Abstract
Objective
To determine the aims, participants, and outcomes of training communication partners of Chinese-speaking persons with aphasia (PWA).
Data Sources
Sixty search terms related to communication partner training (CPT) in Chinese characters were searched in 8 electronic databases (published 1991-2020).
Study Selection
Journal articles written in Chinese that primarily target the Chinese audience and university theses were selected for review. Studies involving CPT and training to enable communication partner to deliver language tasks were included, but reports without PWA or direct training of communication partners were excluded. A final corpus of 37 articles, representing publications of group studies, case studies, qualitative studies, and opinion articles, were selected for full review.
Data Extraction
For all articles, 2 reviewers independently reviewed abstracts, excluding those without PWA or those that did not involve training of communication partners. One reviewer extracted descriptive data of participants with aphasia, communication partners, intervention details of the intervention (purpose, amount, setting, description), outcome measures, results, and clinical guidelines. A second reviewer performed accuracy verifications.
Data Synthesis
Quality of reviewed articles were classified using the American Academy of Neurology levels of evidence. The current review suggested an evidence base of low to medium quality supporting 2 intervention groups: (1) training partners to deliver therapy tasks and (2) training to improve communication between PWA and their communication partners. There was a higher proportion of persons with acute and subacute aphasia involved in these investigations, suggesting evidence on treatment efficacy of CPT in the acute stage.
Conclusions
Additional high-quality research with a better methodological quality, for example, randomized controlled trials or experimental design, are required to strengthen the current evidence of CPT. This systematic review suggests that the inclusion of studies published in languages other than English may influence the findings of mainstream reviews relating to aphasia.
KEYWORDS: Aphasia, Asian Continental Ancestry Group, Rehabilitation, Systematic review
List of abbreviations: AAN, American Academy of Neurology; CP, communication partner; CPT, communication partner training; LOE, languages other than English; PWA, persons with aphasia; PEDro, Physiotherapy Evidence Database; QOL, quality of life; SCED, Single-Case Experimental Design; SLT, speech and language therapist
Aphasia is an acquired language disorder due to damage to brain areas that are responsible for language functions.1 Persons with aphasia (PWA) have impaired language comprehension and production in both oral and written modalities2 and display difficulties from constituting thoughts into formulation of spoken output3 across levels of performance in words, sentences, and discourse.4
Various treatment approaches have been proposed within the field of aphasiology, including impairment-focused interventions, which explicitly target language functions, and social approaches, which focus on broader constructs such as increased life participation or quality of life (QOL). Within social approaches, communication partner training (CPT) is one of the more common interventions, defined as an intervention directed at people other than PWA with the intent of improving PWA's language, communication, participation, and/or well-being.5 More specifically, CPT is an environmental intervention that targets PWA, their family members, and volunteers or health care professionals, with an overarching aim to optimize the communication environment and thereby improve communication between PWA and their communication partners (CPs)5; as such, CPT focuses explicitly on the communication skills of the CPs and, in some cases, also the skills of the PWA.
Training CPs to conduct traditional language exercises with the aim of improving linguistic abilities have been excluded from reviews of CPT5, 6 and is not considered “true CPT.” However, this type of “task shifting,” in which someone other than the speech and language therapist (SLT) is tasked with conducting therapy aimed at discrete communication skills, is not uncommon. Because training CPs for different purposes may be important in contexts in which the ratio of SLTs to patients is unfavorable, this review includes the broad category of training CPs, distinguishing between the subset of studies in which CPs deliver therapy tasks (“task shifting” or “family/caregiver-mediated rehabilitation” in which family members are trained to deliver the therapy tasks) and those that address “true CPT,” which is more narrowly defined as focused on improving communication between the PWA and their CPs and/or addressing broader considerations of well-being and QOL through the training.
Systematic reviews of CPT have been conducted to explore the effects of CPT on language, communication activity and participation, psychosocial adjustment, and QOL for PWA and their CPs.5 It was concluded that CPT was effective in supporting individuals with chronic aphasia, but evidence to support treatment effectiveness for individuals with acute aphasia was insufficient. Subsequently, Simmons-Mackie et al6 provided an updated version in 2016 by reviewing research reported between 2010 and 2013, and reexamined recommendations based on new publications. Both studies included 12 electronic databases with 23 search terms related to CPT (supplemental appendix S114, 18, 19, 20, 22, 25, 26, 27, 28, 29, 31, 32, 33, 34, 36, 37, 38, 40, 41, 43, 44, 46, 47, 48, 49, 79, 80, 81, 82 available online only at http://www.archives-pmr.org/). The findings of the 2 reviews (see details of the review procedures in supplemental appendix S2, available online only at http://www.archives-pmr.org/) represented predominantly English-speaking PWA, although studies conducted in Finnish, Danish, and Swedish are also prominent in the first study. Nevertheless, despite the fact that the participants represented a number of languages other than English (LOE), both reviews were restricted to studies published in English, potentially excluding a relevant and context-sensitive body of literature in other languages.
There are 1.12 billion Chinese speakers worldwide,7 compared with the Western-dominant research of aphasiology, little attention has been given to Chinese PWA, and studies written in Chinese involving PWA are typically excluded in reviews. One may argue that this disproportional lack of attention extends to other Asian languages. Although a small amount of literature has focused on Chinese PWA, it remains unclear if there are additional studies conducted around CPT in Hong Kong, China, and Taiwan (and possibly other Asian countries with a Chinese population) written in Chinese being published in local and/or regional journals that primarily target the Chinese audience. With the assumption that the existing body of knowledge is limited (and potentially representing smaller studies, or those will null findings), it is important to acknowledge the work to date. This present study sought to explore the extent of the Chinese literature on training of CPs and to investigate the effects of training CPs (distinguishing between interventions that rely on task shifting and those that involve CPT in its strict sense) on both the PWA and their CPs in the Chinese population. The 3 research questions guiding this systematic review were (1) What are the characteristics of training for CPs of Chinese PWA in terms of the aims of the intervention? (2) What outcomes are reported for task shifting vs CPT? (3) Does CPT produce a similar positive treatment effect in the Chinese population with aphasia as documented in the systematic reviews of Simmons-Mackie et al5,6 in 2010 and 2016 focusing on studies published in English?
Methods
Research design
Studies that documented training of CPs as an intervention in relation to Chinese PWA were identified through a systematic literature search. Electronic databases documenting literature written in Chinese were searched: Chinese Scientific Journals database, China National Knowledge Infrastructure, and Ariti Library. Moreover, we also included university thesis and dissertation electronic databases in the search: Chinese Electronic Theses and Dissertations Service, National Digital Library of Thesis and Dissertation in Taiwan, CUHK Electronic Theses and Dissertation Collection, HKU Scholars Hub, and ScholarBank@NUS. Search terms in traditional and simplified Chinese characters translated from the 2010 review of Simmons-Mackie et al5 and additional search terms based on Chinese literature were adopted (see full search string in supplemental appendix S1, available online only at http://www.archives-pmr.org/). To allow considerations of all kinds of intervention studies, journal articles reporting investigations with a group design, randomized or nonrandomized controlled trials, case study or single-participant research design, quantitative or qualitative research design, theses, and opinion articles were included. Studies that did not include PWA or did not involve training of CPs were excluded. In contrast to the English-language reviews,5,6 studies that involved training to enable CPs to deliver language tasks were not excluded.
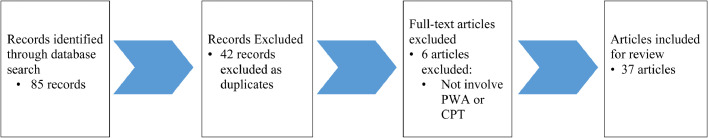
The search included articles published from 1991-2020, with a search process illustrated in fig 1. A total of 85 articles meeting the initial inclusion criteria were identified; 42 records were eliminated as duplicates. Based on the abstract of the remaining 43 articles, 3 articles were rejected because no PWA were involved, and another 3 articles not involving training of CPs were eliminated. A final 37 articles met the criteria for full review.
Fig 1.
Flowchart of systematic review process.
Measures and analysis
Descriptive summary on the characteristics of CPs, PWA, intervention characteristics, outcome measures on PWA's changes (ie, language competence, activities/participation, psychological well-being), and summary on opinion articles were reviewed.
Evaluation on the quality of articles were also conducted by 2 independent reviewers (A.K., and C.C.) (to establish interrater reliability) using 4 classification systems, as in the 2010 review:
-
(1)
American Academy of Neurology (AAN) Classification of Evidence,8 ranging from the highest (Class I) to lowest (Class IV) level of evidence.
-
(2)
Physiotherapy Evidence Database (PEDro) scale,9 which has been adopted to evaluate methodological quality of randomized controlled trials in group studies; it was originally developed to rate the quality of randomized controlled trials in physiotherapy and has been applied to other therapeutic management (ie, voice therapy).10 Group studies are typically evaluated across 11 criteria in the PEDro scale, where the maximum score is 10 (because 1 criterion is not counted toward the total score).
-
(3)
Single-Case Experimental Design (SCED) Scale,11 which was developed to evaluate the methodological quality of single-case studies with established interrater reliability. It provides a quality score based on a 11-item rating scale.
-
(4)
Rating of Qualitative Design,12 which was adopted with a 16-item rating scale (with a full mark of 14 points) for evaluating qualitative studies.
Results
Descriptive review
Of all 37 articles, 12 investigated task-shifting interventions involving training CPs to deliver therapy tasks, 10 investigated CPT, and 1 examined a combination of tasking shifting and CPT. All 13 reports that addressed task shifting were in a group design. Studies exploring CPT (n=11) comprised group design in 5 studies, case study design in 5 studies, and 1 qualitative study. Supplemental tables S1-S4 (available online only at http://www.archives-pmr.org/) provide a summary of the characteristics of participants (including PWA and non-PWA) and CPs, respectively, grouped by “tasking shifting” interventions (see supplemental tables S1 and S2, available online only at http://www.archives-pmr.org/) and CPT (see tables supplemental S3 and S4, available online only at http://www.archives-pmr.org/).
Studies addressing task shifting
All 13 articles addressing task shifting were undertaken in China (see supplemental table S1, available online only at http://www.archives-pmr.org/) and involved a total of 691 PWA. Across the 9 articles that reported the PWA's age and sex, there were 263 male and 184 female participants of PWA and controls aged 18-85 years. Of the 12 articles that reported the etiology of aphasia, all reported stroke/cerebrovascular disease. Four articles reported participants’ chronicity, including 2 articles involving participants in acute phase (0d to 4mo post onset) and 2 articles involving participants across the acute, subacute (4-6mo post onset), and chronic phase (>6mo post onset).
Eleven of the 13 studies investigating task shifting involved family members, 2 studies involved nurses, and 2 involved both family and health care workers (see supplemental table S2, available online only at http://www.archives-pmr.org/). Only 3 articles reported on the number of partners trained. Age and sex of the CPs were mentioned in only 1 of the studies investigating task shifting.
Supplemental table S3 (available online only at http://www.archives-pmr.org/) summarizes the intervention descriptions in the 13 studies examining task shifting through delivering of therapy tasks by family or non-SLT health care workers. All of the studies investigating task shifting were conducted in China and used group training as the intervention mode. Task shifting focused on training partners to conduct impairment-based language tasks with PWA including gestures training, articulation training, and use of communication board to express daily needs.13,15,24 Training time was reported in 8 studies and ranged between 28 and 312 hours. The total hours reflect a combination of the hours provided by SLTs to the CPs in addition to the hours provided by the CPs to the PWA; however, specific details of how the 2 broke down were not given, nor did they mention whether the proportion of hours by the SLTs decreases over the course of training. The location in which CPs delivered the therapy task was mentioned in 10 of the studies, ranging from at home in 6 studies, in hospital in 3 studies, and across home and hospital in 1 study.
Treatment effects of tasking shifting for language/communication tasks
Outcome measures reported in the 13 articles investigating task shifting focused on the outcomes for PWA, in line with the aim of training partners to deliver therapy tasks. Apart from measures for CPs (eg, knowledge of aphasia), the PWA-specific outcomes can be categorized into 3 areas (see supplemental table S4, available online only at http://www.archives-pmr.org/):
-
(1)
Language impairment measures for PWA: Eleven articles reported positive changes in PWA's language impairment outcomes. In particular, statistically significant improvement in language was reported in 9 of 11 articles using outcome measures of standardized language assessment, such as Aphasia Battery in Chinese50 and self-developed rating scales on PWA's comprehension and expression ability.
-
(2)
Activity/participation measures for PWA: Three of the 13 articles included a measure of activity/functional communication and all 3 documented improvements in PWA as measured by a Chinese adaptation of the Improvement in total score of Instrumental Activities of Daily Living,51 Chinese Functional Communication Profile,52 and Barthel Index.53 Two of the 3 articles21,23 reported on statistically significant increase and on both.
-
(3)
Quality of life measures for PWA: Only 1 article measured PWA's QOL using Generic Quality of Life Inventory-74.54 Statistically significant increase in Generic Quality of Life Inventory-74 scale was documented after training partners to deliver therapy tasks.
Studies investigating CPT
Eleven articles explored CPT, involving a total of 242 PWA (supplemental table S5, available online only at http://www.archives-pmr.org/). Unlike the situation in task shifting where all studies were conducted in China, those exploring CPT were more diverse in origin, with 3 articles from China, 2 in the context of Hong Kong, and 6 with participants in Taiwan. Eight studies reported the PWA's age and sex: age ranged from 18-94 years, with 90 male and 66 female participants, including both PWA and controls. Of the 8 articles that reported the etiology of aphasia, all but 1 reported stroke. Six articles reported participants’ chronicity, including 4 articles involving PWA in acute phase and 2 involving people in the chronic phase (>6mo post onset).
Eight of the 11 studies on CPT involved family members, and 2 studies involved nurses (supplemental table S6, available online only at http://www.archives-pmr.org/). Age and sex of the CPs were mentioned in 4 studies, with age ranging between 18 and 80 years, involving 36 male and 108 female participants.
“True CPT,” in which the intervention involved teaching CPs different communication strategies to promote competence in interacting with PWA and educational programs for CPs to gain a better understanding of aphasia and stroke, was the focus of 11 studies (supplemental table S7, available online only at http://www.archives-pmr.org/). Training involving groups of CPs was used in 5 of the studies, a further 5 studies used dyad training, and the final study involved individual training of the conversation partner. The training time ranged from 1-8 hours for those studies addressing CPT only and up to 56 hours for the study involving a combination of CPT and task shifting.15
Treatment effects of CPT in the Chinese-speaking population
Outcome measures for the 9 of 11 articles investigating CPT predominantly focused on functional communication or activity/participation outcomes, as might be expected given the aims of CPT being to improve communication between PWA and CPs. Two articles used impairment measures or qualitative description on a discrete matching task to report outcomes. Four articles reported outcome measures for only the PWA, 2 reported outcomes for just the CP, and the remaining 4 reported outcomes for both. The details of outcomes reported are shown in supplemental table S8 (available online only at http://www.archives-pmr.org/). Specific treatment results documented are given in supplemental appendix S3 (available online only at http://www.archives-pmr.org/).
Opinion articles addressing training of CPs (task shifting and CPT)
Across the 14 opinion articles, 6 proposed practical guidelines without a clear reference to previous publications, and the remaining 8 were based on previous publications in China or the literature from Western countries. Practical guidelines provided and/or summarized can be largely categorized into 3 areas (ie, psychological/emotional, communication skills, language/therapy tasks) (supplemental table S9, available online only at http://www.archives-pmr.org/). Eleven opinion articles included guidelines for CPs to support PWA's psychological well-being by treating PWA with respect and empathy, providing care, and supporting with patience. Guidelines for communication skills were provided in 9 articles, where 3 suggested using solely nonverbal communication (eg, facial expression, gestures, written modality) to communicate with PWA. Twelve articles offered suggestions for how CPs could deliver impairment-based tasks to facilitate PWA's spoken output, such as articulation training and language production training targeting single words to short phrases39,42,45
Research quality review
With reference to the AAN Classification of Evidence (supplemental table S10, available online only at http://www.archives-pmr.org/), of the 10 studies investigating CPT alone, only 1 (a dissertation) met all the criteria listed in Class I evidence. None of the studies investigating task shifting were classed in this category. The top 2 common missing criteria from the group designs were the absence of data at pretreatment baseline and lack of account for participant dropouts. Most (80%, 8/10) of studies addressing CPT were categorized as Class IV. In contrast, although none of the studies investigating task shifting were categorized as Class I evidence, 50% (6/12) met the criteria listed for Class II evidence. Interrater reliability was 87.8% (supplemental table S11, available online only at http://www.archives-pmr.org/). Discrepancies between 2 raters were found in 9 of 37 articles mostly in the criteria of whether (1) articles have presented relevant baseline for treatment groups and baseline was substantially equivalent between 2 groups and (2) at least 80% of participants completed the study and article authors adequately accounted for dropouts. The 2 raters gave opposite ratings (ie, yes/no) for the above 2 criteria.
The PEDro scale was also used to evaluate the 17 group studies (4 addressing CPT, 12 addressing task shifting, 1 study incorporating both). As detailed in supplemental table S12 (available online only at http://www.archives-pmr.org/), the group studies in both task shifting and CPT domains scored in a range from 1-6 (out of a possible 10). Two studies investigating task shifting scored 6, and 1 addressing CPT achieved this score, suggesting that most of these group studies were of middle to low quality. Twelve of the 13 studies involving task shifting met the criteria of measuring outcomes on 85% of participants in contrast to only 2 of the 4 investigating CPT. All studies missed the criteria of concealing allocation, blinding of participants, therapists administering the therapy, and assessors providing measurement on treatment outcome. As shown in supplemental table S11 (available online only at http://www.archives-pmr.org/), interrater reliability (ie, 88.2%) was compatible with reliability measurements of the PEDro scale documented by Maher et al.9 (ie, percentage agreement of 70.3%-98.2%). Discrepancies in rating between raters were found in items of whether the reviewed articles had (1) conducted the same data analysis on treated and untreated participants and (2) explicitly stated both the number of participants allocated to treatment groups initially and number of participants (>85%) measured for treatment outcomes after CPT. Discrepancies may be because of difference in interpretation of the rating scale items between 2 raters, where one focused on whether articles have measured treatment outcomes in more than 85% of participants and the other focused on whether articles explicitly stated both the numbers of participants in initial allocation and measurement of treatment outcomes.
The 5 case studies, all of which investigated CPT, were evaluated using the SCED scale. One case study30 received a score of 8, and the remaining 4 were scored ranging from 0-1 of 10 points (supplemental table S13, available online only at http://www.archives-pmr.org/). Interrater agreement was 80%, which was compatible with the earlier report of Tate et al at 77.0%-96.7%.11 Discrepancies between raters were mostly found in the SCED scale item of whether articles provided “repeatable and precise measures for target behaviors.” All the case studies did not show evidence of generalization and replication across PWA, therapists, or settings. This suggested that high-quality case studies were scarce in the current reviewed articles.
The only qualitative study,35 which explored CPT, was rated using the Rating of Qualitative Design.12 A rating of 12 of 14 points suggested that this was a high-quality qualitative research (supplemental table S14, available online only at http://www.archives-pmr.org/). However, the same study was classified as Class IV in AAN Classification of Evidence because of the lack of an experimental controlled design. Interrater reliability (ie, 92.8%) fell into the range of percentage agreement of the report by Cherney et al12 (60%-100%). Discrepancies between 2 raters were found in presence of (1) treatment fidelity: adherence to treatment was assessed and (2) treatment replicability: clearly described treatment process. Interpretation on the definition of clearly described treatment process may be different between the 2 raters and thus may account for the discrepancy.
Discussion
This is the first systematic review of interventions involving CPT specific to the Chinese population and, in particular, the first that we know of that synthesizes research in this topic published in a language other than English. Training of CPs may be done with different aims, and this study analyzed the literature to synthesize the evidence for 2 broad classes of intervention involving training of other people in the environment to improve the language, communication, or well-being of PWA: that pertaining to training to equip partners to deliver therapy tasks (task shifting) and that pertaining to CPT. Task shifting, defined by the World Health Organization as the “rational redistribution of health care tasks among health workforce teams,”55(p1) has been applied in stroke rehabilitation to encompass delivery of rehabilitation task by nurses, for example, in China,56 or by unpaid caregivers, including family caregivers, for example, in India.57 A Cochrane review has found low- to moderate-quality evidence for caregiver-medicated rehabilitation exercises,58 although the evidence in relation to aphasia is yet to be systematically explored. In task shifting, the explicit focus is not on the quality of the communicative interaction, but on the therapy task and performance of the PWA on measures relevant to that task. This is in contrast to CPT.
CPT has been shown to be effective for individuals with acquired brain injury,59 Alzheimer disease,60 and aphasia.61 However, these studies varied greatly in terms of their inclusion criteria of participants,62 for example, in terms of (1) recruiting volunteers60 vs carers living together with PWA63 as CPs; (2) the treatment methods of CPT (eg, identification of nonfacilitative behaviors that hindered effective communication64 vs use of role play in practicing Supported Conversation for Adults with Aphasia61; and (3) outcome measures (eg, use of main concept analysis to measure story retell ability in PWA65 vs questionnaires to examine satisfaction and comfort level in conversational interaction among PWA66). The current review provides insight into the different purposes of training CPs in the context of Chinese-speaking PWA, documenting a range of training (from “true CPT” to training CPs to provide language tasks and increase PWA's language functions). In contrast to the Simmons-Mackie et al reviews,5,6 this review included all studies that involved training others to deliver therapy tasks. The use of task shifting or partner-delivered therapy tasks appears more common in this context than reported in other contexts. The fact that both groups of intervention involve the training of other people in the environment risks that these interventions be conflated with each other. For this reason, the current systematic review provides an opportunity to critically analyze and compare the literature in terms of participants, nature of the intervention, and outcomes. The findings suggest that while the participants may be similar, the aims, outcomes (eg, improvements in participation, well-being, QOL), and intervention duration are markedly distinct. It therefore seems useful to more explicitly separate these interventions in future research by using terms from the broader context of health care and rehabilitation literature, such as task shifting.
The restriction of systematic reviews to research published in English is not unusual.67 Some evidence exists suggesting that restricting systematic reviews to studies published in English has a negligible effect on findings; however, other evidence indicates that research in LOE may be particularly pertinent in relation to interventions that are culturally specific (eg, complementary and alternative medicine68). In interventions relating to communication and social interaction, language and cultural factors are of relevance.69 Incorporating suitable research published in LOE may, therefore, have important implications for informing culturally- and linguistically-sensitive practice and understanding the clinical context in which these services are provided. In addition to providing evidence regarding delivery of training of CPs within specific cultural and linguistic contexts, such evidence may also shed light on this group of interventions more broadly. Of the 37 articles or theses reviewed, 11 studies addressing CPT represented a range of methodologies including group studies, case studies, and qualitative studies. Based on the AAN Classification of Evidence, articles at the top hierarchy (ie, Class I) imply a better methodological quality, and thus, articles with Class I classification provide a stronger scientific evidence to support CPT. In our current review, 1 article was classified as Class I compared with the 2016 review by Simmons-Mackie et al6 where no studies received this classification. However, the present review results also suggested that the strength of evidence, based on Chinese articles, was not adequate to support treatment efficacy of CPT in the current review because of 3 major reasons discussed below in detail.
Validity and reliability of the language impairment outcome measures
Measure of language impairments in PWA and the corresponding outcome measures that were used in the reviewed articles investigating task shifting varied across the studies. The fact that there was a range of tools, from self-developed rating scales,16,17 standardized language assessments translated in Chinese,50 to standardized language assessment developed for speakers in Western countries70 needs to be highlighted. In addition, all self-developed rating scales in these Chinese studies were developed in the form of a nominal scale without details about the corresponding establishment of reliability and validity; this missing information of the psychometric properties of selected Chinese aphasia batteries and potential lack of objectivity of these measures required one to conclude the treatment effects of CPT with caution. Furthermore, in some of the studies that used a standardized language assessment from Western countries, there was no clear specification on whether the authors had properly adapted or translated to a Chinese version of the standardized language assessment. Because the original Western language assessment did not provide geographically and linguistically validated norms for Chinese-speaking PWA, direct application of norms based on English-speaking PWA to determine the presence and severity of aphasia in Chinese PWA may have been biased and inaccurate.
Clinical implications
Establishing the purpose of training CPs is important, and in most studies reviewed, there was a good match between the purpose of the intervention and the focus of the outcome measure (ie, task shifting interventions measured changes in impairment in PWA). There is the potential for a conflict of purpose between task shifting and CPT where in the first case the intervention sets the partner up to didactically administer tasks that may highlight impairment, and in the latter, the partner must take a more facilitatory role and acknowledge the competence of the PWA and focusing on the interaction. This potential contradiction in roles may be the reason why only 1 study combined the 2 interventions. There has been limited literature on didactic language activities for aphasia within families, and research suggests that families may respond differently to these tasks.71 In contexts in which task shifting is considered necessary because of service availability, for example, careful consideration should be given to how the family and PWA have orientated themselves toward adapting to aphasia and how the risk of face-threatening engagement is balanced against the possible benefits of more intensive practice.71 Use of caregiver-mediated exercises (ie, task shifting) for stroke rehabilitation has been investigated because it is an attractive proposition in contexts in which rehabilitation resources are limited. The current review specific to aphasia rehabilitation supports this finding and suggests the need for further research to explore the effectiveness and cost-effectiveness of task shifting in aphasia rehabilitation.
In terms of CPT, where the purpose is to improve communication between PWA and CPs, the current review adds to the existing reviews of CPT research published in English. Western countries are typically characterized by an individualistic culture that emphasizes values for achieving personal benefits; this is in contrast to Eastern countries that may be more likely to be characterized by a collectivist culture emphasizing in-group goals over personal goals.55,72 Given that a collectivist culture is defined as “giving priority to in-group goals over personal goals,”73(p140) people focus on achieving in-group interdependence instead of personal achievements, and such a difference may affect interaction and influence communication.74 Because of differences in PWA's cultural background in the present and the 2016 reviews by Simmons-Mackie et al, we argue that the focus of the treatment outcome measures of the 2 reviews are subtly different. Four of the 11 reviews addressing CPT in current study (representing collectivist culture) have included mutual ratings on communication satisfaction (ie, CP rating his/her communication satisfaction toward PWA and vice versa). This is methodically different from the majority of psychosocial treatment outcome measures focusing on self-evaluation ratings such as self-confidence, self-perception, and personal emotions in the 2016 review by Simmons-Mackie (representing a more individualistic culture). Training of CPT in the Chinese population may focus on establishing in-group goals aiming to improve communication, such as increasing communication satisfaction between CPs and PWA, which is compatible with the collectivist value of harmony and solidarity within a group (PWA and CPs as a group in this case).75 Nevertheless, albeit the abovementioned cultural differences, the psychological/emotional suggestions drawn from our current articles in Chinese (see supplemental table S9, available online only at http://www.archives-pmr.org/) do not seem to distinguish from the treatment guidelines proposed by researchers in the West. Further examinations of how generational or socioeconomic differences and cultural mismatch between the PWA and caregiver may affect their interactions and CPT are warranted.
Study limitations
Experimental design of randomized controlled trials could provide higher-quality evidence and could better guide clinical practice decisions.76 However, only 1 article in the current review (ie, a dissertation) received Class I classification, and most of the remaining articles (ie, 70.3%) only received Class IV classification. One should also note that ratings concluded from the PEDro scale for evaluating quality of group studies were also compatible with AAN Classification because criteria listed in the PEDro scale included components of randomized controlled trials (eg, random allocation of participants into groups, concealed allocation, blinding of participants and/or investigators).76,77 Most of our current reviewed group studies had adopted a single-group design without the use of a control group to verify that any treatment effects reported was a result of CPT. This conclusion was also made by Simmons-Mackie et al in the 2016 review6; none of the English articles included experimental design components to ensure control and randomization. Hence, this has limited one to conclude the efficacy of CPT among Chinese-speaking PWA. Similar to investigations targeting English speakers, a more well-controlled experimental design, which is critically missing as reflected by this review, should be implemented in the future to increase the strength of evidence in Chinese CPT literature.
Another potential limitation relates to confounding factors of spontaneous recovery. Interestingly, 54.5% (6/11) of our reviewed articles on CPT specifically included PWA in the acute phase. This is different from the 2016 review by Simmons-Mackie in which only 1 article (of 25) involved acute PWA, with 2 reporting statistically significant changes in outcome measures. Qualitative improvements in activity/participation measures for PWA, CP, or both were reported in all 6 of the studies involving PWA in the acute phase. Conclusions supporting treatment efficacy of CPT for these articles may, however, require some caution for interpretation because improvements in outcome measures could be attributed to both the treatment itself and spontaneous recovery. According to Cramer,78 most spontaneous language recovery occurs during first 3 months post onset. Therefore, the confounding factor of spontaneous recovery period in the acute phase of PWA could not provide unbiased conclusion of the efficacy of CPT to PWA during the acute phase. The findings do, however, suggest the potential utility of CPT in the acute phase and provide evidence to support further research.
Conclusions
This is the first systematic review synthesizing on aphasia research published in Chinese focusing on communication partner training. The current findings seemed to support the application of CPT in the Chinese context. Additional high-quality research with a better methodological quality, such as randomized controlled trials as experimental design, are required to strengthen the current evidence of CPT. Given that a much higher proportion of persons with acute and subacute aphasia were involved in the Chinese CPT investigations, the current review has extended the 2016 review by Simmons-Mackie et al specific to evidence on treatment efficacy of CPT among persons with acute aphasia. Synthesizing evidence published in languages other than English is not straightforward and relies on teams that have the requisite clinical and language skills. As the current review shows, however, there is an important role for systematically reviewing research in LOE. This type of review provides the opportunity to contextualize interventions, seek contextually specific implications, and extend existing evidence synthesis.
Footnotes
This project concept arose within the Tavistock Trust for Aphasia–funded Collaboration of Aphasia Trialists (aphasiatrials.org).
Disclosures: none
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.arrct.2021.100152.
Appendix. Supplementary materials
References
- 1.Benson DF, Ardila A. Oxford University Press; New York: 1996. Aphasia: a clinical perspective. [Google Scholar]
- 2.Worrall L, Simmons-Mackie N, Wallace SJ, et al. Let's call it “aphasia”: rationales for eliminating the term “dysphasia. Int J Stroke. 2016;11:848–851. doi: 10.1177/1747493016654487. [DOI] [PubMed] [Google Scholar]
- 3.Damasio AR. Aphasia. N Engl J Med. 1992;326:531–539. doi: 10.1056/NEJM199202203260806. [DOI] [PubMed] [Google Scholar]
- 4.Kong APH. Routledge; London: 2016. Analysis of neurogenic disordered discourse production: from theory to practice. [Google Scholar]
- 5.Simmons-Mackie N, Raymer A, Armstrong E, Holland A, Cherney LR. Communication partner training in aphasia: a systematic review. Arch Phys Med Rehabil. 2010;91:1814–1837. doi: 10.1016/j.apmr.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 6.Simmons-Mackie N, Raymer A, Cherney LR. Communication partner training in aphasia: an updated systematic review. Arch Phys Med Rehabil. 2016;97:2202–2221. doi: 10.1016/j.apmr.2016.03.023. [DOI] [PubMed] [Google Scholar]
- 7.Eberhard DM, Simons GF, Fennig CD. 22nd ed. SIL International; Dallas: 2019. Ethnologue. [Google Scholar]
- 8.AmericanAcademy of Neurology . American Academy of Neurology; St. Paul, MN: 2011. Clinical practice guideline process manual. [Google Scholar]
- 9.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. [PubMed] [Google Scholar]
- 10.da Cunha Pereira G, de Oliveira Lemos I, Gadenz CD, Cassol M. Effects of voice therapy on muscle tension dysphonia: a systematic literature review. J Voice. 2018;32:546–552. doi: 10.1016/j.jvoice.2017.06.015. [DOI] [PubMed] [Google Scholar]
- 11.Tate L, Mcdonald R, Perdices S, et al. Rating the methodological quality of single-subject designs and n-of-1 trials: introducing the Single-Case Experimental Design (SCED) Scale. Neuropsychol Rehabil. 2008;18:385–401. doi: 10.1080/09602010802009201. [DOI] [PubMed] [Google Scholar]
- 12.Cherney LR, Simmons-Mackie N, Raymer A, Armstrong E, Holland A. Systematic review of communication partner training in aphasia: methodological quality. Int J Speech Lang Pathol. 2013;15:535–545. doi: 10.3109/17549507.2013.763289. [DOI] [PubMed] [Google Scholar]
- 13.Kong L, Wang Y, Pan RF. Family rehabilitation therapy on the patients who had spoken language impairment after stroke. Chinese J Rehabil Med. 2002;17:152–155. [Google Scholar]
- 14.Liu XX. A clinical study on efficacy of families coordinating rehabilitation treatment for severe aphasia. Chin J Chin Med. 2010;2:40–41. [Google Scholar]
- 15.Luo YQ, Wang YS. [Collaboration between therapist and family members in application of rehabilitation training in language] [Chinese] Chin J Rehabil Med. 2001;16:303–304. [Google Scholar]
- 16.Xie SL, Zhu MG, Zhang XL, Xue ZJ. The role of community nursing in family rehabilitation of stroke patients with impaired spoken language. Chin J Clin Rehabil. 2002;21:3289. [Google Scholar]
- 17.Hou XR, Li SF. Early guidance of language for aphasia patients induced by stroke. J Xinxiang Med Coll. 2005;22:386–388. [Google Scholar]
- 18.Wang H, Zhu LY, Zhan ZX, Peng Y. Effect of participation of fixed caregivers in extended nursing on rehabilitation of ischemic stroke patients in recovery period. J Nurs. 2017;24:71–74. [Google Scholar]
- 19.He YH. [Investigation on mode of family rehabilitation for elderly stroke patients] [Chinese] Chin J Clin Rehabil. 2002;6:3281. [Google Scholar]
- 20.Kong L. [Effect of family rehabilitation training for different types of aphasia] [Chinese] Chin J Rehabil Med. 2006;21:723–724. [Google Scholar]
- 21.Su WY, Sun D, Yu LP. Family follow-up care in elderly patients with stroke aphasia. Chin Rural Health Serv Admin. 2018;38:1367–1369. [Google Scholar]
- 22.Cheng WP, Zhao XL. Rehabilitative nursing care of cerebral apoplexy patients with aphasia. Chin Nurs Res. 2006;20:336–338. [Google Scholar]
- 23.Huang HM. Effect evaluation of rehabilitation nursing model of hospital-community-family in rehabilitation of patients with stroke. Med Inn China. 2014;11:128–130. [Google Scholar]
- 24.Li C. [Nursing and rehabilitation training techniques for patients with traumatic brain injury induced aphasia] [Chinese] Chin J Ethnomed Ethnopharm. 2010;18:140. [Google Scholar]
- 25.Yang B, Gu JX, Liang ZM, Huang XM, Lin CY, Li B. The application of aphasia strengthening training software system in aphasia after stroke. Guangdong Med J. 2014;3:1852–1854. [Google Scholar]
- 26.Cheng HY. The effect of a psychoeducational intervention on stroke family caregivers’ outcomes and stroke survivors’ utilisation of health and social services. Available at: https://repository.lib.cuhk.edu.hk/tc/item/cuhk-1292047. Accessed October 21, 2021.
- 27.Qiu XCH. Effectiveness of a caregiver-centered empowerment program for Chinese stroke family caregivers. Available at:http://easyaccess.lib.cuhk.edu.hk/login?url=https://search.proquest.com/docview/2154466964?accountid=10371. Accessed October 21, 2021.
- 28.Xiong AL. Application of nurse-patient communication skill training in implementation of the high quality nursing. Nurs Integr Tradit Chin Western Med. 2015;1:128–133. [Google Scholar]
- 29.Liu YL, Hu LJ, Huang ZY, Ye B, He YP. Improve communication between aphasic patients and nurses. Nurs J Chin Peoples Liberation Army. 2003;20:33–34. [Google Scholar]
- 30.Guo YX. [Effect of supported conversation training on aphasic patients and their communication partners] [Chinese]. Available at: https://ndltd.ncl.edu.tw/cgi-bin/gs32/gsweb.cgi/ccd=2dVqCl/record?r1=1&h1=1. Accessed October 21, 2021.
- 31.Mao MZ, Li XL, Lin PJ, Liao SX, Peng YH, Wang XH. [Nursing experience on taking care a stroke-induced aphasic patient] [Chinese]. Available at: http://ir.lib.ypu.edu.tw/handle/310904600Q/3004. Accessed October 21, 2021.
- 32.Lin MJ, Chen YC. The nursing experience of caring for a middle-aged patient with aphasia caused by a stroke. Cheng Ching Med J. 2010;6:50–56. [Google Scholar]
- 33.Lu YW, Wei SY. The nursing experience of caring for a patient with aphasia caused by ischemic stroke. Chang Gung Nurs. 2014;25:449–457. [Google Scholar]
- 34.Lin SY, Wu YH. Nursing experience with an intracranial hemorrhage patient. Changhua J Med. 2004;9:277–281. [Google Scholar]
- 35.Guo DY. [Communication strategies for family members of aphasic patients: family members’ perspective] [Chinese]. Available at: https://hdl.handle.net/11296/2c8r56. Accessed October 21, 2021.
- 36.Zhou YC, Zhou YS, Zhao GH. [Guidelines for family rehabilitation training for stroke-induced aphasia] [Chinese] Gems Health. 2011;11:310. [Google Scholar]
- 37.Chang H, Fu YJ. Progress on rehabilitation nursing of post -stroke patients with aphasia. Chinese Nurs Res. 2007;21:1037–1038. [Google Scholar]
- 38.Chen C, Qin CQ, Li WH. [Effect of early rehabilitation on language recovery of acute stroke-induced aphasic patients] [Chinese] Nurs J Chin Peoples Liberation Army. 2003;20:69–70. [Google Scholar]
- 39.Chen H, Yang YF. [Family rehabilitation and nursing guidelines for hemiplegia patients] [Chinese] Nanfang J Nurs. 1999;6:29–30. [Google Scholar]
- 40.Chen YY. [Use of nonverbal interaction to provide emotional support for aphasic patients] [Chinese] Nurs J Chin Peoples Liberation Army. 2003;20:97. [Google Scholar]
- 41.Yang JL, Wang KY. Nursing care for aphasia patients. VGH Nurs. 2002;19:199–203. [Google Scholar]
- 42.Yue ZQ, Feng YR, Xie YX. [Interaction skills between nurses and aphasic patients] [Chinese] J Chengde Med College. 2002;19:44. [Google Scholar]
- 43.Lan Q, Chu LL. [Communication techniques for interacting with aphasic patients] [Chinese] Nurs J of Chin Peoples Liberation Army. 2008;25:56. [Google Scholar]
- 44.Chen MR, Chen XH. [Rehabilitation and nursing for stroke-induced language impairment] [Chinese] Fujian Med J. 2013;35:153–154. [Google Scholar]
- 45.Zhu GH. [Rehabilitation and nursing experience on 58 cases of stroke-induced aphasia] [Chinese] J Contemp Clin Med. 2012;6:73–74. [Google Scholar]
- 46.Li WW, He XJ. Research progress on speech rehabilitation training for patients with post-stroke aphasia. Chinese Nurs Res. 2018;32:3514–3517. [Google Scholar]
- 47.Di Y. [Nursing and care for emotional condition of stroke-induced aphasic patients] [Chinese] Tianjin J Nurs. 2007;15:115–116. [Google Scholar]
- 48.Xing HR, Wang R, Gao GH. [Nursing care of one patient with motor aphasia due to cerebral thrombosis] [Chinese] Chin J Practical Nurs. 2003;19:25. [Google Scholar]
- 49.Xing HR, Gao G. [Nursing for patients with aphasia due to cerebral thrombosis] [Chinese] Nurs J Chin Peoples Liberation Army. 2003;20:16. [Google Scholar]
- 50.Gao S. Peking Union Medical College and Peking Union Medical College; Beijing: 1993. Shiyuzheng [Aphasia] [Chinese] [Google Scholar]
- 51.Avlund K, Schultz-Larsen K, Kreiner S. The measurement of Instrumental ADL: content validity and construct validity. Aging Clin Exp Res. 1993;5:371–383. doi: 10.1007/BF03324192. [DOI] [PubMed] [Google Scholar]
- 52.Sarno MT. Institution of Rehabilitation Medicine; New York: 1969. The Functional Communication Profile: manual of directions. [Google Scholar]
- 53.Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index: a simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 54.Li L. Psychological Health Scale: Generic Quality of Life Inventory-74. Chin J Psychol. 1998:88–95. [Google Scholar]
- 55.World Health Organization. Task shifting: rational redistribution of tasks among health workforce teams: global recommendations and guidelines. Available at: https://www.who.int/healthsystems/TTR-TaskShifting.pdf. Accessed November 10, 2020.
- 56.Zhou B, Zhang J, Zhao Y, et al. Caregiver-delivered stroke rehabilitation in rural China: the recover randomized controlled trial. Stroke. 2019;50:1825–1830. doi: 10.1161/STROKEAHA.118.021558. [DOI] [PubMed] [Google Scholar]
- 57.Lindley RI, Anderson CS, Billot L, et al. Family-led rehabilitation after stroke in India (ATTEND): a randomised controlled trial. Lancet. 2017;390:588–599. doi: 10.1016/S0140-6736(17)31447-2. [DOI] [PubMed] [Google Scholar]
- 58.Vloothuis JD, Mulder M, Veerbeek JM, et al. Caregiver-mediated exercises for improving outcomes after stroke. Cochrane Database Syst Rev. 2016;12 doi: 10.1002/14651858.CD011058.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Togher L, McDonald S, Code C, Grant S. Training communication partners of people with traumatic brain injury: a randomised controlled trial. Aphasiology. 2004;18:313–335. [Google Scholar]
- 60.Ripich DN. Functional communication with AD patients: a caregiver training program. Alzheimer Dis Assoc Dis. 1994;8:95–109. [PubMed] [Google Scholar]
- 61.Kagan A, Black SE, Duchan JF, Simmons-Mackie N, Square P. Training volunteers as conversation partners using "Supported Conversation for Adults with Aphasia" (SCA): a controlled trial. J Speech Lang Hear R. 2001;44:624–638. doi: 10.1044/1092-4388(2001/051). [DOI] [PubMed] [Google Scholar]
- 62.Turner S, Whitworth A. Conversational partner training programmes in aphasia: a review of key themes and participants’ roles. Aphasiology. 2006;20:483–510. [Google Scholar]
- 63.Booth S, Swabey D. Group training in communication skills for carers of adults with aphasia. Int J Lang Comm Dis. 1999;34:291–309. doi: 10.1080/136828299247423. [DOI] [PubMed] [Google Scholar]
- 64.Simmons-Mackie N, Kearns K, Potechin G. Treatment of aphasia through family member training. Aphasiology. 2005;19:583–593. [Google Scholar]
- 65.Hopper T, Holland A, Rewega M. Conversational coaching: treatment outcomes and future directions. Aphasiology. 2002;16:745–761. [Google Scholar]
- 66.Lyon JG, Cariski D, Keisler L, et al. Communication partners: enhancing participation in life and communication for adults with aphasia in natural settings. Aphasiology. 1997;11:693–708. [Google Scholar]
- 67.Jackson J, Kuriyama A. How often do systematic reviews exclude articles not published in English? J Gen Intern Med. 2019;34:1388–1389. doi: 10.1007/s11606-019-04976-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Song F, Parekh S, Hooper L, et al. Dissemination and publication of research findings: an updated review of related biases. Health Technol Assess. 2010;14:1–93. doi: 10.3310/hta14080. [DOI] [PubMed] [Google Scholar]
- 69.Roger P. Bilingual aphasia: the central importance of social and cultural factors in clinically oriented research. Aphasiology. 1998;12:134–137. [Google Scholar]
- 70.Goodglass H, Kaplan E, Barresi B. 3rd ed. Lippincott Williams & Wilkins; Philadelphia: 2001. BDAE-3: Boston Diagnostic Aphasia Examination. [Google Scholar]
- 71.Bauer A, Kulke F. Language exercises for dinner: aspects of aphasia management in family settings. Aphasiology. 2004;18:1135–1160. [Google Scholar]
- 72.Cohen AB, Wu MS, Miller J. Religion and culture: individualism and collectivism in the East and West. J Cross Cult Psychol. 2016;47:1236–1249. [Google Scholar]
- 73.Schwartz SH. Individualism - collectivism: critique and proposed refinements. J Cross Cult Psychol. 1990;21:139–157. [Google Scholar]
- 74.Li HZ. Communicating information in conversations: a cross-cultural comparison. Int J Intercult Rel. 1999;23:387–409. [Google Scholar]
- 75.Gudykunst WB, Matsumoto Y, Ting-Toomey S, Nishida T, Kim K, Heyman S. The influence of cultural individualism-collectivism, self construals, and individual values on communication styles across cultures. Hum Commun Res. 1996;22:510–543. [Google Scholar]
- 76.Bhide A, Shah PS, Acharya G. A simplified guide to randomized controlled trials. Acta Obstet Gynecol Scand. 2018;97:380–387. doi: 10.1111/aogs.13309. [DOI] [PubMed] [Google Scholar]
- 77.Sullivan GM. Getting off the “gold standard”: randomized controlled trials and education research. J Grad Med Ed. 2011;3:285–289. doi: 10.4300/JGME-D-11-00147.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cramer SC. Repairing the human brain after stroke: I. mechanisms of spontaneous recovery. Ann Neurol. 2008;63:272–287. doi: 10.1002/ana.21393. [DOI] [PubMed] [Google Scholar]
- 79.Getchius TSD, Moses LK, French J, Gronseth GS, England JD, Miyasaki J. AAN guidelines: a benefit to the neurologist. Neurology. 2010;75:1126–1127. doi: 10.1212/WNL.0b013e3181f4d883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lomas J, Pickard L, Bester S, Elbard H, Finlayson A, Zoghaib C. The Communicative Effectiveness Index: development and psychometric evaluation of a functional communication measure for adult aphasia. J Speech Hear Dis. 1989;54:113–124. doi: 10.1044/jshd.5401.113. [DOI] [PubMed] [Google Scholar]
- 81.Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 82.Cheng SK, Lam DJ. Relationships among life stress, problem solving, self-esteem, and dysphoria in Hong Kong adolescents: test of a model. J Soc Clin Psychol. 1997;16:343–355. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.