Abstract
Background
During the COVID-19 pandemic, CF centers shifted to a telehealth delivery model. Our study aimed to determine how people with CF (PwCF) and their families experienced telehealth and assessed its quality and acceptability for future CF care.
Methods
The CF Patient and Family State of Care Survey (PFSoC) was fielded from August 31-October 30, 2020. The PFSoC explored themes of overall telehealth quality, ease of use, desirability, and preference for a future mix of in-person and telehealth care. Demographic covariates considered included: gender, age, CFTR modulator status, and region of residence.
Results
424 PwCF and parents of PwCF responded (47% parents). Most (81%) reported a telehealth visit which included a MD/APP and nurse team members. 91% found telehealth easy to use, and 66% reported similar/higher quality than in-person care. One-third (34%) reported the highest desire for future telehealth care, with 45% (n =212) desiring 50% or more of visits conducted via telehealth. Adults were more likely than parents to report highest desire for future telehealth (64% vs. 36%). Respondents who perceived telehealth as similar/higher quality were more likely to desire future telehealth compared to those who perceived telehealth as lower quality (96% vs. 50%). Mixed methods analysis revealed themes affecting perceptions of telehealth.
Conclusions
PwCF desire for future telehealth was influenced by perception of quality and age. Several themes emerged that need to be explored as telehealth is adapted into the CF chronic care model, especially when thinking about integration into pediatric care.
Keywords: Cystic Fibrosis, Telehealth, COVID-19, Healthcare Utilization, Experience of Care
Abbreviations: CF, Cystic Fibrosis; CFF, Cystic Fibrosis Foundation; CFTR, Cystic Fibrosis Transmembrane Conductance Regulator; COVID-19, Novel SARS-CoV-2 coronavirus; PwCF, People with CF; PFSoC, Patient and Family State of Care Survey; PFT, Pulmonary Function Testing
1. Background
Cystic fibrosis (CF) is a chronic genetic disease that involves multiple organ systems but primarily impairs the lungs and gastrointestinal tract [1]. Survival has increased rapidly over the past 3 decades, largely due to development of highly effective novel drug therapies and advancements in the robust clinical care provided by CF Foundation (CFF) accredited care centers [2,3]. The CF care model prioritizes regular quarterly visits with an interdisciplinary CF care team where treatment plans are updated and maintained in collaboration with people with CF (PwCF) and families. During the COVID-19 pandemic, routine in-person CF clinic visits were interrupted, necessitating a rapid shift to providing multidisciplinary telehealth care.
Prior to the COVID-19 pandemic, limited evidence supported the efficacy of telehealth in the CF care model although several pilot studies explored introduction of outpatient CF telehealth [4], [5], [6], [7], [8], [9], [10]. Small single center studies of feasibility of telehealth in CF found improved access to clinical care for adults living in rural settings [6], large potential cost savings [4], and high levels of patient satisfaction with telehealth [5,6]. However, another study raised concerns with poor patient acceptance of the virtual model and noted no impact on pulmonary function after five years of telehealth interventions [11]. This study also highlighted legal and regulatory barriers to widespread implementation of telehealth practices after completing a 10-year study of telehealth in CF [11].
At the onset of the pandemic in early 2020, a large-scale shift to virtual care occurred to facilitate social distancing, to permit clinics to redistribute resources to meet other healthcare demands, and to promote infection control. These system changes coupled with regulatory and payer changes enabled a rapid adoption of telehealth in CF centers across the world [12]. Two adult CF programs demonstrated successful implementation of a multidisciplinary telehealth model of CF care with PwCF expressing positive regard for telehealth at the beginning of the pandemic [13,14]. Given the rapid and unexpected integration of telehealth into the CF care model, Davis and colleagues designed cross sectional surveys to explore pediatric and adult patient and family experience of telehealth care in the context of the COVID-19 pandemic [15]. Surveys were deployed at 11 CF centers and results indicated that most PwCF and families were highly satisfied with telehealth [15]. This work suggests that multidisciplinary telehealth care in CF was convenient and well accepted by PwCF and their families at the beginning of the pandemic [15]. However, there were several limitations of this work. The CF care centers surveyed were early adopters of telehealth and therefore, may have viewed it more favorably. The surveys were also cross-sectional and may only be representative of when telehealth was mandated due to social distancing. To more broadly understand telehealth experiences of PwCF and families, the CFF developed a Patient and Family State of Care (PFSoC) Survey. The objective of this study was to explore patient and family perceptions on different facets of the use of telehealth in the CF care model.
2. Methods
2.1. Data sources
The PFSoC was distributed to PwCF and families via CF care programs, CFF Community Voice newsletter, and the CFF Facebook page between August 31 and October 30, 2020. It included questions about the care experience and perceptions on the quality of telehealth, access to interdisciplinary care, and the desire for telehealth care as part of the CF care model. It also included open-end questions inviting comments regarding the quality of telehealth care, reasons for their assessment of quality, reasons for higher or lower desire for telehealth care in the future, and suggestions for improving delivery of future telehealth care. A detailed description of survey methods and respondent characteristics compared to a national sample is provided by Dowd and colleagues [16].
2.2 Variables
Telehealth use was surveyed by questions related to receipt of telehealth and mode of telehealth. Telehealth perceptions were surveyed by questions related to ease of use, overall quality of telehealth relative to in-person care, participation of care team members in the telehealth visit, proportion of top-box responses (those reporting scores of 9/9) to questions asking about care quality and ease of participation, and benefits and limitations of telehealth. Additional questions assessed desire for future telehealth in the CF care model; preferred mix between in-person and telehealth services; and recommendations for care model components to continue or change in the future.
Independent variables included self-reported respondent type (adult with CF/parent of a child with CF), use of a modulator (yes/no), gender (male/female), or region of the US (Midwest, Northeast, Southeast, Southwest, and West).
2.3 Analytic approach
Data were summarized with descriptive statistics. Relationships between dependent and independent variables were determined with chi-square (χ2) analyses. We used two-sided significance tests and a P-value threshold of <0.05 to identify significant differences. Analyses were conducted with SPSS (version 26.0). Qualitative analyses for free-text responses were conducted with Atlas.ti (version 8.4.5). We used inductive thematic analysis to identify themes and sub-themes. Qualitative data were independently coded by two reviewers (AVC and PS). Responses between reviewers were evaluated for consensus, and discrepancies were resolved via conversation. Human-subjects approval was granted by Advarra.com (Marshall, Pro00045302).
3. Results
The PFSoC was completed by 424 participants, including 222 adults with CF (52.5%) and 201 parents of a child with CF (47.5%). A majority of respondents were female (59%) and most reported taking a CFTR modulator (71.5%). Respondents were distributed throughout the United States, with roughly one-fifth in the Midwest, Northeast, and Southeast, 28% in the West, and 10% in the Southwest. Respondent characteristics are described in detail by Dowd and colleagues [16].
3.1. Uptake of telehealth during the COVID-19 pandemic
Four-fifths (81%, n=328) of PwCF indicated that they had a telehealth visit, either by phone or video connection, since the start of the COVID-19 pandemic. Among the 76 PwCF that had not had a telehealth visit, the most common reasons were the absence of health concerns (n=30), participation in an in-person visit (n=22), or preference to not receive telehealth services (n=19). Less common reasons included the lack of a request by the care team to schedule a telehealth visit (n=8), concerns regarding co-pays or insurance (n=5), cross-state restrictions on telehealth (n=3), and technical difficulties with telehealth (n=3).
PwCF who received telehealth services most often reported having a video component to their visit (n=287, 88%). Among those that reported receiving a “phone only” telehealth visit (n=40), this approach was chosen based on PwCF preference (n=18) or care team preferences (n=11). Less common reasons included challenges with the video technology (n=5) or a lack of reliable internet (n=3).
3.2. Overall perceptions of telehealth
3.2.1. Ease of use
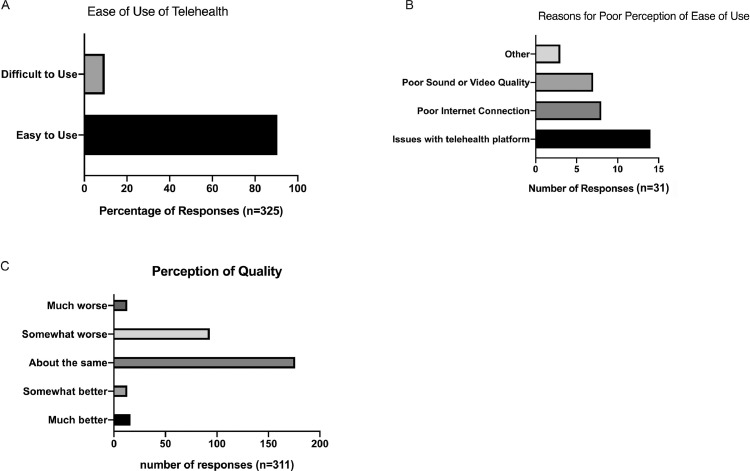
Ninety-one percent (n=294) of PwCF found the telehealth technology easy to use. Those who did not find it easy to use (n=31) cited difficulty using the telehealth platform (n=15, e.g., a need for a more reliable, user-friendly platform; a need to download applications; multiple layers of security), poor sound or video quality (n=7), or poor internet connection (n=6). These data are summarized in Fig. 1 A and B.
Fig. 1.
Ease of Use and Quality Perceptions of Telehealth. A. Overall summary of ease of use data. B. Most common reasons for respondents’ poor perception of ease of use. C. Overall respondents’ perceptions of quality of telehealth.
3.2.2. Quality of care
PwCF were more likely (66%, n=205) to feel that telehealth services were of equal or higher quality than in-person services. Overall quality data are summarized in Fig. 1C.
There were no differences in perceptions of quality among PwCF by respondent type, receipt of a modulator, gender, or region of the country. These data are summarized in Supplemental Figure 1.
3.3.1. Participation of care team in the telehealth visit
Most PwCF (95%) reported that they interacted with a provider (MD/APP) during their last telehealth visit or during an additional phone or video visit. Over half of PwCF reported interacting with a nurse (63%) or dietitian (54%) during their telehealth visit or in an additional phone or video visit. Less than half of patients reported interacting with other members of the multidisciplinary team, including the social worker (44%), respiratory therapist (34%), physical therapist (8%), pharmacist (24%), or mental health coordinator (16%). See Supplemental Figure 2A.
3.3.2. Care interactions
Most PwCF provided a top-box score indicating that every effort was made to ask about topics or concerns that patients wanted to discuss (75%, n=231), help them understand their health issues (73%, n=224), listen to the things that matter most (74%, n=227), include what matters most in choosing what to do next (69%, n=214), provide adequate time with team members (71%, n=219), and schedule the visit at a time that works for the PwCF (73%, n=225). See Supplemental Figure 2B.
3.4. Benefits and limitations of telehealth
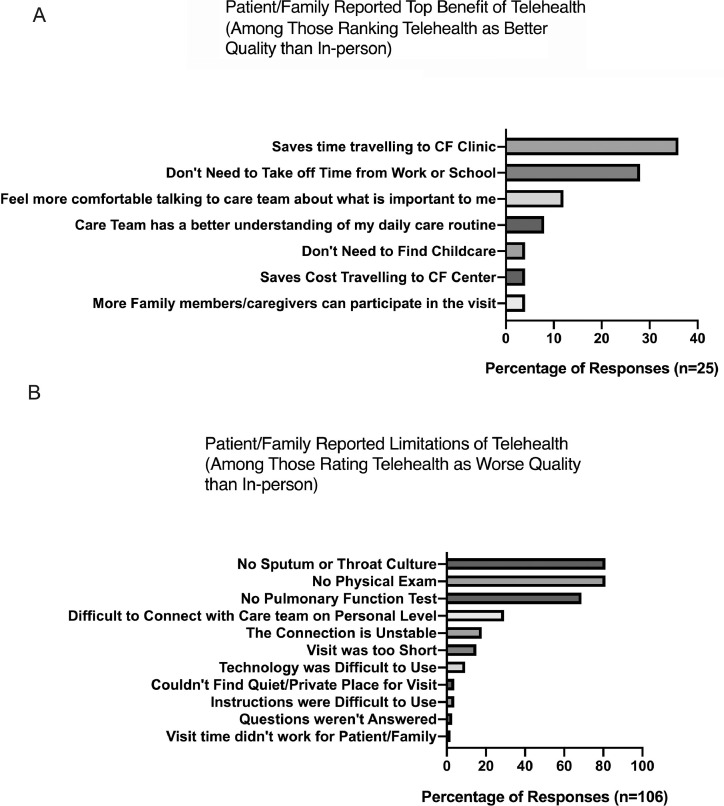
Among PwCF who perceived telehealth as somewhat or much better than in-person care (n=25), the greatest benefit of telehealth was the savings in time spent traveling to the CF clinic, followed by not needing to take time off from work or school. Other benefits are shown in Fig. 2 A.
Fig. 2.
Ranked Responses for Benefits and Limitations of Telehealth. A. Ranked responses for top benefits of telehealth among respondent's who viewed telehealth of high quality. B. Ranked responses of limitations for respondents who felt that telehealth was of poorer quality than in-person care.
Among PwCF who perceived telehealth as somewhat or much worse than in-person care (n=106), more than three-quarters of individuals noted limitations associated with the lack of physical examination (81%, n=86), the lack of a sputum or throat culture (81%, n=86), and the lack of a pulmonary function test (69%, n=73). One-third (29%, n=31) found it difficult to connect with the care team on a personal level, and 18% (n=19) felt that the telehealth connection was unstable. Other limitations are outlined in Fig. 2B.
3.5. Future telehealth in the CF care model
3.5.1. Desire for future telehealth
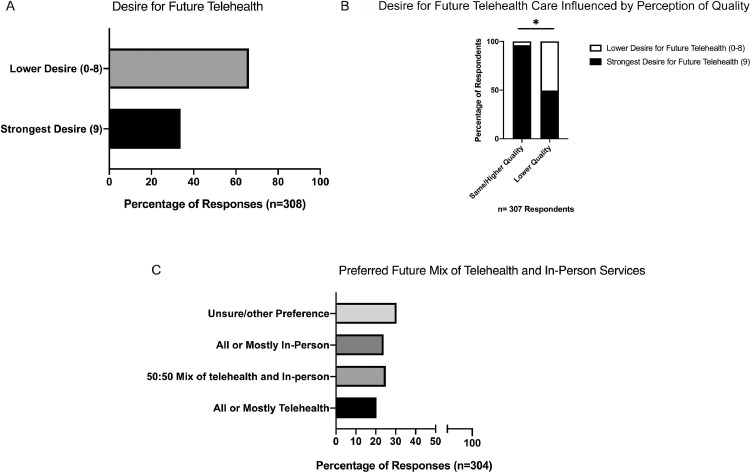
One-third (34%, n=104) of PwCF provided the highest level of desire for telehealth. Overall desire is illustrated in Fig. 3 A. PwCF with the highest desire for future telehealth, were more likely to think that the quality of telehealth care was the same or better than in-person care (96.2%; 100/104) compared to those with lower desire (50%; 102/203). See Figure 3B.
Fig. 3.
Summary of Respondents’ Desire for Future telehealth. A. Distribution of responses regarding strongest desire for telehealth in future CF care. B. The desire for telehealth is significantly influenced by respondents’ perceptions of quality of telehealth (p<0.05). C. Distribution of responses of preference for mix of telehealth and in-person care in future CF care.
Telehealth was more desired by adults with CF (40%, n=66 of 166) than parents of children with CF (26%; n=37 of 141), p=.021. See Supplemental Figure 3A. There were no differences among PwCF who expressed strongest desire for telehealth when compared by modulator status of the respondent (yes/no), gender (male/female), or region of the country. These data are summarized in Supplemental Figure 3 B-D.
PwCF who rated their desire for telehealth as an 8 or lower on a 0-9 rating scale identified a number of changes needed to provide a higher rating for telehealth. The most frequently identified changes included issues related to measurement and testing, the model of care (emphasizing preference for in-person care), and issues of care quality and access. These themes are presented in Table 1 .
Table 1.
What changes would need to be made to telehealth for you to give it a higher rating?a
| Telehealth about the same or better than in person (n=102) |
Telehealth somewhat or much worse than in person (n=101) |
Total (n=203) |
||||
| Measurement and testing | 38 | 37% | 61 | 58% | 99 | 49% |
| Physical exam | 12 | 12% | 29 | 27% | 41 | 20% |
| Pulmonary function testing (in person) | 11 | 11% | 25 | 24% | 36 | 18% |
| Sputum/throat culture | 13 | 13% | 22 | 21% | 35 | 17% |
| Pulmonary function testing (remote) | 7 | 7% | 7 | 7% | 14 | 7% |
| Labs/imaging | 3 | 3% | 10 | 9% | 13 | 6% |
| Testing: Remote | 4 | 4% | 6 | 6% | 10 | 5% |
| Weight/height | 3 | 3% | 4 | 4% | 7 | 3% |
| Testing: In person | 0 | 0% | 6 | 6% | 6 | 3% |
| Care delivery model | 29 | 28% | 41 | 39% | 70 | 34% |
| Care delivered via in-person visits | 26 | 27% | 19 | 18% | 45 | 22% |
| Care delivered via telehealth | 13 | 13% | 7 | 7% | 26 | 13% |
| Criteria for appropriateness of telehealth visit | 8 | 8% | 4 | 4% | 12 | 6% |
| Care delivered via mix of telehealth and in-person clinic visits | 3 | 3% | 3 | 3% | 6 | 3% |
| Care quality/access | 21 | 21% | 30 | 28% | 51 | 25% |
| Multidisciplinary care team/provider | 9 | 9% | 10 | 9% | 19 | 9% |
| Communication/relationships | 7 | 7% | 10 | 9% | 17 | 8% |
| Care quality (unspecified) | 5 | 5% | 6 | 6% | 11 | 5% |
| Preparation for visit | 1 | 1% | 8 | 8% | 9 | 4% |
| Telehealth technology | 7 | 7% | 7 | 7% | 14 | 7% |
| Care Logistics | 4 | 4% | 8 | 8% | 12 | 6% |
| Lack of time/inefficiency | 2 | 2% | 5 | 5% | 7 | 3% |
| Convenience | 2 | 2% | 3 | 3% | 5 | 2% |
| Other | 6 | 6% | 10 | 9% | 16 | 8% |
| No improvements identified | 11 | 11% | 6 | 6% | 17 | 8% |
Responses are limited to PwCF that responded with an 8 or lower to the following question: “On a scale from 0-9, please indicate your desire for future telehealth visits?” (n=204 of 308 respondents). The sample size was further reduced by 1 PwCF that did not respond to the question regarding quality of telehealth.
3.5.2. Preferred mix between in-person and telehealth services
When asked about the mix of telehealth, approximately equal proportions of PwCF preferred all or mostly telehealth (20%, n=62); half and half telehealth and in-person (25%, n=76); or all or mostly in-person care (24%, n=73). The remainder were unsure or had other preferences (31%, n=93). These data are summarized in Fig. 3C. There were no differences in preferred mix of in-person and telehealth visits by age, gender, modulator status, or region of residence in the country.
3.6. PwCF recommendations for improvements to the CF model of care
The qualitative observations of PwCF regarding the CF care model and changes implemented since the pandemic began are delineated in Table 2 . PwCF would like to see continued availability of telehealth and would like to see changes or improvements in measurement and testing associated with telehealth visits.
Table 2.
Patient perspectives on the changes in CF care that have occurred since the coronavirus/COVID-19 pandemic.
| What would you/your child like to see continued in the future? (n=288) | What would you/your child like to see changed in the future? (n=288) | |||
|---|---|---|---|---|
| Care delivery model | 174 | 61% | 53 | 18% |
| Care delivered via telehealth | 114 | 40% | 22 | 8% |
| Care delivered via mix of telehealth and in-person clinic visits | 40 | 14% | 15 | 5% |
| Care delivered via in-person clinic visit | 21 | 7% | 14 | 5% |
| Criteria for appropriateness of telehealth visit | 25 | 9% | - | - |
| Measurement and testing | 27 | 10% | 49 | 17% |
| Safety/infection prevention | 33 | 12% | 6 | 2% |
| Care logistics (e.g., convenience, frequency/time/efficiency of visit, healthcare facility) | 32 | 11% | 17 | 6% |
| Quality of care (e.g., communication, multi-disciplinary team, sharing information) | 24 | 9% | 27 | 9% |
| Insurance/co-pay | 4 | 1% | 5 | 2% |
| Technology for telehealth | 2 | 1% | 5 | 2% |
| Research/treatment development | 1 | 0% | 6 | 2% |
| Other (e.g., COVID-19, mental health, social connection) | 17 | 6% | 20 | 7% |
| None/not applicable | 44 | 16% | 90 | 31% |
4. Discussion
We analyzed a large, nationwide dataset of the experiences of PwCF and families with telehealth from early in the COVID-19 pandemic. This mixed-method analysis was clustered around overall experience of telehealth, perception of quality of telehealth, and desire for future telehealth in the CF care model. We found that the majority of survey respondents felt that telehealth was easy to use (usually limited by technology concerns), and greater than two-thirds of patients felt telehealth was of similar or greater quality than in-person visits. It should be noted, however, that only a small proportion of respondents felt telehealth was of greater quality than in-person care, signaling. that telehealth is not the sole preference of CF care.
Most visits involved physician and advance practice providers and some other members of the multidisciplinary team. The majority of PwCF or families of PwCF felt that their needs were met in telehealth visits. Convenience factors were most commonly cited amongst those who felt telehealth was superior to in-person care, and lack of key assessments (PFTs, etc.) were commonly cited by the one third of patients who felt that telehealth was of poorer quality than in-person visits.
Subgroup analyses did not suggest key demographics differences in assessment of quality. These subgroup data suggest that telehealth is viewed similarly across a broad spectrum of PwCF. This assessment of quality overall compares to themes and quantitative assessment of quality from previously published limited samples [15]. However, this sample did assess a significant number of patients who had not experienced telehealth and this may have influenced perception of telehealth. This survey also includes data regarding PwCF and family perception of telehealth in those who had not experienced this mode of care delivery, which is unique compared to other recent publications of telehealth experience of care [15].
Respondents were more mixed on their desire for future telehealth, in contrast to previously published work [15]; although, we also found that families of children with CF were less likely to desire telehealth than adults, indicating a perception gap between ages that compares similarly to survey data from providers [17]. In contrast, other key demographics did not influence desire for future telehealth. Importantly, the perception of quality is a strong, independent predictor of desire of future telehealth. Respondents were equally distributed in their preference for mix of telehealth and in-person care in the future of CF care. These demographics differences will need further exploration as the optimum population of PwCF for telehealth care is examined in future research.
The study has some noted limitations. It is a relatively small sample size with 20% having not experienced telehealth at the time of the survey, but it adds a larger, national sample to the existing data available on PwCF and family perception. While this data will be helpful to determine the optimal conditions for future telehealth, it will not answer questions about perception after more frequent utilization of telehealth. There is work underway to repeat these analyses to determine the ongoing strength of perception both by the CFF and other smaller networks of CF centers. Finally, analyses regarding perceptions of quality were only differentiated on the basis of respondents’ overall assessment of quality of telehealth. Therefore, additional work will be needed to understand if suggested improvements to telehealth are similar in respondents with differing views on the quality of telehealth.
5. Conclusion
This summary data adds confidence to a growing body of literature of an overall positive perception of telehealth in CF and a desire to use telehealth in the future, especially for visits involving physician and advance practice providers. More research is needed to determine the optimal process for multi-disciplinary telehealth visits, including potential blend of in-person and telehealth models. Further, age differences will require attention in planning for the frequency and mix of telehealth and in-person visits in pediatric versus adult care centers. Finally, establishment of effective at-home monitoring and alleviation of technical issues will need special attention (see companion manuscripts) to adopt telehealth in the CF care model after COVID-19.
Declaration of Competing Interest
There are no conflicts of interest.
Acknowledgements
The authors wish to thank the PwCF and their families for their participation in the survey. Funding provided by NIH (1K08HL138153-01A1 and 2P30DK072482-12) and CFF (Solomon 20Y0 and NELSON20QI0).
Footnotes
This paper is part of a Supplement supported by the Cystic Fibrosis Foundation.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jcf.2021.09.005.
Appendix. Supplementary materials
References
- 1.Quon BS, Rowe SM. New and emerging targeted therapies for cystic fibrosis. BMJ (Clinical research ed) 2016;352:i859. doi: 10.1136/bmj.i859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cystic Fibrosis Foundation Patient Registry: 2019 Annual Data Report. Published 2019. Accessed.
- 3.Lebecque P, Leonard A, De Boeck K, et al. Early referral to cystic fibrosis specialist centre impacts on respiratory outcome. J Cyst Fibros. 2009;8(1):26–30. doi: 10.1016/j.jcf.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Tagliente I, Trieste L, Solvoll T, Murgia F, Bella S. Telemonitoring in Cystic Fibrosis: A 4-year Assessment and Simulation for the Next 6 Years. Interact J Med Res. 2016;5(2):e11. doi: 10.2196/ijmr.5196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gur M, Nir V, Teleshov A, et al. The use of telehealth (text messaging and video communications) in patients with cystic fibrosis: A pilot study. J Telemed Telecare. 2017;23(4):489–493. doi: 10.1177/1357633X16649532. [DOI] [PubMed] [Google Scholar]
- 6.Wood J, Mulrennan S, Hill K, Cecins N, Morey S, Jenkins S. Telehealth clinics increase access to care for adults with cystic fibrosis living in rural and remote Western Australia. J Telemed Telecare. 2017;23(7):673–679. doi: 10.1177/1357633X16660646. [DOI] [PubMed] [Google Scholar]
- 7.Lang RL, Wilson C, Stockton K, Russell T, Johnston LM. CyFiT telehealth: protocol for a randomised controlled trial of an online outpatient physiotherapy service for children with cystic fibrosis. BMC Pulmon Med. 2019;19(1):21. doi: 10.1186/s12890-019-0784-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shakkottai A, Kaciroti N, Kasmikha L, Nasr SZ. Impact of home spirometry on medication adherence among adolescents with cystic fibrosis. Pediatr Pulmonol. 2018;53(4):431–436. doi: 10.1002/ppul.23950. [DOI] [PubMed] [Google Scholar]
- 9.Tomlinson OW, Shelley J, Trott J, Bowhay B, Chauhan R, Sheldon CD. The feasibility of online video calling to engage patients with cystic fibrosis in exercise training. J Telemed Telecare. 2020;26(6):356–364. doi: 10.1177/1357633X19828630. [DOI] [PubMed] [Google Scholar]
- 10.Choyce J, Shaw KL, Sitch AJ, Mistry H, Whitehouse JL, Nash EF. A prospective pilot study of home monitoring in adults with cystic fibrosis (HOME-CF): protocol for a randomised controlled trial. BMC Pulmon Med. 2017;17(1):22. doi: 10.1186/s12890-017-0366-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bella S, Murgia F, Tozzi AE, Cotognini C, Lucidi V. Five years of Telemedicine in Cystic Fibrosis Disease. Clin Ter. 2009;160(6):457–460. [PubMed] [Google Scholar]
- 12.Fisk M, Livingstone A, Pit SW. Telehealth in the Context of COVID-19: Changing Perspectives in Australia, the United Kingdom, and the United States. J Med Internet Res. 2020;22(6):e19264. doi: 10.2196/19264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Compton M, Soper M, Reilly B, et al. A Feasibility Study of Urgent Implementation of Cystic Fibrosis Multidisciplinary Telemedicine Clinic in the Face of COVID-19 Pandemic: Single-Center Experience. Telemed J E Health. 2020;26(8):978–984. doi: 10.1089/tmj.2020.0091. [DOI] [PubMed] [Google Scholar]
- 14.Womack C, Farsin R, Farsad M, Chaudary N. Emerging Alternatives to Conventional Clinic Visits in the Era of COVID-19: Adoption of Telehealth at VCU Adult Cystic Fibrosis Center. Int J Gen Med. 2020;13:1175–1186. doi: 10.2147/IJGM.S274193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis J, Nesmith N, Perkins R, et al. Patient and family perceptions of telehealth as part of the cystic fibrosis care model during COVID-19. J Cyst Fibros. 2021 doi: 10.1016/j.jcf.2021.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dowd C, Van Citters AD, Dieni O, Willis A, Powell L, Sabadosa KA. Design and methods for understanding the state of cystic fibrosis care amid the COVID-19 pandemic. J Cyst Fibros. 2021 doi: 10.1016/j.jcf.2021.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perkins RC, Davis J, NeSmith A, et al. Favorable Clinician Acceptability of Telehealth as Part of the Cystic Fibrosis Care Model during the COVID-19 Pandemic. Ann Am Thorac Soc. 2021 doi: 10.1513/AnnalsATS.202012-1484RL. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.