many countries are implementing budget reductions to social welfare (Hall and Soskice, 2001), it is crucial to retrieve solid evidence on how different retirement policies might impact healthy ageing to balance money saved from cuts to pension systems with direct and indirect costs passed onto healthcare and social support systems. Although our review only focuses on mental health, the burden of mental health and, in particular, of depression is known to be associated with the burden of chronic physical conditions that significantly affect people's quality of later life, their demands for healthcare and other publicly funded services, generating significant societal consequences (Bech et al., 2011; Hughes et al., 2011; Rechel et al., 2013).
Recommendations for future research
Concerning research, it clearly emerges from our analysis that, in order to reduce heterogeneity and accumulate solid evidence, shared methodological standards and definitions should be followed in the future. More extended longitudinal studies should be preferred so as to reduce inverse causality issues and might help disentangle and quantify the different components that mediate the effects of retirement on the risk of depression and its determinants and monitor such association's temporal evolution. It would also be necessary to further differentiate between contextual and individual characteristics to adapt coping strategies at the public health and clinical levels. Special attention should be paid to health inequalities to investigate better socioeconomic status indicators role in the relationship between retirement and health (Adler et al., 1994) and address the impact of specific policies focusing on health promotion for disadvantaged groups (Rechel et al., 2013). Stratifying results by job and retirement type and by socioeconomic status might be helpful to fill the gaps in current literature.
Conclusions
As a matter of fact, despite current trends in extending working lives, life expectancy after regular retirement is projected to grow faster than increases in the pension age, reaching 20.3 years for men and 24.6 years for women in 2050 (OECD, 2011). Therefore, from a societal, welfare and public health perspective, it is essential to invest in ‘third age’ health and wellbeing (Crimmins, 2015). In a progressively ageing society, strengthened efforts are needed to make health interests count in welfare and pension policies and promote health protection after retirement (Moen, 1996). We call for a coordinated advocacy action to identify retirement as a gateway for healthy lifestyles and an entry point for mental health prevention. Multidisciplinary collaborations between social sciences, public and community health, preventive medicine and psychiatry could be fruitfully put in place to generate much-needed evidence on the determinants, mediators and effect modifiers of the association between retirement and depression, as well as to design preventive interventions targeting older workers.
Acknowledgements
For his conceptual insights and helpful discussion, we especially would like to thank the former Minister of Labour and social security, Professor Tiziano Treu.
Data
The datasets supporting the conclusions of this study are available from the corresponding author upon request.
Financial support
The present study is funded by: (i) Fondazione Cariplo, Grant: Aging and social research 2018: people, places and relations. Project: Pension reforms and spatial-temporal patterns in healthy ageing in Lombardy: quasi-natural experimental analysis of linked health and pension data in comparative Italian and European perspective (project n. 2018-0863); and (ii) the Italian Ministry of Health (project n. RF-2016-02364270).
Ethical standards
Ethical approval was not required because this study retrieved and synthesised data from already published studies.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/ 10.1017/S2045796021000627.
click here to view supplementary material
Conflict of interest
The authors declare that they have no competing interests.
References
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL and Syme SL (1994) Socioeconomic status and health. The challenge of the gradient. American Psychologist 49, 15–24. [DOI] [PubMed] [Google Scholar]
- Airagnes G, Lemogne C, Consoli SM, Schuster JP, Zins M and Limosin F (2015) Personality moderates the improvement of depressive symptoms after retirement: evidence from the GAZEL cohort. The American Journal of Geriatric Psychiatry 23, 941–949. [DOI] [PubMed] [Google Scholar]
- Airagnes G, Lemogne C, Hoertel N, Goldberg M, Limosin F and Zins M (2016) Childhood adversity and depressive symptoms following retirement in the Gazel cohort. Journal of Psychiatric Research 82, 80–90. [DOI] [PubMed] [Google Scholar]
- Alavinia SM and Burdorf A (2008) Unemployment and retirement and ill-health: a cross-sectional analysis across European countries. International Archives of Occupational and Environmental Health 82, 39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexopoulos GS (2019) Mechanisms and treatment of late-life depression. Translational Psychiatry 9, 188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anxo D, Ericson T and Miao C (2019) Impact of late and prolonged working life on subjective health: the Swedish experience. The European Journal of Health Economics 20, 389–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardito C, Leombruni R, Blane D and D'errico A (2020) To work or not to work? The effect of higher pension age on cardiovascular health. Industrial Relations: A Journal of Economy and Society 59, 399–434. [Google Scholar]
- Arias-De La Torre J, Vilagut G, Martin V, Molina AJ and Alonso J (2018) Prevalence of major depressive disorder and association with personal and socio-economic factors. Results for Spain of the European Health Interview Survey 2014–2015. Journal of Affective Disorders 239, 203–207. [DOI] [PubMed] [Google Scholar]
- Augner C (2018) Health, education and employment status of Europeans aged 60 to 69 years: results from SHARE survey. Industrial Health 56, 436–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes-Farrell JL (2003) Beyond health and wealth: Attitudinal and other influences on retirement decision-making. In Springer (ed.). Retirement: Reasons, Processes and Results. New York: Springer, pp. 159–187. [Google Scholar]
- Barnett I, Van Sluijs EM and Ogilvie D (2012) Physical activity and transitioning to retirement: a systematic review. American Journal of Preventive Medicine 43, 329–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bech M, Christiansen T, Khoman E, Lauridsen J and Weale M (2011) Ageing and health care expenditure in EU-15. The European Journal of Health Economics 12, 469–478. [DOI] [PubMed] [Google Scholar]
- Begg CB and Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50, 1088–1101. [PubMed] [Google Scholar]
- Behncke S (2012) Does retirement trigger ill health? Health Economics 21, 282–300. [DOI] [PubMed] [Google Scholar]
- Belloni M, Meschi E and Pasini G (2016) The effect on mental health of retiring during the economic crisis. Health Economics 25(Suppl. 2), 126–140. [DOI] [PubMed] [Google Scholar]
- Ben-Shlomo Y and Kuh D (2002) A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology 31, 285–293. [PubMed] [Google Scholar]
- Blake H and Garrouste C (2019) Collateral effects of a pension reform in France. Annals of Economics and Statistics 133, 57–86. [Google Scholar]
- Bland JM and Altman DG (2000) Statistics notes. The odds ratio. British Medical Journal 320, 1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borson S, Barnes RA, Kukull WA, Okimoto JT, Veith RC, Inui TS, Carter W and Raskind MA (1986) Symptomatic depression in elderly medical outpatients. I. Prevalence, demography, and health service utilization. Journal of the American Geriatrics Society 34, 341–347. [DOI] [PubMed] [Google Scholar]
- Bossé R, Aldwin CM, Levenson MR and Ekerdt DJ (1987) Mental health differences among retirees and workers: findings from the normative aging study. Psychology and Aging 2, 383–389. [DOI] [PubMed] [Google Scholar]
- Bosse R, Aldwin CM, Levenson MR and Workman-Daniels K (1991) How stressful is retirement? Findings from the normative aging study. Journal of Gerontology 46, P9–14. [DOI] [PubMed] [Google Scholar]
- Bretanha AF, Facchini LA, Nunes BP, Munhoz TN, Tomasi E and Thume E (2015) Depressive symptoms in elderly living in areas covered by primary health care units in urban area of Bage, RS. Revista Brasileira de Epidemiologia 18, 1–12. [DOI] [PubMed] [Google Scholar]
- Brown P, Brunnhuber K, Chalkidou K, Chalmers I, Clarke M, Fenton M, Forbes C, Glanville J, Hicks NJ, Moody J, Twaddle S, Timimi H and Young P (2006) How to formulate research recommendations. British Medical Journal 333, 804–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butterworth P, Gill SC, Rodgers B, Anstey KJ, Villamil E and Melzer D (2006) Retirement and mental health: analysis of the Australian national survey of mental health and well-being. Social Science & Medicine 62, 1179–1191. [DOI] [PubMed] [Google Scholar]
- Buxton JW, Singleton N and Melzer D (2005) The mental health of early retirees – national interview survey in Britain. Social Psychiatry and Psychiatric Epidemiology 40, 99–105. [DOI] [PubMed] [Google Scholar]
- Calvó-Perxas L, Vilalta-Franch J, Turro-Garriga O, Lopez-Pousa S and Garre-Olmo J (2016) Gender differences in depression and pain: a two-year follow-up study of the survey of health, ageing and retirement in Europe. Journal of Affective Disorders 193, 157–164. [DOI] [PubMed] [Google Scholar]
- Calvo E, Sarkisian N and Tamborini CR (2013) Causal effects of retirement timing on subjective physical and emotional health. The Journal of Gerontology, Series B: Psychological Sciences and Social Sciences 68, 73–84. [DOI] [PubMed] [Google Scholar]
- Carrino L, Glaser K and Avendano M (2020) Later retirement, job strain, and health: evidence from the new state pension age in the United Kingdom. Health Economics 29, 891–912. [DOI] [PubMed] [Google Scholar]
- Celidoni M and Rebba V (2017) Healthier lifestyles after retirement in Europe? Evidence from SHARE. The European Journal of Health Economics 18, 805–830. [DOI] [PubMed] [Google Scholar]
- Choi KS, Stewart R and Dewey M (2013) Participation in productive activities and depression among older Europeans: Survey of Health, Ageing and Retirement in Europe (SHARE). International Journal of Geriatric Psychiatry 28, 1157–1165. [DOI] [PubMed] [Google Scholar]
- Clark A and Oswald AJ (1994) Unhappiness and unemployment. The Economic Journal 104, 648–659. [Google Scholar]
- Costantini L, Pasquarella C, Odone A, Colucci ME, Costanza A, Serafini G, Aguglia A, Belvederi Murri M, Brakoulias V, Amore M, Ghaemi SN and Amerio A (2021) Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): a systematic review. Journal of Affective Disorders 279, 473–483. [DOI] [PubMed] [Google Scholar]
- Coursolle KM, Sweeney MM, Raymo JM and Ho JH (2010) The association between retirement and emotional well-being: does prior work-family conflict matter? The Journal of Gerontology. Series B: Psychological Sciences and Social Sciences 65, 609–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM (2015) Lifespan and healthspan: past, present, and promise. The Gerontologist 55, 901–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeg DJ and Bath PA (2003) Self-rated health, gender, and mortality in older persons: introduction to a special section. The Gerontologist 43, 369–371. [DOI] [PubMed] [Google Scholar]
- De Wind A, Geuskens GA, Ybema JF, Blatter BM, Burdorf A, Bongers PM and Van Der Beek AJ (2014) Health, job characteristics, skills, and social and financial factors in relation to early retirement--results from a longitudinal study in the Netherlands. Scandinavian Journal of Work, Environment & Health 40, 186–194. [DOI] [PubMed] [Google Scholar]
- De Wind A, Geuskens GA, Ybema JF, Bongers PM and Van Der Beek AJ (2015) The role of ability, motivation, and opportunity to work in the transition from work to early retirement – testing and optimizing the early retirement model. Scandinavian Journal of Work, Environment & Health 41, 24–35. [DOI] [PubMed] [Google Scholar]
- Dietz T, Frey S and Kalof L (1987) Estimation with cross-national data: robust and nonparametric approaches. American Sociological Review 52, 380–390. [Google Scholar]
- Drentea P (2002) Retirement and mental health. Journal of Aging and Health 14, 167–194. [DOI] [PubMed] [Google Scholar]
- Duval S and Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56, 455–463. [DOI] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M and Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. British Medical Journal 315, 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eibich P (2015) Understanding the effect of retirement on health: mechanisms and heterogeneity. Journal of Health Economics 43, 1–12. [DOI] [PubMed] [Google Scholar]
- Ekerdt DJ (1987) Why the notion persists that retirement harms health. The Gerontologist 27, 454–457. [DOI] [PubMed] [Google Scholar]
- Farakhan A, Lubin B and O'connor WA (1984) Life satisfaction and depression among retired black persons. Psychological Reports 55, 452–454. [DOI] [PubMed] [Google Scholar]
- Fernández-Niño JA, Bonilla-Tinoco LJ, Manrique-Espinoza BS, Romero-Martinez M and Sosa-Ortiz AL (2018) Work status, retirement, and depression in older adults: an analysis of six countries based on the Study on Global Ageing and Adult Health (SAGE). SSM – Population Health 6, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez ME, Mutran EJ, Reitzes DC and Sudha S (1998) Ethnicity, gender, and depressive symptoms in older workers. The Gerontologist 38, 71–79. [DOI] [PubMed] [Google Scholar]
- Fleischmann M, Xue B and Head J (2020) Mental health before and after retirement – assessing the relevance of psychosocial working conditions: the Whitehall II prospective study of British civil servants. The Journal of Gerontology, Series B: Psychological Sciences and Social Sciences 75, 403–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gall TL, Evans DR and Howard J (1997) The retirement adjustment process: changes in the well-being of male retirees across time. The Journal of Gerontology, Series B: Psychological Sciences and Social Sciences 52, P110–P117. [DOI] [PubMed] [Google Scholar]
- Gayman MD, Pai M, Kail BL and Taylor MG (2013) Reciprocity between depressive symptoms and physical limitations pre- and postretirement: exploring racial differences. Journal of Aging and Health 25, 555–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianfredi V, Nucci D, Fatigoni C, Salvatori T, Villarini M and Moretti M (2020) Extent of primary DNA damage measured by the comet assay in health professionals exposed to antineoplastic drugs: a systematic review and meta-analysis. International Journal of Environmental Research and Public Health 17, 523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill SC, Butterworth P, Rodgers B, Anstey KJ, Villamil E and Melzer D (2006) Mental health and the timing of men's retirement. Social Psychiatry and Psychiatric Epidemiology 41, 515–522. [DOI] [PubMed] [Google Scholar]
- Gum AM, Shiovitz-Ezra S and Ayalon L (2017) Longitudinal associations of hopelessness and loneliness in older adults: results from the US health and retirement study. International Psychogeriatrics 29, 1451–1459. [DOI] [PubMed] [Google Scholar]
- Hailpern SM and Visintainer PF (2003) Odds ratios and logistic regression: further examples of their use and interpretation. The Stata Journal 3, 213–225. [Google Scholar]
- Hall P and Soskice DW (2001) Varieties of Capitalism: The Institutional Foundations of Comparative Advantage. Oxford: Oxford University Press. [Google Scholar]
- Han SH (2021) Health consequences of retirement due to non-health reasons or poor health. Social Science & Medicine 273, 113767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaven B, Brown LJ, White M, Errington L, Mathers JC and Moffatt S (2013) Supporting well-being in retirement through meaningful social roles: systematic review of intervention studies. The Milbank Quarterly 91, 222–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaven B, O'brien N, Evans EH, White M, Meyer TD, Mathers JC and Moffatt S (2016) Mobilizing resources for well-being: implications for developing interventions in the retirement transition. The Gerontologist 56, 615–629. [DOI] [PubMed] [Google Scholar]
- Heller-Sahlgren G (2017) Retirement blues. Journal of Health Economics 54, 66–78. [DOI] [PubMed] [Google Scholar]
- Hernberg S (2001) Work-related factors and mortality – what is the burden? Scandinavian Journal of Work, Environment & Health 27, 157–160. [DOI] [PubMed] [Google Scholar]
- Herzog AR, House JS and Morgan JN (1991) Relation of work and retirement to health and well-being in older age. Psychology and Aging 6, 202–211. [DOI] [PubMed] [Google Scholar]
- Higgins JPT and Green S (2013) Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. London: The Cochrane Collaboration. [Google Scholar]
- Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L and Sterne JA, Cochrane Bias Methods Group & Cochrane Statistical Methods Group (2011) The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. British Medical Journal 343, d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes BB, Kuhn R, Peterson CM, Rothman DS, Solórzano JR, Mathers CD and Dickson JR (2011) Projections of global health outcomes from 2005 to 2060 using the international futures integrated forecasting model. Bulletin of the World Health Organization 89, 478–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insler M (2014) The health consequences of retirement. Journal of Human Resources 49, 195–233. [Google Scholar]
- Jokela M, Ferrie JE, Gimeno D, Chandola T, Shipley MJ, Head J, Vahtera J, Westerlund H, Marmot MG and Kivimäki M (2010) From midlife to early old age: health trajectories associated with retirement. Epidemiology (Cambridge, Mass.) 21, 284–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killinger LZ (2012) Diagnostic challenges in the older patient. Chiropractic & Manual Therapies 20, 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JE and Moen P (2002) Retirement transitions, gender, and psychological well-being: a life-course, ecological model. The Journal of Gerontology, Series B: Psychological Sciences and Social Sciences 57, P212–P222. [DOI] [PubMed] [Google Scholar]
- Kolodziej IWK and García-Gómez P (2019) Saved by retirement: beyond the mean effect on mental health. Social Science & Medicine 225, 85–97. [DOI] [PubMed] [Google Scholar]
- Kremer Y (1985) The association between health and retirement: self-health assessment of Israeli retirees. Social Science & Medicine 20, 61–66. [DOI] [PubMed] [Google Scholar]
- Lang IA, Rice NE, Wallace RB, Guralnik JM and Melzer D (2007) Smoking cessation and transition into retirement: analyses from the English longitudinal study of ageing. Age and Ageing 36, 638–643. [DOI] [PubMed] [Google Scholar]
- Leinonen T, Lahelma E and Martikainen P (2013) Trajectories of antidepressant medication before and after retirement: the contribution of socio-demographic factors. European Journal of Epidemiology 28, 417–426. [DOI] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J and Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Annals of Internal Medicine 151, W65–W94. [DOI] [PubMed] [Google Scholar]
- Lindwall M, Berg AI, Bjälkebring P, Buratti S, Hansson I, Hassing L, Henning G, Kivi M, König S, Thorvaldsson V and Johansson B (2017) Psychological health in the retirement transition: rationale and first findings in the HEalth, Ageing and Retirement Transitions in Sweden (HEARTS) study. Frontiers in Psychology 8, 1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maimaris W, Hogan H and Lock K (2010) The impact of working beyond traditional retirement ages on mental health: implications for public health and welfare policy. Public Health Reviews 32, 532–548. [Google Scholar]
- Matta J, Carette C, Zins M, Goldberg M, Lemogne C and Czernichow S (2020) Obesity moderates the benefit of retirement on health: a 21-year prospective study in the GAZEL cohort. Journal of Psychosomatic Research 131, 109938. [DOI] [PubMed] [Google Scholar]
- Mccall WV and Kintziger KW (2013) Late-life depression: a global problem with few resources. Psychiatric Clinics of North America 36, 475–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mein G, Martikainen P, Hemingway H, Stansfeld S and Marmot M (2003) Is retirement good or bad for mental and physical health functioning? Whitehall II longitudinal study of civil servants. Journal of Epidemiology and Community Health 57, 46–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midanik LT, Soghikian K, Ransom LJ and Tekawa IS (1995) The effect of retirement on mental health and health behaviors: the Kaiser Permanente Retirement Study. The Journal of Gerontology, Series B: Psychological Sciences and Social Sciences 50, S59–S61. [DOI] [PubMed] [Google Scholar]
- Moen P (1996) A life course perspective on retirement, gender, and well-being. Journal of Occupational Health Psychology 1, 131–144. [DOI] [PubMed] [Google Scholar]
- Mojon-Azzi S, Sousa-Poza A and Widmer R (2007) The effect of retirement on health: a panel analysis using data from the Swiss Household Panel. Swiss Medical Weekly 137, 581–585. [DOI] [PubMed] [Google Scholar]
- Mosca I and Barrett A (2016) The impact of voluntary and involuntary retirement on mental health: evidence from older Irish adults. Journal of Mental Health Policy and Economics 19, 33–44. [PubMed] [Google Scholar]
- Nelson JC (2001) Diagnosing and treating depression in the elderly. The Journal of Clinical Psychiatry 62(Suppl. 24), 18–22. [PubMed] [Google Scholar]
- Noh JW, Kwon YD, Lee LJ, Oh IH and Kim J (2019) Gender differences in the impact of retirement on depressive symptoms among middle-aged and older adults: a propensity score matching approach. PLoS One 14, e0212607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD (2011) Pensions at A Glance 2011: Retirement-Income Systems in OECD and G20 Countries. Paris: OECD Publishing. [Google Scholar]
- Okereke OI, Lyness JM, Lotrich FE and Reynolds CF, III (2013) Depression in late-life: a focus on prevention. Focus 11, 22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oksanen T and Virtanen M (2012) Health and retirement: a complex relationship. European Journal of Ageing 9, 221–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olesen K, Rod NH, Madsen IE, Bonde JP and Rugulies R (2015) Does retirement reduce the risk of mental disorders? A national registry-linkage study of treatment for mental disorders before and after retirement of 245,082 Danish residents. Occupational and Environmental Medicine 72, 366–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page MJ, Mckenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, Mcdonald S, Mcguinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P and Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. British Medical Journal 372, n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pahkala K, Kivela SL and Laippala P (1992) Social and environmental factors and major depression in old age. Zeitschrift für Gerontologie und Geriatrie 24, 17–23. [PubMed] [Google Scholar]
- Park H and Kang MY (2016) Effects of voluntary/involuntary retirement on their own and spouses' depressive symptoms. Comprehensive Psychiatry 66, 1–8. [DOI] [PubMed] [Google Scholar]
- Pesaran M, Shin and Y and Smith RP (1999) Pooled mean group estimation of dynamic heterogeneous panels. Journal of the American Statistical Association 94, 621–34. [Google Scholar]
- Portnoi VA (1981) The natural history of retirement. Mainly good news. JAMA 245, 1752–1754. [PubMed] [Google Scholar]
- Rabe-Hesketh S and Skrondal A (2008) Multilevel and Longitudinal Modelling Using Stata. College Station: STATA Press. [Google Scholar]
- Rechel B, Grundy E, Robine JM, Cylus J, Mackenbach JP, Knai C and Mckee M (2013) Ageing in the European Union. Lancet (London, England) 381, 1312–1322. [DOI] [PubMed] [Google Scholar]
- Reitzes DC, Mutran EJ and Fernandez ME (1996) Does retirement hurt well-being? Factors influencing self-esteem and depression among retirees and workers. The Gerontologist 36, 649–656. [DOI] [PubMed] [Google Scholar]
- Rhee MK, Mor Barak ME and Gallo WT (2016) Mechanisms of the effect of involuntary retirement on older adults' self-rated health and mental health. Journal of Gerontological Social Work 59, 35–55. [DOI] [PubMed] [Google Scholar]
- Robroek SJ, Schuring M, Croezen S, Stattin M and Burdorf A (2013) Poor health, unhealthy behaviors, and unfavorable work characteristics influence pathways of exit from paid employment among older workers in Europe: a four-year follow-up study. Scandinavian Journal of Work, Environment & Health 39, 125–133. [DOI] [PubMed] [Google Scholar]
- Ronchetti C, Toffolutti V, Mckee M and Stuckler D (2020) The quantification of the psychiatric revolution: a quasi-natural experiment of the suicide impact of the Basaglia Law. European Journal of Public Health 30, 521–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabbath EL, Lubben J, Goldberg M, Zins M and Berkman LF (2015) Social engagement across the retirement transition among “young-old” adults in the French GAZEL cohort. European Journal of Ageing 12, 311–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salokangas RK and Joukamaa M (1991) Physical and mental health changes in retirement age. Psychotherapy and Psychosomatics 55, 100–107. [DOI] [PubMed] [Google Scholar]
- Schaap R, De Wind A, Coenen P, Proper K and Boot C (2018) The effects of exit from work on health across different socioeconomic groups: a systematic literature review. Social Science & Medicine 198, 36–45. [DOI] [PubMed] [Google Scholar]
- Schwingel A, Niti MM, Tang C and Ng TP (2009) Continued work employment and volunteerism and mental well-being of older adults: Singapore longitudinal ageing studies. Age and Ageing 38, 531–537. [DOI] [PubMed] [Google Scholar]
- Segel-Karpas D, Ayalon L and Lachman ME (2018) Loneliness and depressive symptoms: the moderating role of the transition into retirement. Aging and Mental Health 22, 135–140. [DOI] [PubMed] [Google Scholar]
- Sheppard FH and Wallace DC (2018) Women's mental health after retirement. Journal of Psychosocial Nursing and Mental Health Services 56, 37–45. [DOI] [PubMed] [Google Scholar]
- Shi L and Lin L (2019) The trim-and-fill method for publication bias: practical guidelines and recommendations based on a large database of meta-analyses. Medicine 98, e15987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiba K, Kondo N, Kondo K and Kawachi I (2017) Retirement and mental health: dose social participation mitigate the association? A fixed-effects longitudinal analysis. BMC Public Health 17, 526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim MJ, Gimeno D, Pruitt SL, Mcleod CB, Foster MJ and BC A (2013) A systematic review of retirement as a risk factor for mortality. Applied Demography and Public Health 3, 277–309. [Google Scholar]
- Shultz KS, Morton KR and Weckerle JR (1998) The influence of push and pull factors on voluntary and involuntary early retirees’ retirement decision and adjustment. Journal of Vocational Behavior 53, 45–57. [Google Scholar]
- Smit F, Ederveen A, Cuijpers P, Deeg D and Beekman A (2006) Opportunities for cost-effective prevention of late-life depression: an epidemiological approach. Archives of General Psychiatry 63, 290–296. [DOI] [PubMed] [Google Scholar]
- Soh M, Zarola A, Palaiou K and Furnham A (2016) Work-related well-being. Health Psychology Open 3, 2055102916628380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA and Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283, 2008–2012. [DOI] [PubMed] [Google Scholar]
- Stuckler D (2017) Introduction to natural experiments: from John Snow through to the present: David Stuckler. European Journal of Public Health 27, 17. [Google Scholar]
- Sutton AJ, Duval SJ, Tweedie RL, Abrams KR and Jones DR (2000) Empirical assessment of effect of publication bias on meta-analyses. British Medical Journal 320, 1574–1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ter Hoeve N, Ekblom M, Galanti MR, Forsell Y and Nooijen CFJ (2020) Unfavourable sedentary and physical activity behaviour before and after retirement: a population-based cohort study. BMJ Open 10, e037659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits PA (1983) Dimensions of life events that influence psychological distress: an evaluation and synthesis of the literature. In Academic Press (ed.). Psychosocial Stress: Trends in Theory and Research. New York: Academic Press, pp. 33–103. [Google Scholar]
- Tuohy A, Knussen C and Wrennall MJ (2005) Effects of age on symptoms of anxiety and depression in a sample of retired police officers. Psychology and Aging 20, 202–210. [DOI] [PubMed] [Google Scholar]
- United Nations DOEaSA, Population Division (2015) World Population Ageing 2015. New York: United Nations. [Google Scholar]
- Vahtera J, Westerlund H, Hall M, Sjösten N, Kivimäki M, Sal OP, Ferrie JE, Jokela M, Pentti J, Singh-Manoux A, Goldberg M and Zins M (2009) Effect of retirement on sleep disturbances: the GAZEL prospective cohort study. Sleep 32, 1459–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Den Bogaard L and Henkens K (2018) When is quitting an escape? How different job demands affect physical and mental health outcomes of retirement. European Journal of Public Health 28, 815–819. [DOI] [PubMed] [Google Scholar]
- Van Der Heide I, Van Rijn RM, Robroek SJ, Burdorf A and Proper KI (2013) Is retirement good for your health? A systematic review of longitudinal studies. BMC Public Health 13, 1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Solinge H (2007) Health change in retirement: a longitudinal study among older workers in the Netherlands. Research on Aging 29, 225–256. [Google Scholar]
- Van Solinge H and Henkens K (2005) Couples' adjustment to retirement: a multi-actor panel study. The Journal of Gerontology, Series B: Psychological Sciences and Social Sciences 60, S11–S20. [DOI] [PubMed] [Google Scholar]
- Vigezzi GP, Gaetti G, Gianfredi V, Frascella B, Gentile L, D'errico A, Stuckler D, Ricceri F, Costa G and Odone A (2021) Transition to retirement impact on health and lifestyle habits: analysis from a nationwide Italian cohort. BMC Public Health 21, 1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werkman A, Hulshof PJ, Stafleu A, Kremers SP, Kok FJ, Schouten EG and Schuit AJ (2010) Effect of an individually tailored one-year energy balance programme on body weight, body composition and lifestyle in recent retirees: a cluster randomised controlled trial. BMC Public Health 10, 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westerlund H, Vahtera J, Ferrie JE, Singh-Manoux A, Pentti J, Melchior M, Leineweber C, Jokela M, Siegrist J, Goldberg M, Zins M and Kivimäki M (2010) Effect of retirement on major chronic conditions and fatigue: French GAZEL occupational cohort study. British Medical Journal 341, c6149. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/ 10.1017/S2045796021000627.
click here to view supplementary material