Abstract
Objective:
To investigate discrepancies in results of facial asymmetry analysis using different cone beam computed tomography (CBCT) image reorientation methods and the effectiveness of soft tissue as a reorientation reference for analysis of facial asymmetry.
Materials and Methods:
An asymmetric group of 30 patients with 4 mm or more of chin point (menton [Me]) deviation and a symmetric group of 30 patients with less than 4 mm of deviation of Me were chosen as study subjects. Three orientation methods were used to calculate and compare Me deviation values of the 60 subjects. Two methods used only skeletal landmarks for reference, and one method included the soft tissue landmarks around the eye. Preferences of an expert group for the facial midline as determined by each reorientation method were also examined.
Results:
The examinations showed significant discrepancies in Me deviation values between the three reorientation methods. The expert group showed the greatest preference for the facial midline reorientation method that incorporated soft tissue landmarks of the eye.
Conclusions:
These study findings suggest that the inclusion of soft tissue landmarks, especially those around the eyes, is effective for three-dimensional CBCT image reorientation for facial asymmetry analysis.
Keywords: Facial asymmetry, Cone beam computed tomography image reorientation, Soft tissue reference
INTRODUCTION
Appropriate symmetry is an essential factor in facial esthetics.1 However, a person with a reasonably symmetric face cannot achieve complete facial symmetry.2 Therefore, accurate judgment of the degree of asymmetry is necessary when diagnosing and planning treatment for facial asymmetry, because the prescribed treatment will vary depending on the recognition of the severity of the asymmetry and the symptoms of facial asymmetry.
Facial asymmetry is generally assessed using objective values.3 The posteroanterior (PA) cephalograph has traditionally been used, and it has been reported that some indices of the PA cephalograph are reliable for evaluating asymmetry.4 However, the accuracy of quantitative evaluation is limited because of the overlapping of structures and magnification discrepancies by site, because PA cephalographs require that a three-dimensional (3D) solid structure be projected onto a 2D surface.5,6 The 3D approach to the diagnosis of facial asymmetry has been actively tried recently.3 Three-dimensional digital image diagnosis data go through a process called reorientation, which involves the adjustment of the head position on software images. However, just as the results of asymmetry analysis based on different head positions differ when traditional 2D cephalometry is used,7,8 reorientation also significantly influences the results obtained using 3D digital imaging data, especially in cone beam computed tomography (CBCT).
Patient satisfaction with treatment decision making and treatment outcomes is determined subjectively,9 and it is mainly the soft tissue results that are used by patients to judge treatment outcomes. However, the results of cephalometric analysis of skeletal asymmetry may differ from the results of soft tissue analysis.10 In other words, although skeletal asymmetry exists, it may be disguised by the soft tissues, or although a face may possess skeletal symmetry, it could be asymmetric because of asymmetric soft tissues. Accordingly, considerations of the soft tissues are as important as those of the hard tissues when diagnosing facial asymmetry.11
The purposes of this study were to investigate discrepancies between assessments of facial asymmetry obtained using different CBCT image reorientation methods and to examine the effectiveness of soft tissue as a reorientation reference for analysis of facial asymmetry.
MATERIALS AND METHODS
Subjects
This retrospective study was performed by the Institutional Review Board of Gachon University Gil Hospital. Patients who visited the Department of Orthodontics, Gil Hospital, Gacheon Medical School, between August 2010 and March 2012 with the chief complaint of a need for orthodontic treatment were selected as potential subjects. Deviation of menton (Me) was measured using the vertical bisection line of bilateral latero-orbitale, which is used as a facial midline in 2D cephalometry. Thirty patients with <4 mm of unilateral deviation were allocated to a symmetric group and 30 patients with ≥4 mm of unilateral deviation were allocated to an asymmetric group.12 Subjects included 27 male patients and 33 female patients (mean age: 21.1 ± 7.1 years).
Inclusion criteria were as follows:
A completely formed occlusal plane, ie, fully erupted bilateral upper and lower first molars and permanent incisors.
No congenital midfacial abnormality.
No particular abnormalities of the periocular soft tissues.
The availability of CBCT images with evaluable resolution.
Acquisition of CBCT Images
CBCT (3D eXam scanner, KaVo Dental GmbH, Biberach, Germany) scanning was performed at 120 kV, 5 mA, and 17.8 seconds. The field of view was 230 × 170 mm and the voxel size was 0.3 mm. CBCT was performed with the patients sitting comfortably. Each patient was asked to close his or her mouth in maximum intercuspation and to stare at his or her own eyes with a neutral facial expression in a mirror that was 1.5 m away. CBCT images for all patients were taken for the purpose of orthodontic treatment. Digital image data were obtained from CBCT images and transmitted to a computer for 3D image construction using InVivoDental (Anatomage Inc, San Jose, Calif).
Settings of Reorientation Methods
Three types of reorientation methods were established using hard tissue landmarks, ie, crista galli, anterior nasal spine, basion, orbitale, porion, and medial point of the frontozygomatic suture, and soft tissue landmarks, ie, endocanthion, palpebrale superius, palpebrale inferius, and the midpoint of palpebrale superius and palpebrale inferius (Table 1).
Table 1.
Definitions of Skeletal and Soft Tissue Landmarks
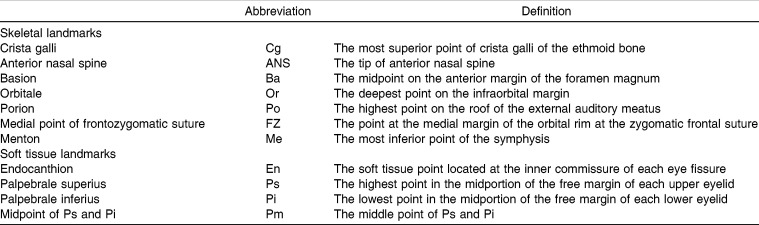
Method A: The plane perpendicular to the horizontal reference plane and passing through right and left Po and right Or and including Cg and Ba was established as the midsagittal reference plane (Figure 1).
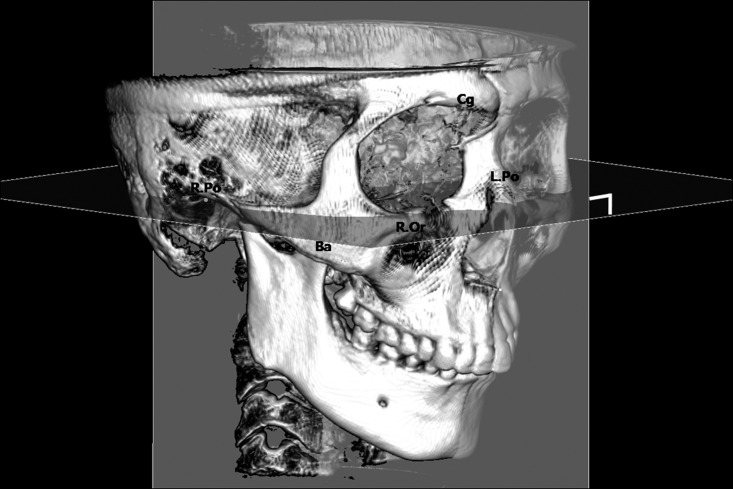
Method B: A midsagittal reference plane passing through Cg, ANS, and Ba was established. The pitch was controlled by equating the z-coordinate value of right Po and right Or (Figure 2).
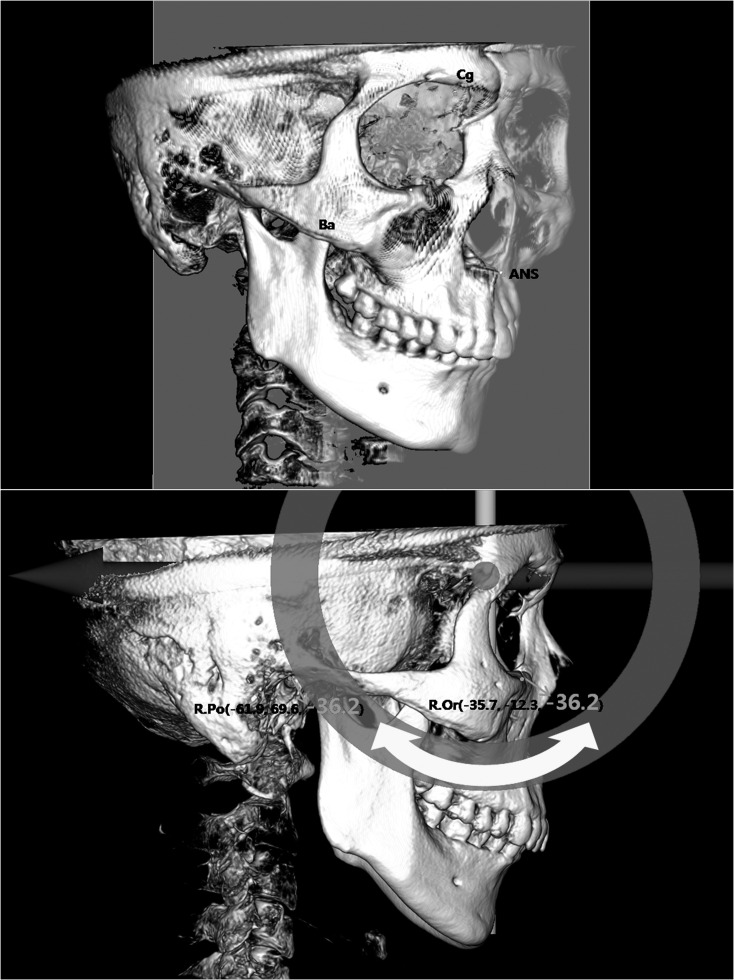
Method C: The yaw was adjusted by equating the y-coordinate values of right and left FZ, the pitch was adjusted by equating the z-coordinate values of right Po and right Or, and the roll was adjusted by equating the z-coordinate values of right and left Pm. Finally, the sagittal plane that passes through the median point of right and left En was established as the midsagittal reference plane (Figure 3).
Figure 1.
Reorientation method A showing the horizontal reference plane (right Po, left Po, right Or) and the midsagittal reference plane (Cg, Ba), which is perpendicular to the horizontal reference plane.
Figure 2.
Reorientation method B showing the midsagittal reference plane (Cg, ANS, Ba) and pitch adjustment (vertical components of the z coordinate values of right Po, and right Or).
Figure 3.
Reorientation method C, which used soft tissue landmarks. (a) After performing rolling adjustment by matching the z-values of Pm bilaterally. (b) The plane that passed through the midpoint of the x-values of En bilaterally was established as the midsagittal reference plane.
Examining Me Deviation Values Using Different Reorientation Methods
Designation of landmarks and reorientation were performed by one examiner. When a landmark was designated on a CBCT image, the 3D volume-rendering view and a multiplanar reconstruction view were used. The value for deviation of Me was defined as the shortest x-axis coordinate value from Me to the midsagittal reference plane and measured using the 3D analysis function in InVivoDental (Anatomage Inc). For convenience, right deviations of Me were given negative values.
Subjective Evaluation of Facial Midline (Expert Preference in the Midsagittal Reference Plane)
The midsagittal reference planes were evaluated subjectively by 12 orthodontists, each with at least 5 years of clinical experience (2 women, 10 men).
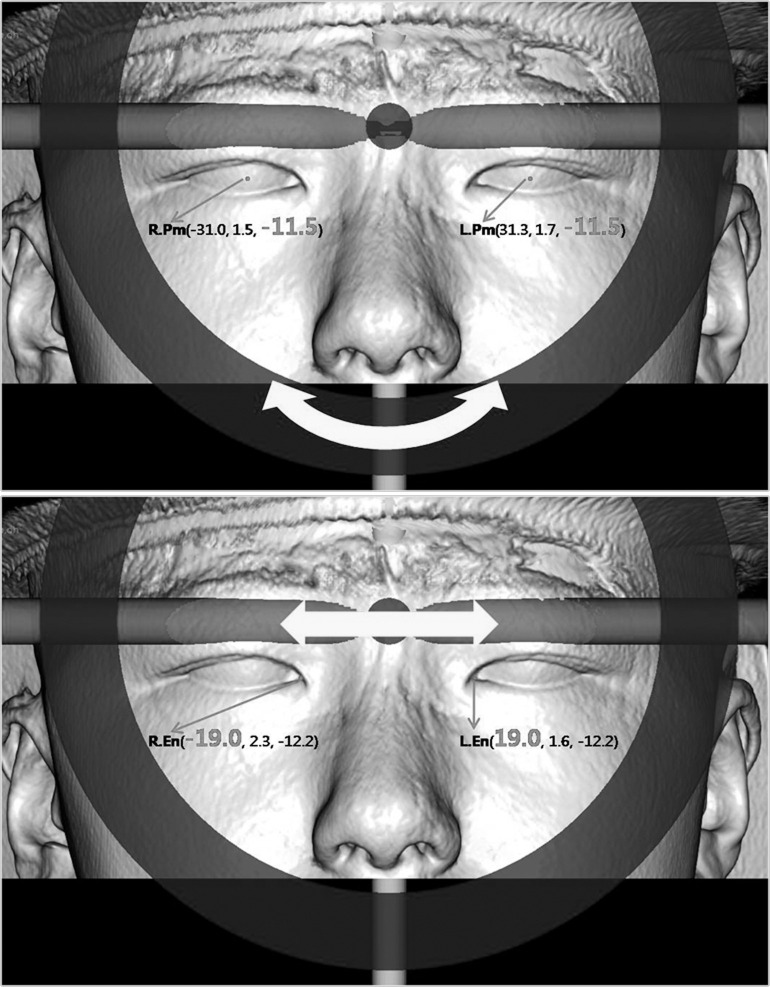
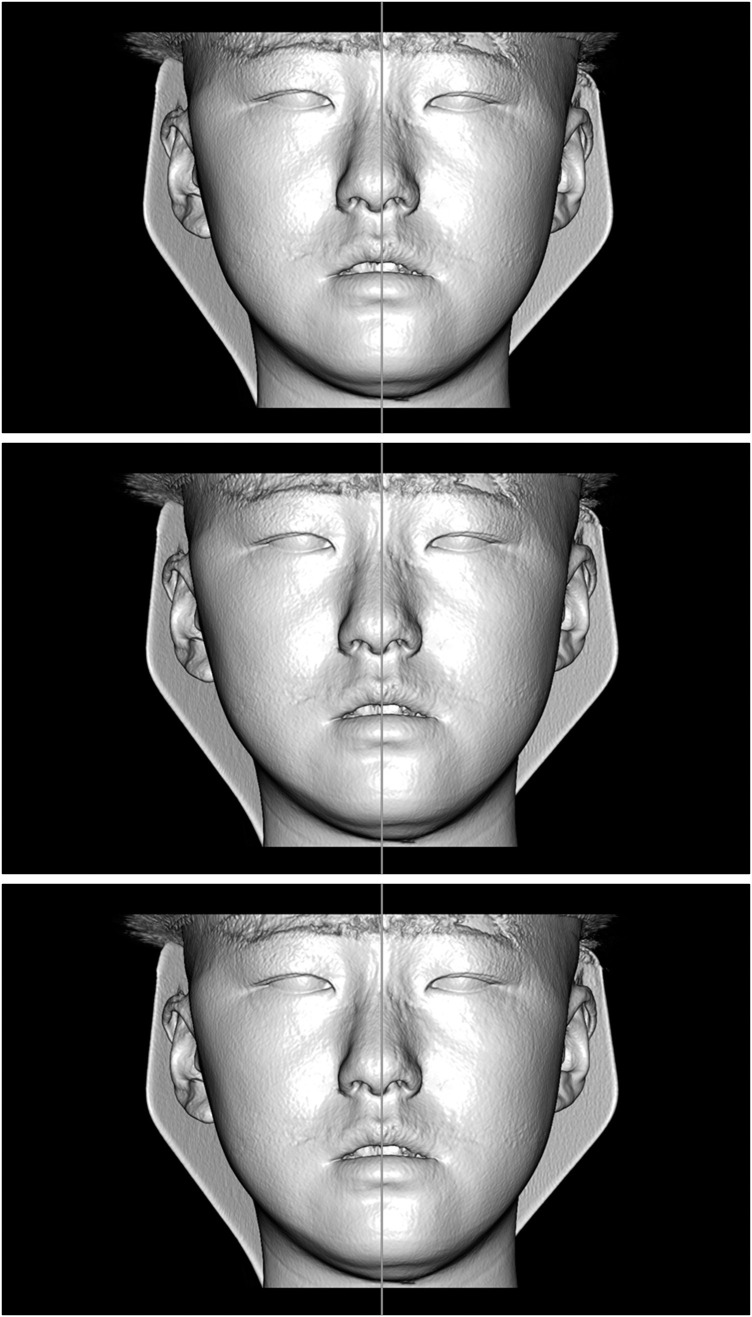
One-hundred eighty frontal-view soft tissue CBCT images, including the midsagittal reference planes derived using the three methods, were constructed for subjective evaluations of the midsagittal reference plane. Three images were made of each subject (60 × 3 = 180) (Figure 4). Evaluators were provided with group identities (asymmetry or symmetry) and the division criterion used (4 mm). No training was provided regarding techniques for establishing a midsagittal reference plane. With a 22-inch monitor, evaluators scored the reconstructions as follows.
Figure 4.
Images of facial midline and soft tissues of one subject, obtained using the three different reorientation methods.
Score 3 points: Image including facial midline was considered to be the most appropriate among the three images of the subject.
Score 2 points: Image including facial midline was considered to be the second most appropriate among the three images of the subject.
Score 1 point: Image including facial midline was considered to be the least appropriate among the three images of the subject.
When scoring images, evaluators were allowed to use each point score only once.
Statistical Analyses
SPSS for Windows 17.0 (SPSS, Chicago, Ill) was used for statistical analyses. Thirty of the 60 study subjects were randomly chosen to assess the reproducibility of asymmetry analysis. Me deviation values were measured twice by one examiner, with an interval of 2 weeks between measurements. Reproducibility of Me deviation values was verified using the paired t-test.
Discrepancies in Me deviation values between reorientation methods and subjective evaluations of facial midline preferences were analyzed using repeated-measures analysis of variance and Bonferroni's post hoc test.
RESULTS
No significant differences were found between the first and second measurements of Me deviation (P > .05).
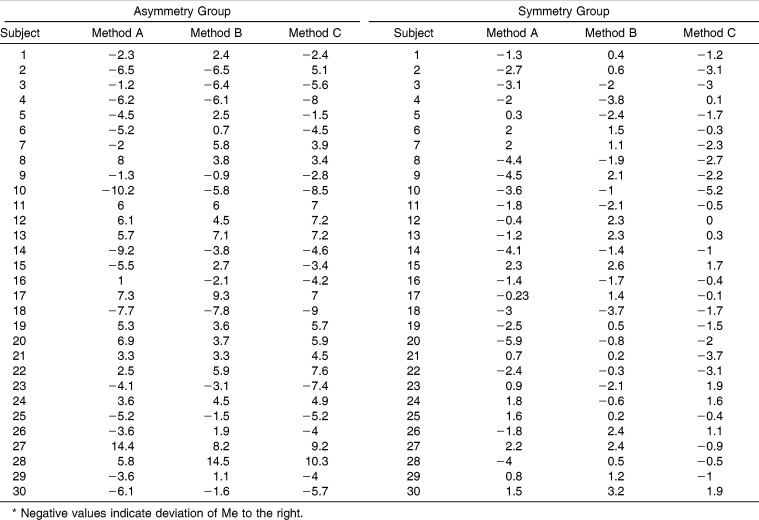
Distances between Me and the midfacial sagittal reference planes established using the three reorientation methods were measured and compared using the paired t-test. A statistically significant difference in Me deviation values was found between the symmetric and asymmetric groups (P < .05) (Table 2).
Table 2.
Me Deviation Values (in Millimeters) by Three Types of Reorientation Methods*
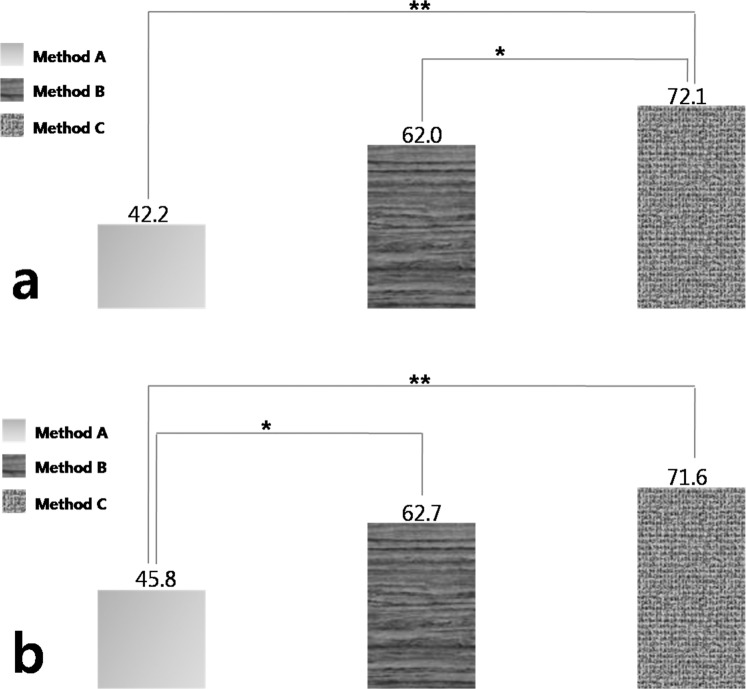
In the asymmetric group, method C produced significantly larger values for deviation than methods A or B (Figure 5). In the symmetry group, method A produced significantly smaller values for deviation than methods B or C (Figure 5).
Figure 5.
Rod graph of average scores of subjective evaluations. (a) The asymmetric group. (b) The symmetric group. * P < .05; ** P < .001.
DISCUSSION
A single specific reorientation method cannot be standardized and used for every diagnosis when CBCT is used. Appropriate CBCT reorientation methods must be selected based on the purpose and use of CBCT.8 Therefore, this study was undertaken to determine which reorientation method is the most useful for the diagnosis of asymmetry by investigating Me deviation value discrepancies and examining the facial midline preferences of an expert group using different reorientation methods.
Determination of the facial midline is significantly influenced by head position. In previous conventional cephalometric imaging studies, a cephalostat, such as an ear rod or head holder, was used to standardize subject positioning.13 However, 3D CBCT enables reorientation using software, avoiding the need for physical restraints. When evaluating asymmetry using CBCT, image reorientation is a critical step because the midsagittal reference plane is determined by appropriate reorientation, and quantitative judgments of right and left facial asymmetry can be done using this reference plane.
We intended to determine which reorientation method was most effective for the analysis of facial asymmetry. We examined two reorientation methods (methods A, B) that use hard tissue landmarks and a third method (method C) that uses a combination of hard tissue and soft tissue landmarks. Me deviation was chosen to represent facial asymmetry, because it has the greatest influence on the recognition of facial asymmetry14 and it changes sensitively by reorientation because it is located at the farthest end of the face.15 Study subjects were allocated to asymmetric or symmetric groups to determine whether the presence of clinical facial asymmetry affects the establishment of facial midline.
Statistically significant differences in Me deviations between reorientation methods were seen in both groups (Table 2). This result concurs with that of Kim et al.8 Accordingly, if the results of facial asymmetry analysis are dependent on the method of reorientation, it must be determined which method most accurately indicates the degree of facial symmetry or asymmetry.
In general, a person with a symmetric face also has some right/left differences in the soft tissue structures, and thus, considerations of facial soft tissue priorities for establishing the facial midline require subjective judgement.10
In this study, efforts were made to find an appropriate reorientation method based on expert group preferences regarding facial midline using three reorientation methods. Twelve orthodontists with at least 5 years of clinical experience showed significantly greater preference for the facial midlines of method C than those of method A in both symmetric and asymmetric groups. In a previous study, among the adjustment factors of reorientation that were examined, roll adjustment was found to be the most significant influence on Me deviation.16
In method A, roll adjustment was performed by using bilateral Po, and in method C, it was done by using the bilateral periocular soft tissue landmarks. It is assumed that the soft tissue structures related to the eyes have a greater influence on overall symmetry when the soft tissue structures around the external ear and eye are not identical and symmetric. This coincides with a previous report, which concluded that the closer a structure is to the midline, the more strongly its asymmetry affects the recognition of overall asymmetry.17,18
From the perspective of treatment of facial asymmetry, the facial midline is not the center line that bisects the pretreated face but an imaginary center line that bisects the right and left halves of the posttreatment face. In other words, the soft tissues that will not be included in the treatment should be expressed symmetrically, and in the parts of the face that will be treated, a facial midline that appropriately expresses the asymmetry should be established. This ultimately determines which part of the face should be included in the treatment plan or in which facial regions the changes after treatment are most crucial in terms of establishing a facial midline. Severt and Proffit19 found that the frequencies of asymmetry were 5% in the upper face, 36% in the middle face, and 74% in the lower face. Farkas20 found that the incidence of periocular asymmetry was less than 2% in the normal population and that the periocular tissues were more symmetric than the nose (7%) or mouth (12%). For this reason, eye landmarks were included in method C. Establishment of the facial midline using the eyes is commonly used in the analysis of a frontal view of the eyes.21 Ras et al.,22 in a stereophotographic study, reported that the vertical bisector of the lateral angle of the eye was the most appropriate facial midline. In this study, roll adjustment was done using z-coordinate values of Pi and Ps of the eyes bilaterally and the x-coordinate values of En bilaterally.
The eyes are important reference points that determine the overall impression of the face, but they may lack reproducibility as a reorientation reference in comparison to hard tissue. In this study, consistent capturing of the soft tissue morphology was attempted by asking each patient to stare at his or her own eyes in a mirror 1.5 m away while seated in a comfortable posture with a neutral facial expression when CBCT was performed. Furthermore, reproducibility of the results of analysis of facial asymmetry was reinforced by the inclusion of hard tissue reference landmarks in adjustment of pitch and yaw, which are relatively less sensitive in terms of establishing the facial midline.
The midsagittal plane derived by CBCT image reorientation is not always the final facial midline, and modification is often necessary depending on the patient's habitual head posture or treatment needs. However, if soft tissue reference marks are actively considered during the reorientation stage, the degree of modification could be minimized, and thus, this method could be used as a means of determining a facial midline that appropriately expresses the actual soft tissue symmetry. Soft tissue landmarks were limited to the eyes in this study; studies of different soft tissue landmarks would be desirable.
CONCLUSIONS
There was a statistically significant difference between reorientation methods in terms of Me deviation value in both asymmetric and symmetric patients.
The study shows that method C, in which periocular landmarks were used along with skeletal landmarks as references, was significantly more accurate than other two methods, which used only hard tissue cephalometric landmarks for reference purposes in the asymmetric group.
The study shows that method C was significantly more accurate than method in the asymmetric/symmetric group.
The results of this study suggest that the inclusion of soft tissue landmarks, especially those around the eye, in an analysis of facial asymmetry provides an effective means of establishing an appropriate facial midline in 3D CBCT image reorientations.
REFERENCES
- 1.Rhodes G. The evolutionary psychology of facial beauty. Ann Rev Psychol. 2006;57:199–226. doi: 10.1146/annurev.psych.57.102904.190208. [DOI] [PubMed] [Google Scholar]
- 2.Peck S, Kataja M. Skeletal asymmetry in esthetically pleasing faces. Angle Orthod. 1991;61:43–48. doi: 10.1043/0003-3219(1991)061<0043:SAIEPF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Grayson B, Cutting C, Bookstein FL, Kim H, McCarthy JG. The three-dimensional cephalogram: theory, technique, and clinical application. Am J Orthod Dentofacial Orthop. 1988;94:327–337. doi: 10.1016/0889-5406(88)90058-3. [DOI] [PubMed] [Google Scholar]
- 4.Grummons DC, Kappeyne van de Coppello MA. A frontal asymmetry analysis. J Clin Orthod. 1987;21:448–465. [PubMed] [Google Scholar]
- 5.Vogel C. Correction of frontal dimensions from head x-rays. Angle Orthod. 1967;37:1–8. doi: 10.1043/0003-3219(1967)037<0001:COFDFH>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Hatcher DC. Science and Practice of Occlusion. Chicago, IL: Quintessence Publishing; 1997. pp. 349–364. [Google Scholar]
- 7.Trpkova B, Prasad NG, Lam EW, Raboud D, Glover KE, Major PW. Assessment of facial asymmetries from posteroanterior cephalograms: validity of reference lines. Am J Orthod Dentofacial Orthop. 2003;123:512–520. doi: 10.1067/mod.2003.S0889540602570347. [DOI] [PubMed] [Google Scholar]
- 8.Kim TY, Baik JS, Park JY, Chae HS, Huh KH, Choi SC. Determination of midsagittal plane for evaluation of facial asymmetry using three-dimensional computed tomography. Imaging Sci Dent. 2011;41:79–84. doi: 10.5624/isd.2011.41.2.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Proffit WR, Phillips C, Dann C IV. Who seeks surgical-orthodontic treatment. Int J Adult Orthod Orthognath Surg. 1990;5:153–160. [PubMed] [Google Scholar]
- 10.Edler R, Wertheim D, Greenhill D. Comparison of radiographic and photographic measurement of mandibular asymmetry. Am J Orthod Dentofacial Orthop. 2003;123:167–174. doi: 10.1067/mod.2003.16. [DOI] [PubMed] [Google Scholar]
- 11.Kim WS, Lee KH, Hwang HS. Comparison of asymmetric degree between maxillofacial hard and soft tissue in facial asymmetric subjects using three-dimensional computed tomography. Korean J Orthod. 2005;35:163–173. [Google Scholar]
- 12.Masuoka N, Muramatsu A, Ariji Y, Nawa H, Goto S, Ariji E. Discriminative thresholds of cephalometric indexes in the subjective evaluation of facial asymmetry. Am J Orthod Dentofacial Orthop. 2007;131:609–613. doi: 10.1016/j.ajodo.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 13.Broadbent BH. A new x-ray technique and its application to orthodontia. Angle Orthod. 1931;1:45–66. [Google Scholar]
- 14.Masuoka N, Muramatsu A, Ariji Y, Nawa H, Goto S, Ariji E. Can cephalometric indices and subjective evaluation be consistent for facial asymmetry. Angle Orthod. 2005;75:651–655. doi: 10.1043/0003-3219(2005)75[651:CCIASE]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Ahn JS, Hwang HS. Relationship between perception of facial asymmetry and posteroanterior cephalometric measurements. Korean J Orthod. 2001;31:489–498. [Google Scholar]
- 16.Ackerman JL, Proffit WR, Sarver DM, Ackerman MB, Kean MR. Pitch, roll, and yaw: describing the spatial orientation of dentofacial traits. Am J Orthod Dentofacial Orthop. 2007;131:305–310. doi: 10.1016/j.ajodo.2006.05.032. [DOI] [PubMed] [Google Scholar]
- 17.Farkas LG, Cheung G. Facial asymmetry in healthy North American Caucasians. An anthropometrical study. Angle Orthod. 1981;51:70–77. doi: 10.1043/0003-3219(1981)051<0070:FAIHNA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Meyer-Marcotty P, Kochel J, Boehm H, Linz C, Klammert U, Stellzig-Eisenhauer A. Face perception in patients with unilateral cleft lip and palate and patients with severe Class III malocclusion compared to controls. J Craniomaxillofac Surg. 2011;39:158–163. doi: 10.1016/j.jcms.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 19.Severt TR, Proffit WR. The prevalence of facial asymmetry in the dentofacial deformities population at the University of North Carolina. lnt J Adult Orthodon Orthognath Surg. 1997;12:171–176. [PubMed] [Google Scholar]
- 20.Farkas LG. Anthropometry of the Head and Face 2nd ed. New York: Raven Press; 1994. pp. 103–111. [Google Scholar]
- 21.Haraguchi S, Iguchi Y, Takada K. Asymmetry of the face in orthodontic patients. Angle Orthod. 2008;78:421–426. doi: 10.2319/022107-85.1. [DOI] [PubMed] [Google Scholar]
- 22.Ras F, Habets LL, van Ginkel FC, Prahl-Andersen B. Method for quantifying facial asymmetry in three dimensions using stereophotogrammetry. Angle Orthod. 1995;65:233–239. doi: 10.1043/0003-3219(1995)065<0233:MFQFAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]