Abstract
Background
We conducted a scoping review focused on various forms of substance use amid the pandemic, looking at both the impact of substance use on COVID-19 infection, severity, and vaccine uptake, as well as the impact that COVID-19 has had on substance use treatment and rates.
Methods
A scoping review, compiling both peer-reviewed and grey literature, focusing on substance use and COVID-19 was conducted on September 15, 2020 and again in April 15, 2021 to capture any new studies. Three bibliographic databases (Web of Science Core Collection, Embase, PubMed) and several preprint servers (EuropePMC, bioRxiv, medRxiv, F1000, PeerJ Preprints, PsyArXiv, Research Square) were searched. We included English language original studies only.
Results
Of 1564 articles screened in the abstract and title screening phase, we included 111 research studies (peer-reviewed: 98, grey literature: 13) that met inclusion criteria. There was limited research on substance use other than those involving tobacco or alcohol. We noted that individuals engaging in substance use had increased risk for COVID-19 severity, and Black Americans with COVID-19 and who engaged in substance use had worse outcomes than white Americans. There were issues with treatment provision earlier in the pandemic, but increased use of telehealth as the pandemic progressed. COVID-19 anxiety was associated with increased substance use.
Conclusions
Our scoping review of studies to date during COVID-19 uncovered notable research gaps namely the need for research efforts on vaccines, COVID-19 concerns such as anxiety and worry, and low- to middle-income countries (LMICs) and under-researched topics within substance use, and to explore the use of qualitative techniques and interventions where appropriate. We also noted that clinicians can screen and treat individuals exhibiting substance use to mitigate effects of the pandemic.
Funding
Study was funded by the Institution for Social and Policy Studies, Yale University and The Horowitz Foundation for Social Policy. DH was funded by a NIDA grant (R01DA048860). The funding body had no role in the design, analysis, or interpretation of the data in the study.
Keywords: COVID-19, Substance use, Lockdown
1. Introduction
Individuals engaging in various forms of substance use are likely greater affected by COVID-19. Broadly, due to stigma, people who engage in substance use are marginalized and poorly served by healthcare services (Volkow, 2020). Such stigma is persistent even among healthcare workers (Brondani et al., 2017). If hospitals are resource scarce, people reporting substance use may not be the priority if they manifest COVID-19 symptoms, possibly exacerbating the effect of both substance use and COVID-19 (Volkow, 2020).
We first provide an overview of three more common variants of substance use and how they relate to COVID-19: tobacco, opioids, cannabis. While there are many more forms of substance use e.g. hallucinogens, amphetamines, for brevity, we only cover three variants here but incorporate a far larger range of substance use in our paper. Regarding tobacco use, the percentage of current and individuals who smoke was higher among severe cases of COVID-9 compared to people who never smoked (Wj et al., 2020, Jj et al., 2020). People who vape nicotine or cannabis may be at risk for COVID-19, with recent work suggesting that some vape aerosols may damage lung tissue and reduce lungs’ ability to respond to infections (Madison et al., 2019).
People currently in treatment for opioid use may be affected by COVID-19 due to reduced access to medication for opioid use disorder (MOUD) given social distancing protocols (Alexander et al., 2020); and vulnerability due to compromised lung function (Volkow, 2020). People who receive methadone may face challenges arising from social distancing, as patients usually can only receive a single directly observed daily dose at a time (Abuse et al., 2015), although in some nations, like the United Kingdom, telemedicine and take-home supplies have been approved to allow medical providers to start and maintain MOUD (Bao et al., 2020, Leppla and Gross, 2020, Cochran et al., 2020). The diversion of resources at the health system level toward the pandemic may also strain MOUD provision, perhaps leading to patient drop out or medication discontinuation (Sun et al., 2020, Sordo et al., 2017). Social distancing may also increase the possibility of opioid overdoses, with fewer bystanders who can reverse the incident through naloxone administration (Volkow, 2020).
Cannabis sales on illegal online markets rose rapidly during the first three months of the pandemic (Farhoudian et al., 2020). This may represent an increase in personal use, which may correspond to greater rates of frequent use (Cerd́a et al., 2020). There has been an increase in alcohol sale and consumption in several nations (Colbert et al., 2020, Daly and Robinson, 2020). Similarly, people who use alcohol excessively may also be at greater risk for COVID-19 (Da et al., 2020); given that alcohol can weaken the body’s defenses against infections (Szabo & Saha, 2015). With social distancing, people who use alcohol may have less structured time meant for non-alcohol related activities (Vaillant, 2009). Without structured activities, people may relapse into problematic alcohol use (Da et al., 2020, Clay and Parker, 2020). Moreover, consumption of alcohol is associated with increased COVID-19 transmission due to people who are under the influence not adhering to social distancing (Pollard et al., 2020). COVID-19-related concerns such as anxiety, worry or fear (e.g. concerns around infection or job loss) may also be related to increased alcohol use (Rodriguez et al., 2020, Capasso et al., 2021) and increases in rates of other forms of substance use (Taylor et al., 2021).
Uptake, readiness and trust around the COVID-19 vaccine may also be related to substance use. Perhaps due to stigma around substance use, limited trust in the medical profession and vaccine development (Mellis et al., 2021), among other reasons, individuals engaging in substance use may be more prone to conspiracy theories, perhaps limiting their receipt of COVID-19 vaccines (Barocas, 2021). Moreover, individuals engaging in substance use may experience structural barriers to vaccination, including inadequate access to transportation and technology, which may limit ability to reach vaccine administration sites (Barocas, 2021). Reduced vaccine uptake may impinge on population-level impact (Donzelli et al., 2018), and COVID-19 control at the population level (Djidjou-Demasse et al., 2020). For example, reduced vaccine uptake may increase the mortality cost of COVID-19 (Djidjou-Demasse et al., 2020) and create clusters of non-vaccinators that disproportionately increase pandemic spread (Salath́e and Bonhoeffer, 2008).
There have been several reviews focused on COVID-19 and various forms of substance use (Vardavas and Nikitara, 2020, Patanavanich and Glantz, 2020, Farsalinos et al., 2020, Ramalho, 2020, Reddy et al., 2020, Mallet et al., 2020, Mallet et al., 2020). For example, one systematic review detailed COVID-19 and smoking, indicating that smoking may be associated with adverse COVID-19 outcomes (Vardavas & Nikitara, 2020). Reviews generally did not consider a large range of substance use, access to treatment for substance use, or the relationship between substance use and COVID-19 vaccine uptake. Detailing a large range of substance use variants is key to understanding the broad scope of COVID-19 on possibly marginalized populations e.g. Black Americans, sexual and gender minority (SGM) populations. Reviews not centering on less common forms of substance use and their relationship with COVID-19 may neglect populations possibly at greater risk during the pandemic. Detailing treatment access for substance use is key, given the disruptions to treatment in this period (Alexander et al., 2020) and the need to modify treatment provision in this regard. Exploring research around substance use and vaccine uptake and readiness is critical as individuals engaging in substance use may experience limited vaccine uptake, which may impact COVID-19 management (Djidjou-Demasse et al., 2020). Overall, monitoring substance use during the pandemic is essential, as people who engage in substance use may be at greater risk for COVID-19, and the economic and social changes resulting from the pandemic may alter substance use patterns (Ornell et al., 2020).
Broadly, understanding the relationship between COVID-19 and substance use is central to mitigating effects of the pandemic. Thus, a current overview of the bilateral impact of substance use and COVID-19 is required. This scoping review compiled peer-reviewed and grey literature in the field to identify gaps in current knowledge of substance use - including treatment access, and COVID-19 (e.g. the increased risk of infection, transmission, complication, co-morbidity, mortality), to support public health efforts, and guide intervention efforts and resource distribution, as large-scale COVID-19 vaccination among the US general public expands.
2. Methods
A scoping review of both peer-reviewed and grey literature was conducted by 11 individuals: 10 researchers from several universities worldwide, from a range of disciplines (e.g. public health, economics, epidemiology, and pharmacy), and an informationist from the Harvey Cushing/John Hay Whitney Medical Library at Yale University. We chose to conduct a scoping review rather than other methods of research synthesis because scoping reviews are appropriate for mapping an area of research (Arksey & O’Malley, 2005); we were not examining the effect of an intervention on an outcome of interest, as per a systematic review (Munn et al., 2018); and substance use outcomes were not sufficiently similar to each other to warrant pooling or formal meta-analysis regarding a specific outcome. Research objectives, inclusion criteria, and methodological techniques were determined before study commencement using the Joanna Briggs Institute (JBI) Reviewers’ Manual 2020 Methodology for JBI Scoping Reviews (Peters et al., 2020). This process adhered to the indicated framework: 1) identifying the research questions; 2) identifying relevant studies; 3) developing a comprehensive search strategy; 4) selecting studies; 5) charting data; and 6) collating, summarizing, and reporting results. The study team developed a search strategy as recommended by the 2020 Methodology for JBI Scoping Reviews (Peters et al., 2020). Reporting of results conformed to PRISMA Extension for Scoping Reviews (PRISMA-ScR) (Tricco et al., 2018). We published a study protocol (Kumar et al., 2021) and registered the study on the Open Science Framework (osf/io/tzgm5) to enhance methodological transparency and improve reproducibility of results and evidence synthesis.
3. Study selection criteria
3.1. Inclusion criteria
Published research (peer reviewed and grey literature such as reports, research letters and briefs, where primary data was collected) investigating substance use and COVID-19 in all populations, settings and study designs e.g. studies with small samples, quantitative and qualitative studies, were included. Primary outcomes included, but were not limited to COVID-19 diagnosis/severity, substance use, access to substance use treatment, social media posts and Google searches about substance use and COVID-19.
All variants of substance use, smokable or otherwise, e.g. alcohol, tobacco, nicotine, cannabis, cocaine, methamphetamine, non-medical use of psychoactive prescription drugs, inhalants, mescaline, nitrous oxide, and opioids (see Appendix Search Strategy for full list).
There were no restrictions on age, region, and gender.
3.2. Exclusion criteria
Commentaries, correspondences, case reports, case series, editorials, and opinion pieces were excluded, as they often contain relatively limited evidence (Turner et al., 2013).
Governmental or other agency guidelines were excluded.
Reviews such as systematic reviews and scoping reviews were excluded, but we reviewed the references in these for inclusion, if applicable.
Non-English studies were excluded through the algorithm used for the search strategy. Past work indicated that excluding non-English language records from a review seemed to have a minimal impact on results (Nussbaumer-Streit et al., 2020, Morrison et al., 2012).
3.3. Study selection
Two independent reviewers (AF, KJ) screened each title and abstract per inclusion/exclusion criteria. Inter-rater reliability estimates were calculated and a third reviewer (NK) acted as a tie breaker when there was lack of consensus. We obtained full-text articles of all potential eligible studies and evaluated article eligibility, similar to the abstract screening phase. If only abstracts and not full texts were available, we contacted authors where necessary if the abstracts did not provide sufficient information (Scherer & Saldanha, 2019).
3.4. Search method
Studies were reviewed across three databases focusing primarily on peer-reviewed literature: Web of Science Core Collection, Embase, and PubMed. These databases were selected as they capture peer-reviewed literature from a range of nations and include studies on substance use. Using similar techniques, we also searched preprint servers such as EuropePMC, bioRxiv, medRxiv, F1000, PeerJ Preprints, PsyArXiv and Research Square. See Appendix for example of search strategy.
The literature search was conducted in September 15, 2020 and then updated in April 15, 2021 to capture any new studies. We searched the literature from January 2020, which was when COVID-19 was reported to the World Health Organization (Huang et al., 2020), until September 2020, and then until April 2021. We conducted a grey literature search using Disaster Lit, HSRProj, Google Scholar, governmental websites, and clinical trials registries (e.g. ClinicalTrial.gov, World Health Organization International Clinical Trials Registry Platform and International Standard Randomized Controlled Trial Number registry). We used search terms similar to our main search to find articles for inclusion. All grey literature was compiled in a folder and reviewed similarly to articles obtained from our database searches. EndNote was used to store, organize, and manage all references (Analytics, 2017). Covidence was used to manage the title/abstract and full-text screening phases (Innovation, 2017).
3.5. Data extraction
Reviewers underwent practice exercises and then separately extracted study details from studies. Reviewers abstracted the study details using a pretested data extraction template. We used a standardized coding protocol to collect information such as: title of study with all author information and month/year published; study setting; study design; description of methodology; description of study sample; type of substance studied; main findings. While our search strategy covered all variants of substance use, included studies generally focused on only the following substances: tobacco, alcohol, opioids. Some studies detailed substances other than tobacco, alcohol, and opioids, such as cannabis and methamphetamine. However, such substances were generally not detailed as the sole focus of the study and were described in tandem with other forms substance use. Such studies were thus coded as multiple substances instead of e.g. cannabis or methamphetamine. We divided studies into the indicated categories, based on substance studied. Tobacco connotes all forms of tobacco and nicotine use, including combustible cigarettes, e-cigarettes, waterpipes, snus and chewing tobacco. Alcohol refers to all forms of alcohol consumption, such as wine, beer, spirits and includes methanol consumption. Opioids include drugs such as heroin, synthetic opioids such as fentanyl, pain relievers available legally by prescription, such as oxycodone, hydrocodone, codeine, and morphine, and medication for opioid use disorder (MOUD) such as methadone and buprenorphine. Multiple substances refer to the use of multiple substances, inclusive of prescription medications used in non-medical circumstances. We did not report p-values, odds ratios, effect size etc. in the Results section as a scoping review serves to identify and analyze knowledge gaps, and the types of available evidence in a given field, not identify and investigate conflicting results, as per a systematic review (Munn et al., 2018).
4. Results
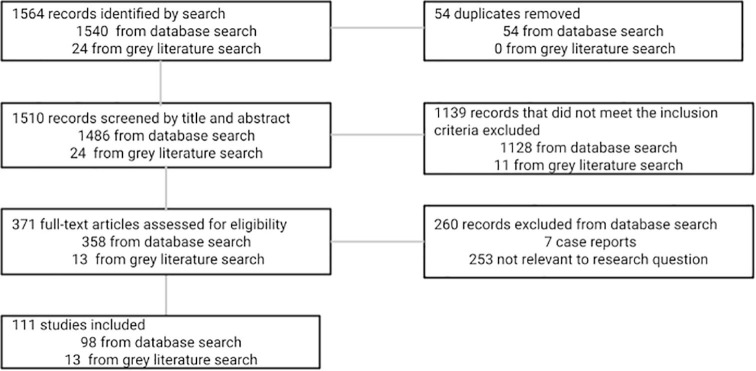
Our search yielded 1564 results (databases: 1540, grey literature: 43) with 54 duplicates, resulting in 1510 articles that were subjected to title and abstract review. Of those, 1139 were excluded at the abstract screening phase as they did not meet our inclusion criteria; most excluded were clearly not relevant to our research questions. Three hundred and seventy-one full-text articles were then screened and 260 were removed because they were case reports (7) or not relevant to the research question (253). The remaining 111 articles were included in the scoping review (Fig. 1 ). Table 1 shows the distribution of study setting, methodology, and sample size for the included studies across 92 countries. Studies were published from April 2020 to March 2021. Forty-eight percent (N = 53) of studies were conducted in the United States, 12% (N = 13) in the United Kingdom, 10% (N = 11) in India, 5% (N = 5) in Italy, 5% (N = 5) in China, 5% (N = 5) in South Africa, with the remaining in various other countries (19%, N = 20). Some studies were conducted in more than one country. Thirtyone percent (N = 34) of studies assessed tobacco-related outcomes, 42% (N = 47) assessed multiple substances, 19% (N = 21) assessed alcohol use, and 7% (N = 8) assessed opioid use. None of the studies identified concerned COVID-19 vaccine trust, readiness or uptake. Of the studies included, 56% (N = 62) were cross-sectional observational quantitative studies, 29% (N = 32) were retrospective observational cohort quantitative studies, 4% (N = 4) were prospective observational quantitative studies, 1% (N = 1) were modeling studies, 8% (N = 9) were qualitative studies, and 3% (N = 2) were mixed methods. No interventions were found, and some quantitative studies had small samples (<20), possibly affecting quality of results. By interventions, we refer to interventions that aim to mitigate effects of substance use during COVID-19. We do not consider the use of telehealth or telemedication on its own a type of intervention e.g. telehealth within an intervention to improve MOUD retention would be classified as an intervention but not the use of telehealth by physicians as a response to social distancing.
Fig. 1.
Flow diagram of search strategy used during the scoping review of substance use in relation to COVID-19.
Table 1.
Study characteristics related to design of study, setting, and sample size.
| Author, Year | Study (Cite/State, location Country) | Study type | Description of sample: N (% male) |
|---|---|---|---|
| Baghdad, Iraq | Cross-sectional Observational study | 284 (66%) | |
| Iran | Retrospective Observational study | N/A | |
| (Baillargeon et al, 2020) | United States | Retrospective Observational study | 22,024 (53%) |
| (Baldacchino et al., 2020) | Iran | Cross-sectional Observational study | N/A |
| (Balhara et al., 2020) | New Delhi, India | Cross-sectional Observational study | 73 (100%) |
| (Bandara et al., 2020) | United States | Cross-sectional Observational study | 16 (N/A) |
| (Barrio et al., 2021) | Spain | Retrospective Observational study | 362 (69%) |
| (Bartel et al., 2020) | Canada | Prospective observational study | 70 (34%) |
| (Bochicchio et al., 2021) | United States | Qualitative study | 16 (0%) |
| (Bommeĺe et al., 2020) | Netherlands | Cross-sectional observational study | 957 (56%) |
| (Bufquin et al., 2021) | United States | Retrospective Observational study | 585 (59%) |
| (Bunting et al., 2021) | N/A | Qualitative study | N/A |
| (Callinan et al., 2021) | Australia | Retrospective Observational study | 2307 (50%) |
| (Cancello et al., 2020) | Lombardy and Piedmont, Italy | Cross-sectional Observational study | 490 (16%) |
| (Cantor et al., 2020) | United States | Cross-sectional Observational study | N/A |
| (Capasso et al., 2021) | United States | Retrospective Observational study | 5850 (47%) |
| (Caponnetto et al., 2020) | Italy | Cross-sectional observational study | 1825 (38%) |
| (Chagúe et al., 2021) | France | Retrospective study observational | 325 (67%) |
| (Charles et al., 2021) | https://www.overleaf.comU/pnritoejdecSt/ta5tf9es58f840de15c0001R3ectbr7o3s9pective | Observational study | 254 (16%) |
| (Chodkiewicz et al., 2020) | Poland | Prospective observational study | 443 (21.4%) |
| (Cransac-Miet et al., 2020) | Cote d’Or, France | Cross-sectional observational study | 195 (61%) |
| (Croff, 2020) | United States | Mixed-methods study | N/A |
| (Czeisler et al., 2020) | United States | Cross-sectional observational study | 5470 (49%) |
| (DeJong et al., 2020) | Netherlands | Qualitative study | 15 (73%) |
| (Diclemente et al., 2020) | United States | Cross-sectional observational study | 6391 (42%) |
| (Dumas et al., 2020) | Canada | Cross-sectional observational study | 1054 (22%) |
| (Farhoudian et al., 2020) | Worldwide | Cross-sectional observational study | 185 (63%) |
| (Gaiha et al., 2020) | United States | Cross-sectional study observational | 4351 (33%) |
| (Ghosh, 2020) | India | Qualitative study | N/A |
| (Glover et al., 2020) | United States, NewZealand, India, South Africa | Cross-sectional observational study | N/A |
| (Graupensperger et al., 2021) | United States | Retrospective observational | 572 (39%) |
| (Grigg & Lenton, 2020) | Australia | Cross-sectional observational study | 100 (65%) |
| (Gritsenko et al., 2020) | Belarus, Russia | Retrospective Observational study | 939 (19%) |
| (Heerfodt & Heerfordt, 2020) | Worldwide | Retrospective Observational study | N/A |
| (Hochstatter et al., 2020) | Wisconsin, United States | Retrospective Observational study | 64 (75%) |
| (Holland et al., 2021) | United States | Cross-sectional Observational study | N/A |
| (Hopkinson et al., 2020) | United Kingdom | Prospective observational study | 2,401,982 (37%) |
| (Horigian et al., 2020) | United States | Cross-sectional Observational study | 1008 (52%) |
| (Hurley, 2021) | United States | Mixed-methods study | 24 (0%) |
| (Ismael et al., 2021) | Brazil | Retrospective Observational study | 993 (N/A) |
| (Jackson et al., 2020) | United Kingdom | Cross-sectional Observational study | 53,002 (49%) |
| (Jacob et al., 2021) | United Kingdom | Cross-sectional observational study | 691 (39%) |
| (Janmohamed et al., 2020) | United States | Cross-sectional Observational study | N/A |
| (Joyce et al., 2020) | Canada | Cross-sectional observational study | 508 (0%) |
| (Joyce et al., 2021) | United States | Qualitative study | 22 (NA) |
| (Ebrahimi Kalan et al., 2020) | Ardabil, Iran | Cross-sectional Observational study | 193 (64%) |
| (Kale et al., 2020) | United Kingdom | Cross-sectional observational Study | 2791 (48%) |
| (Kamiński et al., 2020) | Worldwide | Cross-sectional Observational study | 33,890 (N/A) |
| (Kayhan Tetik et al., 2020) | Malatya, Turkey | Cross-sectional Observational study | 357 (66.9%) |
| (Khatri et al., 2021) | United States | Cross-sectional Observational study | N/A |
| (Killgore et al., 2021) | United States | Retrospective Observational study | 5931 (43%) |
| (Kim et al., 2020) | United Kingdom | Cross-sectional Observational study | 182 (73%) |
| (Klemperer et al., 2020) | United States | Cross-sectional Observational study | 366 (69%) |
| (Koopmann et al., 2020) | Germany | Cross-sectional Observational study | 2102 (N/A) |
| (Kowitt et al., 2020) | United States | Cross-sectional Observational study | 777 (50%) |
| (Koyama et al., 2021) | Japan | Retrospective Observational study | 5120 (NA/) |
| (Krawczyk et al., 2021) | United States | Qualitative study | 1000 (N/A) |
| Kumar et al., 2020 (1) | United States | Cross-sectional Observational study | N/A |
| Kumar et al., 2020 (2) | United States | Cross-sectional Observational study | N/A |
| (Lechner et al., 2020) | Ohio, United States | Retrospective Observational study | 1958 (20%) |
| (Lee et al., 2021) | United States | Retrospective Observational study | 71,502 (NA) |
| (Li et al., 2020) (1) | United States | Modeling study | N/A |
| (Li et al., 2020) (2) | China | Retrospective Observational study | 954 (49%) |
| (Luk et al., 2020) | Hong Kong | Cross-sectional Observational study | 1501 (48%) |
| (McDonald et al., 2020) | United States | Retrospective Observational study | 2391 (60%) |
| (McKnight-Eily et al., 2021) | United States | Cross-sectional Observational study | 2008 |
| (Mcphee et al., 2020) | United States | Cross-sectional Observational study | 1127(65%) |
| (Mellis et al., 2021) | United States | Cross-sectional Observational study | 1118 (32%) |
| (Costa Monteiro et al., 2020) | Los Angeles, United States | Retrospective Observational study | 112 (66%) |
| (Narasimha et al., 2020) | Bangalore, India | Retrospective Observational study | 96 (100%) |
| (Neill et al., 2020) | Australia | Retrospective Observational study | 5068 (17%) |
| (Niedzwiedz et al., 2020) | United Kingdom | Prospective observational study | 27,141 (48%) |
| (Palamar & Acosta, 2020) | New York, United States | Cross-sectional Observational study | 128 (38%) |
| (Panagiotidis et al., 2020) | Greece | Cross-sectional Observational study | 705 (25%) |
| (Perski et al., 2020) | United Kingdom | Retrospective Observational study | 164,986 (N/A) |
| (Pettigrew et al., 2021) | United Kingdom, Australia, New Zealand | Cross-sectional Observational study | 1509 (50%) |
| (Pollard et al., 2020) | United States | Retrospective Observational study | 1540 (42%) |
| (Radfar et al, 2020) | N/A | Cross-sectional Observational study | 177 (58%) |
| (Rodriguez et al., 2020) | United States | Cross-sectional Observational study | 754 (100%) |
| (Rogers et al., 2020) | United States | Cross-sectional Observational study | 160 (57%) |
| (Rolland et al., 2020) | France | Cross-sectional Observational study | 11,391 (22%) |
| (Rosenbaum et al., 2021) | United States | Retrospective Observational study | 82,049 |
| (Rosoff-Verbit et al., 2021) | et al, | United States Cross-sectional study | observational |
| (Rozanova et al., 2020) | Kyiv, Ukraine | Qualitative study | 123 (56%) |
| (Sahu et al., 2020) | India | Cross-sectional Observational study | 153 (69%) |
| (Saurabh et al., 2021) | India | Cross-sectional Observational study | 911 (64%) |
| (Siddiqi et al., 2020) | Pakistan | Retrospective Observational study | 6014 |
| (Sidor et al., 2020) | Poland | Cross-sectional Observational study | 1097 (54%) |
| (Silczuk, 2020) | Poland | Cross-sectional Observational study | 117 (45%) |
| (Slavova et al., 2020) | Kentucky, United States | Retrospective Observational study | N/A |
| (Sokolovsky et al., 2020) | United States | Cross-sectional Observational study | 312 (49%) |
| (Stanton et al., 2020) | Australia | Cross-sectional Observational study | 1491 (33%) |
| (Starks et al., 2020) | United States | Cross-sectional Observational study | 910 (100%) |
| (Streck et al., 2021) | United States | Cross-sectional Observational study | 222 (53%) |
| (Sun et al., 2020) | China | Retrospective Observational study | 6416 (47%) |
| (Tattan-Birch et al., 2020) | United Kingdom | Cross-sectional Observational study | 3179 (46%) |
| (Taylor et al., 2021) | United States, Canada | Cross-sectional Observational study | 3075 (49%) |
| (Tsigaris & da Silva, 2020) | Europe | Cross-sectional Observational study | N/A |
| (Tucker et al, 2020) | United States | Cross-sectional Observational study | 90 (72%) |
| (Umucu & Lee, 2020) | United States | Cross-sectional Observational study | 269 (56%) |
| (Uscher-Pines et al., 2020) | United States | Qualitative study | 18 (N/A) |
| (Uvais, 2020) | India | Retrospective Observational study | N/A |
| (Vallecillo et al., 2020) | Spain | Cross-sectional Observational study | 27 (74%) |
| (Wang et al., 2020) | United States | Retrospective Observational study | 7,510,380 (53%) |
| (Wardell et al., 2020) | Canada | Retrospective Observational study | 320 (55%) |
| (Westrupp et al., 2020) | Australia | Cross-sectional Observational study | 2365 (19%) |
| (White et al., 2021) | United States | Cross-sectional Observational study | 776 (59%) |
| (Yach et al., 2020) | Italy, India, South Africa, United Kingdom, United States | Retrospective Observational study | 6800 (N/A) |
| (Yazdi et al., 2020) | Austria | Cross-sectional Observational study | 127 (67%) |
| (Yehudai et al., 2020) | Israel, Russia | Mixed-methods study | 291 (46%) |
Note: Studies reporting (N/A) for sample characteristics have not been conducted e.g. trials.
Table 2 detailed a synthesis of results organized by the four main substance categories studied.
Table 2.
Synthesis of results organized by substance studied.
| Author, Year | Main findings |
|---|---|
| Tobacco | |
| Individuals who smoked presented with a lower COVID-19 mortality rate compared to diabetic patients and diabetic+ smoking. | |
| Bommeĺe et al., 2020 | Individuals who smoke and were somewhat stressed were more likely to have increased their smoking during the pandemic. |
| (Cancello et al., 2020) | Among the 105 individuals who smoked habitually, 38% reported an increase in the TC consumption during lockdown. |
| (Caponnetto et al., 2020) | Individuals who both smoked and vaped reported a slight decrease in daily tobacco consumption during the pandemic. |
| Chagúe et al., 2021 | Among current individuals who smoke (n = 43), 13 (30.3%) declared increased tobacco consumption during the pandemic. |
| (Cransac-Miet et al., 2020) | 26% of individuals who smoke increased their tobacco consumption by > 25% during the pandemic. |
| (Gaiha et al., 2020) | COVID-19 diagnosis was five times more likely among ever-users of EC only. |
| (Heerfodt & Heerfordt, 2020) | There was no increase in the number of searches for smoking cessation on Google in the first months of the COVID-19 pandemic. |
| Hopkinson et al., 2020 | Current individuals who smoke were more likely to report COVID-19 symptoms. |
| Jackson et al., 2020 | Compared with individuals who have never smoked, prevalence of confirmed COVID-19 was higher among current but not individuals who previously smoked. |
| (Joyce et al., 2021) | COVID-19-induced environmental changes had mixed effects, facilitating quitting for some and impeding quitting for others. |
| (Janmohamed et al., 2020) | A topic related to CBD product preference emerged after COVID-19 was first reported. |
| Ebrahimi Kalan et al., 2020 | The average time between the onset of COVID-19 symptoms and hospitalization was approximately 4 days for individuals who smoke WPs, 3 days for individuals who smoke TC, and 5 days for never--individuals who smoke. |
| Kale et al., 2020 | Among current vapers (n = 397), 9.7% self-reported vaping less than usual since COVID-19. |
| Kamiński et al., 2020 | Of a total of 2,250 tweets posted by tobacco industry accounts, 58 (2.6%) mentioned COVID-19. |
| Kayhan Tetik et al., 2020 | There was a difference in the success of those who quit smoking before the pandemic and those who quit during it. |
| Klemperer et al., 2020 | There were positive correlations between perceived risk of harm from COVID-19 due to TC or EC use and motivation to quit for both TCs and ECs. |
| (Kowitt et al., 2020) | Majority of respondents (70.80%) reported intentions to quit smoking in the next six months due to COVID-19. |
| (Koyama et al., 2021) | There was a 32.1% increase in the number of cigarettes smoked and 11.9% of respondents quit smoking. |
| (Li et al., 2021) | Tobacco usage was associated with a large increase in the severity of COVID-19 symptoms. |
| (Pettigrew et al., 2021) | In Australia, New Zealand, and the United Kingdom, tobacco users appeared to be receptive to smoking-cessation messaging about how tobacco use increased COVID-19 susceptibility. |
| (Rosoff-Verbit et al., 2021) | Participants (n = 42) reported that COVID-19 had made it easier to quit tobacco usage |
| (Saurabh et al., 2021). | Current tobacco usage appeared to reduce the risk of contracting COVID-19 (n = 911). |
| (Siddiqi et al., 2020) | During the pandemic, many have ceased or initiated tobacco use. |
| (Sokolovsky et al., 2020) | Campus closures prompted many young adults to use tobacco less frequently. Streck et al., 2021 Of opioid users who also used tobacco (n = 145), most reported that tobacco usage increased COVID-19 susceptibility. |
| (Tsigaris & da Silva, 2020) | Nations with a higher number of individuals who smoked showed fewer COVID-19 cases. |
| (White et al., 2021) | Perceptions of risk related to tobacco use and COVID-19 have variable impacts on tobacco usage. |
| Yach et al., 2020 | EC use marginally increased during lockdown. |
| Kumar et al., 2020 (1) | COVID-19 news events may be related to perceptions around vaping. |
| Kumar et al., 2020 (2) | The online vaping environment may be affected by the pandemic. |
| (Li et al., 2020) | A 1% increase in weighted proportion of vapers in each state was associated with a 0.31 increase in the number of COVID-19 cases. |
| (Costa Monteiro et al., 2020) | Former and current smoking status were associated with invasive mechanical ventilation due to COVID-19. |
| (Perski et al., 2020) | There was no evidence for changes in smoking cessation app downloads attributable to the start of the pandemic. |
| Tattan-Birch et al., 2020 | Odds of self-reported COVID-19 were greater among current individuals who smoke (20.90%). |
| Alcohol | |
| (Aghababaeian et al., 2020) | From March 7 to April 8, 2020, all Iranian provinces reported methanol poisoning cases. |
| (Balhara et al., 2020) | Five patients (6.60%) reported alcohol withdrawal during the pandemic. |
| (Chodkiewicz et al., 2020) | Most (73%) respondents consumed alcohol, followed by smoking tobacco (25%). |
| (Kim et al., 2020) | 20% of individuals increased or decreased their normal alcohol consumption during lockdown. |
| (Koopmann et al., 2020) | 37.70% reported no change in their alcohol drinking behavior, 19.40% reported drinking less or much less and 34.70% reported drinking more or much more alcohol since the begin of the lockdown. |
| (Lechner et al., 2020) | Alcohol consumption increased as the pandemic progressed. |
| (Mcphee et al., 2020) | Frequency of solitary drinking increased post-social-distancing relative to pre-social-distancing. |
| (Narasimha et al., 2020) | The average number of alcohol withdrawal cases reported increased following lockdown. |
| (Neill et al., 2020) | Heavier drinking prepandemic, middle age, and average or higher income, were associated with increased drinking during the pandemic. |
| (Rodriguez et al., 2020) | Psychological distress and perceived threat related to COVID-19 were associated with a greater number of heavy drinking episodes. |
| (Silczuk, 2020) | Over 53% of screened doctors indicated that alcohol consumption escalated during the pandemic. |
| (Wardell et al., 2020) | Past 30-day coping motives predicted increased past 30-day alcohol use during the pandemic. |
| Opioids | |
| (Bandara et al., 2020) | Ten of 16 systems reduced the scale of their OAT during the pandemic. |
| (Rozanova et al., 2020) | While OPWH maintained HIV and substance use therapy throughout the lockdown, there was great anxiety about the availability of treatment services. |
| (Slavova et al., 2020) | After the COVID-19 state of emergency declaration, there was a 17% increase in the number of EMS opioid overdose runs. |
| (Uscher-Pines et al., 2020) | Most participants reported changing their typical clinical care patterns to help patients remain at home and minimize COVID-19 exposure. |
| Multiple substances | |
| (Baldacchino et al., 2020) | N/A Croff et al, 2020 |
| (Czeisler et al., 2020) | 13.30% of respondents increased substance use to cope with COVID-19 stress. |
| (DeJong et al., 2020) | During the pandemic, the use of psychoactive substances differed between the patients in treatment compared to those in stable recovery. |
| (Dumas et al., 2020) | Most adolescents (49.30%) were engaging in solitary substance use during the pandemic. |
| (Farhoudian et al., 2020) | Participants (69%) reported a decrease in drug supply during the pandemic. |
| (Ghosh, 2020) | Those who needed substance use treatment during lockdown faced multiple problems. |
| (Glover et al., 2020) | N/A |
| (Grigg & Lenton, 2020) | 34% of participants reported that the main drug they used in the past month was different to the main drug they used in February 2020. |
| (Hochstatter et al., 2020) | During the pandemic, there was no difference in the proportion of people using alcohol (41%) or cannabis (32%) compared to before the pandemic. |
| (Joyce et al., 2020) | Of participating mothers, 54.90% did not change their substance use during the pandemic. |
| (Luk et al., 2020) | Exposure to claims that smoking/drinking alcohol can protect against COVID-19 were associated with increased tobacco use for current individuals who smoke (N = 280)). |
| (Palamar & Acosta, 2020) | Older participants and those reporting past-year use of more drugs were more likely to use drugs during virtual raves. |
| (Sidor et al., 2020) | An increase in alcohol consumption during the pandemic was seen in 14.60% of participants. |
| (Stanton et al., 2020) | Those who reported an increase in smoking during the pandemic were more likely to have higher depression, anxiety, and stress symptoms. |
| (Starks et al., 2020) | The proportion reporting cannabis use declined (34.50% versus 45.70% pre-COVID-19). |
| Uvais, 2020 | Interest in the search term ‘how to quit smoking’ showed an increase early in the pandemic. |
| (Wang et al., 2020) | Patients who engaged in substance use were at increased risk for COVID-19. |
| (Westrupp et al., 2020) | During the pandemic period parents reported higher alcohol consumption. |
| (Yehudai et al., 2020) | Secular more than religious students reported higher levels of TC (45.70% vs. 31.60%), alcohol (83% vs. 57.40%), and cannabis (29.70% vs. 14.70%) use. |
| (Yoon et al., 2020) | During the pandemic, the opioid Twitter network had less disinformation. |
Note: N/A refers to in-progress studies. AOR: adjusted odds ratio; EC: e-cigarette; CI: confidence interval; EMS: emergency medical services; HR: hazard ratio; OAT: opioid agonist therapy; OPWH: older people with HIV; PRR: prevalence risk ratio; RSV: relative search value; TC: traditional cigarette; WP: water pipe.
4.1. Overview of research by substance studied
The sample sizes for the studies included in the review ranged from very small (<20) to several million. As this is a scoping review, we did not weigh the results quantitatively, but the sample sizes and methodologies, in part, affected the conclusions we drew. However, outcomes were too dissimilar to conduct a meta-analysis. Thus, we first drew conclusions around the following key results based on a study with a sample size > 70 million (Wang et al., 2020). Patients engaging in substance use were at increased risk for COVID-19, an effect that was strongest for individuals who used opioids, followed by individuals who used tobacco. COVID-19 patients engaging in substance use had worse outcomes (death, hospitalization) than general COVID-19 patients, and Black Americans with COVID-19 who engaged in substance use had worse outcomes than white Americans.
Across all substances, we noticed some key themes. Studies documented increasing prevalence of substance use and increased risks for COVID-19 (Wang et al., 2020, Jacob et al., 2021). Factors for increased prevalence and risk were also described, generally focusing on anxiety and psychological distress (Rodriguez et al., 2020, Taylor et al., 2021). Studies also linked COVID-19 related anxieties (e.g. job loss, fear of infection) to changes in substance use rates (Bufquin et al., 2021). Finally, changes in treatment provision were documented. Studies reported reduced treatment provision early in the pandemic, but as the pandemic progressed (Balhara et al., 2020, Bandara et al., 2020, Hochstatter et al., 2020), providers were incorporating telemedicine and other techniques (Sahu et al., 2020, Busch et al., 2021).
4.2. Tobacco
Twenty-two studies addressed tobacco use, with 45% (N = 10) addressing e-cigarette use. Several studies documented increased prevalence of use, e.g. a retrospective observational multi-country study reported an increase in e-cigarette use during the pandemic among individuals who currently smoke (Yach et al., 2020). Other studies highlighted tobacco use as a risk factor for COVID-19. For example, one study found that COVID-19 diagnosis was five times more likely among youth ever-users of e-cigarettes in the United States (Gaiha et al., 2020). A United Kingdom study found that the prevalence of COVID-19 was higher in individuals who currently smoked compared to individuals who previously smoked or had never smoked (Jackson et al., 2020). Possible risks of tobacco use may then have resulted in increased risk perceptions, with a US cross-sectional observational study of tobacco users indicating that most users believed that the risk of COVID-19 was greater for users of their tobacco product than for non-users (White et al., 2021). COVID-19 anxieties were also related to tobacco use, where a US cross-sectional observational study of college students indicated that COVID-19 related news exposure and seeking were related to decreased odds of pausing smoking or vaping (Sokolovsky et al., 2021).
4.3. Alcohol
Twelve studies addressed alcohol use. Multiple studies indicated increases in alcohol consumption across the pandemic e.g. a cross-sectional UK study of adults indicated that more than one in six participants increased their alcohol consumption during lockdown and a large proportion of these were younger adults (Jacob et al., 2021). Providing further insight, several studies detailed factors for increased alcohol consumption. One study found that psychological distress and COVID-19 related anxiety were associated with a higher number of heavy drinking episodes among American adults (Rodriguez et al., 2020). Findings from a cross-sectional observational study with a US-based social media sample indicated that anxiety and depression was related to increased alcohol use among those aged > 40 years (Capasso et al., 2021). Treatment provision was a common theme, with a cross-sectional observational study of Indian individuals undergoing treatment for problematic alcohol use finding that very few participants attempted to procure disulfuram during the pandemic, and even fewer were able to do so successfully (Balhara et al., 2020).
4.4. Opioids
Four studies detailed opioid use. A common theme was the shift in treatment provision as the pandemic progressed. For example, one cross-sectional observational quantitative study found that most American prison systems surveyed had reduced the scale of their medication for opioid use disorder (MOUD) programs during the pandemic and changed dispensation processes to ensure physical distancing (Bandara et al., 2020). We also indicated several studies around increases in overdoses linked to the pandemic. For example, an observational study of state emergency medical services found an increase in opioid overdoses following the declaration of a state of emergency in Kentucky, United States (Slavova et al., 2020). Similarly, a retrospective observational study of the incidence of opioid overdoses in US hospital system indicated that the pandemic was associated with an increase in the proportion of opioid overdoses within emergency department visits (Rosenbaum et al., 2021). Overdoses also seemed to be greater in marginalized communities e.g. a cross-sectional study indicated that as the pandemic progressed in Philadelphia the number of opioid-related overdose deaths was higher among non-Hispanic Black individuals than among non-Hispanic white individuals (Khatri et al., 2021).
4.5. Multiple substances
Twenty-one studies explored multiple substances, unlike the previous sections which focused on a single form of substance use. A key theme was the increased risk for COVID-19 associated with engaging in substance use especially for marginalized communities. For example, a retrospective observational study which detailed US electronic health records data of 73,099,850 patients, of whom 12,030 had a diagnosis of COVID-19, found that individuals engaging in substance use, especially those who used opioids, had increased risk for COVID-19 and its adverse outcomes (Wang et al., 2020) - with an increased risk for Black Americans. As with previous sections, several studies detailed the relationship between increased substance use and anxiety e.g. a cross-sectional study of Canadian mothers found that the majority of respondents did not change their substance use patterns, but several did and these were more likely to be individuals with anxiety disorders (Joyce et al., 2020). Similarly, a cross-sectional observational Australian study found that individuals who experienced higher tobacco and alcohol consumption during the pandemic were more likely to have depression, anxiety and stress (Stanton et al., 2020). Anxiety around the pandemic were also linked to substance use, where a cross-sectional survey of US restaurant employees indicated that working employees experienced higher levels of psychological distress, drug and alcohol use compared to furloughed employees (Bufquin et al., 2021). Transitions in treatment provision were also observed, where early in the pandemic a United States cross-sectional observational study did not find changes in alcohol or cannabis use during the pandemic but respondents attended fewer recovery support meetings and were less confident in their ability to stay sober (Hochstatter et al., 2020). However, as the pandemic progressed, telemedicine became commonplace in managing treatment provision e.g. a cross-sectional survey of Indian healthcare providers indicated that online consultation was key to managing substance use (Sahu et al., 2020).
5. Discussion
5.1. Overview
In this scoping review, we provide a comprehensive synthesis of the published literature around substance use in the COVID-19 era. This work builds on previous reviews around various forms of substance use (Vardavas and Nikitara, 2020, Patanavanich and Glantz, 2020, Farsalinos et al., 2020, Ramalho, 2020, Reddy et al., 2020, Mallet et al., 2020). Past reviews generally focused on a narrow range of substance use variants and did not consider a broad range of substance use variants, including treatment access for substance use. We assessed numerous outcomes, for example: COVID-19 diagnosis/severity, substance use, access to substance use treatment, social media posts and Google searches about substance use and COVID-19.
5.2. Key findings
We found that individuals engaging in substance use had increased risk for COVID-19 severity (Wang et al., 2020), especially among Black patients. Similarly, the number of opioid-related overdose deaths was higher among Black individuals compared to white individuals during the pandemic (Khatri et al., 2021). There was minimal research around individuals engaging in substance use and increased risk of COVID severity. Findings were also limited around substance use-related outcomes among groups such as Hispanic Americans and women. The limited research in this area may be due to a priority for research on other aspects of COVID-19, and a diversion of resources away from treatment for substance use, especially among marginalized communities (Melamed et al., 2020, Silva and Kelly, 2020) indirectly increasing health concerns around substance use (Venkatesan, 2020). Marginalized communities, such as individuals engaging in substance use, face greater risk of COVID-19 and its adverse outcomes possibly due to chronic medical conditions and reduced access to healthcare (Tai et al., 2020). We highlight the need to screen and treat individuals who engage in substance use (e.g. population based screening in primary care), especially among understudied marginalized communities who engage in substance use, to mitigate effects of the pandemic. We acknowledge the challenges in screening for substance use, such as stigma, and socioe-conomic status (Jones, 2005). Electronic screening that can be delivered through webportals, e-mails, and smartphones may address the both COVID-19-related and systemic barriers to screening (Donoghue et al., 2014, Ghosh and Sharma, 2021). The self-guided nature of electronic screening may be useful given the shortage of healthcare professionals that may be diverted from substance use care and treatment (Ghosh & Sharma, 2021). The pandemic may also have created a larger pool of patients that can be reached for screening, as individuals are referred for COVID-19 testing, or quarantined after contact tracing (Ghosh & Sharma, 2021).
5.3. Changes in treatment provision
We noted the changes in treatment provision as the pandemic progressed. At the start of the pandemic, some US incarcerated individuals who engaged in opioid use and some Indian patients who engaged in alcohol use were not able to access treatment e.g. need for an in-person visit to commence buprenorphine and methadone initiation (Harris et al., 2020). Social distancing and other similar measures may also have reduced treatment provision (Volkow, 2020). While there have been attempts to adapt MOUD to social distancing (Substance Abuse and Mental Health Services Administration, 2020), we noted that disulfiram provision for problematic alcohol use may not have been similarly modified. More recently, take-home privileges have been expanded for methadone maintenance treatment. As the pandemic progressed, telehealth use in substance use treatment has become more acceptable (Sahu et al., 2020) perceived as easy to use (Molfenter et al., 2021) and implement (Busch et al., 2021). While buprenorphine induction can now be conducted via telehealth, several US jurisdictions lack a physician able to prescribe buprenorphine. Thus, increased flexibility in induction procedures and greater medical licensing privileges may improve MOUD treatment outcomes. With the recent focus on telephone-initiated MOUD, an unexpected outcome has been the de-emphasizing of urine drug testing in monitoring patients, perhaps reducing stigma and improving patient outcomes (Pytell & Rastegar, 2021). We also suggest investigating possible negative consequences, such as increased diversion and nonadherence to treatment (Blanco et al., 2020), keeping in mind that some patients use diverted buprenorphine therapeutically (Silverstein et al., 2020).
5.4. COVID-19-related anxiety
We also noted that substance use may be associated with COVID-19 anxiety, worry or fear. For example, COVID-19-related anxiety was related to substance use coping motives among a US sample (Rogers et al., 2020); broad substance use among a population-representative sample of American and Canadian adults (Taylor et al., 2021), and alcohol use among those aged > 40 years in a US-based social media sample (Capasso et al., 2021). Substance use as a coping mechanism or a response to during large-scale events is well-documented (Vlahov et al., 2002, Moise and Ruiz, 2004, Xiaolu et al., 2017) and given the scale of the pandemic, it is unsurprising that substance use is used as a coping mechanism (Du et al., 2020). We put forward that substance use treatment programs include a component that addresses COVID-19-related concerns among patients (Wahlund et al., 2021).
5.5. Limited scope of forms of substance use studied
The bulk of included studies here centered on forms of substance use involving tobacco and alcohol, with minimal focus on opioids and other substances, due to a lack of research. We noted that substances such as cannabis and methamphetamine were included in studies coded as multiple substances, but such substances were not the main focus of any included studies. The limited focus on substances other than alcohol or tobacco may be due to alcohol or tobacco contributing to the greatest loss of disability-adjusted life years, compared to other substances (Peacock et al., 2018), or due to availability and ease of access compared to other substances. We put forward a need for research into a larger range of foci around other forms of substance use as the pandemic progresses, especially cannabis and methamphetamine given the increase in the use of these substances in recent years (Hasin, 2018, Jones et al., 2020).
5.6. Limited focus on the COVID-19 vaccine
None of the studies identified in our review concerned COVID-19 vaccine trust, readiness or uptake. The limited studies regarding the vaccine and substance use may be because large scale vaccination in the US is relatively recent, and vaccine studies around forms of substance use are not yet a research focus. Better understanding around vaccine mistrust by individuals engaging in substance use may improve vaccine trust and uptake (Barocas, 2021). Research around ways to limit barriers to vaccination uptake among individuals engaging in substance use may also aid vaccine receipt (Barocas, 2021, Mellis et al., 2021). We propose more research around COVID-19 vaccines and substance use, especially interventions in this arena. Interventions designed to increase vaccination uptake among individuals with mental illness (Miles et al., 2020), e.g. educational or distribution interventions, can be adapted for the substance use environment (Mellis et al., 2021), perhaps augmenting COVID-19 control at the population level (Djidjou-Demasse et al., 2020).
5.7. Limited focus on long COVID
We did not identify any studies around long COVID and substance use. Long COVID refers to a condition where people have recovered from COVID-19 but still report effects of the infection or have had the usual symptoms for far longer than commonly expected (Mahase, 2020). Individuals engaging in substance use are often at greater risk for COVID-19 and may similarly be at risk for long COVID. We suggest further work that explores long COVID in this population, mitigating the effects of the pandemic.
5.8. Limited use of qualitative techniques
A broad range of methods were applied to study substance use in line with the pandemic. However, we noticed limited use of qualitative techniques. The limited qualitative research may be due to beliefs that more prestigious peer-reviewed substance use journals are not open to qualitative research (Rhodes et al., 2010), the relatively limited funding for COVID-19 specific qualitative research, the complexities of conducting qualitative research in a pandemic, usually involving face-to-face meetings (Vindrola-Padros et al., 2020), and the time it takes to conduct and analyze qualitative data (Harding & Whitehead, 2013). Limited qualitative work around substance use and COVID-19 may obscure understanding on how marginalization and structural forces shape substance use within the pandemic (Rhodes et al., 2010); as qualitative research can aid understanding of natural phenomena with an emphasis on the lived experiences around disease, care and pandemic responses (Al-Busaidi, 2008, Teti et al., 2020), complementing and supplementing quantitative findings (Pope & Mays, 1995).
5.9. Lack of intervention studies
None of the studies identified in our scoping review were interventions. The lack of intervention studies may be because the research was conducted in the early phases of the pandemic and interventions, especially randomized controlled trials, take time to design, conduct, analyze and disseminate, and often involve face-to-face research. Randomized controlled trials are key to determining effectiveness of interventions (Gerstein et al., 2019) and are essential to improving health of marginalized communities during the pandemic. We propose that researchers incorporate more qualitative techniques, and conduct interventions, to complement existing quantitative research on substance use and COVID-19. We suggest incorporating telehealth and web-based health interventions to reach clients who are unable to receive in-person treatment (Clay, 2020). Interventions can also be included with electronic screening for forms of substance use, perhaps reaching a larger patient population (Ghosh and Sharma, 2021). As the shift toward telehealth may reduce stigma among patients (Pytell & Rastegar, 2021), novel interventions can be developed. Given the evidence around online social support in aiding substance use treatment outcomes (Bergman et al., 2020, Rozanova et al., 2020); we suggest interventions that explore social support or other similar techniques to improve substance use outcomes (Kumar et al., 2020). Treatment providers can informally encourage patients to seek social support from their family, friends or peers.
5.10. Lack of studies in LMICs
Studies were conducted in a large range of nations, aligned to regions where the impact of the pandemic was relatively severe, but the largest proportion were in high-income nations (83%, n = 93), with very few (13%, n = 14) in low- to middle-income countries (LMICs). The paucity of substance use research in LMICs may be due to limited resources (Ali et al., 2006, McGregor et al., 2014), lack of equitable research and funding partnerships (McGregor et al., 2014, Maalouf et al., 2019), and redistribution of resources amid COVID-19, among other factors. Recent work has expressed concerns regarding limited COVID-19 research centered in LMICs (Cattani, 2020), which could worsen pandemic progression when combined with LMICs’ inadequate healthcare infrastructure (Walker et al., 2020) potentially leading to long-term consequences such as increasing numbers of overdose deaths. We build on these findings, indicating the lack of COVID-19 research in the substance use context within LMICs, noting that data is being collected and monitored in LMICs, but not yet published. We believe that the currently limited work around substance use and COVID-19 in LMICs could reduce substance use healthcare provision in LMICs, such as MOUD programs; and by not measuring changes in substance use during the pandemic we may miss important shifts and lose prior achievements regarding substance use in LMICs.
5.11. Limitations
Our findings should be read in line with some limitations. Although we searched several databases and gray literature sources, we may have missed some studies. Not all authors we reached out to responded and we thus may have missed some unpublished work. The main strengths of the study are that we synthesized the research on substance use during COVID-19 and used a reproducible and clear procedure for the scoping review. We indicated the substance studied, location, methodology, sample characteristics, along with data extraction and search strategies. Moreover, we centered solely on the scope of substance use and COVID-19 research. Despite the limitations, our review has important implications for interventions around mitigating reduced health outcomes around substance use due to the pandemic.
6. Conclusion
For people who consumed alcohol or recreational drugs prior to the COVID-19 pandemic, consumption has increased substantially in the U.S. and Canada during the pandemic. Moreover, COVID-19 has further reduced access to target populations and increased difficulty in obtaining timely data to monitor changes in patterns of drug use and overdoses (Volkow & Blanco, 2021). Patients who engaged in substance use were also at increased risk for COVID-19, an effect that was strongest for individuals who used opioids, followed by individuals using tobacco (Volkow & Blanco, 2021). While the scope of substance use and COVID-19 research was broad, we noted limited work on substances other than tobacco and alcohol. Marginalized communities, such as individuals engaging in substance use, face greater risk of COVID-19 and its adverse outcomes possibly due to chronic medical conditions and reduced access to healthcare (Tai et al., 2020). We noted that Black individuals may be at greater risk for COVID-19 severity and overdose deaths compared to white individuals. We indicated issues with treatment provision earlier in the pandemic, but increased use of telehealth as the pandemic progressed. We indicated that substance use may be associated with COVID-19 anxiety, worry or fear. Substance use research is critical during COVID-19, and we indicated that some areas were clearly under-studied potentially limiting adequate treatment and vaccine uptake among patients. There were a range of methodologies applied within substance use, and COVID-19 research, but qualitative techniques and interventions were not commonly used. There was also limited research around COVID-19 vaccines, and within LMICs. Clinicians can screen and treat individuals engaging in substance use to mitigate effects of the pandemic, focus research efforts on COVID-19 vaccines, concerns such as anxiety and worry, LMICs and under-researched topics within substance use, and explore the use of qualitative techniques and interventions where appropriate.
7. Availability of data and materials
The datasets used and analyzed are available from the corresponding author on reasonable request.
Author contributions
NK and KJ wrote the first draft. NK, KN, KJ, MW, KK, LG, RP, SSM, DH, MC, JS, AF contributed to the manuscript write-up and review.
CRediT authorship contribution statement
Navin Kumar: Conceptualization, Methodology, Writing – review & editing. Kamila Janmohamed: Conceptualization, Methodology, Writing – review & editing. Kate Nyhan: Writing – review & editing. Silvia S. Martins: Writing – review & editing. Magdalena Cerda: Writing – review & editing. Deborah Hasin: Writing – review & editing. Jenny Scott: Writing – review & editing. Afia Sarpong Frimpong: Writing – review & editing. Richard Pates: Writing – review & editing. Lilian A. Ghandour: Writing – review & editing. Mayyada Wazaify: Writing – review & editing. Kaveh Khoshnood: Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Navin Kumar received funding from the Foundation for a Smoke-Free World for a separate project.
Acknowledgements
We thank the reviewers and editors for their assistance. Study was funded by the Institution for Social and Policy Studies, Yale University and The Horowitz Foundation for Social Policy. DH was funded by a NIDA grant (R01DA048860). The funding body had no role in the design, analysis, or interpretation of the data in the study.
Appendix.
Search strategy
-
1
exp Coronavirus/
-
2
exp Coronavirus Infections/
-
3
(coronavirus* or corona virus* or OC43 or NL63 or 229E or HKU1 or HCoV* or ncov* or covid* or sars-cov* or sarscov* or Sars-coronavirus* or Severe Acute Respiratory Syndrome Coronavirus*).mp.
4 (or/1–3) and ((20191* or 202*).dp. or 20190101:20301231.(ep).) [this set is the sensitive/broad part of the search]
-
5
4 not (SARS or SARS-CoV or MERS or MERS-CoV or Middle East respiratory syndrome or camel* or dromedar* or equine or coronary or coronal or covidence* or covidien or influenza virus or HIV or bovine or calves or TGEV or feline or porcine or BCoV or PED or PEDV or PDCoV or FIPV or FCoV or SADS-CoV or canine or CCov or zoonotic or avian influenza or H1N1 or H5N1 or H5N6 or IBV or murine corona*).mp. [line 5 removes noise in the search results]
-
6
((pneumonia or covid* or coronavirus* or corona virus* or ncov* or 2019-ncov or sars*).mp. or exp pneumonia/) and Wuhan.mp.
-
7
(2019-ncov or ncov19 or ncov-19 or 2019-novel CoV or sars-cov2 or sars-cov-2 or sarscov2 or sarscov-2 or Sars-coronavirus2 or Sars-coronavirus-2 or SARS-like coronavirus* or coronavirus-19 or covid19 or COVID-19 or covid 2019 or ((novel or new or nouveau) adj2 (CoV or nCoV or covid or coronavirus* or corona virus or Pandemi*2)) or ((covid or covid19 or COVID-19) and pandemic*2) or (coronavirus* and pneumonia)).mp.
-
8
COVID-19.rx,px,ox. or severe acute respiratory syndrome coronavirus 2.os.
-
9
.
| (”32240632″ | or | ”32236488″ | or | ”32268021″ | or | ”32267941″ | or | ”32169616″ | or |
| ”32267649″ | or | ”32267499″ | or | ”32267344″ | or | ”32248853″ | or | ”32246156″ | or |
| ”32243118″ | or | ”32240583″ | or | ”32237674″ | or | ”32234725″ | or | ”32173381″ | or |
| ”32227595″ | or | ”32185863″ | or | ”32221979″ | or | ”32213260″ | or | ”32205350″ | or |
| ”32202721″ | or | ”32197097″ | or | ”32196032″ | or | ”32188729″ | or | ”32176889″ | or |
| ”32088947″ | or | ”32277065″ | or | ”32273472″ | or | ”32273444″ | or | ”32145185″ | or |
| ”31917786″ | or | ”32267384″ | or | ”32265186″ | or | ”32253187″ | or | ”32265567″ | or |
| ”32231286″ | or | ”32105468″ | or | ”32179788″ | or | ”32152361″ | or | ”32152148″ | or |
| ”32140676″ | or | ”32053580″ | or | ”32029604″ | or | ”32127714″ | or | ”32047315″ | or |
| ”32020111″ | or | ”32267950″ | or | ”32249952″ | or | ”32172715″).ui. |
-
10
or/6–9 [Lines 6 to 9 are specific to COVID-19]
-
11
11 5 or 10
-
12
11 and 20191201:20301231.(dt).
-
13
(covid* or ncov* or 2019-novel CoV or SARS-CoV2 or SARS-CoV-2 or SARSCoV2 or SARSCov-2 or ”severe acute respiratory syndrome coronavirus 2″).mp.
-
14
(coronavirus* or corona virus*).mp. and 2020*.dp.
-
15
((novel or new or ”2019″ or ”19″ or pandemic or crisis or outbreak or Wuhan or China) adj3 (coronavirus* or corona virus*)).mp.
-
16
COVID-19.rx.
-
17
coronavirus infections/ and 2020*.dp.
-
18
Pneumonia, Viral/ and 2020*.dp. 19 or/13–18
20 12 or 19
-
21
[from the CADTH hedge]
-
22
(coronavirus/ or betacoronavirus/ or coronavirus infections/) and (disease outbreaks/ or epidemics/ or pandemics/)
-
23
(nCoV* or 2019nCoV or 19nCoV or COVID19* or COVID or SARS-COV-2 or SARSCOV-2 or SARSCOV2 or Severe Acute Respiratory Syndrome Coronavirus 2 or Severe Acute Respiratory Syndrome Corona Virus 2).ti,ab,kf,nm,ot,ox,rx,px.
-
24
((new or novel or ”19″ or ”2019″ or Wuhan or Hubei or China or Chinese) adj3 (coronavirus* or corona virus* or betacoronavirus* or CoV or HCoV)).ti,ab,kf,ot.
-
25
((coronavirus* or corona virus* or betacoronavirus*) adj3 (pandemic* or epidemic* or outbreak* or crisis)).ti,ab,kf,ot.
-
26
((Wuhan or Hubei) adj5 pneumonia).ti,ab,kf,ot. 27 or/22–26
-
28
limit 27 to yr=”2019 -Current”
-
29
20 [homegrown]
-
30
27 [CADTH] 31 20 or 27
-
32
(epidemic or pandemic or crisis or social* distan* or quarantin* or self-isolat* or recession*).mp. or economic recession/
-
33
[substance use]
-
34
[opioid use]
-
35
substance-related disorders/ or opioid-related disorders/ or heroin dependence/ or morphine dependence/ or opium dependence/ or substance abuse, intra-venous/ or substance abuse, oral/ or substance withdrawal syndrome/ or methadone/ or opi* substitution treatment/ or opi* substitution therapy/ or opi* agonist treatment/ or opi* sub*/ or opi* interven*/ or opi* treat*/
-
36
((opioid* or opiate* or heroin or amphetamine*) adj3 (abus* or dependen* or disorder* or addict* or misus* or ”use” or ”user” or ”users” or ”usage” or ”using” or ”used”)).mp.
-
37
exp Narcotics/po
-
38
(OUD or IDU or PWID).mp.
-
39
(”injection drug use” or ”intravenous drug use”).mp.
-
40
[smoking and vaping]
-
41
exp smoking/
-
42
”tobacco use disorder”/
-
43
smoking cessation/
-
44
”tobacco use cessation”/
-
45
vaping/
-
46
Electronic Nicotine Delivery Systems/
-
47
marijuana abuse/ or exp ”marijuana use”/
-
48
exp tobacco products/
-
49
(smoking or smoker* or cigarette* or ecig* or e-cig* or tobacco or snuff or snus or cannabis or marijuana or vape or vaping or vaper or vapers or vaped or cigar*).mp.
-
50
[alcohol]
-
51
exp alcohol-related disorders/
-
52
(alcohol* or ”alcohol use” or alcohol abuse* or wine* or beer* or liquor* or spirits).mp.
-
53
[big picture]
-
54
exp substance-related disorders/ or illicit drugs/
-
55
((substance* adj3 (abus* or dependen* or disorder* or addict* or misus* or ”use” or ”user” or ”users” or ”usage” or ”using” or ”used”)) or addiction* or addict*).mp.
-
56
[additional substances]
-
57
aerosol propellant*.mp.
-
58
((sniff* or huff* or inhal*) adj2 aerosol*).mp.
-
59
inhalant abuse.mp.
-
60
huffing.mp.
-
61
aliphatic nitrites.mp.
-
62
(amphetamine* or speed).mp.
-
63
anabolic steroid*.mp.
-
64
doping in sports/ and exp steroids/
-
65
performance-enhancing substances/
-
66
(phencyclidine or PCP or angel dust).mp.
-
67
exp Benzodiazepines/ae
-
68
benzodiazepine*.mp.
-
69
cocaine.mp.
-
70
(ecstasy or MDMA).mp.
-
71
exp Hallucinogens/ae
-
72
N-Methyl-3,4-methylenedioxyamphetamine/
-
73
(GBH or GBL or gamma-hydroxybutyrate).mp.
-
74
4-Butyrolactone/
-
75
glue.mp.
-
76
(hashish or heroin).mp.
-
77
exp ”hypnotics and sedatives”/
-
78
hypnotics.mp.
-
79
inhalant*.mp.
-
80
(LSD or Lysergic Acid Diethylamide).mp.
-
81
mescaline/
-
82
mescaline.mp.
-
83
exp amphetamines/
-
84
methamphetamine*.mp.
-
85
methylxanthine*.mp.
-
86
nicotine.mp. or nicotine chewing gum/ or nicotine/
-
87
(nitrous oxide or laughing gas).mp.
-
88
((OTC or over the counter) adj1 (drug* or medication*)).mp.
-
89
nonprescription drugs/ae
-
90
oxycodone.mp.
-
91
paint thinner*.mp.
-
92
amyl nitrite.mp.
-
93
poppers.mp.
-
94
psilocybe.mp.
-
95
salvia divinorum.mp.
-
96
sedative*.mp.
-
97
stimulant*.mp.
-
98
tranquilizer*.mp.
-
99
designer drugs/
-
100
telehealth/
-
101
telemed*/
-
102
interven*/ 103 or/33–99
104 100 and (31 or 32)
-
105
limit 101 to (english language and yr=”2020 -Current”)
-
106
[compare with the similar search, without line 32] 107 100 and 31
-
108
limit 104 to (english language and yr=”2020 -Current”)
-
109
[the difference]
-
110
105 not 106
References
- Abuse, Substance and others. Federal guidelines for opioid treatment programs. HHS publication no(SMA) PEP15-FEDGUIDEOTP. 2015.
- Aghababaeian H., Hamdanieh L., Ostadtaghizadeh A. Alcohol intake in an attempt to fight COVID-19: A medical myth in Iran. Alcohol (Fayetteville, NY) 2020 November;88:29–32. doi: 10.1016/j.alcohol.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Busaidi Z.Q. Qualitative research and its uses in health care. Sultan Qaboos University Medical Journal. 2008;8(1):11. [PMC free article] [PubMed] [Google Scholar]
- Alexander G.C., Stoller K.B., Haffajee R.L., Saloner B. An epidemic in the midst of a pandemic: opioid use disorder and COVID-19. American College of Physicians. 2020 doi: 10.7326/M20-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali N., Hill C., Kennedy A., Ijsselmuiden C. What factors influence national health research agendas in low and middle income countries. Record Paper. 2006;5 [Google Scholar]
- Analytics C. Clarivate Analytics; Philadelphia, PA: 2017. Endnote X8 for windows. [Google Scholar]
- Arksey H., O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19–32. [Google Scholar]
- Baillargeon J, Polychronopoulou E, Kuo YF, Raji MA. The Impact of Substance Use Disorder on COVID-19 Outcomes. Psychiatric Services. 0;0(0):appi.ps.202000534. PMID: 33138712. [DOI] [PMC free article] [PubMed]
- Baldacchino A., Radfar S.R., Jong C., Rafei P., Yunesian M., Gerra G., et al. COVID-19 and Substance Use Disorder: Study Protocol for the International Society of Addiction Medicine Practice and Policy Interest Group Global Survey. Basic and Clinical Neuroscience. 2020;06(11):201–208. doi: 10.32598/bcn.11.covid19.2545.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balhara Y.P.S., Singh S., Narang P. Effect of lockdown following COVID-19 pandemic on alcohol use and help-seeking behavior: Observations and insights from a sample of alcohol use disorder patients under treatment from a tertiary care center. Psychiatry and Clinical Neurosciences. 2020;74(8):440–441. doi: 10.1111/pcn.13075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandara S., Kennedy-Hendricks A., Merritt S., Barry C., Brendan S. Early Effects of COVID-19 on Programs Providing Medications for Opioid Use Disorder in Jails and Prisons. Journal of Addiction Medicine. 2020;14(5):e257–e260. doi: 10.1097/ADM.0000000000000718. [DOI] [PubMed] [Google Scholar]
- Bao Y., Williams A.R., Schackman B.R. COVID-19 Could Change the Way We Respond to the Opioid Crisis—for the Better. Psychiatric Services. 2020 doi: 10.1176/appi.ps.202000226. appi–ps. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barocas J.A. Business Not as Usual—Covid-19 Vaccination in Persons with Substance Use Disorders. New England Journal of Medicine. 2021;384(2):e6. doi: 10.1056/NEJMpv2035709. [DOI] [PubMed] [Google Scholar]
- Barrio P, Baldaqúı N, Andreu M, Kilian C, Rehm J, Gual A, et al. Abstinence Among Alcohol Use Disorder Patients During the COVID-19 Pandemic: Insights From Spain. Alcoholism: Clinical and Experimental Research. 2021;45(4):802–807. Available from: https://onlinelibrary.wiley.com/ doi/abs/10.1111/acer.14555. [DOI] [PubMed]
- Bartel SJ, Sherry SB, Stewart SH. Self-isolation: A significant contributor to cannabis use during the COVID-19 pandemic. Substance Abuse. 2020;41(4):409–412. PMID: 33044893. Available from: https://doi.org/10.1080/08897077.2020.1823550. [DOI] [PubMed]
- Bergman B.G., Kelly J.F., Fava M., Evins A.E. Elsevier; 2020. Online recovery support meetings can help mitigate the public health consequences of COVID-19 for individuals with substance use disorder. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C., Compton W.M., Volkow N.D. Opportunities for research on the treatment of substance use disorders in the context of COVID-19. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.3177. [DOI] [PubMed] [Google Scholar]
- Bochicchio LA, Drabble LA, Riggle EDB, Munroe C, Wootton AR, Hughes TL. Understanding Alcohol and Marijuana Use among Sexual Minority Women during the COVID-19 Pandemic: A Descriptive Phenomenological Study. Journal of Homosexuality. 2021;68(4):631–646. PMID: 33439793. Available from: https://doi.org/10.1080/00918369.2020.1868187. [DOI] [PMC free article] [PubMed]
- Bommeĺe J., Hopman P., Hipple Walters B., Geboers C., Croes E., Fong G., et al. The double-edged relationship between COVID-19 stress and smoking: Implications for smoking cessation. Tobacco Induced Diseases. 2020;07:18. doi: 10.18332/tid/125580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brondani M.A., Alan R., Donnelly L. Stigma of addiction and mental illness in healthcare: the case of patients’ experiences in dental settings. PloS one. 2017;12(5):e0177388. doi: 10.1371/journal.pone.0177388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bufquin D., Park J.Y., Back R.M., de Souza Meira J.V., Hight S.K. Employee work status, mental health, substance use, and career turnover intentions: An examination of restaurant employees during COVID-19. International Journal of Hospitality Management. 2021;93:102764. doi: 10.1016/j.ijhm.2020.102764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunting AM, Frank D, Arshonsky J, Bragg MA, Friedman SR, Krawczyk N. Socially-supportive norms and mutual aid of people who use opioids: An analysis of Reddit during the initial COVID-19 pandemic. Drug and Alcohol Dependence. 2021;222:108672. Available from: https://www.sciencedirect.com/ science/article/pii/S0376871621001678. [DOI] [PMC free article] [PubMed]
- Busch A.B., Sugarman D.E., Horvitz L.E., Greenfield S.F. Telemedicine for treating mental health and substance use disorders: reflections since the pandemic. Neuropsychopharmacology. 2021;1–3 doi: 10.1038/s41386-021-00960-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callinan S., Mojica-Perez Y., Wright C.J.C., Livingston M., Kuntsche S., Laslett A.M., et al. Purchasing, consumption, demographic and socioeconomic variables associated with shifts in alcohol consumption during the COVID-19 pandemic. Drug and Alcohol Review. 2021;40(2):183–191. doi: 10.1111/dar.13200. https://onlinelibrary.wiley.com/doi/abs/10.1111/dar.13200 Available from. [DOI] [PubMed] [Google Scholar]
- Cancello R., Soranna D., Zambra G., Zambon A., Invitti C. Determinants of the Lifestyle Changes during COVID-19 Pandemic in the Residents of Northern Italy. International Journal of Environmental Research and Public Health. 2020;17 doi: 10.3390/ijerph17176287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantor J., Stein B.D., Saloner B. Telehealth Capability Among Substance Use Disorder Treatment Facilities in Counties With High Versus Low COVID-19 Social Distancing. Journal of Addiction Medicine. 2020;14(6) doi: 10.1097/ADM.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capasso A., Jones A.M., Ali S.H., Foreman J., Tozan Y., DiClemente R.J. Increased alcohol use during the COVID-19 pandemic: The effect of mental health and age in a cross-sectional sample of social media users in the US. Preventive Medicine. 2021;145:106422. doi: 10.1016/j.ypmed.2021.106422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caponnetto P., Inguscio L., Saitta C., Maglia M., Benfatto F., Polosa R. Smoking behavior and psychological dynamics during COVID-19 social distancing and stay-at-home policies: A survey. Health Psychology Research. 2020;05:8. doi: 10.4081/hpr.2020.9124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattani M. Global coalition to accelerate COVID-19 clinical research in resource-limited settings. Lancet. 2020 doi: 10.1016/S0140-6736(20)30798-4. 30798–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerd́a M., Mauro C., Hamilton A., Levy N.S., Santaella-Tenorio J., Hasin D., et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use. JAMA Psychiatry. 2020;77(2):165–171. doi: 10.1001/jamapsychiatry.2019.3254. disorder from 2008 to 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chagúe F., Boulin M., Eicher J., Bichat F., Saint-Jalmes M., Cransac A., et al. Alarming increased rate of smoking and associated lifestyle behaviours in patients with chronic cardiac diseases during COVID-19 pandemic related lockdown. Archives of Cardiovascular Diseases Supplements. 2021;13(1):127. [Google Scholar]
- Charles NE, Strong SJ, Burns LC, Bullerjahn MR, Serafine KM. Increased mood disorder symptoms, perceived stress, and alcohol use among college students during the COVID-19 pandemic. Psychiatry Research. 2021;296:113706. Available from: https://www.sciencedirect.com/science/article/ pii/S0165178121000032. [DOI] [PMC free article] [PubMed]
- Chodkiewicz J., Talarowska M., Miniszewska J., Nawrocka N., Biliński P. Alcohol Consumption Reported during the COVID-19 Pandemic: The Initial Stage. International Journal of Environmental Research and Public Health. 2020:06. doi: 10.3390/ijerph17134677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clay R. American Psychological Association; 2020. Advice for treating and preventing substance use during COVID-19. [Google Scholar]
- Clay J.M., Parker M.O. Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis? The Lancet Public Health. 2020;5(5):e259. doi: 10.1016/S2468-2667(20)30088-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran G., Bruneau J., Cox N., Gordon A.J. Taylor & Francis; 2020. Medication treatment for opioid use disorder and community pharmacy: Expanding care during a national epidemic and global pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colbert S., Wilkinson C., Thornton L., Richmond R. COVID-19 and alcohol in Australia: industry changes and public health impacts. Drug and Alcohol Review. 2020 doi: 10.1111/dar.13092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa Monteiro A.C., Suri R., Emeruwa I.O., Stretch R.J., Cortes Lopez R.Y., Sherman A., et al. Obesity and Smoking as Risk Factors for Invasive Mechanical Ventilation in COVID-19: a Retrospective, Observational Cohort Study. medRxiv. 2020 doi: 10.1371/journal.pone.0238552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cransac-Miet A., Zeller M., Chague F., Faure A., Bichat F., Danchin N., et al. Impact of COVID-19 lockdown on lifestyle adherence in stay-at-home patients with chronic coronary syndromes: Towards a time bomb. International Journal of Cardiology. 2020;09 doi: 10.1016/j.ijcard.2020.08.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croff J.M. Understanding the effects of COVID-19 on maternal substance use. Osu Center for Health Sciences. 2020 [Google Scholar]
- Czeisler M., Lane R., Petrosky E., Wiley J., Christensen A., Njai R., et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic - United States, June 24–30, 2020. MMWR Morbidity and Mortality Weekly Report. 2020;08(69):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da B.L., Im G.Y., Schiano T.D. COVID-19 hangover: a rising tide of alcohol use disorder and alcohol-associated liver disease. Hepatology. 2020 doi: 10.1002/hep.31307. [DOI] [PubMed] [Google Scholar]
- Daly M., Robinson E. Problem drinking before and during the COVID-19 crisis in US and UK adults: Evidence from two population-based longitudinal studies. medRxiv. 2020 [Google Scholar]
- DeJong C., DeJong V.J., Pols R., Verbrugge C., Baldacchino A. Psychological Impact of the Acute COVID-19 period on patients with substance use disorder. Basic and Clinical. Neuroscience. 2020;11 doi: 10.32598/bcn.11.covid19.2543.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diclemente RJ, Capasso A, Ali SH, Jones AM, Foreman J, Tozan Y. Knowledge, beliefs, mental health, substance use, and behaviors related to the COVID-19 pandemic among U.S. adults: A national online survey. 2020. [DOI] [PMC free article] [PubMed]
- Djidjou-Demasse R., Michalakis Y., Choisy M., Sofonea M.T., Alizon S. Optimal COVID-19 epidemic control until vaccine deployment. medRxiv. 2020 [Google Scholar]
- Donoghue K., Patton R., Phillips T., Deluca P., Drummond C. The effectiveness of electronic screening and brief intervention for reducing levels of alcohol consumption: a systematic review and meta-analysis. Journal of Medical Internet Research. 2014;16(6):e142. doi: 10.2196/jmir.3193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donzelli G., Palomba G., Federigi I., Aquino F., Cioni L., Verani M., et al. Misinformation on vaccination: A quantitative analysis of YouTube videos. Human Vaccines & Immunotherapeutics. 2018;14(7):1654–1659. doi: 10.1080/21645515.2018.1454572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du J., Fan N., Zhao M., Hao W., Liu T., Lu L., et al. Expert consensus on the prevention and treatment of substance use and addictive behaviour-related disorders during the COVID-19 pandemic. General Psychiatry. 2020;33(4) doi: 10.1136/gpsych-2020-100252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumas T., Ellis W., Litt D. What Does Adolescent Substance Use Look Like During the COVID-19 Pandemic? Examining Changes in Frequency, Social Contexts, and Pandemic-Related Predictors. Journal of Adolescent Health. 2020;07:67. doi: 10.1016/j.jadohealth.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahimi Kalan M., Ghobadi H., Ben Taleb Z., Ward K., Adham D., Matin S., et al. Descriptive characteristics of hospitalized adult smokers and never-smokers with COVID-19. Tobacco Induced Diseases. 2020;05(18):46. doi: 10.18332/tid/122759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farhoudian A., Radfar S.R., Ardabili H.M., Rafei P., Ebrahimy M., Zonoozi A.K., et al. A global survey on changes in the supply, price and use of illicit drugs and alcohol, and related complications during the 2020 COVID-19 pandemic. medRxiv. 2020 doi: 10.3389/fpsyt.2021.646206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farsalinos K., Barbouni A., Niaura R. Systematic review of the prevalence of current smoking among hospitalized COVID-19 patients in China: could nicotine be a therapeutic option? Internal and Emergency Medicine. 2020:1–8. doi: 10.1007/s11739-020-02355-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaiha S.M., Cheng J., Halpern-Felsher B. Association Between Youth Smoking, Electronic Cigarette Use, and COVID-19. Journal of Adolescent Health. 2020;67(4):519–523. doi: 10.1016/j.jadohealth.2020.07.002. Available from: http: //www.sciencedirect.com/science/article/pii/S1054139X20303992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstein H.C., McMurray J., Holman R.R. Real-world studies no substitute for RCTs in establishing efficacy. Lancet (London, England) 2019;393(10168):210. doi: 10.1016/S0140-6736(18)32840-X. [DOI] [PubMed] [Google Scholar]
- Ghosh G.K. Coping in Lockdown Study (CILS): The experiences of people who prior to COVID-19, and or currently, smoked, used any form of tobacco or nicotine product, drank alcohol, or used cannabis or other drugs. Journal of Health and Social Sciences. 2020;09(5):265–272. [Google Scholar]
- Ghosh A., Sharma K. The American journal of drug and alcohol abuse. 2021. Screening and brief intervention for substance use disorders in times of COVID-19: potential opportunities, adaptations, and challenges; pp. 1–6. [DOI] [PubMed] [Google Scholar]
- Glover M, Phillips CV, Shepherd R, Selket K, Paramanthen K. Coping in Lockdown Study (CILS): The experiences of people who prior to COVID-19, and or currently, smoked, used any form of tobacco or nicotine product, drank alcohol, or used cannabis or other drugs.; 2020.
- Graupensperger S., Fleming C.B., Jaffe A.E., Rhew I.C., Patrick M.E., Lee C.M. Changes in Young Adults’ Alcohol and Marijuana Use, Norms, and Motives From Before to During the COVID-19 Pandemic. Journal of Adolescent Health. 2021;68(4):658–665. doi: 10.1016/j.jadohealth.2021.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigg J., Lenton S. Findings from the Ecstasy and Related Drugs Reporting System 2020. 2020. Impacts of COVID-19 and associated restrictions on people who use illicit stimulants in Western Australia. [Google Scholar]
- Gritsenko V., Skugarevsky O., Konstantinov V., Khamenka N., Marinova T., Reznik A., et al. COVID 19 Fear, Stress, Anxiety, and Substance Use Among Russian and Belarusian University Students. International Journal of Mental Health and Addiction. 2020 doi: 10.1007/s11469-020-00330-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harding T., Whitehead D., et al. Elsevier-Mosby; Marrickville, Sydney: 2013. Analysing data in qualitative research. [Google Scholar]
- Harris M., Johnson S., Mackin S., Saitz R., Walley A.Y., Taylor J.L. Low barrier tele-buprenorphine in the time of COVID-19: a case report. Journal of Addiction Medicine. 2020 doi: 10.1097/ADM.0000000000000682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D.S. US epidemiology of cannabis use and associated problems. Neuropsychopharmacology. 2018;43(1):195–212. doi: 10.1038/npp.2017.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heerfodt C., Heerfordt I.M. Has there been an increased interest in smoking cessation during the first months of the COVID-19 Panddemic? A Google Trends study. Public Health. 2020;183:6–7. doi: 10.1016/j.puhe.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochstatter K., Akhtar W., Dietz S., Pe-Romashko K., Gustafson D., Shah D., et al. Potential Influences of the COVID-19 Pandemic on Drug Use and HIV Care Among People Living with HIV and Substance Use Disorders: Experience from a Pilot mHealth Intervention. AIDS and Behavior. 2020;07 doi: 10.1007/s10461-020-02976-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland K.M., Jones C., Vivolo-Kantor A.M., Idaikkadar N., Zwald M., Hoots B., et al. Trends in US Emergency Department Visits for Mental Health, Overdose, and Violence Outcomes Before and During the COVID-19 Pandemic. JAMA Psychiatry. 2021;78(4):372. doi: 10.1001/jamapsychiatry.2020.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkinson NS, Rossi N, Moustafa JES, Laverty AA, Quint JK, Freydin MB, et al. Current tobacco smoking and risk from COVID-19: results from a population symptom app in over 2.4 million people. 2020. [DOI] [PubMed]
- Horigian V.E., Schmidt R.D., Feaster D.J. Loneliness, Mental Health, and Substance Use among US Young Adults during COVID-19. Journal of Psychoactive Drugs. 2020;53(1):1–9. doi: 10.1080/02791072.2020.1836435. [DOI] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley EA, Piña K, Cegielski V, Noel-Macdonnell JR, Miller MK. Recovering from substance use disorders during the early months of the COVID-19 pandemic: A mixed-methods longitudinal study of women in Kansas City. Journal of Substance Abuse Treatment. 2021;129:108378. [DOI] [PMC free article] [PubMed]
- Innovation V.H. Melbourne; Australia: 2017. Covidence systematic review software. [Google Scholar]
- Ismael F., Zaramella B., Battagin T., Bizario J., Gallego J., Villela V., et al. Substance Use in Mild-COVID-19 Patients: A Retrospective Study. Frontiers in Public Health. 2021;9:143. doi: 10.3389/fpubh.2021.634396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson S., Brown J., Shahab L., Steptoe A., Fancourt D. COVID-19, smoking and inequalities: a study of 53 002 adults in the UK. Tobacco Control. 2020 doi: 10.1136/tobaccocontrol-2020-055933. 08:tobaccocontrol–2020. [DOI] [PubMed] [Google Scholar]
- Jacob L., Smith L., Armstrong N.C., Yakkundi A., Barnett Y., Butler L., et al. Alcohol use and mental health during COVID-19 lockdown: A cross-sectional study in a sample of UK adults. Drug and Alcohol Dependence. 2021;219:108488. doi: 10.1016/j.drugalcdep.2020.108488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janmohamed K., Soale A.N., Forastiere L., Tang W., Sha Y., Demant J., et al. Intersection of the Web-Based Vaping Narrative With COVID-19: Topic Modeling Study. J Med Internet Res. 2020 Oct;22(10):e21743. doi: 10.2196/21743. http://www.jmir.org/2020/10/e21743/ Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jj Z., Dong X., Yy Cao, Yuan Yd, Yb Yang, Yq Yan, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020 doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- Jones H.E. The challenges of screening for substance use in pregnant women: commentary on the 4P’S plus tool. Journal of Perinatology. 2005;25(6):365–367. doi: 10.1038/sj.jp.7211293. [DOI] [PubMed] [Google Scholar]
- Jones C.M., Olsen E.O., O’Donnell J., Mustaquim D. Resurgent methamphetamine use at treatment admission in the United States, 2008–2017. American Journal of Public Health. 2020;110(4):509–516. doi: 10.2105/AJPH.2019.305527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyce KM, Cameron EE, Sulymka J, Protudjer J, Roos LE. Changes in Maternal Substance Use During the COVID-19 Pandemic. PsyArXiv; 2020. Available from: psyarxiv.com/htny8. [PubMed]
- Joyce A.A., Styklunas G.M., Rigotti N.A., Neil J.M., Park E.R., Kruse G.R. Quit Experiences among Primary Care Patients Enrolled in a Smoking Cessation Pilot RCT Early in the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021;18(3):1011. doi: 10.3390/ijerph18031011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kale D, Herbec A, Perski O, Jackson SE, Brown J, Shahab L. Associations between vaping and Covid-19: cross-sectional findings from the HEBECO study. 2020. [DOI] [PMC free article] [PubMed]
- Kamiński M, Muth A, Bogdański P. Smoking, Vaping, and Tobacco Industry During COVID-19 Pandemic: Twitter Data Analysis. Cyberpsychology, Behavior, and Social Networking. 2020. PMID: 32757951. Available from: https://doi.org/10.1089/cyber.2020.0384. [DOI] [PubMed]
- Kayhan Tetik B., Tekinemre I., Ta¸s S. The Effect of the COVID-19 Pandemic on Smoking Cessation Success. Journal of Community Health. 2020:07. doi: 10.1007/s10900-020-00880-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatri U.G., Pizzicato L.N., Viner K., Bobyock E., Sun M., Meisel Z.F., et al. Racial/Ethnic Disparities in Unintentional Fatal and Nonfatal Emergency Medical Services-Attended Opioid Overdoses During the COVID-19 Pandemic in Philadelphia. JAMA Network Open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.34878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Lucas D.A., Dailey N.S. Alcohol dependence during COVID-19 lockdowns. Psychiatry Research. 2021;296 doi: 10.1016/j.psychres.2020.113676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.U., Majid A., Judge R., Crook P., Nathwani R., Selvapatt N., et al. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. The Lancet Gastroenterology. Hepatology. 2020:08. doi: 10.1016/S2468-1253(20)30251-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klemperer EM, West JC, Peasley-Miklus C, Villanti AC. Change in Tobacco and Electronic Cigarette Use and Motivation to Quit in Response to COVID-19. Nicotine Tobacco Research. 2020 04;22(9):1662–1663. Available from: https://doi.org/10.1093/ntr/ntaa072. [DOI] [PMC free article] [PubMed]
- Koopmann A, Georgiadou E, Kiefer F, Hillemacher T. Did the General Population in Germany Drink More Alcohol during the COVID-19 Pandemic Lockdown? Alcohol and Alcoholism. 2020 06;55(6):698– 699. Available from: https://doi.org/10.1093/alcalc/agaa058. [DOI] [PMC free article] [PubMed]
- Kowitt SD, Cornacchione Ross J, Jarman KL, Kistler CE, Lazard AJ, Ranney LM, et al. Tobacco Quit Intentions and Behaviors among Cigar Smokers in the United States in Response to COVID-19. International journal of environmental research and public health. 2020 July;17(15). Available from: https://europepmc.org/articles/PMC7432467. [DOI] [PMC free article] [PubMed]
- Koyama S., Tabuchi T., Okawa S., Kadobayashi T., Shirai H., Nakatani T., et al. Changes in Smoking Behavior Since the Declaration of the COVID-19 State of Emergency in Japan: A Cross-sectional Study From the Osaka Health App. Journal of Epidemiology. 2021 doi: 10.2188/jea.JE20200533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krawczyk N., Bunting A.M., Frank D., Arshonsky J., Gu Y., Friedman S.R., et al. “How will I get my next week’s script?” Reactions of Reddit opioid forum users to changes in treatment access in the early months of the coronavirus pandemic. International Journal of Drug Policy. 2021 Feb doi: 10.1016/j.drugpo.2021.103140. 103140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar N, Soale AN, Janmohamed K, Sha Y, Forastiere L, Airoldi EM. Global Pandemic May Reduce Levels of Online Misinformation: The Case Of E-Cigarettes; 2020. Available from: https://doi. org/10.17605/OSF.IO/GMCRK.
- Kumar N, Janmohamed K, Soale AN, Forastiere L, Shen C, Verma N, et al. Vaping-related news events and their relationship with online perceptions of vaping: A computational interrupted time series analysis with large-scale public data; 2020. Available from: https://doi.org/10.17605/OSF. IO/HZVJB.
- Kumar N., Howell B.A., Oles W., Janmohamed K., Lee S.T., O’Connor P.G., et al. The role of social network support on treatment outcomes for medication for opioid use disorder: a systematic review. medRxiv. 2020 doi: 10.1016/j.jsat.2021.108367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar N., Janmohamed K., Nyhan K., Martins S.S., Cerda M., Hasin D., et al. Substance use and substance use disorder, in relation to COVID-19: protocol for a scoping review. Systematic Reviews. 2021 Dec;10(1):48. doi: 10.1186/s13643-021-01605-9. Available from: https://systematicreviewsjournal.biomedcentral. com/articles/10.1186/s13643-021-01605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- lechner WV, Laurene KR, Patel S, Anderson M, Grega DR C andKeanne. Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings. , 110, 106527 https://doiorg/. 2020;110. [DOI] [PMC free article] [PubMed]
- Lee B.P., Dodge J.L., Leventhal A., Terrault N.A. Retail Alcohol and Tobacco Sales During COVID-19. Annals of Internal Medicine. 2021 Mar doi: 10.7326/M20-7271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leppla I.E., Gross M.S. Optimizing Medication Treatment of Opioid Use Disorder During COVID-19 (SARS-CoV-2) Journal of Addiction Medicine. 2020 doi: 10.1097/ADM.0000000000000678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D., Croft D.P., Ossip D.J., Xie Z. Are Vapers More Susceptible to COVID-19 Infection? medRxiv. 2020 https://www.medrxiv.org/content/10.1101/2020.05.05.20092379v1 Available from: [Google Scholar]
- Li J., Long X., Zhang Q., Fang X., Li N., Fedorova B., et al. Tobacco Smoking Confers Risk for Severe COVID-19 Unexplainable by Pulmonary Imaging. Journal of Internal Medicine. 2020;289(4):574–583. doi: 10.1111/joim.13190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luk TT, Zhao S, Weng X, Wong JYH, Wu YS, Ho SY, et al. Exposure to health misinformation about COVID-19 and increased tobacco and alcohol use: a population-based survey in Hong Kong. Tobacco Control. 2020. Available from: https://tobaccocontrol.bmj.com/content/early/2020/ 08/27/tobaccocontrol-2020-055960. [DOI] [PubMed]
- Maalouf F.T., Alamiri B., Atweh S., Becker A.E., Cheour M., Darwish H., et al. Mental health research in the Arab region: challenges and call for action. The Lancet Psychiatry. 2019;6(11):961–966. doi: 10.1016/S2215-0366(19)30124-5. [DOI] [PubMed] [Google Scholar]
- Madison M.C., Landers C.T., Gu B.H., Chang C.Y., Tung H.Y., You R., et al. Electronic cigarettes disrupt lung lipid homeostasis and innate immunity independent of nicotine. The Journal of Clinical Investigation. 2019;129(10) doi: 10.1172/JCI128531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahase E. Covid-19: What do we know about “long covid”? bmj. 2020;370. [DOI] [PubMed]
- Mallet J., Dubertret C., Le Strat Y. Addictions in the COVID-19 era: Current evidence, future perspectives a comprehensive review. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2020;110070 doi: 10.1016/j.pnpbp.2020.110070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald D.J., Zhang L., DeHart W.B. The Impact of COVID-19 on Admission Rates for Individuals with Substance Use Disorders. HCA Healthcare Journal of Medicine. 2020;1:433–438. doi: 10.36518/2689-0216.1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGregor S., Henderson K.J., Kaldor J.M. How are health research priorities set in low and middle income countries? A systematic review of published reports. PloS One. 2014;9(10):e108787. doi: 10.1371/journal.pone.0108787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKnight-Eily L.R., Okoro C.A., Strine T.W., Verlenden J., Hollis N.D., Njai R., et al. Racial and Ethnic Disparities in the Prevalence of Stress and Worry, Mental Health Conditions, and Increased Substance Use Among Adults During the COVID-19 Pandemic — United States, April and May 2020. MMWR Morbidity and Mortality Weekly Report. 2021 Feb;70(5):162–166. doi: 10.15585/mmwr.mm7005a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcphee M., Keough M., Rundle S., Heath L., Wardell J., Hendershot C. Depression, Environmental Reward, Coping Motives and Alcohol Consumption During the COVID-19 Pandemic. Frontiers in Psychiatry. 2020;10:11. doi: 10.3389/fpsyt.2020.574676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melamed O.C., Hauck T.S., Buckley L., Selby P., Mulsant B.H. COVID-19 and persons with substance use disorders: Inequities and mitigation strategies. Substance Abuse. 2020;41(3):286–291. doi: 10.1080/08897077.2020.1784363. [DOI] [PubMed] [Google Scholar]
- Mellis A.M., Kelly B.C., Potenza M.N., Hulsey J.N. Trust in a COVID-19 vaccine among people with substance use disorders. Drug and Alcohol Dependence. 2021;220:108519. doi: 10.1016/j.drugalcdep.2021.108519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles L.W., Williams N., Luthy K.E., Eden L. Adult vaccination rates in the mentally ill population: an outpatient improvement project. Journal of the American Psychiatric Nurses Association. 2020;26(2):172–180. doi: 10.1177/1078390319831763. [DOI] [PubMed] [Google Scholar]
- Moise IK, Ruiz MO. Hospitalizations for substance abuse disorders before and after Hurricane Katrina: spatial clustering and area-level predictors, New Orleans, 2004 and 2008. 2016. [DOI] [PMC free article] [PubMed]
- Molfenter T., Roget N., Chaple M., Behlman S., Cody O., Hartzler B., et al. Use of Telehealth in Substance Use Disorder Services During and After COVID-19: Online Survey Study. JMIR Mental Health. 2021;8(2) doi: 10.2196/25835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison A., Polisena J., Husereau D., Moulton K., Clark M., Fiander M., et al. The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. International Journal of Technology Assessment in Health Care. 2012;28(2):138. doi: 10.1017/S0266462312000086. [DOI] [PubMed] [Google Scholar]
- Munn Z., Peters M.D., Stern C., Tufanaru C., McArthur A., Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narasimha V.L., Shukla L., Mukherjee D., Menon J., Huddar S., Panda U.K., et al. Complicated Alcohol Withdrawal-An Unintended Consequence of COVID-19 Lockdown. Alcohol Alcohol. 2020;55(4):350–353. doi: 10.1093/alcalc/agaa042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neill E, Meyer D, Toh WL, van Rheenen TE, Phillipou A, Tan EJ, et al. Alcohol use in Australia during the early days of the COVID-19 pandemic: Initial results from the COLLATE project. Psychiatry and Clinical Neurosciences. 2020;74(10):542–549. Available from: https://onlinelibrary.wiley.com/ doi/abs/10.1111/pcn.13099. [DOI] [PMC free article] [PubMed]
- Niedzwiedz C.L., Green M.J., Benzeval M., Campbell D.D., Craig P., Demou E., et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: Longitudinal analyses of the UK Household Longitudinal Study. Journal of Epidemiology and Community Health. 2020 Sep;75(3):224–231. doi: 10.1136/jech-2020-215060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussbaumer-Streit B., Klerings I., Dobrescu A., Persad E., Stevens A., Garritty C., et al. Excluding non-English publications from evidence-syntheses did not change conclusions: a meta-epidemiological study. Journal of Clinical Epidemiology. 2020;118:42–54. doi: 10.1016/j.jclinepi.2019.10.011. [DOI] [PubMed] [Google Scholar]
- Ornell F., Moura H.F., Scherer J.N., Pechansky F., Kessler F., von Diemen L. The COVID-19 pandemic and its impact on substance use: implications for prevention and treatment. Psychiatry Research. 2020:113096. doi: 10.1016/j.psychres.2020.113096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Acosta P. Virtual raves and happy hours during COVID-19: New drug use contexts for electronic dance music partygoers. International Journal of Drug Policy. 2020;102904 doi: 10.1016/j.drugpo.2020.102904. http://www.sciencedirect.com/science/article/pii/S0955395920302437 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panagiotidis P., Rantis K., Holeva V., Parlapani E., Diakogiannis I. Changes in Alcohol Use Habits in the General Population, during the COVID-19 Lockdown in Greece. Alcohol and Alcoholism. 2020;55(6):702–704. doi: 10.1093/alcalc/agaa092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patanavanich R., Glantz S.A. Smoking is associated with COVID-19 progression: a meta-analysis. Nicotine & Tobacco Research. 2020 doi: 10.1093/ntr/ntaa082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peacock A., Leung J., Larney S., Colledge S., Hickman M., Rehm J., et al. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction. 2018;113(10):1905–1926. doi: 10.1111/add.14234. [DOI] [PubMed] [Google Scholar]
- Perski O., Herbec A., Shahab L., Brown J. Influence of the SARS-CoV-2 Outbreak on the Uptake of a Popular Smoking Cessation App in UK Smokers: Interrupted Time Series Analysis. JMIR Mhealth Uhealth. 2020 doi: 10.2196/19494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters M.D., Marnie C., Tricco A.C., Pollock D., Munn Z., Alexander L., et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evidence Synthesis. 2020;18(10):2119–2126. doi: 10.11124/JBIES-20-00167. [DOI] [PubMed] [Google Scholar]
- Pettigrew S, Jun M, Roberts I, Nallaiah K, Bullen C, Rodgers A. The Potential Effectiveness of COVID-Related Smoking Cessation Messages in Three Countries. Nicotine Tobacco Research. 2021 Mar. [DOI] [PMC free article] [PubMed]
- Pollard M.S., Tucker J.S., Green H.D. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Network Open. 2020;3(9):e2022942. doi: 10.1001/jamanetworkopen.2020.22942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope C., Mays N. Qualitative research: reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. bmj. 1995;311(6996):42–45. doi: 10.1136/bmj.311.6996.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pytell J.D., Rastegar D.A. Down the drain: Reconsidering routine urine drug testing during the COVID-19 pandemic. Journal of Substance Abuse Treatment. 2021;120:108155. doi: 10.1016/j.jsat.2020.108155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radfar SR, De Jong CA, Farhoudian A, Ebrahimi M, Rafei P, Vahidi M, et al. Reorganization of Substance Use Treatment and Harm Reduction Services during the COVID-19 Pandemic: A Global Survey. [DOI] [PMC free article] [PubMed]
- Ramalho R. Alcohol consumption and alcohol-related problems during the COVID-19 pandemic: a narrative review. Australasian Psychiatry. 2020 doi: 10.1177/1039856220943024. 1039856220943024. [DOI] [PubMed] [Google Scholar]
- Reddy R.K., Charles W.N., Sklavounos A., Dutt A., Seed P.T., Khajuria A. The effect of smoking on COVID-19 severity: a systematic review and meta-analysis. Journal of Medical Virology. 2020 doi: 10.1002/jmv.26389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes T., Stimson G.V., Moore D., Bourgois P. Qualitative social research in addictions publishing: Creating an enabling journal environment. The International Journal on Drug Policy. 2010;21(6):441. doi: 10.1016/j.drugpo.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez L.M., Litt D.M., Stewart S.H. Drinking to cope with the pandemic: The unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addictive Behaviors. 2020;110 doi: 10.1016/j.addbeh.2020.106532. Available from: http://www.sciencedirect. com/science/article/pii/S0306460320306626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers A.H., Shepherd J.M., Garey L., Zvolensky M.J. Psychological factors associated with substance use initiation during the COVID-19 pandemic. Psychiatry Research. 2020;293:113407. doi: 10.1016/j.psychres.2020.113407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolland B., Haesebaert F., Zante E., Benyamina A., Haesebaert J., Franck N. Global Changes and Factors of Increase in Caloric/Salty Food Intake, Screen Use, and Substance Use During the Early COVID-19 Containment Phase in the General Population in France: Survey Study. JMIR Public Health and Surveillance. 2020 Sep;6(3) doi: 10.2196/19630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum J., Lucas N., Zandrow G., Satz W.A., Isenberg D., D’Orazio J., et al. Impact of a shelter-in-place order during the COVID-19 pandemic on the incidence of opioid overdoses. The American Journal of Emergency Medicine. 2021;41:51–54. doi: 10.1016/j.ajem.2020.12.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosoff-Verbit Z., Logue-Chamberlain E., Fishman J., Audrain-McGovern J., Hawk L., Mahoney M., et al. The Perceived Impact of COVID-19 among Treatment-Seeking Smokers: A Mixed Methods Approach. International Journal of Environmental Research and Public Health. 2021 Jan;18(2):505–517. doi: 10.3390/ijerph18020505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozanova J., Shenoi S., Zaviryukha I., Zeziulin O., Kiriazova T., Rich K., et al. Social Support is Key to Retention in Care during Covid-19 Pandemic among Older People with HIV and Substance Use Disorders in Ukraine. Substance Use & Misuse. 2020;55(11):1902–1904. doi: 10.1080/10826084.2020.1791183. PMID: 32666857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahu P., Mathur A., Ganesh A., Nair S., Chand P., Murthy P. Acceptance of e-consult for Substance Use Disorders during the COVID 19 pandemic: A study from India. Asian Journal of Psychiatry. 2020;54 doi: 10.1016/j.ajp.2020.102451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salath́e M., Bonhoeffer S. The effect of opinion clustering on disease outbreaks. Journal of The Royal Society Interface. 2008;5(29):1505–1508. doi: 10.1098/rsif.2008.0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saurabh S, Verma MK, Gautam V, Kumar N, Jain V, Goel AD, et al. Tobacco, alcohol use and other risk factors for developing symptomatic COVID-19 vs asymptomatic SARS-CoV-2 infection: a case–control study from western Rajasthan, India. Transactions of The Royal Society of Tropical Medicine and Hygiene. 2021 Jan. [DOI] [PMC free article] [PubMed]
- Scherer R.W., Saldanha I.J. How should systematic reviewers handle conference abstracts? A view from the trenches. Systematic Reviews. 2019;8(1):264. doi: 10.1186/s13643-019-1188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqi K., Siddiqui F., Khan A., Ansaari S., Kanaan M., Khokhar M., et al. The Impact of COVID-19 on Smoking Patterns in Pakistan: Findings From a Longitudinal Survey of Smokers. Nicotine Tobacco Research. 2020 Mar;23(4):765–769. doi: 10.1093/ntr/ntaa207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidor A, Rzymski P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients. 2020 Jun;12(6):1657. Available from: http://dx.doi.org/10.3390/nu12061657. [DOI] [PMC free article] [PubMed]
- Silczuk A. Threatening increase in alcohol consumption in physicians quarantined due to coronavirus outbreak in Poland: the ALCOVID survey. Journal of Public Health. 2020 07;42(3):461–465. Available from: https://doi.org/10.1093/pubmed/fdaa110. [DOI] [PMC free article] [PubMed]
- Silva M.J., Kelly Z. The escalation of the opioid epidemic due to COVID-19 and resulting lessons about treatment alternatives. Am J Manag Care. 2020;26(7):e202–e204. doi: 10.37765/ajmc.2020.43386. [DOI] [PubMed] [Google Scholar]
- Silverstein S.M., Daniulaityte R., Miller S.C., Martins S.S., Carlson R.G. On my own terms: Motivations for self-treating opioid-use disorder with non-prescribed buprenorphine. Drug and Alcohol Dependence. 2020;210:107958. doi: 10.1016/j.drugalcdep.2020.107958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S., Rock P., Bush H.M., Quesinberry D., Walsh S.L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug and Alcohol Dependence. 2020;214:108176. doi: 10.1016/j.drugalcdep.2020.108176. http://www.sciencedirect.com/science/article/pii/S0376871620303410 Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokolovsky A.W., Hertel A.W., Micalizzi L., White H.R., Hayes K.L., Jackson K.M. Preliminary Impact of the COVID-19 Pandemic on Smoking and Vaping in College Students. Addictive Behaviors. 2020 Dec;115 doi: 10.1016/j.addbeh.2020.106783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokolovsky A.W., Hertel A.W., Micalizzi L., White H.R., Hayes K.L., Jackson K.M. Preliminary impact of the COVID-19 pandemic on smoking and vaping in college students. Addictive Behaviors. 2021;115:106783. doi: 10.1016/j.addbeh.2020.106783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sordo L., Barrio G., Bravo M.J., Indave B.I., Degenhardt L., Wiessing L., et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. bmj. 2017;357 doi: 10.1136/bmj.j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton R., To Q.G., Khalesi S., Williams S.L., Alley S.J., Thwaite T.L., et al. Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. International Journal of Environmental Research and Public Health. 2020 Jun;17(11):4065. doi: 10.3390/ijerph17114065. Available from: http://dx.doi.org/10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starks TJ, Jones SS, Sauermilch D, Benedict M, Adebayo T, Cain D, et al. Evaluating the impact of COVID-19: A cohort comparison study of drug use and risky sexual behavior among sexual minority men in the U.S.A. Drug and Alcohol Dependence. 2020;216:108260. Available from: http://www. sciencedirect.com/science/article/pii/S0376871620304257. [DOI] [PMC free article] [PubMed]
- Streck J.M., Kalkhoran S., Bearnot B., Gupta P.S., Kalagher K.M., Regan S., et al. Perceived Risk, Attitudes, and Behavior of Cigarette Smokers and Nicotine Vapers Receiving Buprenorphine Treatment for Opioid Use Disorder during the COVID-19 Pandemic. Drug and Alcohol Dependence. 2021 Nov;218 doi: 10.1016/j.drugalcdep.2020.108438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Mental Health Services Administration. Opioid Treatment Program (OTP) Guidance; 2020.
- Sun Y., Bao Y., Kosten T., Strang J., Shi J., Lu L. Challenges to opioid use disorders during COVID-19. The American Journal on Addictions. 2020;29(3):174. doi: 10.1111/ajad.13031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabo G., Saha B. Alcohol’s effect on host defense. Alcohol Research: Current Reviews. 2015;37(2):159. [PMC free article] [PubMed] [Google Scholar]
- Tai D.B.G., Shah A., Doubeni C.A., Sia I.G., Wieland M.L. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clinical Infectious Diseases. 2020 doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tattan-Birch H, Perski O, Jackson S, Shahab L, West R, Brown J. COVID-19, smoking, vaping and quitting: a representative population survey in England. Addiction. Available from: https: //onlinelibrary.wiley.com/doi/abs/10.1111/add.15251. [DOI] [PMC free article] [PubMed]
- Taylor S., Paluszek M.M., Rachor G.S., McKay D., Asmundson G.J. Substance use and abuse, COVID-19-related distress, and disregard for social distancing: A network analysis. Addictive Behaviors. 2021;114:106754. doi: 10.1016/j.addbeh.2020.106754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teti M., Schatz E., Liebenberg L. SAGE Publications Sage CA; Los Angeles, CA: 2020. Methods in the Time of COVID-19: The Vital Role of Qualitative Inquiries. [Google Scholar]
- Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D., et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of Internal Medicine. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- Tsigaris P., da Silva J.A.T. Smoking Prevalence and COVID-19 in Europe. Nicotine Tobacco Research. 2020;22:1646–1649. doi: 10.1093/ntr/ntaa121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker J.S., D’Amico E.J., Pedersen E.R., Garvey R., Rodriguez A., Klein D.J. Behavioral Health and Service Usage During the COVID-19 Pandemic Among Emerging Adults Currently or Recently Experiencing Homelessness. Journal of Adolescent Health. 2020 Oct;67(4):603–605. doi: 10.1016/j.jadohealth.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner R.M., Bird S.M., Higgins J.P. The impact of study size on meta-analyses: examination of under-powered studies in Cochrane reviews. PloS one. 2013;8(3):e59202. doi: 10.1371/journal.pone.0059202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umucu E., Lee B. Examining the Impact of COVID-19 on Stress and Coping Strategies in Individuals With Disabilities and Chronic Conditions. Rehabilitation Psychology. 2020 May;65(3):193–198. doi: 10.1037/rep0000328. [DOI] [PubMed] [Google Scholar]
- Uscher-Pines L, Sousa J, Raja P, Mehrotra A, Barnett M, Huskamp HA. Treatment of opioid use disorder during COVID-19: Experiences of clinicians transitioning to telemedicine. Journal of Substance Abuse Treatment. 2020;118:108124. Available from: http://www.sciencedirect.com/ science/article/pii/S0740547220303809. [DOI] [PMC free article] [PubMed]
- Uvais NA. Interests in quitting smoking and alcohol during COVID-19 pandemic in India: A Google Trends study. Psychiatry and Clinical Neurosciences. 2020;74(10):550–551. Available from: https: //onlinelibrary.wiley.com/doi/abs/10.1111/pcn.13118. [DOI] [PMC free article] [PubMed]
- Vaillant G.E. Harvard University Press; 2009. The natural history of alcoholism revisited. [Google Scholar]
- Vallecillo G., Perelĺo R., Gu¨erri R., Fonseca F., Torrens M. Clinical Impact of COVID-19 on People with Substance Use Disorders. Journal of Public Health. 2020 Apr;43(1):9–12. doi: 10.1093/pubmed/fdaa181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vardavas C.I., Nikitara K. COVID-19 and smoking: A systematic review of the evidence. Tobacco Induced Diseases. 2020;18 doi: 10.18332/tid/119324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatesan P. COVID-19 diagnostics—not at the expense of other diseases. The Lancet Microbe. 2020;1(2):e64. doi: 10.1016/S2666-5247(20)30041-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindrola-Padros C., Chisnall G., Cooper S., Dowrick A., Djellouli N., Symmons S.M., et al. Carrying Out Rapid Qualitative Research During a Pandemic: Emerging Lessons From COVID-19. Qualitative Health Research. 2020 doi: 10.1177/1049732320951526. 1049732320951526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlahov D., Galea S., Resnick H., Ahern J., Boscarino J.A., Bucuvalas M., et al. Increased use of cigarettes, alcohol, and marijuana among Manhattan, New York, residents after the September 11th terrorist attacks. American Journal of Epidemiology. 2002;155(11):988–996. doi: 10.1093/aje/155.11.988. [DOI] [PubMed] [Google Scholar]
- Volkow N.D. Collision of the COVID-19 and Addiction Epidemics. Annals of Internal Medicine. 2020;173(1):61–62. doi: 10.7326/M20-1212. PMID: 32240293. Available from: https://doi.org/10.7326/M20-1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N.D., Blanco C. Research on substance use disorders during the COVID-19 pandemic. Journal of Substance Abuse Treatment. 2021;129:108385. doi: 10.1016/j.jsat.2021.108385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlund T., Mataix-Cols D., Lauri K.O., de Schipper E., Lj́otsson B., Aspvall K., et al. Brief online cognitive behavioural intervention for dysfunctional worry related to the COVID-19 pandemic: a randomised controlled trial. Psychotherapy and Psychosomatics. 2021;90(3):191–199. doi: 10.1159/000512843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker P.G., Whittaker C., Watson O.J., Baguelin M., Winskill P., Hamlet A., et al. The impact of COVID-19 and strategies for mitigation and suppression in low-and middle-income countries. Science. 2020 doi: 10.1126/science.abc0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q.Q., Kaelber D.C., Xu R., Volkow N.D. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Molecular Psychiatry. 2020 doi: 10.1038/s41380-020-00880-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell JD, Kempe T, Rapinda KK, Single A, Bilevicius E, Frohlich JR, et al. Drinking to Cope During COVID-19 Pandemic: The Role of External and Internal Factors in Coping Motive Pathways to Alcohol Use, Solitary Drinking, and Alcohol Problems. Alcoholism: Clinical and Experimental Research. 2020;44(10):2073–2083. Available from: https://onlinelibrary.wiley.com/doi/abs/ 10.1111/acer.14425. [DOI] [PubMed]
- Westrupp E.M., Bennet C., Berkowitz T., Youssef G.J., Toumbourou J.W., Tucker R., et al. Comparison to pre-pandemic data; 2020. and family mental health and functioning in Australia during COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A.M., Li D., Snell L.M., O’Connor R., Hoetger C., Croft D., et al. Perceptions of tobacco product-specific COVID-19 risk and changes in tobacco use behaviors among smokers, e-cigarette users, and dual users. Nicotine & Tobacco Research. 2021 doi: 10.1093/ntr/ntab053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wj Guan, Zy Ni, Hu Y., Liang Wh, Cq Ou, Jx He, et al. Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiaolu R., Wenwen W., Ali R., Xu L., Hong W., Min Z., et al. Feasibility of studying a brief intervention to help Chinese villagers with problem alcohol use after an earthquake. Alcohol and Alcoholism. 2017;52(4):472–476. doi: 10.1093/alcalc/agx014. [DOI] [PubMed] [Google Scholar]
- Yach D. Tobacco Use Patterns in Five Countries During the COVID-19 Lockdown. Nicotine. Tobacco Research. 2020;22(9):1671–1672. doi: 10.1093/ntr/ntaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yazdi K, Fuchs-Leitner I, Rosenleitner J, Gerstgrasser NW. Impact of the COVID-19 Pandemic on Patients With Alcohol Use Disorder and Associated Risk Factors for Relapse. Frontiers in Psychiatry. 2020 Dec;11. [DOI] [PMC free article] [PubMed]
- Yehudai M., Bender S., Gritsenko V., Konstantinov V., Reznik A., Isralowitz R. COVID-19 Fear, Mental Health, and Substance Misuse Conditions Among University Social Work Students in Israel and Russia. International Journal of Mental Health and Addiction. 2020;6:1–8. doi: 10.1007/s11469-020-00360-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon S., Odlum M., Broadwell P., Davis N., Cho H., Deng N., et al. Application of social network analysis of COVID-19 related tweets mentioning cannabis and opioids to gain insights for drug abuse research. Studies in health technology and informatics. 2020;272:5. doi: 10.3233/SHTI200479. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7337407/ [DOI] [PMC free article] [PubMed] [Google Scholar]
References
Further reading
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed are available from the corresponding author on reasonable request.