Abstract
Background
Due to the COVID-19 pandemic, there was an uptake of telehealth in cystic fibrosis care. Previous studies show disparities in telehealth use based on socioeconomic status (SES). We aimed to: (1) understand telehealth use and perceptions and (2) identify the facilitators and barriers to telehealth use among people with CF and their families (PwCF) from diverse racial/ethnic and socioeconomic backgrounds.
Methods
We conducted an analysis of the 2020 Cystic Fibrosis State of Care surveys completed by PwCF (PFSoC), CF Care Programs (SoC1) and the CF Foundation Patient Registry (CFFPR).
Results
A total of 424 PwCF and 286 programs responded to the PFSoC and SoC1. Among PwCF, 90% self-identified as White, 6% as Hispanic/Latino, and 2% as Black. Racial/ethnic minorities were less likely to have had a telehealth visit (p=.015). This difference was pronounced among the Hispanic/Latino population (p<.01). Telehealth use did not differ by health insurance and was similarly offered independent of financial status. Compared to PwCF who denied financial constraints, those who reported financial difficulties found telehealth more difficult to use (p=.018) and were less likely to think that their concerns (p=.010) or issues that mattered most to them (p=.020) were addressed during telehealth. Programs perceived lack of technology, language barriers, and home conditions as barriers to telehealth in vulnerable populations.
Conclusion
PFSoC and SoC1 identified differences in telehealth use and care perceptions by ethnicity, race, and socioeconomic characteristics. Further studies are needed to understand how telehealth can change access to CF care in diverse subpopulations.
Keywords: Telehealth, Socioeconomic status, Racial/ethnic minorities
Abbreviations: CF, Cystic Fibrosis; CFCP, CF Care Program; CFF, Cystic Fibrosis Foundation; CFFPR, Cystic Fibrosis Foundation Patient Registry; CFTR, Cystic fibrosis transmembrane conductance regulator; PFSoC, Patient and Family CF State of Care Survey; PwCF, People with CF and families of patients with CF; SoC1, CF Care Program State of Care Survey Version 1 2020; TDI, The Dartmouth Institute for Health Policy & Clinical Practice; SARS-CoV-2, Severe Acute Respiratory Syndrome Due to Coronavirus 2; SES, Socioeconomic Status; TH, Telehealth
1. Introduction
As the cystic fibrosis (CF) care center network rapidly adopted telehealth during the COVID-19 pandemic [1], concerns were raised regarding further exacerbation of racial/ethnic and socioeconomic status (SES) disparities [2], [3], [4], [5], [6], [7], [8], [9], [10]. In the general population, racial/ethnic minorities and people with low SES experience decreased access to health care and are more likely to report lower satisfaction with the health care system [11], [12], [13]. While telehealth does not universally address all issues related to healthcare access in these populations [14,15], it may increase access by eliminating travel time and cost and may improve patient satisfaction [16] if critical constraints are addressed to prevent telehealth from further decreasing access to care.
The 2019 CF Foundation Patient Registry (CFFPR) reports that 9.4% of people with CF (PwCF) identify as Hispanic/Latino, 4.7% as Black, and 3.8% as other non-White race [17]. PwCF from racial/ethnic minority backgrounds and/or low SES experience greater burden of disease, increased health care utilization, and worse outcomes that parallel those in the general population [2,5,6,[18], [19], [20]]. Socioeconomic inequities (e.g., access to financial resources, household income, parental education, social support) and adverse environmental exposures (smoking) in the CF population have been previously associated with lung function decline and increased infection rates [21,22]. In addition, survey data shows that PwCF from racial/ethnic minority backgrounds and/or low SES report lower quality of life even after adjusting for disease severity [23]. Care experience and quality of care have been previously described in PwCF, but there are limited reports that examine care delivery and experience among PwCF from minority backgrounds or those with low SES, particularly in telehealth [24].
Our objective was to understand access to and experiences with telehealth among PwCF from diverse racial/ethnic and/or socioeconomic backgrounds, as well as facilitators and barriers to use of telehealth services during the COVID-19 pandemic in these vulnerable populations. Specifically, we sought to identify whether differences in telehealth use, care quality, and barriers or facilitators are associated with racial/ethnic and socioeconomic characteristics of PwCF.
2. Methods
2.1. Data sources
Three data sources were used: (a) the Patient and Family CF State of Care Survey (PFSoC) distributed to PwCF via care programs, Community Voice newsletter, and CF Foundation (CFF) Facebook page between August 24 and October 30, 2020; (b) the CF Program State of Care Survey Version 1 (SoC1) distributed to CFF accredited centers between July 29 and September 18, 2020 [1]; and (c) the CFFPR [17]. Community Voice is a network of PwCF created by CFF. Through Community Voice PwCF can connect with each other virtually and actively shape research and programs for the CF community [25].
The PFSoC data was not linked to the SoC1 or CFFPR. SoC1 and CFFPR were linked at the program level. Information related to the racial/ethnic/socioeconomic breakdown of program respondents was not captured. Respondents of SoC1 are physician program directors.
Human subjects approval was granted by a central institutional review board (Advarra), protocol (Marshall, Pro00045302).
2.2. Variables
Independent PFSoC variables included self-identified racial or ethnic minority status and financial struggles during the COVID-19 pandemic, as defined by reported concerns paying for one or more of the following essentials: co-pays, food, housing, utilities, transportation, medication, or other care, and reported insurance status, categorized into (a) Medicare (alone or with any other insurance); (b) Medicaid (alone or with other insurance, excluding Medicare); or (c) other insurance (private, military or other insurance, excluding Medicare or Medicaid). PwCF who selected no insurance (n=1), preferred not to answer (n=4), or did not answer the question related to insurance (n=86) were excluded. For consistency, we use the terms “Black” for Black or African American and “Hispanic/Latino” for Hispanic, Latino/a, or the gender-neutral Latinx. The term vulnerable population was used to include racial/ethnic minorities and/or people of low SES. We used the term minority for race and ethnicity other than non-Hispanic white. Telehealth was defined as a virtual visit conducted by phone or internet connection, with or without a video component.
Dependent PFSoC variables focused on four telehealth areas: access, quality, interest, and barriers. Telehealth access was surveyed by questions related to receipt of telehealth, mode of meeting with care team, and ease of access. Telehealth quality was surveyed by questions related to overall quality relative to in-person care; proportion of top-box responses to questions asking about concerns, shared decision-making as measured by collaboRATE [25], [26], and perceptions of adequate time with provider; scheduling at a time that worked, telehealth coverage by insurance, need for a co-pay, and ability to find a quiet, private place to participate. Telehealth interest was defined as a desire for future telehealth and preference for in-person versus telehealth care. PwCF who identified lower quality of care for telehealth relative to in-person care were asked to answer another set of questions to further describe barriers of teleheath care, which included difficulty using the technology, unclear instructions, unstable connection, inability to find a quiet/private space, inability to schedule at a time that worked, visit too short, questions unanswered, lack of physical exam, lack of pulmonary function test, and lack of sputum or throat culture. Some questions overlapped with but were more detailed than previous questions asked under quality of care.
SoC1 responses were assessed across programs. Free-text responses to the question, “Sometimes a crisis creates both positive and negative effects. What effect has the use of telehealth had on disadvantaged populations?” were analyzed to identify barriers and facilitators using qualitative analysis methods.
2.3. Analytic approach
Data were summarized with descriptive statistics. Relationships between variables were determined with chi-square tests for categorical data (and, where appropriate, Fisher's exact tests to account for small sample sizes), and Kruskal Wallis H tests for ranked data. Analyses were conducted with SPSS (version 26.0). Qualitative analyses for free-text responses were conducted with Atlas.ti (version 8.4.5). We used inductive thematic analysis to identify themes and sub-themes. All qualitative data were independently coded by two reviewers (AVC and PS). Responses between reviewers were evaluated for consensus, and discrepancies were resolved via conversation.
3. Results
3.1. Sample characteristics
The PFSoC was completed by 424 patients and the SoC1 by 286 programs. Complete demographics of PFSoC responders are reported elsewhere in this issue [1].
The characteristics of the sample are summarized in Table 1 . More than 10% (n=35) of PFSoC respondents identified as a racial or ethnic minority, nearly 27% (n=109) had financial concerns as a result of the COVID-19 pandemic, and 34% (n=116) had public insurance. People who reported financial concerns due to the COVID-19 pandemic were more likely to identify as a racial or ethnic minority (43%, n=15 vs. 24%, n=73; p=.017), and were more likely to have Medicaid (41%, n=29) compared to Medicare (29%, n=13) or all other insurance types (20%, n=40) (p<.001). There was no difference in insurance type by racial/ethnic minority group. When compared to the 2020 CFFPR, PFSoC responders were more likely to be White; in addition, PFSoC responders were less likely to have Medicaid and more likely to have private insurance than CFFPR participants (Table 1). While the PFSoC responders are a subgroup of CFFPR participants, they do not entirely represent the CFFPR population.
Table 1.
Characteristics of SoCs respondents and the 2020 CF Foundation Patient Registry.
| Characteristics of SoCs responders | PFSoCs n (%) | CFFPR n (%) | p-value |
|---|---|---|---|
| Race/ethnicity SoCs | |||
| Any racial or ethnic minority | 35 (10.4%) | 5270 (16.4%) | 0.003* |
| Hispanic/Latino | 22 (6.5%) | 3049 (9.5%) | 0.062 |
| Black | 8 (2.4%) | 1434 (4.5%) | 0.062 |
| American Indian / Alaskan Native | 3 (0.9%) | 195 (0.6%) | Not calc. |
| White (excluding any racial or ethnic minority) | 303 (89.6%) | 26825 (83.6%) | 0.003* |
| Concerns about paying for necessities, as a result of the COVID-19 pandemic1 | |||
| Any financial concerns (yes) | 109 (26.8%) | N/A | |
| Food | 49 (12.1%) | N/A | |
| Housing | 44 (10.8%) | N/A | |
| Utilities | 47 (11.6%) | N/A | |
| Transportation | 28 (6.9%) | N/A | |
| Medication | 50 (12.3%) | N/A | |
| Co-pays | 41 (10.1%) | N/A | |
| Other care | 50 (12.3%) | N/A | |
| Insurance status | |||
| Medicare | 45 (13.2%) | 3285 (10.2%) | 0.070 |
| Medicaid | 71 (20.9%) | 10707 (33.4%) | <0.001⁎⁎ |
| Other insurance | 224 (65.9%) | 17845 (55.6%) | <0.001⁎⁎ |
Example question: As a result of the coronavirus/COVID-19 pandemic, have you had any concerns about paying for food? See appendix for full questionnaire details.
statistically significant p<0.05,
p<0.01 See Methods.
3.2. Racial/ethnic characteristics as a predictor of telehealth access, quality, interest, and perceived barriers
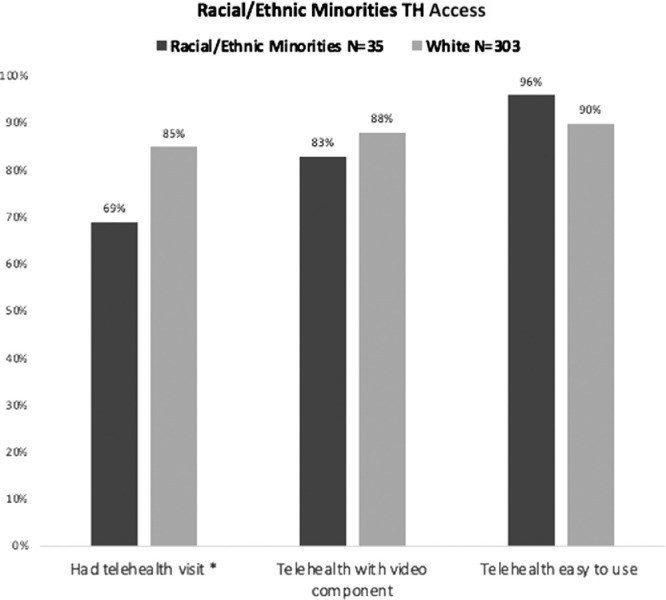
Access to telehealth: PwCF from a racial or ethnic minority group were significantly less likely to have had a telehealth visit, compared to people who identified only as White (69%, n=24 vs. 85%, n=257, p=.015). Within the Hispanic/Latino subgroup (n=22), differences in telehealth utilization were more pronounced wherein only 54% (n=12) had a telehealth visit. Within the Black subgroup (n=8), differences in mode of telehealth existed, as Black responders were less likely to have a video component of their visit compared to all others (57%, n=4 vs. 89%, n=250 p<.05). We found no statistically significant difference in the proportion of PFSoC respondents that cited that “the care team has not been in contact to schedule a telehealth visit” or “I did not want to receive care in this way”. Reasons cited by racial /ethnic minorities for no telehealth visit included: in-person visits during that time (n=5), care team has not been in contact to schedule a telehealth visit (n=3), I did not want to receive care in this way (n=3), I do not know if telehealth visits are covered by insurance (n=1), concerns about co-pays and other costs (n=1), language barriers (n=1), no health concerns (n=1), six responders did not provide an answer.
Quality of telehealth: There were no differences between reports based on race or ethnicity.
Interest in telehealth: There were no differences between reports based on race or ethnicity with respect to future desire for telehealth.
Barriers to telealth: Two respondents (29%) who identified as a racial/ethnic minority and one (1%) who identified as White felt that their questions were not answered by the care teams (Fig. 1 ).
Fig. 1.
Racial/Ethnic group telehealth access. TH=Telehealth, *statistically significant p<0.05
3.3. Financial impact of the pandemic as a predictor of telehealth access, quality, interest, and perceived barriers
PwCF experienced financial adversities due to COVID-19. While 28% (n=118) of respondents noted no change in employment, nearly one quarter (24%, n=102) had switched to working from home, and 20% (n=60) had reduced or eliminated their work hours (e.g., hours/salary reduced, laid off, furloughed, retired, quit, or leave of absence). One quarter of respondents (27%, n=109) reported concerns paying for essentials due to the COVID-19 pandemic, including paying for medication, other care, food, utilities, housing, and co-pays (10-12% each). There was less concern about paying for transportation (7%).
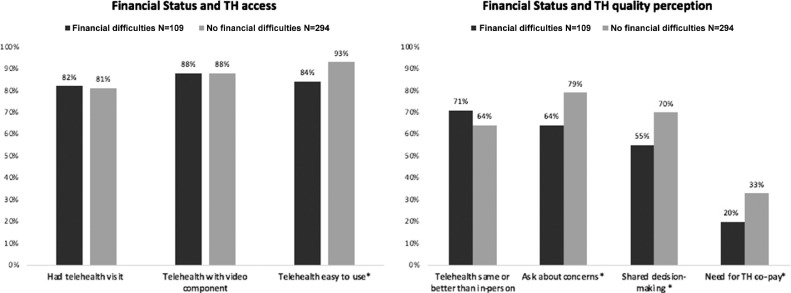
Access to telehealth: PwCF with financial concerns were less likely to think that telehealth was easy to use than those without financial concerns (84%, n=74 vs. 93%, n=219; p=.018) (Fig. 2 ).
Fig. 2.
PwCF financial status and telehealth access and quality perception. TH=Telehealth, *statistically significant p<0.05.
Quality of telehealth: PwCF who reported financial difficulties were less likely to think their care team asked about their concerns (64%, n=54 vs. 79%, n=177; p=.010) or included them in shared decision-making (55%, n=45 vs 69%, n=154; p=.02). In addition, they were less likely to have paid a co-pay or other cost for telehealth services compared to those with no reported financial difficulties due to COVID-19 (20.0%, n=14 vs. 33%, n=60; p=.045).
Interest in and barriers to telehealth: There were no differences between PwCF who reported financial difficulties and those who did not with respect to future desire for or barriers to telehealth.
3.4. Insurance type as a predictor of telehealth access, quality, interest, and barriers
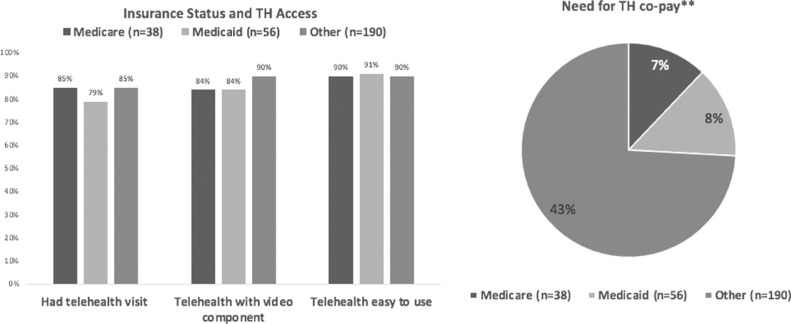
Access to, interest in, quality and barriers to telehealth: Insurance type was not associated with differences in access, interest, quality or barriers to telehealth services.
Few PwCF with Medicare (6.7%) or Medicaid (8.0%) reported having a co-pay for telehealth services. Almost half of the PFSoC responders with other insurances (43%) had a co-pay with telehealth (Fig. 3 ).
Fig. 3.
Insurance Status and Access and Need for a Co-pay to TH TH=telehealth; **statistically significant p<0.01
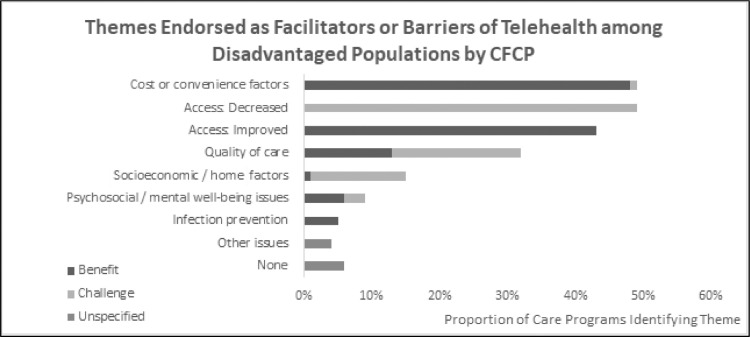
3.5. Facilitators and barriers to telehealth among vulnerable populations as reported by CF care programs
Programs provided free-text responses to the question, “Sometimes a crisis creates both positive and negative effects. What effect has the use of telehealth had on disadvantaged populations?” The answers were classified as shown in Fig. 4 (detailed listings of themes are available in Appendix Table 2). According to CF care programs, telehealth had a mixed impact on vulnerable populations. While half of programs (48%, n=134) indicated that telehealth made care less costly or more convenient or otherwise improved access to care, half of the programs (49%, n=136) indicated that telehealth limited access to care among PwCF from vulnerable populations. The programs identified travel cost, work, and child care as major facilitators of telehealth compared to in-person care. A quarter of programs identified barriers to telehealth associated with lack of technology/equipment (24%, n=66) or inability to connect to the Internet (23%, n=65). Fourteen percent of programs (n=40) indicated challenges associated with socioeconomic/home factors. In addition, 13 programs (5%) identified language barriers as a challenge to telehealth. A small proportion of programs indicated the positive impact of telehealth on psychosocial well-being (6%, n=17) and infection prevention (5%, n=14) among vulnerable populations.
Fig. 4.
Facilitators and barriers of CF care centers regarding the effect of telehealth on vulnerable populations: Qualitative summary from CF care programs (n=280)
4. Discussion
We describe important differences in access to and experiences with telehealth among PwCF who identified as a racial/ethnic minority or were socioeconomically disadvantaged.
Financial constraints were not associated with decreased use of telehealth and PwCF who reported financial difficulties associated with COVID-19 did not endorse increased cost of care due to co-pay or other costs for telehealth services. Responses to the PFSoC indicated that telehealth use during the COVID-19 pandemic did not differ by health insurance status, and insurance type was not associated with reported differences in access, quality, interest in, or barriers to telehealth services. Unsurprisingly, PwCF with public insurance were less likely to have paid a co-pay for telehealth services compared to those with other insurances. These findings suggest that the interventions implemented by the state and federal agencies and private insurers to support telehealth coverage, eliminating co-pays and similarly reimbursing telehealth visits with in-person care, were successful and suggest that telehealth may provide a mechanism for reducing socioeconomic barriers to accessing care.
PwCF from minority groups who responded to the PFSoC were less likely to have had a telehealth visit than respondents identifying as White. This difference was more pronounced in the Hispanic/Latino subgroup. Black respondents were less likely to have a video component of their telehealth visit compared to all others. Limited video use among racial and ethnic minorities in the general population has been attributed to decreased access of devices, broadband access, and reliable cellphone data plans [27]. Furthermore, data in the general population show that when racial/ethnic minorities are offered telehealth, they are as likely as the white population to utilize it [28]. The data were obtained in the middle of the pandemic, so we are unable to discern if there were group differences in the rate of uptake as the pandemic progressed.
The SoC1 responses identified language barriers as a challenge to telehealth, which may explain the lower utilization in Hispanic/Latino PwCF. Including an interpreter synchronously as part of the multidisciplinary telehealth visit may increase access to telehealth in the Hispanic/Latino group. Other reasons for the apparent access disparity to telehealth for PwCF from racial/ethnic minority, cannot be determined from our surveys; it is important, in the interest of equity, to understand if these differences are related to decreased interest or lack of opportunity to telehealth care.
Care programs were split on the merits of telehealth for vulnerable populations: whereas half indicated that telehealth improved access to care another half indicated that telehealth limited access to care for these populations. These results may suffer from provider perception and personal bias. It is also noteworthy that PwCF from minority groups and who reported financial difficulties were more likely to think that their questions were not fully answered during telehealth visits, a perception that calls for further investigation. Overall, the different perceptions and experiences of the vulnerable populations with CF with telehealth, present important challenges and opportunities for self-examination. Previous studies on implicit bias in health care have found evidence of racial/ethnic and class bias among health care providers. Implicit bias influenced patient-provider interactions, treatment decisions, and patient health outcomes in the vulnerable populations [29,30]. Exploring implicit bias among providers may be important for reducing inequities in CF care.
We believe that important conclusions can be drawn from our data, but there are some weaknesses to our study. This study is limited by the relatively small number of respondents who represent racial/ethnic minorities. The proportion of minority PFSoC respondents was slightly lower than the proportion of minority patients in the CFFPR, so the total number of minority respondents was smaller than we would have liked. The PFSoC was intended for distribution to the general CF population, and an interest in comparing the experience of low SES and minority groups was developed after the survey had been distributed, no attempt was made to purposefully sample these groups and the PFSoC was distributed in English without a Spanish version.
5. Conclusion
PFSoC, SoC1, and program surveys identified differences in telehealth use and care perceptions by ethnicity, race, and socioeconomic characteristics. In order for telehealth to be part of an equitable CF care model, further studies are needed to better understand barriers and facilitators of telehealth use among PwCF from diverse ethnic, racial, and socioeconomic backgrounds.
CRediT author statement
All authors should have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Dana Albon: Supervision; Validation; Visualization; Roles/Writing - original draft; Writing - review & editing.
Aricca D. Van Citters: Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Roles/Writing - original draft; Writing - review & editing.
Thida Ong: Validation; Visualization; Roles/Writing - original draft; Writing - review & editing.
Olivia Dieni: Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Roles/Writing - original draft; Writing - review & editing.
Christopher Dowd: Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Roles/Writing - original draft; Writing - review & editing.
Anne Willis: Validation; Visualization; Roles/Writing - original draft; Writing - review & editing.
Kathryn A. Sabadosa: Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Roles/Writing - original draft; Writing - review & editing.
Peter Scalia: Validation; Visualization; Roles/Writing - original draft; Writing - review & editing.
Kimberly Reno: Validation; Visualization; Roles/Writing - original draft; Writing - review & editing.
Gabriela R. Oates: Validation; Visualization; Roles/Writing - original draft; Writing - review & editing.
Michael S. Schechter: Supervision; Validation; Visualization; Roles/Writing - original draft; Roles/Writing - review & editing.
Funding sources
This work was supported by the Cystic Fibrosis Foundation and a grant from the Cystic Fibrosis Foundation to A.V.C., P.S. at The Dartmouth Institute for Health Policy and Clinical Practice (NELSON20QI0).
Declaration of Competing Interest
While I received grant support from CFF and private pharmaceutical companies, I have no conflict of interest to report related to this manuscript.
Acknowledgement
We are grateful to the people with CF and families for their time to respond to our survey, especially during the challenges imposed by the COVID-19 pandemic. We thank the entire CF Care Center Network for their prompt responses to our request to complete two surveys while adapting to a rapidly changing care environment.
Footnotes
This paper is part of a Supplement supported by the Cystic Fibrosis Foundation.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jcf.2021.09.006.
Appendix. Supplementary materials
References
- 1.Dowd C, Van Citters AD, Dieni O, Willis A, Powell L, Sabadosa K. Design and methods for understanding the state of cystic fibrosis care amid the COVID-19 pandemic. J Cyst Fibros. 2021;20(S3):S3–S8. doi: 10.1016/j.jcf.2021.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McGarry ME, Williams WA, 2nd, McColley SA. The demographics of adverse outcomes in cystic fibrosis. Pediatr Pulmonol. 2019;54(Suppl 3):S74–S83. doi: 10.1002/ppul.24434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McGarry ME, Neuhaus JM, Nielson DW, Ly NP. Regional variations in longitudinal pulmonary function: a comparison of Hispanic and non-Hispanic subjects with cystic fibrosis in the United States. Pediatr Pulmonol. 2019;54(9):1382–1390. doi: 10.1002/ppul.24377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson B, Ngueyep R, Schechter MS, Serban N, Swann J. Does distance to a cystic fibrosis center impact health outcomes? Pediatr Pulmonol. 2018;53(3):284–292. doi: 10.1002/ppul.23940. [DOI] [PubMed] [Google Scholar]
- 5.Schechter MS, Margolis PA. Relationship between socioeconomic status and disease severity in cystic fibrosis. J Pediatrics. 1998;132(2):260–264. doi: 10.1016/s0022-3476(98)70442-1. [DOI] [PubMed] [Google Scholar]
- 6.O'Connor GT, Quinton HB, Kneeland T, Kahn R, Lever T, Maddock J, et al. Median household income and mortality rate in cystic fibrosis. Pediatrics. 2003;111(4 Pt 1):e333–e339. doi: 10.1542/peds.111.4.e333. [DOI] [PubMed] [Google Scholar]
- 7.Ong T, Schechter M, Yang J, Peng L, Emerson J, Gibson RL, et al. Socioeconomic Status, Smoke Exposure, and Health Outcomes in Young Children With Cystic Fibrosis. Pediatrics. 2017;139(2) doi: 10.1542/peds.2016-2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oates GR, Stepanikova I, Gamble S, Gutierrez HH, Harris WT. Adherence to airway clearance therapy in pediatric cystic fibrosis: Socioeconomic factors and respiratory outcomes. Pediatr Pulmonol. 2015;50(12):1244–1252. doi: 10.1002/ppul.23317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balmer DF, Schall JI, Stallings VA. Social disadvantage predicts growth outcomes in preadolescent children with cystic fibrosis. J Cyst Fibros. 2008;7(6):543–550. doi: 10.1016/j.jcf.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 10.Quon BS, Psoter K, Mayer-Hamblett N, Aitken ML, Li CI, Goss CH. Disparities in access to lung transplantation for patients with cystic fibrosis by socioeconomic status. Am J Respir Crit Care Med. 2012;186(10):1008–1013. doi: 10.1164/rccm.201205-0949OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xesfingi S, Vozikis A. Patient satisfaction with the healthcare system: Assessing the impact of socio-economic and healthcare provision factors. BMC Health Serv Res. 2016;16:94. doi: 10.1186/s12913-016-1327-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Becker G, Newsom E. Socioeconomic status and dissatisfaction with health care among chronically ill African Americans. Am J Public Health. 2003;93(5):742–748. doi: 10.2105/ajph.93.5.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McMaughan DJ, Oloruntoba O, Smith ML. Socioeconomic Status and Access to Healthcare: Interrelated Drivers for Healthy Aging. Front Public Health. 2020;8:231. doi: 10.3389/fpubh.2020.00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.George S, Hamilton A, Baker RS. How Do Low-Income Urban African Americans and Latinos Feel about Telemedicine? A Diffusion of Innovation Analysis. Int J Telemed Appl. 2012;2012 doi: 10.1155/2012/715194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramirez AV, Ojeaga M, Espinoza V, Hensler B, Honrubia V. Telemedicine in Minority and Socioeconomically Disadvantaged Communities Amidst COVID-19 Pandemic. Otolaryngol Head Neck Surg. 2021;164(1):91–92. doi: 10.1177/0194599820947667. [DOI] [PubMed] [Google Scholar]
- 16.Lin NY, Ramsey RR, Miller JL, McDowell KM, Zhang N, Hommel K, et al. Telehealth delivery of adherence and medication management system improves outcomes in inner-city children with asthma. Pediatr Pulmonol. 2020;55(4):858–865. doi: 10.1002/ppul.24623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cystic Fibrosis Foundation . Bethesda; Maryland: 2020. Cystic Fibrosis Foundation Patient Registry: 2019 Annual Data Report to the Center Directors. [Google Scholar]
- 18.Schechter MS, McColley SA, Silva S, Haselkorn T, Konstan MW, Wagener JS, et al. Association of socioeconomic status with the use of chronic therapies and healthcare utilization in children with cystic fibrosis. The Journal of pediatrics. 2009;155(5):634–639. doi: 10.1016/j.jpeds.2009.04.059. e1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schechter MS. Non-genetic influences on cystic fibrosis lung disease: the role of sociodemographic characteristics, environmental exposures, and healthcare interventions. Semin Respir Crit Care Med. 2003;24(6):639–652. doi: 10.1055/s-2004-815660. [DOI] [PubMed] [Google Scholar]
- 20.Schechter MS, Shelton BJ, Margolis PA, Fitzsimmons SC. The association of socioeconomic status with outcomes in cystic fibrosis patients in the United States. Am J Respir Crit Care Med. 2001;163(6):1331–1337. doi: 10.1164/ajrccm.163.6.9912100. [DOI] [PubMed] [Google Scholar]
- 21.Oates GR, Baker E, Rowe SM, Gutierrez HH, Schechter MS, Morgan W, et al. Tobacco smoke exposure and socioeconomic factors are independent predictors of pulmonary decline in pediatric cystic fibrosis. J Cyst Fibros. 2020;19(5):783–790. doi: 10.1016/j.jcf.2020.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oates GR, Harris WT, Rowe SM, Solomon GM, Dey S, Zhu A, et al. Area Deprivation as a Risk Factor for Methicillin-resistant Staphylococcus aureus Infection in Pediatric Cystic Fibrosis. Pediatr Infect Dis J. 2019;38(11) doi: 10.1097/INF.0000000000002419. e285-e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quittner AL, Schechter MS, Rasouliyan L, Haselkorn T, Pasta DJ, Wagener JS. Impact of socioeconomic status, race, and ethnicity on quality of life in patients with cystic fibrosis in the United States. Chest. 2010;137(3):642–650. doi: 10.1378/chest.09-0345. [DOI] [PubMed] [Google Scholar]
- 24.Homa K, Sabadosa KA, Marrow LC, Marshall BC. Experience of care from perspective of individulas with cystic fibrosis and families: results of 70 CF Foundation accredited programs in USA. J Cyst Fibros. 2015;14(4):515–522. doi: 10.1016/j.jcf.2014.12.011. [DOI] [PubMed] [Google Scholar]
- 25.https://www.cff.org/Get-Involved/Connect/Community-Voice
- 26.Elwyn G, Barr PJ, Grande SW, Thompson R, Walsh T, Ozanne EM. Developing CollaboRATE: a fast and frugal patient-reported measure of shared decision making in clinical encounters. Patient Educ Counseling. 2013;93(1):102–107. doi: 10.1016/j.pec.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 27.Eberly L.A., Kallan M.J., Julien H.M., Haynes N., Khatana S., Nathan A.S., Snider C., Chokshi N.P., Eneanya N.D., Takvorian S.U., Anastos-Wallen R., Chaiyachati K., Ambrose M., O'Quinn R., Seigerman M., Goldberg L.R., Leri D., Choi K., Gitelman Y., Kolansky D.M., …, Adusumalli S. Patient Characteristics Associated With Telemedicine Access for Primary and Specialty Ambulatory Care During the COVID-19 Pandemic. JAMA network open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Graetz I, Gordon N, Fung V, Hamity C, Reed ME. The Digital Divide and Patient Portals: Internet Access Explained Differences in Patient Portal Use for Secure Messaging by Age, Race, and Income. Medical care. 2016;54(8):772–779. doi: 10.1097/MLR.0000000000000560. [DOI] [PubMed] [Google Scholar]
- 29.Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105(12):e60–e76. doi: 10.2105/AJPH.2015.302903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haider AH, Schneider EB, Sriram N, Dossick DS, Scott VK, Swoboda SM, Losonczy L, Haut ER, Efron DT, Pronovost PJ, Freischlag JA, Lipsett PA, 3rd Cornwell EE, MacKenzie EJ, Cooper LA. Unconscious race and class bias: its association with decision making by trauma and acute care surgeons. J Trauma Acute Care Surg. 2014;77(3):409–416. doi: 10.1097/TA.0000000000000392. PMID: 25159243. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.