Abstract
Objective:
To determine the influence of two adhesion boosters on shear bond strength and on the bond failure location of indirectly bonded brackets.
Materials and Methods:
Sixty bovine incisors were randomly divided into three groups (n = 20), and their buccal faces were etched using 37% phosphoric acid. In group 1 (control), brackets were indirectly bonded using only Sondhi adhesive. In groups 2 and 3, the adhesion boosters Enhance Adhesion Booster and Assure Universal Bonding Resin, respectively, were applied before bonding with Sondhi. Maximum bond strength was measured with a universal testing machine, and the location of bond failure was evaluated using the Adhesive Remnant Index (ARI). One-way analysis of variance followed by the Tukey test (P < .05) was used to compare the shear bond strength among groups, and the differences in ARI scores were evaluated using the Kruskal-Wallis test (P < .05). The Pearson correlation coefficient was calculated to determine whether there was any correlation between bond strength and ARI scores.
Results:
The mean shear bond strength in group 3 was significantly higher (P < .01) than in the other groups. Evaluation of the locations of bond failure revealed differences (P < .05) among the three groups. There was a moderate correlation between bond strength and ARI scores within group 3 (r = 0.5860, P < .01).
Conclusion:
In vitro shear bond strength was acceptable in all groups. The use of the Assure adhesion booster significantly increased both the shear bond strength of indirectly bonded brackets and the amount of adhesive that remained on the enamel after bracket debonding.
Keywords: Adhesion booster, Indirect bonding, Bracket
INTRODUCTION
Indirect bracket bonding is a process with two stages: the positioning of brackets in the working cast and their transfer to the patient's mouth using trays.1 Most current protocols for indirect bonding are based on the method introduced by Thomas.2 In this technique, brackets with a composite custom base are bonded to the teeth using a chemically cured adhesive, so that one part of the adhesive is applied to the custom base and the other is applied to the previously conditioned enamel.2 Over the years, this technique has been refined, and new variations have been described3–6; however, the basic process remains the same.
During recent decades, great progress in the development of orthodontic adhesives has ensured that orthodontists successfully bond brackets to teeth surfaces.7 However, some studies have shown that about 2% to 6% of indirectly bonded brackets still fail for different reasons.8–10
Bracket debonding during orthodontic treatment is a substantial problem for orthodontists. Its consequences include increased treatment time, additional material and personnel costs, and extra patient visits.11 Additionally, some techniques pose greater problems. In lingual orthodontics, for example, indirect bonding is mandatory because of anatomic variations of bonding surfaces and the difficulty in obtaining a direct view. Therefore, single-tooth trays have to be used in the case of bracket rebonding, and there is the consequent risk of imprecision in repositioning and longer clinical treatment than in the case of direct rebonding.
According to some authors, the interface between the custom base and the adhesive is weak when the Thomas technique is used.6,12 Linn et al.13 conducted an in vitro evaluation of indirect bracket bonding and found little or no adhesive on the enamel surface after bracket debonding, which suggests that bonding failures occurred mainly in the region between the enamel and the custom base. To improve the adhesion of indirectly bonded brackets using the Thomas technique, the use of adhesion boosters has been suggested.6,14–16
Adhesion boosters were developed to reduce bonding failures. They incorporate hydrophilic monomers and other adhesion enhancers into the primer.17 The addition of hydrophilic monomers to adhesive systems facilitates resin infiltration into the etched enamel; this reduces interfacial porosity and adhesive defects, resulting in better bond strength after polymerization.18
Bracket bonding failures and some clinical conditions require higher bond strength, as in the case of bonding premolars and molars, hypocalcified teeth, or teeth with fluorosis or when working with uncooperative patients.19 Hence, there should be options for achieving greater adhesion between the orthodontic device and the tooth. The effects of adhesion boosters on direct bracket bonding11,17,18,20,21 have been evaluated, and the results have been varied. However, no studies have evaluated the effect of adhesion boosters on indirect bracket bonding. This study determined the effect of two adhesion boosters, Enhance Adhesion Booster and Assure Universal Bonding Resin, on shear bond strength and the location of bond failure in indirect bracket bonding.
MATERIALS AND METHODS
Sixty bovine mandibular incisors, free of caries, wear, fracture, or any other visible defects, were selected and stored in distilled water until the beginning of the experiment. To prepare the specimens, the roots were cut and a hole was made on the palatal surface of each tooth using a high-speed diamond round bur to facilitate pulp removal with a curette. The crowns were placed in plastic cylinders using chemically cured resin, so that the buccal faces were above the acrylic mount and parallel to its base. Two V-shaped grooves were made on opposite sides of the upper margin of each cylinder to ensure the correct positioning of the transfer trays in the specimens in a later phase of the study.6
Impressions of the specimens were taken using condensation silicone (Zetaplus, Zhermack SpA, Badia Polesine, RO, Italy), and type IV dental plaster (Durone, Dentsply Ind and Com, Rio de Janeiro, Brazil) was poured. The plaster models dried for 24 hours. A layer of insulation agent, diluted in water in a 1∶1 ratio, was applied to the models, and 20 minutes were allowed for drying. Next, the bases of mandibular central incisor metal brackets (Kirium, Abzil-3M Unitek, Sao Paulo, Brazil) were sandblasted using 50-µm aluminum oxide for 1 second and a compressed air jet. A small amount of Transbond XT resin (3M Unitek, Monrovia, Calif) was applied to the metal mesh of the brackets, which were then placed on the center of the buccal faces of the teeth. A 453.59-g load was applied to the center of each bracket using a Gilmore needle to standardize the amount of resin. Excess material was removed with a scaler (Figure 1a). The brackets were then light-cured for 40 seconds (10 seconds per side) at a distance of 2 to 3 mm with a light-emitting diode lamp and at a light intensity of 1100 mW/cm2.
Figure 1.
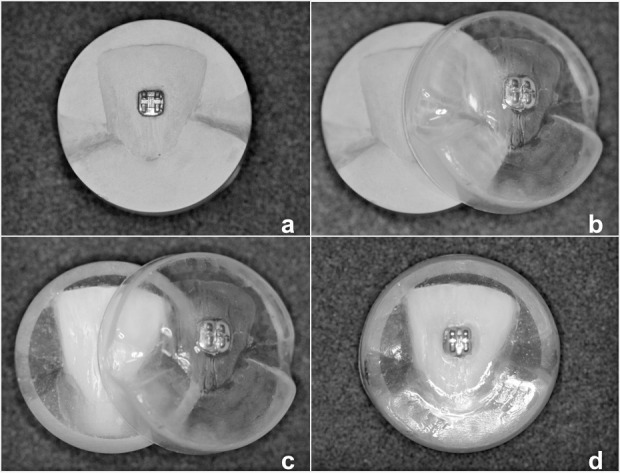
Indirect bonding procedure. (a) Bracket placement on the plaster model. (b) Transfer tray removal. (c) Bracket in transfer tray and bovine tooth. (d) Transfer tray positioned in the tooth.
The transfer trays were made with 1-mm thick flexible thermoplastic resin (FGM Dental Products, Joinville, SC, Brazil) in a vacuum-forming machine, cut at a point 3 mm below the upper margin of the models, and immersed in water for 30 minutes. The trays were then carefully removed from the models (Figure 1b), and the custom resin bases were photopolymerized for 20 seconds. After that, the custom bases were sandblasted with 50-µm aluminum oxide for 1 second and oil-free compressed air to remove possible residues of insulation agent, plaster, or any other contaminant.
All teeth were cleaned with a rubber cup and pumice stone, rinsed with water for 10 seconds, and dried with oil-free compressed air. Immediately after this, the enamel was conditioned with 37% phosphoric acid (Email Preparator Blue, Ivoclar-Vivadent AG, Schaan, Liechtenstein) for 30 seconds, rinsed with water for 20 seconds, and dried with oil-free compressed air until the enamel acquired a white appearance.
The specimens were randomly divided into three equal groups (n = 20), and a different bonding protocol was used for each group.
Group 1 (control): Brackets were bonded indirectly using the adhesive Sondhi Rapid Set (3M Unitek, Monrovia, Calif) according to the manufacturer's instructions. The transfer trays were positioned in the teeth (Figure 1c,d), slightly pressed for 30 seconds, and removed after 2 minutes.
Group 2: Two layers of the chemically activated booster Enhance Adhesion Booster (Reliance Orthodontic Products Inc, Itasca, Ill) were applied to the enamel, and one layer was applied to the custom base, followed by a brief application of compressed air. After 60 seconds, the brackets were bonded using the Sondhi adhesive, as in the control group.
Group 3: Two layers of the booster Assure Universal Bonding Resin (Reliance Orthodontic Products Inc, Itasca, Ill) were applied to the enamel, and one layer was applied to the custom base, followed by a brief application of compressed air. Sixty seconds later, the brackets were bonded using the Sondhi adhesive in the same way as in the control group.
Immediately after bonding, the teeth were stored in distilled water at room temperature for 24 hours; next, thermocycling was performed for 500 cycles at 5°C and 55°C. After this, the specimens underwent shear bond strength tests. A mechanical testing machine (Kratos, Industrial Equipment, Cotia, SP, Brazil) with a 1-kN load and at a speed of 0.5 mm/min was used to determine the maximum shear strength required to debond the brackets. The specimens were placed in the machine so that the chisel was as close as possible to the tooth/bracket base interface, allowing the force to be applied parallel to the bracket base (Figure 2). The force was recorded in Newtons for each specimen and divided by the area of the bracket base to estimate the shear bond strength in megapascals (MPa).
Figure 2.

Specimen orientation in the universal testing machine.
After bracket debonding, the buccal surfaces of each tooth were examined using an optical stereomicroscope, and the Adhesive Remnant Index (ARI) was applied to determine the location of bond failure. The ARI scores were: 0 = no adhesive on the tooth surface; 1 = less than 50% of the adhesive is left on the tooth; 2 = more than 50% of adhesive is left on the tooth; 3 = 100% of the adhesive is left on the tooth.22
Mean shear bond strengths, standard deviations (SDs), and minimum and maximum values were calculated for each group. The data regarding bond strength were evaluated with the Shapiro-Wilk method to verify their normality. One-way analysis of variance and the Tukey post hoc test were employed to detect possible differences in shear bond strength between groups. The nonparametric Kruskal-Wallis test was used to detect differences between ARI scores. A Pearson correlation coefficient was calculated to determine whether there was any correlation between bond strength and the ARI scores. The level of significance was set at 5%.
RESULTS
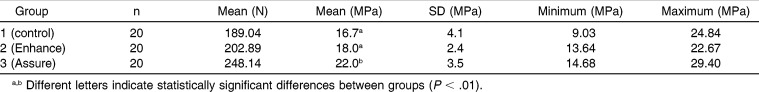
The results of shear bond strength tests are shown in Table 1. The mean shear bond strength value in group 3 was significantly greater (P < .01) than those of the other groups, which were similar to each other.
Table 1.
Mean Shear Bond Strengths and SDs by Group
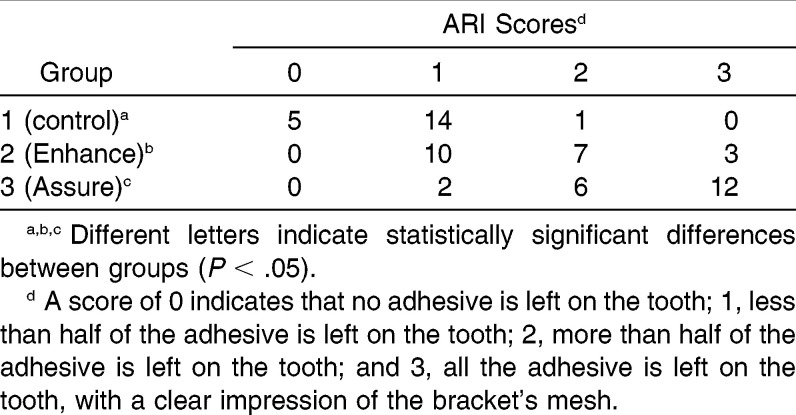
Table 2 shows the ARI scores for each group. There were differences in the ARI scores of the three groups, and group 3 had the most specimens with a score of 3 (P < .05).
Table 2.
Scores for ARI by Group
Neither group 1 nor group 2 showed any correlation between bond strength and ARI scores. The Pearson correlation coefficient showed a moderate positive correlation between bond strength and ARI scores within group 3 (r = 0.5860, P < .01).
DISCUSSION
Several recent studies have investigated the effect of adhesion boosters on direct bracket bonding and rebonding.7,11,17,18,21,23,24 Results have varied; some studies found an increase in shear bond strength of new24 or rebonded7 brackets, others found acceptable levels of bond strength of brackets bonded under saliva contamination,21 and still others found no differences.11,17,18 However, the effects of these products on indirect bracket bonding have not been studied. Therefore, this study evaluated the effect of two adhesion boosters on shear bond strength and the location of bond failure in indirect bracket bonding.
Previous studies showed that bovine and human enamel are similar in physical properties, composition, and bond strength.25,26 Additionally, bovine enamel has been shown to be a reliable substitute for human enamel in adhesion studies.26,27 Therefore, our study used bovine incisors because of their similarity to human enamel, in addition to their availability and their low cost.
Some authors have suggested that bond strengths of 5.9 to 9.7 MPa are appropriate for clinical treatments28,29; however, the minimum in vitro bond strength required for reliable orthodontic bonding remains unknown. The mean bond strength obtained in vitro in the three groups in this study ranged from 16.7 to 22.0 MPa, values that would be appropriate for orthodontic treatment according to several authors.28,29
Mean shear bond strength in group 2 (Enhance) was slightly greater than mean bond strength in the control group, but the difference was not statistically significant. Egan et al.23 used human premolars to evaluate the efficacy of the Enhance Adhesion Booster when used together with a conditioner that contained methyl methacrylate (Plastic Conditioner, Reliance Products Inc) for direct bracket bonding. They concluded that the use of those products did not increase the bond strength of rebonded brackets.
When the Assure adhesion booster was used (group 3), there was a significant increase (P < .01) in shear bond strength in comparison with the control group (group 1) and the group that received Enhance (group 2). Some studies20,21 evaluated the effect of this booster on direct bracket bonding in cases of saliva or blood contamination and found that Assure produced adequate bond strength under dry and humid conditions. In this sense, the results of our study indicate that the adhesion booster Assure is capable of increasing the shear bond strength of brackets bonded indirectly using the Thomas technique.
The analysis of ARI scores revealed significant differences between the three groups (P < .05). In the control group, most test specimens had scores of 1 (70%) or 0 (25%), which indicated that little adhesive material was left on the enamel after bracket debonding. This result is in agreement with the findings of Linn et al.,13 who found that 75% of specimens that were indirectly bonded using the Sondhi adhesive had an ARI of 1 and that the other 25% had an ARI of 0. In groups 2 and 3, no test specimens had a score of 0, and most had a score of 1 (50%) or 2 (35%) and 2 (30%) or 3 (60%), respectively. Therefore, there was more adhesive residue on the enamel when adhesion boosters were used, particularly when Assure was applied. This may indicate that there was a bond strength increase at the enamel-adhesive interface, which made it stronger than the adhesive-bracket interface.
The Pearson correlation coefficient showed a moderate correlation between bond strength and ARI scores within group 3. Previous studies12,13 found no strong correlation between bond strength and amount of adhesive remnant. However, because of differences in bonding protocols, one must be careful about drawing conclusions on the basis of comparisons of the studies.
Although manufacturers claim that both adhesive boosters evaluated in this study can adequately improve adhesion for indirect bracket bonding with the Thomas technique,15 the differences in shear bond strength, as well as in ARI on enamel, may be attributed to differences in their chemical composition.24,30 O'Brien et al.30 found that the location of bonding failure is affected by the type of adhesive material used. Enhance Adhesion Booster contains biphenyl dimethacrylate and Na-N-tolyglycine glycidyl methacrylate; according to the manufacturer, this material increases the adhesion of chemically cured, light-cured, or dual-cured systems applied to different surfaces, such as enamel and resin. In contrast, Assure Universal Bonding Resin is a hydrophilic primer composed of biphenyl dimethacrylate and hydroxyethyl methacrylate, which is indicated to increase adhesion to enamel, dentin, metal, and resin surfaces.
The results of this study suggest that when the orthodontist needs greater bond strength for indirect bracket bonding, the adhesion booster Assure Universal Bonding Resin may be used. However, several factors may affect bracket bonding in patients. These factors are difficult to reproduce in the laboratory, and this in vitro study therefore cannot be understood as a comprehensive representation of clinical cases. In the oral cavity, bonded brackets are exposed to variations in humidity and temperature. These variables may lead to stress on the adhesive and on the brackets, which may affect bond strength.31 Therefore, thermocycling was used to produce a better simulation of the intraoral conditions. In this study, we used single-tooth trays. Indirect bonding performed in vivo usually uses full-arch trays, which causes a decrease in the bond strength because of the placement of thicker adhesive and the movement of the tray during initial setting of the adhesive.16 Moreover, the testing machine measured only the shear bond strength necessary to debond brackets, whereas in the oral cavity, a combination of forces (shearing, traction, and torsion) may be present. Furthermore, the load in this in vitro study was static and increased constantly, whereas in vivo forces arise abruptly and fluctuate or are cyclical (dynamic). Consequently, shear bond strength in vitro may be greater than that found in vivo.24 Despite these limitations, in vitro studies are necessary because they provide guidelines for the selection of optimal adhesive procedures.
CONCLUSIONS
In vitro shear bond strength was acceptable in all groups.
The use of the adhesion booster Assure Universal Bonding Resin significantly increased both the bond strength in indirect bracket bonding and the amount of adhesive material that remained on enamel after bracket debonding.
REFERENCES
- 1.Miles PG, Weyant RJ. A comparison of two indirect bonding adhesives. Angle Orthod. 2005;75:1019–1023. doi: 10.1043/0003-3219(2005)75[1019:ACOTIB]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Thomas RG. Indirect bonding, simplicity in action. J Clin Orthod. 1979;13:93–105. [PubMed] [Google Scholar]
- 3.Hickham JH. Predictable indirect bonding. J Clin Orthod. 1993;27:215–217. [PubMed] [Google Scholar]
- 4.Miles PG. Indirect bonding with a flowable light-cured adhesive. J Clin Orthod. 2002;36:646–647. [PubMed] [Google Scholar]
- 5.Sondhi A. Efficient and effective indirect bonding. Am J Orthod Dentofacial Orthop. 1999;115:352–359. doi: 10.1016/s0889-5406(99)70252-0. [DOI] [PubMed] [Google Scholar]
- 6.Thompson MA, Drummond JL, BeGole EA. Bond strength analysis of custom base variables in indirect bonding techniques. Am J Orthod Dentofacial Orthop. 2008;133:9.e15–20. doi: 10.1016/j.ajodo.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 7.Chung CH, Fadem BW, Levitt HL, Mante FK. Effects of two adhesion boosters on the shear bond strength of new and rebonded orthodontic brackets. Am J Orthod Dentofacial Orthop. 2000;118:295–299. doi: 10.1067/mod.2000.104810. [DOI] [PubMed] [Google Scholar]
- 8.Thiyagarajah S, Spary DJ, Rock WP. A clinical comparison of bracket bond failures in association with direct and indirect bonding. J Orthod. 2006;33:198–204. doi: 10.1179/146531205225021615. [DOI] [PubMed] [Google Scholar]
- 9.Deahl ST, Salome N, Hatch JP, Rugh JD. Practice-based comparison of direct and indirect bonding. Am J Orthod Dentofacial Orthop. 2007;132:738–742. doi: 10.1016/j.ajodo.2006.01.037. [DOI] [PubMed] [Google Scholar]
- 10.Miles PG, Weyant RJ. A clinical comparison of two chemically-cured adhesives used for indirect bonding. J Orthod. 2003;30:331–336. doi: 10.1093/ortho/30.4.331. [DOI] [PubMed] [Google Scholar]
- 11.Vicente A, Bravo LA, Romero M, Ortíz AJ, Canteras M. Bond strength of brackets bonded with an adhesion promoter. Br Dent J. 2004;196:482–485. doi: 10.1038/sj.bdj.4811178. [DOI] [PubMed] [Google Scholar]
- 12.Yi GK, Dunn WJ, Taloumis LJ. Shear bond strength comparison between direct and indirect bonded orthodontic brackets. Am J Orthod Dentofacial Orthop. 2003;124:577–581. doi: 10.1016/s0889-5406(03)00503-1. [DOI] [PubMed] [Google Scholar]
- 13.Linn BJ, Berzins DW, Dhuru VB, Bradley TG. A comparison of bond strength between direct and indirect bonding methods. Angle Orthod. 2006;76:289–294. doi: 10.1043/0003-3219(2006)076[0289:ACOBSB]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Klocke A, Shi J, Kahl-Nieke B, Bismayer U. Bond strength with custom base indirect bonding techniques. Angle Orthod. 2003;73:176–180. doi: 10.1043/0003-3219(2003)73<176:BSWCBI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Indirect bonding technique – custom base. Itasca, IL: Reliance Orthodontic Products Inc; at website: www.relianceorthodontics.com/store/files/instructions/CustomBaseOutline041509.pdf. [Google Scholar]
- 16.Polat O, Karaman AI, Buyukyilmaz T. In vitro evaluation of shear bond strengths and in vivo analysis of bond survival of indirect-bonding resins. Angle Orthod. 2004;74:405–409. doi: 10.1043/0003-3219(2004)074<0405:IVEOSB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Wenger NA, Deacon S, Harradine NW. A randomized control clinical trial investigating orthodontic bond failure rates when using Orthosolo universal bond enhancer compared to a conventional bonding primer. J Orthod. 2008;35:27–32. doi: 10.1179/146531207225022392. [DOI] [PubMed] [Google Scholar]
- 18.Vicente A, Bravo LA, Romero M, Ortíz AJ, Canteras M. Effects of 3 adhesion promoters on the shear bond strength of orthodontic brackets: an in-vitro study. Am J Orthod Dentofacial Orthop. 2006;129:390–395. doi: 10.1016/j.ajodo.2004.08.022. [DOI] [PubMed] [Google Scholar]
- 19.Newman GV, Newman RA, Sun BI, Jack Ha JL, Ozsoylu SA. Adhesion promoters, their effect on the bond strength of metal brackets. Am J Orthod Dentofacial Orthop. 1995;108:237–241. doi: 10.1016/s0889-5406(95)70015-3. [DOI] [PubMed] [Google Scholar]
- 20.Nemeth BR, Wiltshire WA, Lavelle CL. Shear/peel bond strength of orthodontic attachments to moist and dry enamel. Am J Orthod Dentofacial Orthop. 2006;129:396–401. doi: 10.1016/j.ajodo.2004.12.017. [DOI] [PubMed] [Google Scholar]
- 21.Schaneveldt S, Foley TF. Bond strength comparison of moisture-insensitive primers. Am J Orthod Dentofacial Orthop. 2002;122:267–273. doi: 10.1067/mod.2002.126594. [DOI] [PubMed] [Google Scholar]
- 22.Artun J, Bergland S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am J Orthod. 1984;85:333–340. doi: 10.1016/0002-9416(84)90190-8. [DOI] [PubMed] [Google Scholar]
- 23.Egan FR, Alexander SA, Cartwright GE. Bond strength of rebonded orthodontic brackets. Am J Orthod Dentofacial Orthop. 1996;109:64–70. doi: 10.1016/s0889-5406(96)70164-6. [DOI] [PubMed] [Google Scholar]
- 24.Vijayakumar A, Venkateswaran S, Krishnaswamy NR. Effects of three adhesion boosters on the shear bond strength of new and rebonded brackets—an in vitro study. World J Orthod. 2010;11:123–128. [PubMed] [Google Scholar]
- 25.Nakamichi I, Iwaku M, Fusayama T. Bovine teeth as possible substitutes in adhesion test. J Dent Res. 1983;62:1076–1081. doi: 10.1177/00220345830620101501. [DOI] [PubMed] [Google Scholar]
- 26.Oesterle LJ, Shellhart WC, Belanger GK. The use of bovine enamel in bonding studies. Am J Orthod Dentofacial Orthop. 1998;114:514–519. doi: 10.1016/s0889-5406(98)70171-4. [DOI] [PubMed] [Google Scholar]
- 27.Saleh F, Taymour N. Validity of using bovine teeth as a substitute for human counterparts in adhesive tests. East Mediterr Health J. 2003;9:201–207. [PubMed] [Google Scholar]
- 28.Greenlaw R, Way DC, Galil KA. An in vitro evaluation of a visible light-cured resin as an alternative to conventional resin bonding systems. Am J Orthod Dentofacial Orthop. 1989;96:214–220. doi: 10.1016/0889-5406(89)90458-7. [DOI] [PubMed] [Google Scholar]
- 29.Reynolds IR. A review of direct orthodontic bonding. Br J Orthod. 1975;2:171–178. [Google Scholar]
- 30.O'Brien KD, Watts DC, Read MJ. Residual debris and bond strength—is there a relationship. Am J Orthod Dentofacial Orthop. 1988;94:222–230. doi: 10.1016/0889-5406(88)90031-5. [DOI] [PubMed] [Google Scholar]
- 31.Brauchli L, Zeller M, Wichelhaus A. Shear bond strengths of seven self-etching primers after thermo-cycling. J Orofac Orthop. 2011;72:371–380. doi: 10.1007/s00056-011-0041-4. [DOI] [PubMed] [Google Scholar]