Abstract
The optimum amounts and types of leisure-time physical activity (LTPA) for cardiovascular disease (CVD) prevention among Chinese retired adults are unclear. The prospective study enrolled 26,584 participants (mean age [SD]: 63.3 [8.4]) without baseline disease from the Dongfeng-Tongji cohort in 2013. Cox-proportional hazard models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs). During a mean 5.0 (1.5) years of follow-up, 5704 incident CVD cases were documented. Compared with less than 7.5 metabolic equivalent of task-hours per week (MET-hours/week) of LTPA, participating LTPA for 22.5–37.5 MET-hours/week, which was equivalent to 3 to 5 times the world health organization (WHO) recommended minimum, was associated with a 18% (95% CI 9 to 25%) lower CVD risk; however, no significant additional benefit was gained when exceeding 37.5 MET-hours/week. Each log10 increment of MET-hours/week in square dancing and cycling was associated with 11% (95% CI 2 to 20%) and 32% (95% CI 21 to 41%), respectively, lower risk of incident CVD. In Chinese retired adults, higher LTPA levels were associated with lower CVD risk, with a benefit threshold at 3 to 5 times the recommended physical activity minimum. Encouraging participation in square dancing and cycling might gain favourable cardiovascular benefits.
Subject terms: Cardiology, Risk factors, Disease prevention, Epidemiology
Introduction
Physical inactivity is one of the major modifiable risk factors for cardiovascular disease (CVD)1,2, the leading cause of morbidity and mortality globally3,4. The World Health Organization (WHO) recommends every adult to maintain a minimum of 150 min of moderate-intensity or 75 min of vigorous-intensity activity per week, which is equivalent to 7.5 weekly metabolic equivalent of task-hours ([MET]-hours/week) of physical activity (PA), to experience health benefits5. However, almost one-fourth of the adults worldwide did not meet such recommendations6, and even more failed to achieve these levels in post-retirement population7,8. In addition to the declining physical function with advancing age9,10, pattern and amount of PA in retired adults differ greatly from that in their working counterparts, mainly characterized by a marked reduction in occupational and transportation domains of PA and higher participation in leisure-time physical activity (LTPA)7,11. Thus, identifying the optimal amount and type of LTPA for retired adults has become a key priority to guide future recommendation and optimize CVD prevention.
Cumulative studies from western countries have suggested that recreational activities might be more effective to offset the risks of CVD in older adults12–14. However, the prospective evidence remained limited regarding the association between incident CVD and recreational activities with Chinese characteristics, such as square dancing, a popular activity enjoyed widespread popularity among middle-aged and older Chinese15,16. Furthermore, the prolonged sedentary time in retired adults during the past decades is increasingly striking, which also contributes to an elevated risk of CVD17–19. Recent prospective study reported that more activity might attenuate the detrimental association of prolonged sedentary time with CVD20. However, most of the previous studies assessed merely common sedentary behaviour such as watching TV21,22; it remains unclear about the relation between Mahjong and health status among Chinese23.
In the present study of retired adults from the Dongfeng-Tongji cohort, we examined the association of LTPA with the risk of incident CVD and its major components. We also evaluated the dose–response associations of CVD with total and different types of LTPA separately. Additionally, we investigated the association of combined categories of sedentary behaviour and LTPA with the risk of CVD.
Results
Baseline characteristics of study participants by LTPA levels
Of the 26,584 participants (43% male and 57% female; mean [SD] age: 63.3 [8.4] years) included in the present study, the median LTPA was 21 MET-hours/week (interquartile range, 11.3–42 MET-hours/week), and 18.2% of the participants (n = 4832) did not meet the WHO recommended PA minimum (< 7.5 MET-hours/week) at baseline. In general, the most common type of leisure activity performed by retired adults was walking (77.7%), followed by square dancing (10.8%), jogging (5.0%) and cycling (4.7%). Table 1 showed the baseline characteristics of study participants according to LTPA categories. Comparing with inactive participants, those with higher levels of LTPA were tended to be educated more, smoke less, drink more, eat more fruit and vegetables, have lower BMI, and have less sedentary time (P < 0.01).
Table 1.
Baseline characteristics of study participants according to leisure-time physical activity.
| Characteristics | Leisure-time physical activity, MET-hours/week† | P value‡ | |||
|---|---|---|---|---|---|
| < 7.5 | 7.5 to < 22.5 | 22.5 to < 37.5 | ≥ 37.5 | ||
| Participants, n | 4832 | 8600 | 4329 | 8823 | |
| Male, n (%) | 1904 (39.4) | 3578 (41.6) | 1855 (42.9) | 4143 (47.0) | < 0.001 |
| Age, years | 62.9 (9.2) | 63.7 (8.4) | 63.2 (8.2) | 63.3 (7.9) | < 0.001 |
| Education, n (%) | < 0.001 | ||||
| Primary school or below | 1072 (22.2) | 1703 (19.8) | 882 (20.4) | 1729 (19.6) | |
| Middle school | 1773 (36.7) | 3105 (36.1) | 1561 (36.1) | 3398 (38.5) | |
| High school or beyond | 1954 (40.4) | 3745 (43.6) | 1863 (43.0) | 3650 (41.4) | |
| Smoking status, n (%) | < 0.001 | ||||
| Never | 3491 (72.3) | 6303 (73.3) | 3153 (72.8) | 6338 (71.8) | |
| Former | 363 (7.5) | 840 (9.8) | 463 (10.7) | 1001 (11.4) | |
| Current | 969 (20.1) | 1437 (16.7) | 703 (16.2) | 1465 (16.6) | |
| Drinking status, n (%) | |||||
| Never | 3535 (73.2) | 6104 (71.0) | 3022 (69.8) | 5886 (66.7) | < 0.001 |
| Former | 181 (3.8) | 372 (4.3) | 211 (4.9) | 458 (5.2) | |
| Current | 1102 (22.8) | 2106 (24.5) | 1082 (25.0) | 2464 (27.9) | |
| Consumption of foods (≥ 5 times/week, %) | |||||
| Meat | 1941 (40.2) | 3432 (39.9) | 1690 (39.0) | 3549 (40.2) | 0.622 |
| Fruits | 2456 (50.8) | 4926 (57.3) | 2506 (57.9) | 5465 (61.9) | < 0.001 |
| Vegetables | 4568 (94.5) | 8269 (96.2) | 4160 (96.1) | 8487 (96.2) | < 0.001 |
| BMI, kg/m2 | 24.1 (3.3) | 24.1 (3.2) | 23.9 (3.1) | 24.0 (3.0) | 0.002 |
| Hypertension, yes (%) | 2538 (52.5) | 4920 (57.2) | 2388 (55.2) | 5057 (57.3) | < 0.001 |
| Hyperlipidemia, yes (%) | 1782 (36.9) | 3405 (39.6) | 1674 (38.7) | 3328 (37.7) | 0.008 |
| Diabetes, yes (%) | 731 (15.1) | 1534 (17.8) | 683 (15.8) | 1468 (16.6) | < 0.001 |
| Family history of CVD, n (%) | 607 (12.6) | 1128 (13.1) | 571 (13.2) | 1168 (13.2) | 0.708 |
| LTPA (MET-hours/week) | 1.4 (2.3) | 16.6 (4.7) | 30.0 (3.9) | 67.3 (37.0) | < 0.001 |
| Total sedentary time (hours/week) | 23.7 (15.1) | 22.3 (12.2) | 22.5 (12.2) | 22.3 (12.0) | < 0.001 |
| Screen activities, (hours/week) | 20.6 (12.9) | 19.6 (10.3) | 20.0 (10.6) | 19.6 (10.1) | < 0.001 |
| Playing Mahjong, (hours/week) | 3.1 (7.4) | 2.8 (6.5) | 2.6 (6.1) | 2.7 (6.4) | < 0.001 |
BMI, body mass index; MET, metabolic equivalent of task.
Data are means (SD) for continuous variables or number (percentages) for categorical variables. Missing data were 149, 58, 61, 2814, 264, 301, 224, 230, 26 and 241 for education, smoking status, drinking status, BMI, meat, fruits, vegetables, Mahjong, TV and total sedentary time.
†< 7.5, 7.5–22.5, 22.5–37.5, and ≥ 37.5 MET-hours/week represented < 1, 1–3, 3–5, and ≥ 5 times of the minimum recommended LTPA level, respectively.
‡P values were derived from one-way analysis of variance (ANOVA) for continuous variables, and Chi-square test for the categorical variables.
Association of LTPA with incident CVD
During a mean 5.0 (1.5) years of follow-up, we documented 5704 incident CVD cases, including 4659 incident CHD cases and 1045 incident stroke cases. Table 2 presented the association between LTPA and incident CVD. Compared with participants reporting LTPA less than the recommended minimum of 7.5 MET-hours/week, an 18% lower risk (HR, 0.82 [95% CI 0.75 to 0.91]) was seen for those with 3 to 5 times the recommended minimum (22.5–37.5 MET-hours/week); however, no significant additional benefit was gained when exceeding 5 times the recommended minimum (> 37.5 MET-hours/week; HR, 0.81 [95% CI 0.73 to 0.90]). The adjusted HRs (95% CIs) for CVD across categories of LTPA (7.5 to ≤ 22.5, 22.5 to ≤ 37.5, > 37.5 MET-hours/week) were 0.93 (0.86 to 1.01), 0.82 (0.75 to 0.91) and 0.81 (0.73 to 0.90), respectively (Ptrend < 0.001). Similar associations were observed for both CHD (Ptrend = 0.006) and stroke (Ptrend = 0.001). Sensitivity analysis by extended adjustment or further exclusions did not appreciably alter the association (Supplementary Table S1 online). In stratified analysis, we found that the result was more obvious in male (HR 0.80 [95%CI 0.73 to 0.87]; Pinteraction = 0.02); and the cardiovascular benefits were consistent across age, education, smoking status, drinking status, BMI, hypertension, hyperlipidemia and diabetes. (Pinteraction > 0.05; Supplementary Fig. S1 online).
Table 2.
The association of leisure-time physical activity with cardiovascular disease.
| Leisure-time physical activity, MET-hours/week∗ | P trend | ||||
|---|---|---|---|---|---|
| < 7.5 | 7.5 to < 22.5 | 22.5 to < 37.5 | ≥ 37.5 | ||
| Incident CVD | |||||
| Cases/person years | 1112/23,581 | 1939/42,539 | 857/21,780 | 1796/44,495 | |
| Model 1† | Ref. | 0.93 (0.87 to 1.00) | 0.82 (0.75 to 0.90) | 0.84 (0.78 to 0.91) | < 0.001 |
| Model 2‡ | Ref. | 0.93 (0.86 to 1.01) | 0.82 (0.75 to 0.91) | 0.81 (0.73 to 0.90) | < 0.001 |
| Incident CHD | |||||
| Cases/person years | 876/24,079 | 1585/43,352 | 702/22,132 | 1496/45,211 | |
| Model 1 | Ref. | 0.98 (0.90 to 1.06) | 0.87 (0.79 to 0.96) | 0.91 (0.84 to 0.99) | 0.010 |
| Model 2 | Ref. | 0.97 (0.89 to 1.05) | 0.86 (0.77 to 0.96) | 0.86 (0.77 to 0.97) | 0.006 |
| Incident stroke | |||||
| Cases/person years | 236/25,744 | 354/46,648 | 155/23,653 | 300/48,344 | |
| Model 1 | Ref. | 0.78 (0.67 to 0.92) | 0.69 (0.56 to 0.85) | 0.64 (0.54 to 0.76) | < 0.001 |
| Model 2 | Ref. | 0.81 (0.68 to 0.97) | 0.72 (0.58 to 0.90) | 0.65 (0.50 to 0.83) | 0.001 |
∗< 7.5, 7.5–22.5, 22.5–37.5, and ≥ 37.5 MET-hours/week represented < 1, 1–3, 3–5, and ≥ 5 times of the minimum recommended LTPA level, respectively.
†Adjusted for age and sex.
‡Additionally adjusted for education, smoking status, alcohol intake, consumption of food (meat, vegetables, and fruit), hypertension, hyperlipidemia, diabetes, BMI, MET-hours/week, total sedentary time, and family history of CVD.
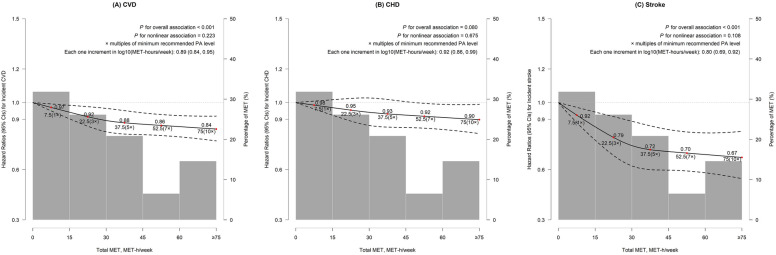
Cubic spline analysis showed that any level of LTPA was associated with significantly lower risks of CVD and stroke (PCVD < 0.001, Fig. 1A; Pstroke < 0.001, Fig. 1C). Each one increment in log10 (MET-hours/week) was associated with 11%, 8%, and 20% lower risks of CVD (HR 0.89 [95% CI 0.84 to 0.95]), CHD (HR, 0.92 [95% CI 0.86 to 0.99]), and stroke (HR 0.80 [95% CI 0.69 to 0.92]), respectively (Fig. 1). Compared with no baseline LTPA, the most rapid decrease in CVD risk was seen before 3 times the WHO recommended minimum of PA. For total LTPA, the risks decreased by 8% for CVD (95% CI 2 to 14%) and 21% for stroke (95% CI 8 to 32%), respectively at 3 times the recommended minimum.
Figure 1.
Adjusted hazard ratios for CVD, stroke and CHD according to levels of leisure-time physical activity. (A) Association between leisure-time physical activity and incident CVD. (B) Association between leisure-time physical activity and incident CHD. (C) Association between leisure-time physical activity and incident stroke. The multivariable models were adjusted for age, sex, education, smoking status, alcohol intake, consumption of food (meat, vegetables, and fruit), hypertension, hyperlipidemia, diabetes, BMI, total sedentary time, and family history of CVD.
Association between different types of LTPA and incident CVD
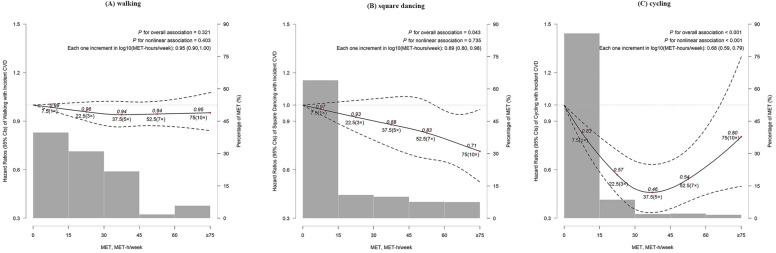
When examining specific types of LTPA, a monotonic decrease in CVD risk was seen with increasing levels of square dancing (Each one increment in log10 [MET-hours/week]: HR, 0.89 [95% CI 0.80 to 0.98]; Fig. 2B), and such association was mainly restricted to female (P = 0.014; Supplementary Fig. S2 online). However, For cycling, we identified a U-shaped curve for the association, with the maximum observed cardiovascular benefit accrued with 37.5 MET-hours/week, equivalent to about 9 h cycling per week (HR, 0.46 [95% CI 0.33 to 0.63]); Fig. 2C). No significant association was seen for other types of LTPA (Fig. 2 and Supplementary Fig. S3 online).
Figure 2.
Adjusted hazard ratios for CVD according to levels of different types of leisure-time physical activity. (A) Association between walking and incident CVD. (B) Association between square dancing and incident CVD. (C) Association between cycling and incident CVD. The multivariable models were adjusted for age, sex, education, smoking status, alcohol intake, consumption of food (meat, vegetables, and fruit), hypertension, hyperlipidemia, diabetes, BMI, total sedentary time, other LTPA, and family history of CVD.
Interaction between LTPA and sedentary
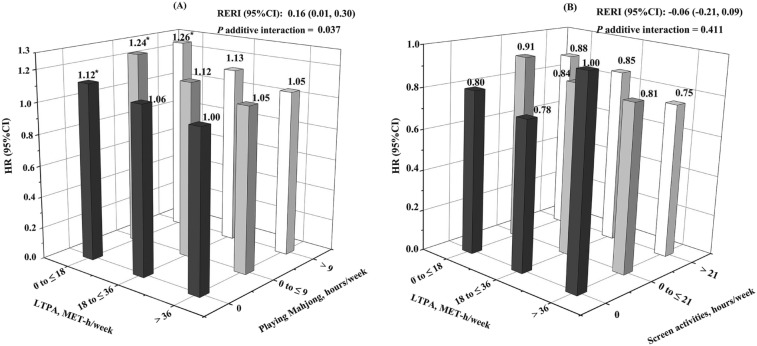
Participants reported prolonged time spent playing Mahjong have a significantly higher risk of incident CVD in comparison with those not playing (HR comparing extreme categories, 1.09 [95% CI 1.00 to1.18]; Ptrend = 0.022), whereas no significant association was observed for screen activities (HR comparing extreme categories, 0.98 [95% CI 0.81 to1.20]; Supplementary Table S2 online). In addition, our findings showed significant additive interactions of LTPA and playing Mahjong for incident CVD (Padditive interaction = 0.037; Fig. 3A), no significance was found for screen activities (Padditive interaction = 0.411; Fig. 3B). Compared with the most active participants (i.e., those with more than 36 MET-hours/week), those in the bottom LTPA tertile had a significantly higher risk of CVD, regardless of time spent playing Mahjong. No such association was seen for screen activities.
Figure 3.
The joint effect of LTPA and sedentary behavior on incident CVD. (A) The joint effect of LTPA and Mahjong playing on incident CVD. (B) The joint effect of LTPA and screen activities on incident CVD. The multivariable models were adjusted for age, sex, education, smoking status, alcohol intake, consumption of food (meat, vegetables, and fruit), hypertension, hyperlipidemia, diabetes, BMI, MET-hours/week, and family history of CVD. *P < 0.05. †The number was 26,354 for Mahjong and incident CVD analysis; the number was 26,558 for screen activities and incident CVD analysis. ‡The hazard ratios (95% CI) from the most active to the least active group were: 1 (reference), 1.06 (1.00 to 1.16), 1.12 (1.01 to 1.24), 1.05 (0.90 to 1.21), 1.12 (0.96 to 1.30), 1.24 (1.07 to 1.44), 1.05 (0.90 to 1.21), 1.13 (0.97 to 1.32), 1.26 (1.08 to 1.47), respectively, in (A). ¶The hazard ratios (95% CI) from the most active to the least active group were: 1 (reference), 0.78 (0.45 to 1.35), 0.80 (0.51 to 1.25), 0.81 (0.57 to 1.14), 0.84 (0.59 to 1.19), 0.91 (0.64 to 1.30), 0.75 (0.53 to 1.07), 0.85 (0.60 to 1.22), 0.88 (0.61 to 1.25), respectively, in (B).
Discussion
In this prospective study of Chinese retired adults, our results supported that meeting the WHO recommended minimum was associated with significantly lower CVD risk and further suggested the optimal benefit by reaching 3 to 5 times the recommended minimum. Encouraging retired adults to participate in square dancing and cycling might gain favourable cardiovascular benefits. Interestingly, we found that those with high LTPA level might mitigate the excess risk of CVD associated with sedentary behaviour, particularly playing Mahjong.
Our finding of reduced CVD risk associated with higher LTPA level was consistent with previous studies24–28. A historically prospective cohort study of 416,175 healthy individuals from Taiwan found that, compared with inactive individuals, those who were meeting PA recommendations had a 32% lower risk of CVD mortality (HR, 0.68 [95% CI 0.61 to 0.76])29. A pooled analysis (661,137 participants, about 14.2 years follow-up) found the benefit threshold of a 42% lower risk of CVD mortality (HR, 0.58 [95% CI 0.56 to 0.61]) with LTPA of 3 to 5 times the recommended minimum (22.5–40.0 MET-hours/week) compared with no LTPA30. Furthermore, another study of 88,140 US adults indicated that no additional cardiovascular health benefit was found when doing more than 10 times the recommended LTPA31. Despite focusing on working adults, these studies investigated only fatal CVD, and the present study of retired adults further extended previous findings by showing appreciable benefits related to incident CVD when exceeding the WHO recommendations. The beneficial effect in male might because that the LTPA level was higher than that in female (mean [SD]: 35 [36] in male and 31 [32] in female; P < 0.001). The relatively lower risk of stroke associated with LTPA observed in our study was in line with the effect of walking in the cohort study with 73,265 participants32 and another Japanese study with 74,913 participants25, which might be due to the better improvement of cerebral blood flow and perfusion through LTPA33.
The interesting finding was that square dancing was associated with a lower CVD risk. A cross-sectional study of 1944 adults in China found a 30% lower prevalence of CHD among adults with moderate or high frequency in walking or square dancing34. To date, only one prospective cohort study of 48,390 British adults, reported that dancing was associated with a 46% lower risk of cardiovascular mortality during a mean of 9.7 years of follow-up35. The present study found that a monotonic decrease in CVD risk with increasing levels of square dancing. Despite the different outcomes (CVD mortality versus incidence) investigated, the lacked consistency in the magnitude of CVD benefits could be interpreted by the between-racial differences in intensity of dance performed in China and western countries. Square dancing, a popular LTPA type in China, can be easily accepted by low-income people36. The superior benefits of square dancing over other types of leisure activity may be due to the lessened daily mental stress through its direct social and entertaining components37. To our knowledge, the present study was the first prospective study to explore the association between square dancing and incident CVD among retired adults, suggesting that promoting participation in this new kind of leisure activity might be a prioritized strategy for CVD prevention. In addition, the benefit of cycling was similar with the results in UK biobank, which might derive from the relatively higher intensity of cycling38.
Notably, this study firstly identified that a higher risk of CVD among retired adults who played Mahjong during leisure times, and found that exceeding 36 MET-hours/week of LTPA, which was roughly equivalent to 8 h/week of moderate-intensity PA, could eliminate the adverse effect of playing Mahjong. In line with our finding, a recent prospective study of 149,077 participants identified elimination of the adverse sitting effects in the group with over 35.5 MET-hours/week of PA39. Similarly, a harmonized meta-analysis of over 1 million individuals also found that 7–9 h of moderate-intensity PA per week might eliminate the elevated mortality risks associated with prolonged sitting time40. Moreover, we observed that the effect of playing mahjong on CVD incidence seemed to be stronger in magnitude than that in screen activities. It is plausible that playing mahjong typically occurs in the card room, which might be accompanied by high exposure of second-hand smoke, thus increasing CVD risk41. These findings together highlight the importance of active participation in LTPA in CVD prevention, especially among those with prolonged sedentary time.
The major strengths of the present study are the prospective design, high response rates for baseline and follow-up surveys, and inclusion of participants after retirement, which minimizes confounding from other domains of PA including occupation and transportation. To our best knowledge, this is the first prospective study reported the inverse association of square dancing with incident CVD among Chinese retired adults. The present study had certain limitations. First, as with most large population studies, information of LTPA in the present study was self-reported at baseline, and the LTPA change during the follow-up period was not accounted. However, misclassification might be random and thus would bias the association towards the null42. Second, the possibility of reverse causality cannot be completely ruled out in the present study43; however, we excluded CVD and cancer at baseline, and CVD cases occurring during the first year of follow-up to address the issue of reverse causation. Finally, despite carefully controlling for a variety of covariates, residual confounding remains possible.
Conclusions
Higher LTPA levels were associated with a lower risk of CVD, a benefit threshold for CVD prevention was achieved at 3 to 5 times the recommended PA minimum. Encouraging retired adults to participate in square dancing and cycling might gain favourable cardiovascular benefits. These data will be informative for future updates for guidelines with respect to the appropriate amount and type of leisure activity for CVD prevention.
Methods
Study population
The present study was based on the Dongfeng-Tongji (DFTJ) cohort, which has been reported previously44. Briefly, the DFTJ cohort is an ongoing prospective cohort in Shiyan, Hubei, China, which was established in 2008 and recruited retired employees of the Dongfeng Motor Corporation (DMC) quinquennially. The present study enrolled 38,295 participants from the survey from April to October 2013, and baseline information of whom was collected by questionnaire and physical examination. After excluding 10,254 participants with coronary heart disease (CHD, n = 6457), stroke (n = 2406), severely abnormal electrocardiogram (n = 838) and cancer (n = 2686) in 2013, 1402 participants with missing data for LTPA and 55 participants reported implausible information on LTPA, and leaved 26,584 participants in the final analysis. The flowchart of study population was presented in Supplementary Fig. S4 online.
Assessment of leisure-time physical activity and sedentary behaviour
LTPA and sedentary behaviour were assessed through the questionnaire in 2013. For those reporting participation in LTPA at least twice per month, we multiplied the MET intensity45,46 by frequency and time spent on this activity and summed across activities to estimate overall LTPA energy expenditure in MET-hours/week. Detailed information was listed in Supplementary Table S3 and eMethods online.
Assessment of covariates
Covariates comprised age, sex (male/female), education (primary or below, middle, high school or beyond), body mass index (BMI), smoking status (current, former, never), alcohol intake status (current, former, never), hypertension (yes/no), hyperlipidemia (yes/no), diabetes (yes/no), consumption frequency of meat, vegetables, fruit (≥ 5 times/week), LTPA (MET-hours/week), total sedentary time (hours/week) and family history of CVD (yes/no), which were measured at baseline. Further details on the assessment of covariates are provided in eMethods.
Ascertainment of outcome
The diagnosis of CVD was based on International Classification of Disease (ICD) codes of the World Health Organization (10th revision) by clinicians of Sinopharm Dongfeng General Hospital through medical insurance system and the medical record reviews47. The outcome of interest in the present study was incident CVD, including CHD and stroke48 that occurred from baseline survey until December 31, 2018. Incident CHD was defined as the first hospital admission with an occurrence of angina pectoris (ICD-10 code I20), acute myocardial infarction (AMI, I21), subsequent myocardial infarction (I22), other forms of acute (I24) or chronic (I25) heart disease, percutaneous transluminal coronary angioplasty or coronary artery bypass graft, and cardiac arrest (I46) or death with CHD (I20-I25) as the underlying cause during follow-up49. Incident stroke (I60-I61, I63-I64, I69.0-I69.1, and I69.3-I69.4) was defined as the first sudden or rapid onset of a typical neurological deficit caused by vascular origin over 24 h or until death47.
Statistical analysis
Because of the skewed distribution of calculated MET-hours/week, data of LTPA was logarithmically transformed before statistical analysis (log10 [MET-hours/week]). We also created four categories for calculated MET-hours/week: < 7.5, 7.5 to < 22.5, 22.5 to < 37.5, ≥ 37.5 MET-hours/week, to reflect multiples of the 2010 PA recommendations from WHO, equivalent to insufficient LTPA, 1–3 times, 3–5 times, and 5 or more times the minimum recommended level5,30. Cox-proportional hazard models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the association of LTPA with the risk of incident CVD with adjustments for age and sex in model 1, and additionally adjusted for education, BMI, smoking status, alcohol intake status, hypertension, hyperlipidemia, diabetes, consumption of food (meat, vegetables, fruit), MET-hours/week, total sedentary time and family history of CVD in model 2. Test for linear trends across categories of LTPA was derived by assigning the median value for each category.
The restricted cubic spline was used to delineate the dose–response relationship of LTPA levels with incident CVD, CHD and stroke. Those reporting more than the 90th percentile of total LTPA were assigned a value of 75 MET-hours/week (n = 2316)50. In addition, we further examined whether the dose–response association between LTPA and CVD risk differed across participants with different types of LTPA.
We also applied stratification analysis for association between LTPA and incident CVD according to several potential confounders at baseline. To evaluate the potential modification by subgroups, we used the Wald test for dichotomous variables and the likelihood ratio test for multi-level variables for interaction between LTPA and subgroups variable51. We also assessed the joint association of LTPA with sedentary behaviour by creating combined exposures, using those who were the most physically active (> 36 MET-hours/week of LTPA plus 0 h/week for Mahjong or 0 h/week for screen activities, respectively) as the reference group. The significance of additive interaction was indicated by a value of the relative excess risk due to interaction greater than zero52.
To test the robustness of results, we performed sensitivity analysis by extended adjustment for household activity, excluding participants reporting over 6 h of LTPA per day (n = 189), excluding participants retired 5 years before the mandatory age for retirement (n = 5882; 55 years for male and 50 years for female), or excluding CVD cases occurred during the first year of follow-up (n = 665).
All statistical analyses were performed using the SAS 9.4 software package (SAS Institute, Cary, North Carolina, USA).
Ethics approval and consent to participate
The study was approved by the Ethics Committee of School of Public Health, Tongji Medical College, Huazhong University of Science and Technology (2012-10). All participants provided written informed consent to partake in the study.
Consent for publication
All participants were consent for publication.
Supplementary Information
Acknowledgements
The chief acknowledgement is to the participants, the project staff, and the Sinopharm Dongfeng General Hospital for providing the electronic linkage to hospital admission data.
Author contributions
X.W.M., K.Y. and T.C.W. planned the study. X.W.M. and K.Y. carried out the statistical analyses, interpreted the data, and drafted the manuscript. P.P.L., R.D.N., W.D.L., H.T.C., H.G. and X.X.L. contributed to the data collection and data cleaning. Y.Y., H.D.Y., X.M.Z., M.A.H., G.L. and H.G. provided substantial scientific input in interpreting the results and revised drafts critically. All authors approved the final version for publication.
Funding
This work was supported by the National Key Program of Research and Development of China (2016YFC0900800), the National Natural Science Foundation of China (81930092), the Fundamental Research Funds for the Central Universities (2019kfyXMBZ015), and the 111 Project and the Program for Changjiang Scholars and Innovative Research Team in University.
Data availability
The data of this study are available from the corresponding author upon reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Xuanwen Mu and Kuai Yu.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-03475-6.
References
- 1.Young DR, et al. Sedentary behavior and cardiovascular morbidity and mortality: A science advisory from the American Heart Association. Circulation. 2016;134:e262–279. doi: 10.1161/CIR.0000000000000440. [DOI] [PubMed] [Google Scholar]
- 2.Bull FC, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020;54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2017 DALYs and HALE Collaborators Global, regional, and national disability-adjusted life-years (dalys) for 359 diseases and injuries and healthy life expectancy (hale) for 195 countries and territories, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1859–1922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Cardiovascular diseases (cvds). https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1.
- 5.World Health Organization. Global recommendations on physical activity for health., https://apps.who.int/iris/bitstream/handle/10665/44399/9789245599975_chi.pdf. [PubMed]
- 6.Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6:e1077–e1086. doi: 10.1016/S2214-109X(18)30357-7. [DOI] [PubMed] [Google Scholar]
- 7.Slingerland AS, et al. Aging, retirement, and changes in physical activity: Prospective cohort findings from the globe study. Am. J. Epidemiol. 2007;165:1356–1363. doi: 10.1093/aje/kwm053. [DOI] [PubMed] [Google Scholar]
- 8.Godfrey A, et al. The association between retirement and age on physical activity in older adults. Age Ageing. 2014;43:386–393. doi: 10.1093/ageing/aft168. [DOI] [PubMed] [Google Scholar]
- 9.Laukkanen P, Heikkinen E, Kauppinen M. Muscle strength and mobility as predictors of survival in 75–84-year-old people. Age Ageing. 1995;24:468–473. doi: 10.1093/ageing/24.6.468. [DOI] [PubMed] [Google Scholar]
- 10.Larsson L, et al. Sarcopenia: Aging-related loss of muscle mass and function. Physiol. Rev. 2019;99:427–511. doi: 10.1152/physrev.00061.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evenson KR, Rosamond WD, Cai J, Diez-Roux AV, Brancati FL. Influence of retirement on leisure-time physical activity: The atherosclerosis risk in communities study. Am. J. Epidemiol. 2002;155:692–699. doi: 10.1093/aje/155.8.692. [DOI] [PubMed] [Google Scholar]
- 12.Dhaliwal SS, Welborn TA, Howat PA. Recreational physical activity as an independent predictor of multivariable cardiovascular disease risk. PLoS ONE. 2013;8:e83435. doi: 10.1371/journal.pone.0083435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donneyong MM, Taylor KC, Kerber RA, Hornung CA, Scragg R. Is outdoor recreational activity an independent predictor of cardiovascular disease mortality—NHANES III? Nutr. Metab. Cardiovasc. Dis. 2016;26:735–742. doi: 10.1016/j.numecd.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Thomas IC, et al. Associations of recreational and non-recreational physical activity with coronary artery calcium density vs. volume and cardiovascular disease events: The multi-ethnic study of atherosclerosis. Eur. Heart J. Cardiovasc. Imaging. 2020;21:132–140. doi: 10.1093/ehjci/jez271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peng F, et al. Exploring factors influencing whether residents participate in square dancing using social cognitive theory: A cross-sectional survey in Chongqing, China. Medicine. 2020;99:e18685. doi: 10.1097/MD.0000000000018685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liao J, Chen S, Chen S, Yang YJ. Personal and social environmental correlates of square dancing habits in Chinese middle-aged and older adults living in communities. J. Aging Phys. Act. 2019;27:696–702. doi: 10.1123/japa.2018-0310. [DOI] [PubMed] [Google Scholar]
- 17.Touvier M, et al. Changes in leisure-time physical activity and sedentary behaviour at retirement: A prospective study in middle-aged French subjects. Int. J. Behav. Nutr. Phys. Act.. 2010;7:14. doi: 10.1186/1479-5868-7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eaton CB, et al. Sedentary lifestyle and risk of coronary heart disease in women. Med. Sci. Sports Exerc. 1995;27:1535–1539. [PubMed] [Google Scholar]
- 19.Pandey A, et al. Continuous dose-response association between sedentary time and risk for cardiovascular disease: A meta-analysis. JAMA Cardiol. 2016;1:575–583. doi: 10.1001/jamacardio.2016.1567. [DOI] [PubMed] [Google Scholar]
- 20.Chomistek AK, et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease: Results from the women's health initiative. J. Am. Coll. Cardiol. 2013;61:2346–2354. doi: 10.1016/j.jacc.2013.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ford ES, Caspersen CJ. Sedentary behaviour and cardiovascular disease: A review of prospective studies. Int. J. Epidemiol. 2012;41:1338–1353. doi: 10.1093/ije/dys078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Warren TY, et al. Sedentary behaviors increase risk of cardiovascular disease mortality in men. Med. Sci. Sports Exerc. 2010;42:879–885. doi: 10.1249/MSS.0b013e3181c3aa7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang R, et al. Melancholy or mahjong? Diversity, frequency, type, and rural-urban divide of social participation and depression in middle- and old-aged Chinese: A fixed-effects analysis. Soc. Sci. Med. 2019;238:112518. doi: 10.1016/j.socscimed.2019.112518. [DOI] [PubMed] [Google Scholar]
- 24.Bennett DA, et al. Association of physical activity with risk of major cardiovascular diseases in Chinese men and women. JAMA Cardiol. 2017;2:1349–1358. doi: 10.1001/jamacardio.2017.4069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kubota Y, Iso H, Yamagishi K, Sawada N, Tsugane S. Daily total physical activity and incident cardiovascular disease in Japanese men and women: Japan public health center-based prospective study. Circulation. 2017;135:1471–1473. doi: 10.1161/CIRCULATIONAHA.116.026557. [DOI] [PubMed] [Google Scholar]
- 26.Stewart RAH, et al. Physical activity and mortality in patients with stable coronary heart disease. J. Am. Coll. Cardiol. 2017;70:1689–1700. doi: 10.1016/j.jacc.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 27.Abbott RD, Rodriguez BL, Burchfiel CM, Curb JD. Physical activity in older middle-aged men and reduced risk of stroke: The Honolulu Heart Program. Am. J. Epidemiol. 1994;139:881–893. doi: 10.1093/oxfordjournals.aje.a117094. [DOI] [PubMed] [Google Scholar]
- 28.Kubota Y, Iso H, Yamagishi K, Sawada N, Tsugane S. Daily total physical activity and incident stroke: The Japan public health center-based prospective study. Stroke. 2017;48:1730–1736. doi: 10.1161/STROKEAHA.117.017560. [DOI] [PubMed] [Google Scholar]
- 29.Wen CP, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: A prospective cohort study. Lancet. 2011;378:1244–1253. doi: 10.1016/S0140-6736(11)60749-6. [DOI] [PubMed] [Google Scholar]
- 30.Arem H, et al. Leisure time physical activity and mortality: A detailed pooled analysis of the dose-response relationship. JAMA Intern. Med. 2015;175:959–967. doi: 10.1001/jamainternmed.2015.0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao M, Veeranki SP, Li S, Steffen LM, Xi B. Beneficial associations of low and large doses of leisure time physical activity with all-cause, cardiovascular disease and cancer mortality: A national cohort study of 88,140 US adults. Br. J. Sports Med. 2019;53:1405–1411. doi: 10.1136/bjsports-2018-099254. [DOI] [PubMed] [Google Scholar]
- 32.Noda H, et al. Walking and sports participation and mortality from coronary heart disease and stroke. J. Am. Coll. Cardiol. 2005;46:1761–1767. doi: 10.1016/j.jacc.2005.07.038. [DOI] [PubMed] [Google Scholar]
- 33.Schmidt W, Endres M, Dimeo F, Jungehulsing GJ. Train the vessel, gain the brain: Physical activity and vessel function and the impact on stroke prevention and outcome in cerebrovascular disease. Cerebrovasc. Dis. 2013;35:303–312. doi: 10.1159/000347061. [DOI] [PubMed] [Google Scholar]
- 34.Jia X, et al. Cardiovascular diseases in middle aged and older adults in China: The joint effects and mediation of different types of physical exercise and neighborhood greenness and walkability. Environ. Res. 2018;167:175–183. doi: 10.1016/j.envres.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 35.Merom D, Ding D, Stamatakis E. Dancing participation and cardiovascular disease mortality: A pooled analysis of 11 population-based British cohorts. Am. J. Prev. Med. 2016;50:756–760. doi: 10.1016/j.amepre.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 36.Zhang Y, Xie G, Huang J, Li S. A new leisure-time physical activity in China: Square dancing. Minerva Med. 2019;110:180–181. doi: 10.23736/S0026-4806.18.05932-3. [DOI] [PubMed] [Google Scholar]
- 37.Gao L, Zhang L, Qi H, Petridis L. Middle-aged female depression in perimenopausal period and square dance intervention. Psychiatr. Danub. 2016;28:372–378. [PubMed] [Google Scholar]
- 38.Celis-Morales CA, et al. Association between active commuting and incident cardiovascular disease, cancer, and mortality: Prospective cohort study. BMJ. 2017;357:j1456. doi: 10.1136/bmj.j1456. [DOI] [PubMed] [Google Scholar]
- 39.Stamatakis E, et al. Sitting time, physical activity, and risk of mortality in adults. J. Am. Coll. Cardiol. 2019;73:2062–2072. doi: 10.1016/j.jacc.2019.02.031. [DOI] [PubMed] [Google Scholar]
- 40.Ekelund U, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388:1302–1310. doi: 10.1016/S0140-6736(16)30370-1. [DOI] [PubMed] [Google Scholar]
- 41.Stillman F, et al. Second-hand tobacco smoke in public places in urban and rural China. Tob. Control. 2007;16:229–234. doi: 10.1136/tc.2006.018333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tanaka S, Tanaka S, Kawakami K. Methodological issues in observational studies and non-randomized controlled trials in oncology in the era of big data. Jpn. J. Clin. Oncol. 2015;45:323–327. doi: 10.1093/jjco/hyu220. [DOI] [PubMed] [Google Scholar]
- 43.Sattar N, Preiss D. Reverse causality in cardiovascular epidemiological research: More common than imagined? Circulation. 2017;135:2369–2372. doi: 10.1161/CIRCULATIONAHA.117.028307. [DOI] [PubMed] [Google Scholar]
- 44.Wang F, et al. Cohort profile: The Dongfeng-Tongji cohort study of retired workers. Int. J. Epidemiol. 2013;42:731–740. doi: 10.1093/ije/dys053. [DOI] [PubMed] [Google Scholar]
- 45.Ainsworth BE, et al. 2011 compendium of physical activities: A second update of codes and met values. Med. Sci. Sports Exerc. 2011;43:1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 46.Chen M, et al. Different physical activity subtypes and risk of metabolic syndrome in middle-aged and older Chinese people. PLoS ONE. 2013;8:e53258. doi: 10.1371/journal.pone.0053258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.World Health Organisation. International statistical classification of diseases and related health problems, 10th revision.
- 48.Israel, R. A. Wiley statsref: Statistics Reference Online.
- 49.Lai X, et al. Dose-response relationship between serum uric acid levels and risk of incident coronary heart disease in the Dongfeng-Tongji cohort. Int. J. Cardiol. 2016;224:299–304. doi: 10.1016/j.ijcard.2016.09.035. [DOI] [PubMed] [Google Scholar]
- 50.Chekroud SR, et al. Association between physical exercise and mental health in 1.2 million individuals in the USA between 2011 and 2015: A cross-sectional study. Lancet Psychiatry. 2018;5:739–746. doi: 10.1016/S2215-0366(18)30227-X. [DOI] [PubMed] [Google Scholar]
- 51.Meyer K. Factor-analytic models for genotype × environment type problems and structured covariance matrices. Genet. Sel. Evol. 2009;41:21. doi: 10.1186/1297-9686-41-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li R, Chambless L. Test for additive interaction in proportional hazards models. Ann. Epidemiol. 2007;17:227–236. doi: 10.1016/j.annepidem.2006.10.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data of this study are available from the corresponding author upon reasonable request.