Abstract
Penetrating globe injury can lead to serious vision loss and even loss of the eye. Intraocular foreign bodies (IOFBs) are a major cause of traumatic globe injury commonly seen in work-related accidents. We present a unique case of a large IOFB that was fully embedded within the choroid, where enucleation was pursued due to inability to safely remove the IOFB.
Keywords: Intraocular foreign body, ruptured globe, trauma
Penetrating globe injury can lead to serious vision loss and even loss of the eye. The incidence of intraocular foreign bodies (IOFB) out of all open globe injuries ranges from 18% to 41%, and the majority (55%–91%) of all IOFB are metallic.1 The mechanism of injury, extent of ocular damage, and size of the IOFB contribute to the final prognosis.2 Surgical management depends on the location and size of the IOFB as well as the extent of surrounding ocular damage. Herein we present a unique case of a large IOFB that was fully embedded within the choroid, where enucleation was pursued.
CASE REPORT
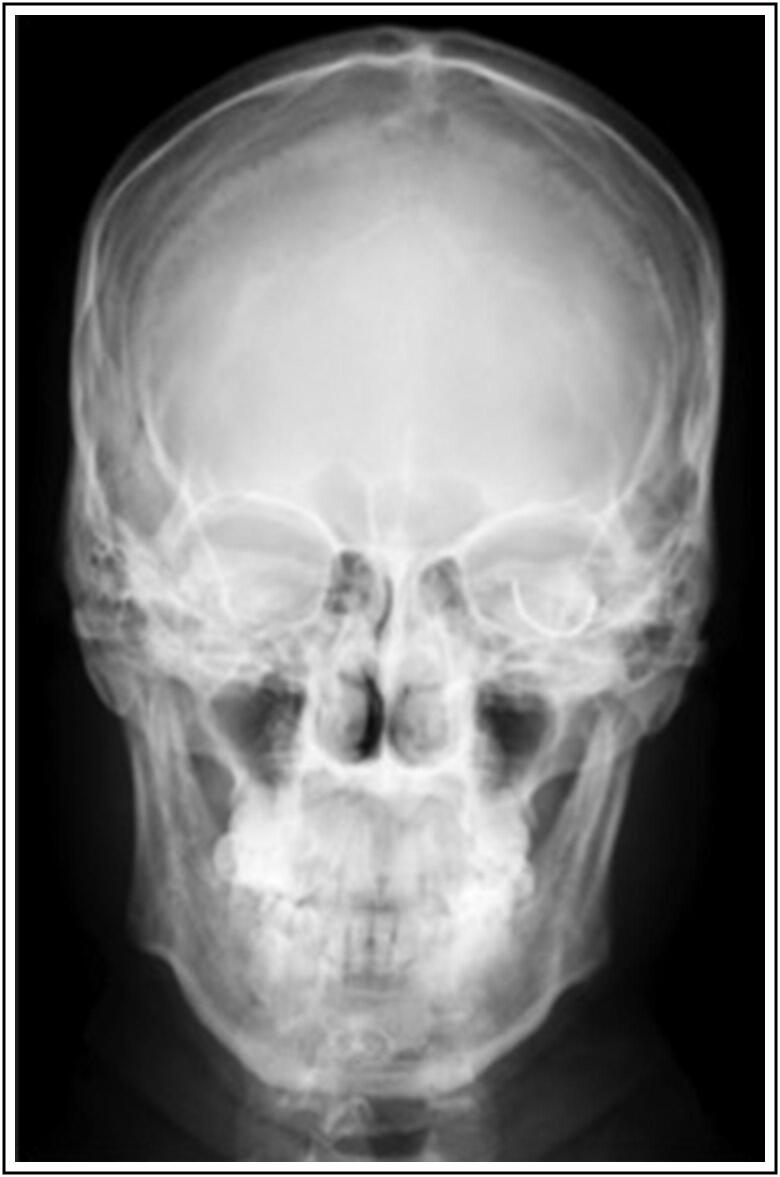
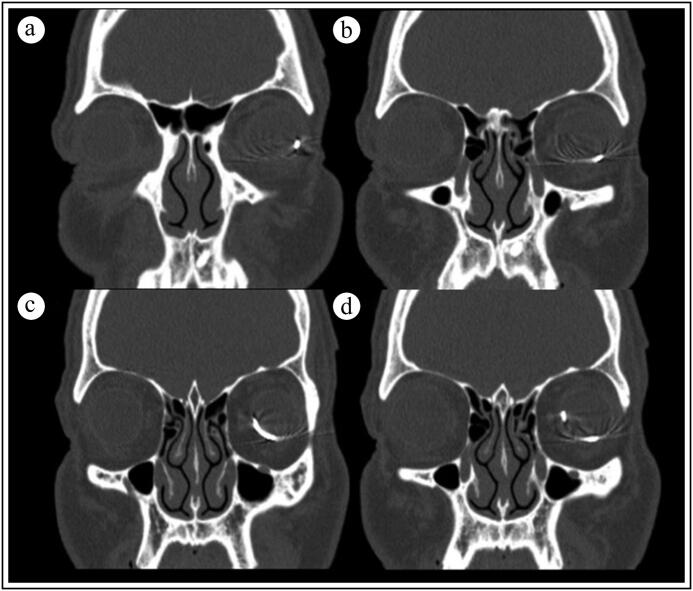
A 33-year-old man presented with acute-onset left eye pain and vision loss after operating a nail gun without eye protection. He was found to have hand motion vision in the left eye, with an afferent pupillary defect. Anterior segment exam revealed a central 3.0-mm full-thickness corneal laceration with disrupted lens material in the anterior chamber. X-ray revealed a metallic curvilinear IOFB measuring at least 2.0 cm in length (Figure 1). Computed tomography confirmed a hyperintense foreign body following the inferior hemicircumference of the left globe (Figure 2).
Figure 1.
Face x-ray revealing a curvilinear foreign body within the left orbit.
Figure 2.
Computed tomography of the orbit (a–d) revealing a curvilinear intraocular foreign body spanning the inferior hemisphere of the left globe.
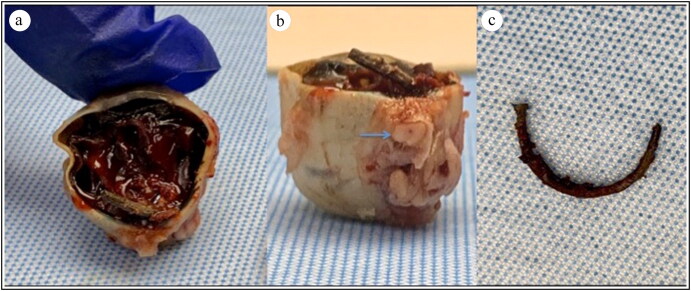
The patient was taken to the operating room for globe exploration and repair within 24 hours after the initial injury. A 360-degree conjunctival peritomy with inferior rectus disinsertion revealed an intact sclera without extrascleral foreign body extension. Following corneal laceration repair and anterior chamber washout, pars plana lensectomy and vitrectomy were performed. A tract of choroidal hemorrhage and retinal detachment were noted inferotemporally. The tip of the nail was visualized inferior to the optic nerve. Attempts at nail retrieval with intraocular forceps and magnet were unsuccessful given the embedment of the nail within the choroid. Intravitreal antibiotics were administered. Due to worsening intraocular inflammation and pain postoperatively and the anticipated low visual potential of the eye with further surgical attempt at nail removal, the patient opted to undergo enucleation. Pathologic globe evaluation revealed the curvilinear nail embedded entirely in the choroid (Figure 3).
Figure 3.
Enucleated gross globe specimen showing (a) dense vitreous hemorrhage with curvilinear nail embedded entirely in the choroid, (b) coursing inferior to the optic nerve (arrow). (c) 2.5-cm nail following removal from the globe.
DISCUSSION
IOFBs are a major cause of traumatic globe injury commonly seen in work-related accidents without the use of eye protection. Surgical management of metallic IOFB depends on the location and mobility of the IOFB. Removal of a posterior IOFB is typically pursued via a pars plana vitrectomy, with the advantage of concurrently clearing media opacities. Forceps or an electromagnet is used to remove the metallic object. When the foreign body is embedded in the retina or choroid, a sclerotomy may be performed for direct retrieval.
In a series by Greven et al, 88% of 59 reviewed IOFBs were located in the posterior chamber, with 52% embedded in the retina/choroid.3 The authors described a technique using indirect ophthalmoscopy to localize the IOFB embedded in the retina/choroid and remove it directly through a sclerotomy overlying it. Subsequent retinal cryopexy and scleral buckle placement were performed in order to decrease vitreous traction. In the same review, the authors found that the most common mechanism of injury (59%) was hammering metal on metal. These injuries were associated with a good visual prognosis because they involved small metallic foreign bodies. However, in our case, the patient was operating a nail gun, which led to the entire nail penetrating the globe.
In the case presented here, the entire body of the nail was firmly embedded within the choroid and only the tip was visualized within the posterior chamber. The entrance wound was through the cornea, and there was no extrascleral exit wound or evidence of protrusion through the sclera. Due to the curvature and extensive length of the nail entirely embedded within the inferior choroid, sclerotomy and nail manipulation were not pursued due to risk of irreparable damage without likelihood for vision improvement.
IOFBs pose a unique surgical challenge and can incur significant ocular morbidity. This report describes a rare case of a 2.5-cm curvilinear nail with complete embedment within the choroid, impeding its removal and necessitating enucleation. This case additionally highlights the importance of proper eye protection to avoid devastating ocular injury.
References
- 1.Loporchio D, Mukkamala L, Gorukanti K, et al. Intraocular foreign bodies: a review. Surv Ophthalmol. 2016;61:582–596. doi: 10.1016/j.survophthal.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 2.De Juan E, Sternberg P, Michels RG. Penetrating ocular injuries. Types of injuries and visual results. Ophthalmology. 1983;90:1318–1322. doi: 10.1016/S0161-6420(83)34387-6. [DOI] [PubMed] [Google Scholar]
- 3.Greven CM, Engelbrecht NE, Slusher MM, et al. Intraocular foreign bodies: management, prognostic factors, and visual outcomes. Ophthalmology. 2000;107:608–612. doi: 10.1016/S0161-6420(99)00134-7. [DOI] [PubMed] [Google Scholar]