Abstract
Objective
To investigate which tests of hand sensibility correlate with functional outcomes in patients with upper limb traumatic nerve injuries and to assess if composite scales of sensibility correlate with functions.
Data Sources
MEDLINE, Embase, and Cochrane Central Register of Controlled Trials were searched in May 2020, with a supplementary search in July 2020. Reference lists of the included publications were hand searched.
Study Selection
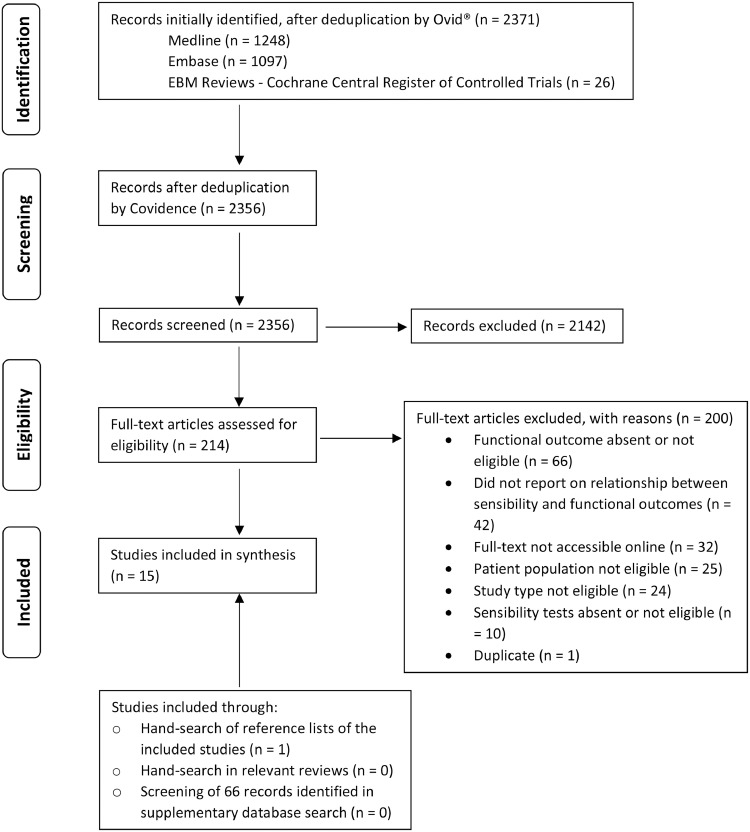
Database search found 2437 records. Eligible studies reported on inferential association between sensibility tests and functions pertaining to adults after upper limb nerve repair. Two reviewers independently assessed eligibility. Fifteen publications were included.
Data Extraction
Extracted data contain patient characteristics, surgical procedure, follow-up duration, sensibility tests, and functional assessments. Two reviewers independently assessed data quality.
Data Synthesis
Fifteen publications involving 849 patients were reviewed. All publications reported on median and/or ulnar nerve injuries. Monofilament tests correlated with Short-Form Health Survey (r=0.548, P<.05), pick-up test (r=0.45, P<.05), and function domain of Patient-Rated Wrist and Hand Evaluation Questionnaire (PRWHE) (r=0.58, P<.05). The 8 studies of static and moving 2-point discrimination provided conflicting correlations with activities of daily living (ADL) and/or the pick-up test. Data for area localization and object/shape identification were equivocal as well. No data were found for Ten test and vibration tests. Rosén score sensory domain correlated with ADL (r=0.59; 95% confidence interval [CI], 0.41-0.72) and PRWHE function domain (r=−0.56, P<.05). Medical Research Council sensory scale was related to pick-up test; return to work status; and Disabilities of the Arm, Shoulder, and Hand questionnaire.
Conclusions
Monofilament tests allow practitioners to gather sensibility data meaningful to patients’ overall recovery of functions after upper limb nerve trauma. For 2-point discrimination and other sensibility tests, practitioners should be aware that improvement in test performance does not necessarily translate to improved hand function. Findings from the composite scales indicate that hand sensibility, in general, is related to functions. Future research on other common sensibility tests is recommended to explore how the test relates to patients’ functions.
KEYWORDS: Activities of daily living, Correlation of data, Peripheral nerve injuries, Recovery of function, Rehabilitation, Touch
List of abbreviations: ADL, activities of daily living; CI, confidence interval; DASH, Disabilities of the Arm, Shoulder, and Hand; m, moving; MRC, Medical Research Council; PNI, peripheral nerve injury; PRWHE, Patient-Rated Wrist and Hand Evaluation; SF-36, Short Form-36 Health Survey; SHFT, Sollerman Hand Function Test; s, static; SWMF, Semmes-Weinstein monofilament; 2-PD, 2-point discrimination; WEST, Weinstein Enhanced Sensory Test
Upper limb peripheral nerve injuries (PNIs) can often result in loss of sensory functions of the hand.1,2 A variety of clinical instruments have been developed to measure hand sensibility and studied on patients recovering from upper limb nerve trauma.3,4 These include Semmes-Weinstein monofilament (SWMF),5 static (s) and moving (m) 2-point discrimination (2-PD),6,7 vibratory sensation test,8 Ten test,9 shape/texture identification,10 area localization,11 and more. There are also composite scoring systems, including the Medical Research Council (MRC) sensory scale12 and Rosén score sensory domain,13 which incorporate 2 or more of the individual instruments to capture the broad construct of sensibility.
As far as we know, despite the popularity of some of these tests, no systematic discussion exists on if improvements in sensibility measured by these instruments translate to an improvement in patients’ daily functions. It is well established that PNI of the upper limb can have a profound effect on patients’ ability to perform activities of daily living (ADL), ability to perform work duties, and quality of life.14, 15, 16, 17, 18 Jaquet et al14 found that 24% of patients with median and/or ulnar injuries still had loss of income even after 17.7 months. A test that better correlates with the functional aspects of life could therefore offer more meaningful information about a patient's recovery.
To help health care professionals select the optimal tests of sensibility, there have been ongoing discussions on the psychometric properties of sensibility tests, such as reliability and validity, in a variety of injuries and other neurologic conditions.19, 20, 21, 22 However, in the context of upper limb PNI, there still exist uncertainties in choosing the optimal sensibility tests. For example, Jerosch-Herold4 identified that 2-PD has limited validity and responsiveness yet remains widely used in the PNI setting. By gathering evidence on the correlation between sensibility tests and patients’ functions, we hope to add a novel perspective to help health care professionals make a more informed choice when selecting sensibility tests in the population with PNI. Although there have been studies that contain data of association between sensibility and functions,11,13, 14, 15 many focused on only 1 sensibility test or 1 functional outcome. On the other hand, our review provides an additional bird's-eye view on their correlations, and our results can also be used as a springboard to measure sensibility more robustly and comprehensively going forward.
Besides individual sensibility tests, it is also important to elucidate if the composite such as the MRC sensory scale and Rosén score sensory domain correlate with patients’ functions because they are often used to represent the general recovery of patients’ sensibility. When Rosén and Lundborg13 constructed the Rosén score, they found a correlation between the sensory domain and patients’ estimation of the effect of injury on ADL (r=0.59; 95% CI, 0.41-0.72). However, more work is needed to elucidate if patients with better sensibility have better daily functions. This may strengthen or reduce the value of the significant efforts being made to help regain sensibility, such as sensory reeducation,23 neuroprotection of sensory neurons,24 and sensory nerve transfer.25
There are 2 objectives for this systematic review focused on traumatic upper limb PNI. The primary objective was to assess which individual tests of hand sensibility correlate with functional outcomes. The secondary objective was to assess if the MRC sensory scale and Rosén score sensory domain correlate with functions.
Methods
This systematic review was performed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses.26
Criteria for considering studies for this review
The research question and eligibility criteria were established a priori. Inclusion criteria were (1) full-length publications; (2) English publications; (3) studies that involved adult patients (age>18y); (4) patients had surgical repair of traumatic upper limb nerve injuries (traumatic brachial plexopathy and/or distal nerve injuries); and (5) studies reporting on sensibility and functional outcomes with inferential measures of association.
Examples of sensibility measures or sensory tests included in search terms were SWMF, s2-PD, m2-PD, vibratory sensation test, Ten test, object identification, localization, sensory nerve action potential,27 sensory domain of Rosén score, and MRC sensory scales.
The scope of functional outcomes captured the ability to perform functional activities. We included hands-on tests derived from ADL, such as the Sollerman Hand Function Test (SHFT),28 or quantitative questionnaires assessing ADL, such as the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire29 and Patient-Rated Wrist and Hand Evaluation (PRWHE).30 Tests that assess sensorimotor performance of the hand were also deemed relevant (eg, Moberg pick-up test31). To capture a broader perspective, return to work status and assessments of quality of life such as the Short Form-36 Health Survey (SF-36)32 were also considered. Simple motor measures such as strength and range of motion were not deemed to encompass the broad construct of functional outcome and were not included. Search terms used are presented in appendices 1 and 2.
Exclusion criteria were (1) case reports and gray literature (eg, annual reports, theses, conference proceedings); (2) studies focused exclusively on pediatric patients; (3) isolated digital nerve injuries; (4) nerve compression and neuropathy; and (5) amputations and iatrogenic injuries. Isolated digital nerve injuries were excluded because they often result in very specific functional loss of a single digit rather than impairments in gross functions.33 Nerve compression and neuropathy were excluded because they are usually unrelated to trauma.
Data sources and searches
The search was conducted on May 16, 2020, via Ovida on MEDLINE, Embase, Evidence-Based Medicine Reviews: Cochrane Central Register of Controlled Trials inception to search date. Search terms from sensibility measures were combined with OR: monofilament OR 2 point discrimination OR . . .; keywords representing functional outcomes were combined with OR: DASH OR PRWHE OR . . .; keywords describing patient population were combined with OR: median nerve OR ulnar nerve OR . . . . The 3 categories (sensibility, functions, patient population) were combined with AND. Limiters were “English Language” and “Humans.” A supplementary search was done on July 7, 2020, to include new search terms informed by the first round of review. Full search strategies are presented in appendices 1 and 2.
Study selection
Screening and selection of studies was conducted on Covidence.b Titles and abstracts were screened independently by 2 study authors. References excluded by both reviewers were excluded. The studies remaining had their full texts assessed by each reviewer, and conflicts were resolved by discussion. Reference lists of the included studies were hand searched to identify additional eligible publications. Relevant reviews identified from the search results were also hand searched to identify eligible primary studies.
Data extraction and critical appraisal
Two reviewers (L.C. and E.O.) performed data extraction and quality appraisal. All data were obtained from published materials. Some included studies contained patient-level data, whereas some presented summarized data only. Major discrepancies were resolved by discussions. Data form and appraisal checklist (appendix 3) were adapted from the National Institute for Health and Care Excellence: Methods for the Development of NICE Public Health Guidance (Third edition), appendices K and G.34 The appraisal checklist contains 3 items on external validity and 6 items on internal validity. Each item is rated 0-2. A score of 5 of 6 is needed for high external validity, and 9 of 12 is needed for high internal validity.
Data analysis
Interrater reliability for study selection was assessed by Cohen's κ.35 Study level data on associations between sensibility and functional outcomes were identified for each sensibility test and presented in tabular format.
Results
Study selection
Study selection is summarized in figure 1. Interrater agreement for title and abstract screening was moderate (κ=0.43), and agreement for full-text selection was substantial (κ=0.78).37 Fifteen studies were included.
Fig 1.
Adapted flow diagram from Preferred Reporting Items for Systematic Reviews and Meta-Analyses.36 Abbreviation: EBM, Evidence-Based Medicine.
Update of literature search and results
To ensure the results of the review is up to date, an updated literature search was performed on July 10, 2021, with the same strategy and databases outlined in appendices 1 and 2. An additional limiter of publication year of 2020 to present was added. A total of 209 records were found; stepwise screening of title, abstract, and full-text identified no eligible studies.
Study characteristics
Study characteristics are summarized in table 1. Of the 15 included studies, all were published between 1987 and 2019. Nine studies were level IV evidence, 3 were III, and 3 were II, according to the Oxford Centre for Evidence-based Medicine classification.50 The 15 studies reported on 849 patients, most of which were male. Mean age of patients in each study ranged from 20-42 years. Sample sizes ranged from 14-220 (mean, 53±51). The nerves injured were either median (n=524, 62%), ulnar (n=219, 26%), or both (n=106, 12%). Types of transection were either complete, partial, or not reported. Locations of lesion were mostly at wrist, forearm, or elbow. Most injuries were repaired by primary suture. Some studies did not specify surgery delay, but primary suture usually implied direct suture of nerve ends within 1 week of injury.52 The mean follow-up time ranged from 1-8.1 years.
Table 1.
Characteristics and quality of included studies
| Author, Region | Level of Evidence* | Sample Size, Mean Age and Range (Y) | Nerves Injured (Location) | Surgery Technique (Delay) | Mean Follow-Up and Range (Y) | External/ Internal Validity† |
|---|---|---|---|---|---|---|
| Brink and Mackel,38 US | Prognostic IV | 26, NA (adults) | Median and/or ulnar complete‡ (wrist) | Suture or graft (NA) | 1 (0.5-1.9) | Mid/mid |
| Bruyns et al,39 Netherlands | Prognostic III | 81, 31 (18-58) | Median and/or ulnar (elbow to wrist) | Primary repair | NA | High/high |
| Chassard et al,40 France | Prognostic IV | 22, 30 (5-66) | Median and ulnar (forearm to wrist) | Primary nerve suture; nerve graft (1-6m) | 6.7 (1-14.7) | Low/mid |
| Emamhadi et al,15 Iran | Prognostic II | 106, 33 (12-68) | Median complete/partial (between shoulder and wrist) | Primary suture; external neurolysis or graft (< 29m) | <2 y, n=25 2-5 y, n=43 >5 y, n=38 | Mid/high |
| Fonseca et al,41 Canada | Diagnostic III | 32, 42±16 | Median or ulnar, complete/partial (about half at volar wrist) | Suture or nerve reconstruction (<2wk) | 4.7 (1-8) | High/high |
| Jaquet et al,14 Netherlands | Prognostic II | 220, 31 (5-73) | Median and/or ulnar, complete/partial (elbow to wrist) | Primary repair | 1.5 (0.1-14.4) | High/high |
| Jerosch-Herold,42 1993, UK | Prognostic IV | 14, 38 (19-61) | Median complete/partial (wrist) | Primary repair | 4 (2-7.5) | High/high |
| Jerosch-Herold,43 2000, UK | Prognostic IV | 41, 33 (12-72) | Median complete (forearm to wrist) | Epineural/perineural suture or grafting, or both (average 3d) | 2.8 (0.8-7.5) | Mid/high |
| Marsh11 UK§ | Prognostic IV | 21, 23 (6-57) | Median and/or ulnar complete (elbow to wrist) | Nerve suture (0-111d) | 3.9 (0.6-11.2) | High/high |
| Onne,44 NA|| | Not applicable | 30, 20 (4-46) | Median complete (NA) | NA (NA) | ≥4y | Mid/high |
| Rosén,45 Sweden | Prognostic IV | 25, 27 (10-53) | Median/ulnar complete (distal forearm) | Conventional suture or tubulization (≤2wk) | 3 (2-5) | Mid/mid |
| Rosén and Lundborg,13 Sweden | Diagnostic III | 70, median=28 (5-72) | Median and/or ulnar, complete/partial (distal forearm to wrist) | Primary suture; primary silicone tube; grafting (NA) | 2 (0.3-5.7) | Mid/high |
| Sahin et al,46 Turkey | Prognostic IV | 40, 29 (18-57) | Median/ulnar complete (wrist) | Epineural suture (average 9.3d) | 1 (0.5-2.5) | Mid/high |
| Selma et al,47 Turkey | Prognostic IV | 28, 25 (4-45) | Median (wrist) | Epineurial suture (0d for most) | 2.1 (1-4) | High/mid |
| Vordemvenne et al,48 Germany | Prognostic II | 65, 28 (2-69) | Median complete/partial and/or ulnar complete (forearm to wrist) | Microsurgical or group fascicular suture (≤1d) | 8.1 (1-12.9) | Mid/high |
| Wong et al,49 Netherlands | Prognostic IV | 28, 28±12 | Median (mean distance between lesion and index fingertip was 25cm) | Primary repair; autologous nerve grafts (NA) | 5.2 (1.5-10.7) | Mid/mid |
Abbreviations: NA, not available; UK, United Kingdom; US, United States.
Based on Levels of Evidence by Oxford Centre for Evidence-Based Medicine.50
Criteria of assessment reported in appendix 3.
Complete/partial denotes the extent of transection, if mentioned by the study.
A portion of the data on patient recruitment was extracted from a previous publication by Marsh and Barton.51
Quality assessment
Internal and external validity are presented in table 1. A total of 67% of studies demonstrated high internal validity. Inadequate control of extraneous variables and omission of correlation strength were recurring limitations identified. Ratings of internal validity only pertained to the relevant analysis of correlations and/or associations and are not applicable to other results reported by the studies. A total of 38% demonstrated high external validity. For some studies, the reporting of study design or recruitment method were incomplete. Details on individual quality items are presented in appendix 3.
Results for sensibility measures
Associations between sensibility measures and functional outcomes are presented in table 2. Correlation coefficient (r) denotes correlation strength. There is no defined nomenclature for correlation strength, but some guidelines have been proposed: absolute value of r<0.25, little relationship; 0.25-0.50, low to fair; 0.50-0.75, moderate to good; >0.75, strong.55 Some studies used factor analysis. Factor loadings measure the correlation between the variable of interest and the factor, with loadings >0.4 generally considered meaningful.55 Each factor represents a cluster of items highly correlated among themselves.55
Table 2.
Relationship between sensibility measures and functional outcomes
| Study | Functional Outcomes | Relationship With Sensibility Tests | Factors Controlled |
|---|---|---|---|
| Monofilament tests | |||
| Bruyns et al39 | RTW within 1 y | Groups of RTW and no RTW had SWMF score of 2.9 and 3.5 (P=.001) (SWMF scored from 1-5, 5 representing the largest diameter). | Sex, age, hand dominance |
| Emamhadi et al15 | SF-36 | Correlation with SWMF: r=0.548, P=.0001, Spearman. | \ |
| Fonseca et al41 | PRWHE–function domain | Correlation with SWMF: r=0.58, P<.01, 2-tailed, Pearson. | \ |
| Jerosch-Herold,43 2000 | Modified pick-up | Correlation with Weinstein Enhanced Sensory Test: r=0.45, P=.009, Spearman. | \ |
| Onne44,* | Pick-up test | Correlation with von Frey hair: r=−0.66, P<.01, Pearson. | Age |
| Rosén and Lundborg13 | Finger dexterity (task 4, 8, 10 of SHFT) | By factor analysis, SWMF and finger dexterity both have meaningful loadings (0.58, 0.63) to the sensory factor. | NA |
| Static 2-PD | |||
| Brink and Mackel38 | Simplified pick-up test | No association between 2-PD (<18 vs >18mm) and pick-up (normal/satisfactory vs mediocre/poor performance), P>.1, Fisher exact test. | \ |
| Chassard et al40 | Functional score defined as the mean of modified pick-up test, shape recognition, texture recognition | r=unk, P<.005, multiple regression. | Age |
| Onne44,* | Pick-up test | r=−0.22, P=.22, Pearson. | Age |
| Jerosch-Herold42 1993 | Modified pick-up | r=0.81, P<.001, partial correlation analysis. | Age, surgery delay, time since injury |
| ADL tests with 4 daily tasks | r=−0.524, P=nonsignificant, partial correlation analysis. | ||
| Jerosch-Herold43 2000 | Modified pick-up | r=−0.38, P=.015, Spearman. | Age |
| Rosén45 | ADL questionnaire | r=unk, P>.05, Spearman. | \ |
| Rosén and Lundborg13 | Finger dexterity | By factor analysis, s2-PD and finger dexterity both had meaningful loadings (0.84, 0.63) to the sensory factor. | NA |
| Moving 2-PD | |||
| Chassard et al40 | Functional score | r=unk, P<.005, multiple regression. | Age |
| Marsh11 | Modified pick-up | r=0.13, P=0.21, Pearson. | Age, surgery delay, time since surgery |
| Wong et al49 | Modified pick-up | r=0.19, P=unk, Spearman. | \ |
| Jerosch-Herold42 1993 | Modified pick-up | r=0.78, P<.001, partial correlation analysis. | Age, surgery delay, time since injury |
| ADL test | r=−0.553, P=0.041, partial correlation analysis. | ||
| Rosén45 | ADL questionnaire | Influence of m2-PD on ADL was weak with stepwise multiple regression. | Grip strength, cold intolerance, age |
| Area localization | |||
| Marsh11 | Modified pick-up | r=0.48, P=.001, Pearson. | Age, surgery delay, time since surgery |
| Jerosch-Herold42 1993 | Modified pick-up |
r=0.516, P=nonsignificant, partial correlation analysis. |
Age, surgery delay, time since injury |
| ADL test | r=−0.57, P=.045, partial correlation analysis. | ||
| Jerosch-Herold43 2000 | Modified pick-up | r=0.29, P=.07, Spearman. | \ |
| Rosén45 | ADL questionnaire | r=unk, P>.05, Spearman. | \ |
| Object/shape identification | |||
| Brink and Mackel38 | Sensory component of a simplified pick-up test | No correlation between the no. of errors in object identification (round vs edgy) and pick-up, r=−0.039, P>.1, Spearman. | \ |
| Wong et al49 | Modified pick-up | Moberg recognition test and pick-up did not correlate well, r=0.35, P>.05, Spearman. | \ |
| Jerosch-Herold42 1993 | Modified pick-up | Identification time and accuracy correlated with pick-up, r=0.683 and 0.697, P<.001, partial correlation analysis. | Age, surgery delay, time since injury |
| ADL test | Identification time did not correlate with ADL, r=−0.369, P=nonsignificant; accuracy did correlate, r=−0.471, P=0.042, partial correlation analysis. | ||
| Rosén45 | ADL questionnaire | Shape identification, object identification, and the number of correctly identified items in a modified pick-up test were not significantly related to ADL, r=unk, P>.05, Spearman. | \ |
| Rosén and Lundborg13 | Finger dexterity | By factor analysis, shape/texture identification and finger dexterity both had meaningful loadings (0.70, 0.63) to the sensory factor. | NA |
| Sensory nerve action potential amplitude | |||
| Sahin et al46 | SHFT | r=0.111, P=.50, Pearson. | \ |
| Rosén score sensory domain | |||
| Fonseca et al41 | PRWHE–function domain | r=−0.56, P<.01, 2-tailed, Pearson. | \ |
| Rosén and Lundborg13 | Estimation of effect of injury on ADL via visual analog scale | r=0.59; 95% CI, 0.41-0.72; Spearman. | \ |
| Vordemvenne et al48 | DASH | In a 3-factor analysis (factors: sensory, motor, ADL), sensory domain of Rosén score and DASH both had meaningful loadings (0.874, 0.552) on the sensory factor. Sensory domain of Rosén score loaded weakly (0.195) on the ADL factor (a factor primarily contributed by the pain/discomfort domain of Rosén score and DASH). |
NA |
| MRC sensory scales† | |||
| Jaquet et al14 | RTW-yes/no | Poor sensory recovery had an odds ratio of 2.94 for inability to return to work; 95% CI, 1.50–5.76; P=.002. | Age, sex |
| Selma et al47 | Moberg's pick-up | Means of the pick-up performance between 2 groups (S3+, S4 vs S1, S2, S2+, S3) were different, P<.05, Mann-Whitney U. | \ |
| Vordemvenne et al48 | DASH | In the 3-factor analysis, MRC sensory score and DASH both had meaningful loadings (0.863, 0.552) on the sensory factor. MRC sensory score loaded weakly (0.123) on the ADL factor. |
NA |
Monofilament tests
Monofilament tests consistently demonstrated correlation with functional assessments. SWMF correlated with SF-36 (r=0.548, P=.0001) and PRWHE function domain (r=0.58, P<.01).15,41 Factor analysis by Rosén and Lundborg13 also suggested a correlation between SWMF and finger dexterity. In the study by Bruyns et al,39 a significant difference in SWMF score was present between patients who returned to work vs those who did not (P=.001). In addition, Weinstein Enhanced Sensory Test (r=0.45, P=.009) and von Frey hair (r=-0.66, P<.01) both correlated with the pick-up test.11,43,44
Two-point discrimination
Results for s2-PD were equivocal. No significant correlation was demonstrated with ADL.42,45 Two studies demonstrated strong and low to fair correlations with pick-up test (r=0.81, P<.001; r=−0.38, P=.015),42,43 whereas 2 others found no association.11,38,44 Chassard et al40 showed a significant correlation with their functional score (r=unknown, P<.005). Factor analysis suggested a correlation with finger dexterity.13
For m2-PD, Jerosch-Herold42 found a moderate correlation with ADL (r=−0.553, P=.041), whereas Rosén45 demonstrated that the correlation may be accounted for by covariates including grip strength and cold intolerance. Evidence on its relationship with pick-up test was mixed, with both significant (r=0.78, P<.001)42 and nonsignificant or weak correlations.11,49 Chassard et al40 demonstrated a significant correlation with their functional score (r=unknown, P<.005).
Area localization
For the ability to localize touch stimulus applied to distinct skin areas, 1 study found a moderate correlation with ADL (r=−0.57, P=.045),42 whereas another found no correlation.45 Its correlation with pick-up test was demonstrated with fair association by Marsh11 (r=0.48, P=.001), but 2 other studies found no significance.42,43
Object and/or shape identification
Accuracy of object identification was shown to correlate with ADL (r=−0.471, P=.042), but the speed of identification was not.42 Rosén45 found no aspect of object identification correlated with the ADL questionnaire. The correlations with pick-up test were demonstrated with significance in 1 study (r=0.683 and 0.697, P<.001)42 but nonsignificance in another 2.38,49 Factor analysis suggested that shape and/or texture identification and finger dexterity were related.13
Sensory nerve action potential amplitude
Sahin et al46 addressed the relationship between sensory nerve action potential and SHFT, and no significant correlation was demonstrated.
Rosén score sensory domain and MRC sensory scales
Although factor analysis suggested equivocal results for their correlation with DASH,48 other evidences were all supportive. Rosén score sensory domain correlated with PRWHE function domain (r=−0.56, P<.01) and ADL (r=0.59; 95% CI, 0.41-0.72).13,41 Lower score on MRC sensory scale predicted inability to return to work (odds ratio, 2.94; 95% CI, 1.50-5.76; P=.002) and was also associated with poorer pick-up performance (P<.05).14,47
Discussion
Monofilament tests correlated with various functional assessments in all studies. Evidences for s2-PD, m2-PD, area localization, and object identification were each equivocal. Evidences for vibratory sensory test, Ten test, sensory nerve action potential, and other sensibility measures were scarce. For MRC sensory scale and Rosén score sensory domain, most studies demonstrated their association with functional outcomes.
Heterogeneity in sensibility tests and functional outcomes
The lack of standardization in some sensibility measures makes it difficult to generalize results across studies. The objects used and the procedures in testing object and/or shape identification were not consistent.13,38,42,45,49 The outcomes of identification also measured different aspects of the performance, such as accuracy and speed.42 For the MRC sensory scale, different versions have also been used.14,47,48
A similar problem exists for ADL and pick-up test. The concept of ADL was quantified differently, including questionnaire,45 visual analog scale,13 and observed performance of daily tasks.42 For the pick-up test, 1 study simplified the test by using balls.38 Another study reported the test results differently, where a combined score was reported as the mean score of the pick-up test, shape recognition, and texture recognition.40 The score of the pick-up test was therefore diluted. The variability in functional outcomes reported in literature makes it unfeasible to quantitatively aggregate the data for each sensibility test, which limits the robustness of our findings.
It is also important to examine the psychometric properties of the functional assessments. Pick-up test has high interrater reliability and test-retest reliability.56,57 Validity and reliability of PRWHE is supported by systematic review.58 These properties for DASH and SHFT are also well supported.28,59 Some functional assessments on ADL were developed or validated by the study authors,13,42,45 and their psychometric properties may vary.
Interpretation of correlation and confounding variables
Some studies reported statistical significance only, and the strength of correlation or effect size cannot be assessed.40,45,47 In contrast, there were correlations with moderate strength but statistically nonsignificant.42 The nonsignificance may be because of small sample size,42 and the results may still have clinical value.
Eight studies did not control for extraneous variables when examining the relationship between sensibility and functional outcomes.13,15,38,41,46, 47, 48, 49 Seven studies controlled for 1 or more of age, surgery delay, follow-up time, sex, hand dominance, grip strength, and cold intolerance, as shown in table 2.11,14,39,40,42,43,45 These variables may or may not be related to sensibility test performance or function outcomes; below are what the included studies found. Age correlated with SWMF, s2-PD, and m2-PD for median nerve lacerations at wrist.47 The effect of age on ADL and DASH was found equivocal.45,48 The nerves injured (median vs ulnar)46,48 and the extent of injury (partial vs complete transection)41,42 had no significant association with ADL performance, although 1 study showed significant difference in SHFT results between median and ulnar nerve injuries.45 The prognostic value of the number of nerves injured (combined median-ulnar injuries vs isolated nerve injuries) on return to work status was inconsistent.14,39 Surgery delay (0-111 days) was not found to affect pick-up test performance.11 The timing of follow-up since surgery did not correlate with pick-up performance.43
Study limitations
A limitation is the literature search only yielded studies related to median and ulnar nerve injuries. There were no studies pertaining to other upper limb nerve injury distributions, such as brachial plexus injury. Although the sensory innervation of hand is mostly supplied by median and ulnar nerve,60 it is also important to examine more proximal injuries on the brachial plexus. This limits the generalizability of our systematic review and also identifies a potential gap in the literature on upper limb nerve injuries for further exploration. This review targeted adults. Some studies included pediatric patients,11,13,15,40,43,45,47, 48, 49 but they were usually a small proportion. Although only studies in English were considered, this review still captured studies from 9 different countries. Eight studies did not control for extraneous variables as shown in table 2.13,15,38,41,46, 47, 48, 49 The relationship between these variables and sensibility tests or functional outcomes is equivocal as previously discussed.
Study strengths
The search strategy was thoughtfully designed. The search terms included a wide array of functional assessments to encapsulate their diversity, although many did not yield relevant results. Besides specific names of sensibility tests and functional assessments, general terminologies such as “sensibility,” “sensory,” and “recovery of function” were used to increase sensitivity of the search. The reviewers also conducted a supplementary search to capture additional relevant terms informed by the original search to further pursue comprehensiveness.
Clinical implications and future research
When choosing a sensibility test, one also needs to consider its psychometric properties and simplicity of use.61 Reliability of SWMF to measure hand sensibility has been demonstrated by 2 systematic reviews.4,62 Responsiveness of SWMF and Weinstein Enhanced Sensory Test (WEST) was demonstrated by Rosén et al63 and Jerosch-Herold64 with effect size of 1.5 between 3 and 48 months, and 1.2 between 6 and 18 months, respectively. Although the use of SWMF apparatus was reported to be time consuming in busy clinics,65 WEST was subsequently developed for improved portability and more rapid testing.66 Given these attributes, along with their correlations with SF-36, PRWHE function domain, and pick-up test (r=0.548, 0.58, 0.45 respectively; P<.05),15,41,43 SWMF and WEST allow rehabilitation professionals to reliably gather data on hand sensibility that are meaningful to patients’ functions.
The validity and responsiveness of 2-PD have been challenged by previous study.4 In this review, the correlations between s2-PD or m2-PD and pick-up test or ADL were equivocal, it is therefore questionable if improved 2-PD translates to improved functions. The widespread use of 2-PD to assess hand sensibility remains to be justified by future research. For other sensibility tests, evidences from this review are equivocal and limited by the lack of standardization of tests. Their clinical use is subject to practitioners’ discretion.
Interestingly, MRC sensory scale and Rosén score sensory domain demonstrate correlations with functions in this review, although both contain 2-PD as a component. The use of 2-PD may therefore be more appropriate in conjunction with other sensibility tests to represent the broad construct of sensibility rather than used alone.
Among the sensibility tests with limited data for their correlation with functions, Ten test is gaining popularity for its simplicity without special equipment,9 and its use in hand trauma patients was recently shown to have high interrater reliability and responsiveness.67 Future research is recommended to explore its relationship with hand functions.
Conclusions
Monofilament tests demonstrated consistent correlations with assessments on patients’ hand functions, quality of life, and ability to work. They allow practitioners to gather hand sensibility data relevant to patients’ overall recovery of functions after nerve injury. For 2-PD and other sensibility tests, improvement in test performance does not necessarily translate to improved hand function in trauma patients, and practitioners should be aware of this limitation. MRC sensory scale and Rosén score sensory domain demonstrated correlations with hand functions and activities of daily living. Results from these composite scores indicate that patients with better sensibility in general tend to have better hand functions and capacity for daily activities, and this bolsters the value of the endeavors made to improve sensibility recovery in patients with upper limb PNI.
Suppliers
-
a.
Ovid; Ovid Technologies Inc.
-
b.
Covidence; Veritas Health Innovation Ltd.
Footnotes
Presented to the Canadian Association of Physical Medicine & Rehabilitation, May 28, 2021, virtual.
Supported by the Blusson Integrated Cures Partnership - Rick Hansen Foundation (grant no. GR015197). Michael J. Berger is supported by the Vancouver Coastal Health Research Institute Mentored Clinician-Scientist Award (grant no. GR015189). Liheng Chen is supported by the Flexible and Enhanced Learning course as a part of Doctor of Medicine Undergraduate Program at the University of British Columbia.
Disclosures: none
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.arrct.2021.100159.
Appendix. Supplementary materials
References
- 1.He B, Zhu Z, Zhu Q, et al. Factors predicting sensory and motor recovery after the repair of upper limb peripheral nerve injuries. Neural Regen Res. 2014;9:661–672. doi: 10.4103/1673-5374.130094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ruijs ACJ, Jaquet J, Kalmijn S, Giele H, Hovius SER. Median and ulnar nerve injuries: a meta-analysis of predictors of motor and sensory recovery after modern microsurgical nerve repair. Plast Reconstr Surg. 2005;116:484–494. doi: 10.1097/01.prs.0000172896.86594.07. [DOI] [PubMed] [Google Scholar]
- 3.Novak CB. Evaluation of hand sensibility: a review. J Hand Ther. 2001;14:266–272. doi: 10.1016/s0894-1130(01)80004-1. [DOI] [PubMed] [Google Scholar]
- 4.Jerosch-Herold C. Assessment of sensibility after nerve injury and repair: a systematic review of evidence for validity, reliability and responsiveness of tests. J Hand Surg Br. 2005;30:252–264. doi: 10.1016/j.jhsb.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Weinstein S. Tactile sensitivity of the phalanges. Percept Mot Skills. 1962;14:351–354. doi: 10.2466/pms.1962.14.3.351. [DOI] [PubMed] [Google Scholar]
- 6.Dellon AL, Mackinnon SE, Crosby PM. Reliability of two-point discrimination measurements. J Hand Surg. 1987;12:693–696. doi: 10.1016/s0363-5023(87)80049-7. [DOI] [PubMed] [Google Scholar]
- 7.Dellon AL. The moving two-point discrimination test: clinical evaluation of the quickly adapting fiber/receptor system. J Hand Surg. 1978;3:474–481. doi: 10.1016/s0363-5023(78)80143-9. [DOI] [PubMed] [Google Scholar]
- 8.Reggars JW. Vibratory sensation testing: practice tip. COMSIG Rev. 1995;4:14–15. [Google Scholar]
- 9.Strauch B, Lang A, Ferder M, Keyes-Ford M, Freeman K, Newstein D. The Ten test. Plast Reconstr Surg. 1997;99:1074–1078. doi: 10.1097/00006534-199704000-00023. [DOI] [PubMed] [Google Scholar]
- 10.Rosén B, Lundborg G. A new tactile gnosis instrument in sensibility testing. J Hand Ther. 1998;11:251–257. doi: 10.1016/s0894-1130(98)80020-3. [DOI] [PubMed] [Google Scholar]
- 11.Marsh D. The validation of measures of outcome following suture of divided peripheral nerves supplying the hand. J Hand Surg Br. 1990;15B:25–34. doi: 10.1016/0266-7681_90_90043-4. [DOI] [PubMed] [Google Scholar]
- 12.Medical Research Council . In: Peripheral nerve injuries. Seddon HJ, editor. Her Majesty's Stationer Office; London, United Kingdom: 1954. Results of nerve suture. editor. [Google Scholar]
- 13.Rosén B, Lundborg G. A model instrument for the documentation of outcome after nerve repair. J Hand Surg. 2000;25A:535–543. doi: 10.1053/jhsu.2000.6458. [DOI] [PubMed] [Google Scholar]
- 14.Jaquet J, Luijsterburg A, Kalmijn S, Kuypers P, Hofman A, Hovius S. Median, ulnar, and combined median-ulnar nerve injuries: functional outcome and return to productivity. J Trauma. 2001;51:687–692. doi: 10.1097/00005373-200110000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Emamhadi M, Behzadnia H, Andalib S. Long-term surgical outcome of median nerve injuries. Formos J Surg. 2019;52:71–75. [Google Scholar]
- 16.Novak CB, Anastakis DJ, Beaton DE, Katz J. Patient-reported outcome after peripheral nerve injury. J Hand Surg. 2009;34:281–287. doi: 10.1016/j.jhsa.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 17.Rosberg H, Carlsson KS, Cederlund RI, Ramel E, Dahlin LB. Costs and outcome for serious hand and arm injuries during the first year after trauma - a prospective study. BMC Public Health. 2013;13:501. doi: 10.1186/1471-2458-13-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ciaramitaro P, Mondelli M, Logullo F, et al. Traumatic peripheral nerve injuries: epidemiological findings, neuropathic pain and quality of life in 158 patients. J Peripher Nerv Syst. 2010;15:120–127. doi: 10.1111/j.1529-8027.2010.00260.x. [DOI] [PubMed] [Google Scholar]
- 19.Suda M, Kawakami M, Okuyama K, et al. Validity and reliability of the Semmes-Weinstein Monofilament Test and the Thumb Localizing Test in patients with stroke. Front Neurol 2020. 2021;11 doi: 10.3389/fneur.2020.625917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bagherzadeh Cham M, Mohseni-Bandpei MA, Bahramizadeh M, Kalbasi S, Biglarian A. Reliability of Semmes-Weinstein monofilaments and tuning fork on pressure and vibration sensation measurements in diabetic patients. Iran Rehabil J. 2019;17:1–8. [Google Scholar]
- 21.Taylor SC, Atkinson G, Dixon J, Robinson JR, Ryan CG. Test-retest reliability of the two-point discrimination test on the sole of the foot in people with multiple sclerosis. Physiol Meas. 2020;41:11NT01. doi: 10.1088/1361-6579/abc4c6. [DOI] [PubMed] [Google Scholar]
- 22.Ehrenbrusthoff K, Ryan CG, Grüneberg C, Martin DJ. A systematic review and meta-analysis of the reliability and validity of sensorimotor measurement instruments in people with chronic low back pain. Musculoskelet Sci Pract. 2018;35:73–83. doi: 10.1016/j.msksp.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 23.Rosén B, Balkeniu C, Lundborg G. Sensory re-education today and tomorrow: a review of evolving concepts. Br J Hand Ther. 2003;8:48–56. [Google Scholar]
- 24.Hart AM, Terenghi G, Wiberg M. Neuronal death after peripheral nerve injury and experimental strategies for neuroprotection. Neurol Res. 2008;30:999–1011. doi: 10.1179/174313208X362479. [DOI] [PubMed] [Google Scholar]
- 25.Domeshek LF, Novak CB, Patterson JMM, et al. Nerve transfers—a paradigm shift in the reconstructive ladder. Plast Reconstr Surg Glob Open. 2019;7:e2290. doi: 10.1097/GOX.0000000000002290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mallik A, Weir AI. Nerve conduction studies: essentials and pitfalls in practice. J Neurol Neurosurg Psychiatry. 2005;76(Suppl 2):ii23–ii31. doi: 10.1136/jnnp.2005.069138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sollerman C, Ejeskär A. Sollerman Hand Function Test: a standardised method and its use in tetraplegic patients. Scand J Plast Reconstr Surg Hand Surg. 1995;29:167–176. doi: 10.3109/02844319509034334. [DOI] [PubMed] [Google Scholar]
- 29.Hudak PL, Amadio PC, Bombardier C, et al. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder, and Head) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 30.MacDermid JC. Development of a scale for patient rating of wrist pain and disability. J Hand Ther. 1996;9:178–183. doi: 10.1016/s0894-1130(96)80076-7. [DOI] [PubMed] [Google Scholar]
- 31.Moberg E. Objective methods for determining the functional value of sensibility in the hand. J Bone Joint Surg Br. 1958;40-B:454–476. doi: 10.1302/0301-620X.40B3.454. [DOI] [PubMed] [Google Scholar]
- 32.Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 33.Jain A, Dunlop R, Hems T, Tang JB. Outcomes of surgical repair of a single digital nerve in adults. J Hand Surg Eur Vol. 2019;44:560–565. doi: 10.1177/1753193419846761. [DOI] [PubMed] [Google Scholar]
- 34.National Institute for Health and Clinical Excellence . 3rd ed. National Institute for Health and Care Excellence; London, UK: 2012. Methods for the development of NICE public health guidance. [PubMed] [Google Scholar]
- 35.Cohen J. A Coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- 36.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 37.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 38.Brink EE, Mackel R. Sensorimotor performance of the hand during peripheral nerve regeneration. J Neurol Sci. 1987;77:249–266. doi: 10.1016/0022-510x(87)90127-4. [DOI] [PubMed] [Google Scholar]
- 39.Bruyns CNP, Jaquet J, Schreuders TAR, Kalmijn S, Kuypers PDL, Hovius SER. Predictors for return to work in patients with median and ulnar nerve injuries. J Hand Surg. 2003;28A:28–34. doi: 10.1053/jhsu.2003.50026. [DOI] [PubMed] [Google Scholar]
- 40.Chassard M, Pham E, Comtet JJ. Two-point discrimination tests versus functional sensory recovery in both median and ulnar nerve complete transections. J Hand Surg Br. 1993;18B:790–796. doi: 10.1016/0266-7681(93)90247-d. [DOI] [PubMed] [Google Scholar]
- 41.Fonseca MCR, Lalone E, Claro da Silva N, et al. Construct validity of the Patient-Rated Wrist and Hand Evaluation questionnaire (PRWHE) for nerve repair in the hand. Musculoskelet Sci Pract. 2019;40:40–44. doi: 10.1016/j.msksp.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 42.Jerosch-Herold C. Measuring outcome in median nerve injuries. J Hand Surg. 1993;18B:624–628. doi: 10.1016/0266-7681(93)90019-c. [DOI] [PubMed] [Google Scholar]
- 43.Jerosch-Herold C. Should sensory function after median nerve injury and repair be quantified using two-point discrimination as the critical measure? Scand J Plast Reconstr Surg Hand Surg. 2000;34:339–343. doi: 10.1080/028443100750059129. [DOI] [PubMed] [Google Scholar]
- 44.Onne L. Recovery of sensibility and sudomotor activity in the hand after nerve suture. Acta Chir Scand Suppl. 1962;(Suppl 300):1–69. [PubMed] [Google Scholar]
- 45.Rosén B. Recovery of sensory and motor function after nerve repair. A rationale for evaluation. J Hand Ther. 1996;9:315–327. doi: 10.1016/s0894-1130(96)80037-8. [DOI] [PubMed] [Google Scholar]
- 46.Şahin F, Atalay NŞ, Akkaya N, Ercidoğan Ö, Başakçı B, Kuran B. The correlation of neurophysiological findings with clinical and functional status in patients following traumatic nerve injury. J Hand Surg Eur Vol. 2013;39E:199–206. doi: 10.1177/1753193413479507. [DOI] [PubMed] [Google Scholar]
- 47.Selma P, Emre O, Oguz P, Ersin N, Oya B. Evaluation of the improvement of sensibility after primary median nerve repair at the wrist. Microsurgery. 1998;18:192–196. doi: 10.1002/(sici)1098-2752(1998)18:3<192::aid-micr13>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 48.Vordemvenne T, Langer M, Ochman S, Raschke M, Schult M. Long-term results after primary microsurgical repair of ulnar and median nerve injuries. A comparison of common score systems. Clin Neurol Neurosurg. 2007;109:263–271. doi: 10.1016/j.clineuro.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 49.Wong K, Coert J, Robinson P, Meek M. Comparison of assessment tools to score recovery of function after repair of traumatic lesions of the median nerve. Scand J Plast Reconstr Surg Hand Surg. 2006;40:219–224. doi: 10.1080/02844310600652878. [DOI] [PubMed] [Google Scholar]
- 50.OCEBM Levels of Evidence Working Group . March 2009. Levels of evidence.https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009 Available at. Accessed November 15, 2020. [Google Scholar]
- 51.Marsh D, Barton N. Does the use of the operating microscope improve the results of peripheral nerve suture? J Bone Joint Surg Br. 1987;69-B:625–630. doi: 10.1302/0301-620X.69B4.3301860. [DOI] [PubMed] [Google Scholar]
- 52.Allan CH. Primary nerve repair: indications and results. J Am Soc Surg Hand. 2004;4:195–199. [Google Scholar]
- 53.Waylett-Rendall J. Sensibility evaluation and rehabilitation. Orthop Clin North Am. 1988;19:43–56. [PubMed] [Google Scholar]
- 54.Mackinnon SE, Dellon AL. Thieme; New York: 1988. Surgery of the peripheral nerve. [Google Scholar]
- 55.Portney LG. F.A. Davis; Philadelphia: 2020. Foundations of clinical research: applications to evidence-based practice. 4th ed. ed. [Google Scholar]
- 56.Ng CL, Ho DD, Chow SP. The Moberg pickup test: results of testing with a standard protocol. J Hand Ther. 1999;12:309–312. doi: 10.1016/s0894-1130(99)80069-6. [DOI] [PubMed] [Google Scholar]
- 57.Amirjani N, Ashworth NL, Olson JL, Morhart M, Ming Chan K. Discriminative validity and test-retest reliability of the Dellon-modified Moberg pick-up test in carpal tunnel syndrome patients. J Peripher Nerv Syst. 2011;16:51–58. doi: 10.1111/j.1529-8027.2011.00312.x. [DOI] [PubMed] [Google Scholar]
- 58.Mehta SP, MacDermid JC, Richardson J, MacIntyre NJ, Grewal R. A systematic review of the measurement properties of the patient-rated wrist evaluation. J Orthop Sports Phys Ther. 2015;45:289–298. doi: 10.2519/jospt.2015.5236. [DOI] [PubMed] [Google Scholar]
- 59.Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14:128–146. [PubMed] [Google Scholar]
- 60.Moore KL, Dalley AF, Agur AMR. 7th ed. Wolters Kluwer/Lippincott Williams & Wilkins Health; Philadelphia: 2014. Clinically oriented anatomy. [Google Scholar]
- 61.Lee Y, Bang H, Kim DJ. How to establish clinical prediction models. Endocrinology and metabolism (Seoul) 2016;31:38–44. doi: 10.3803/EnM.2016.31.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hoard AS. ProQuest Dissertations Publishing; Denton: 2012. Reliability of the Semmes-Weinstein monofilaments in identifying peripheral neuropathy in the hand: a systematic review. [Google Scholar]
- 63.Rosén B, Dahlin LB, Lundborg G. Assessment of functional outcome after nerve repair in a longitudinal cohort. Scand J Plast Reconstr Surg Hand Surg. 2000;34:71–78. doi: 10.1080/02844310050160204. [DOI] [PubMed] [Google Scholar]
- 64.Jerosch-Herold C. A study of the relative responsiveness of five sensibility tests for assessment of recovery after median nerve injury and repair. J Hand Surg Br. 2003;28:255–260. doi: 10.1016/s0266-7681(03)00017-2. [DOI] [PubMed] [Google Scholar]
- 65.Strauch B, Lang A. The Ten test revisited. Plast Reconstr Surg. 2003;112:593–594. doi: 10.1097/01.PRS.0000070680.25190.E6. [DOI] [PubMed] [Google Scholar]
- 66.Weinstein S. Fifty years of somatosensory research: from the Semmes-Weinstein monofilaments to the Weinstein enhanced sensory test. J Hand Ther. 1993;6:11–22. [PubMed] [Google Scholar]
- 67.Berger MJ, Regan WR, Seal A, Bristol SG. Reliability of the “Ten test” for assessment of discriminative sensation in hand trauma. J Plast Reconstr Aesthet Surg. 2016;69:1411–1416. doi: 10.1016/j.bjps.2016.06.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.