Abstract
Background
Pulmonary endothelial injury and microcirculatory thromboses likely contribute to hypoxemic respiratory failure, the most common cause of death, in patients with COVID‐19. Randomized controlled trials (RCTs) suggest differences in the effect of therapeutic heparin between moderately and severely ill patients with COVID‐19. We did a systematic review and meta‐analysis of RCTs to determine the effects of therapeutic heparin in hospitalized patients with COVID‐19.
Methods
We searched PubMed, Embase, Web of Science, medRxiv, and medical conference proceedings for RCTs comparing therapeutic heparin with usual care, excluding trials that used oral anticoagulation or intermediate doses of heparin in the experimental arm. Mantel‐Haenszel fixed‐effect meta‐analysis was used to combine odds ratios (ORs).
Results and Conclusions
There were 3 RCTs that compared therapeutic heparin to lower doses of heparin in 2854 moderately ill ward patients, and 3 RCTs in 1191 severely ill patients receiving critical care. In moderately ill patients, there was a nonsignificant reduction in all‐cause death (OR, 0.76; 95% CI, 0.57‐1.02), but significant reductions in the composite of death or invasive mechanical ventilation (OR, 0.77; 95% CI, 0.60 0.98), and death or any thrombotic event (OR, 0.58; 95% CI, 0.45‐0.77). Organ support‐free days alive (OR, 1.29; 95% CI, 1.07‐1.57) were significantly increased with therapeutic heparin. There was a nonsignificant increase in major bleeding. In severely ill patients, there was no evidence for benefit of therapeutic heparin, with significant treatment‐by‐subgroup interactions with illness severity for all‐cause death (P = .034). In conclusion, therapeutic heparin is beneficial in moderately ill patients but not in severely ill patients hospitalized with COVID‐19.
Keywords: anticoagulation, clinical trials, COVID‐19, heparin, meta‐analysis
Essentials.
Trials suggest differences in the effect of therapeutic heparin based on severity of COVID‐19.
We did a meta‐analysis to determine the effect of therapeutic heparin in hospitalized patients.
In the moderately ill, there was a significant reduction in death or mechanical ventilation.
In the severely ill, there was no evidence for benefit of therapeutic heparin.
1. INTRODUCTION
Pulmonary inflammation, endothelial injury, and microcirculatory thromboses likely contribute to hypoxemic respiratory failure, the most common cause of death in patients with COVID‐19. Observational data suggest that heparin anticoagulation decreases the risk of critical illness and death in those hospitalized for COVID‐19. 1 , 2 , 3 , 4 , 5 Heparin anticoagulants are of particular interest for the treatment of COVID‐19 due to their additional anti‐inflammatory and potentially antiviral properties. 6 , 7 , 8 Randomized controlled trials (RCTs) suggest that therapeutic heparin anticoagulation is beneficial in patients hospitalized for COVID‐19 with moderate illness, but of no benefit and potential harm when provided to patients with critical illness. 9 , 10 Given the disparate findings in these two patient populations and safety concerns regarding bleeding, there is hesitancy to adopt therapeutic heparin as standard care in moderately ill patients with COVID‐19. 11 We conducted a systematic review and meta‐analysis of available RCTs of therapeutic‐dose heparin anticoagulation compared with usual care to determine the effects of therapeutic heparin in hospitalized patients with COVID‐19.
2. METHODS
This systematic review and meta‐analysis was reported according to the Preferred Reporting for Systematic Reviews and Meta‐Analyses guidelines. 12 We searched PubMed, Embase, and Web of Science, using terms (“heparin” OR “dalteparin” OR “enoxaparin” OR “tinzaparin” OR “anticoagulation”) AND (“SARS‐CoV‐2” OR “COVID” OR “coronavirus” OR “COVID‐19”) AND (“randomized” OR “randomised” OR “clinical trials”), with no language restrictions. We also searched the grey literature, which included medRxiv, and medical conference proceedings. We included RCTs comparing therapeutic‐dose heparin anticoagulation with usual care in hospitalized adults with moderate or severe COVID‐19. Moderate illness was defined as admission to hospital ward level of care, not already mechanically ventilated, and not imminently requiring mechanical ventilation or critical care. Severe illness was defined as admission to hospital with clinically intensive level of care. We restricted the search to RCTs published from March 1, 2019, to October 8, 2021. We excluded trials that used oral anticoagulation or used intermediate dosing of heparin in the experimental arm. Heparin was defined as either unfractionated intravenous or low‐molecular‐weight subcutaneous forms of heparin; both forms are within the same drug class, exert their anticoagulant effect by amplifying the activity of antithrombin and have similar nonanticoagulant effects. 13 Two reviewers (MS and GT) independently screened title, abstract, and full text of retrieved articles for inclusion. Any disagreement or uncertainty was resolved by consensus. We used the Cochrane risk of bias tool to assess risk of bias in the included trials. 14
Prespecified outcomes included all‐cause death, death or invasive mechanical ventilation, death or organ support, death or major thrombotic event, death or any thrombotic event, major thrombotic events, major bleeding as defined by the ISTH, 15 ventilator‐free days alive, and organ support–free days alive. Major thrombotic events were defined as the composite of myocardial infarction, pulmonary embolism, ischemic stroke, or systemic arterial embolism. Any thrombotic events were defined as major thrombotic events or deep vein thromboses. Definition of organ support–free days alive are described in detail in the published protocols of the included clinical trials. 16 , 17 Ventilator‐free days, and organ support–free days alive were analyzed using ordinal logistic regression; death was assigned the worst outcome (a value of −1) in these analyses. 18
We used forest plots to display the results of the meta‐analysis. Mantel‐Haenszel fixed‐effect meta‐analyses were used to combine odds ratios (ORs) of outcomes reported in available RCTs separately for moderately ill ward patients and severely ill intensive care unit (ICU) patients, using a chi‐squared test to estimate P values for interaction between treatment and severity of illness. The variance attributed to pooled results reflects only sampling error due to the play of chance at randomization. Homogeneity of ORs is not required for fixed‐effect pooled ORs to be informative. 19 Heterogeneity was evaluated using I‐square values. I‐square values of ≈25% suggests low, 50% moderate, and 75% high between‐trial heterogeneity. 20 Statistical analyses were performed using Stata version 15 (StataCorp, College Station, TX, USA).
3. RESULTS AND DISCUSSION
There were four trials that compared therapeutic heparin to usual care using lower doses of heparin (see Figure 1). 9 , 10 , 21 , 22 Three trials included moderately ill ward patients with COVID‐19: a multiplatform trial integrating the Antithrombotic Therapy to Ameliorate Complications of COVID‐19 (ATTACC), Accelerating COVID‐19 Therapeutic Interventions and Vaccines‐4 Antithrombotics Inpatient Platform Trial (ACTIV‐4a) and the Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community‐Acquired Pneumonia (REMAP‐CAP) 9 the Coagulopathy of COVID‐19, A Pragmatic Randomized Controlled Trial of Therapeutic Anticoagulation Versus Standard Care as a Rapid Response to the COVID‐19 Pandemic (RAPID), 21 and the Systemic Anticoagulation With Full Dose Low Molecular Weight Heparin (LMWH) Versus Prophylactic or Intermediate Dose LMWH in High Risk COVID‐19 Patients (HEP‐COVID) trial). 22 Three trials included severely ill patients with COVID‐19: a separate multiplatform trial conducted by the same investigators evaluated therapeutic heparin in severely ill ICU patients, 23 a small phase II randomized trial of mechanically ventilated patients (Therapeutic Versus Prophylactic Anticoagulation for Severe COVID‐19: A Randomized Phase II Clinical Trial [HESACOVID]), 24 and the HEP‐COVID trial, which also included severely ill patients, with randomization stratified according to disease severity. 22 We excluded the Therapeutic versus Prophylactic Anticoagulation for Patients Admitted to Hospital with COVID‐19 and Elevated D‐dimer Concentration (ACTION) trial, as it combined therapeutic anticoagulation with rivaroxaban in moderately ill patients and therapeutic enoxaparin in severely ill patients, without reporting any of our prespecified outcomes by illness severity. 25 We also excluded the Effect of Intermediate‐Dose Versus Standard‐Dose Prophylactic Anticoagulation on Thrombotic Events, Extracorporeal Membrane Oxygenation Treatment, or Mortality Among Patients With COVID‐19 Admitted to the Intensive Care Unit (INSPIRATION) 26 and the trial of Perepu et al, 27 as these trials used intermediate dose heparin in their experimental arms. The risk of bias assessment of the included trials is presented in Table S1. There were deviations from the intended experimental intervention in the two multiplatform trials where lower‐than‐therapeutic doses of heparin were administered in ≈20% of patients allocated to the experimental arms. 9 , 10 Additionally, the outcomes of organ support were not blindly adjudicated by an independent clinical events committee in the multiplatform trials. There was no information on protocol deviations, and no prespecified statistical analysis plan provided or information on blinded evaluation of the secondary outcomes in the HESACOVID trial. 24 The risk of bias was considered low for the RAPID and the HEP‐COVID trials. 21 , 22
FIGURE 1.
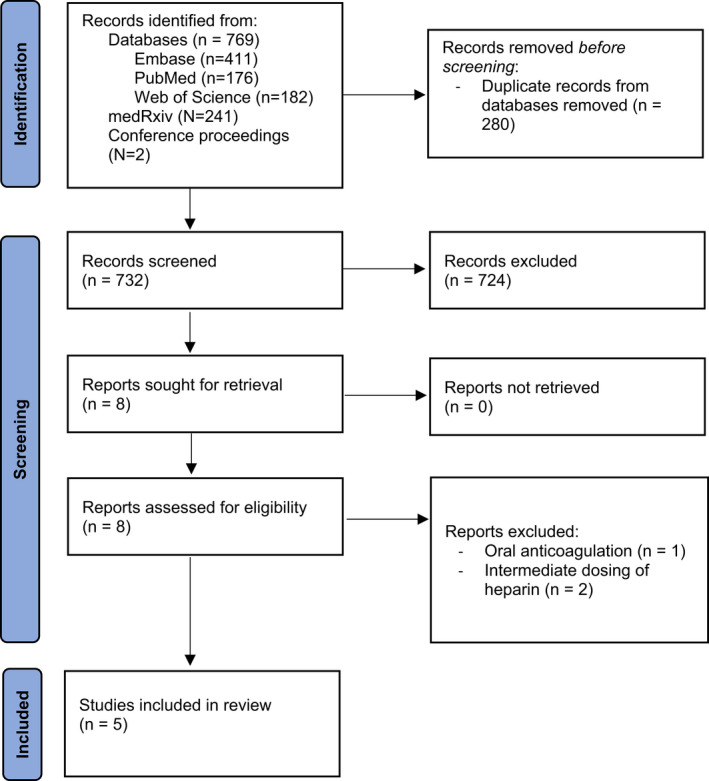
Preferred Reporting for Systematic Reviews and Meta‐Analyses diagram
Figure 2 shows meta‐analyses of three trials in moderately ill patients. Data from the HEP‐COVID trial contributed to the meta‐analysis of the outcomes of death or any thrombotic event and major bleeding, as to date only these outcomes were presented by illness severity. 22 There was nonsignificant reduction in all‐cause death (OR, 0.76; 95% CI, 0.57‐1.02), but significant reductions in the composite of death or invasive mechanical ventilation (OR, 0.77; 95% CI, 0.60‐0.98), death or organ support (OR, 0.77; 95% CI, 0.63‐0.93), death or major thrombotic event (OR, 0.64; 95% CI, 0.48‐0.86), death or any thrombotic event (OR, 0.58; 95% CI, 0.45‐0.77), and major thrombotic events (OR, 0.47; 95% CI, 0.24‐0.90). Ventilator‐free days alive (OR, 1.30; 95% CI 1.05‐1.61) and organ support–free days alive (OR, 1.29; 95% CI, 1.07‐1.57) were significantly increased with therapeutic heparin. Conversely, there was a nonsignificant increase in major bleeding. Figure 3 shows meta‐analyses of the three trials in severely ill patients.
FIGURE 2.
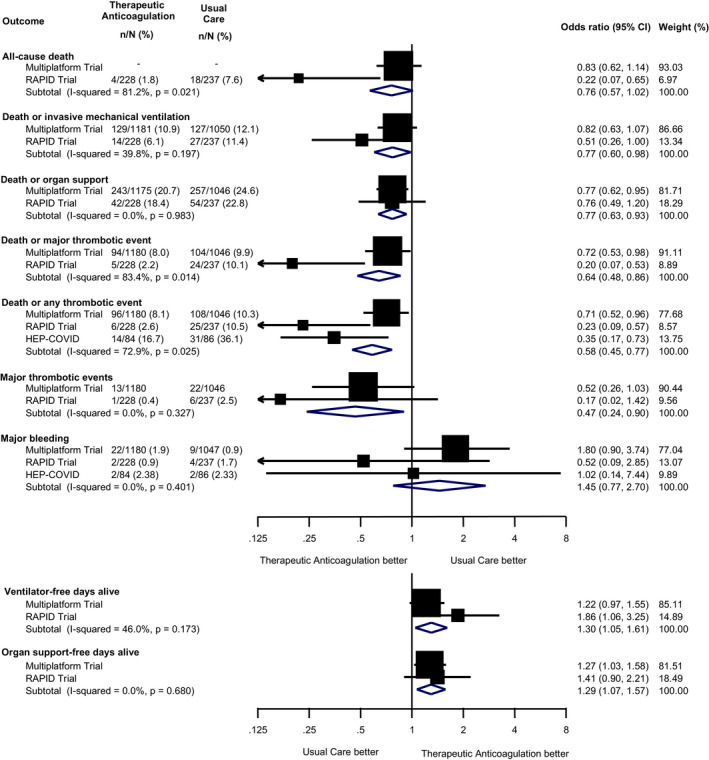
Meta‐analyses of effectiveness and safety outcomes in randomised trials comparing therapeutic heparin with usual care in moderately ill ward patients with COVID‐19. Mantel‐Haenszel fixed‐effect meta‐analyses of the RAPID trial, the multiplatform trial and HEP‐COVID trial in moderately ill ward patients. 9 , 21 , 22 Squares and horizontal lines show treatment effects and their 95% confidence intervals in each trial. The area of each square is proportional to the weight the trial received in the meta‐analysis. Diamonds show estimated treatment effects and 95% confidence intervals from meta‐analyses. Odds ratios for ventilator‐free and organ support–‐free days alive are from ordinal logistic regression in both trials; death was assigned the worst outcome (a value of −1). Absolute values were not available for all‐cause death from the multiplatform trial. Major thrombotic events were defined as the composite of myocardial infarction, pulmonary embolism, ischemic stroke or systemic arterial embolism; any thrombotic events were defined as a major thrombotic event or deep vein thrombosis; major bleeding defined by the ISTH Scientific and Standardization Committee. The observation time for the outcomes in the trials were 28 days for the multiplatform trial (with the exception of organ support–free days, which was calculated for an observation time of 21 days), 28 days for the RAPID trial, and 30 days for HEP‐COVID trial 16 , 17 , 23
FIGURE 3.
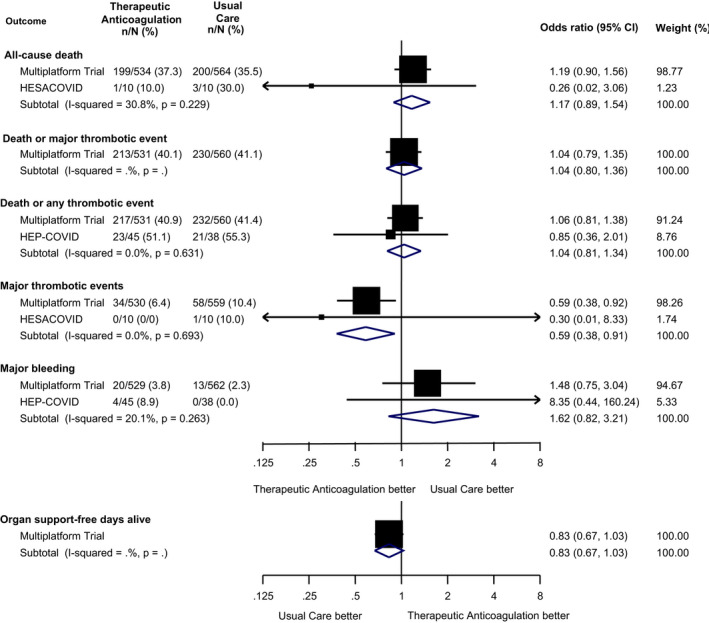
Meta‐analyses of effectiveness and safety outcomes in randomised trials comparing therapeutic heparin with usual care in severely ill intensive care unit (ICU) patients with COVID‐19. Mantel‐Haenszel fixed‐effect meta‐analyses of the multiplatform trial, HESACOVID and HEP‐COVID in severely ill ICU patients. 10 , 22 , 24 Squares and horizontal lines show treatment effects and their 95% confidence intervals in each trial. The area of each square is proportional to the weight the trial received in the meta‐analysis. Diamonds show estimated treatment effects and 95% confidence intervals from meta‐analyses. Odds ratios for organ support–free days alive are from ordinal logistic regression; death was assigned the worst outcome (a value of −1). Major thrombotic events were defined as the composite of myocardial infarction, pulmonary embolism, ischemic stroke, or systemic arterial embolism; any thrombotic events were defined as a major thrombotic event or deep vein thrombosis; major bleeding defined by the ISTH Scientific and Standardization Committee. The observation time for the outcomes in the trials were 28 days for the multiplatform trial (with the exception of organ support–free days, which was calculated for an observation time of 21 days), and 30 days for HEP‐COVID trial 10 , 23
Figure 4 shows analyses of the interaction between treatment effect and severity of illness. In severely ill patients, there was no evidence to suggest a benefit of therapeutic heparin. There were significant treatment‐by‐subgroup interactions with severity of illness for all‐cause death (P for interaction = .034), all‐cause death or major thrombotic event (P = .017), death or any thrombotic event (P = 0.002), and organ support–free days alive (P = .003). There was no evidence for treatment‐by‐subgroup interactions for major thrombotic events and major bleeding.
FIGURE 4.
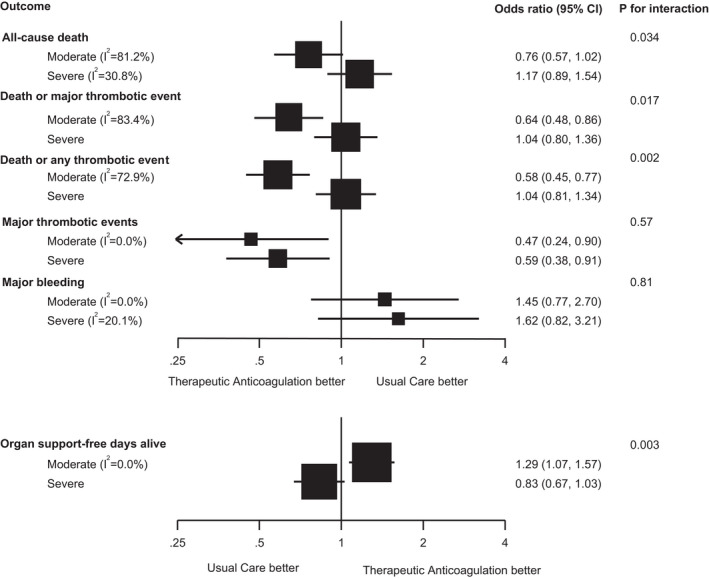
Analyses of the interaction between treatment effect and severity of illness of therapeutic heparin versus usual care in patients with COVID‐19. The analysis is based on Mantel‐Haenszel fixed‐effect meta‐analyses of the RAPID trial, HEP‐COVID trial, and the multiplatform trial in moderately ill ward patients, 9 , 21 , 22 and results of the multiplatform trial, HESACOVID, and HEP‐COVID trial in severely ill ICU patients. 10 , 22 , 24 Squares and horizontal lines show treatment effects and their 95% confidence intervals in each subgroup. The area of each square is proportional to the inverse of the variance in the subgroup. Odds ratios for organ support‐free days alive are from ordinal logistic regression in all trials; death up to 28 days was assigned the worst outcome (a value of −1) in all trials. The P values for interaction are for the comparison of treatment effects between moderately and severely ill patients and were derived from a chi‐squared test. Major thrombotic events were defined as the composite of myocardial infarction, pulmonary embolism, ischemic stroke, or systemic arterial embolism; any thrombotic events were defined as a major thrombotic event or deep vein thrombosis; major bleeding defined by the ISTH Scientific and Standardization Committee. 15 The observation time for the outcomes in the trials were 28 days for the multiplatform trials (with the exception of organ support free days which was calculated for an observation time of 21 days), 28 days for the RAPID trial and 30 days for the HEP‐COVID trial 16 , 17 , 23
This meta‐analysis included three available trials of therapeutic heparin in moderately ill ward patients with COVID‐19, which were not individually conclusive. 11 Findings for five effectiveness outcomes (death or invasive mechanical ventilation, death or organ support, ventilator‐free days alive, organ support–free days alive, major thrombotic events) were consistent between trials, with significant differences in favor of therapeutic heparin. There was high heterogeneity in the findings for all‐cause death and the composites of death or major thrombotic event, and death or any thrombotic event. This suggests that there are competing nonmodifiable causes of death aside from micro‐ and macrovascular thromboses. By contrast to positive treatment effects in ward patients, there were no such effects in severely ill ICU patients. We found significant treatment‐by‐subgroup interactions with severity of illness for all‐cause death, all‐cause death or major thrombosis, all‐cause death or any thrombosis, and organ support–free days alive, with evidence of benefit with therapeutic heparin in moderately ill ward patients, but not in severely ill ICU patients. Conversely, there were no treatment‐by‐subgroup interactions for major thrombotic events and major bleeding, with benefit in both groups for therapeutic heparin to prevent major thrombotic events with non‐significant, numeric increases in major bleeding. We speculate that the different effect of therapeutic heparin in moderately ill compared to severely ill patients was because the latter were too ill for this treatment to alter the cascade of endothelial injury and microvascular thromboinflammation, emphasizing the need for early treatment. However, there were consistent and significant reductions in major thrombotic events in the severely and moderately ill, which suggests that therapeutic heparin is an effective anticoagulant protecting against large‐vessel thrombosis and thromboembolism in patients with COVID‐19. 28 , 29
A recently published meta‐analysis by Ortega‐Paz et al 30 differs from ours, concluding that prophylactic anticoagulation should be preferred over intermediate or therapeutic dose anticoagulation for hospitalized patients with COVID‐19, whether moderately or severely ill. The authors combined trials using different types and doses of anticoagulants in the experimental arm, including rivaroxaban and intermediate‐ or therapeutic‐dose heparin. This variation in type and dose of anticoagulant is likely associated with variation in treatment effect, as different types and doses of anticoagulants have different mechanisms of action, off‐target effects, and safety profiles. Pooling trials with different experimental regimens could therefore submerge important treatment effects of single regimens. Our conclusions differ, as we only pooled data from trials of therapeutic‐ compared to lower dose‐dose heparin. Also, Ortega‐Paz et al 30 evaluated effectiveness only for the outcomes of all‐cause death and large‐vessel thrombosis, while we also analyzed outcomes such as organ support–free days alive and the composite of death or thrombosis, which more completely evaluate the effect of pulmonary and systemic thromboinflammation on health and health resource use.
A limitation of this meta‐analysis, like the majority of published meta‐analyses, is that it did not analyze patient‐level data. Only five trials were included, which may be considered a limitation, but early and timely synthesis of trial‐level data is important in the setting of the ongoing COVID‐19 pandemic. A strength of this research is the harmonized definitions used in three of the included trials. 9 , 21 , 22 Also, the fact that the results of these different multicenter trials (conducted in different settings) are generally in agreement further supports the robustness of the findings of this meta‐analysis. There are multiple other ongoing trials evaluating therapeutic versus prophylactic anticoagulation, so an updated meta‐analysis will be important. 31 , 32 However, in the face of the ongoing pandemic, our findings provide sufficient evidence to support the adoption of therapeutic heparin as standard care in moderately ill hospitalized patients with COVID‐19 who are at low risk of bleeding. In conclusion, this meta‐analysis showed that therapeutic heparin is beneficial in moderately ill ward patients, but not in severely ill patients hospitalized with COVID‐19.
RELATIONSHIP DISCLOSURE
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
Concept and design: MS, BRdC, M Cushman, PJ. Acquisition, analysis, or interpretation of data: MS, BRdC, PJ. Drafting of the manuscript: MS, BRdC, M Cushman, PJ. Critical revision of the manuscript: MS, BRdC, GHT, HR, MAH, LBK, FNÁ, MOA, PDJ, DL, M Carrier, AB, MF, SM, AYYL, KET, EMN, M Cushman, PJ. Statistical analysis: BRdC. All authors approved the final manuscript and submission.
Supporting information
Appendix S1
Sholzberg M, da Costa BR, Tang GH, et al; on behalf of the RAPID Trial Investigators . Meta‐analysis of randomized trials of therapeutic heparin for COVID‐19: A meta‐analysis. Res Pract Thromb Haemost. 2021;5:e12638. doi: 10.1002/rth2.12638
Michelle Sholzberg and Bruno R. da Costa contributed equally to the manuscript.
Handling Editor: Pantep Angchaisuksiri
Funding information
This study was funded by Task 54, Defense Research Development Canada, Department of National Defense, Ottawa, Canada. The funders had no role in the study design; conduct, collection, management, analysis, or interpretation of data; or in preparation or review of the manuscript or the approval of the manuscript for submission.
Handling Editor: Pantep Angchaisuksiri
Contributor Information
Michelle Sholzberg, Email: michelle.sholzberg@unityhealth.to, @sholzberg.
Grace H. Tang, @ghltang.
Hassan Rahhal, @hassanr_27.
Musaad AlHamzah, @1Musaad.
Lisa Baumann Kreuziger, @Lbkreuziger.
Fionnuala Ní Áinle, @fniainle.
Mozah Obaid Almarshoodi, @MozahDr.
Paula D. James, @james_paulad.
David Lillicrap, @DavidLillicrap.
Marc Carrier, @MarcCarrier.
Michael Fralick, @FralickMike.
Saskia Middeldorp, @MiddeldorpS.
Agnes Y. Y. Lee, @AggieLeeMD.
Elnara Márcia Negri, @ElnaraNegri.
Mary Cushman, @MaryCushmanMD.
REFERENCES
- 1. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2019;18(5):1094‐1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McGonagle D, O'Donnell JS, Sharif K, Emery P, Bridgewood C. Immune mechanisms of pulmonary intravascular coagulopathy in COVID‐19 pneumonia. Lancet Rheumatol. 2020;2(7):e437‐e445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020;395(10229):1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nopp S, Moik F, Jilma B, Pabinger I, Ay C. Risk of venous thromboembolism in patients with COVID‐19: a systematic review and meta‐analysis. Res Pract Thromb Haemost. 2020;4(7):1178‐1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Paranjpe I, Fuster V, Lala A, et al. Association of treatment dose anticoagulation with in‐hospital survival among hospitalized patients with COVID‐19. J Am Coll Cardiol. 2020;76(1):122‐124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Clausen TM, Sandoval DR, Spliid CB, et al. SARS‐CoV‐2 infection depends on cellular heparan sulfate and ACE2. Cell. 2020;183(4):1043‐1057.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Buijsers B, Yanginlar C, Maciej‐Hulme ML, de Mast Q, van der Vlag J. Beneficial non‐anticoagulant mechanisms underlying heparin treatment of COVID‐19 patients. EBioMedicine. 2020;59:102969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mycroft‐West CJ, Su D, Pagani I, et al. Heparin inhibits cellular invasion by SARS‐CoV‐2: structural dependence of the interaction of the spike s1 receptor‐binding domain with heparin. Thromb Haemost. 2020;120(12):1700‐1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lawler PR, Goligher EC, Berger JS, et al. Therapeutic anticoagulation with heparin in noncritically ill patients with Covid‐19. N Engl J Med. 2021;385:790‐802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Goligher EC, Bradbury CA, McVerry BJ, et al. Therapeutic anticoagulation with heparin in critically ill patients with Covid‐19. N Engl J Med. 2021;385:777‐789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ten Cate H. Surviving Covid‐19 with heparin? N Engl J Med. 2021;385:845‐846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Heparin PC, Drugs R. Heparin and related drugs: beyond anticoagulant activity. ISRN Pharmacol. 2013;2013:910743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 15. Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non‐surgical patients. J Thromb Haemost. 2005;3(4):692‐694. [DOI] [PubMed] [Google Scholar]
- 16. Houston BL, Lawler PR, Goligher EC, et al. Anti‐thrombotic therapy to ameliorate complications of COVID‐19 (ATTACC): study design and methodology for an international, adaptive Bayesian randomized controlled trial. Clin Trials. 2020;17(5):491‐500. [DOI] [PubMed] [Google Scholar]
- 17. Sholzberg M, Tang GH, Negri E, et al. Coagulopathy of hospitalised COVID‐19: a pragmatic randomised controlled trial of therapeutic anticoagulation versus standard care as a rapid response to the COVID‐19 pandemic (RAPID COVID COAG – RAPID Trial): a structured summary of a study protocol for a randomised controlled trial. Trials. 2021;22(1):202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. REMAP‐CAP Investigators , Gordon AC, Mouncey PR, et al. Interleukin‐6 receptor antagonists in critically ill patients with Covid‐19. N Engl J Med. 2021;384(16):1491‐1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. WHO Solidarity Trial Consortium , Pan H, Peto R, Henao‐Restrepo A‐M, et al. Repurposed antiviral drugs for covid‐19 ‐ interim WHO solidarity trial results. N Engl J Med. 2021;384(6):497‐511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. da Costa BR, Juni P. Systematic reviews and meta‐analyses of randomized trials: principles and pitfalls. Eur Heart J. 2014;35(47):3336‐3345. [DOI] [PubMed] [Google Scholar]
- 21. Sholzberg M, Tang GH, Rahhal H, et al. Effectiveness of therapeutic heparin versus prophylactic heparin on death, mechanical ventilation, or intensive care unit admission in moderately ill patients with Covid‐19 admitted to hospital: RAPID randomised clinical trial. BMJ. 2021;375:n2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Spyropoulos AC, Goldin M, Giannis D, et al. Efficacy and safety of therapeutic‐dose heparin vs standard prophylactic or intermediate‐dose heparins for thromboprophylaxis in high‐risk hospitalized patients with COVID‐19: The HEP‐COVID randomized clinical trial. JAMA Intern Med. 2021. doi: 10.1001/jamainternmed.2021.6203. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Goldin M, Giannis D, Diab W, et al. Treatment‐dose LMWH versus prophylactic/intermediate dose heparins in high‐risk COVID‐19 inpatients: rationale and design of the HEP‐COVID trial. Thromb Haemost. 2021. [DOI] [PubMed] [Google Scholar]
- 24. Lemos ACB, do Espírito Santo DA, Salvetti MC, et al. Therapeutic versus prophylactic anticoagulation for severe COVID‐19: a randomized phase II clinical trial (HESACOVID). Thromb Res. 2020;196:359‐366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lopes RD, de Barros E, Silva PGM, et al. Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID‐19 and elevated D‐dimer concentration (ACTION): an open‐label, multicentre, randomised, controlled trial. Lancet. 2021;397(10291):2253‐2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. INSPIRATION Investigators , Sadeghipour P, Talasaz AH, et al. Effect of intermediate‐dose vs standard‐dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID‐19 admitted to the intensive care unit: the INSPIRATION randomized clinical trial. JAMA. 2021;325(16):1620‐1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Perepu US, Chambers I, Wahab A, et al. Standard prophylactic versus intermediate dose enoxaparin in adults with severe COVID‐19: a multi‐center, open‐label, randomized controlled trial. J Thromb Haemost. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Poor HD. Pulmonary thrombosis and thromboembolism in COVID‐19. Chest. 2021;160(4):1471‐1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Iba T, Levy JH, Levi M, Connors JM, Thachil J. Coagulopathy of coronavirus disease 2019. Crit Care Med. 2020;48(9):1358‐1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ortega‐Paz L, Galli M, Capodanno D, et al. Safety and efficacy of different prophylactic anticoagulation dosing regimens in critically and non‐critically ill patients with COVID‐19: a systematic review and meta‐analysis of randomized controlled trials. Eur Heart J Cardiovasc Pharmacother. 2021. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bikdeli B. Anticoagulation in COVID‐19: randomized trials should set the balance between excitement and evidence. Thromb Res. 2020;196:638‐640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tritschler T, Mathieu M‐E, Skeith L, et al. Anticoagulant interventions in hospitalized patients with COVID‐19: a scoping review of randomized controlled trials and call for international collaboration. J Thromb Haemost: JTH. 2020;18(11):2958‐2967. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1


