Abstract
Background:
Exposure to high fluoride levels in drinking water can lead to a number of adverse effects in children, including cognitive dysfunction. Despite being endemic for fluorosis, studies on its effect on the cognitive function of children are lacking in Kerala.
Aims:
The aim of this study was to compare the cognitive function of school children with fluorosis with that of normal children and to correlate between the severity of dental fluorosis and cognitive function.
Settings and Design:
Cross-sectional study, conducted in collaboration with the National Fluorosis Control Programme, among school children in Alappuzha district, Kerala.
Methods:
Children aged 8–10 years, studying in 2 lower primary schools in Alappuzha district with confirmed fluorosis were selected, and compared with healthy age- and sex-matched children from the same school. Raven's Standard Progressive Matrices and MISIC digit span subtest were used to assess the cognitive function.
Statistical Analysis:
Continuous variables were assessed by independent samples t test and categorical variables by Chi-square test. The relationship between severity of dental fluorosis and grade of cognitive impairment was assessed using Spearman's correlation.
Results:
There were 60 children each in fluorosis and control groups. The mean age of the children was 8.95 ± 0.50. Only 15% of the children with fluorosis scored Grade I and II Raven's SPM grades (Intellectually superior/above the average) versus 30% in the control group. None of the children without fluorosis scored Grade V (intellectually impaired) category versus 20% in the fluorosis group. The mean digit span was significantly higher in the control group. A strong positive correlation between severity of dental fluorosis and Raven's SPM grades was found (Spearman's correlation coefficient = 0.740).
Conclusions:
Fluorosis is associated with impaired cognition in children. There is a positive correlation between severity of dental fluorosis and the grade of cognitive impairment.
Keywords: Cognitive function, dental fluorosis, MISIC digit span test, Raven's SPM
INTRODUCTION
People of at least 19 states in India are drinking fluoride contaminated water above World Health Organization's (WHO) maximum allowed concentration of 1.5 mg/L.[1,2] Around 62 million people in India suffer from fluorosis-related health problems, of which 6 million are children below the age of 14 years.[3] Though fluoride prevents dental caries at low concentrations in drinking water, exposure to high fluoride levels in drinking water can give rise to a number of adverse effects.[4] As the level and duration of fluoride exposure increases, these can range from mild dental fluorosis to severe skeletal and non-skeletal fluorosis, including neurological manifestations.[5] Further, fluoride being a highly reactive ion, interacts with multiple body tissues, and has been linked to preterm delivery, abortions, still births and also has detrimental effects on developing brain.[3,6]
In the south Indian state of Kerala, out of the fourteen districts, two districts, Alappuzha and Palakkad, are considered endemic for fluorosis.[7] Dental fluorosis, a convenient biomarker of fluoride exposure has been reported to have prevalence of 35.6% in Alappuzha district.[8] Despite being endemic for fluorosis and having high prevalence of dental fluorosis, the association between fluorosis and cognitive function of children in this region has not been investigated yet. This is the first study conducted in Kerala to study the association between fluorosis and cognitive function. In this study, we aimed to assess the effect of fluorosis on the cognitive function of school-going children in Alappuzha district, Kerala, comparing children with dental fluorosis with those without. We also aimed to investigate the relationship between severity of dental fluorosis and the cognitive function of children with fluorosis.
METHODS
A cross-sectional study was carried out among children aged 8–10 yrs studying in two lower primary schools in Alappuzha district, Kerala from January 2018 to December 2018. The study was conducted after obtaining clearance from the Institutional Ethics Committee. Informed written consent was taken from the guardians of all children participating in the study and from children themselves. This study was conducted in collaboration with the National Programme for Prevention and Control of Fluorosis (NPPCF) implemented by the Department of Health Services, after getting permission from the District Medical Officer, Alappuzha.
The inclusion criteria of the study were children 8–10 years of age with normal antenatal, birth and developmental history, who were continuous residents of the study area since birth, presence of dental fluorosis, drinking water fluoride concentration >1 parts per million (ppm) and urine fluoride level >1 mg/mL.
The exclusion criteria of the study were children with anemia (hemoglobin < 11.5 g/dL) and hypothyroidism (thyroid stimulating hormone [TSH] > 5.0 IU/mL), history of head injury or other neurological disorder, congenital or acquired diseases affecting intelligence, history of chronic illness or on any chronic medication. Children with severe extrinsic stains on the teeth which interfere with assessment of dental fluorosis status and those who had a change in the source of drinking water since birth were also excluded.
Control group consisted of children aged 8-10 years with normal antenatal, birth, and developmental history, who were continuous residents of the study area since birth and having no evidence of dental fluorosis.
Sample size
Khan et al. in a 2015 study of 6–12-year-old children revealed that 25% of children with dental fluorosis had extremely low or borderline intelligence quotient (IQ) scores whereas none of children without fluorosis had extremely low or borderline IQ scores.[9] Previous community-based studies have documented varied prevalence rates for intellectual disability (ID) among children in India, ranging between 1% and 4%.[10,11] Arora NK, et al. in a multi-centric study that evaluated the prevalence of neurodevelopmental disorders in children across five regions in India, reported a prevalence of intellectual disability to be 3.1% in children between 2 to 6 years and 5.2% in children between 6 to 9 years of age.[12]
Assuming prevalence of cognitive dysfunction in fluorosis group to be 25% and control group to be 5.2%, the sample size required (for a power of 80%), was calculated to be 48 each in the two groups using the Pocock's formula[13]
Sampling and study procedure
Under the National Programme for Prevention and Control of Fluorosis implemented by department of health services, school children are routinely screened for dental fluorosis.[7] From this database, those children with dental fluorosis are picked up and their urine tested to confirm fluorosis (urine fluoride level >1 mg/mL by fluoride ion meter). Severity of dental fluorosis in these children is graded using Dean's Fluorosis Index.[14] This data was availed and two lower primary schools (Govt. L P school, Kalarcode and C.M.S. L.P school, Kommady) were randomly selected by lottery method. Permission was obtained from the Assistant Educational Officer, Alappuzha and the headmasters of the two schools to conduct the study.
A total of 60 children with fluorosis (30 from each school) and an equal number of healthy age and sex matched children without fluorosis from the same school were selected by simple random sampling. The areas selected for the study were similar in climatic conditions, with majority of the population belonging to medium socio-economic status with similar standards of living, quality of education, medical facilities and cultural status. The children included in the study had comparable physical health and nutrition. All the children studying in the two schools were residing within a radius of 1-2 kilometers. The study procedure was explained in detail to the children and their parents. Consent forms were given and those who were willing for the study were included. Parents and children were interviewed. Blood samples for hemoglobin and TSH testing were collected at Government T D Medical College Hospital, Alappuzha.
The cognitive function of the two populations was assessed by two well validated neuropsychometric tests: Raven's standard progressive matrices and Malin's Intelligence Scale for Indian Children (MISIC) digit span test.
Study tools and definitions
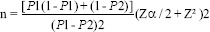
Dean's Fluorosis Index was used to assess the severity of dental fluorosis.[14] It was graded as normal, questionable, very mild, mild, moderate, and severe, and for purpose of this study coded as 0, 1, 2, 3, 4, 5 respectively [Figure 1].
Figure 1.
Dean's fluorosis index - grading and code
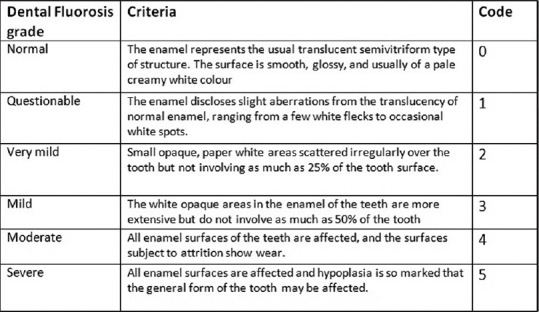
The Raven's Standard Progressive Matrices (Raven's SPM) is a 60-item test for measuring abstract reasoning, considered a nonverbal estimate of fluid intelligence.[15] It is independent of the educational status or experience of the test taker, and is well validated in groups ranging from 5-year-olds to the elderly.[16] It consists of 60 multiple choice questions, listed in order of increasing difficulty. The booklet comprises five sets (A to E) of 12 items each (e.g., A1 through A12), with items within a set becoming increasingly difficult. All items are presented in black ink on a white background. Children were given a time limit of 30 minutes, to complete the test, according to the test manual. The results obtained were converted into percentile and then overall score was graded as per the guidelines of Raven's SPM manual [Figure 2].
Figure 2.
Raven's Standard Progressive Matrices - grading
Malin's Intelligence Scale for Indian Children (MISIC) is an Indian adaptation of the Weschler Intelligence Scale for Children (WISC) developed to assess the cognitive abilities of children.[17] This is used for children aged 6 to 15 years. This battery comprises 11 sub-tests, one among which is the digit span test. Digit spans of increasing length were presented, and the children were asked to repeat strings of digits. Scores were taken as total number of correct trials forward and backward.
Statistical analysis
Analysis of data was carried out using Statistical Package for the Social Sciences (SPSS) software, version 25.0 (IBM). Categorical variables were presented as percentage. Quantitative variables were expressed as Mean ± standard deviation. The proportion of children with cognitive impairment in both groups was compared using Chi-square test. The relationship between severity of dental fluorosis and grade of cognitive impairment was assessed using Spearman's correlation. The MISIC digit span scores and Raven's SPM raw score were compared between the groups, using independent samples t test.
RESULTS
A total of 120 subjects were included in the study, 60 each in the fluorosis and control groups, after applying inclusion and exclusion criteria. Of the 60 children in each group, 31 (52%) were females and the rest were males. The mean age of the children was 8.95 ± 0.50, majority being 9 years old. Of the 60 children with fluorosis, 51 (85%) had moderate, moderately severe or severe dental fluorosis. The rest had mild dental fluorosis. All the 60 children had urine fluoride level > 1 mg/mL and drinking water fluoride level >1 ppm. The demographic profile of children in the two groups, and their distribution according to age and gender are given in Table 1.
Table 1.
Demographic profile of children
| No fluorosis | Fluorosis | Total | ||
|---|---|---|---|---|
| Age | 8 | 9 (15%) | 9 (15%) | 18 |
| 9 | 45 (75%) | 45 (75%) | 90 | |
| 10 | 6 (10%) | 6 (10%) | 12 | |
| Total | 60 | 60 | 120 | |
| Mean Age | 8.95 ± 0.50 | 8.95 ± 0.50 | ||
| Sex | Male | 29 (45%) | 29 (45%) | 58 |
| Female | 31 (55%) | 31 (55%) | 62 | |
| Total | 60 | 60 | 120 |
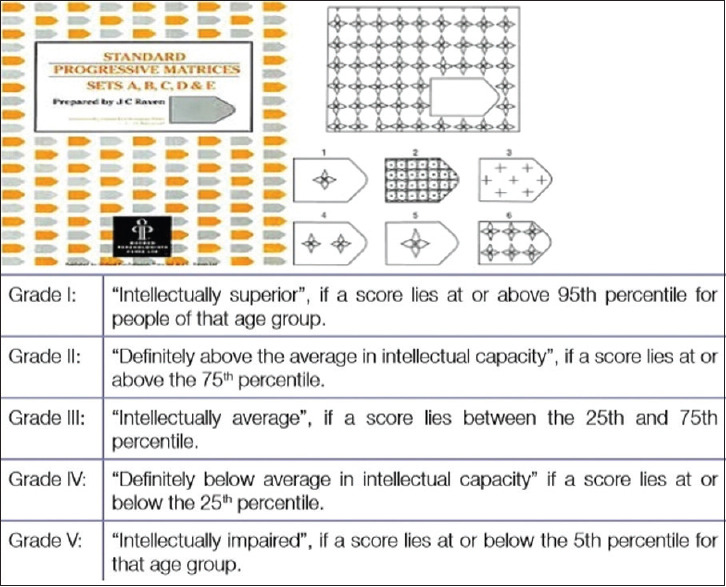
On comparingthe Raven's SPM grades between the two groups, it was observed that in both groups, majority (55%) belonged to the Grade III (intellectually average) category [Figure 3]. But, 30% of the children without fluorosis had Grade I (Intellectually superior) and Grade II (Definitely above the average in intellectual capacity) scores as compared to only 15% of those with fluorosis. None of the children without fluorosis had scores in the Grade V (Intellectually impaired) category whereas 20% of the fluorosis affected children belonged to the same [Table 2]. The differences observed were statistically significant (P = 0.001). The mean raw score in the fluorosis group (26.15) was found to be significantly lower than the control group (31.05) (P = 0.021) by independent samples t test [Table 3].
Figure 3.
Comparison of Raven's SPM grades between children with and without fluorosis
Table 2.
Comparison of Raven’s SPM grades between children with and without fluorosis
| Fluorosis | Total | |||
|---|---|---|---|---|
| No | Yes | |||
| Raven’s SPM Grade | 1 (intellectually superior) | 6 (10%) | 0 (0%) | 6 |
| 2 (above average) | 12 (20%) | 9 (15%) | 21 | |
| 3 (intellectually average) | 33 (55%) | 33 (55%) | 66 | |
| 4 (below average) | 9 (15%) | 6 (10%) | 15 | |
| 5 (intellectually impaired) | 0 (0%) | 12 (20%) | 12 | |
| Total | 60 | 60 | 120 | |
| Chi-Square | 19.029 | P value 0.001 | ||
Table 3.
Comparison between Mean Raven’s SPM Raw scores between both groups- Independent T test
| N | Mean raw score | Standard Deviation | Standard Error Mean | |
|---|---|---|---|---|
| Fluorosis group | 60 | 26.15 | 11.865 | 1.532 |
| Control group | 60 | 31.05 | 11.063 | 1.428 |
| Mean difference 0.764 | Standard difference 0.384 | t -2.340 | P value 0.021 | |
Further, the relationship between the severity of dental fluorosis and Raven's SPM grades was analyzed. An increase in Raven's SPM grade was observed with increase in Dean's fluorosis Index. Among children with grade I, none had dental fluorosis, with grade II, majority had mild fluorosis, whereas among children with grade V, all had moderate to severe fluorosis. A strong positive correlation between severity of dental fluorosis and Raven's SPM grades was found (Spearman's correlation coefficient = 0.740) [Table 4].
Table 4.
Correlation between severity of dental fluorosis (Dean’s fluorosis Index) and Raven’s SPM grades – Spearman’s correlation
| Dean’s | Raven’s SPM Grade | Total | |||||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| Fluorosis index | Grade I | Grade II | Grade III | Grade IV | Grade V | ||
| 1 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 2 | 0 | 6 | 3 | 0 | 0 | 9 | |
| 3 | 0 | 3 | 21 | 3 | 0 | 27 | |
| 4 | 0 | 0 | 9 | 3 | 6 | 18 | |
| 5 | 0 | 0 | 0 | 0 | 6 | 6 | |
| Total | 9 | 33 | 6 | 12 | 60 | ||
| Spearman’s Correlation coefficient | 0.452 | Asymptotic Standard Error 0.080 | P .000 | ||||
With MISIC digit span subtest, the forward and backward digit spans were compared between the two groups. The mean forward digit span was found to be significantly higher in the normal children (5.50 ± 0.809) than those with fluorosis (5.20 ± 0.676). The mean backward digit span in the fluorosis group was 3.20 ± 0.605 whereas that in the control group was 3.50 ± 0.676 (P = 0.012) [Table 5].
Table 5.
Comparison of MISIC digit span between the groups - Independent samples t test
| N | Mean | Standard Deviation | Standard Error Mean | ||
|---|---|---|---|---|---|
| Forward digit span | |||||
| Fluorosis group | 60 | 5.20 | 0.819 | 0.106 | |
| Control group | 60 | 5.50 | 0.676 | 0.087 | |
| [t -2.187, P value 0.031] | |||||
| Backward digit span | |||||
| Fluorosis group | 60 | 3.20 | 0.605 | 0.078 | |
| Control group | 60 | 3.50 | 0.676 | 0.087 | |
| [t -2.560, P value 0.012] |
DISCUSSION
In this cross-sectional study, two groups of 60 children each, with and without fluorosis selected from two primary schools in Alappuzha district were studied. The exclusion criteria were designed in such a way that the effect of fluorosis on cognitive function could be looked for specifically avoiding most of the confounding factors. Fluorosis was already confirmed in the children in the fluorosis group by dental and urine examination. Further, an exposure to high fluoride through drinking water was also confirmed in these children.
Fluorosis and cognitive function
In our study, 30% of the children without fluorosis had grade I (Intellectually superior) and grade II (Definitely above the average in intellectual capacity) scores. None of them had scores in the grade V (Intellectually impaired) category. Meanwhile, only 15% of the children with fluorosis scored grade II and nobody scored grade I. Furthermore, 20% of the fluorosis affected children belonged to the intellectually impaired category (grade V). The differences observed were statistically significant (P = 0.001).
Similar results were reported in earlier studies by Khan et al. and Sudhir et al. who compared intelligence quotient of children living in high and low fluoride areas.[9,18] In the study by Sudhir et al. among 13-15-year-old school children from Nalgonda District, Andhra Pradesh, only 7.8% children had IQ grade 3 (intellectually average) in the high fluoride area, compared to 29.1% children in the low fluoride area.[18] None of the children from high fluoride area had an IQ grade 1 or 2 (Intellectually superior or definitely above the average). In our study also, none of the children with fluorosis had a grade I score, but 15% had grade II scores.
In the study by Khan et al., it was found that majority of the children (74.8%) living in low fluoride area had an IQ grade 2 (definitely above the average) compared to only 16.7% in the high fluoride area.[9] None of the children from the low fluoride area had an IQ grade 4 or 5 (definitely below average or intellectually impaired). On the other hand, majority of children (58.1%) from high fluoride area fell under IQ grade 3 (intellectually average). None of the children from high fluoride area had an IQ grade 1 (intellectually superior). In our study, there was no difference between the two groups with regard to the proportion of children who scored grade III (intellectually average). Only 6 out of 120 children with grade I score (intellectually superior) were found in our study, and they were all belonging to the fluorosis free group. No children with grade V score (intellectually impaired), was found in this group. Another study, by Shivaprakash et al. in 7–11-year-old school children from Bagalkot district, Karnataka, also showed similar results.[19] In that study, 72.5% of children with dental fluorosis had extremely low or borderline IQ scores whereas 47.5% of children without fluorosis had extremely low or borderline IQ scores.
Severity of dental fluorosis and cognitive dysfunction
Of the 60 children with fluorosis in our study, 51 (85%) had moderate, moderately severe or severe dental fluorosis. The rest (15%) had only mild dental fluorosis. All these 60 children had urine fluoride level >1 mg/mL and drinking water fluoride level >1 ppm. Majority of the children (66.67%) suffering from very mild dental fluorosis were found to have RSPM grade II scores. Most of the children with mild fluorosis index (65.9%) were found to have grade III scores followed by grade II and IV (15.9% each) scores. None of the children with moderate and severe fluorosis were found to have grade I and II scores. All the 12 children in the intellectually impaired (Grade V) group had either moderate or severe dental fluorosis. These clearly show a strong correlation between severity of fluorosis and IQ grade (Spearman's correlation coefficient = 0.740). This observation also throws light on the possibility that the presence of dental fluorosis may be regarded as a marker for fluoride-induced cognitive impairment as suggested by Spittle.[20]
In our study, MISIC digit span subtest mean scores (forward and backward) were found to be significantly higher in the normal children than those with fluorosis, which indicates an affection of attention and working memory in fluorosis affected children. Similar results were found in the study by Choi et al., on cognitive functions in Chinese children with lifetime exposure to fluoride.[21] It was found that Wechsler Intelligence Scale for Children-Revised (WISC-IV) digit span subtest was a sensitive outcome measure showing significantly lower forward and backward digit span scores in children with moderate and severe fluorosis.
The effect of certain trace elements in water such as Arsenic and Lead on intellectual ability of children was investigated by few studies. A study by Wang et al. concluded that children's IQ can be affected by high concentrations of either arsenic or fluoride.[22] But the study by Amador et al., demonstrated that though fluoride and arsenic may adversely affect IQ scores, in comparison to fluoride, the effect attributable to arsenic was smaller.[23] In that study, though blood levels of lead were analyzed, they concluded that the observed deficits in IQ scores could not be attributed to lead exposure. These facts warrant further research to explore the effect of other environmental toxins on cognitive development.
Mechanisms of fluoride neurotoxicity were explored in a few animal studies. Elevated fluoride levels in multiple brain regions especially hippocampus, was detected by Mullenix et al. in a study, in rats exposed to high levels of fluoride in drinking water at weaning.[24] Excitotoxicity was proposed as a central mechanism in fluoride neurotoxicity, in a review by Baylock. He points out that, fluoride complexes through multiple mechanisms such as generation of reactive oxygen species and lipid peroxidation products, decreased superoxide dismutase, synaptic injury, impaired glutamate transporters, and mitochondrial dysfunction leads to excitotoxicity.[25] Glutamate receptor-mediated synaptic pruning is known to be critical in brain maturation.[26] These facts concur with longitudinal studies linking higher prenatal fluoride exposure to cognitive development delay in infants and adverse cognitive outcomes in children.[27,28]
To the best of our knowledge, this is the first study conducted in Kerala to study the association between fluorosis and cognitive function. The children enrolled in the fluorosis group were those with dental fluorosis, confirmed by urine fluoride testing, further their drinking water was also tested for high fluoride level which establishes exposure to excess fluoride. The neuropsychometric tests performed to assess the cognitive function were Raven's SPM and MISIC digit span subtest which are relatively culture-independent and reflect diverse functional domains, including memory, attention and tracking, visuospatial organization and reasoning, motor, and dexterity skills.
Limitations
This is only a comparative study; hence causality between fluorosis and cognitive dysfunction cannot be established. Cognitive function of an individual is known to be influenced by complex interactions between various genetic and socio-economical factors. Though we have tried our best to select a homogenous sample with that regard, complete exclusion of such factors is not possible. Other heavy metals such as arsenic and lead were not analyzed in our study, which could very well contribute to cognitive dysfunction. Further research is needed to assess their individual impact as well as interaction with fluoride.
CONCLUSION
This study establishes a significant relationship between the presence of fluorosis and impaired cognition in children. The severity of dental fluorosis has a positive correlation with the grade of cognitive dysfunction. Fluorosis being a preventable cause of cognitive impairment in children, appropriate measures must be employed to reduce the level of fluoride in drinking water to the optimal level, in endemic areas. These could include installation of more number of reverse osmosis (RO) plants at the community level with the help of local governing bodies and also providing RO water purifiers at subsidized rates to homes. It would also be beneficial to screen children with dental fluorosis for cognitive impairment, so as to initiate cognitive rehabilitation therapy.
Key message
Fluorosis is associated with impaired cognition in children. There is a positive correlation between severity of dental fluorosis and the grade of cognitive impairment. Fluorosis being a preventable cause of cognitive impairment, provision of safe drinking water and screening of children with dental fluorosis for cognitive impairment is necessary.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
District Medical Officer Alappuzha, Assistant educational officer, Alappuzha, and the head masters of Govt LP school Kalarkode and CMS LP school Kommady.
REFERENCES
- 1.WHO (World Health Organization). Guidelines for Drinking-Water Quality. 4th ed. Geneva: WHO; 2011b. [Google Scholar]
- 2.Arlappa N, Qureshi AI, Srinivas R. Fluorosis in India: An overview. Int J Res Dev Health. 2013;1:97–102. [Google Scholar]
- 3.Susheela AK. Fluorosis: Indian Scienario: A Treatise on Fluorosis. New Delhi, India: Fluorosis Research and Rural Development Foundation; 2001. [Google Scholar]
- 4.Kauffman JM. Water fluoridation: A review of recent research and actions. J Am Physicians Surg. 2005;10:38–44. [Google Scholar]
- 5.Reddy DR. Neurology of endemic skeletal fluorosis. Neurol India. 2009;57:7–12. doi: 10.4103/0028-3886.48793. [DOI] [PubMed] [Google Scholar]
- 6.Susheela AK, Toteja GS. Prevention and control of fluorosis and linked disorders: Developments in the 21st Century-Reaching out to patients in the community and hospital settings for recovery. Indian J Med Res. 2018;148:539–47. doi: 10.4103/ijmr.IJMR_1775_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Programme for Prevention and Control of Fluorosis (NPPCF). Revised Guidelines (2014). Government of India. Available from: http://cghealth.nic.in/ehealth/2017/Instructions/NPPCFnewguidelinebyGOI.pdf .
- 8.Gopalakrishnan P, Vasan RS, Sarma PS, Nair KS, Thankappan KR. Prevalence of dental fluorosis and associated risk factors in Alappuzha district, Kerala. Natl Med J India. 1999;12:99–103. [PubMed] [Google Scholar]
- 9.Khan SA, Singh RK, Navit S, Chadha D, Johri N, Navit P, et al. Relationship between dental fluorosis and intelligence quotient of school going children in and around Lucknow district: A cross-sectional study. J Clin Diagn Res. 2015;9:ZC10–5. doi: 10.7860/JCDR/2015/15518.6726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lakhan R, Ekúndayò OT, Shahbazi M. An estimation of the prevalence of intellectual disabilities and its association with age in rural and urban populations in India. J Neurosci Rural Pract. 2015;6:523–8. doi: 10.4103/0976-3147.165392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kishore T, Nagar RK. Role of NGOs in Identification Camps for Persons with Intellectual Disabilities in India. Disability, CBR & Inclusive Development [Internet] 2012. Feb, [[Last cited on 2020 Jul 15];22:97-104]. Available from: http://dcidj.org/article/view/89. doi:10.5463/dcid.v22i3.89 .
- 12.Arora NK, Nair MKC, Gulati S, Deshmukh V, Mohapatra A, Mishra D, et al. Neurodevelopmental disorders in children aged 2-9 years: Population-based burden estimates across five regions in India. PLoS Med. 2018;15:e1002615. doi: 10.1371/journal.pmed.1002615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pocock SJ. Clinical Trials: A Practical Approach. New York, NY: John Wiley & Sons; 1983. [Google Scholar]
- 14.Dean HT. Washington, D.C: American Association for the Advancement of Science; 1942. The investigation of physiologic effects by epidemiological method. In: Fluorine and Dental Health; pp. 23–31. [Google Scholar]
- 15.Raven JC, Court JH, Raven J. Raven manual: Section 3. The Standard Progressive Matrices. Oxford: Oxford Psychologists Press; 1992. [Google Scholar]
- 16.Raven J. The Raven's progressive matrices: Change and stability over culture and time. Cogn Psychol. 2000;41:1–48. doi: 10.1006/cogp.1999.0735. [DOI] [PubMed] [Google Scholar]
- 17.Malin AJ. Manual for Malin's Intelligence Scale for Indian Children (MISIC) Lucknow: Indian Psychological Corporation; 1969. [Google Scholar]
- 18.Sudhir KM, Chandu GN, Prashant GM, Reddy VVS. Effect of fluoride exposure on Intelligence quotient (IQ) among 13-15 year old school children of known endemic area of fluorosis, Nalgonda District, Andhra Pradesh. J Indian Assoc Public Health Dent. 2009;7:88–94. [Google Scholar]
- 19.Shivaprakash PK, Ohri K, Noorani H. Relation between dental fluorosis and intelligence quotient in school children of Bagalkot district. J Indian Soc Pedod Prev Dent. 2011;29:117–20. doi: 10.4103/0970-4388.84683. [DOI] [PubMed] [Google Scholar]
- 20.Spittle B. Dental fluorosis as a marker for fluoride-induced cognitive impairment. Fluoride. 2018;49:3–4. [Google Scholar]
- 21.Choi AL, Zhang Y, Sun G, Bellinger DC, Wang K, Yang XJ, et al. Association of lifetime exposure to fluoride and cognitive functions in Chinese children: A pilot study. Neurotoxicol Teratol. 2015;47:96–101. doi: 10.1016/j.ntt.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 22.Wang S-X, Wang Z-H, Cheng X-T, Li J, Sang Z-P, Zhang X-D, et al. Arsenic and fluoride exposure in drinking water: Children's IQ and growth in Shanyin county, Shanxi province, China. Environ Health Perspect. 2007;115:643–7. doi: 10.1289/ehp.9270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rocha-Amador D, Navarro ME, Carrizales L, Morales R, Calderón J. Decreased intelligence in children and exposure to fluoride and arsenic in drinking water. Cad Saude Publica. 2007;23(Suppl 4):S579–87. doi: 10.1590/s0102-311x2007001600018. [DOI] [PubMed] [Google Scholar]
- 24.Mullenix PJ, Denbesten PK, Schunior A, Kernan WJ. Neurotoxicity of sodium fluoride in rats. Neurotoxicol Teratol. 1995;17:169–77. doi: 10.1016/0892-0362(94)00070-t. [DOI] [PubMed] [Google Scholar]
- 25.Bloylock RL. Excitotoxicity: A possible central mechanism in fluoride neurotoxicity. Fluoride. 2004;37:301–14. [Google Scholar]
- 26.Selemon LD. A role for synaptic plasticity in the adolescent development of executive function. Transl Psychiatry. 2013;3:e238. doi: 10.1038/tp.2013.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bashash M, Thomas D, Hu H, Martinez-Mier EA, Sanchez BN, Basu N, et al. Prenatal fluoride exposure and cognitive outcomes in children at 4 and 6-12 years of age in Mexico. Environ Health Perspect. 2017;125:097017. doi: 10.1289/EHP655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Valdez Jiménez L, López Guzmán OD, Cervantes Flores M, Costilla-Salazar R, Calderón Hernández J, Alcaraz Contreras Y, et al. In utero exposure to fluoride and cognitive development delay in infants. NeuroToxicology. 2017;59:65–70. doi: 10.1016/j.neuro.2016.12.011. [DOI] [PubMed] [Google Scholar]


