Abstract
Life’s Simple 7 is an initiative of the American Heart Association developed for stratifying risk factors associated with adverse vascular outcomes and premature mortality. While this scale has been widely used, there is limited information on its applicability to individuals living in remote communities where risk factors and lifestyles differ from those found in urban settings. This longitudinal prospective study aimed to assess, according to the Life’s Simple 7 scale, all-cause mortality in community-dwelling middle-age and older adults of Amerindian ancestry living in rural Ecuador. A total of 933 Atahualpa residents aged ≥ 40 years who received baseline interviews and procedures for measurement of cardiovascular health (CVH) metrics were enrolled and followed-up for a median of 8 years (interquartile range: 4–9 years). Using a Poisson regression model (adjusted for age at baseline, gender and the level of education), the predicted incidence rate of mortality was 4.22 per 100 person-years (95% C.I.: 2.48–5.97) for individuals with 0–1 CVH metrics in the ideal range, which decreased to 1.23 (95% C.I.: 0.24–2.21) for those with five ideal metrics. In an adjusted Cox-proportional hazard model that included all the CVH metrics, having three or more metrics in the ideal range significantly reduced the mortality hazard ratio when compared with individuals having 0–2 ideal metrics. Study results emphasize the usefulness of the Life’s Simple 7 scale to estimate mortality risk in Amerindians living in remote communities. Control of CVH metrics should prove cost-effective for reducing premature deaths in underserved populations.
Keywords: Life’s Simple 7, Cardiovascular health metrics, All-cause mortality, Population-based cohort, Rural communities, Amerindians
1. Introduction
In 2010, an American Heart Association (AHA) initiative developed a scale for defining ideal cardiovascular health status (Lloyd-Jones et al., 2010). This scale has been called Life’s Simple 7, and is composed of four health behaviors: cigarette smoking, the body mass index, physical activity, and a healthy diet; and three health factors: blood pressure, fasting glucose and total cholesterol blood levels. Each of these cardiovascular health (CVH) metrics was stratified as ideal, intermediate, or poor according to well-defined parameters. The scale has been widely used in individuals from different races/ethnic groups as well as in people living in urban centers or rural areas, and has demonstrated an overall good correlation with diverse conditions and diseases despite differences across cultural context as well as regional disparities in cardiovascular risk factors (Ahmed et al., 2020, Del Brutto et al., 2013a, Folsom et al., 2011, Patterson et al., 2016, Zhang et al., 2020).
Several longitudinal studies have also addressed the influence of Life’s Simple 7 on mortality (Ahmad et al., 2019, Dong et al., 2012, Han et al., 2019, Lin et al., 2015). However, information on the value of this scale in predicting mortality among people living in remote or rural communities is limited. Taking the opportunity of the Atahualpa Project Cohort, this longitudinal prospective study aimed to assess all-cause mortality according to the Life’s Simple 7 scale in community-dwelling middle-age and older adults of Amerindian ancestry living in rural Ecuador.
2. Methods
2.1. Study population
This longitudinal prospective study was conducted in Atahualpa, a rural Ecuadorian village, where previous cross-sectional studies on clinical correlates of the cardiovascular health status have been carried out (Del Brutto et al., 2013b). Characteristics of the village and its residents have been detailed elsewhere (Del Brutto et al., 2014). Atahualpa is an isolated and underserved community. Residents are homogeneous regarding race/ethnicity (Amerindian ancestry), dietary habits (based on oily fish intake, vegetables, fruits, and carbohydrates), and lifestyles. Almost all men belong to the blue-collar class – working as artisan carpenters – and most women are homemakers. Inhabitants get around within the village on foot or by bicycle, since very few of them own a motor vehicle.
2.2. Study design
Data from this study will be available from the corresponding author upon reasonable request. The study was approved by the I.R.B. of Hospital-Clínica Kennedy (FWA 00030727). All Atahualpa residents aged ≥ 40 years were identified by means of annual door-to-door surveys (from June 2012 to June 2019) and those who signed a comprehensive informed consent were enrolled. Participants were screened yearly to determine changes in vital status. In addition, field investigators continuously reminded participants’ proxies to notify us in the event of death. Those who emigrated or declined consent were taken out of the cohort at the administrative censoring date of the last annual survey when the individual was interviewed. Persons who died were censored at the time of death. Outcomes were further evaluated by proxy-delivered medical history and death certificates, which were revised to confirm the date and to get insights on the possible cause of death. For the current analysis, the last censoring date was set as June 2021.
2.3. Assessment of cardiovascular health metrics
Interviews and procedures for determining CVH metrics followed the recommendations and cutoffs proposed by the AHA (Lloyd-Jones et al., 2010). This study took into account the presence of CVH metrics in the ideal range, which included: 1) smoking status: never or quit > 1 year; 2) body mass index: <25 kg/m2; 3) physical activity: ≥150 min/week of moderate intensity or ≥ 75 min/week of vigorous intensity or equivalent combination; 4) healthy diet: 4–5 components based on 5 health dietary components (≥4.5 cups fruits and vegetables per day, ≥two 3.5-oz servings fish per week, ≥three 1-oz equivalent servings fiber-rich whole grains per day, <1,500 mg sodium per day, and ≤ 450 kcal sugar-sweetened beverages per week); 5) blood pressure: untreated and < 120/<80 mmHg; 6) fasting glucose: untreated and < 100 mg/dL; and 7) total cholesterol blood levels: untreated and < 200 mg/dL
2.4. Statistical analysis
In unadjusted analyses, continuous variables were compared by linear models and categorical variables by the chi-square or Fisher exact test as appropriate. To compute the person-years of follow-up we considered the time from enrollment to the last censoring date, study drop-out, or time of death. Using Poisson regression models, we calculated the mortality incidence rate ratio (IRR) according to the number of CVH metrics in the ideal range. Cox-proportional hazard models adjusted for age, gender and level of education, were fitted to calculate the hazard ratio (HR) with its 95% confidence interval (CI) in order to estimate the risk for all-cause mortality according to individual CVH metrics as well as to categories of CVH metrics in the ideal range. For the latter, scores of 0–1 and those of 6–7 were merged because only four and 12 participants had 0 and 7 ideal CVH metrics, respectively. All data analyses were carried out by using STATA version 17 (College Station, TX, USA).
3. Results
A total of 933 Atahualpa residents aged ≥ 40 years were enrolled. The total follow-up was 6,134 years and the median follow-up was 8 years (interquartile range: 4–9 years). Individuals censored before the end of the study were those who emigrated (n = 58), declined further consent (n = 64), or died (n = 140) during follow-up; however, they also contributed to the total time of follow-up.
The mean (±SD) age of study participants at the time of enrollment was 57.2 ± 12.8 years (median age: 54 years; age range: 40 to 93 years), 505 (54%) were women, and 529 (57%) had primary school education only. Forty-two individuals (5%) had 6–7 metrics in the ideal range, 97 (10%) had 5, 229 (25%) had 4, 305 (33%) had 3, 195 (21%) had 2, and the remaining 65 (7%) had 0–1 ideal metrics. Individual ideal CVH metrics included: 1) smoking status: 890 (57%); body mass index: 310 (33%); physical activity: 435 (47%); healthy diet: 170 (18%); blood pressure: 324 (35%); fasting glucose: 332 (36%); and total cholesterol blood levels: 567 (61%).
In unadjusted analysis, individuals who died during the study years had less ideal CVH metrics than those who remained alive (2.6 ± 1.1 versus 3.3 ± 1.2; p < 0.001). Likewise, individual who died were older at baseline and were less educated than those who survived. Several CVH metrics in the ideal range (physical activity, blood pressure, fasting glucose, and total cholesterol blood levels) were also less frequent among subjects who died during the follow-up; in contrast, survivors had less often a body mass index in the ideal range than those who died (Table 1).
Table 1.
Characteristics of Atahualpa residents across categories of vital status at the censoring date (unadjusted analyses).
| Variable | Total series (n = 933) | Vital status at censoring date |
||
|---|---|---|---|---|
| Dead (n = 140) | Alive (n = 793) | p value | ||
| Age at baseline, years (mean ± SD) | 57.2 ± 12.8 | 66.7 ± 12.5 | 53.2 ± 12.7 | <0.001* |
| Female gender, n (%) | 505 (54) | 71 (51) | 434 (55) | 0.379 |
| Primary school education, n (%) | 529 (57) | 111 (79) | 418 (53) | <0.001* |
| Never smoker or quite > 1 year, n (%) | 890 (95) | 132 (94) | 758 (96) | 0.499 |
| Body mass index < 25 kg/m2, n (%) | 310 (33) | 57 (41) | 253 (32) | 0.041* |
| Ideal physical activity, n (%) | 435 (47) | 42 (30) | 393 (50) | <0.001* |
| Healthy diet, n (%) | 170 (18) | 20 (14) | 150 (19) | 0.191 |
| Blood pressure < 120/<80 mmHg, n (%) | 324 (35) | 14 (10) | 310 (39) | <0.001* |
| Fasting glucose < 100 mg/dL, n (%) | 332 (36) | 31 (22) | 301 (38) | <0.001* |
| Total cholesterol < 200 mg/dL, n (%) | 567 (61) | 70 (50) | 497 (63) | 0.004* |
| Total metrics in the ideal range (mean ± SD) | 3.2 ± 1.2 | 2.6 ± 1.1 | 3.3 ± 1.2 | <0.001* |
*Statistically significant result.
Using a Poisson regression model (adjusted for age at baseline, gender and the level of education), the predicted incidence rate of mortality was 4.22 per 100 person-years (95% C.I.: 2.48–5.97) for individuals with 0–1 CVH metrics in the ideal range, which decreased to 1.23 (95% C.I.: 0.24–2.21) for those with five ideal metrics.
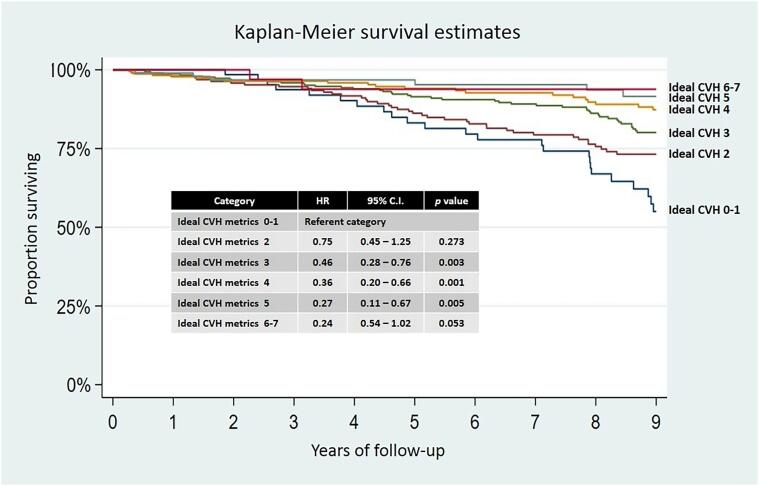
Using Cox-proportional hazard models evaluating individual CVH metrics, having ideal physical activity (HR: 0.55; 95% C.I.: 0.36–0.82), ideal blood pressure (HR: 0.39; 95% C.I.: 0.22–0.69) and ideal total blood cholesterol levels (HR: 0.61; 95% C.I.: 0.44–0.86) were inversely associated with mortality, after adjusting for age, gender y levels of education. In all these models, increasing age and male gender remained independently significant in the above-mentioned associations. Using a different Cox-proportional hazard model that included all the CVH metrics (also adjusted for age, gender and level of education), having three or more CVH metrics in the ideal range significantly reduced the mortality HR when compared with individuals having 0–1 and 2 ideal metrics (Fig. 1).
Fig. 1.
Kaplan-Meier survival curves and Hazard Ratios with 95% confidence intervals for all-cause mortality according to the number of cardiovascular health metrics in the ideal range, adjusted for age, gender, and level of education.
4. Discussion
In this cohort of community-dwelling middle-aged and older adults living in a remote setting, a higher number of ideal CVH metrics was inversely associated with the risk of all-cause mortality. This inverse relationship was roughly linear as shown in the Poisson regression and Cox-proportional hazard models, and was independent of increasing age, gender and the level of education. Study results also show that having more than five CVH metrics in the ideal range did not change the overall outcome as mortality risk was not further reduced compared with those who have only five ideal CVH metrics. In contrast, having up to one ideal CVH metric did not increase mortality risk when compared to individuals who have two ideal CVH metrics. Regarding the association of individual CVH metrics, having ideal physical activity, blood pressure and total blood cholesterol levels were independently associated with a reduced mortality risk, after adjusting for the above-mentioned confounders. Also, in unadjusted analysis, an ideal body mass index was directly associated with increased mortality risk which may be related to the so-called “obesity paradox” (Oreopoulos et al., 2008). This association vanished in multivariate models probably due to the effect of covariates.
As previously noted, several studies have addressed the utility of the Life’s Simple 7 scale for predicting adverse vascular outcomes and mortality across different races/ethnic groups and populations (Ahmad et al., 2019, Ahmed et al., 2020, Del Brutto et al., 2013a, Dong et al., 2012, Folsom et al., 2011, Han et al., 2019, Lin et al., 2015, Patterson et al., 2016, Zhang et al., 2020). In the multi-ethnic Northern Manhattan Study, the HR for all-cause mortality was not significantly lower for individuals with five or more ideal CVH metrics when compared to that of those with two ideal metrics (0.59 [95% C.I.: 0.43–81] versus 0.87 [95% C.I.: 0.43–0.81]); the difference, however, did become significant when only vascular deaths were computed (Dong et al., 2012). In the National Health and Nutrition Examination Surveys (NHANES), long-term all-cause mortality after a stroke was inversely associated with the number of CVH metrics in the ideal range; individuals with ≥ 4 ideal metrics had lower all-cause mortality than those with 0–1 ideal metrics (HR: 0.51; 95% C.I.: 0.29–0.92) (Lin et al., 2015). In another study that included the NHANES population, the adjusted HR for mortality in individuals with ≥ 5 ideal CVH metrics was 0.46 (95% C.I.: 0.35–0.61) compared to individuals with 0–1 ideal metrics (Han et al., 2019). These longitudinal studies were conducted in the US, and results may not be comparable with those of the present study. To the best of our knowledge, there are no reported findings about mortality predicted by the Life’s Simple 7 scale among individuals living in remote communities of Latin America. It is well known that lifestyles and cardiovascular risk factors are different in remote rural settings, and the results of the present study may help health authorities to plan region-specific preventive and intervention programs aimed at reducing premature mortality.
The present study has several strengths that include the population-based design, the homogeneity of the study population, the systematic assessment of CVH metrics by means of uniform and standardized protocols, and the detailed follow-up. Study limitations include low generalizability to other settings, absence of cause of death sub-analysis due to suspected inaccuracies in death certificates and verbal autopsy reports, and the fact that some unmeasured confounders may have accounted for part of the disclosed inverse relationship between ideal CVH metrics and mortality. In addition, CVH metrics were measured at baseline and they may have changed after a median of eight years of follow-up, leading to over or underestimation of actual associations. However, this population has been closely followed and many individuals had repeated determinations of one or more CVH metrics over the study years. Our records did not identify major changes in CVH metrics with the exception of a transient but significant decline in physical activity and dietary habits among older adults during the past year as a result of the SARS-CoV-2 pandemic (Del Brutto et al., 2021).
5. Conclusion
Study results confirm the utility of the Life’s Simple 7 scale in estimating mortality risk in Amerindians living in remote communities. Measures aimed at controlling these risk factors should prove cost-effective at reducing premature mortality in remote underserved populations where health resources are already stretched to their limits. However, this is not an easy task and presents even greater challenges in the context of poverty and illiteracy. Risk reduction programs require collaborative efforts that should start at home and be disseminated through educational centers, the work place and social gatherings (Sanchez. 2018). Further studies in similar populations are warranted to confirm our findings.
6. Source of funding
Universidad Espíritu Santo – Ecuador.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Ahmad M.I., Chevli P.A., Barot H., Soliman E.Z. Interrelationships between American Heart Association’s life’s simple 7, ECG silent myocardial infarction, and cardiovascular mortality. J. Am. Heart Assoc. 2019;8 doi: 10.1161/JAHA.118.011648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed A., Pinto Pereira S.M., Lennon L., Papacosta O., Whincup P., Wannamethee G. Cardiovascular health and Stroke in older British men. Prospective findings from the British Regional Heart Study. Stroke. 2020;51(11):3286–3294. doi: 10.1161/STROKEAHA.120.030546. [DOI] [PubMed] [Google Scholar]
- Del Brutto O.H., Dong C., Rundek T., Elkind M.S.V., Del Brutto V.J., Sacco R.L. Cardiovascular health status among Caribbean Hispanics living in Northern Manhattan and Ecuadorian natives/mestizos in rural coastal Ecuador: a comparative study. J. Commun. Health. 2013;38(4):634–641. doi: 10.1007/s10900-013-9658-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Brutto, O.H., Mera, R.M., Rumbea, D.A., Pérez, P., Recalde, B.Y., Sedler, M.J., 2021. Body composition in community-dwelling older adults before and after SARS-CoV-2 infection: a longitudinal prospective study in a rural village struck by the pandemic. J. Prim. Care Community Health. https://doi.org/10.1177/21501327211047781. [DOI] [PMC free article] [PubMed]
- Del Brutto O.H., Peñaherrera E., Ochoa E., Santamaría M., Zambrano M., Del Brutto V.J. Door-to-door survey of cardiovascular health, stroke and ischemic heart disease in rural coastal Ecuador — The Atahualpa Project. Methodology and operational definitions. Int. J. Stroke. 2014;9(3):367–371. doi: 10.1111/ijs.12030. [DOI] [PubMed] [Google Scholar]
- Del Brutto O.H., Santamaría M., Ochoa E., Peñaherrera E., Santibáñez R., Pow-Chon-Long F., Zambrano M., Del Brutto V.J. Population-based study of cardiovascular health in Atahualpa, a rural village of coastal Ecuador. Int. J. Cardiol. 2013;168(2):1618–1620. doi: 10.1016/j.ijcard.2013.01.017. [DOI] [PubMed] [Google Scholar]
- Dong C., Rundek T., Wright C.B., Anwar Z., Elkind M.S.V., Sacco R.L. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across Whites, Blacks, and Hispanics. The Northern Manhattan Study. Circulation. 2012;125(24):2975–2984. doi: 10.1161/CIRCULATIONAHA.111.081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folsom A.R., Yatsuya H., Nettleton J.A., Lutsey P.L., Cushman M., Rosamond W.D. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J. Am. Coll. Cardiol. 2011;57(16):1690–1696. doi: 10.1016/j.jacc.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han L., You D., Ma W., Astell-Burt T., Feng X., Duan S., Qi L.u. National trends in American Heart Association revised life’s simple 7 metrics associated with risk of mortality among US adults. JAMA Netw. Open. 2019;2(10):e1913131. doi: 10.1001/jamanetworkopen.2019.13131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin M.P., Ovbiagele B., Markovic D., Towfighi A. “Life’s simple 7” and long-term mortality after stroke. J. Am. Heart Assoc. 2015;5 doi: 10.1161/JAHA.114.001470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Jones D., Hong Y., Labarthe D., Mozaffarian D., Appel L.J., Van Horn L., Greenlund K., Daniels S., Nichol G., Tomaselli G.F., Arnett D.K., Fonarow G.C., Ho P.M., Lauer M.S., Masoudi F.A., Robertson R.M., Roger V., Schwamm L.H., Sorlie P., Yancy C.W., Rosamond W.D. Defining and setting national goals for cardiovascular health promotion. The American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- Oreopoulos A., Padwal R., Kalantar-Zadeh K., Fonarow G.C., Norris C.M., McAlister F.A. Body mass index and mortality in heart failure: a meta-analysis. Am. Heart J. 2008;156(1):13–22. doi: 10.1016/j.ahj.2008.02.014. [DOI] [PubMed] [Google Scholar]
- Patterson F., Zhang G., Davey A., Tan Y., Ma G.X. American Heart Association’s ideal cardiovascular health metrics in under-represented Asian Americans. J. Commun. Health. 2016;41(6):1282–1289. doi: 10.1007/s10900-016-0217-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez E. Life’s simple 7. Vital but not easy. J. Am. Heart Assoc. 2018;7 doi: 10.1161/JAHA.118.009324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M., Shi Y.u., Shi O., Zhao Z., Zhang X., Li C., Huang Z., Zhao L., Wang L., Li Y., Li X. Geographical variations in cardiovascular health in China: a nationwide population-based survey of 74,726 adults. Lancet Reg. Health West. Pac. 2020;3:100033. doi: 10.1016/j.lanwpc.2020.100033. [DOI] [PMC free article] [PubMed] [Google Scholar]