Abstract
Given the racial disparities in cervical cancer screening, incidence, and mortality, the purpose of this study was to estimate cervical cancer screening behaviors through self-reported Pap testing among racial groups in the U.S. This cross-sectional study utilized the Behavioral Risk Factor Surveillance System (BRFSS) data to compare Pap testing behaviors among women of different racial groups. The BRFSS data from 2014, 2016, and 2018 were chosen because these were the most recent years of data capturing cervical cancer screening information. The primary outcome was self-reported Pap testing behavior (yes/no). Racial groups were analyzed with the original categorical responses for the race/ethnicity variable to investigate Pap testing behaviors across all racial groups. Statistical analyses included descriptive statistics and a multivariable binomial logistic regression model to assess differences of Pap testing by race after adjusting for covariates. Among the 538,218 females included, 88.81% (95% CI: 88.60–89.03) reported receiving a Pap test. Pap testing behaviors differed significantly between racial groups in 2014, 2016, and 2018 (p < 0.001 for all years). Compared to White women, Asians (OR: 0.169, 95% CI: 0.149–0.191), Native Hawaiians/other Pacific Islanders (OR: 0.339, 95% CI: 0.249–0.462), American Indians or Alaskan Natives (OR: 0.664, 95% CI: 0.532–0.829), Hispanics (OR: 0.726, 95% CI: 0.670–0.786), and other non-Hispanic races (OR: 0.439, 95% CI: 0.323–0.598) were significantly less likely to receive Pap test. Racial disparities in cervical cancer screening with Pap tests exist for Asians, Native Hawaiians/other Pacific Islanders, American Indians or Alaskan Natives, Hispanics, and other non-Hispanics.
Keywords: Cervical cancer screening, Pap test, Racial disparities, Health disparities, Women’s health
1. Introduction
With the introduction of the Pap test, cervical cancer in the U.S. has decreased by over 70% since the 1950′s (Safaeian et al., 2007); however, racial disparities in cervical cancer still persist in the U.S. Cervical cancer incidence is higher among females of Black or Hispanic race (8.3 and 9.3 per 100,000 females, respectively) compared to White race (7.4 per 100,000 females) (U.S. Cancer Statistics Working Group). Certain racial groups also exhibit less frequent preventive screening practices and disproportionate mortality rates (Hall et al., 2018, Lowe, 2017).
To improve preventive care for women’s health, Healthy People 2030 aims to increase cervical cancer screening (Healthy People 2030). Estimates from the 2018 National Health Interview Survey (NHIS) revealed that the overall cervical cancer screening rate reached 80.5% in the U.S., but women’s cervical cancer screening rates have recently demonstrated a problematic decrease across years (Healthy People 2030). Additionally, considering the overall cervical cancer screening rate alone could potentially mask lower testing rates among subgroups within this population.
The disparate rates of cervical cancer incidence are particularly alarming because medically underserved and underscreened populations account for more than 60% of diagnoses, with socioeconomic status and race/ethnicity being influential factors (Scarinci et al., 2010). Therefore, these populations at risk of experiencing cervical cancer disparities because of low preventive screening must be identified. Identifying at risk populations can inform delivery of strategies to mitigate these disparities, such as community-based interventions that have been shown to increase preventive screening for cervical cancer among diverse populations (Lowe, 2017, Scarinci et al., 2010). Our study aims to estimate cervical cancer screening behaviors through self-reported Pap testing among racial groups in the U.S. in 2014, 2016, and 2018. We hypothesized that racial disparities exist in Pap testing behaviors based on the racial and ethnic groups persons identified with.
2. Materials and methods
2.1. Population
Using 2014, 2016, and 2018 Behavioral Risk Factor Surveillance System (BRFSS) data ([dataset]), this cross-sectional study compared Pap testing behaviors among women of different racial groups. The BRFSS data is administered by the Centers for Disease Control and Prevention and captures cervical cancer screening information in even-numbered years among a nationally representative sample (BRFSS, 2013). The American Cancer Society (ACS) guidelines for cervical cancer screening recommend Pap tests for women aged 21–65 (Fontham et al., 2020); however, our study population included ages 18–69 due to the five-year age categories within the BRFSS data.
2.2. Measures
The primary outcome was cervical cancer screening behavior, operationalized as a self-reported receipt of Pap test (yes/no). To assess self-reported receipt of Pap test, we used the following question asked in even-numbered years of BRFSS data: “Have you ever had a Pap test?” (BRFSS, 2018) We only included participants with a valid yes or no response to this question in the study population. The key independent variable was self-reported race/ethnicity, which was assessed through the “computed race-ethnicity grouping” variable in BRFSS data, and the original categorical responses for this variable were retained in analyses to investigate Pap testing behaviors across all racial/ethnic groups.
2.3. Covariates
The geographical regions of South, Northeast, Midwest, West, and U.S. Territories were based on the person’s state of residence following the U.S. Census Regions and Divisions with State FIPS code (United States Census Bureau). Metropolitan status is calculated based on the metropolitan statistical area (MSA), but this variable is only populated for respondents not answering via cell phone or those not living in U.S. Territories (BRFSS, 2018). The variable for year corresponds to the BRFSS data year (i.e., 2014, 2016, 2018). Remaining covariates were obtained from self-reported answers to BRFSS questionnaires.
2.4. Statistical analysis
We followed analysis procedures outlined by BRFSS by applying weight, cluster, and strata variables to obtain nationally representative population-based estimates and odds ratios representing the general population of U.S. women (BRFSS, 2019b). Descriptive statistics were produced for characteristics of the female study population. Population-based estimates with 95% confidence intervals (95% CI) were produced for Pap testing behaviors for the overall study population combined across years. We performed Rao-Scott chi-square tests separately for each year of data to investigate differences in Pap testing by race/ethnicity. To evaluate the trends of Pap testing across years, we compared the percentages of self-reported Pap testing from 2014, 2016, and 2018 using simple linear regression. A simple binomial logistic regression model produced unadjusted odds ratios (OR) for Pap testing by race/ethnicity.
A multivariable binomial logistic regression model was used to assess differences of Pap testing by race/ethnicity after adjusting for covariates, where adjusted odds ratios (aOR) and 95% CI were estimated. Variables included in the model sought to capture population and environmental characteristics, which collectively influence persons’ health behaviors as outlined in the Andersen Behavioral Model (Andersen, 1995). The modal category for each variable was chosen as the reference group, except for age, MSA, and year. For age, 60–64 was chosen as the reference given that this was the second most populated category behind 65–69, but utilizing 65–69 as the reference would have inadvertently included many females outside of the ACS’s recommended screening age. The ‘Not in an MSA’ category was chosen as the reference for MSA, and the earliest year of data (i.e., 2014) was chosen as the reference for year. Analyses were completed using SAS, version 9.4 (SAS Institute, Cary, NC) with a priori levels of significance at 0.05 and two-sided hypothesis testing. This study was approved as exempt by the primary author’s Institutional Review Board, and analyses were completed from 2020 to 2021.
3. Results
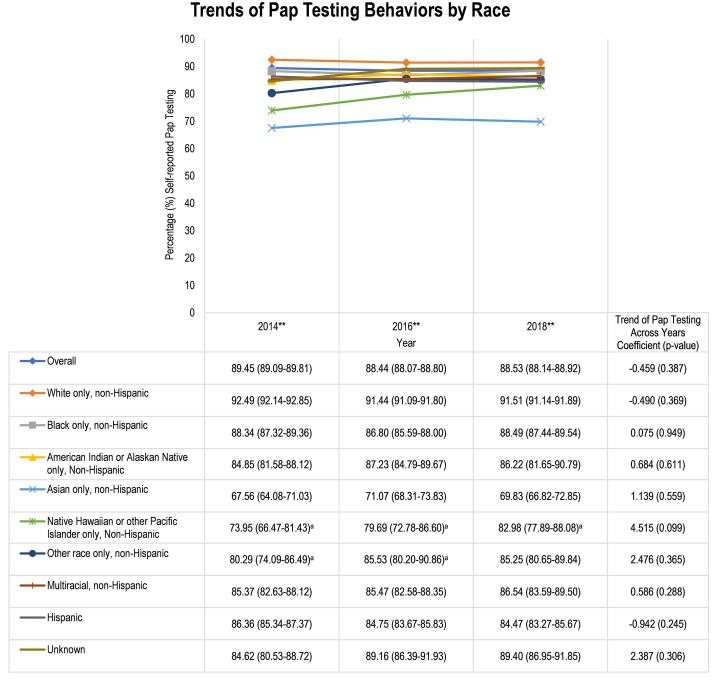
Across 2014, 2016, and 2018, a total of 538,218 females were captured in the study population. The majority self-identified as White and non-Hispanic, lived in the South, and were married and employed (Table 1). For cervical cancer screening behaviors, 88.81% (95% CI: 88.60–89.03) of females reported receiving a Pap test, and 81.06% (95% CI: 80.85–81.27) screened within the past 1–3 years. In unadjusted analyses, Pap testing behaviors differed significantly between racial groups each year (Fig. 1, p < 0.001 for all years). In 2014, 2016, and 2018, Whites reported the highest rates of Pap testing (range: 91.44%-92.49%), and Asians (range: 67.56%-71.07%) and Native Hawaiians/other Pacific Islanders (range: 73.95%–82.98%) consistently screened the lowest. Native Hawaiians/other Pacific Islanders demonstrated the largest increase in testing rates from 73.95% (95% CI: 66.47–81.43) in 2014 to 82.98% (95% CI: 77.89–88.08) in 2018. The trend across years for self-reported Pap testing did not significantly change in the overall population or within any racial/ethnic subgroup.
Table 1.
Characteristics of Female Study Population and Regression Model of Pap Testing Behaviors.a
| Characteristics | Female Study Population Weighted Freq. (95% CI) N = 538,218 | Rates of Pap Testing Weighted Freq. (95% CI) N = 538,218 | Pap Testingb, cAdjusted Odds Ratio (95% CI) N = 538,218 |
|---|---|---|---|
| Race | |||
| White only, non-Hispanic | 60.93 (60.65–61.20) | 91.83 (91.62–92.04) | Ref |
| Black only, non-Hispanic | 12.64 (12.45–12.83) | 87.85 (87.21–88.48) | 0.957 (0.884–1.037) |
| American Indian or Alaskan Native only | 0.98 (0.94–1.02) | 86.07 (84.09–88.05) | 0.664 (0.532–0.829) |
| Asian only, non-Hispanic | 5.05 (4.87–5.24) | 69.55 (67.77–71.33) | 0.169 (0.149–0.191) |
| Native Hawaiian, Pacific Islander only | 0.22 (0.20–0.24) | 78.70 (74.80–82.59) | 0.339 (0.249–0.462) |
| Other race only, non-Hispanic | 0.35 (0.33–0.38) | 83.69 (80.56–86.82) | 0.439 (0.323–0.598) |
| Multiracial, non-Hispanic | 1.42 (1.36–1.47) | 85.75 (84.10–87.41) | 0.942 (0.811–1.095) |
| Hispanic | 17.14 (16.90–17.38) | 85.18 (84.55–85.82) | 0.726 (0.670–0.786) |
| Unknown | 1.27 (1.21–1.33) | 87.83 (85.99–89.66) | 0.683 (0.555–0.841) |
| Region | |||
| South | 37.65 (37.47–37.83) | 89.47 (89.12–89.83) | Ref |
| Northeast | 17.52 (17.38–17.65) | 87.68 (87.16–88.20) | 0.836 (0.777–0.899) |
| Midwest | 21.20 (21.07–21.32) | 89.67 (89.30–90.05) | 0.975 (0.915–1.040) |
| West | 22.36 (22.20–22.52) | 87.79 (87.29–88.30) | 0.963 (0.893–1.038) |
| U.S. territories | 1.27 (1.25–1.29) | 88.32 (87.35–89.28) | 0.923 (0.802–1.062) |
| Age | |||
| 18–24 | 14.22 (13.98–14.45) | 48.29 (47.38–49.20) | 0.080 (0.070–0.091) |
| 25–29 | 9.03 (8.87–9.20) | 89.30 (88.64–89.97) | 0.429 (0.371–0.495) |
| 30–34 | 10.66 (10.47–10.84) | 94.29 (93.79–94.78) | 0.659 (0.566–0.768) |
| 35–39 | 9.03 (8.87–9.18) | 95.99 (95.60–96.39) | 0.895 (0.765–1.047) |
| 40–44 | 9.73 (9.56–9.90) | 96.17 (95.74–96.60) | 0.864 (0.735–1.015) |
| 45–49 | 8.59 (8.45–8.74) | 96.69 (96.29–97.09) | 0.999 (0.844–1.182) |
| 50–54 | 10.88 (10.72–11.05) | 96.75 (96.42–97.07) | 0.964 (0.830–1.119) |
| 55–59 | 9.78 (9.64–9.93) | 96.94 (96.64–97.24) | 1.019 (0.881–1.180) |
| 60–64 | 10.11 (9.97–10.26) | 96.99 (96.71–97.27) | Ref |
| 65–69 | 7.97 (7.85–8.08) | 96.43 (96.10–96.76) | 0.754 (0.651–0.873) |
| Marital status | |||
| Married | 50.82 (50.54–51.10) | 96.33 (96.16–96.50) | Ref |
| Divorced | 11.60 (11.44–11.76) | 96.34 (95.97–96.72) | 0.864 (0.764–0.977) |
| Widowed | 4.14 (4.05–4.23) | 95.38 (94.82–95.95) | 0.679 (0.583–0.790) |
| Separated | 3.12 (3.02–3.21) | 92.38 (91.47–93.30) | 0.681 (0.585–0.792) |
| Never married | 24.72 (24.46–24.98) | 68.58 (67.95–69.21) | 0.382 (0.355–0.411) |
| Member of unmarried couple | 5.17 (5.04–5.31) | 87.85 (86.92–88.78) | 0.828 (0.737–0.929) |
| Unknown | 0.43 (0.39–0.47) | 82.82 (78.35–87.30) | 0.543 (0.361–0.819) |
| Education | |||
| Never attended school/only kindergarten | 0.24 (0.20–0.27) | 87.40 (82.78–92.02) | 0.251 (0.158–0.400) |
| Elementary | 3.95 (3.81–4.08) | 89.04 (87.86–90.22) | 0.312 (0.266–0.366) |
| Some high school | 8.17 (7.99–8.36) | 84.45 (83.46–85.44) | 0.382 (0.340–0.428) |
| High school graduate | 25.21 (24.97–25.45) | 84.45 (83.97–84.94) | 0.440 (0.409–0.475) |
| Some college or technical school | 33.14 (32.87–33.40) | 87.97 (87.58–88.36) | 0.704 (0.654–0.758) |
| College graduate | 29.12 (28.90–29.35) | 94.79 (94.57–95.01) | Ref |
| Unknown | 0.17 (0.15–0.19) | 82.51 (77.94–87.08) | 0.366 (0.238–0.563) |
| Metropolitan status | |||
| In the center city of an MSA | 12.73 (12.58–12.88) | 92.53 (92.02–93.03) | 1.010 (0.873–1.168) |
| Outside the center city of an MSA but inside the county | 8.50 (8.36–8.63) | 92.84 (92.12–93.55) | 0.956 (0.812–1.126) |
| Inside a suburban county of the MSA | 5.98 (5.88–6.08) | 94.25 (93.64–94.86) | 1.165 (0.980–1.386) |
| Not in an MSA | 6.43 (6.34–6.52) | 93.68 (93.06–94.30) | Ref |
| Unknown | 66.36 (66.19–66.53) | 86.62 (86.34–86.90) | 1.093 (0.954–1.252) |
| Employment | |||
| Employed for wages | 49.86 (49.58–50.14) | 91.62 (91.36–91.88) | Ref |
| Self-employed | 6.88 (6.74–7.02) | 93.72 (93.11–94.32) | 0.946 (0.841–1.065) |
| Out of work for ≥ 1 year | 3.16 (3.05–3.26) | 88.00 (86.80–89.20) | 0.961 (0.832–1.110) |
| Out of work for < 1 year | 3.07 (2.97–3.17) | 84.14 (82.81–85.46) | 1.004 (0.885–1.139) |
| A homemaker | 12.19 (12.00–12.39) | 94.57 (94.14–95.00) | 1.252 (1.123–1.395) |
| A student | 7.21 (7.03–7.39) | 43.56 (42.29–44.84) | 0.367 (0.340–0.395) |
| Retired | 8.77 (8.64–8.89) | 97.22 (96.98–97.45) | 1.156 (1.009–1.325) |
| Unable to work | 8.27 (8.13–8.41) | 92.63 (92.10–93.16) | 0.826 (0.729–0.936) |
| Unknown | 0.59 (0.54–0.65) | 78.61 (75.05–82.17) | 0.627 (0.493–0.797) |
| Income | |||
| <$10,000 | 6.15 (6.01–6.28) | 82.54 (81.54–83.54) | 0.833 (0.738–0.941) |
| $10,000-$14,999 | 4.91 (4.78–5.03) | 88.22 (87.18–89.25) | 1.017 (0.878–1.179) |
| $15,000-$19,999 | 6.91 (6.77–7.05) | 87.30 (86.48–88.12) | 0.978 (0.871–1.098) |
| $20,000-$24,999 | 7.91 (7.76–8.07) | 87.67 (86.87–88.47) | 0.929 (0.830–1.040) |
| $25,000-$34,999 | 8.55 (8.39–8.70) | 88.42 (87.70–89.15) | 0.849 (0.763–0.945) |
| $35,000-$49,999 | 10.87 (10.70–11.04) | 91.17 (90.58–91.75) | 0.978 (0.878–1.089) |
| $50,000-$74,999 | 12.52 (12.34–12.69) | 92.57 (92.05–93.09) | 0.902 (0.817–0.995) |
| ≥$75,000 | 27.80 (27.56–28.05) | 93.76 (93.43–94.09) | Ref |
| Unknown | 14.39 (14.18–14.59) | 78.67 (77.96–79.38) | 0.637 (0.583–0.698) |
| Health insurance | |||
| Yes | 87.19 (86.99–87.40) | 89.88 (89.67–90.10) | Ref |
| No | 12.38 (12.18–12.59) | 82.47 (81.70–83.24) | 0.622 (0.578–0.671) |
| Unknown | 0.42 (0.38–0.47) | 53.53 (48.46–58.60)d | 0.343 (0.256–0.460) |
| Veteran status | |||
| Yes | 2.26 (2.18–2.34) | 94.25 (93.18–95.31) | 1.542 (1.236–1.924) |
| No | 97.70 (97.62–97.78) | 88.69 (88.47–88.91) | Ref |
| Unknown | 0.04 (0.03–0.05) | 85.60 (77.32–93.89)d | 1.121 (0.469–2.677) |
| General health status | |||
| Excellent | 18.96 (18.75–19.18) | 87.88 (87.37–88.38) | 0.979 (0.910–1.052) |
| Very good | 32.40 (32.14–32.65) | 88.52 (88.13–88.90) | Ref |
| Good | 30.70 (30.44–30.96) | 88.12 (87.72–88.53) | 1.028 (0.962–1.098) |
| Fair | 13.22 (13.03–13.41) | 91.44 (90.94–91.93) | 1.213 (1.107–1.329) |
| Poor | 4.47 (4.36–4.59) | 92.03 (91.33–92.73) | 0.893 (0.775–1.028) |
| Unknown | 0.25 (0.22–0.28) | 86.40 (82.04–90.77) | 0.682 (0.436–1.068) |
| Difficulty visiting doctor's office alone | |||
| Yes | 7.50 (7.36–7.63) | 90.42 (89.77–91.07) | 0.939 (0.846–1.041) |
| No | 92.31 (92.17–92.44) | 88.69 (88.46–88.91) | Ref |
| Unknown | 0.20 (0.17–0.22) | 85.67 (81.15–90.20) | 0.613 (0.384–0.980) |
| Year | |||
| 2014 | 34.35 (34.11–34.60) | 89.45 (89.09–89.81) | Ref |
| 2016 | 35.31 (35.05–35.56) | 88.44 (88.07–88.80) | 0.828 (0.778–0.881) |
| 2018 | 30.34 (30.11–30.57) | 88.53 (88.14–88.92) | 0.828 (0.774–0.886) |
Abbreviations: BRFSS = Behavioral Risk Factor Surveillance System; MSA = Metropolitan statistical area; VA = Veterans Affairs. Unknown indicates responses “don’t know/Not sure/Refused” or “not asked/missing.”
Outcome variable = Self-report of Pap test [yes vs. no (ref.)].
Boldface indicates statistical significance (p < 0.05)
Use caution when interpreting estimate due to 95% confidence interval being wider than 10; this is recommended by the BRFSS (BRFSS, 2019a).
Fig. 1.
Trends of Pap Testing Behaviors by Race. Columns represent the weighted percentages (95% confidence intervals) for females who self-reported screening for cervical cancer with Pap test; age parameters follow the American Cancer Society's 2012–2019 guidelines for cervical cancer screening. Female sample size per year: 2014 = 187,300; 2016 = 188,564; 2018 = 162,354. Unknown race indicates responses “don’t know/Not sure/Refused” or “not asked/missing.” Trends of Pap testing across years were evaluated by comparing the percentages of self-reported Pap testing from 2014, 2016, and 2018 using simple linear regression. **Chi-square detected significant difference in Pap testing behaviors across groups (2014: p < 0.001; 2016: p < 0.001; 2018: p < 0.001). aUse caution when interpreting estimate due to 95% confidence interval being wider than 10; this is recommended by the BRFSS (BRFSS, 2019a).
There were significant differences in Pap testing behaviors by racial/ethnic groups. Without adjusting for covariates, all racial/ethnic groups had significantly lower odds of screening compared to White females, including females identifying as Black (OR: 0.643, 95% CI: 0.602–0.687), American Indian or Alaskan Native (OR: 0.550, 95% CI: 0.465–0.650), Asian (OR: 0.203, 95% CI: 0.186–0.222), Native Hawaiian/other Pacific Islander (OR: 0.329, 95% CI: 0.260–0.415), other non-Hispanic race (OR: 0.456, 95% CI: 0.362–0.575), multiracial (OR: 0.535, 95% CI: 0.466–0.615), Hispanic (OR: 0.511, 95% CI: 0.483–0.542), and unknown race (OR: 0.642, 95% CI: 0.539–0.763).
After adjusting for covariates, the following racial groups were significantly less likely to screen with Pap test compared to White women: Asians were 83% less likely (aOR: 0.169, 95% CI: 0.149–0.191); Native Hawaiians/other Pacific Islanders were 66% less likely (aOR: 0.339, 95% CI: 0.249–0.462); American Indians or Alaskan Natives were 34% less likely (aOR: 0.664, 95% CI: 0.532–0.829); Hispanics were 27% less likely (aOR: 0.726, 95% CI: 0.670–0.786); and other non-Hispanic races were 56% less likely (aOR: 0.439, 95% CI: 0.323–0.598). No significant screening differences were found between Whites compared to Blacks (aOR: 0.957, 95% CI: 0.884–1.037) or multiracial groups (aOR: 0.942, 95% CI: 0.811–1.095).
In addition to screening differences between racial/ethnic groups, other characteristics were also found to be significantly associated with women’s likelihood to screen with Pap test (Table 1). Women were significantly less likely to screen with Pap test if they were younger (18–34 years old), had lower educational status (less than college graduate), were not married, or did not have health insurance.
4. Discussion
The overall screening rate with the Pap test remains high at nearly 89%. However, racial disparities in cervical cancer screening with Pap tests exist and persist across years for Asian, Native Hawaiian/other Pacific Islander, American Indian or Alaskan Native, Hispanic, and other non-Hispanic racial groups when compared to Whites. However, Pap testing behaviors are similar for White, Black, and multiracial groups. While Black and White females have similar screening rates, cervical cancer incidence and mortality remain higher among non-Hispanic Black females than non-Hispanic White females (Yoo et al., 2017). Native Hawaiian/other Pacific Islanders and Asians consistently screened below other racial groups each year, so these underscreened females remain at risk of undetected cervical cancer.
Our findings for the national population-based estimates of cervical cancer screening practices add timely scientific knowledge to the prior literature about differences in Pap testing by race/ethnicity. A study utilizing the NHIS found similar Pap testing rates for White and Black racial groups and identified lower testing among non-Hispanic Asians (Hall et al., 2018). In contrast, a study of the Health Information National Trends Survey 5 documented lower cervical cancer screening among Hispanic and White females compared to Black females, and the positive influence of maintaining healthcare checkups differed by race (Orji and Yamashita, 2021). Our findings build upon these prior works to document additional minority racial/ethnic groups experiencing disparities in Pap testing through more recent years along with outlining additional characteristics that influence Pap testing behaviors. Further, the novelty of our findings lies in the more detailed categorization of racial/ethnic groups and tracking of racial disparity trends for Pap testing across recent years.
Prior literature supports our findings of associations between Pap testing behaviors with women’s characteristics, outside of race/ethnicity. The previously mentioned NHIS study found lower Pap testing among younger women (21–30 years old) with lower educational status and without health insurance (Hall et al., 2018). Another study utilizing the Health Information National Trends Survey to investigate racial and ethnic differences in Pap testing found lower testing among non-married women without health insurance, but this study only included women of White, Black, or Hispanic races/ethnicities (Hirth et al., 2016). In contrast, our work provides a comprehensive investigation of Pap testing behaviors inclusive of all racial/ethnic groups. Findings contribute detailed scientific information about cervical cancer screening behaviors via Pap testing across all racial/ethnic groups captured in the BRFSS.
Based on the persistent racial disparities in Pap testing identified in this study, it is critical to consider the potential drivers of these disparities. In addition to race/ethnicity, this study among a nationally representative sample of females in the U.S. found the likelihood of Pap testing to be associated with geographic location, age, education status, income status, employment, health insurance coverage, veteran status, and general health status. Therefore, the potential drivers of these disparities could be best conceptualized as social determinants of health (SDOH). In recognizing the importance of SDOH in cancer screening disparities, a recent systematic review highlighted the utility of interventions based on SDOH to promote preventive cancer screening (Mohan and Chattopadhyay, 2020). Systemic racism also likely contributes to the lower cervical cancer screening practices of different racial/ethnic groups, where increasing trust with healthcare providers and implementing person-centered care are critical steps to increase cervical cancer screening uptake (Fuzzell et al., 2021).
Recently, in 2020, the ACS recognized the primary HPV test as the preferred method of cervical cancer screening while recognizing the traditionally recommended Pap test as an acceptable method when the HPV test is unavailable (Fontham et al., 2020). With this guideline change and the alarming racial disparities for Pap testing, special attention should be given to different racial groups to promote health equity in cervical cancer screening and subsequent cervical cancer incidence and survival outcomes as the implementation of the HPV test continues to progress.
4.1. Study limitations and strengths
The cross-sectional nature of this study is a limitation because we were not able to track women’s cervical cancer screening behaviors across time. Even with this limitation, the strengths of this study include the ability of findings to highlight racial disparity trends in cervical cancer screening behaviors across multiple years and the high generalizability to female populations across the entire U.S. Because the data are from the U.S. population, findings may not be generalizable to international settings.
5. Conclusions
Women who self-identify their race/ethnicity as Asian, Native Hawaiian/other Pacific Islander, American Indian or Alaskan Native, Hispanic, and other non-Hispanic may be less likely to screen for cervical cancer with the Pap test.
CRediT authorship contribution statement
Cassidi C. McDaniel: Conceptualization, Methodology, Software, Formal analysis, Investigation, Visualization, Writing – original draft, Writing – review & editing. Hayleigh H. Hallam: Conceptualization, Methodology, Software, Investigation, Writing – original draft. Tiffany Cadwallader: Conceptualization, Methodology, Software, Investigation, Writing – original draft. Hee Yun Lee: Conceptualization, Investigation, Writing – review & editing, Supervision. Chiahung Chou: Conceptualization, Methodology, Formal analysis, Investigation, Visualization, Writing – review & editing, Supervision, Project administration.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: McDaniel was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number TL1TR003106. The content is solely the authors' responsibility and does not necessarily represent the official views of the National Institutes of Health. McDaniel was also supported by the American Foundation for Pharmaceutical Education (AFPE) under the AFPE Pre-Doctoral Fellowship. These sponsors had no role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication. Hallam, Cadwallader, Lee, and Chou have no relevant conflicts of interest to disclose.
Acknowledgments
Acknowledgments
Data statement: Data from the Behavioral Risk Factor Surveillance System (BRFSS) is publicly available for download from the Centers for Disease Control and Prevention (CDC).
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- [dataset], Behavioral Risk Factor Surveillance System: Annual Survey Data, 2014, 2016, and 2018. CDC, Atlanta, GA.
- Andersen Ronald M. Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? J. Health Soc. Behav. 1995;36(1):1. doi: 10.2307/2137284. [DOI] [PubMed] [Google Scholar]
- BRFSS, 2013. The BRFSS data user guide https://www.cdc.gov/brfss/data_documentation/pdf/UserguideJune2013.pdf (accessed 20 August 2020).
- BRFSS, 2018. LLCP 2018 Codebook Report https://www.cdc.gov/brfss/annual_data/2018/pdf/codebook18_llcp-v2-508.pdf (accessed 05 October 2021).
- BRFSS, 2019a. Comparability of Data BRFSS 2018 https://www.cdc.gov/brfss/annual_data/2018/pdf/compare-2018-508.pdf (accessed 07 October 2021).
- BRFSS, 2019b. Complex Sampling Weights and Preparing 2018 BRFSS Module Data for Analysis https://www.cdc.gov/brfss/annual_data/2018/pdf/Complex-Smple-Weights-Prep-Module-Data-Analysis-2018-508.pdf (accessed 21 October 2020).
- Fontham Elizabeth T.H., Wolf Andrew M.D., Church Timothy R., Etzioni Ruth, Flowers Christopher R., Herzig Abbe, Guerra Carmen E., Oeffinger Kevin C., Shih Ya‐Chen Tina, Walter Louise C., Kim Jane J., Andrews Kimberly S., DeSantis Carol E., Fedewa Stacey A., Manassaram‐Baptiste Deana, Saslow Debbie, Wender Richard C., Smith Robert A. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J. Clin. 2020;70(5):321–346. doi: 10.3322/caac.21628. [DOI] [PubMed] [Google Scholar]
- Fuzzell Lindsay N., Perkins Rebecca B., Christy Shannon M., Lake Paige W., Vadaparampil Susan T. Cervical cancer screening in the United States: Challenges and potential solutions for underscreened groups. Prev. Med. 2021;144:106400. doi: 10.1016/j.ypmed.2020.106400. [DOI] [PubMed] [Google Scholar]
- Hall I.J., Tangka F.K.L., Sabatino S.A., Thompson T.D., Graubard B.I., Breen N. Patterns and Trends in Cancer Screening in the United States. Prev. Chronic Dis. 2018;15:E97. doi: 10.5888/pcd15.170465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthy People 2030, Increase the proportion of females who get screened for cervical cancer https://health.gov/healthypeople/objectives-and-data/browse-objectives/cancer/increase-proportion-females-who-get-screened-cervical-cancer-c-09 (accessed 15 July 2021).
- Hirth Jacqueline M., Laz Tabassum Haque, Rahman Mahbubur, Berenson Abbey B. Racial/Ethnic Differences Affecting Adherence to Cancer Screening Guidelines Among Women. J. Womens Health (Larchmt) 2016;25(4):371–380. doi: 10.1089/jwh.2015.5270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe Nancy K. Racial Disparity in the Prevalence of Cervical Cancer. J. Obstet. Gynecol. Neonatal Nurs. 2017;46(3):323–324. doi: 10.1016/j.jogn.2017.04.002. [DOI] [PubMed] [Google Scholar]
- Mohan Giridhar, Chattopadhyay Sajal. Cost-effectiveness of Leveraging Social Determinants of Health to Improve Breast, Cervical, and Colorectal Cancer Screening: A Systematic Review. JAMA Oncol. 2020;6(9):1434. doi: 10.1001/jamaoncol.2020.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orji Amarachukwu F., Yamashita Takashi. Racial disparities in routine health checkup and adherence to cancer screening guidelines among women in the United States of America. Cancer Causes Control. 2021;32(11):1247–1256. doi: 10.1007/s10552-021-01475-5. [DOI] [PubMed] [Google Scholar]
- Safaeian Mahboobeh, Solomon Diane, Castle Philip E. Cervical cancer prevention–cervical screening: science in evolution. Obstet. Gynecol. Clin. North Am. 2007;34(4):739–760. doi: 10.1016/j.ogc.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarinci Isabel C., Garcia Francisco A.R., Kobetz Erin, Partridge Edward E., Brandt Heather M., Bell Maria C., Dignan Mark, Ma Grace X., Daye Jane L., Castle Philip E. Cervical cancer prevention: new tools and old barriers. Cancer. 2010:NA–NA. doi: 10.1002/cncr.25065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Cancer Statistics Working Group, U.S. Cancer Statistics Data Visualizations Tool, based on 2020 submission data (1999-2018): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute, released in June 2021. https://www.cdc.gov/cancer/dataviz (accessed 05 October 2021).
- United States Census Bureau, Census regions and divisions of the United States https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf (accessed 20 August 2020).
- Yoo Wonsuk, Kim Sangmi, Huh Warner K., Dilley Sarah, Coughlin Steven S., Partridge Edward E., Chung Yunmi, Dicks Vivian, Lee Jae-Kwan, Bae Sejong, Chang Jeffrey S. Recent trends in racial and regional disparities in cervical cancer incidence and mortality in United States. PLoS One. 2017;12(2):e0172548. doi: 10.1371/journal.pone.017254810.1371/journal.pone.0172548.g00110.1371/journal.pone.0172548.g00210.1371/journal.pone.0172548.g00310.1371/journal.pone.0172548.g00410.1371/journal.pone.0172548.t00110.1371/journal.pone.0172548.s001. [DOI] [PMC free article] [PubMed] [Google Scholar]