Abstract
Objective:
To assess the volumetric changes and the maxillary response of the naso-maxillary complex (NMC) following rapid maxillary expansion (RME).
Materials and Methods:
Thirty consecutive patients (14 males and 16 females) with a mean age at first observation of 9.5 ± 1.8 years for males and of 11.8 ± 1.7 years for females, presenting a posterior unilateral or bilateral crossbite and requiring RME, were selected for the study. Each patient underwent expansion to correct the transverse occlusal relationships. Computed tomography scans were taken before RME (T1) and at the end of the active expansion phase (T2). Measurements were performed on scanned images. The Kolmogorov-Smirnov test was performed; the mean differences between measurements at T1 and T2 were compared using the t-test (α = .05).
Results:
All volumetric, maxillary, transverse skeletal anterior and posterior variables as well as all dental anterior and posterior linear and angular variables representing the NMC displayed statistically highly significant increases after RME (P < .001).
Conclusions:
After RME the total volume of the NMC increased by 12%, the nasal volume by 17%, and the maxillary volume by 10.6%. The maxillary and the nasal contributions represented 69.75% and 30.25%, respectively.
Keywords: Rapid maxillary expansion, Computed tomography, Transverse dimension, Naso-maxillary complex
INTRODUCTION
Transverse maxillary deficiency is generally concomitant with the presence of posterior crossbite, arch form deformation, dental crowding, and narrowing of the nasal cavity.1,2 The correction of this deformity can be done in growing patients with rapid maxillary expansion (RME) through midpalate suture opening using a Hyrax expanding device. The effects of this appliance have been demonstrated3,4 to be dental based on increasing interdental distances and teeth axial inclination and skeletal based on enlargement of the maxillary base, widening of the nasal cavity, and increasing of maxillary sinus volume (MSV).
The RME effects have been noted in such neighboring structures as the internasal, naso-maxillary, and fronto-maxillary sutures5 and even the spheno-occipital synchondrosis in youngsters.6 Disarticulating these sutures will lead to anatomical changes in the nasal cavity with an increase in the nasal volume,7–12 which decreases the nasal airway resistance, establishes predominant nasal respiration, and improves the nasal airway ventilation.13,14 This procedure has also been proved to offer an effective method for treating children with obstructive sleep apnea syndrome.15
The study of the treatment effects of RME has been carried out on dental casts, lateral and posteroanterior cephalograms, and by finite element methods. Using a two-dimensional (2D) cephalometric radiograph to evaluate a three-dimensional (3D) object has been proven to have some limitations as a result of projection problems, landmark identification, measurement errors, and superimposition of different structures.16,17
Advances in technology have led to changes in the method of evaluating RME treatment effects, progressing from 2D to 3D and from linear and angular to volumetric approaches. The use of computed tomography (CT) and, later, cone beam CT has been of great interest and help to clinicians attempting to acquire 3D images and reconstructions of objects in order to be able to apply 3D and volumetric measurements.3,4,18–22
The objectives of this study were (1) to assess the volumetric changes of the naso-maxillary complex (NMC) following RME, (2) to quantify maxillary and nasal contributions to these changes, and (3) to identify maxillary response.
MATERIALS AND METHODS
This project was conducted in coherence with the Helsinki Agreement for research on humans, and the study design was approved by the Institutional Review Board and Independent Ethics Committee of the School of Dentistry, Lebanese University, Beirut, Lebanon. Signed informed consent forms were obtained for all participants in the study.
Subject Selection
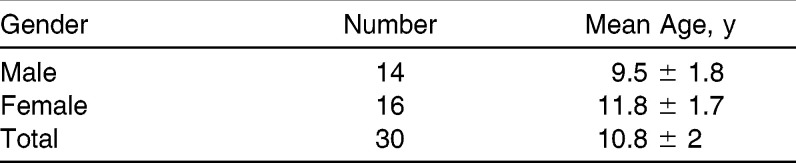
Thirty consecutive healthy subjects (mean age at first observation of 9.5 ± 1.8 years for males and 11.8 ± 1.7 years for females) presenting with unilateral or bilateral posterior crossbite and requiring a RME procedure as a part of their comprehensive orthodontic treatment were selected for this study. The gender and age distributions of the selected subjects are shown in Table 1.
Table 1.
Gender and Age Distribution of the Selected Group
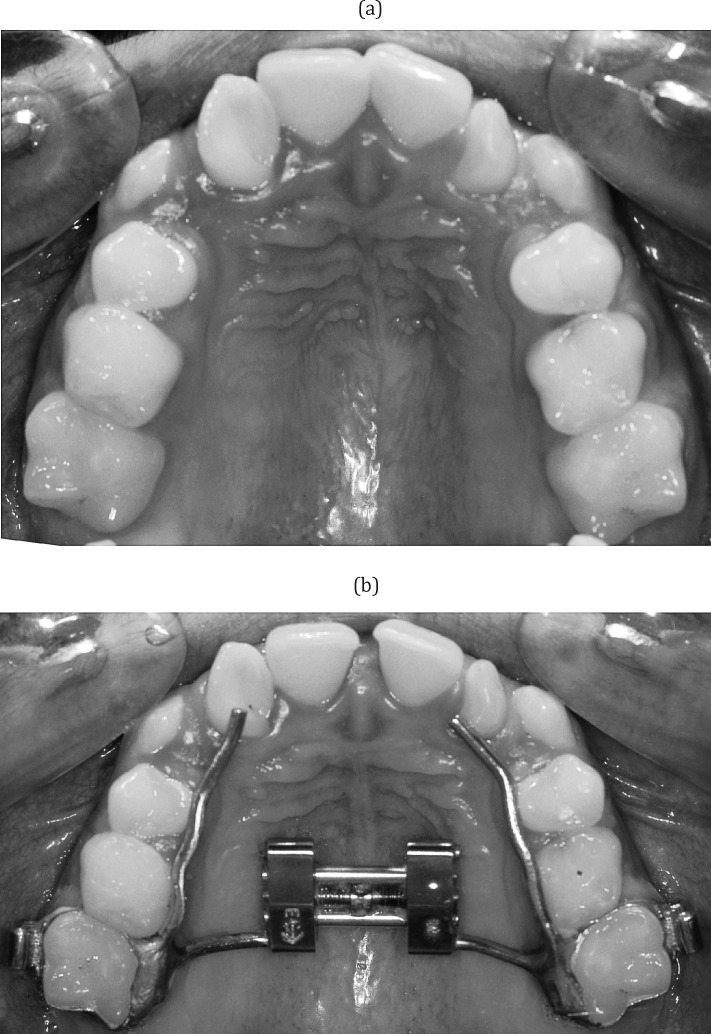
Therapeutic Procedure
A pretreatment CT image (T1) was taken as part of the initial orthodontic records for all patients. The subjects received a traditional tooth-borne Hyrax-type maxillary expander with bands cemented on the first permanent molars, as shown in Figure 1. The expansion screw was activated twice a day (0.25 mm per turn, 0.5 mm daily) until posterior dental crossbite overcorrection was achieved. At the end of the active phase, another CT image (T2) was acquired on the day the appliance was tied off, and the screw was kept in place for an additional 6 months. Neither brackets nor wires were used until the CT images were taken at T2.
Figure 1.
Hyrax-type expansion appliance used in the study before (a) and after (b) suture opening.
Radiographic Examination
All radiographic examinations were performed by the same trained technician at the same scanner console supported with a Denta-scan reconstruction program that was used to study the maxillofacial region (Prospeed, General Electric Medical Systems, Milwaukee, Wis). This machine is equipped with one detector row and has a minimal rotation time of 1 second, given a collimation of 1 mm. Subsequent scans were taken with a 1-mm slice thickness, 1-mm interval, at 100 mAs, with a 13.7-cm field of view, a 512 × 512 matrix, and a 0° gantry angle, and at 120 KV.
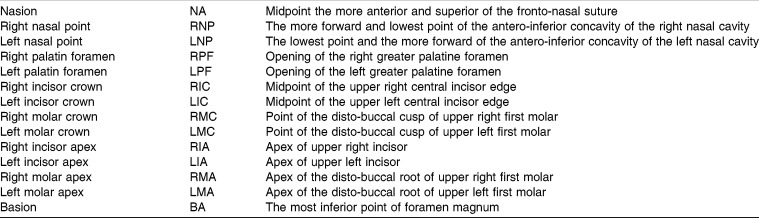
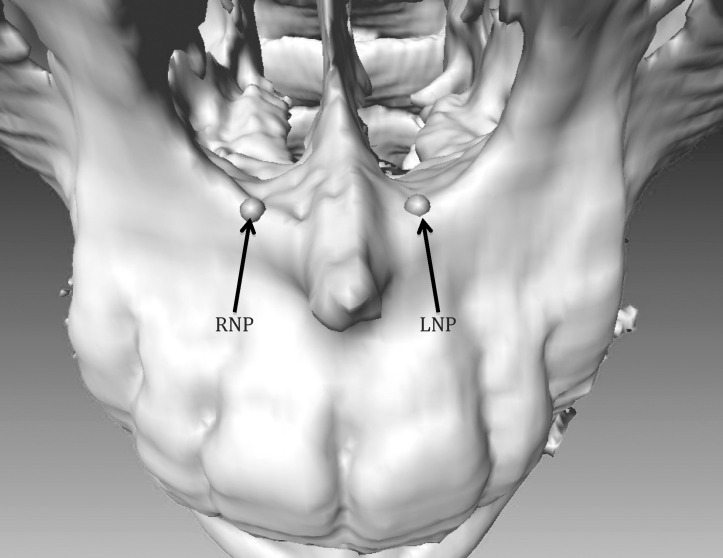
Software Manipulation
All DICOM-formatted images were rendered into volumetric images using AMIRA software (Mercury Computer Systems, Berlin, Germany). 3D reconstructions were done as well as sagittal, axial, and coronal volumetric slices with a threshold set at 200 and a “Data Window” of a minimum at −400 and a maximum at 4000, and they were used to position all landmarks. These landmarks are presented in Table 2 and shown in Figures 2 and 3. The same examiner located the landmarks for all patients.
Table 2.
Definition of Landmarks
Figure 2.
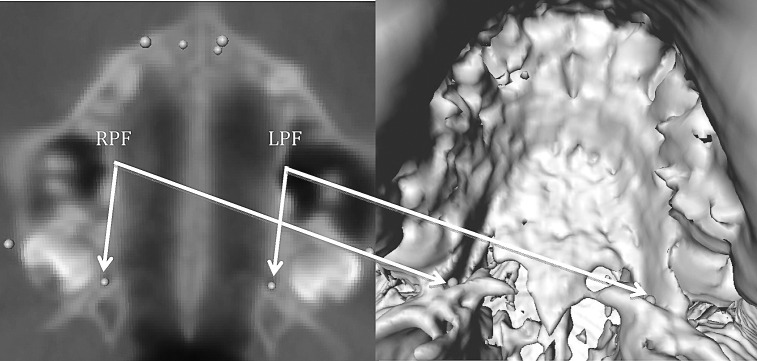
Landmark localization of points RNP and LNP on 3D reconstruction.
Figure 3.
Landmark localization of points RPF and LPF on 3D reconstruction and on volumetric slices.
A geometric model was constructed from these landmarks, consisting of two parts, as shown in Figures 4 and 5; the nasal volume B delimited on the top by Nasion point with a base formed by nasal and palatin foramen points right and left inferiorly, and the maxillary volume C, which is limited by the base of volume B, superiorly and incisor and molar crown points right and left inferiorly. The total volume A is the sum of B and C. A software was designed to calculate distances, angles, and volumes required using the 3D coordinates x, y, and z of different landmarks obtained from the AMIRA software.
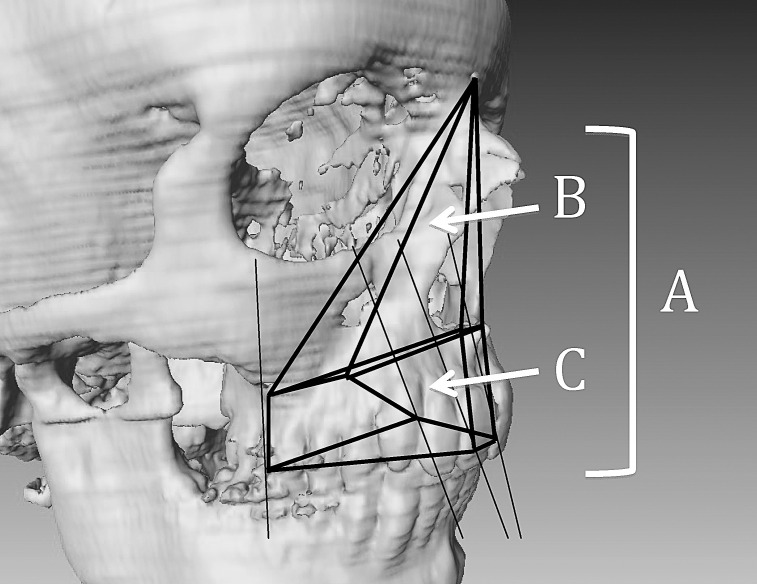
Figure 4.
Structured representation of the naso-maxillary complex: B is the nasal volume and C the maxillary volume. The total volume A is the sum of B and C.
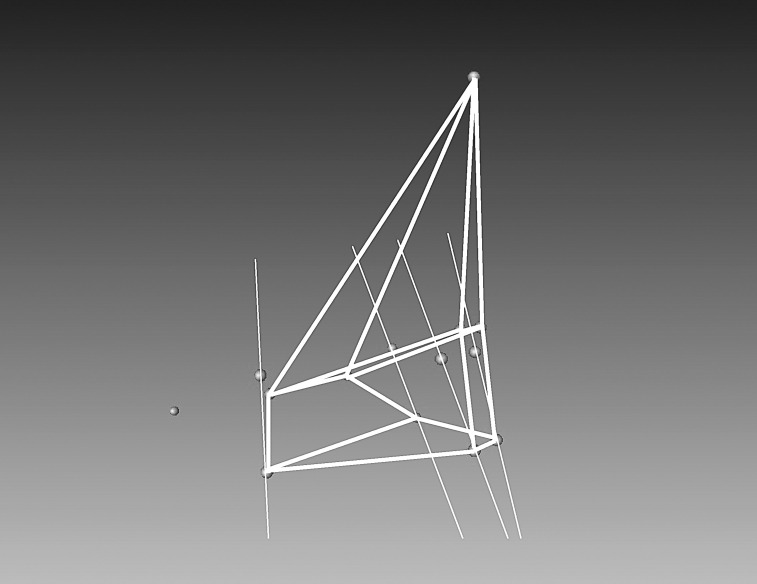
Figure 5.
Schematic representation of the naso-maxillary complex by joining different landmarks.
Statistical Analysis
To test the intraexaminer reliability, 10 patients were randomly selected and the same examiner remeasured their images after 2 weeks. The difference between the duplicate measurements was analyzed using the Pearson correlation coefficient; their means were 0.873 for the linear measurements, 0.792 for the angular measurements, and 0.935 for the volumetric measurements.
Descriptive statistics, including means, standard deviations, and ranges, were calculated for all measurements before and after treatment. The Student's paired t-test was used with the significance level set at 5% in order to assess if there were any significant differences among the matched pairs between means of all variables. The Kolmogorov-Smirnov test was used to verify the normality of the variables.
Statistical analysis was carried out with SAS software (version 9.1, SAS Institute, Cary, NC), with a significance level of .05.
RESULTS
All measurement error coefficients for intraexaminer reproducibility for repeated linear, angular, and volumetric measures presented positive correlations and were found to be within acceptable limits, ranging between 0.792 and 0.935. The Kolmogorov-Smirnov test confirmed the normal distribution; the values of all linear, angular, and volumetric variables analyzed had no significant differences, giving a P > .005.
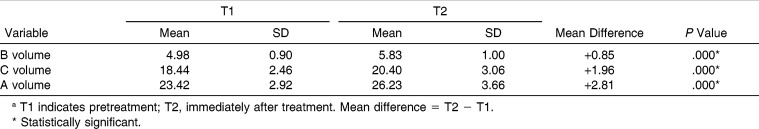
Volumetric Changes of the NMC Following RME
All volumetric variables representing the NMC displayed statistically high significant increases after RME (P < .001), as shown in Table 3. The total volume (A) increased by 2.81 mm3 or 12%; in addition, there were increases in nasal volume (B) of 0.85 mm3 and in the maxillary volume (C) of 1.96 mm3, which are equivalent, respectively, to 17% and 10.6%.
Table 3.
Means, Standard Deviations (SDs), and Mean Differences of Volumetric Variables (mm3)a
The maxillary contribution of 1.96 mm3 represented 69.75% of the total volume increase of 2.81 mm3; on the other hand, the increase of nasal volume by 0.85 mm3 represented an estimated 30.25% of the total increase.
Maxillary Response to RME
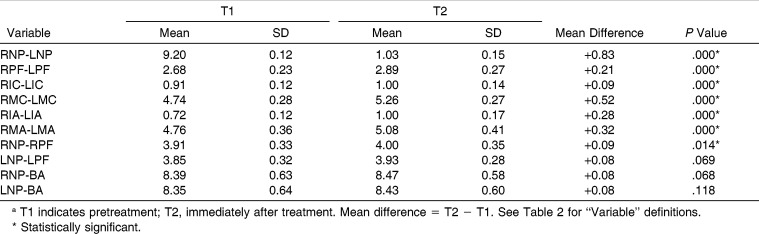
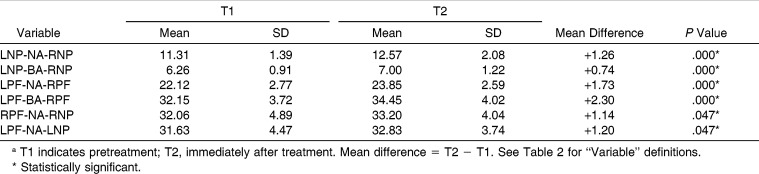
The midpalatal suture was successfully opened in all patients. Maxillary dental and skeletal, linear, and angular variables are represented in Tables 4 and 5.
Table 4.
Means, Standard Deviations (SDs), and Mean Differences of Linear Variables (mm)a
Table 5.
Means, Standard Deviations (SDs), and Mean Differences of Angular Variables (°)a
All maxillary transverse skeletal anterior (RNP-LNP, LNP-NA-RNP, and LNP-BA-RNP) and posterior (RFP-LPF, LPF-NA-RPF, and LPF-BA-RPF) variables, as well as dental anterior (RIC-LIC and RIA-LIA) and posterior (RMC-LMC and RMA-LMA) linear and angular variables, showed statistically high significant increases (P < .001) after RME.
The maxillary sagittal response was statistically different between both sides. The right hemimaxillary skeletal length increased significantly with its two variables, RNP-RPF and RPF-NA-RNF, but only the change in the angular variable LPF-NA-LNP was significant in the left hemimaxilla (P < .005).
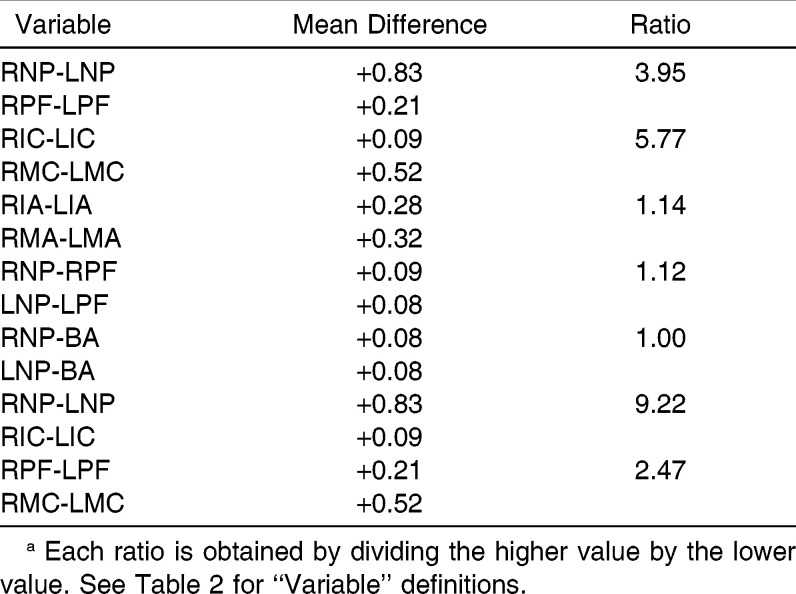
The ratios of linear variables are represented in Table 6. The skeletal expansion was 3.95 times greater on the anterior than on the posterior part of the maxilla (RNP-LNP/RFP-LPF). The dental expansion was 5.77 and 1.14 times greater, respectively, on the crown and the apex of the molars than on the incisors (RMC-LMC/RIC-LIC and RIA-LIA/RMA-LMA). The sagittal skeletal response was almost identical on both sides: RNP-RPF/LNP-LPF was 1.12 and RNP-BA/LNP-BA was equal to 1. The vertical opening of the suture was greater on the dental arch than on the maxillary base in the molar area (RMC-LMC/RPF-LPF = 2.47) and less important in the incisor region (RNP-LNP/RIC-LIC = 9.22).
Table 6.
Ratios of Different Linear Variablesa
DISCUSSION
The objectives of this study were to assess the volumetric changes of the NMC following RME, to quantify maxillary and nasal contributions to these changes, and to identify maxillary response.
Volumetric Changes of the NMC Following RME
The vast majority of research on this topic has been conducted using a 2D evaluation model23–25; only a few studies have been accomplished concerning volumetric evaluation in general26,27 and affecting specifically the NMC after RME.4,7–12,19,21
The results of this study were in accordance with other published results showing a volumetric increase of different components of the nasomaxillary complex. Previous studies tried to demonstrate that RME reduces nasal airway resistance and increases nasal volume. Using 3D simulation and modeling programs, Görgülü et al.11 found a significant nasal volume increase of 12.14%. A significant increase in nasal volume was shown also using acoustic rhinometry;9 Babacan et al.8 estimated this increase to be 13.80% without decongestant and 15.16% with decongestant, while others12 found a significant increase of nasal cavity volume by 15.20% and nasopharynx volume by 16.20%. Palaisa et al.10 concluded that RME is usually accompanied by increases in area and volume of the nasal cavity, and these changes remained stable 3 months after treatment. The nasal volume increase of 17% reported in this study was quite close to values published in previous studies.8–12
Several articles focused on evaluating RME effects on MSV; Pangrazio-Kulbersh et al.4 noticed a significant increase of between 6% and 11%, while others12 didn't find any significant difference in MSV. Maxillary volume modifications following RME have not been evaluated. Different 2D and 3D studies have addressed the dentoalveolar effects and/or the linear maxillary skeletal measurements modifications following RME. We tried to isolate the maxillary skeletal component from its dentoalveolar entity; the maxillary volume, represented by C, increased by 1.96 mm3, which was equivalent to 10.6%.
The total naso-maxillary volume increase was obtained through a maxillary contribution of 69.75% and a nasal contribution of 30.25%. The predominance of the maxillary contribution may be due to the triangular pattern of suture opening with the base at the maxillary anterior part.5
Maxillary Response to RME
The main clinical relevance of dental and skeletal modifications resulting from RME was expressed in the transverse direction and less in the vertical and sagittal dimensions, while dental expansion was greater than skeletal expansion.22,28 Garrett et al.21 showed the influence of the binding effect of the alveolar process on the transverse dimension, which increases from the anterior to the posterior maxilla. Cross and McDonald25 noted an increase in dental and skeletal maxillary widths, and they concluded that there is some evidence that age and maturity of patients will influence the expansion pattern; their sample comprised 25 children with a mean age of 13 years and 4 months. The findings of the later studies were similar to the ones reported in the present observation, with a significant increase of all linear and angular transverse variables (Tables 4 and 5).
An individual variation in the maxillary sagittal response was noticed, which was statistically different between both sides. The increase of the right hemimaxillary skeletal length (RNP-RPF) compared to the left side (LNP-LPF) was statistically significant but was considered to be clinically irrelevant (Table 4). This difference in response to RME, advocated by Oliveira et al.18 and Podesser et al.,20 could constitute a normal result to the individual variations existing among our patients.
Chung and Font24 found that the mean increases of maxillary interpremolar width, maxillary intermolar width, maxillary width, nasal width, and interorbital width were, respectively, 110.7%, 104.5%, 30.1%, 23.1%, and 3.3% of the screw expansion. These data support the triangular pattern of vertical suture opening, which decreases in magnitude from dental arch to basal bone.19 These findings are interpreted in our study by the magnitude of increase on the dental arch more than on the maxillary base in the molar area (RMC-LMC/RPF-LPF = 2.47) (Table 6) and by a predominant maxillary contribution of 69.75% and a limited nasal contribution of 30.25% to the total increase in nasomaxillary volume (Table 1). The greater magnitude of skeletal increase, more than the dental increase in the incisor region (RNP-LNP/RIC-LIC = 9.22), could be due to a partial closure of the midline diastema by traction of transseptal periodontal fibers.
Our findings concerning sagittal suture opening following RME were in concordance with the results reported by other authors29 and different from those of Christie et al.3 The suture response presented a triangular pattern, with the widest part positioned anteriorly: the ratio of anterior/posterior skeletal suture opening (RNP-LNP/RPF-LPF) was 3.95. Suture response evaluation could be better visualized through 3D than through 2D imaging as a result of the absence of structure superimpositions and the ease of landmark identification and reproducibility. Further prospective studies are needed to validate these results and to evaluate the relationship between nasal volume increase and mode of breathing.
CONCLUSIONS
Within the limitations of this prospective study,
There were volumetric increases of different components of the nasomaxillary complex. The total volume (A) increased by 2.81 mm3, or 12%, including increases in the nasal volume (B) of 0.85 mm3 and in the maxillary volume (C) of 1.96 mm3, which are equivalent, respectively, to 17% and 10.6%.
The maxillary contribution of 1.96 mm3 to the total volume increase of 2.81 mm3 represented 69.75%, and the nasal contribution was estimated to 30.25% as a result of the increase of nasal volume of 0.85 mm3.
All maxillary transverse skeletal anterior and posterior variables as well as dental anterior and posterior linear and angular variables showed statistically highly significant increases.
The suture response to RME presented a triangular opening pattern in the vertical direction, which decreases in magnitude from dental arch to basal bone, as well as in the sagittal direction, with the widest part being positioned anteriorly.
ACKNOWLEDGMENTS
The authors are indebted to Professor José Braga for providing the research support from the Anthropobiology Laboratory at Toulouse University, Toulouse, France. We also thank Professor Ziad Salameh for reviewing the manuscript and Ing Haÿtham Eid for his technical support.
REFERENCES
- 1.Harrison JE, Ashby D. Orthodontic treatment for posterior crossbites. Cochrane Database Syst Rev. 2002;1:CD000979. doi: 10.1002/14651858.CD000979. [DOI] [PubMed] [Google Scholar]
- 2.Ramires T, Maia RA, Barone JR. Nasal cavity changes and the respiratory standard after maxillary expansion. Braz J Otorhinolaryngol. 2008;74:763–769. doi: 10.1016/S1808-8694(15)31388-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Christie KF, Boucher N, Chung CH. Effects of bonded rapid palatal expansion on the transverse dimensions of the maxilla: a cone-beam computed tomography study. Am J Orthod Dentofacial Orthop. 2010;137:S79–S85. doi: 10.1016/j.ajodo.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 4.Pangrazio-Kulbersh V, Wine P, Haughey M, Pajtas B, Kaczynski R. Cone beam computed tomography evaluation of changes in the naso-maxillary complex associated with two types of maxillary expanders. Angle Orthod. 2012;82:448–457. doi: 10.2319/072211-464.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Habersack K, Karoglan A, Sommer B, Benner KU. High-resolution multislice computerized tomography with multiplanar and 3-dimensional reformation imaging in rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2007;131:776–781. doi: 10.1016/j.ajodo.2005.09.030. [DOI] [PubMed] [Google Scholar]
- 6.Leonardi R, Cutrera A, Barbato E. Rapid maxillary expansion affects the spheno-occipital synchondrosis in youngsters: a study with low-dose computed tomography. Angle Orthod. 2010;80:106–110. doi: 10.2319/012709-56.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ribeiro ANC, de Paiva JB, Rino-Neto J, Illipronti-Filho E, Trivino T, Mongelli Fantini S. Upper airway expansion after rapid maxillary expansion evaluated with cone beam computed tomography. Angle Orthod. 2012;82:458–463. doi: 10.2319/030411-157.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Babacan H, Sökücü O, Doruk C, Ay S. Rapid maxillary expansion and surgically assisted rapid maxillary expansion effects on nasal volume. Angle Orthod. 2006;76:66–71. doi: 10.1043/0003-3219(2006)076[0066:RMEASA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Doruk C, Sökücü O, Biçakçi AA, Yilmaz U, Tas F. Comparison of nasal volume changes during rapid maxillary expansion using acoustic rhinometry and computed tomography. Eur J Orthod. 2007;29:251–255. doi: 10.1093/ejo/cjl069. [DOI] [PubMed] [Google Scholar]
- 10.Palaisa J, Ngan P, Martin C, Razmus T. Use of conventional tomography to evaluate changes in the nasal cavity with rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2007;132:458–466. doi: 10.1016/j.ajodo.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 11.Görgülü S, Gokce SM, Olmez H, Sagdic D, Ors F. Nasal cavity volume changes after rapid maxillary expansion in adolescents evaluated with 3-dimensional simulation and modeling programs. Am J Orthod Dentofacial Orthop. 2011;140:633–640. doi: 10.1016/j.ajodo.2010.12.020. [DOI] [PubMed] [Google Scholar]
- 12.Smith T, Ghoneima A, Stewart K, et al. Three-dimensional computed tomography analysis of airway volume changes after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2012;141:618–626. doi: 10.1016/j.ajodo.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 13.Oliveira De Felippe NL, Da Silveira AC, Viana G, Kusnoto B, Smith B, Evans CA. Relationship between rapid maxillary expansion and nasal cavity size and airway resistance: short- and long-term effects. Am J Orthod Dentofacial Orthop. 2008;134:370–382. doi: 10.1016/j.ajodo.2006.10.034. [DOI] [PubMed] [Google Scholar]
- 14.Iwazaki T, Saitoh I, Takemoto Y, et al. Improvement of nasal airway ventilation after rapid maxillary expansion evaluated with computational fluid dynamics. Am J Orthod Dentofacial Orthop. 2012;141:269–278. doi: 10.1016/j.ajodo.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 15.Villa MP, Malagola C, Pagani J, et al. Rapid maxillary expansion in children with obstructive sleep apnea syndrome: 12-month follow-up. Sleep Med. 2007;8:128–134. doi: 10.1016/j.sleep.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 16.Athanasiou AE. Orthodontic Cephalometry. London: Mosby-Wolfe; 1995. [Google Scholar]
- 17.Lagravère MO, Gordon JM, Guedes IH, et al. Reliability of traditional cephalometric landmarks as seen in three-dimensional analysis in maxillary expansion treatments. Angle Orthod. 2009;79:1047–1056. doi: 10.2319/010509-10R.1. [DOI] [PubMed] [Google Scholar]
- 18.Oliveira NL, Da Silveira AC, Kusnoto B, Viana G. Three-dimensional assessment of morphologic changes of the maxilla: a comparison of 2 kinds of palatal expanders. Am J Orthod Dentofacial Orthop. 2004;126:354–362. doi: 10.1016/j.ajodo.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 19.Garib DG, Henriques JFC, Janson G, Freitas MR, Coelho RA. Rapid maxillary expansion—tooth tissue-borne versus tooth-borne expanders: a computed tomography evaluation of dentoskeletal effects. Angle Orthod. 2005;75:548–557. doi: 10.1043/0003-3219(2005)75[548:RMETVT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Podesser B, Williams S, Crismani AG, Bantleon HP. Evaluation of the effects of rapid maxillary expansion in growing children using computer tomography scanning: a pilot study. Eur J Orthod. 2007;29:37–44. doi: 10.1093/ejo/cjl068. [DOI] [PubMed] [Google Scholar]
- 21.Garrett BJ, Caruso JM, Rungcharassaeng K, Farrage JR, Kim JS, Taylor GD. Skeletal effects to the maxilla after rapid maxillary expansion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2008;134:8.e1–8.e11. doi: 10.1016/j.ajodo.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 22.Lagravère MO, Carey JP, Heo G, Toogood RW, Major PW. Transverse, vertical, and anteroposterior changes from bone-anchored maxillary expansion vs traditional rapid maxillary expansion: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2010;137:304.e1–304.e12. doi: 10.1016/j.ajodo.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 23.Lamparski DG, Jr, Rinchuse DJ, Close JM, Sciote JJ. Comparison of skeletal and dental changes between 2-point and 4-point rapid palatal expanders. Am J Orthod Dentofacial Orthop. 2003;123:321–328. doi: 10.1067/mod.2003.10. [DOI] [PubMed] [Google Scholar]
- 24.Chung CH, Font B. Skeletal and dental changes in the sagittal, vertical, and transverse dimensions after rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2004;126:569–575. doi: 10.1016/j.ajodo.2003.10.035. [DOI] [PubMed] [Google Scholar]
- 25.Cross DL, McDonald JP. Effect of rapid maxillary expansion on skeletal, dental, and nasal structures: a postero-anterior cephalometric study. Eur J Orthod. 2000;22:519–528. doi: 10.1093/ejo/22.5.519. [DOI] [PubMed] [Google Scholar]
- 26.Bassil-Nassif N, Bouserhal J, Garcia R. Facial volumes and vertical growth type: a three dimensional comparative study. Orthod Fr. 2010;81:127–137. doi: 10.1051/orthodfr/2010011. [DOI] [PubMed] [Google Scholar]
- 27.Bassil-Nassif N, Bouserhal J, Treil J, Braga J, Garcia R. Sexual dimorphism and facial cavities: a volumetric study by 3D imaging. Orthod Fr. 2011;82:217–222. doi: 10.1051/orthodfr/2011116. [DOI] [PubMed] [Google Scholar]
- 28.Lagravère MO, Heo G, Major PW, Flores-Mir C. Meta-analysis of immediate changes with rapid maxillary expansion treatment. J Am Dent Assoc. 2006;137:44–53. doi: 10.14219/jada.archive.2006.0020. [DOI] [PubMed] [Google Scholar]
- 29.Silva Filho OG, Silva Lara T, Almeida AM, Silva HC. Evaluation of the midpalatal suture during rapid palatal expansion in children: a CT study. J Clin Pediatr Dent. 2005;29:231–238. doi: 10.17796/jcpd.29.3.kvu17822u2056508. [DOI] [PubMed] [Google Scholar]