Abstract
The objective of this initiative was to conduct a comprehensive opioid overdose vulnerability assessment in Indiana and evaluate spatial accessibility to opioid use disorder treatment, harm reduction services, and opioid response programs. We compiled 2017 county-level (n = 92) data on opioid-related and socioeconomic indicators from publicly available state and federal sources. First, we assessed the spatial distribution of opioid-related indicators in a geographic information system (GIS). Next, we used a novel regression-weighted ranking approach with mean standardized covariates and an opioid-involved overdose mortality outcome to calculate county-level vulnerability scores. Finally, we examined accessibility to opioid use disorder treatment services and opioid response programs at the census tract-level (n = 1511) using two-step floating catchment area analysis. Opioid-related emergency department visit rate, opioid-related arrest rate, chronic hepatitis C virus infection rate, opioid prescription rate, unemployment rate, and percent of female-led households were independently and positively associated with opioid-involved overdose mortality (p < 0.05). We identified high-risk counties across the rural–urban continuum and primarily in east central Indiana. We found that only one of the 19 most vulnerable counties was in the top quintile for treatment services and had naloxone provider accessibility in all of its census tracts. Findings from our vulnerability assessment provide local-level context and evidence to support and inform future public health policies and targeted interventions in Indiana in areas with high opioid overdose vulnerability and low service accessibility. Our approach can be replicated in other state and local public health jurisdictions to assess opioid-involved public health vulnerabilities.
Keywords: Opioid vulnerability assessment, Opioid-involved overdose, Geographical information system, Indiana, Two-step floating catchment area analysis
1. Background
With 1246 opioid overdose deaths in 2019 (18.5 deaths per 100,000 population), Indiana’s opioid-involved overdose mortality level continues to increase. (Indiana Department of Health, 2021) In Marion County, Indiana, the rise in overdoses involving fentanyl is linked to the rapid increase of opioid-involved overdose rates among younger, male, and Black populations. (Phalen et al., 2018) This led to opioid-involved overdose mortality rates among Blacks surpassing those of Whites during 2018. (Furr-Holden et al., 2021) Scott County, Indiana, was at the epicenter of an HIV outbreak in 2014–2015 linked to injection of prescription opioids. (Conrad et al., 2015) Following this outbreak, Van Handel et al.’s national HCV and HIV vulnerability assessment identified 10 counties in Indiana among the most at-risk to outbreaks linked to injection drug use. (Van Handel et al., 2016) Inspired by this national assessment, a 2016 state-level Indiana Department of Health-led HCV vulnerability assessment identified 15 additional at-risk counties. (Box et al., 2017) In light of the escalation of the opioid crisis during the coronavirus pandemic, (Grinspoon, 2020, Slavova et al., 2020, Sutfim, 2020) including within Marion County, Indiana (Indianapolis), (Glober et al., 2020) it is essential to understand where opioid-involved overdose vulnerabilities are greatest, both to leverage resources effectively and to inform the development of targeted local responses and statewide policies. Identification of vulnerable areas can be used to enhance access to medication for opioid use disorder (MOUD), expand and sustain harm reduction programming, and bolster overdose education and naloxone distribution programs.
The goal of this opioid overdose vulnerability assessment was to highlight the local communities in Indiana at greatest risk of fatal opioid overdose and other adverse opioid-related outcomes. To the best of our knowledge, there has not been a prior published statewide community-level assessment of opioid-involved overdose vulnerability in Indiana. Our team, comprised of academic researchers, Indiana public health experts, and staff from the Centers for Disease Control and Prevention (CDC) and the Council of State and Territorial Epidemiologists (CSTE), worked collaboratively to conduct an opioid-involved overdose vulnerability assessment utilizing publicly available data. We employed a multifaceted approach using statistical modeling, geographic information systems (GIS), and novel spatial accessibility measures to identify areas that are at-risk of opioid-related harm and highlight areas that need additional resources to address the opioid overdose crisis.
2. Methods
Our methodological approach was adapted from the 2016 Van Handel et al. nationwide vulnerability assessment for injection-related HIV and HCV infections as well as from other opioid and HCV vulnerability assessment frameworks. (Van Handel et al., 2016, Missouri Department of Health and Senior Services, 2020, Sharareh et al., 2020, Rickles et al., 2018) For our assessment, we identified indicators associated with the primary outcome of interest, opioid-involved overdose mortality, at the county-level (n = 92) in Indiana. We also carried out accessibility analyses to quantify census tract-level availability of drug treatment and overdose prevention and response resources across the state. Our assessment was reviewed by the Tufts University Health Sciences Institutional Review Board and was determined to be non-human subjects research.
2.1. Data sources
Together with the Indiana Department of Health, we compiled county-level surveillance data, relevant to the opioid crisis, from state and federal data systems for the year 2017. Opioid-related event data included opioid-involved overdose deaths, opioid-related emergency department visits, and chronic HCV cases from the online Indiana Department of Health public health statistics data portal. (Indiana Department of Health, 2021) We retrieved opioid-related arrest data from the Indiana Laboratory Information Management System (IN.gov Management Performance Hub, 2018) and obtained opioid prescription rate data from online CDC county-level retail opioid prescription maps displaying data from the IQVIA Xponent database. (Centers for Disease Control and Prevention, 2017) To assess county-level opioid use disorder (OUD) treatment and harm reduction access, we collected address-level 2020 Indiana services data from the Indiana Department of Health and from the Substance Abuse and Mental Health Services Administration (SAMHSA) treatment locator. (Substance Abuse and Mental Health Services Administration, 2021) To measure accessibility to opioid response programs (ORP), we leveraged an existing shapefile on 2018 naloxone providers from the Indiana Department of Health. (Indiana Department of Health, 2018) We compiled community-level demographic and social determinants of health indicators, at the county-level, from the Census Bureau’s American Community Survey (ACS). (Census, 2018) For all compiled ACS indicators, we used county-level 5-year estimates for the years 2013 to 2017. To leverage a rural–urban classification system designed specifically for Indiana, we applied the Purdue University Indiana County Classification System. (Ayres et al., 2013)
2.2. Indicators
Core Indicators. Based on previous vulnerability assessments and subject matter expertise, (Van Handel et al., 2016, Rickles et al., 2018) we included core indicators found to be strongly associated with opioid-involved overdose mortality rates: opioid-related emergency department visits (non-fatal emergency department visits involving any opioid overdose per 100,000 population), opioid-related arrests (arrests with laboratory-confirmed opioids per 100,000 population), chronic HCV cases (confirmed and probable cases of chronic HCV per 100,000 population), opioid prescriptions (number of retail opioid prescriptions per 100,000 population), and median income (based on the income distribution of all households in the county, including those with no income). Opioid-involved overdose mortality (deaths from drug poisoning involving any opioid) was used as the core outcome indicator.
Covariates. To assess and control for county-level demographic and socioeconomic measures, we assessed: percentage of the population that was non-Hispanic White, non-Hispanic Black or African American, and Hispanic or Latino; percentage of households that are female-led, married-couple, rented, and crowded (households with occupancy of more than one person per room), with vehicle access, and with Internet subscriptions; percent of residents with a disability, with health insurance, and below the 100% Federal Poverty Level; unemployment rate; educational attainment rate; teen birth rate; and the Gini index. We created a services coverage proxy covariate, calculated as the number of OUD services per 100,000 population. OUD services included syringe services programs (SSPs), sometimes known as needle exchange programs, and service locations offering MOUD, as well as OUD therapy and counselling services. Due to shifting trends in rural versus urban drug overdose rates and other vulnerability assessments related to the opioid crisis identifying urbanicity and rurality as risk factors, we included a rural–urban covariate. (Mack et al., 2017, Batdorf, 2020, Short et al., 2020) This classification system splits counties into rural, rural/mixed, and urban categories by population density, size of largest city or town, and a subjective indicator (county identity). (Ayres et al., 2013)
2.3. Analyses
GIS Mapping and Spatial Analyses. After compiling all county-level outcome and covariate data, we joined the tabular data to an Indiana county boundary shapefile in a GIS and developed thematic maps to assess the initial spatial distributions of all core indicators and covariates. We geocoded and mapped all address-level OUD and ORP services data and used service locations and county-level population data for subsequent geostatistical analyses to assess access to services, described in detail below. We used ArcGIS 10.7.1 (ESRI, Redlands, CA) for all GIS mapping and spatial analyses.
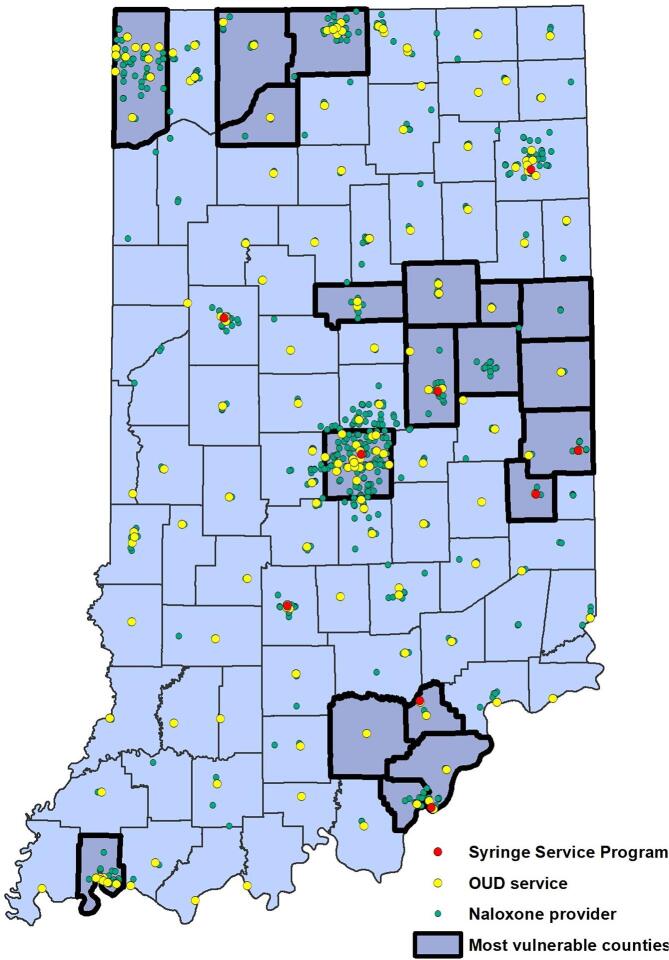
Services Accessibility Analysis. To assess the spatial distribution and accessibility of OUD services in Indiana in relation to opioid-involved overdose vulnerability, we first assessed the spatial distribution of OUD services including MOUD treatment services, SSPs, OUD therapy and counselling, and ORP naloxone providers in relation to identified vulnerable counties (Appendix 1). Then, we used a two-step floating catchment area (2SFCA) method to calculate accessibility to OUD service providers and ORPs. (Luo and Wang, 2003, Wang and Luo, 2005) The 2SFCA method is an extension of the provider-to-population ratio in which supply, the number of providers, is assessed over demand at the population level. In the first step, we calculated the provider-to-population ratio for all providers where the denominator was population centers within a specific drive-time threshold distance from the provider location. In the second step, we summed the provider-to-population ratios of all the providers within the threshold distance limit from a population weighted centroid. The model can be expressed mathematically as:
where, Sj is the number of providers at location j; d is the drive-time between the provider and the population weighted centroid; Pk is the population of location k, where the population weighted centroid of the census tract falls within the threshold distance; D is the threshold distance for the search radius; and Ai is the accessibility score at location i.
Appendix 1.
Location of opioid use disorder services, including medication for opioid use disorder treatment services, naloxone providers, as well as syringe services programs sometimes known as needle exchange programs.
For this assessment, we calculated the accessibility to OUD treatment providers and ORPs using the 2SFCA method. We used a geocoded list of OUD treatment services including MOUD, OUD therapy, and OUD counselling services in Indiana compiled from the Indiana Department of Health and SAMHSA as the providers and census tracts as the unit of analysis. To measure accessibility to ORPs, we leveraged an existing list of geocoded naloxone providers available from the Indiana Department of Health. To calculate the accessibility index, we utilized the University of South Wales Floating Catchment Area 2 (USW-FCA2), a freely available ArcGIS add-in tool developed by Langford et al. (Langford et al., 2015)
Statistical Analyses. We examined measures of central tendency as well as maximum and minimum values for all indicators. For this vulnerability assessment, we calculated opioid-involved overdose vulnerability scores based on a regression-weighted quintile ranking approach. We constructed bivariate negative binomial regression models with counts of opioid-involved overdose deaths as the outcome, standardized core-indicators and covariates as predictors, and the log of county population as an offset. (Sharareh et al., 2020) Prior to regression modelling, we standardized all indicators and covariates to a mean of zero and a standard deviation of one. We assessed associations between opioid overdose deaths and 18 covariates for inclusion in the final weighted vulnerability scoring. All five core indicators were selected a priori. We selected covariates that were significant at a p < 0.2 level in the bivariate models for consideration for use in the final vulnerability assessment scores, a commonly utilized criterion for selecting covariates. (Maldonado and Greenland, 1993) For model diagnostics (not for the estimation of vulnerability scores), we created a linear multivariable regression model. We assessed multicollinearity among the 11 selected covariates and the five core indicators by calculating tolerance and variance inflation factors (VIFs). Indicators with a tolerance < 0.2 and a VIF > 10 were removed. Among collinear covariates, we elected to keep those with higher tolerance values. Due to significant collinearity, we dropped three covariates (married-couple household percent, renter household percent, and percent of population in poverty).
After finalizing the selection of indicators, we calculated quintile ranks for each of the core indicators and remaining covariates. We weighted these quintile ranks by the variable’s standardized bivariate regression coefficient and calculated the vulnerability score by summing the weighted quintile ranks via the following function:
where, β is the standardized regression coefficient from the bivariate negative binominal regression models and X is the indicator or covariate’s quintile rank, ranging from 1 to 5. Counties with higher vulnerability scores were more vulnerable to opioid-involved overdose mortality. We also conducted a sensitivity analysis using a multivariable negative binomial regression model to check the robustness of our models. We conducted the statistical analyses using SAS 9.4 (Cary, North Carolina) and Stata 16 (College Station, Texas).
3. Results
Using descriptive GIS mapping, we identified high rates of opioid-involved overdose mortality, opioid-related emergency department visits, and opioid-related arrests in east central Indiana. In comparison, southwest Indiana had relatively low levels for all three variables, with the exception of Vanderburgh County. The urban centers of Indianapolis in Marion County and Lake County (including Gary and East Chicago) accounted for 30% of all opioid overdose deaths in 2017.
We identified eight covariates based on the significance level of p < 0.2 for inclusion in our vulnerability score calculations. These covariates were percentage of female-led households (β = 0.31), unemployment rate (β = 0.29), Gini index (β = 0.16), percentage of the population above 25 years of age without a high-school diploma (β = 0.15), percentage of the population with a disability (β = 0.12), percentage of the population that was non-Hispanic Black (β = 0.12), OUD services per capita (β = −0.16), and percentage of the population with Internet access (β = −0.16). Both OUD services per capita and percentage of the population with Internet access were found to be protective covariates. Additionally, all core indicators identified a priori met the significance level threshold of p < 0.2: opioid-related emergency department visit rate (β = 0.49), opioid-related arrest rate (β = 0.34), opioid prescription rate (β = 0.32), chronic HCV rate (β = 0.32), and median income (β = −0.14) (Table 1).
Table 1.
Factors associated with opioid-involved overdose vulnerability rankings in Indiana counties (n = 92).
| Variable | Variable Type | Source | Mean | Std. Dev. | Min | Max | β | p-value |
|---|---|---|---|---|---|---|---|---|
| Opioid-involved overdose deaths per 100,000 population | Core Outcome | IDOH Stats Explorer https://gis.in.gov/apps/isdh/Meta/Stats_Layers.htm, 2017 | 8.80 | 16.31 | 0 | 77.10 | ||
| Opioid-related emergency department visits per 100,000 population | Core Indicator | IDOH Stats Explorer https://gis.in.gov/apps/isdh/Meta/Stats_Layers.htm, 2017 |
100.80 | 82.58 | 0 | 391.50 | 0.49 | <0.0001 |
| Opioid-related arrests per 100,000 population | Core Indicator | Indiana Laboratory Information Management System https://hub.mph.in.gov/dataset/drug-submissions-to-indiana-state-police-laboratories, 2017 | 53.54 | 56.24 | 0 | 262.79 | 0.34 | <0.0001 |
| Opioid prescriptions per 100,000 population | Core Indicator | CDC Opioid Prescribing Rate Maps https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html, 2017 |
72962.6 | 24037.7 | 3600.0 | 124400.0 | 0.32 | 0.0008 |
| Chronic hepatitis C cases per 100,000 population | Core Indicator | IDOH Stats Explorer https://gis.in.gov/apps/isdh/Meta/Stats_Layers.htm, 2017 |
147.0 | 130.1 | 0 | 1060.0 | 0.32 | 0.0031 |
| Percentage of female-led households | Covariate | ACS, 2017 5-year estimates, 2013–2017 | 10.3 | 2.0 | 6.1 | 16.7 | 0.31 | 0.0001 |
| Unemployment rate | Covariate | ACS, 2017 5-year estimates, 2013–2017 | 5.45 | 1.34 | 2.90 | 8.50 | 0.29 | 0.0008 |
| Gini Index (a measure of inequality) | Covariate | ACS, 2017 5-year estimates, 2013–2017 | 0.42 | 0.03 | 0.34 | 0.51 | 0.16 | 0.0608 |
| Percentage of the population above 25 years of age without a high school diploma | Covariate | ACS, 2017 5-year estimates, 2013–2017 | 12.4 | 4.2 | 3.8 | 36.7 | 0.15 | 0.1476 |
| Percentage of the population with disability | Covariate | ACS, 2017 5-year estimates, 2013–2017 | 15.2 | 2.6 | 7.7 | 20.8 | 0.12 | 0.1542 |
| Percentage of the population that is non-Hispanic Black | Covariate | ACS, 2017 5-year estimates, 2013–2017 | 2.7 | 4.4 | 0.07 | 27.4 | 0.12 | 0.1266 |
| Median income (United States Dollar) | Core Indicator | ACS, 2017 5-year estimates, 2013–2017 | 27043.5 | 3517.9 | 20728.0 | 43758.0 | −0.14 | 0.0612 |
| Opioid use disorder services per 100,000 population | Covariate | IDOH Public Health Geographics https://gis.in.gov/apps/isdh/meta/resources_layers.htm, 2020 SAMHSA treatment locator https://findtreatment.samhsa.gov/locator, 2020 |
5.2 | 3.3 | 0 | 16.9 | −0.16 | 0.0568 |
| Percentage of the population with Internet access | Covariate | ACS, 2017 5-year estimates, 2013–2017 | 72.3 | 6.3 | 54.8 | 92.5 | −0.16 | 0.0532 |
The Abbreviations: β: Beta coefficients from bivariate negative binomial regression model with opioid-involved overdose deaths as the outcome, standardized indicators and covariates as predictors, and log of the population as an offset. IDOH: Indiana Department of Health. CDC: Centers for Disease Control and Prevention. SAMHSA: Substance Abuse and Mental Health Services Administration.
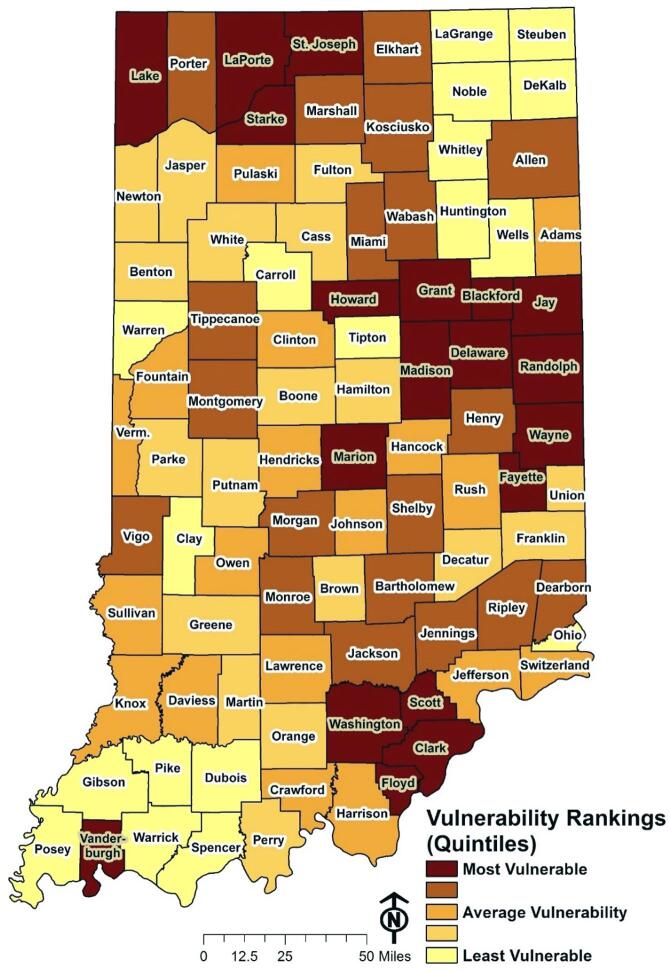
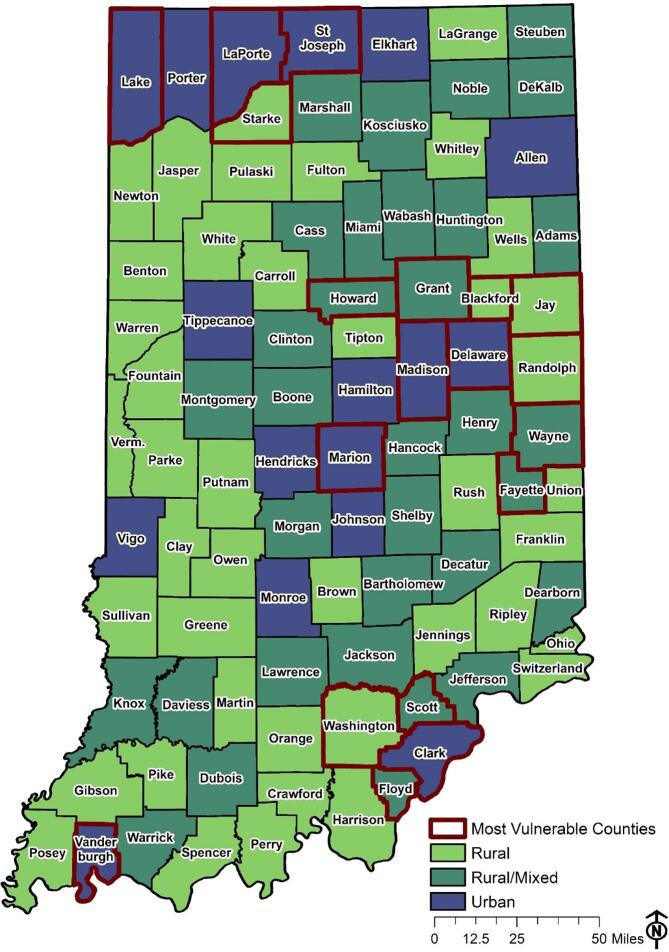
Through our county-level opioid-involved overdose vulnerability rankings, we identified 19 counties to be the most vulnerable, of which 10 are located in east central Indiana, four are located in northwest Indiana, four are located in southern Indiana, and one is located in southwest Indiana. Scott County, the previous epicenter of the 2014–2015 HIV outbreak, is included among the most vulnerable counties. Counties with the highest population densities were commonly among the most vulnerable, including: Marion, Lake, and Vanderburgh. Southwest and northeast Indiana counties had relatively low vulnerability levels, with the exception of the highly populated counties of Vanderburgh and Allen (Fig. 1, Table 2). Among the highest quintile of identified vulnerability, opioid-involved mortality rates ranged from 7.8 per 100,000 in Delaware County to 76.2 per 100,000 in Wayne County with an average of 32.7, while counts ranged from 2 in Blackford County to 232 in Marion County with an average of 38.2. In the lowest quintile of vulnerability, rates ranged from 0 to 16.9 in Ohio County with an average of 4.1, while counts ranged from 0 to 5 in Warrick County with an average of 1.1 (Table 2). Following the Purdue University rural–urban classification scheme, we found eight urban, six rural/mixed, and five rural counties within the most vulnerable category (Appendix 2). Urban counties contained 57% (172 out of 303) of identified OUD services. Rural counties contained 14%, while rural/mixed counties contained 29%.
Fig. 1.
Opioid-involved overdose vulnerability rankings split into quintiles, with the top quintile being the top 19 most vulnerable counties in the state of Indiana as identified in this vulnerability assessment.
Table 2.
Overall opioid-involved overdose vulnerability quintiles for all Indiana counties Overall opioid-involved overdose vulnerability is displayed by quintile for all 92 Indiana counties. The first quintile represents the most vulnerable counties, while the fifth quintile represents the least vulnerable counties. Counties in each quintile are listed alphabetically. The range and average opioid-involved overdose mortality rates per 100,000 and opioid-involved overdose mortality counts are included for each quintile.
| Quintile 1 Rate: 7.76–76.15 (32.68) Count: 2–232 (38.16) | Quintile 2 Rate: 4.64–34.54 (17.09) Count: 2–43 (13.89) | Quintile 3 Rate 0–31.96 (11.59) Count: 0–24 (4.67) | Quintile 4 Rate: 0–27.68 (11.92) Count: 0–37 (4.61) | Quintile 5 Rate: 0–16.92 (4.12) Count: 0–5 (1.11) |
|---|---|---|---|---|
| Blackford | Allen | Adams | Benton | Carroll |
| Clark | Bartholomew | Clinton | Boone | Clay |
| Delaware | Dearborn | Crawford | Brown | DeKalb |
| Fayette | Elkhart | Daviess | Cass | Dubois |
| Floyd | Henry | Fountain | Decatur | Gibson |
| Grant | Jackson | Hancock | Franklin | Huntington |
| Howard | Jennings | Harrison | Fulton | LaGrange |
| Jay | Kosciusko | Hendricks | Greene | Noble |
| Lake | Marshall | Jefferson | Hamilton | Ohio |
| LaPorte | Miami | Johnson | Jasper | Pike |
| Madison | Monroe | Knox | Martin | Posey |
| Marion | Montgomery | Lawrence | Newton | Spencer |
| Randolph | Morgan | Owen | Orange | Steuben |
| Scott | Porter | Pulaski | Parke | Tipton |
| St. Joseph | Ripley | Rush | Perry | Warren |
| Starke | Shelby | Sullivan | Putnam | Warrick |
| Vanderburgh | Tippecanoe | Switzerland | Union | Wells |
| Washington | Vigo | Vermillion | White | Whitley |
| Wayne | Wabash |
Appendix 2.
Rural-urban status of the most vulnerable Indiana counties for opioid-involved overdose mortality using the Purdue University Indiana County Classification System.
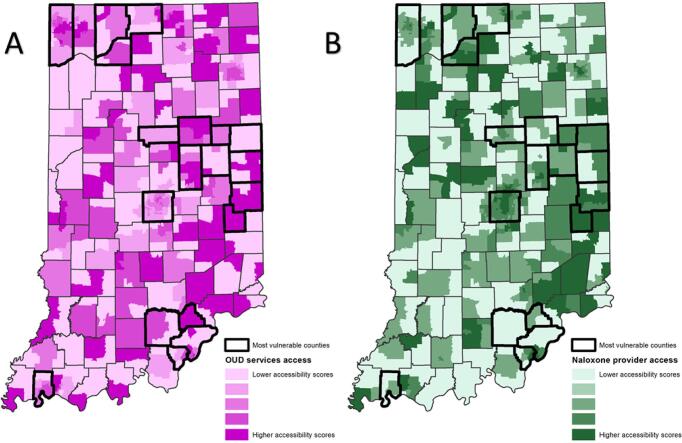
From analysis of the spatial accessibility indices, derived from the 2SFCA method, we found that only two of the 19 most vulnerable counties ranked high on the OUD treatment services accessibility index, with all census tracts within the top quintile for highest provider to population ratios in a 30-minute drive-time catchment area (Fig. 2.A). Similarly, only one of the 19 most vulnerable counties ranks high on accessibility to naloxone providers with all census tracts within the top quintile (Fig. 2.B). Fifteen of the 19 most vulnerable counties ranked had at least one census tract that ranked in the lowest quintile of OUD treatment services accessibility index, and 14 of the 19 most vulnerable counties had at least one census tract that ranked in the lowest quintile of naloxone provider accessibility.
Fig. 2.
Spatial accessibility index of opioid use disorder treatment services as well as for naloxone providers. A) Spatial accessibility index output for OUD treatment services from the two-step floating catchment method with highlighted top and bottom quintile census tracts respectively showing highest and lowest accessibility. B) Spatial accessibility index output for naloxone providers from the two-step floating catchment method with highlighted top and bottom quintile census tracts respectively showing highest and lowest accessibility.
4. Discussion
To better understand opioid-involved overdose vulnerabilities in Indiana, we used publicly available data in a novel regression-weighted quintile rank statistical approach to assess vulnerability and two 2SFCAs to assess OUD treatment services and naloxone provider accessibility. Our vulnerability assessment identified counties at-risk for elevated opioid-involved overdose mortality in Indiana. Among these vulnerable counties, 2SFCA analyses highlighted OUD treatment service and naloxone provider access disparities at the census tract-level and communities that could benefit from targeted interventions. In addition to the preselected five core indicators, we identified and selected eight additional covariates, which were independently and significantly associated (p < 0.2) with county-level opioid-involved overdose mortality in Indiana.
When compared to the 2016 national CDC and the 2016 state-level Indiana Department of Health-led HIV and HCV outbreak vulnerability assessments that identified at-risk Indiana counties, (Van Handel et al., 2016, Box et al., 2017) we found four counties—Fayette, Scott, Starke, and Washington—to have overlapping vulnerability among all three assessments. Focusing public health prevention efforts on counties vulnerable to opioid-involved overdose mortality as well as HCV and HIV outbreaks may be particularly impactful and cost effective. (Perlman and Jordan, 2018, Bulled and Singer, 2011)
From our services accessibility analysis, only Fayette County was found to have all census tracts in the top quintile for OUD treatment services and naloxone provider accessibility. Twelve of the 19 identified vulnerable counties had census tracts within the lowest quintile for both OUD treatment services and naloxone provider accessibility, highlighting in-county service access gaps and disparities (Fig. 2). Interestingly, we identified counties with high-ranking access to OUD treatment services but low-ranking access to naloxone providers such as Grant, Randolph, and Scott counties, as well as counties with high ranking access to naloxone providers but low ranking access to OUD treatment services such as Delaware, Jay, and Marion counties. As we identified OUD services per capita as a county-level protective factor in our analysis, targeting future OUD service expansion efforts in vulnerable communities with accessibility gaps may help maximize limited resources.
We envision three critical pathways for OUD service expansion efforts: enhanced access to MOUD including buprenorphine and methadone maintenance treatment, which are both effective at reducing the risk of opioid-involved overdose mortality; (Larochelle et al., 2018, Sordo et al., 2017, Morgan et al., 2019, Fullerton et al., 2014) expanded and sustained harm reduction programming, including SSPs; (Larochelle et al., 2019, Kapadia et al., 2021, Hawk et al., 2015) and bolstered overdose education and naloxone distribution programs. (Larochelle et al., 2019, Dwyer et al., 2015, Walley et al., 2013) In addition, it is critical that these OUD service expansion efforts be accompanied by policies and programs aimed at reducing existing community barriers to OUD services such as the scarcity of clinicians with sufficient training, regulatory and financial obstacles, as well as barriers from stigma against OUD treatment and harm reduction services, especially in rural counties in Indiana. (Madras et al., 2020, Indiana University, 2020)
Previous studies have reported significant differences between rural and urban areas such as higher rates of heroin and synthetic opioids, other than methadone (e.g., fentanyl), involved with overdose deaths in urban areas, and higher rates of natural and semisynthetic (e.g., oxycodone) opioid-involved with overdose deaths in rural areas. (Hedegaard and Spencer, 2021) Prior vulnerability assessments related to the opioid crisis have also found rural–urban classification to be significantly associated with opioid-involved mortality. (Van Handel et al., 2016, Batdorf, 2020, Short et al., 2020) However, in our analysis, rural–urban classification was not significantly associated (p > 0.2) with opioid-involved overdose mortality and was not selected as a covariate; we identified vulnerable Indiana counties across the rural–urban spectrum (Appendix 2). Customization of local interventions will be crucial to maximize effectiveness due to the complex differences between rural, rural/mixed, and urban areas. For example, compared to urban areas, rural or rural/mixed communities may face additional challenges such as limited transportation options or burdensome travel times. (National Rural Health Association, 2017)
Among the 13 total core indicators and covariates included in the vulnerability assessment, we identified eight demographic or social determinants of health indicators that were significantly associated (p < 0.2) with opioid-involved overdose mortality in Indiana, including: median income, unemployment rate, Gini index, percent of female-led households, percent without a high school diploma, percent with a disability, percent with Internet access, and percent non-Hispanic Black. Our finding of these risk factors for opioid overdose deaths in Indiana supports previous research indicating strong associations between high socioeconomic marginalization and higher rates of overdose. (van Draanen et al., 2020, Altekruse et al., 2020, El-Bassel et al., 2021) Despite declining opioid prescription rates, researchers posit that the continued rise of opioid-involved overdose mortality rates indicates that opioid prescribing is only a single component of a complex web of critical factors and social determinants of health that are driving the opioid crisis. (Dasgupta et al., 2018) Many of these key socioeconomic variables were also commonly found as significant covariates among multiple other vulnerability assessments related to the opioid crisis. (Missouri Department of Health and Senior Services, 2020, Rickles et al., 2018, South Dakota Department of Health, 2019, Iowa Department of Public Health, 2019, Brown School of Public Health, 2019) These risk factors were of additional relevance at the time of this vulnerability assessment as the coronavirus pandemic began to disparately affect socioeconomically marginalized populations (Grinspoon, 2020, Opioid Response Network, 2020) and as substantial increases in opioid-involved overdose deaths were noted. (CDC Health Alert Network, 2020, Grinspoon, 2020, Slavova et al., 2020, Sutfim, 2020, Glober et al., 2020)
Of particular importance is the racial dimension of the ongoing opioid crisis. Black and Hispanic persons who use drugs have also been discriminatorily criminalized in parallel with the 1980s War on Drugs where Black and Hispanic persons were incarcerated at higher rates when compared to other racial/ethnic groups. (Mauer, 2009, Bechteler et al., 2017, Mitchell and Caudy, 2017, Substance Abuse and Mental Health Services Administration, 2020) While the racial/ethnic disparities in opioid prescribing practices, with lower prescription rates in Black communities, (Singhal et al., 2016) may have resulted in lower rates of overdose deaths involving prescription opioids during the first wave of the opioid crisis from the mid-1990s to 2010, (Paulozzi et al., 2011) the shift to synthetic opioids such as fentanyl during the third wave of the crisis has led to a drastic increase in opioid-involved overdoses among Black and Hispanic populations. (Friedman et al., 2021, Ciccarone, 2019, Alexander et al., 2018) Black opioid-involved overdose mortality rates have rapidly increased in multiple states. (Agency for Healthcare Research and Quality, 2020, James and Jordan, 2018, Hernandez et al., 2020, Minnesota Department of Health, 2018) This includes Indiana, where drug overdose mortality rates for Black populations surpassed those for non-Hispanic White populations in 2017. (Helmick, 2019, Watson et al., 2018)
Racial inequities also manifest in differing levels of access to and use of harm reduction and treatment services for OUD. As buprenorphine access has been deregulated and made more widely available through private physicians, (Hansen and Roberts, 2012) barriers to methadone access remain high as federal regulations persist. (McBournie et al., 2019) These differing levels of regulation generate inequity through the racial/ethnic geographic segregation of treatment capacity for these two treatments found in a national county-level analysis. (Goedel et al., 2020) Counties that are highly segregated non-Hispanic White have more buprenorphine services per capita, while counties that are highly segregated Black and Hispanic have more methadone services per capita. (Goedel et al., 2020) An assessment of New York City found that buprenorphine treatment usage was highest in areas with low percentages of Black, Hispanic, and low income residents, while methadone treatment usage was highest in areas with high percentages of low income and Hispanic residents. (Hansen et al., 2016, Hansen et al., 2013) A nationally representative study found that from 2012 to 2015, Hispanic and non-Hispanic White patients accounted for 94.9% of office-based buprenorphine prescription visits. (Lagisetty et al., 2019) While assessing the spatial distribution of OUD services locations in Indiana for the creation of the spatial accessibility index, of the 14 identified that offer methadone, 12 were in or next to census tracts in the top quintile for percentage of the population that is non-Hispanic Black. Additionally, Indianapolis EMS records from 2011 to 2018 show that the rate of emergency naloxone administrations was higher among non-Hispanic White decedents when compared to non-Hispanic Black decedents. (Ray et al., 2020) As long as Black and Hispanic populations continue to have substantially lower access to prevention, harm reduction, treatment, response, and recovery services for OUD, (Office of Behavioral Health Equity, 2020) future solutions targeting the opioid crisis will require detailed, thoughtful, holistic, and culturally competent measures that intentionally promote the well-being and healing of Black, Hispanic, and other racial and ethnic communities. (Substance Abuse and Mental Health Services Administration, 2020)
The presence of these demographic and social determinants of health, including racial inequity, merits a broader drug user health approach for future public health policies and targeted interventions in Indiana. Taking a drug user health approach allocates importance to both opioid-involved overdose prevention through access to harm reduction and OUD treatment services and addressing the accumulated challenges related to health and quality of life that are associated with opioid use and related comorbidities. A focus on the underlying drivers of addiction is needed to help address the underlying social and structural disparities in insurance coverage, stable housing, criminalization and incarceration rates, as well as stigma against substance use disorders. (El-Bassel et al., 2021, Volkow, 2021) While a drug user approach may be more difficult to support, implement, and sustain, it may be critical to address the intertwined OUD, opioid-involved overdose, and HCV crises. (Kattakuzhy and Rosenthal, 2020)
One component of such an approach in Indiana could be the increase of community-level harm reduction programs such as SSPs. In 2014–2015, there was a community outbreak of HIV and HCV linked to injection drug use in Scott County, Indiana. (Conrad et al., 2015) One of the critical responses to the public health emergency was the temporary authorization of an SSP in Scott County, which proved effective at drastically reducing the number of new HIV and HCV infections in the rural community. (Kishore et al., 2019) In particular, modelling of the outbreak has elucidated that an earlier response may have resulted in prevention, if not mitigation, highlighting the importance of proactive instead of reactive policies. (Gonsalves and Crawford, 2018, Goedel et al., 2020) SSPs have proven effective at reducing the HIV and HCV transmission risks, especially when in combination with MOUD, (Aspinall et al., 2014, Platt et al., 2017) enhancing MOUD effectiveness by increasing treatment referrals, linkages, and retention rates, (Hagan et al., 2000, Hood et al., 2020) while also serving as key connections to overdose education and naloxone distribution. (Lambdin et al., 2020) However, barriers such as stigma and laws against possession of drug paraphernalia continue to mire progress toward the introduction of more SSPs. (Kishore et al., 2019) Furthermore, SSP authorization is still challenged in Indiana even as the expiration of the current state-level authorization bill has been extended to July 2026. As new restrictions against SSPs are under debate across the country in 2021, even Scott County has witnessed a two to one vote by county officials ending the SSP originating from the 2014–2015 outbreak. (Knowles, 2021) This rollback and ongoing debate over the continued authorization of SSPs raises the importance of reiterating the lessons learned from the Scott County outbreak—that SSPs are effective in preventing opioid-related harms and the importance of acting proactively instead of reactively. (Cooke and Gonsalves, 2021)
Several limitations should be considered when reflecting on these findings. Due to the limitations of publicly available opioid-involved overdose mortality data, we conducted our analyses primarily at the county-level. We used chronic HCV in lieu of acute HCV as a proxy for injection drug use due to low counts per county of acute HCV. Due to the limited sample size, 92 counties, our novel regression-weighted quintile ranking methodology uses bivariate regression models instead of a multivariable model. To address its limitations, we conducted several model diagnostics and conducted a sensitivity analysis. The sensitivity analysis showed that the vulnerability index obtained from the utilized regression weighted rank approach was highly correlated with the vulnerability estimates obtained from a multivariable negative binomial model (Coefficient of correlation: 0.81, Appendix 3).
Further limitations specific to the 2SFCA analyses include that we used OUD treatment services data from 2020 and Indiana naloxone provider services data from 2018, while the rest of analysis leveraged 2017 data. While this may limit the comparability between the vulnerability and 2SFCA analyses, we decided that assessing accessibility in a way that reflects current realities is the best approach for a cross-sectional assessment to accurately inform policymaking and intervention responses related to OUD services. Our data did not allow 2SFCA to calculate travel times for services outside Indiana but close to the state border, possibly resulting in edge effects around the state border. In addition, due to the lack of census tract-level data to describe OUD prevalence, our 2SFCA models utilized total population as the denominator for the provider to population ratios. Furthermore, due to data constraints, the 2SFCA analyses treated all identified OUD and naloxone services as having the same patient capacity when, in reality, providers such as waivered buprenorphine practitioners have varying patient limits. It is possible that areas with many small-capacity OUD service locations may be identified as having more access than a location with a few higher-capacity OUD service locations. However, it is important to note that only a limited number of buprenorphine waivered physicians prescribe buprenorphine. Furthermore, those who prescribe buprenorphine commonly treat fewer patients relative to their waivered capacity. (Duncan et al., 2020)()
5. Conclusion
Given the ongoing devastation tied to the opioid crisis across the United States, as well as its further exacerbation during the coronavirus pandemic, our rapid, rigorous, and policy-informing opioid-involved overdose vulnerability assessment can help to inform activities and responses by public health officials on the state and local levels. Our vulnerability ranking approach, which builds on previous vulnerability assessments at the national level, highlighted a number of counties that are highly vulnerable to opioid overdose and related comorbidities, providing local public health officials with salient findings to inform targeted public health responses. Findings from this vulnerability assessment provide local-level context and evidence to support ongoing and enhanced harm reduction services, particularly in areas with high opioid overdose vulnerability and low access to services. Specifically, our findings provide support for continuing SSPs in highly vulnerable Clark, Fayette, Madison, Marion, and Wayne counties; reopening an SSP in Scott County; and new harm reduction programs in the highly vulnerable counties currently without SSPs including Blackford, Delaware, Floyd, Grant, Howard, Jay, Lake, LaPorte, Madison, Randolph, St. Joseph, Starke, Vanderburgh, and Washington counties. Our approach can be used as a model to identify vulnerable communities in any state and inform public health prevention and harm reduction efforts to curb the escalating national opioid crisis.
6. Financial disclosure statement
The Council of State and Territorial Epidemiologists (CSTE) provided technical assistance to this Indiana Opioid Overdose Vulnerability Assessment through the Tufts University School of Medicine. This project is funded through the Centers for Disease Control and Prevention’s (CDC’s) National Center for Injury Prevention and Control (NCIPC) and supported by Cooperative Agreement number CDC-RFA-OT18-1804: Technical Assistance for Response to Public Health or Healthcare Crises. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC.
CRediT authorship contribution statement
Jare L. Sawyer: wrote the initial draft of the manuscript, contributed to GIS data visualization and spatial analyses, and led review and editing of the final manuscript. Shikhar Shrestha: assisted with methodology, data visualization, and led statistical and spatial analyses. Jennifer C. Pustz: assisted with data visualization using GIS software and running spatial analyses. Robert Gottlieb: facilitated access to local data curation, assisted with geospatial data visualization, and interpretation of findings. Deborah Nichols: assisted with local data curation and interpretation of findings. Michelle Van Handel: assisted with project conceptualization, data curation, methodology, validation, and interpretation of findings. Cailyn Lingwall: assisted with project conceptualization, funding acquisition, and project supervision. Thomas J. Stopka: was responsible for funding acquisition, leading the overall investigation, supervising staff, geospatial visualization, validation, and interpretation of findings. All authors assisted in writing and editing manuscript drafts and approving the final manuscript.
Appendix.
Appendix 3.
Results from sensitivity analysis using a multivariable negative binomial regression model. The sensitivity analysis highlighted that the vulnerability index obtained from the regression weighted rank approach was highly correlated with vulnerability estimates obtained from a multivariable negative binomial model approach with a coefficient of correlation of 0.81.
| Variable | Beta coefficient | Standard error | p-value |
|---|---|---|---|
| Opioid-related emergency department visits per 100,000 population | 0.38 | 0.09 | <0.0001 |
| Opioid-related arrests per 100,000 population | −0.01 | 0.06 | 0.845 |
| Opioid prescriptions per 100,000 population | 0.08 | 0.08 | 0.3037 |
| Chronic hepatitis C cases per 100,000 population | 0.2 | 0.08 | 0.0093 |
| Percentage of female-led households | 0.12 | 0.12 | 0.3008 |
| Unemployment rate | 0.02 | 0.1 | 0.8061 |
| Gini Index (a measure of inequality) | 0.02 | 0.08 | 0.8092 |
| Percentage of the population above 25 years of age without a high school diploma | 0.08 | 0.09 | 0.3877 |
| Percentage of the population with disability | 0.06 | 0.09 | 0.4816 |
| Percentage of the population that is non-Hispanic Black | −0.03 | 0.15 | 0.8572 |
References
- Agency for Healthcare Research and Quality, Substance Abuse and Mental Health Services Administration. Blacks Experiencing Fast-Rising Rates of Overdose Deaths Involving Synthetic Opioids Other Than Methadone.; 2020. https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/dataspotlight-opioid.pdf.
- Alexander M.J., Kiang M.V., Barbieri M. Trends in black and white opioid mortality in the United States, 1979–2015. Epidemiology. 2018;29(5):707–715. doi: 10.1097/EDE.0000000000000858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altekruse, S.F., Cosgrove, C.M., Altekruse, W.C., Jenkins, R.A., 2020, Blanco C. Socioeconomic risk factors for fatal opioid overdoses in the United States: Findings from the Mortality Disparities in American Communities Study (MDAC). Genberg BL, ed. PLoS ONE. 2020;15(1):e0227966. doi:10.1371/journal.pone.0227966. [DOI] [PMC free article] [PubMed]
- Aspinall E.J., Nambiar D., Goldberg D.J., et al. Are needle and syringe programmes associated with a reduction in HIV transmission among people who inject drugs: a systematic review and meta-analysis. Int. J. Epidemiol. 2014;43(1):235–248. doi: 10.1093/ije/dyt243. [DOI] [PubMed] [Google Scholar]
- Ayres J., Waldorf B., McKendree M., Hoelscher L. Purdue University; 2013. Defining Rural Indiana—The First Step.https://www.extension.purdue.edu/extmedia/EC/EC-766-W.pdf [Google Scholar]
- Batdorf, S., 2020, County-Level Vulnerability to HIV, HCV, and Overdose Mortality West Virginia, 2016-2017. West Virginia Department of Health and Human Resources.
- Bechteler, S., Kane-Willis, K., Metzger, 2017. Whitewashed: The African American Opioid Epidemic. The Chicago Urban League.
- Box, K., Pontones, P., Stover, D., et al. Indiana 2016 Viral Hepatitis Epidemiologic Profile. Indiana State Department of Health; 2017. https://www.in.gov/isdh/27850.htm.
- Brown School of Public Health. The VILLAGE Prevention Plan: Improving Prevention Efforts and Health Outcomes for People Who Use Drugs. Findings from the VILLAGE Project: A Jurisdictional Plan for Rhode Island.; 2019. https://preventoverdoseri.org/wp-content/uploads/2019/11/VILLAGE-Prevention-Plan.pdf.
- Bulled N., Singer M. Syringe-mediated syndemics. AIDS Behav. 2011;15(7):1539–1545. doi: 10.1007/s10461-009-9631-1. [DOI] [PubMed] [Google Scholar]
- CDC Health Alert Network. Increase in Fatal Drug Overdoses Across the United States Driven by Synthetic Opioids Before and During the COVID-19 Pandemic.; 2020.
- Census.gov. 2013-2017 ACS 5-year Estimates. Published 20 https://www.census.gov/programs-surveys/acs/technical-documentation/table-and-geography-changes/2017/5-year.html.
- Centers for Disease Control and Prevention. U.S. County Prescribing Rates, 2017.; 2017. https://www.cdc.gov/drugoverdose/maps/rxcounty2017.html.
- Ciccarone D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int. J. Drug Policy. 2019;71:183–188. doi: 10.1016/j.drugpo.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrad, C., Bradley, H., Broz, D., et al., 2015, Community Outbreak of HIV Infection Linked to Injection Drug Use of Oxymorphone — Indiana, 2015. Published online May 1, 2015. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6416a4.htm. [PMC free article] [PubMed]
- Cooke, W., Gonsalves, G., 2021, Closing an Indiana county’s syringe services program would be a public health disaster. STAT. https://www.statnews.com/2021/06/01/syringe-services-program-closure-scott-county-public-health-disaster/. Published June 2021.
- Dasgupta N., Beletsky L., Ciccarone D. Opioid crisis: no easy fix to its social and economic determinants. Am. J. Public Health. 2018;108(2):182–186. doi: 10.2105/AJPH.2017.304187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan Alexandra, Anderman Jared, Deseran Travis. Monthly Patient Volumes of Buprenorphine-Waivered Clinicans in the US. Substance Use and Addiction. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.14045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwyer K., Walley A.Y., Langlois B.K., et al. Opioid education and nasal naloxone rescue kits in the emergency department. West J. Emerg. Med. 2015;16(3):381–384. doi: 10.5811/westjem.2015.2.24909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N., Shoptaw S., Goodman-Meza D., Ono H. Addressing long overdue social and structural determinants of the opioid epidemic. Drug Alcohol Dependence. 2021;222 doi: 10.1016/j.drugalcdep.2021.108679. [DOI] [PubMed] [Google Scholar]
- Friedman, J., Mann, N.C., Hansen, H., et al., 2021, Racial/Ethnic, Social, and Geographic Trends in Overdose-Associated Cardiac Arrests Observed by US Emergency Medical Services During the COVID-19 Pandemic. JAMA Psychiatry. Published online May 26, 2021. doi:10.1001/jamapsychiatry.2021.0967. [DOI] [PMC free article] [PubMed]
- Fullerton C.A., Kim M., Thomas C.P., et al. Medication-assisted treatment with methadone: assessing the evidence. PS. 2014;65(2):146–157. doi: 10.1176/appi.ps.201300235. [DOI] [PubMed] [Google Scholar]
- Furr-Holden D., Milam A.J., Wang L., Sadler R. African Americans now outpace whites in opioid-involved overdose deaths: a comparison of temporal trends from 1999 to 2018. Addiction. 2021;116(3):677–683. doi: 10.1111/add.15233. [DOI] [PubMed] [Google Scholar]
- Glober, N., Mohler, G., Huynh, P., et al., 2020, Impact of COVID-19 Pandemic on Drug Overdoses in Indianapolis. J Urban Health. Published online October 1, 2020:1-6. doi:10.1007/s11524-020-00484-0. [DOI] [PMC free article] [PubMed]
- Goedel W.C., Shapiro A., Cerdá M., Tsai J.W., Hadland S.E., Marshall B.D.L. Association of racial/ethnic segregation with treatment capacity for opioid use disorder in counties in the United States. JAMA Netw Open. 2020;3(4) doi: 10.1001/jamanetworkopen.2020.3711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goedel W.C., King M.R.F., Lurie M.N., et al. Implementation of syringe services programs to prevent rapid human immunodeficiency virus transmission in rural counties in the United States: a modeling study. Clin. Infectious Dis. 2020;70(6):1096–1102. doi: 10.1093/cid/ciz321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonsalves G.S., Crawford F.W. Dynamics of the HIV outbreak and response in Scott County, IN, USA, 2011–15: a modelling study. Lancet HIV. 2018;5(10):e569–e577. doi: 10.1016/S2352-3018(18)30176-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinspoon, P., 2020, A tale of two epidemics: When COVID-19 and opioid addiction collide. Harvard Health Publishing. https://www.health.harvard.edu/blog/a-tale-of-two-epidemics-when-covid-19-and-opioid-addiction-collide-2020042019569. Published 2020.
- Hagan H., McGough J.P., Thiede H., Hopkins S., Duchin J., Alexander E.R. Reduced injection frequency and increased entry and retention in drug treatment associated with needle-exchange participation in Seattle drug injectors. J. Subst. Abuse Treat. 2000;19(3):247–252. doi: 10.1016/s0740-5472(00)00104-5. [DOI] [PubMed] [Google Scholar]
- Hansen, H., Roberts, S.K., 2012, Two Tiers of Biomedicalization: Methadone, Buprenorphine, and the Racial Politics of Addiction Treatment. In: Netherland J, ed. Advances in Medical Sociology. Emerald Group Publishing Limited; 2012:79-102. doi:10.1108/S1057-6290(2012)0000014008.
- Hansen H.B., Siegel C.E., Case B.G., Bertollo D.N., DiRocco D., Galanter M. Variation in use of buprenorphine and methadone treatment by racial, ethnic, and income characteristics of residential social areas in New York City. J. Behav. Health Serv. Res. 2013;40(3):367–377. doi: 10.1007/s11414-013-9341-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen H., Siegel C., Wanderling J., DiRocco D. Buprenorphine and methadone treatment for opioid dependence by income, ethnicity and race of neighborhoods in New York City. Drug Alcohol Depend. 2016;164:14–21. doi: 10.1016/j.drugalcdep.2016.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawk K.F., Vaca F.E., D’Onofrio G. Reducing fatal opioid overdose: prevention, treatment and harm reduction strategies. Yale J. Biol. Med. 2015;88(3):235–245. [PMC free article] [PubMed] [Google Scholar]
- Hedegaard Holly, Spencer Merianne Rose. Urban-rural differences in drug overdose death rates, 1999-2019. NCHS Data Brief. 2021;403 [PubMed] [Google Scholar]
- Helmick R. Drug overdose trends among black Indiana Residents: 2013-2017. OJPHI. 2019;11(1) doi: 10.5210/ojphi.v11i1.9916. [DOI] [Google Scholar]
- Hernandez A., Branscum A.J., Li J., MacKinnon N.J., Hincapie A.L., Cuadros D.F. Epidemiological and geospatial profile of the prescription opioid crisis in Ohio, United States. Sci. Rep. 2020;10(1):4341. doi: 10.1038/s41598-020-61281-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood J.E., Banta-Green C.J., Duchin J.S., et al. Engaging an unstably housed population with low-barrier buprenorphine treatment at a syringe services program: Lessons learned from Seattle, Washington. Substance Abuse. 2020;41(3):356–364. doi: 10.1080/08897077.2019.1635557. [DOI] [PubMed] [Google Scholar]
- IN.gov Management Performance Hub. DRUG SUBMISSIONS TO INDIANA STATE POLICE LABORATORIES. Published 2018. https://www.in.gov/mph/1229.htm.
- Indiana Department of Health. Naloxone Providers (2018). Published online 2018. https://maps.indiana.edu/previewMaps/Infrastructure/Facilities_Naloxone_Providers_ISDH.html.
- Indiana Department of Health. Stats Explorer. https://gis.in.gov/apps/isdh/Meta/Stats_Layers.htm.
- Indiana University. Stigma around substance use disorder higher in rural areas, new IU study finds. Addictions. https://addictions.iu.edu/news/stigma-rural-urban.html. Published September 2020.
- Iowa Department of Public Health, Bureau of HIV, STD, and Hepatitis. Iowa County-Level Vulnerability Assessments for Risk of Opioid Overdoses and Rapid Dissemination of HIV and Hepatitis C.; 2019.
- James K., Jordan A. The opioid crisis in black communities. J. Law Med. Ethics. 2018;46(2):404–421. doi: 10.1177/1073110518782949. [DOI] [PubMed] [Google Scholar]
- Kapadia, S.N., Griffin, J.L., Waldman, J., Ziebarth, N.R., Schackman, B.R., Behrends, C.N., 2021, A Harm Reduction Approach to Treating Opioid Use Disorder in an Independent Primary Care Practice: a Qualitative Study. J GEN INTERN MED. Published online January 19, 2021. doi:10.1007/s11606-020-06409-6. [DOI] [PMC free article] [PubMed]
- Kattakuzhy, S., Rosenthal, E., 2020, To Eliminate Hepatitis C in People Who Inject Drugs, Stop Ignoring Drug-user Health. Clinical Infectious Diseases. Published online May 23, 2020:ciaa607. doi:10.1093/cid/ciaa607. [DOI] [PubMed]
- Kishore S., Hayden M., Rich J. Lessons from Scott county — progress or paralysis on harm reduction? N. Engl. J. Med. 2019;380(21):1988–1990. doi: 10.1056/NEJMp1901276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowles, H., 2021, Rural Indiana county ends needle swap that helped fight HIV — sparking fears of another outbreak. Washington Post. https://www.washingtonpost.com/health/2021/06/05/indiana-needle-exchange-hiv/. Published June 5, 2021.
- Lagisetty, P.A., Ross, R., Bohnert, A., Clay, M., Maust, D.T., 2019, Buprenorphine Treatment Divide by Race/Ethnicity and Payment. JAMA Psychiatry. Published online May 8, 2019. doi:10.1001/jamapsychiatry.2019.0876. [DOI] [PMC free article] [PubMed]
- Lambdin B.H., Bluthenthal R.N., Wenger L.D., et al. Overdose education and naloxone distribution within syringe service programs — United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(33):1117–1121. doi: 10.15585/mmwr.mm6933a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langford, M., Fry, R., Higgs, G., 2015, USW-FCA2: An ArcGIS Add-In Tool to Compute Enhanced Two-Step Floating Catchment Area Accessibility Scores.
- Larochelle M.R., Bernson D., Land T., et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: a cohort study. Ann. Intern. Med. 2018;169(3):137–145. doi: 10.7326/M17-3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larochelle M.R., Bernstein R., Bernson D., et al. Touchpoints - Opportunities to predict and prevent opioid overdose: a cohort study. Drug Alcohol Depend. 2019;204 doi: 10.1016/j.drugalcdep.2019.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo W., Wang F. Measures of spatial accessibility to health care in a GIS environment: synthesis and a case study in the Chicago Region. Environ. Plann. B Plann. Des. 2003;30(6):865–884. doi: 10.1068/b29120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mack K.A., Jones C.M., Ballesteros M.F. Illicit drug use, illicit drug use disorders, and drug overdose deaths in metropolitan and nonmetropolitan areas — United States. MMWR Surveill. Summ. 2017;66(19):1–12. doi: 10.15585/mmwr.ss6619a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madras, B.K., Ahmad, N.J., Wen, J., Sharfstein, J., Prevention, Treatment, and Recovery Working Group of the Action Collaborative on Countering the U.S. Opioid Epidemic. Improving Access to Evidence-Based Medical Treatment for Opioid Use Disorder: Strategies to Address Key Barriers Within the Treatment System. NAM Perspectives. Published online April 27, 2020. doi:10.31478/202004b. [DOI] [PMC free article] [PubMed]
- Maldonado G., Greenland S. Simulation study of confounder-selection strategies. Am. J. Epidemiol. 1993;138(11):923–936. doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]
- Mauer, M., 2020, The Changing Racial Dynamics of the War on Drugs. Published online April 2009. https://www.sentencingproject.org/wp-content/uploads/2016/01/The-Changing-Racial-Dynamics-of-the-War-on-Drugs.pdf.
- McBournie, A., Duncan, A., Connolly, E., Rising, J., 2019, Methadone Barriers Persist, Despite Decades Of Evidence. Health Affairs Blog. Published online September 2019. doi:10.1377/hblog20190920.981503/full/.
- Minnesota Department of Health. Race Rate Disparity in Drug Overdose Death.; 2018. https://www.health.state.mn.us/communities/opioids/documents/raceratedisparity.pdf.
- Missouri Department of Health and Senior Services, Bureau of Reportable Disease Informatics. Missouri Opioid Overdose and Bloodborne Infection Vulnerability Assessments 2020.; 2020. http://health.mo.gov/data/opioids/assessments.php.
- Mitchell O., Caudy M.S. Race differences in drug offending and drug distribution arrests. Crime Delinquency. 2017;63(2):91–112. doi: 10.1177/0011128714568427. [DOI] [Google Scholar]
- Morgan J.R., Schackman B.R., Weinstein Z.M., Walley A.Y., Linas B.P. Overdose following initiation of naltrexone and buprenorphine medication treatment for opioid use disorder in a United States commercially insured cohort. Drug Alcohol Depend. 2019;200:34–39. doi: 10.1016/j.drugalcdep.2019.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Rural Health Association. Treating the Rural Opioid Epidemic. Published online February 2017. https://www.ruralhealthweb.org/NRHA/media/Emerge_NRHA/Advocacy/Policy%20documents/Treating-the-Rural-Opioid-Epidemic_Feb-2017_NRHA-Policy-Paper.pdf.
- Office of Behavioral Health Equity, Substance Abuse and Mental Health Services Administration. Double Jeopardy: COVID-19 and Behavioral Health Disparities for Black and Latino Communities in the U.S. (Submitted by OBHE).; 2020. https://www.samhsa.gov/sites/default/files/covid19-behavioral-health-disparities-black-latino-communities.pdf.
- Opioid Response Network. The Opioid Epidemic and COVID-19: How Social Determinants of Health Create Differential Impacts.; 2020. https://opioidresponsenetwork.org/documents/SDH_OUD-COVID-19.pdf.
- Paulozzi, L., Jones, C., Mack, K., Rudd, R., 2011, Vital Signs: Overdoses of Prescription Opioid Pain Relievers --- United States, 1999--2008. Published online November 4, 2011. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6043a4.htm.
- Perlman D.C., Jordan A.E. The syndemic of opioid misuse, overdose, HCV, and HIV: structural-level causes and interventions. Curr. HIV/AIDS Rep. 2018;15(2):96–112. doi: 10.1007/s11904-018-0390-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phalen P., Ray B., Watson D.P., Huynh P., Greene M.S. Fentanyl related overdose in Indianapolis: estimating trends using multilevel Bayesian models. Addict. Behav. 2018;86:4–10. doi: 10.1016/j.addbeh.2018.03.010. [DOI] [PubMed] [Google Scholar]
- Platt, L., Minozzi, S., Reed, J., et al., 2017, Needle syringe programmes and opioid substitution therapy for preventing hepatitis C transmission in people who inject drugs. Cochrane Database Syst Rev. 9:CD012021. doi:10.1002/14651858.CD012021.pub2. [DOI] [PMC free article] [PubMed]
- Ray B., Lowder E., Bailey K., Huynh P., Benton R., Watson D. Racial differences in overdose events and polydrug detection in Indianapolis, Indiana. Drug Alcohol Depend. 2020;206 doi: 10.1016/j.drugalcdep.2019.107658. [DOI] [PubMed] [Google Scholar]
- Rickles M., Rebeiro P.F., Sizemore L., et al. Tennessee’s In-state Vulnerability Assessment for a “Rapid Dissemination of Human Immunodeficiency Virus or Hepatitis C Virus Infection” Event Utilizing Data About the Opioid Epidemic. Clin. Infect. Dis. 2018;66(11):1722–1732. doi: 10.1093/cid/cix1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharareh N., Hess R., White S., Dunn A., Singer P.M., Cochran J. A vulnerability assessment for the HCV infections associated with injection drug use. Prev. Med. 2020;134 doi: 10.1016/j.ypmed.2020.106040. [DOI] [PubMed] [Google Scholar]
- Short E., Orkis L., Ma M., Watkins S. Public Health Impacts of the Opioid Epidemic Vulnerability to Bloodborne Infections and Overdose Death. Pennsylvania Department of Health; 2020. Bureau of Epidemiology. [Google Scholar]
- Singhal A., Tien Y.-Y., Hsia R.Y. Racial-ethnic disparities in opioid prescriptions at emergency department visits for conditions commonly associated with prescription drug abuse. PLoS One. 2016;11(8) doi: 10.1371/journal.pone.0159224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S., Rock P., Bush H.M., Quesinberry D., Walsh S.L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214 doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sordo L., Barrio G., Bravo M.J., et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357 doi: 10.1136/bmj.j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South Dakota Department of Health. South Dakota Vulnerability Assessment Risk of Opioid Overdose, HIV, and Viral Hepatitis.; 2019. https://doh.sd.gov/statistics/ vulnerabilityassessment.aspx.
- Substance Abuse and Mental Health Services Administration. The Opioid Crisis and the Black/African American Population: An Urgent Issue. Office of Behavioral Health Equity; 2020.
- Substance Abuse and Mental Health Services Administration. SAMHSA Treatment Locator. https://findtreatment.samhsa.gov/locator.
- Sutfim L. Opioid Overdoses Surge during COVID-19 Pandemic; MDHHS Promotes Treatment and Resources. Michigan.gov; 2020. https://www.michigan.gov/som/0,4669,7-192-29942_34762-535078--,00.html.
- van Draanen J., Tsang C., Mitra S., Karamouzian M., Richardson L. Socioeconomic marginalization and opioid-related overdose: a systematic review. Drug Alcohol Depend. 2020;214 doi: 10.1016/j.drugalcdep.2020.108127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Handel M.M., Rose C.E., Hallisey E.J., et al. County-level vulnerability assessment for rapid dissemination of HIV or HCV infections among persons who inject drugs, United States. J. Acquir. Immune Defic. Syndr. 2016;73(3):323–331. doi: 10.1097/QAI.0000000000001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N.D. To end the opioid crisis, we must address painful social disparities. Drug Alcohol Dependence. 2021;222 doi: 10.1016/j.drugalcdep.2021.108678. [DOI] [PubMed] [Google Scholar]
- Walley A.Y., Xuan Z., Hackman H.H., et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346 doi: 10.1136/bmj.f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F., Luo W. Assessing spatial and nonspatial factors for healthcare access: towards an integrated approach to defining health professional shortage areas. Health Place. 2005;11(2):131–146. doi: 10.1016/j.healthplace.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Watson, D., Duwve, J., Marion, G., Weathers, T., Huynh, P., Nannery, R., 2018, The Changing Landscape of the Opioid Epidemic in Marion County and Evidence for Action. Indiana University Richard M. Fairbanks School of Public Health; 2018. https://www.rmff.org/wp-content/uploads/2018/10/Richard-M.-Fairbanks-Opioid-Report-October-2018.pdf.