Abstract
Aggressive angiomyxoma is a rare locally invasive mesenchymal neoplasm of unknown pathogenesis arising predominantly in pelvic and perineal tissues of adult women. Surgical excision is the classical management but is associated with the risk of recurrence, especially with incomplete excision. There is a proposed role for adjuvant hormonal therapy. We report a very rare case of urethral aggressive angiomyxoma, managed by surgical excision, in a 40-year-old woman who presented with severe hematuria with clot retention.
Keywords: Angiomyxoma, hematuria, vulvar mass
Aggressive angiomyxoma (AAM) is a rare locally aggressive neoplasm of mesenchymal origin that arises predominantly in the pelvic, perineal, and vulvar regions of adult women, especially those of reproductive age. Radical excision of the AAM masses is the usual management.1,2 We report a very rare case of female urethral AAM with an unusual presentation.
CASE REPORT
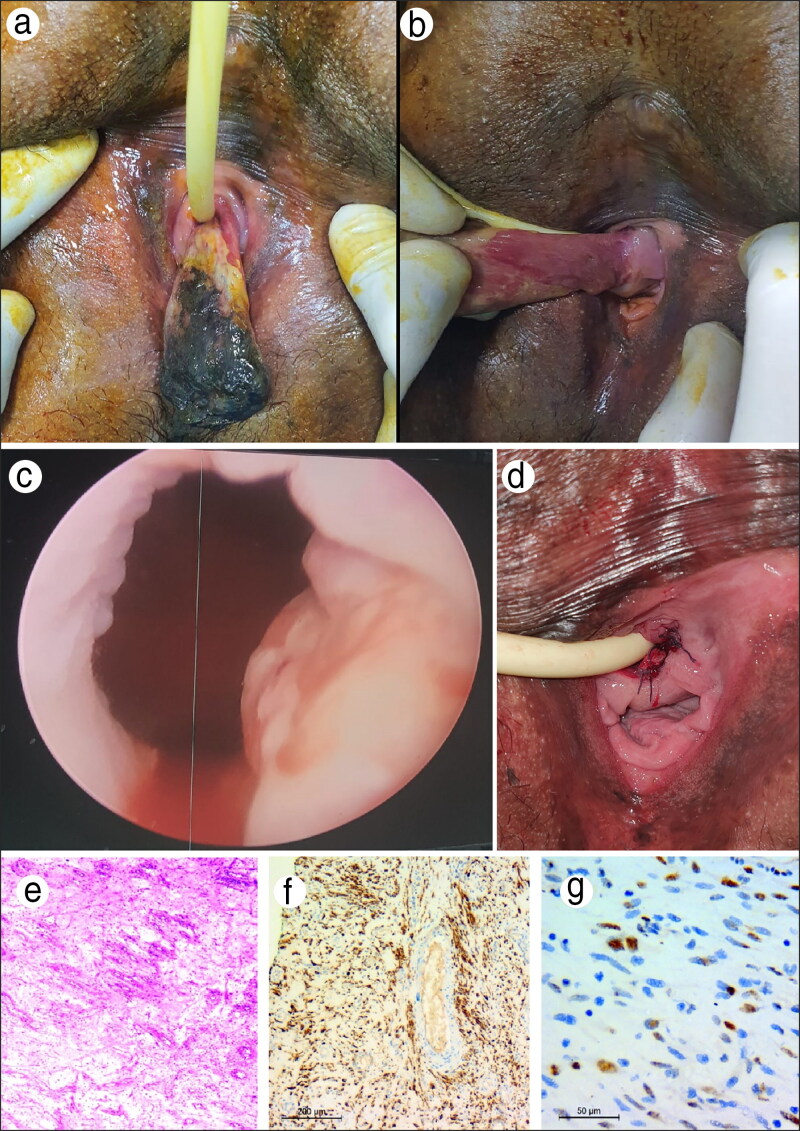
A 40-year-old woman presented with hematuria and clot retention with a rapidly growing periurethral polypoidal mass within the previous 2 months. Examination revealed a periurethral oblong fleshy polypoidal mass of about 7 × 3 cm with a bluish ischemic tip. The patient reported recurrent hematuria and clot retention with an indwelling urethral catheter for 1 month (Figure 1a, 1b). Multiphasic computed tomography with contrast showed a large blood clot within the bladder lumen with otherwise normal kidneys and normal pelvic organs. Other than a history of hypertension, the patient had no significant medical and surgical history. She had two previous normal deliveries. Cystourethroscopy revealed an intraluminal blood clot without evident extension of the mass inside the urethral or bladder lumen. A suspicious mucosa at the left side of the bladder neck and a small polypoidal lesion at the posterior bladder wall were found (Figure 1c). Biopsy of the bladder lesions together with surgical excision of the paraurethral mass was done after cystourethroscopy. The urethral catheter was left for 10 days after mass excision.
Figure 1.
(a, b) The relation of the mass to the urethra with urethral catheter. (c) Cystoscopy showing suspicious mucosa at the bladder neck. (d) Postoperative picture after the mass was excised. (e–g) Histopathology showing (e) a hypocellular lesion with bland-looking neoplastic spindle to stellate cells with small-sized blood vessels in a myxoid background, with neoplastic cells showing immunoreactivity for (f) desmin and (g) estrogen receptor.
Pathology of the periurethral mass revealed keratinized stratified squamous epithelium overlying locally infiltrative tumor growth with myxoid stroma and spindle and stellate cells of bland nuclei and no mitoses associated with haphazard dilated capillaries and scattered large thick-walled blood vessels (Figure 1e). The specimen showed positive immunohistochemistry for desmin and estrogen receptor (Figures 1f, 1g), and staining with Alcian blue stain confirmed the diagnosis of AAM. A biopsy of the bladder and bladder neck showed acute on top of chronic inflammation with normal urothelium and an edematous lamina propria–mixed inflammatory infiltrate.
A monthly injection of gonadotropin-releasing hormone agonists was initiated 2 months after surgery to minimize the risk of tumor recurrence. At 6-month follow-up, no sequelae were found, and the patient had normal voiding functions.
DISCUSSION
AAM is a rare soft tissue neoplasm with a predilection for the pelvic, perineal, and vulvar regions of adult women of reproductive age. In extremely rare cases, AAM has been reported in men involving the scrotum, spermatic cord, or prostate.3,4 It is considered an aggressive tumor associated with a high risk of local recurrence after surgery; distant metastasis has been reported in only two case reports.1,5
AAM usually poses a diagnostic dilemma, and it is often misdiagnosed at presentation. AAM usually appears as a painless, slowly growing mass with a wide scope of presentations based on the site.6 For the evaluation of AAM, ultrasound and magnetic resonance imaging can be utilized, and both show characteristic imaging features. Imaging can be used for evaluation of deep tumor extension and planning of radical surgery.7 The differential diagnosis of AAM in the periurethral area includes lipoma, urethral diverticulum, vaginal cyst, Gartner’s cyst, Bartholin cyst, pelvic organ prolapse, hernia of the canal of Nuck, and vulvar abscesses.6
No clear recommendations or guidelines could be found regarding management, but radical surgery with wide margins remains the first line of treatment in case series and reports. Depending on the presence of estrogen and progesterone receptors in tumor cells, hormonal therapy with gonadotropin-releasing hormone agonists, tamoxifen, or raloxifene has been proposed for prevention against tumor recurrence or preoperative reduction of extensive masses.2,6,8,9
The periurethral site poses a challenge for achieving adequate excision without harming the external urethral sphincter. Although the patient had gross hematuria with clots, diagnostic cystoscopy precluded evident extension of AAM inside the bladder or urethral lumen; hence, local surgical excision with biopsy of the bladder and urethral mucosa was performed. Adjuvant hormonal therapy can be used to reduce the risk of recurrence where wide excision may be harmful.
In conclusion, we report the second case of periurethral AAM, with the new presentation of hematuria with clots and urine retention. Although it is rare, AAM should be kept in the differential diagnosis of perineal, pelvic, and vulvar masses. Radical excision guided by adequate preoperative imaging should be the aim whenever possible.
References
- 1.Haldar K, Martinek IE, Kehoe S.. Aggressive angiomyxoma: a case series and literature review. Eur J Surg Oncol. 2010;36(4):335–339. doi: 10.1016/j.ejso.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Dalvi AN, Garale MN, Churiwala JJ, et al. Pararectal angiomyxoma: a diagnostic dilemma. J Surg Case Rep. 2019;2019(12):rjz331. doi: 10.1093/jscr/rjz331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu Z, Yan J, Tang G.. Aggressive angiomyxoma of the prostate: a case report. Medicine (Baltimore). 2018;97(51):e13716. doi: 10.1097/MD.0000000000013716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kirkilessis G, Kakavia K, Bougiouklis D, et al. Aggressive angiomyxoma to 57-year old man. J Surg Case Rep. 2020; 2020(9):rjaa313. doi: 10.1093/jscr/rjaa313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blandamura S, Cruz J, Faure Vergara L, et al. Aggressive angiomyxoma: a second case of metastasis with patient's death. Hum Pathol. 2003;34(10):1072–1074. doi: 10.1053/S0046-8177(03)00419-2. [DOI] [PubMed] [Google Scholar]
- 6.Foust-Wright C, Allen A, Shobeiri SA.. Periurethral aggressive angiomyxoma: a case report. Int Urogynecol J. 2013;24(5):877–880. doi: 10.1007/s00192-012-1867-z. [DOI] [PubMed] [Google Scholar]
- 7.Zhao CY, Su N, Jiang YX, et al. Application of ultrasound in aggressive angiomyxoma: eight case reports and review of literature. World J Clin Cases. 2018;6(14):811–819. doi: 10.12998/wjcc.v6.i14.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun NX, Li W.. Aggressive angiomyxoma of the vulva: case report and literature review. J Int Med Res. 2010;38(4):1547–1552. doi: 10.1177/147323001003800439. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz PE, Hui P, McCarthy S.. Hormonal therapy for aggressive angiomyxoma: a case report and proposed management algorithm. J Low Genit Tract Dis. 2014;18(2):E55–E61. doi: 10.1097/LGT.0b013e3182a22019. [DOI] [PubMed] [Google Scholar]