Highlights
-
•
People with lower-limb loss even with community walking ability have high annual fall and injury rates.
-
•
True fall and injury risk may be obscured if exposure to risk measured by person-steps over time is not considered.
-
•
Risk was higher for amputees with limited walking ability per person-step exposure over time.
-
•
Incorporating person-step exposure over time clarifies fall and injury risk level.
Keywords: Falls, Injuries, Amputation, Prostheses, Daily steps, Physical activity
Abbreviations: CI, Confidence Intervals; GEEs, Generalized Estimating Equations; IRR, Incidence Rate Ratios; PLL, People with Lower-limb Loss; TFA, Transfemoral Amputation; TTA, Transtibial Amputations
Abstract
People with lower-limb loss (PLL) have high annual fall and injury rates. People with transtibial amputations have better walking function than those with transfemoral amputations but paradoxically incur more fall-related injuries. Risk exposure, however, has not been previously considered. This study examined whether all-cause fall and injury incidence per person-step exposure over time varied in PLL of different walking abilities. The prospective cohort design, conducted at a major medical center, included five assessments 1-month apart. Walking ability level was categorized by Houghton Scale scores: ≥9 indicating community walking and ≤ 8 indicating limited community-household walking. Accelerometer-measured daily step counts were collected via StepWatch4 monitors. The main outcome measures, self-reported all-cause falls and injuries were assessed using the standard National Health Injury Survey. Generalized estimating equations, using Poisson distributions and log of step count as an offset, determined fall and injury incidence rate ratio [IRR] according to walking ability level. Ten people, aged 33–63 years with amputations of different causes and levels, were assessed monthly over five months. The community walking group (n = 6) had six falls and seven injuries; the limited community walking group (n = 4) had four falls and three injuries. For PLL, limited community walking ability was associated with higher incidence of falls (IRR = 6.10, 95%CI = 1.12–33.33, p = 0.037) and injuries (IRR = 8.56, 95%CI = 1.73–42.40, p = 0.009) when accounting for person-steps. Considering per person-step exposure over time added precision to fall and injury risk assessment that clarified the risks: PLL with limited community walking ability have higher fall and injury risks.
1. Introduction
After amputation, people with lower-limb loss (PLL) face lifelong challenges within their communities (Roepke et al., 2017). Most PLL have amputations due to chronic and progressive conditions such as diabetes and peripheral arterial disease that limit their overall function (Ziegler-Graham et al., 2008). Though PLL with traumatic amputations are younger and healthier, related physical and psychological complications (Perkins et al., 2012) and common age-related disorders affect prosthetic function over their lifetimes (Wong and Chihuri, 2019). Roughly half of PLL in the United States receive a prosthesis for ambulation, though health costs and service disparities may lower this proportion globally (Webster et al., 2012). Even with a prosthesis, the loss of lower limb joints and musculature leads to balance impairment (Wong et al., 2013), gait asymmetries (Nolan et al., 2003), and reduced physical activity (Parker et al., 2010). Despite the best efforts and functional gains during initial training, limited functional mobility is a reality for most PLL and many never reach the independent community walking level even years after amputation (Wong et al., 2016).
In addition to limited walking ability, falls among PLL are common. Annual fall rates for community-dwelling PLL range from 40 to 80% (Hunter et al., 2017) and have been associated with lower balance confidence (Miller et al., 2001) and balance ability (Wong et al., 2015). Balance ability degrades with age, and the rate of falls in elderly PLL are among the highest (Hunter et al., 2017). PLL with more impaired balance have had more falls compared to less impaired PLL (Wong et al., 2015, Dite et al., 2007) However, when balance ability and self-reported balance confidence have been included together in multivariable explanatory models for falls, PLL with better balance had increased likelihood of falling (Wong and Chihuri, 2019, Wong et al., 2015).
Falls can compound the challenges of limited walking ability for PLL, by decreasing balance confidence, inhibiting physical activity, or introducing secondary injury (Miller et al., 2001, Chihuri and Wong, 2018). Fall-related injuries occur most often during ambulation, with ramps and stairs posing special risks; injuries also occur during activities of daily living and basic mobility tasks (Wong et al., 2016). Fall and fall-related injury rates among PLL exceed the rates reported for other vulnerable populations such as older people (Wong et al., 2016). Specific subgroups of PLL, such as those with chronic vascular disease or transtibial amputations (TTA), have elevated risks of fall-related injuries (Chihuri and Wong, 2018). People with chronic vascular conditions are intuitively considered more vulnerable to falls and injury (Wong et al., 2016). Conversely, it seems paradoxical that people with TTA, who have intact knee anatomy and typically higher walking ability compared to people with transfemoral amputations (TFA), would experience more fall-related injuries (Chihuri and Wong, 2018, Wong et al., 2020).
People with better walking ability may be more active and thus be exposed to greater risk over similar time periods (Wong and Chihuri, 2019). Fall and injury rates for PLL have typically been reported annually (Miller et al., 2001, Wong et al., 2015, Kim et al., 2019), introducing recall bias especially in retrospective studies over lengthy periods of time (Blome and Augustin, 2015). In addition, falls may not lead to injury, and injuries may result from non-fall events. Reporting annual rates does not consider variations in setting or physical activity. Some highly active individuals may take over 10,000 steps per day and/or engage in community sports activity (Parker et al., 2010). But far more PLL are limited to household ambulation and may fall at home just getting out of bed (Chihuri and Wong, 2018). Estimating physical activity levels with self-reported scales, however, lacks validity (Lamb et al., 2005). Considering each individual’s falls or injuries in relation to their specific directly monitored physical activity level prospectively over predetermined periods could provide more accurate risk assessments based on exposure.
One prospective longitudinal study examined injury per person-time exposure over a four-year period and found that 56% fell and 27% suffered injuries requiring medical care (Wong et al., 2016). Fall incidence was 14.1/1000 person-months, although physical activity over each month was not assessed (Wong et al., 2016). Over the years, studies of sports injury incidence have progressed from reporting injuries per season, to injuries per games and practices, to injuries per minutes played (Stovitz and Shrier, 2012). Similarly, studies of traffic safety now adjust for immediate exposure risk which otherwise could bias results. For example, a recent epidemiological analysis found a crude decrease in motor vehicle crash incidence associated with ridesharing (Morrison et al., 2020). However, when accounting for traffic volume exposure, which varied during the day, an increased risk of crashes associated with ridesharing was revealed (Morrison et al., 2020). Thus, a more nuanced understanding of fall and injury incidence in PLL may be gained by examining fall and injury incidence in the context of a time-variant proxy for risk exposure such as an individual’s average daily step counts varying over time.
Though PLL may fall and incur injuries during activities without using the prosthetic limb, the primary difference in exposure risk between people with and without lower-limb amputation can be defined as individual physical activity measured by average daily person-steps. The purpose of this study was to determine all-cause fall and injury rates for PLL over time taking into account daily per person-step exposure. We hypothesized that PLL at the community walking level might fall more, but because of higher physical activity and greater per person-step exposure would be at relatively lower risk of falls and injuries than PLL with limited community walking ability. A second hypothesis was that falls and injuries would not always occur together.
2. Methods
2.1. Design
This prospective repeated-measure cohort study was approved by the participating medical center Institutional Review Board and met the guidelines for protecting human subject safety and privacy (#AAAR-7523). Written informed consent was obtained for all participants, who then had five assessments scheduled 4-weeks apart including: pre- and post-treatment assessments, and three follow-up assessments. Between pre- and post-treatment assessments, all participants received physical therapy treatment that consisted of four separate 1-hour sessions comprised of joint mobilization and stretching, weight-bearing strengthening exercises, and functional training. No treatment or instructions for continued exercise or activity were given during follow-up.
2.2. Participants
Adults aged 18–70 y, of any sex or race, were eligible for inclusion if they had a unilateral TTA or TFA of any cause. Volunteers who had completed initial prosthetic training and were living in the community were recruited from the local support groups, prosthetic clinics, and medical center. All participants could walk independently with their prosthesis at least three m, with or without using a walking aid before inclusion. Potential participants were excluded if they could not understand the study description for any reason; had diagnosed medical conditions affecting balance including blindness, vestibular disorders, traumatic brain injury, and hemiplegia; or had medical conditions making exercise dangerous such as uncontrolled hypertension or unstable angina. Planned sample size for the 1-year funding period was 10 participants, based on a past interventional study (Wong et al., 2016), to allow for 50 data collection points.
2.3. Procedures
Participants completed the study questionnaire and all assessments. All data were obtained by the investigators after training on all assessments.
Questionnaire data included individual characteristics, amputation and medical history, prosthetic information, and walking ability level classified by the Houghton score (Wong et al., 2016, Houghton et al., 1992). The self-reported 7-question Houghton scale combines prosthetic wear time, use of walking aids and the prosthesis, and steadiness when walking indoors and outdoors in three conditions, and has demonstrated criterion-related validity and reliability (Wong et al., 2016, Houghton et al., 1992, Miller et al., 2001). Houghton scores of ≥ 9 initially suggested to describe successful prosthetic mobility in community settings (Houghton et al., 1992) were later found to categorize significantly different balance and walking abilities assessed by performance and self-reported measures (Wong et al., 2016). Thus, community walking ability was categorized as Houghton scores ≥ 9, functionally comparable to the Medicare Functional Classification level K-3 or higher; while scores ≤ 8 indicated limited community-household walking ability, comparable to the K-2 level or lower (Wong et al., 2016).
To capture daily step count remotely, a StepWatch4 Modus Health Step Activity Monitor (https://modushealth.com) was strapped just above the lateral prosthetic ankle to collect step counts for an objective measure of physical activity, defined as average daily step count (Hordacre et al., 2014). Participants were instructed to not remove the StepWatch4 monitor between assessments. Accelerometer data were downloaded and stored using the laptop base station and processed with StepWatch4 software, with prosthetic steps multiplied by two to represent total steps taken, as previously validated (Hordacre et al., 2014). Average daily step count was derived from the last full week of 24-hour/day data collection closest in time to each evaluation assessment to ensure capture of both weekday and weekend step activity.
2.4. Outcomes
The primary outcomes were incidence of all-cause falls and injuries retrospectively assessed during the structured interview using National Health Injury Survey questions (Chen et al., 2009). A fall was defined as an unexpected loss of balance resulting in the individual’s body on the ground, floor, or lower level (Kim et al., 2019, Lamb et al., 2005, Chen et al., 2009). Detailed fall and injury circumstances were obtained together at intake to provide descriptive participant information and during study surveillance for each 4-week period for analysis (Lamb et al., 2005).
Additional qualitative information about any falls occurring between assessments was obtained via structured interview questions from the National Health Injury Survey including number of falls, how and where falls occurred, what caused the falls, and whether injury occurred (Chen et al., 2009). Fall mechanisms were classified as slips when involving slick surfaces such as ice, water, or oil; trips when involving a kick or toe catch on obstacles such as steps or curbs, rugs or floor objects; and falls when involving any knee collapse or other non-specified cause (Stevens et al., 2014). Fall locations were classified primarily as indoor or outdoor. Injury information was also obtained using the structured National Health Injury Survey questions, with injury defined as the person having hurt any bodypart (Chen et al., 2009). Specific information included number of injuries and injured body parts, such as amputated residual-limb, non-amputated sound limb, back, head, upper-limb, or other. Additional detail included injury types, how the injury occurred such as during a fall, what activity was occurring at the time of injury, and whether the injury severity required treatment from friend/family/self, advice from a health care professional, treatment from emergency responders, medical consult in a clinic or emergency room, or hospitalization including surgery (Chen et al., 2009).
2.5. Data analysis
Descriptive statistics were computed for demographic data and baseline clinical variables, such as falls, injuries, and functional status. Frequency distributions were computed to describe fall type or location and injury type (i.e. fall-related or other). Differences between those with and without falls or injuries were assessed using nonparametric tests (Fisher’s exact, Mann Whitney U).
Generalized estimating equations (GEEs) using the Poisson distribution and log of step count exposure as an offset were used to assess Incidence Rate Ratios (IRR) for falls and injuries by walking ability status. Data was not imputed for missing values. GEEs estimate the parameters of a generalized linear model accounting for correlation within individuals such as repeated falls and injuries over time intervals. The within participant repeated-measures over time account for varying risk exposure based on individual physical activity and allows for estimation of IRR instead of risk-ratios or odds-ratios that can be derived from cross-sectional studies. Two separate models were used to evaluate fall and injury incidence per person-step exposure taken during each intervening visit and follow up period. The predictor variable was walking ability status adjusting for step count as an offset. IRR and 95% confidence intervals (CI) were used to estimate the incidence of falls and injuries comparing PLL with community versus limited community-household walking ability. Assumptions for Poisson distribution were met: 1) falls and injuries were a count per unit of time, described by a Poisson distribution, 2) falls and injuries occurred independently, 3) the log of the mean rates, log(λ), were linear functions of time, and 4) there was no overdispersion—mean and variance were close for falls and injuries separately. Statistical significance was set at p < 0.05. All analyses performed using SPSS statistical software, 2017 (IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp).
3. Results
3.1. Sample
Overall, 11 participants were recruited and enrolled. One was lost to follow up, thus 10 participants aged 48.7 ± 12.5 y (33–63) had repeated assessments. Eight had available data at all time points while two missed a combined four follow up assessments due to residual limb skin injuries. The sample consisted of seven men and three women; seven TTA and three TFA. Six had peripheral artery disease (three with diabetes), two had trauma, and two had non-chronic medical amputation causes. Two used microprocessor knee prostheses. Initially, six were categorized as community walkers and four were limited community-household walkers (Table 1).
Table 1.
Baseline Participant Characteristics (identifying personal characteristics withheld).
| Participant | Amputation Etiology | Amputation Level | Prosthesis | Walking Ability Level | Houghton Score |
|---|---|---|---|---|---|
| 1 | Vascular | TT | 1C62 Triton, Otto Bock | Community | 11 |
| 2 | Medical | TT | Taleo, Otto Bock | Community | 12 |
| 3 | Medical | TF | CLeg + CWalk, Otto Bock | Limited | 8 |
| 4 | Vascular | TF | CLeg4 + 1C60 Triton, Otto Bock | Community | 10 |
| 5 | Vascular | TT | 1C62 Triton, Otto Bock | Community | 9 |
| 6 | Trauma | TT | Re-flex Rotate, Össur | Limited | 7 |
| 7 | Trauma | TF | 3R80 + 1C60 Triton, Otto Bock | Community | 12 |
| 8 | Vascular | TT | Agilex, Freedom Innovation | Limited | 8 |
| 9 | Vascular | TT | Runway, Freedom Innovation | Community | 9 |
| 10 | Vascular | TT | Agilex, Freedom Innovation | Limited | 5 |
Etiology: Medical = non-chronic medical cause, Trauma = trauma-related, Vascular = peripheral artery disease.
Amputation Level: TF = transfemoral amputation; TT = transtibial amputation.
Walking Ability: Community: community walkers (K3-K4), Limited: limited community-household walkers (K1-K2).
3.2. Main finding
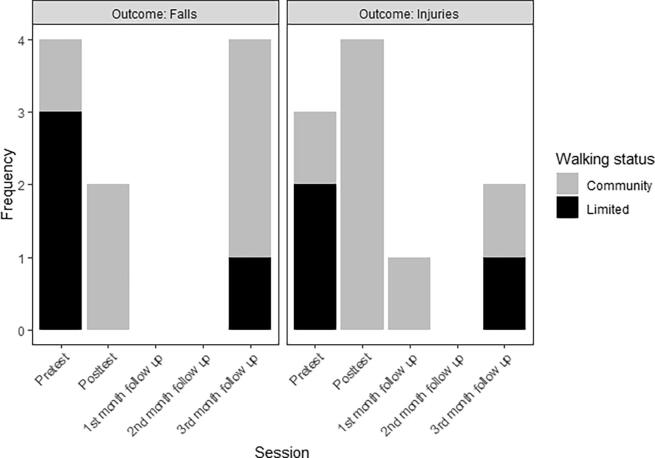
All-cause fall and injury rates were significantly different depending on community or limited community-household walking ability category. The community walking group (n = 6) had six falls and seven injuries; the limited walking group (n = 4) had four falls and three injuries. Physical activity measured by steps per day varied between groups and over time (Table 2). Per steps taken, limited walkers fell and were injured at a higher rate compared to community walkers (16.90 vs 1.99 per 1 million steps) and (12.68 vs. 2.33 per 1 million steps), respectively. When accounting for individual per person-step exposure over time in PLL, limited walking ability was associated with significantly more falls (IRR = 6.10, 95%CI = 1.12–33.33, p = 0.037) and injuries (IRR = 8.56, 95%CI = 1.73–42.40, p = 0.009) compared to community walking ability. All three PLL with TFA experienced a fall at least once and two were injured. Over the study duration, injury occurrences appeared to reduce in number (Fig. 1).
Table 2.
Average daily step count (±SD) as a measure of physical activity and risk exposure over time by walking ability level.
| Walking Ability | Pretest | Posttest | 1st month follow up | 2nd month follow up | 3rd month follow up |
|---|---|---|---|---|---|
| All | 2625 ± 1732 | 2592 ± 1376 | 2627 ± 1727 | 2535 ± 1802 | 2152 ± 1549 |
| Limited | 1875 ± 2084 | 2183 ± 1540 | 1453 ± 1527 | 479 ± 252* | 778 ± 676* |
| Community | 3054 ± 1495 | 2866 ± 1328 | 3215 ± 1612 | 3221 ± 1511 | 2610 ± 1503 |
Walking Ability: Community: community walkers (K3-K4), Limited: limited community-household walkers (K1-K2).
* Note: only 2 participants available for these measures.
Fig. 1.
Frequency of falls and injuries by assessment and walking status.
3.3. Fall and injury circumstances
Falls and injuries did not consistently occur together. Fall circumstances varied with most occurring indoors (8/10, 80%). Falls were most often due to non-specific reasons, with just two tripping incidents when the prosthetic foot caught on obstacles—a toolbox and a rug—and no slips on slick surfaces. No falls occurred when simply walking; but one fall occurred when the microprocessor knee gave way while stepping backwards. Unusual circumstances accounted for three other falls that involved carrying packages, being twisted around by a grandchild, and rushing for the bus on an unfamiliar walking route. One fall occurred due to seizure. Three falls occurred when the participant forgot they had taken off the prosthesis and fell on the residual limb. Notably, only 60% of falls resulted in injury (6/10).
Circumstances associated with injury incidence also varied and not all injuries involved falls (6/10, 60%). One injury unrelated to falls occurred when the participant scraped the residual limb getting out of a swimming pool. More commonly, non-fall injuries were related to unusual increases in walking leading to one hamstring strain and two skin injuries to the anterior distal residual limb. Injuries most often affected the residual limb (6/10, 60%); primarily the skin (9/10, 90%), with just one affecting muscle. Only one injury required more than self-care, specifically prosthetist fit and alignment adjustment after a non-fall residual limb injury that required three weeks to resolve resulting in a missed follow up assessment. Another participant with TTA reported residual limb soreness during the treatment period requiring prosthetist socket fit adjustment that did not occur in time to complete the follow up assessments. No falls or injuries occurred during physical therapy.
4. Discussion
This prospective study introduced an exposure component to all-cause fall and injury risk assessment by accounting for individual per person-step exposure assessed repeatedly over 4-months. Both fall and injury risks were found higher for PLL with limited walking ability than for PLL with community walking ability. The direct repeated-measures of individual physical activity using average daily steps utilized monthly surveillance to minimize recall bias and provide robust data that clarified the exposure adjusted risk of falling and incurring injury of any cause. PLL with limited walking ability were > 6 times more likely to fall, taking into account person-step exposure, than those with community walking ability. Not all falls led to injuries. The injury IRR when accounting for person-step exposure was in the same direction: PLL with limited walking ability were > 8 times more likely to be injured than those with community walking ability. Assessing falls per step for people with visual impairment has provided more accurate fall risk assessment than annual fall rates (Ramulu et al., 2019) and varying steps per day over time and between groups (Table 2) highlights the relevance of considering risk exposure. This study provided a more precise assessment of all-cause fall and injury risk than previously reported for PLL by controlling for varying person-steps over time with repeated-measures of individual PLL that adds a novel exposure concept to fall and injury risk analysis.
The study outcomes contribute nuanced context to paradoxical findings from retrospective studies that PLL with TTA were more likely to suffer fall-related injuries than people with TFA despite higher levels of prosthetic function (Chihuri and Wong, 2018). Retrospective research reporting annual group-level fall rates are vulnerable to recall bias particularly when memory may be impaired (Miller et al., 2001, Wong et al., 2015, Kim et al., 2019). Prospective studies benefit from more direct reporting over shorter periods that minimize recall bias. For instance, in contrast to a retrospective study of falls over 1-year (Kim et al., 2019), our results found that not all falls occurred while wearing the prosthesis. Neglecting risk exposure can also affect assessment accuracy. Simple fall or injury incidence may obscure the different exposure levels to fall opportunities between more sedentary PLL and others who walk throughout the day (Chihuri and Wong, 2018). Accounting for individual variations in physical activity using monitored daily steps in this prospective study provided per person-step exposure context that avoided potentially biased self-reported physical activity (Lamb et al., 2005) to better understand all-cause fall and injury risk among PLL. Additional larger studies of similar design are needed to understand the risks for specific amputation levels.
The 16.9 per million steps fall and injury rate for limited walkers may approximate 16.9 incidents over an average year of accumulated physical activity because one million steps correspond approximately to 2740 daily steps—comparable to the 2152–2625 average daily steps in this study (Table 2) and the 2378 for mixed functional level TTA and 2560 steps K-4 level TFA in other studies (Hordacre et al., 2014, Halsne et al., 2013). Some people with TTA may walk multiple times this daily step rate (Parker et al., 2010) thus substantially increasing their person-step exposure. Leg weakness, poor balance, and limitations in navigating home and community obstacles may explain why PLL with limited walking ability were > 6 times more likely to fall than community walkers. Controlling for risk exposure with daily per person-steps over time confirmed the intuitive finding that PLL with better walking ability were less likely to fall or incur injury than those with limited walking ability.
Not all falls caused injury; and not all injuries were caused by falls. Falls occurred both indoors and outdoors, but most falls occurred indoors consistent with research that found more falls occurred in the home than in community (Anderson et al., 2021). The results suggest that PLL are exposed to falls whether or not they access the outdoor settings that present attentional and cognitive challenges identified as risks for falls (Coffey et al., 2012). One participant attributed falling to hurrying for a bus while walking on an unfamiliar route. Two others described fall circumstances that required dual task processing (Hunter et al., 2019), such as twisting while playing with a grandchild and carrying packages while walking. Only one fall occurred due to known prosthetic limitations: microprocessor knees can protect from falls during forward walking by defaulting to a locked knee, but only later-generation algorithms account for stepping backwards. Even without falls, residual limb injuries occurred due to prosthetic fit and alignment issues or increased physical activity, consistent with past research (Highsmith et al., 2016). PLL with limited walking ability may have elevated injury risk due to chronic vascular conditions that make skin more vulnerable (Wong et al., 2020). Consistent with the finding that PLL have episodes of delayed healing and recovery (Meikle et al., 2002), two participants had minor skin injuries that depressed their walking ability for weeks after a period of improvement. While incidence of fall-related injury in PLL is high (Wong et al., 2016), the study results suggest that not all falls are consequential and that residual limb injuries occur without falls.
4.1. Strengths and limitations
This study had several limitations. First, the sample size limited individualized reporting and generalizability of the results despite statistical significance, although repeated-measures strengthened the analysis. For instance, sample size precluded separate subgroup assessment of amputation cause and level. However, the quasi-experimental design with repeated-measures over consistent time periods allowed within-participant observations with each participant acting as their own control. Treatment outcome was not a study aim, and hence was not reported, although treatment could affect fall and injury incidence. Thus, results cannot be generalized to PLL not receiving physical therapy. Second, structured interviews at prospective monthly assessments provided clarity for every fall and injury event and reduced potential recall bias, however, all retrospective reporting methods can result in memory errors. Third, some non-prosthetic steps may not have been recorded, though prosthetic step counts measured by accelerometer provide more accurate physical activity assessment than other methods. Lastly, inclusion of injuries unrelated to prosthetic use is less specific than fall-related injury. However, including all-cause injuries provides a more comprehensive picture of PLL lived experience. Future longitudinal research investigating potential impacts of physical therapy beyond initial prosthetic training to develop walking ability when PLL remain highly vulnerable to falls and injury could provide insight into potential injury prevention initiatives.
5. Conclusion
This study accounted for per person-step exposure varying over time to demonstrate that PLL with limited walking ability were at higher risk for all-cause falls and injury than PLL with community walking ability. The study results explain the observed paradox of higher functioning PLL with TTA being more likely to experience falls annually (Wong et al., 2015). The true fall and injury risk can be obscured if low physical activity and thus lower individual exposure risk is ignored. The novel inclusion of per person-step exposure over time in the analysis of fall and injury incidence clarified the risk level for PLL of different walking abilities. Considering individual activity level varying over time adds an important exposure component to fall and injury risk assessment that could be applied to other populations.
CRediT authorship contribution statement
Stanford T. Chihuri: Conceptualization, Methodology, Formal analysis, Writing – original draft, Visualization. Gregory A. Youdan Jr: Methodology, Investigation, Data curation. Christopher K. Wong: Conceptualization, Methodology, Investigation, Resources, Supervision, Funding acquisition, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgement
The authors would also like to thank Carly Adler, DPT, Kayla Moran, DPT, and Emily Vandervort, DPT, who all helped with data collection.
Disclosure Statement
This paper was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1TR001873. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Stanford T. Chihuri, Email: stc2126@cumc.columbia.edu.
Christopher K. Wong, Email: ckw7@cumc.columbia.edu.
References
- Anderson C.B., Miller M.J., Murray A.M., et al. Falls after dysvascular transtibial amputation: a secondary analysis of falling characteristics and reduced phys8ical performance. PM&R. 2021;13:19–29. doi: 10.1002/pmrj.12376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blome C., Augustin M. Measuring change in quality of life: bias in prospective and retrospective evaluation. Value Health. 2015;18(1):110–115. doi: 10.1016/j.jval.2014.10.007. [DOI] [PubMed] [Google Scholar]
- Chen L.H., Warner M., Fingerhut L., et al. Injury episodes and circumstances: national health interview survey, 1997-2007. National Center for Health Statistics. Vital. Health Stat. 2009;10(241) [PubMed] [Google Scholar]
- Chihuri S.T., Wong C.K. Factors associated with the likelihood of fall-related injury among people with lower limb loss. Injury Epi. 2018;5(1):42. doi: 10.1186/s40621-018-0171-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey L., O’Keeffe F., Gallagher P., Desmond D., Lombard-Vance R. Cognitive functioning in persons with lower limb amputations: a review. Disabil. Rehabil. 2012;34(23):1950–1964. doi: 10.3109/09638288.2012.667190. [DOI] [PubMed] [Google Scholar]
- Dite W., Connor H.J., Curtis H.C. Clinical identification of multiple fall risk early after unilateral transtibial amputation. Arch. Phys. Med. Rehabil. 2007;88(1):109–114. doi: 10.1016/j.apmr.2006.10.015. [DOI] [PubMed] [Google Scholar]
- Halsne E.G., Waddingham M.G., Hafner B.J. Long-term activity in and among persons with transfemoral amputation. J. Rehabil. Res. Dev. 2013;50(4):515–530. doi: 10.1682/jrrd.2012.04.0066. [DOI] [PubMed] [Google Scholar]
- Highsmith M.J., Kahle J.T., Klenow T.D., Andrews C.R., Lewis K.L., Bradley R.C., Ward J.M., Orriola J.J., Highsmith J.T. Interventions to manage residual limb ulceration due to prosthetic use in individuals with lower extremity amputation: a systematic review of the literature. Technol. Innov. 2016;18(2):115–123. doi: 10.21300/18.2-3.2016.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hordacre B., Barr C., Crotty M. Use of an activity monitor and GPS device to assess community activity and participation in transtibial amputees. Sensors. 2014;14(4):5845–5859. doi: 10.3390/s140405845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houghton A.D., Taylor P.R., Thurlow S., et al. Success rates for rehabilitation of vascular amputees: implications for preoperative assessment and amputation level. Br. J. Surg. 1992;79:753–755. doi: 10.1002/bjs.1800790811. [DOI] [PubMed] [Google Scholar]
- Hunter S.W., Batchelor F., Hill K.D., Hill A.-M., Mackintosh S., Payne M. Risk factors for falls in people with a lower limb amputation: a systematic review. PM R. 2017;9(2):170–180.e1. doi: 10.1016/j.pmrj.2016.07.531. [DOI] [PubMed] [Google Scholar]
- Hunter S.W., Bobos P., Frengopoulos C., Macpherson A., Viana R., Payne M.W. Cognition predicts mobility change in lower extremity amputees between discharge from rehabilitation and 4-month follow-up: a prospective cohort study. Arch. Phys. Med. Rehabil. 2019;100(11):2129–2135. doi: 10.1016/j.apmr.2019.05.030. [DOI] [PubMed] [Google Scholar]
- Kim J., Major M.J., Hafner B., Sawers A. Frequency and circumstances of falls reported by ambulatory unilateral lower limb prostheses users: a secondary analysis. PM&R. 2019;11(4):344–353. doi: 10.1016/j.pmrj.2018.08.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb S.E., Jorstad-Stein E.C., Hauer K., et al. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe Consensus. J. Am. Geri. Soc. 2005;53(9):1618–1622. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- Meikle B., Devlin M., Garfinkel S. Interruptions to amputee rehabilitation. Arch. Phys. Med. Rehabil. 2002;83(9):1222–1228. doi: 10.1053/apmr.2002.33657. [DOI] [PubMed] [Google Scholar]
- Miller W.C., Deathe A.B., Speechley M. Lower extremity prosthetic mobility: a comparison of 3 self-report scale. Arch. Phys. Med. Rehabil. 2001;82:1432–1440. doi: 10.1053/apmr.2001.25987. [DOI] [PubMed] [Google Scholar]
- Miller W., Speechley M., Deathe B. The prevalence of risk factors of falling and fear of falling among lower extremity amputees. Arch. Phys. Med. Rehabil. 2001;82:1031–1037. doi: 10.1053/apmr.2001.24295. [DOI] [PubMed] [Google Scholar]
- Morrison C.N., Rundle A.G., Branas C.C., Chihuri S., Mehranbod C., Li G. The unknown denominator problem in population studies of disease frequency. Spatial Spatio-temporal Epidemiol. 2020;35:100361. doi: 10.1016/j.sste.2020.100361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolan L., Wit A., Dudziñski K., Lees A., Lake M., Wychowañski M. Adjustments in gait symmetry with walking speed in trans-femoral and trans-tibial amputees. Gait Posture. 2003;17(2):142–151. doi: 10.1016/s0966-6362(02)00066-8. [DOI] [PubMed] [Google Scholar]
- Parker K., Kirby R.L., Adderson J., Thompson K. Ambulation of people with lower-limb amputations: relationship between capacity and performance measures. Arch. Phys. Med. Rehabil. 2010;91(4):543–549. doi: 10.1016/j.apmr.2009.12.009. [DOI] [PubMed] [Google Scholar]
- Perkins Z.B., De’Ath H.D., Sharp G., et al. Factors affecting outcome after traumatic limb amputation. Br. J. Surg. 2012;99(suppl 1):75–86. doi: 10.1002/bjs.7766. [DOI] [PubMed] [Google Scholar]
- Ramulu P.Y., Mihailovic A., West S.K., Friedman D.S., Gitlin L.N. What is a falls risk factor? Factors associated with falls per time or per step in individuals with glaucoma. J. Am. Geriatr. Soc. 2019;67(1):87–92. doi: 10.1111/jgs.15609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roepke A.M., Williams R.M., Turner A.P., et al. A longitudinal study of social participation after dysvascular lower extremity amputation. Am. J. Phys. Med. Rehabil. 2017;96:741–747. doi: 10.1097/PHM.0000000000000745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens J.A., Mahoney J.E., Ehrenreich H. Circumstances and outcomes of falls among high risk community-dwelling older adults. Injury Epi. 2014;1:5. doi: 10.1186/2197-1714-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stovitz S.D., Shrier I. Injury rates in team sport events: tackling challenges in assessing exposure time. Br. J. Sports Med. 2012;46(14):960–963. doi: 10.1136/bjsports-2011-090693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster J.B., Hakimi K.N., Williams R.M., Turner A.P., Norvell D.C., Czerniecki J.M. Prosthetic fitting, use, and satisfaction following lower-limb amputation: a prospective study. J. Rehabil. Res. Dev. 2012;49(10):1493. doi: 10.1682/JRRD.2012.01.0001. [DOI] [PubMed] [Google Scholar]
- Wong C.K., Chen C., Welsh J. Preliminary assessment of balance with the Berg Balance Scale in adults who have a leg amputation and dwell in the community: Rasch rating scale analysis. Phys. Ther. 2013;93:1520–1529. doi: 10.2522/ptj.20130009. [DOI] [PubMed] [Google Scholar]
- Wong C., Chen C., Blackwell W., Rahal R., Benoy S. Balance ability measured with the Berg Balance Scale: a determinant of fall history in community-dwelling adults with leg amputation. J. Rehabil. Med. 2015;47(1):80–86. doi: 10.2340/16501977-1882. [DOI] [PubMed] [Google Scholar]
- Wong C.K., Chihuri S., Li G. The risk of fall-related injury in community-dwelling people with lower limb amputation: a prospective cohort study. J. Rehabil. Med. 2016;48:80–85. doi: 10.2340/16501977-2042. [DOI] [PubMed] [Google Scholar]
- Wong C.K., Chihuri S.T. Impact of vascular disease, amputation level, and the mismatch between balance ability and balance confidence in a cross-sectional study of the likelihood of falls among people with limb loss: perception versus reality. Am. J. Phys. Med. Rehabil. 2019;98(2):130–135. doi: 10.1097/PHM.0000000000001034. [DOI] [PubMed] [Google Scholar]
- Wong C.K., Varca M.J., Stevenson C.E., et al. The impact of a 4-session physical therapy program emphasizing manual therapy and exercise on the balance and prosthetic walking ability of people with lower limb amputation: a pilot study. J. Prosthet. Orthot. 2016;28(3):95–100. [Google Scholar]
- Wong C.K., Gibbs W., Chen E.S. Use of the Houghton Scale to classify community and household walking ability in people with lower limb amputation: Criterion-related validity. Arch. Phys. Med. Rehabil. 2016;97(7):1130–1136. doi: 10.1016/j.apmr.2016.01.022. [DOI] [PubMed] [Google Scholar]
- Wong C.K., Chihuri S.T., Santo E., et al. Relevance of medical comorbidities for functional mobility in people with lower limb loss: retrospective explanatory models for a clinical walking measure and a patient-reported functional outcome. Physiotheraphy. 2020;107:133–141. doi: 10.1016/j.physio.2020.01.002. [DOI] [PubMed] [Google Scholar]
- Ziegler-Graham K., MacKenzie E.J., Ephraim P.L., Travison T.G., Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch. Phys. Med. Rehabil. 2008;89(3):422–429. doi: 10.1016/j.apmr.2007.11.005. [DOI] [PubMed] [Google Scholar]