Abstract
Invasive fungal infection often complicates patients with severe viral infection, especially those admitted to critical care units. Severe SARS-CoV-2 infection has been no exception and a significant association with Aspergillus spp. has been documented, resulting in high patient mortality. In this summary we describe the clinical presentation, the underlying diseases most commonly linked with this association, radiological manifestations and therapeutic management of CAPA.
Keywords: COVID-19, aspergillosis, CAPA, SARS-CoV-2, co-infection
INTRODUCTION
The relationship between invasive aspergillosis (IA) and viral infection, mainly influenza A, in critically ill patients with acute respiratory distress syndrome (ARDS) is widely known nowadays. Since 1972, when this association was first published [1], this association had hardly been described. However, in 2011, and following the remarkable advancements made in diagnostic techniques for influenza infection—that is, a real-time polymerase chain reaction (PCR) performed on nasopharyngeal throat swabs—and invasive aspergillosis, the role of invasive pulmonary aspergillosis (IPA) complicating severe influenza became more evident.
Indeed, several publications demonstrated a strong association between the two diseases [2,3]. In one particular paper, investigators developed the AspICU algorithm [4] to define IPA in critical care patients with viral infections.
One of the most important publications in this field detailed the relationship between viral infections and Aspergillus in 40 patients admitted to intensive care units (ICU) in two tertiary hospitals in Belgium. Investigators described up to 23% of patients with severe influenza infections had further complications due to Aspergillus [3,5].
That all stated, when patients with IA were compared with those without infection, mortality rates were much higher (51% vs 28%, respectively) [6]. Clinical forms of IA in these patients present some differences with respect to immunosup-pressed people, with more atypical findings [7]. There is a high variability in clinical manifestations, ranging from tracheo-bronchitis to invasive and angioinvasive disease [5].
COVID-19-ASSOCIATED PULMONARY ASPERGILLOSIS
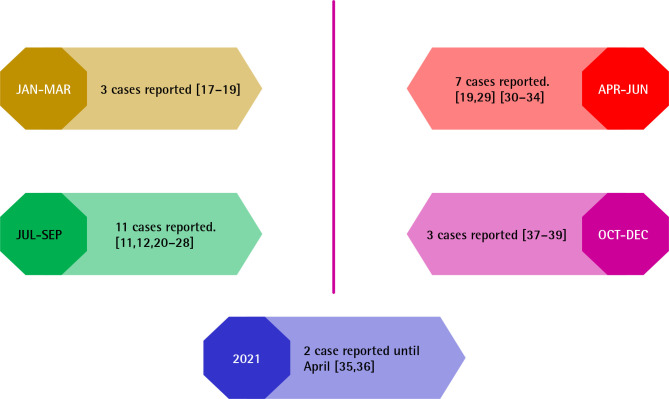
Therefore, when the COVID-19 pandemic arrived, physicians first expected to observe an increase in the incidence of Aspergillus spp. cases in relation to SARS-CoV-2 viral infection. In December 2019, autopsy reports described deceased patients with severe SARS-CoV-2 infection who developed co-infection with Aspergillus spp. In the following months, different case series were also reported (Figure 1). For example, Marr et al. [8] reported 20 cases of COVID-19-associated pulmonary aspergillosis (CAPA) occurring at Johns Hopkins University (Baltimore, MD, USA) and Hospital Clinic of Barcelona (Barcelona, Spain) before June 2020. Thanks to this international, multicenter CAPA series, we have acquired some key learnings.
Figure 1.
Quarterly timeline about cases reported for coronavirus disease–associated pulmonary aspergillosis.
First, radiographic manifestations are difficult to interpret. Chest x-rays may not be clear due to diffuse lung damage to the lung parenchyma caused by the viral infection—associated with inflammatory changes—and possible ARDS. Although cavitation and necrosis occur occasionally, no radiographic reports describe manifestations classically seen in angioinvasive cases [3,7].
Second, most of these patients had underlying diseases, predominantly prior lung disease that required ICU admission with respiratory support for more than nine days.
Third, performing cultures of respiratory samples, mainly tracheal aspirates, was the most common diagnostic testing approach. In the study by Marr et al. [8], only 25% of serum galactomannan (GM) was positive among patients with CAPA. Conversely, because of invasive diagnostic strategies used in both centers and the lower rate of angioinvasion, 17 of 20 (85%) respiratory cultures tested positive. This observance may be attributable to the fact that these patients were in early stages of the disease. In this series, mortality rates were relatively low.
Furthermore, Salmanton-Garcia et al. [9] reported 186 cases of CAPA across 17 different countries collected from Fungiscope (a global emerging fungal infection registry; https://www.clinicaltrials.gov; National Clinical Trial identifier NCT01731353) and a literature search. In this large series, we found again that 97.8% of patients were admitted to the ICU, and 94.1% required mechanical ventilation. Investigators observed median days until CAPA diagnosis of 10, which was similar to data reported in the multicentric series by Marr et al. [8]. A notable difference between both studies is that up to 60.8% of total CAPA were diagnosed with a positive GM, mainly due to bronchoalveolar lavage (BAL). This data suggests that these patients were in advanced stages of the disease with the presence of angioinvasion. Also, described mortality rates (52.2%) were higher.
Due to the importance of this entity, a group of 22 experts from six continents and 14 countries gathered together to develop guidelines for the management, diagnosis and treatment of CAPA [10]. In this review, they proposed three clinical forms: i) proven aspergillosis when invasive growth of Aspergillus was evidenced in histopathological and/or microbiological samples obtained from a sterile tissue; ii) probable aspergillosis when Aspergillus spp. evidence was obtained from BAL or blood (culture, GM, or Aspergillus PCR); iii) possible aspergillosis when compatible radiological findings were described together with mycological evidence obtained via non-bronchoscopic lavage. In conclusion, should clinical findings elicit suspicion and meet inclusion criteria, it is necessary to initiate diagnostic tests for CAPA, so as to avoid a rapid and undesirable evolution towards more invasive forms.
As high mortality has been reported in cases of CAPA, [11,12] early and adequate therapy is crucial. Traditionally, voriconazole or isavuconazole has AI evidence for the treatment of IA in main guidelines [13]. However, both drugs are quite different. Table 1 summarizes potential advantages with the use of isavuconazole. Remarkably, isavuconazole has fewer interactions than voriconazole. This fact is of main interest in patients with COVID-19, especially in those who require ICU admission. Baniasadi et al. [14] reported data from a prospective study about drug-drug interactions among patients in ICU, and voriconazole was one of the more frequently involved drugs due to its ability to inhibit CYP3A4 [15]. Secondarily, voriconazole interacts with corticosteroids, some sedative drugs and remdesivir. Isavuconazole is metabolized differently via CYP2C19, CYP2C9, and CYP3A4, which makes the possibility of drug-drug interaction significantly lower. The use of voriconazole must therefore be associated with therapeutic drug monitoring on a weekly basis, given its drug-drug interaction and great interpersonal variability due to genetic polymorphisms of CYP3A4.
Table 1.
Main advantages of isavuconazole versus voriconazole.
| Broad spectrum. |
| Linear and predictable pharmacokinetics. |
| Not influenced by genetic polymorphisms or by diet. |
| Few intervariabilities. |
| Does not need therapeutic drug monitoring. |
| High volume of distribution; high dose in lung. |
| Few interactions with other drugs. |
| Few side effects. |
| Cyclodextrin-free. |
| Can be used in renal failure, dialysis, and hemodialysis. |
Finally, it is important to note that critically ill patients with SARS-CoV-2 infection may suffer from other fungal infections [16]. Like other patients admitted to the ICU, critically ill patients with SARS-CoV-2 can develop candidemia due to prolonged ICU length of hospital stay, invasive medical devices, use of broad-spectrum antibiotics and corticosteroids, etc. More occasionally, though, other fungal infections like Pneumocystis jirovecci or mucormycosis have been described.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Fischer JJ, Walker DH. Invasive Pulmonary Aspergillosis Associated With Influenza. JAMA J Am Med Assoc 1979; 241:1493–1494. [PubMed] [Google Scholar]
- 2.Van De Veerdonk FL, Kolwijck E, Lestrade PPA, et al. Influenza-associated aspergillosis in critically ill patients. Am J Respir Crit Care Med 2017; 196:524–527 [DOI] [PubMed] [Google Scholar]
- 3.Vanderbeke L, Spriet I, Breynaert C, Rijnders BJA, Verweij PE, Wauters J. Invasive pulmonary aspergillosis complicating severe influenza: epidemiology, diagnosis and treatment. Curr. Opin. Infect. Dis. 2018; 31:471–480. [DOI] [PubMed] [Google Scholar]
- 4.Verweij PE, Rijnders BJA, Brüggemann RJM, et al. Review of influenza-associated pulmonary aspergillosis in ICU patients and proposal for a case definition: an expert opinion. Intensive Care Med 2020; 46:19. Doi: 10.1007/s00134-020-06091-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jenks JD, Nam HH, Hoenigl M. Invasive aspergillosis in critically ill patients: Review of definitions and diagnostic approaches. Mycoses. 2021; 64(9):1002-1014. doi: 10.1111/myc.13274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schauwvlieghe AFAD, Rijnders BJA, Philips N, et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Respir Med 2018; 6:782–792. [DOI] [PubMed] [Google Scholar]
- 7.Koehler P, Bassetti M, Kochanek M, Shimabukuro-Vornhagen A, Cornely OA. Intensive care management of influenza-associated pulmonary aspergillosis. Clin. Microbiol. Infect. 2019; 25:1501–1509. [DOI] [PubMed] [Google Scholar]
- 8.Marr KA, Platt A, Tornheim JA, et al. Aspergillosis complicating severe coronavirus disease. Emerg Infect Dis 2021; 27:18–25. Doi: 10.3201/eid2701.202896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salmanton-García J, Sprute R, Stemler J, Bartoletti M, Dupont D, Valerio M, et al. COVID-19-Associated Pulmonary Aspergillosis, March-August 2020. Emerg Infect Dis. 2021;27(4):1077-1086. doi: 10.3201/eid2704.204895.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koehler P, Bassetti M, Chakrabarti A, et al. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis 2021; 21(6):e149-e162. doi: 10.1016/S1473-3099(20)30847-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bartoletti M, Pascale R, Cricca M, et al. Epidemiology of invasive pulmonary aspergillosis among COVID-19 intubated patients: a prospective study. Clin Infect Dis. 2020. Jul 28:ciaa1065. doi: 10.1093/cid/ciaa1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.White PL, Dhillon R, Cordey A, et al. A National Strategy to Diagnose Coronavirus Disease 2019–Associated Invasive Fungal Disease in the Intensive Care Unit. Clin Infect Dis. 2020. Aug 29;ciaa1298. doi: 10.1093/cid/ciaa1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia-Vidal C, Alastruey-Izquierdo A, Aguilar-Guisado M, et al. Clinical practice guideline for the management of invasive diseases caused by Aspergillus: 2018 Update by the GEMICOMED-SEIMC/ REIPI Documento de consenso del GEMICOMED perteneciente a la Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica (SEIMC) sobre el tratamiento de las infecciones invasoras producidas por Aspergillus. Enferm Infecc Microbiol Clin (Engl Ed). 2019;37(8):535-541. doi: 10.1016/j.eimc.2018.03.018 [DOI] [PubMed] [Google Scholar]
- 14.Baniasadi S, Farzanegan B, Alehashem M. Important drug classes associated with potential drug-drug interactions in critically ill patients: highlights for cardiothoracic intensivists. Ann Intensive Care 2015; 5:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.M.Pereira J, A. Paiva J. Antimicrobial Drug Interactions in the Critically Ill Patients. Curr Clin Pharmacol 2013; 8:25–38. [PubMed] [Google Scholar]
- 16.Pemán J, Ruiz-Gaitán A, García-Vidal C, et al. Fungal co-infection in COVID-19 patients: Should we be concerned? Rev. Iberoam. Micol. 2020; 37:41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen X, Zhao B, Qu Y, et al. Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely associated with drastically elevated interleukin 6 (IL-6) level in critically ill COVID-19 patients. medRxiv. 2020; [DOI] [PMC free article] [PubMed]
- 18.Lescure FX, Bouadma L, Nguyen D, et al. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect Dis 2020; 20:697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alanio A, Dellière S, Fodil S, Bretagne S, Mégarbane B. Prevalence of putative invasive pulmonary aspergillosis in critically ill patients with COVID-19. Lancet Respir. Med. 2020; 8:e48–e49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Helleberg M, Steensen M, Arendrup MC. Invasive aspergillosis in patients with severe COVID-19 pneumonia. Clin. Microbiol. Infect. 2021; 27:147–148.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Arkel ALE, Rijpstra TA, Belderbos HNA, van Wijngaarden P, Verweij PE, Bentvelsen RG. COVID-19-associated pulmonary aspergillosis. Am. J. Respir. Crit. Care Med. 2020; 202:132–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blaize M, Mayaux J, Nabet C, et al. Fatal Invasive Aspergillosis and Coronavirus Disease in an Immunocompetent Patient. Emerg Infect Dis 2020; 26:1636–1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ghelfenstein-Ferreira T, Saade A, Alanio A, et al. Recovery of a triazole-resistant Aspergillus fumigatus in respiratory specimen of COVID-19 patient in ICU–A case report. Med Mycol Case Rep 2021; 31:15–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Santana MF, Pivoto G, Alexandre MAA, et al. Confirmed invasive pulmonary aspergillosis and COVID-19: The value of postmortem findings to support antemortem management. Rev Soc Bras Med Trop 2020; 53:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nasir N, Farooqi J, Mahmood SF, Jabeen K. COVID-19-associated pulmonary aspergillosis (CAPA) in patients admitted with severe COVID-19 pneumonia: An observational study from Pakistan. Mycoses 2020; 63:766–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lamoth F, Glampedakis E, Boillat-Blanco N, Oddo M, Pagani JL. Incidence of invasive pulmonary aspergillosis among critically ill COVID-19 patients. Clin. Microbiol. Infect. 2020; 26:1706–1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Van Biesen S, Kwa D, Bosman RJ, Juffermans NP. Detection of invasive pulmonary aspergillosis in COVID-19 with Nondirected BAL. Am. J. Respir. Crit. Care Med. 2020; 208:1171–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Falces-Romero I, Ruiz-Bastián M, Díaz-Pollán B, et al. Isolation of Aspergillus spp. in respiratory samples of patients with COVID-19 in a Spanish Tertiary Care Hospital. Mycoses 2020; 63:1144–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prattes J, Valentin T, Hoenigl M, Talakic E, Reisinger AC, Eller P. Invasive pulmonary aspergillosis complicating COVID-19 in the ICU-A case report. Med Mycol Case Rep 2021; 31:2–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koehler P, Cornely OA, Böttiger BW, et al. COVID-19 associated pulmonary aspergillosis. Mycoses 2020; 63:528–534.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rutsaert L, Steinfort N, Van Hunsel T, et al. COVID-19-associated invasive pulmonary aspergillosis. Ann. Intensive Care. 2020; 10:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang J, Yang Q, Zhang P, et al. Clinical characteristics of invasive pulmonary aspergillosis in patients with COVID-19 in Zhejiang, China: A retrospective case series. Crit Care 2020; 24:299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meijer EFJ, Dofferhoand ASM, Meis JF, Hoiting O, Buil JB. Azole-resistant COVID-19-associated pulmonary aspergillosis in an immunocompetent host: A case report. J Fungi 2020; 6:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mohamed A, Hassan T, Trzos-Grzybowska M, et al. Multi-triazole-resistant Aspergillus fumigatus and SARS-CoV-2 co-infection: A lethal combination. Med Mycol Case Rep 2021; 31:11–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hakamifard A, Hashemi M, Fakhim H, Aboutalebian S, Hajiahmadi S, Mohammadi R. Fatal disseminated aspergillosis in an immunocompetent patient with COVID-19 due to Aspergillus ochraceus. J Med Mycol 2021; 31(2):101124. doi: 10.1016/j.mycmed.2021.101124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Imoto W, Himura H, Matsuo K, et al. COVID-19-associated pulmonary aspergillosis in a Japanese man: A case report. J Infect Chem-other 2021; 27:911–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sasoni N, Rodriguez Müller M, Posse G, González J, Leonardelli F, Garcia-Effron G. SARS-CoV-2 and Aspergillus section Fumigati coinfection in an immunocompetent patient treated with corticosteroids. Rev Iberoam Micol 2021; 38:16–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haglund A, Christensen S, Kristensen L, Gertsen JB, Buus L, Lausch KR. Invasive pulmonary aspergillosis and hyperthermia in an immunocompetent patient with COVID-19. Med Mycol Case Rep 2021; 31:29–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Witting C, Quaggin-Smith J, Mylvaganam R, Peigh G, Angarone M, Flaherty JD. Invasive pulmonary aspergillosis after treatment with tocilizumab in a patient with COVID-19 ARDS: a case report. Diagn Microbiol Infect Dis. 2021;99(4):115272. doi: 10.1016/j.diagmicrobio.2020.115272 [DOI] [PMC free article] [PubMed] [Google Scholar]