Sir,
Dorsal intraspinal Schwannoma and Meningioma are commonly encountered lesions for compressive myelopathy. Meniogioma is situated in posterolateral aspect of vertebral canal with or without dural tail and ginkgo leaf sign, usually affecting dorsal spine and females while Schwannoma is located anteriorly and may extend into intervertebral canal along intercostal nerve presenting as dumbbell. We are presenting a case of tubercular lesion exclusively as isolated intraspinal mass with enlarged intervertebral canal thus mimicking with Schwannoma. A 37-year-old male reported with progressive paraparesis of 4 months duration. He had sensory involvement below nipple with radicular pain along left intercostal nerve on cough. There was no history of fever, cough, injury, and bladder-bowel involvement. There were no subcutaneous nodules, café-au-let spots, or lymphadenopathy. Cranial examination was noncontributory. Fundoscopy did not show any sign of papilloedema. Both upper limbs were normal. He had upper motor neuron type of paraparesis. There was no atrophy and fasciculation. Abdominal and cremasteric reflexes were absent. Plantar reflexes were bilaterally up going. Knee and ankle reflexes were brisk. Sensory involvement was below D4 cord level. The posterior column was also affected below D7 level. There was no focal spinal deformality and tenderness. He was diagnosed as dorsal sensory-motor compressive myelopathy with possibility of Meningioma or Schwannoma. His complete blood picture, X-Ray chest, X-Ray spine, and ultrasound abdomen were normal. Quantiferon TB Gold and Mantoux test were positive. Magnetic resonance imaging (MRI) spine [Figures 1, 2a and b] depicted left extramedullary intraspinal space-occupying lesion extending into intervertebral canal and paravertebral compartment from D3 to D5 with diffuse hyperintensity in D4 & D6 vertebral body. There was burrowing of lesion into D4 vertebral body at midline with well-defined edges. Patient refused for any surgical intervention to be undertaken for definite histopathological diagnosis. In the view of positive Quantiferon TB Gold, he was put on classical antitubercular treatment. He showed improvement in the power from grade 2 to 3 after 3 months of therapy. He recovered almost full after 10 months of treatment. Repeat MRI Spine [Figures 3 and 4] exhibited disappearance of whole lesion, thus avoided surgical decompression thereby delayed vertebral deformality. Tuberculoma should always be kept in the mind in the differential diagnosis of intraspinal mass lesion which can be medically cured.
Figure 1.

The intraspinal T2 hypointense lesion extending from D3 to D5; and is also extending ventrally and involving D4 Vertebral body with hyperintensity in D4. vertebral body. The D6 vertebral body is also diffusely hyperintense
Figure 2.
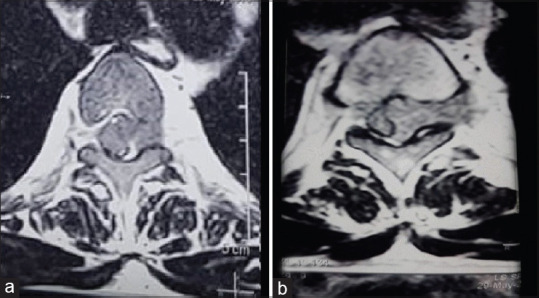
a & b: Axial T2 section of MRI at mid-D3 and D4 vertebral level showing extradural lesion with extension into left D4 intervertebralcanal
Figure 3.

Sagittal section MRI Showing disappearance of lesion after anti-tuberculear lesion with intact spinous process
Figure 4.

Axial section of post-therapy MRI depicting complete disappearance of lesion
DISCUSSION
Tuberculosis may involve almost all segments of the spine. It usually initiates from paradiscal region leading to erosion of vertebral edges and narrowing of disc space. It may further progress to collapse of vertebrae and formation of cold abscess. Rarely it may present exclusively as a mass lesion in intraspinal region.[1] Our case was of intraspinal extramedullary tubercular mass extruding through intervertebral canal into thorax as if it is dumb-bell Schwannoma having both intra and extra-spinal components with neck in the canal. Rajgopalan et al. presented a similar case of dumb-bell shaped spinal tumour in a 20-year-old female.[2] It may be purely intradural extramedullary without extradural component.[3,4] Pre-treatment diagnostic confirmation may avoid the surgical intervention thereby delayed postoperative sequelae like kyphosis which may lead to neurological deficit on progression. Other commonly encountered space-occupying lesion of dorsal spine is Meningioma which may mimic with such rare tubercular presentation.[5] Tuberculosis should always be kept in the differential diagnosis of intraspinal lesion. The establishment of diagnosis may be easy if it is associated with supplementary findings like tubercular lung, lymphadenopathy, constitutional symptoms, and positive quantiferon TB gold. It may be treated conservatively without the need of surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Quispe D, Alvarodo M, Rivas D, Gonzales I. Extramedullary intradural tuberculosis: A case report and review of the literature. Rev Neurol. 2018;66:21–4. [PubMed] [Google Scholar]
- 2.Rajgopalan M, Srivastava A, Dhammi IK, Jain AK. Tuberculosis ‘The great masquerader’ presenting as dumb-bell- shaped intradural extramedullary tumor in a 20-year-old female. J Clin Orthop Trauma. 2017;8:168–70. doi: 10.1016/j.jcot.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roca B. Intradural extramedullary tuberculoma of the spinal cord: A review of reported cases. J Infect. 2005;50:425–31. doi: 10.1016/j.jinf.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 4.Kumar R, Kasliwal MK, Srivastava R, Sharma BS. Tuberculoma presenting as an intradural extramedullary lesion. Pediatr Neurosurg. 2007;43:541–3. doi: 10.1159/000108805. [DOI] [PubMed] [Google Scholar]
- 5.Shim DM, Oh SK, Kim TK, Chae SU. Intradural extramedullary tuberculoma mimicking en plaque meningioma. Clin Orthop Surg. 2010;2:260–3. doi: 10.4055/cios.2010.2.4.260. [DOI] [PMC free article] [PubMed] [Google Scholar]


