Abstract
Purpose
This study assessed the prevalence of turnover intention and explored associated factors on turnover intention among healthcare workers during the COVID-19 pandemic in China.
Methods
An institutional-based cross-sectional study was conducted from July to February 13th to 20th, 2020, in 31 provinces of mainland China. A total of 1403 healthcare workers were recruited. Hierarchical logistic regressions were used to identify potential factors associated with turnover intention among Chinese health care workers.
Results
The prevalence of turnover intention among healthcare workers was 10.1% during the COVID-19 pandemic in China. Results of hierarchical regression revealed that working in Grade II hospital (OR = 1.78), technician (OR = 0.30), daily working hours over 12 h (OR = 2.92), frequency of mask replacement between 4 and 8 h (OR = 3.51), refuse volunteer to frontline (OR = 1.68), patient–physician relation unchanged (OR = 1.73), depression (OR = 2.21) and lower social support (OR = 1.75) were significantly associated with the risk of turnover intention. Additionally, healthcare worker’s psychosocial syndemic (OR = 6.13) was positively associated with turnover intention.
Conclusion
Turnover intention is relatively prevalent among healthcare workers during the COVID-19 pandemic in China, and the factors contributing to turnover intention were complex and varied. Early screening of high-risk groups for turnover intention among healthcare workers and more psychosocial health care and physical protection are needed during the COVID-19 pandemic in China.
Keywords: COVID-19, healthcare workers, turnover intention, China
Introduction
In December 2019, a novel coronavirus, named Coronavirus disease 2019 (COVID-19) with unknown origin broke out in Wuhan, the capital city of Hubei province in China.1 Due to its widespread infectiousness and high rate of infection, it has posed a major threat to national public health. According to Nature, COVID-19 has met the necessary epidemiological criteria 2 for declaring a pandemic.2 Globally, as of July 2021, there have been more than 180 million people confirmed cases of COVID-19, including more than 4 million deaths.3 Besides, the disease can cause blood-stream, urinary infections and other secondary infections, which makes the prevention and treatment of various regions are facing a huge burden.4
COVID-19 pandemic is an unprecedented challenge for the world. Healthcare workers, the main force in the fight against the pandemic, are at greater risk than others.5 A recent systematic review indicated the Infection rates among healthcare workers were 10.1%,6 while Spain reported 20.4%7 of confirmed COVID-19 cases were HCW, which suggested that healthcare workers are more likely to be infected with COVID-19 than non-healthcare workers.6,8 A sense of frustration and helplessness occurred in healthcare professionals due to the sudden role reversal from a healthcare provider to the COVID-19 confirmed or suspected patient potentially.9 Studies have found that during the COVID-19 pandemic, healthcare workers are under both physical and mental stress,10–12 from 2.2% to 14.5% of health care workers suffered from severe stress, anxiety and depression.13 Similarly, during the SARS period, the incidence of mental problems among healthcare workers increased significantly.14 The negative data reported by social media may erode public trust and aggravate healthcare worker’s psychological pressure.15,16 Healthcare workers work in an environment of high intensity, high pressure and full of stress, which makes them more prone to fatigue and produces psychological disorders than the general population, and even serious turnover intention.11,15
Turnover intention refers to the probability that an employee voluntarily leaves his or her job in the period ahead17 and was considered to be the strongest predictor of actual leaving or actual turnover among healthcare personnel.18 The high rate of turnover intention in healthcare workers has become an obstacle in the development of the healthcare system, especially during COVID-19 period.19 In normal times, 55.2% of Iraqi doctors,20 35.5% nurses in Italy21 and 30.5% doctors in South Korea22 reported intend to leave their jobs due to working and security conditions,20 poor work environment21 and perceived threats.22 During the pandemic, multiple studies showed that 76.9%23 and 52%24 of healthcare workers had low willingness to work due to psychosocial pressure,23 confidence in workplace safety.24 This is consistent with previous findings that turnover intentions of healthcare workers during COVID-19 were higher than turnover before COVID-19.25 Moreover, long working hours,26 nurses,27 income change,28 and lack of proper protective equipment29 can also lead to healthcare worker’s turnover intention during COVID-19 period. Physician turnover can lead to unsatisfactory patient expectations and lower patient satisfaction, thus significantly affecting the quality of medical care and facility management.30 To ensure the stability of the physician team during COVID-19 period,19 measures to prevent turnover are necessary.31
COVID-19 and the turnover intention of healthcare workers have become major challenges, placing a heavy burden on society.32 It is of great significance to understand the relation between COVID-19 and turnover intention. Therefore, the purpose of this study is to analyze the current situation and influencing factors of healthcare worker’s turnover intention during COVID-19 pandemic in China, to provide an objective basis for preventing the turnover phenomenon in the context of COVID-19 and protecting the mental health of healthcare workers.
Methods
Procedure and Participants
This cross-sectional study was conducted among Chinese healthcare workers in 31 provinces, China, from February 13th to 20th, 2020. Face-to-face investigation during this emergency period is extremely challenging so that we carry out an anonymous online survey among Chinese healthcare workers. We used respondent-driven sampling to recruit samples. Three healthcare workers (also known as seeds) were selected from major tertiary healthcare institutions in Hubei, Jiangsu, and Shanxi provinces. The anonymous questionnaire was conducted by WeChat, one of the largest social applications in China. We excluded the incomplete or nonconforming questionnaires (answer time less than 100 seconds, the same IP address) for quality control. A total of 1435 healthcare workers were interviewed, while 2% of people declined to complete the questionnaire. Finally, 1403 participants completed the questionnaire. Eligible participants included doctors, nurses, CDC, pharmacists, technicians, etc.
This study received ethical approval from the Medical Ethics Committee of Xuzhou Medical University and it was conducted in accordance with the Declaration of Helsinki.
Measures
Turnover Intention
A single item (yes or no) was being used to measure turnover intention: “Have you considered leaving your current job within a month?”
Mental Health Problems
Mental health problems were assessed by using Chinese-language validated Depression Anxiety Stress Scale −21 (DASS-21).33 The scale consists of three subscales, depression (eg, “I couldn’t seem to experience any positive feeling at all”), anxiety (eg, “I was aware of dryness of my mouth”) and stress (eg, “I find it hard to wind down”). Each subscale was measured by seven items and rated on a 4-point Likert scale (0 = did not apply to me at all, 3 = applied to me very much or most of the time). The higher the score, the more negative the emotional states in the past week. The following cut-off scores are used for each subscale: depression (DASS-depression >9), anxiety (DASS-anxiety >7), and stress (DASS-stress >14).34 In this study, Cronbach’s α values of depression (0.861), anxiety (0.918) and stress subscales (0.912) were all acceptable.
Perceived Social Support
A 12-item perceived Social Support (PSS)35 Scale was used to assess social support. The scale consists of three subscales, which Including support from families (eg, “My family really tries to help me”), friends (eg, “My friends really try to help me”), and significant others (eg, “There is a person who is around when I am in need”) (four items per subscale). Each item was evaluated by a 7-point Likert scale (1 = strongly disagree, 7 = strongly agree). The total score of social support is the cumulative score of all subscales, with higher score indicating greater social support.
Covariates
Sociodemographic characteristics (age, gender, risk zone, education, organization, marital status, working at a designated hospital for COVID-19, job type, technical title, working time, and self-rated health), COVID-19 pandemic related factors (frequency of mask replacement, trained for COVID-19, time spent on COVID-19 news each day, volunteer to the frontline, concerned about income being affected by COVID-19, household transmission-related fears), Patient-physician related factors (discriminated against for nature of their job, medical workplace violence and patient–physician relations) and Psychosocial factors (depression, anxiety, pressure and social support) were considered in our study.
Statistical Analysis
All variables were treated as categorical variables which expressed as percentages. Bivariate logistic regression was performed to detect the potential risk factors associated with turnover intention. We also create a syndemic count variable by counting the number of psychosocial problems of each participant and allocating participants into different groups based on the number of their syndemic variables.
Hierarchical regression models were used for robustness checks by using the variables that were at least marginally significant (p<0.05) in the bivariate analysis. Model (1) consisted of only sociodemographic characteristics. Model (2) also included COVID-19 pandemic related factors. We combined patient-physician related factors in Model (3). Finally, we added psychosocial factors in Model (4). We documented the Nagelkerke’s R2 for each model to evaluate goodness of fit. All statistical tests 2 sides, evaluated as significant at the p<0.05 level. All statistical analysis were performed by using SPSS (version 23.0 for Windows; IBM SPSS Statistics, Armonk, NY, USA) software.
Results
Participant Sociodemographic Characteristics
The sociodemographic characteristics of the healthcare workers are summarized in Table 1. Of all the participants, the ages ranged from 20 to 60 years, with 82.1% of the participants being younger than 40 years old. The majority of respondents were females (68.4%), married (69.9%), doctor (60.2%), and worked in Grade III hospitals (72.7%). In addition, 58.4% of participants working in a designated hospital for COVID-19 and the majority (76.4%) of participants lived in middle-risk areas. Furthermore, half of participants were employed with a bachelor’s degree or higher level of education (54.3%) and with an elementary professional title (43.3%).
Table 1.
Sociodemographic Characteristics (n = 1403)
| Characteristics | Frequency | Row % |
|---|---|---|
| Gender | ||
| Male | 444 | 31.6 |
| Female | 959 | 68.4 |
| Age (years) | ||
| 20–29 | 446 | 31.8 |
| 30–39 | 706 | 50.3 |
| 40–49 | 182 | 13.0 |
| 50–59 | 69 | 4.9 |
| Risk zone | ||
| Low-risk area | 192 | 13.7 |
| Medium risk area | 1072 | 76.4 |
| High-risk area | 139 | 9.9 |
| Work at a designated hospital for COVID-19 | ||
| Yes | 819 | 58.4 |
| No | 584 | 41.6 |
| Organization | ||
| Grade III hospital | 1020 | 72.7 |
| Grade II hospital | 180 | 12.8 |
| Basic medical institution | 95 | 6.8 |
| Infectious hospital | 8 | 0.6 |
| Others | 100 | 7.1 |
| Marital status | ||
| Never married | 403 | 28.7 |
| Married | 981 | 69.9 |
| Divorced | 17 | 1.2 |
| Widowed | 2 | 0.1 |
| Education | ||
| Junior college | 98 | 7.0 |
| Bachelor | 762 | 54.3 |
| Master | 471 | 33.6 |
| Doctor | 72 | 5.1 |
| Job type | ||
| Doctor | 845 | 60.2 |
| Nurse | 344 | 24.5 |
| Technician | 92 | 6.6 |
| Pharmacist | 18 | 1.3 |
| CDC | 13 | 0.9 |
| Others | 91 | 6.5 |
| Technical title | ||
| None | 123 | 8.8 |
| Elementary | 608 | 43.3 |
| Intermediate | 459 | 32.7 |
| Senior | 213 | 15.2 |
Potential Factors Associated with Turnover Intention
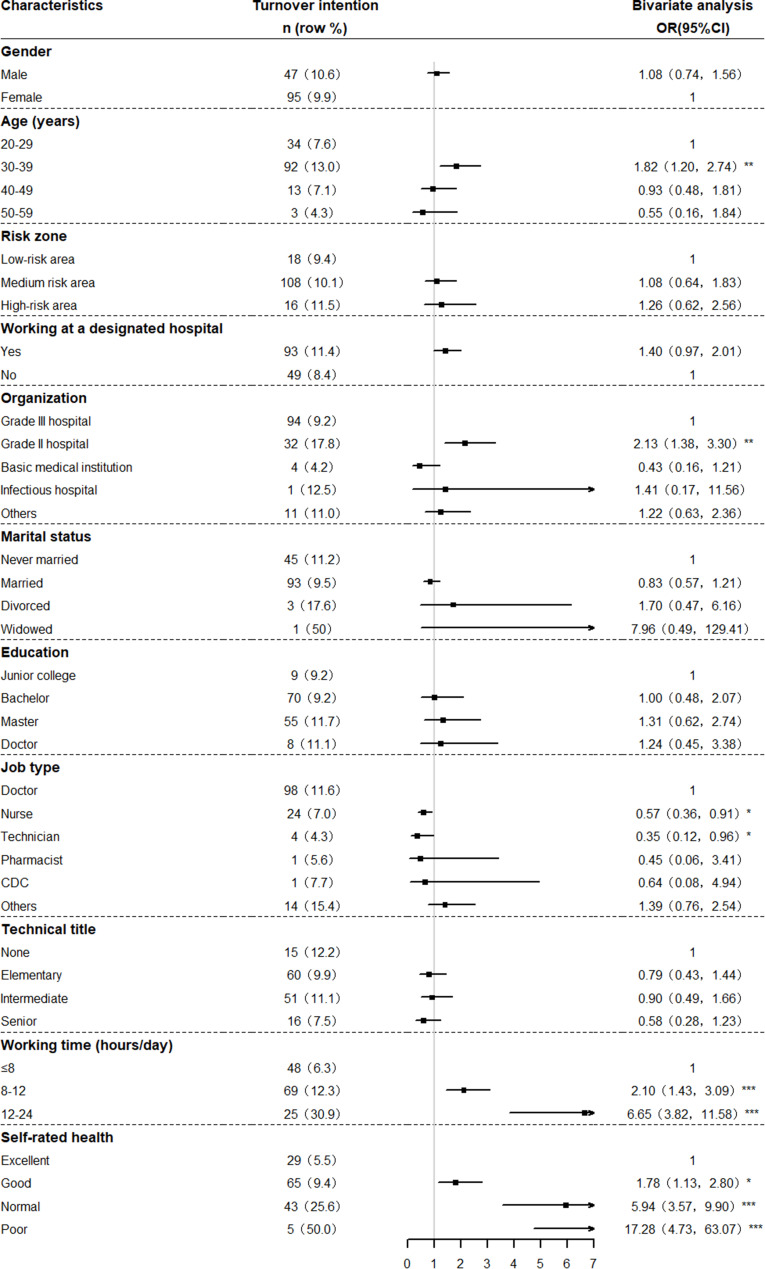
In the bivariate analysis, five sociodemographic characteristics (age, organization, job type, daily working hours, self-rated health) were significant with turnover intention among healthcare workers (p < 0.05). The older-aged group (30–39 years of age) were 1.82 times more likely (OR = 1.82, 95% CI = 1.20–2.74) to have turnover intention compared with the younger aged group (20–29 years of age). Healthcare workers who worked in a Grade II hospital (OR = 2.13, 95% CI = 1.38–3.30) were predictive of greater vulnerability to turnover intention compared with those who worked in Grade III hospitals. Nurses (OR = 0.57, 95% CI = 0.36–0.91) and technicians (OR = 0.35, 95% CI = 0.12–0.96) demonstrated a substantial decrease in turnover intention compared with doctors. In addition, participants with longer work hours (ORs = 2.10 and 6.65, respectively) or worse self-rated health (ORs = 1.78, 5.94 and 17.28, respectively) also at higher risk of turnover intention (Figure 1).
Figure 1.
Sociodemographic characteristics by turnover intention (n = 1403).
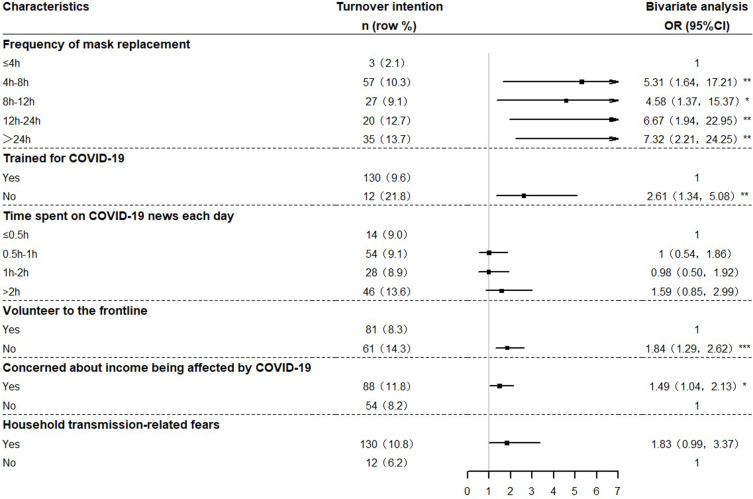
Replacing masks over 4 h (ORs = 5.31, 4.58, 6.67 and 7.32, respectively) and healthcare workers who refused volunteer to frontline (OR = 1.84, 95% CI = 1.29–2.62) were more likely to have turnover intention. Healthcare workers who were not trained for COVID-19 (OR = 2.61, 95% CI = 1.34–5.08), worried about household transmission (OR = 1.83, 95% CI = 0.99–3.37) and income change (OR = 1.49, 95% CI = 1.04–2.13) were also significantly associated with severe turnover intention (Figure 2).
Figure 2.
COVID-19 pandemic related factors by turnover intention (n = 1403).
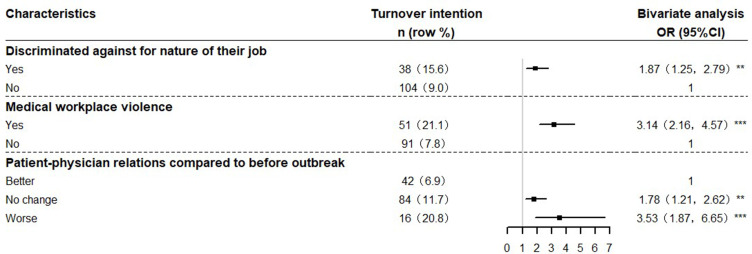
Figure 3 shows that all patient-physician related factors were found to have a significant association with turnover intention. The patient–physician relation unchanged (OR = 1.78, 95% CI = 1.21–2.62) and worse group (OR = 3.53, 95% CI = 1.87–6.65) were more likely to have turnover intention compared with the better patient–physician relation group. Healthcare workers discriminated against for nature of their job (OR = 1.87, 95% CI = 1.25–2.79) and experienced medical workplace violence during the pandemic (OR = 3.14, 95% CI = 2.16–4.57) demonstrated a substantial increase in turnover intention.
Figure 3.
Patient-physician related factors by turnover intention (n = 1403).
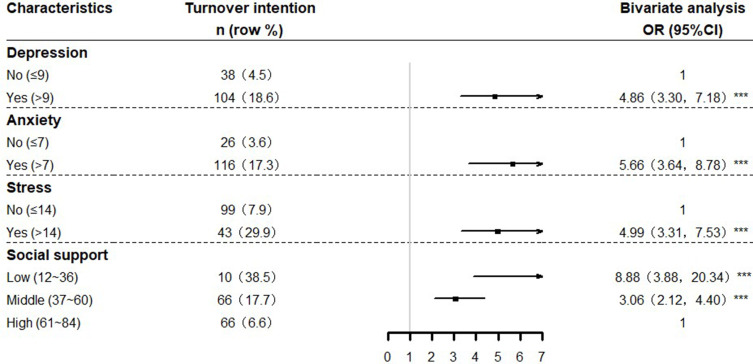
The results from the bivariate analysis among psychosocial factors indicated that healthcare workers who perceived lower level of social support (ORs = 3.06 and 8.88, respectively). Healthcare workers with depressive symptoms (OR = 4.86, 95% CI = 3.30–7.18), anxiety (OR = 5.66, 95% CI =3.64–8.78) and stress (OR = 4.99, 95% CI = 3.31–7.53) were at higher risk of turnover intention (Figure 4).
Figure 4.
Psychosocial factors by turnover intention (n = 1403).
Factors Associated with Turnover Intention in Hierarchical Regression
Table 2 presents the results from the hierarchical regression models. Model (1) showed that among healthcare workers, worked in a Grade II hospital (OR = 1.77, 95% CI = 1.10–2.86), working hours between 12 and 24 h (OR = 3.42, 95% CI = 1.80–6.51), and worse self-rated health (ORs = 1.66, 4.17, and 13.06, respectively) demonstrated a substantial increase in turnover intention. Additionally, technicians were less likely (OR = 0.34, 95% CI = 0.11–0.99) to have turnover intention compared with the doctor. Model (2) demonstrated that the frequency of each mask change is between 4 and 8 h (OR = 3.82, 95% CI = 1.15–12.71) or more than 24 h (OR = 4.03, 95% CI = 1.17–13.85), not trained for COVID-19 (OR = 2.44, 95% CI = 1.12–5.36) and not volunteered to a frontline job (OR = 1.89, 95% CI = 1.26–2.81) were significantly associated with increased odds of having a turnover intention. Model (3) showed that healthcare workers who experienced medical workplace violence during the pandemic (OR = 1.99, 95% CI = 1.27–3.09) and patient–physician relation unchanged (OR = 1.78, 95% CI = 1.15–2.68) demonstrated a substantial increase in turnover intention. In this model, technician and aaily working hours between 8 and 12 h were no longer significant. When Psychosocial factors were combined in Model (4), the effects of self-rated health, frequency of mask replacement over 24 h, trained for COVID-19 and medical workplace violence were no longer significant, and the medical technician (OR = 0.30, 95% CI = 0.09–0.93), high-level of depression (OR = 2.21, 95% CI =1.31–3.71) and mid-level of social support (OR = 1.75, 95% CI = 1.14–2.67) were significantly associated with lower or higher odds of having a turnover intention. However, the effects of several factors in the previous model (self-rated health, frequency of mask replacement over 24 h, trained for COVID-19 and medical workplace violence) were no longer significant, Model (4) including all candidate variables, and the rose of Nagelkerke’s R2 from 0.156 to 0.288, indicating a relatively good fit for the model.
Table 2.
Association Between Sociodemographic Characteristics and COVID-19 Pandemic-Related Factors, Patient-Physician Related Factors, and Psychosocial Factors (Presented as Odds Ratios (OR)) (n = 1403)
| Characteristics | Model (1) | Model (2) | Model (3) | Model (4) |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Sociodemographic | ||||
| Age (years) | ||||
| 20–29 | Reference | |||
| 30–39 | 1.38 (0.88,2.16) | 1.41 (0.89,2.23) | 1.48 (0.93,2.37) | 1.46 (0.90,2.37) |
| 40–49 | 0.72 (0.36,1.47) | 0.76 (0.37,1.57) | 0.84 (0.40,1.75) | 0.79 (0.37,1.70) |
| 50–59 | 0.39 (0.11,1.37) | 0.50 (0.14,1.76) | 0.63 (0.18,2.23) | 0.62 (0.17,2.25) |
| Organization | ||||
| Grade III hospital | Reference | |||
| Grade II hospital | 1.77 (1.10,2.86) * | 1.93 (1.19,3.15) ** | 1.87 (1.14,3.08) * | 1.78 (1.06,2.97) * |
| Basic medical institution | 0.36 (0.12,1.06) | 0.42 (0.14,1.24) | 0.36 (0.12,1.08) | 0.35 (0.11,1.06) |
| Infectious hospital | 1.64 (0.18,15.07) | 1.48 (0.14,16.2) | 2.03 (0.18,22.9) | 1.69 (0.13,21.27) |
| Others | 1.00 (0.46,2.15) | 0.97 (0.44,2.16) | 0.85 (0.38,1.90) | 0.89 (0.39,2.05) |
| Job type | ||||
| Doctor | Reference | |||
| Nurse | 0.67 (0.41,1.11) | 0.75 (0.45,1.27) | 0.83 (0.49,1.40) | 0.81 (0.47,1.39) |
| Technician | 0.34 (0.11,0.99) * | 0.32 (0.11,0.97) * | 0.34 (0.11,1.03) | 0.30 (0.09,0.93) * |
| Pharmacist | 0.44 (0.05,3.58) | 0.37 (0.04,3.03) | 0.33 (0.04,2.83) | 0.36 (0.04,3.07) |
| CDC | 0.66 (0.07,5.94) | 0.55 (0.06,5.37) | 0.73 (0.07,7.54) | 0.49 (0.04,5.63) |
| Others | 1.47 (0.71,3.03) | 1.14 (0.53,2.45) | 1.4 (0.64,3.05) | 1.24 (0.55,2.80) |
| Working time (hours/day) | ||||
| ≤8 | Reference | |||
| 8–12 | 1.50 (0.99,2.27) | 1.57 (1.02,2.40) * | 1.53 (0.99,2.37) | 1.38 (0.88,2.15) |
| 12–24 | 3.42 (1.80,6.51) *** | 4.32 (2.21,8.45) *** | 3.71 (1.85,7.43) *** | 2.92 (1.41,6.04) ** |
| Self-rated health | ||||
| Excellent | Reference | |||
| Good | 1.66 (1.04,2.65) * | 1.61 (1.00,2.60) * | 1.53 (0.95,2.48) | 1.22 (0.73,2.02) |
| General | 4.17 (2.41,7.24) *** | 3.70 (2.10,6.51) *** | 2.93 (1.63,5.24) *** | 1.75 (0.95,3.25) |
| Poor | 13.06 (3.09,55.12) *** | 10.97 (2.61,46) ** | 7.40 (1.59,34.50) * | 4.86 (0.95,24.84) |
| Pandemic related factors | ||||
| Frequency of mask replacement | ||||
| ≤4h | Reference | |||
| 4–8h | 3.82 (1.15,12.71) * | 3.99 (1.18,13.47) * | 3.51 (1.03,12.03) * | |
| 8–12h | 2.41 (0.69,8.42) | 2.59 (0.73,9.19) | 2.27 (0.63,8.10) | |
| 12–24h | 3.34 (0.92,12.15) | 3.52 (0.95,13.01) | 2.80 (0.75,10.52) | |
| >24h | 4.03 (1.17,13.85) * | 4.40 (1.26,15.33) * | 3.35 (0.95,11.82) | |
| Trained for COVID-19 | ||||
| Yes | Reference | |||
| No | 2.44 (1.12,5.36) * | 2.43 (1.09,5.41) * | 2.25 (0.96,5.25) | |
| Volunteer to the frontline | ||||
| Yes | Reference | |||
| No | 1.89 (1.26,2.81) ** | 1.84 (1.23,2.76) ** | 1.68 (1.10,2.56) * | |
| Concerned about income being affected by COVID-19 | ||||
| Yes | 1.46 (0.99,2.17) | 1.36 (0.91,2.03) | 1.23 (0.81,1.86) | |
| No | Reference | |||
| Patient-physician related factors | ||||
| Discriminated against for nature of their job | ||||
| Yes | 1.21 (0.76,1.94) | 0.93 (0.57,1.52) | ||
| No | Reference | |||
| Medical workplace violence | ||||
| Yes | 1.99 (1.27,3.09) ** | 1.51 (0.95,2.39) | ||
| No | Reference | |||
| Patient-physician relations compared to before | ||||
| Better | Reference | |||
| No change | 1.76 (1.15,2.68) ** | 1.73 (1.12,2.67) * | ||
| Worse | 1.80 (0.85,3.83) | 1.59 (0.73,3.48) | ||
| Social psychological factors | ||||
| Depression | ||||
| No | Reference | |||
| Yes | 2.21 (1.31,3.73) ** | |||
| Anxiety | ||||
| No | Reference | |||
| Yes | 1.73 (0.97,3.08) | |||
| Stress | ||||
| No | Reference | |||
| Yes | 1.39 (0.82,2.33) | |||
| Social support | ||||
| Low | 3.45 (1.24,9.62) ** | |||
| Middle | 1.75 (1.14,2.67) ** | |||
| High | Reference | |||
| Nagelkerke’s R2 | 0.156 | 0.197 | 0.223 | 0.288 |
Notes: Model (1): Sociodemographic. Model (2): Sociodemographic + COVID-19 Pandemic related factors. Model (3): Sociodemographic + COVID-19 Pandemic related factors + Patient-physician related factors. Model (4): Sociodemographic + COVID-19 Pandemic related factors + Patient-physician related factors + Psychosocial factors. *P<0.05. **P<0.01. ***P<0.001.
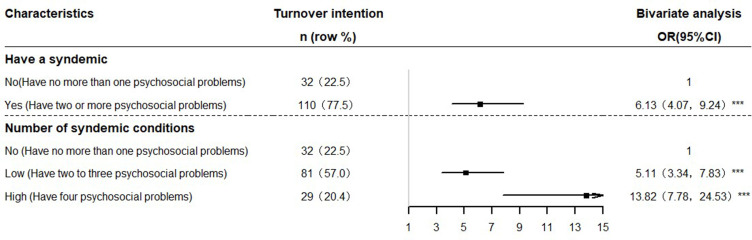
Syndemic Effect of Psychosocial Variables
Final syndemic analysis results are presented in Figure 5. 77.5% of participants suffered from a psychosocial syndemic (having two or more psychosocial problems). It was found that a psychosocial syndemic had a magnifying effect on turnover intention (OR = 6.13, 95% CI 4.07–9.24). When the number of syndemic factors was divided into the non-syndemic (having no more than one psychosocial health problems), low-level syndemic (having two or three psychosocial health problems) and high-level syndemic (having four or five psychosocial health problems). We found that low-level syndemic group and high-level syndemic group were more likely to have turnover intention than the non-syndemic group (OR = 5.11, 95% CI 3.34–7.83; OR = 13.82, 95% CI 7.78–24.53, respectively).
Figure 5.
Associations between the number of syndemic conditions and turnover intention among healthcare workers.
Discussion
Deadly pandemics and large-scale pandemics have challenged human existence throughout history.36 Healthcare workers plays a central role in confronting with a COVID-19 pandemic. Human resources are the most important asset in the health system and are essential to improve the quality of health care services.37 In this survey, we found that 10.1% of the healthcare workers have turnover intention. The turnover intention of healthcare workers in the context of COVID-19 is consistent with the research results of South Korea (8%),22 but significantly lower than that of healthcare workers in the ordinary period.38,39 This is because our survey was conducted at the beginning of the pandemic, so the turnover intention of healthcare workers in this period was lower than a long-term turnover intention in normal period. Our findings are helpful to better understand the factors associated with healthcare worker’s turnover intention during COVID-19 period thus contributing to the protection of the loss of medical human resources, which is the main force against COVID-19.
Sociodemographic Characteristics on Turnover Intention
Our results revealed that Grade II hospitals are 1.78 times more likely to have turnover intention than Grade III hospital. Recent studies have shown that the medical resources of Grade III hospitals are more abundant, and human resources and equipment in Grade II hospitals are more urgent than those in Grade III hospitals.40 We speculate that during the COVID-19 pandemic, with a large number of patients, the healthcare workers in Grade II hospitals are under great pressure due to the shortage of staff or medical resources, which leads to the willingness to leave. Similarly, the lack of human resources will also lead to longer working hours. Netherlands, Germany, and Belgium studies have shown that working-time-related factors significantly affect intention to stay.41 During the pandemic, the workload of healthcare workers working overtime can not only increase the willingness of doctors to leave their existing professions but also cause the increase in unnecessary management costs, endanger the continuity of patient care, and even threaten the function of the healthcare system.
Besides, different job types can also account for the difference in turnover intention. Among participants, doctors are more likely to have turnover intention than technicians. Healthcare workers are front-line soldiers in the fight against the pandemic. They are faced with isolation, high transmission risk and long duty,42,43 which also makes the higher incidence of mental illness and job burnout for clinicians.44 Most technicians work in the second line, which reduces the chance of having direct contact with patients and is less likely to be infected. Their mental health problems are much lower than that of clinicians, and the turnover intention is relatively less.45,46
COVID-19 Pandemic Related Factors on Turnover Intention
Participants who change their masks for longer periods of time are more likely to have turnover intention. We assumed that a shortage of personal protective equipment (PPE) may explain the increased turnover intention. Severe shortage of PPE is mainly due to high demand and abuse of PEE, causing a threat to the healthcare workers lives.47 A large number of healthcare workers have died of COVID-19 due to lack of PPE,48–50 while others continue to struggle with the pandemic.51 Many doctors are performing their duty without any PPE and are at high risk of becoming infected,52 leading to increased willingness to leave their jobs.53 Our study found that people who did not volunteer to front-line were more likely to have a willingness to have turnover intention. Volunteer service can enable participants to enrich their social life, gain a sense of mental health, and benefit others.54 Those people who did not volunteer to front-line work have a strong sense of self-protection and lack a certain dedication spirit. It is necessary to strengthen professional responsibility education.
Patient-Physician Related Factors on Turnover Intention
Patient–physician relation is a complex psychosocial interplay of vulnerability, trust, and authority in a professional setting.55 Psychologically, people feel unsafe, uneasy, and anxious when the living environment changes56. Close-minded attitudes and rumors can also flourish when the cause of a pandemic is not clear.57 Anxiety, nervousness, fear and other psychological states will lead to a decrease in patients’ trust in healthcare workers, leading to workplace violence against doctors in the workplace.58 There is an urgent need to improve the patient–physician relations to reduce the occurrence of workplace violence and thus reduce the turnover intention of healthcare workers.59
Psychosocial Factors on Turnover Intention
In addition, we found that among the psychosocial factors, depression, and a low level of social support were associated with an increased incidence of turnover intention. Healthcare workers with turnover intention were frequently reported with significant depressive symptoms.60,61 Previous studies have established the relations between psychological status and turnover intention, including depression, fear, anxiety, and perceived threat.62–64 The reasons for the psychological problems of healthcare workers during COVID-19 are complex: high risk of infection, high intensity of work, isolation from family members, and lack of protective equipment may all lead to depression of healthcare workers.65 However, the effects of anxiety and stress were insignificant in the multivariate analysis, and we speculated that this was because anxiety and stress acted through depression, and the effects of anxiety and stress were offset by depression. Therefore, it is necessary to take measures to prevent the depression,66 thus reducing turnover intention. Unfortunately, the rapid human-to-human transmission of COVID-19 prevents traditional face-to-face psychological interventions.67 Increased and more widely available services, such as telephone hotlines, online counseling, and regular psychological counseling for psychosocial problems among healthcare workers, are desperately needed. Accordingly, lack of adequate social support is also identified as a hazard factor for turnover intention. A high level of social support can effectively reduce anxiety and stress.68–70 29–35% of hospital staff suffered from high emotional disturbance during the SARS pandemic.71 Furthermore, some studies show that social support also plays a critical role in the psychological regulation of depression patients, and there is a strong negative correlation between the high level of social support and depressive disorder.72,73 Thus, social support may have an indirect and significant correlations with turnover intention through mental health status.74 A high level of social support can reduce health care workers’ turnover intention by alleviate psychological problems.
Limitations
Several limitations should be noted in our study. First, our study data may be biased due to the entire self-report data. Secondly, it is difficult to explain the causal relationship between risk factors and turnover intention because of the cross-sectional study design. Third, compared with the large number of healthcare workers at the frontlines fighting COVID-19, this online survey might not be representative of Chinese medical personnel as some healthcare workers affected most by the outbreak were missed by the study.
Conclusions
In conclusion, turnover intention is relatively prevalent among healthcare workers during the COVID-19 pandemic period in China, but is lower than usual. Findings indicated that the factors contributing to turnover intention including worked in a Grade II hospital, doctor, working time over 12 h, frequency of mask replacement less than 4 h a time, patient–physician relations unchanged and mid-level social support. Therefore, comprehensive intervention is needed from psychological, behavioral and social aspects, such as relieving work stress, providing psychological counseling, providing adequate social support and protective equipment.
Acknowledgments
The authors would like to thank all the participants involved in the survey. Hao Hou and Yifei Pei are co-first authors of this study.
Funding Statement
This work was supported by the National Natural Science Foundation of China [grant number 82003484] and Universities’ philosophy and social science researches in Jiangsu Province [2020SJA1053], Natural Science Foundation for Colleges Universities in Jiangsu Province [20KJB330005].
Disclosure
The authors declare no conflicts of interest.
References
- 1.Esakandari H, Nabi-Afjadi M, Fakkari-Afjadi J, Farahmandian N, Miresmaeili SM, Bahreini E. A comprehensive review of COVID-19 characteristics. Biol Proced Online. 2020;22:19. doi: 10.1186/s12575-020-00128-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Remuzzi A. COVID-19 and Italy: what next? Free PMC Article. 2020;395:1225–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Coronavirus (COVID-19) Dashboard. Avaliable from: https://covid19.who.int/. Accessed July 30, 2021.
- 4.Zhang H, Zhang Y, Wu J, et al. Risks and features of secondary infections in severe and critical ill COVID-19 patients. Emerg Microbes Infect. 2020;9(1):1958–1964. doi: 10.1080/22221751.2020.1812437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Radonovich LJ Jr, Bessesen MT, Cummings DA, et al. The Respiratory Protection Effectiveness Clinical Trial (ResPECT): a cluster-randomized comparison of respirator and medical mask effectiveness against respiratory infections in healthcare personnel. BMC Infect Dis. 2016;16:243. doi: 10.1186/s12879-016-1494-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sahu AK, Thazhathidathil AV, Mathew R, Aggarwal P, Bhoi S. COVID-19 in health care workers -A systematic review and meta-analysis. Am J Emerg Med. 2020;38:1727–1731. doi: 10.1016/j.ajem.2020.05.113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Health Alert and Emergency Coordination Centre of Spanish Ministry of Health. Status of COVID-19 in Spain. Avaliable from: https://covid19.isciii.es/. Accessed May 24, 2020.
- 8.Misra-Hebert AD, Jehi L, Ji X, et al. Impact of the COVID-19 pandemic on healthcare workers’ risk of infection and outcomes in a large, integrated health system. J Gen Intern Med. 2020;35(11):3293–3301. doi: 10.1007/s11606-020-06171-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rana W, Mukhtar S, Mukhtar S. Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian J Psychiatr. 2020;51:102080. doi: 10.1016/j.ajp.2020.102080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yanez JA, Afshar Jahanshahi A, Alvarez-Risco A, Li J, Zhang SX. Anxiety, distress, and turnover intention of healthcare workers in Peru by their distance to the epicenter during the COVID-19 crisis. Am J Trop Med Hyg. 2020;103(4):1614–1620. doi: 10.4269/ajtmh.20-0800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care. 2020;9(3):241–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu P, Fang Y, Guan Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54(5):302–311. doi: 10.1177/070674370905400504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bohlken J, Schomig F, Lemke MR, Pumberger M, Riedel-Heller SG. [COVID-19 pandemic: stress experience of healthcare workers - A short current review]. Psychiatr Prax. 2020;47(4):190–197. German. doi: 10.1055/a-1159-5551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chong MY, Wang WC, Hsieh WC, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br Psychiatr. 2004;185:127–133. doi: 10.1192/bjp.185.2.127 [DOI] [PubMed] [Google Scholar]
- 15.Abbas J, Wang D, Su Z, Ziapour A. The role of social media in the advent of COVID-19 pandemic: crisis management, mental health challenges and implications. Risk Manag Healthc Policy. 2021;14:1917–1932. doi: 10.2147/RMHP.S284313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shuja KH, Aqeel M, Jaffar A, Ahmed A. COVID-19 pandemic and impending global mental health implications. Psychiatr Danub. 2020;32(1):32–35. doi: 10.24869/psyd.2020.32 [DOI] [PubMed] [Google Scholar]
- 17.March JG, Simon HA. Organizations. Rochester, NY, USA: Social Science Electronic Publishing; 1958:105–132. [Google Scholar]
- 18.Chao M-C, Jou R-C, Liao -C-C, Kuo C-W. Workplace stress, job satisfaction, job performance, and turnover intention of health care workers in rural Taiwan. Asia Pac J Public Health. 2015;27(2):NP1827–1836. doi: 10.1177/1010539513506604 [DOI] [PubMed] [Google Scholar]
- 19.Azizi MR, Atlasi R, Ziapour A, Abbas J, Naemi R. Innovative human resource management strategies during the COVID-19 pandemic: a systematic narrative review approach. Heliyon. 2021;7(6):e07233. doi: 10.1016/j.heliyon.2021.e07233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ali Jadoo SA, Aljunid SM, Dastan I, et al. Job satisfaction and turnover intention among Iraqi doctors–a descriptive cross-sectional multicentre study. Hum Resour Health. 2015;13:21. doi: 10.1186/s12960-015-0014-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sasso L, Bagnasco A, Catania G, et al. Push and pull factors of nurses’ intention to leave. J Nurs Manag. 2019;27(5):946–954. doi: 10.1111/jonm.12745 [DOI] [PubMed] [Google Scholar]
- 22.Jang Y, You M, Lee S, Lee W. Factors associated with the work intention of hospital workers’ in south korea during the early stages of the COVID-19 outbreak. Disaster Med Public Health Prep. 2020;1–8. doi: 10.1017/dmp.2020.164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wong EL, Wong SY, Kung K, Cheung AW, Gao TT, Griffiths S. Will the community nurse continue to function during H1N1 influenza pandemic: a cross-sectional study of Hong Kong community nurses? BMC Health Serv Res. 2010;10:107. doi: 10.1186/1472-6963-10-107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barnett DJ, Levine R, Thompson CB, et al. Gauging U.S. Emergency Medical Services workers’ willingness to respond to pandemic influenza using a threat- and efficacy-based assessment framework. PLoS One. 2010;5(3):e9856. doi: 10.1371/journal.pone.0009856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nashwan AJ, Abujaber AA, Villar RC, Nazarene A, Al-Jabry MM, Fradelos EC. Comparing the Impact of COVID-19 on Nurses’ Turnover Intentions before and during the Pandemic in Qatar. J Pers Med. 2021;11(6):456. doi: 10.3390/jpm11060456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Said RM, El-Shafei DA. Occupational stress, job satisfaction, and intent to leave: nurses working on front lines during COVID-19 pandemic in Zagazig City, Egypt. Environ Sci Pollut Res Int. 2021;28(7):8791–8801. doi: 10.1007/s11356-020-11235-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen HM, Liu CC, Yang SY, Wang YR, Hsieh PL. Factors related to care competence, workplace stress, and intention to stay among novice nurses during the coronavirus disease (COVID-19) pandemic. Int J Environ Res Public Health. 2021;18(4):2122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Song L, Wang Y, Li Z, Yang Y, Li H. Mental health and work attitudes among people resuming work during the COVID-19 pandemic: a Cross-Sectional Study in China. Int J Environ Res Public Health. 2020;17(14):5059. doi: 10.3390/ijerph17145059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Irshad M, Khattak SA, Hassan MM, Majeed M, Bashir S. Withdrawn: how perceived threat of Covid-19 causes turnover intention among Pakistani nurses: a moderation and mediation analysis. Int J Ment Health Nurs. 2021;30(1):350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duffield C, O’Brien-Pallas L. The causes and consequences of nursing shortages: a helicopter view of the research. Aust Health Rev. 2003;26(1):186–193. doi: 10.1071/AH030186 [DOI] [PubMed] [Google Scholar]
- 31.Lu Y, Hu XM, Huang XL, et al. The relationship between job satisfaction, work stress, work-family conflict, and turnover intention among physicians in Guangdong, China: a cross-sectional study. BMJ Open. 2017;7(5):e014894. doi: 10.1136/bmjopen-2016-014894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Labrague LJ, Santos JAA, de Los Santos JAA. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J Nurs Manag. 2021;29(3):395–403. doi: 10.1111/jonm.13168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taouk M, Lovibond P, Laube R. Psychometric properties of a Chinese version of the 21-item depression anxiety stress scales (DASS21). In Report for New South Wales Transcultural Mental Health Centre. Sydney: Cumberland Hospital; 2001. [Google Scholar]
- 34.Lovibond S, Lovibond P. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney, NSW: Psychology Foundation of Australia; 1995. [Google Scholar]
- 35.Dahlem NW, Zimet GD, Walker RR. The multidimensional scale of perceived social support: a confirmation study. J Clin Psychol. 1991;52(6):756–761. doi: [DOI] [PubMed] [Google Scholar]
- 36.Morens DM, Daszak P, Markel H, Taubenberger JK. Pandemic COVID-19 joins history’s pandemic legion. mBio. 2020;11(3). doi: 10.1128/mBio.00812-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization. World health report: working together for health. World Health Organization; 2006. [Google Scholar]
- 38.Ferede A, Kibret GD, Million Y, Simeneh MM, Belay YA, Hailemariam D. Magnitude of turnover intention and associated factors among health professionals working in public health institutions of North Shoa Zone, Amhara Region, Ethiopia. Biomed Res Int. 2018;2018:3165379. doi: 10.1155/2018/3165379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ryu S. Turnover Intention among Field Epidemiologists in South Korea. Int J Environ Res Public Health. 2020;17(3):949. doi: 10.3390/ijerph17030949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu X, Wang D, Xiong J, Tang Y, Cheng Y, Chen Q. Comparison of critical care resources between second-class hospitals and third-class hospitals in Guizhou Province of China. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2020;32(2):230–234. doi: 10.3760/cma.j.cn121430-20191225-00043 [DOI] [PubMed] [Google Scholar]
- 41.Steinmetz S, de Vries DH, Tijdens KG. Should I stay or should I go? The impact of working time and wages on retention in the health workforce. Hum Resour Health. 2014;12:23. doi: 10.1186/1478-4491-12-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11–17. doi: 10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang WR, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 Epidemic in China. Psychother Psychosom. 2020;89(4):242–250. doi: 10.1159/000507639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Imo UO. Burnout and psychiatric morbidity among doctors in the UK: a systematic literature review of prevalence and associated factors. BJPsych Bulletin. 2017;41(4):197–204. doi: 10.1192/pb.bp.116.054247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fang XH, Wu L, Lu LS, et al. Mental health problems and social supports in the COVID-19 healthcare workers: a Chinese explanatory study. BMC Psychiatry. 2021;21(1):34. doi: 10.1186/s12888-020-02998-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang S, Qiu Y, He J. Meta-analysis of the impact of role stress on the turnover intention of medical staff in tertiary hospitals. Ann Palliat Med. 2021;10(1):469–478. doi: 10.21037/apm-20-2446 [DOI] [PubMed] [Google Scholar]
- 47.Shortage of personal protective equipment endangering health workers worldwide. Avaliable from: http://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide. Accessed March 18, 2021.
- 48.Nearly 17,000 Italian health workers infected with virus: study. Avaliable from: http://www.straitstimes.com/world/europe/nearly-17000-italian-health-workers-infected-with-virus-study. Accessed March 18, 2021.
- 49.Campbell D, Busby M. “Not fit for purpose”: UK medics condemn Covid-19 protection. Available from: https://www.theguardian.com/society/2020/mar/16/not-fit-for-purpose-uk-medics-condemn-covid-19-protection. Accessed March 18, 2021.
- 50.Infections amongst healthcare workers increase by 75pc in a Week. May JJ, I I. Available from: http://www.dawn.com/news/1553678/infections-amongst-healthcare-workers-increase-by-75pc-in-a-week. Accessed March 18, 2021.
- 51.Chirico F, Nucera G, Magnavita N. COVID-19: protecting healthcare workers is a priority. Infect Control Hosp Epidemiol. 2020;41(9):1117. doi: 10.1017/ice.2020.148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.UK doctors finding it harder to get PPE kit to treat Covid-19 patients, research reveals; 2020. Available from: http://www.theguardian.com/society/2020/apr/27/uk-doctors-finding-it-harder-to-get-ppe-kit-to-treat-covid-19-patients-research-reveals. Accessed March 18, 2021.
- 53.Menon V, Padhy SK. Ethical dilemmas faced by health care workers during COVID-19 pandemic: issues, implications and suggestions. Asian J Psychiatr. 2020;51:102116. doi: 10.1016/j.ajp.2020.102116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Samson A, Lavigne RM, MacPherson P. Self-fulfillment despite barriers: volunteer work of people living with HIV. AIDS Care. 2009;21(11):1425–1431. doi: 10.1080/09540120902814403 [DOI] [PubMed] [Google Scholar]
- 55.QT, Inc. v. Mayo Clinic Jacksonville, 2006 US Dist. LEXIS 33668, at 10 (N.D. III; 2006.
- 56.Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci. 2020;74(4):281–282. doi: 10.1111/pcn.12988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rong X. Coronavirus a common foe the global village must fight together. Available from: https://www.globaltimes.cn/content/1178729.shtml. Accessed March 18, 2021.
- 58.Ren SY, Gao RD, Chen YL. Fear can be more harmful than the severe acute respiratory syndrome coronavirus 2 in controlling the Corona virus disease 2019 epidemic. World j Clin Cases. 2020;8(4):652–657. doi: 10.12998/wjcc.v8.i4.652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gan Y, Gong Y, Chen Y, et al. Turnover intention and related factors among general practitioners in Hubei, China: a cross-sectional study. BMC Fam Pract. 2018;19(1):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tan BYQ, Chew NWS, Lee GKH, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173(4):317–320. doi: 10.7326/M20-1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liang Y, Wu K, Zhou Y, Huang X, Zhou Y, Liu Z. Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in China: a comparison with the general population. Int J Environ Res Public Health. 2020;17(18):6550. doi: 10.3390/ijerph17186550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mo Y, Deng L, Zhang L, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag. 2020;28(5):1002–1009. doi: 10.1111/jonm.13014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Irshad M, Khattak SA, Hassan MM, Majeed M, Bashir S. How perceived threat of Covid-19 causes turnover intention among Pakistani nurses: a moderation and mediation analysis. Int J Ment Health Nurs. 2020. doi: 10.1111/inm.12775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barnett MLG, Grabowski DC. Nursing homes are ground zero for COVID-19 pandemic. JAMA Health Forum. 2020;1(3):e200369. doi: 10.1001/jamahealthforum.2020.0369 [DOI] [PubMed] [Google Scholar]
- 65.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Abbas J. The impact of coronavirus (SARS-CoV2) epidemic on individuals mental health: the protective measures of Pakistan in managing and sustaining transmissible disease. Psychiatr Danub. 2020;32(3–4):472–477. doi: 10.24869/psyd.2020.472 [DOI] [PubMed] [Google Scholar]
- 67.Liu S, Yang L, Zhang C, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiat. 2020;7(4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549. doi: 10.12659/MSM.923549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Labrague LJ, De Los Santos JAA. COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J Nurs Manag. 2020;28:1653–1661. doi: 10.1111/jonm.13121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Özmete E, Pak M. The relationship between anxiety levels and perceived social support during the pandemic of COVID-19 in Turkey. Soc Work Public Health. 2020;35(7):603–616. doi: 10.1080/19371918.2020.1808144 [DOI] [PubMed] [Google Scholar]
- 71.Maunder R, May RM, McLean AR, Pattison J, Weiss RA. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philos Trans R Soc Lond B Biol Sci. 2004;359(1447):1117–1125. doi: 10.1098/rstb.2004.1483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.McDowell TL, Serovich JM. The effect of perceived and actual social support on the mental health of HIV-positive persons. AIDS Care. 2007;19(10):1223–1229. doi: 10.1080/09540120701402830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Li L, Lee SJ, Thammawijaya P, Jiraphongsa C, Rotheram-Borus MJ. Stigma, social support, and depression among people living with HIV in Thailand. AIDS Care. 2009;21(8):1007–1013. doi: 10.1080/09540120802614358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ravangard R, Dianat S, Shokrpour N. The factors affecting hospital employees’ turnover intentions: a case of Iran. Health Care Manage. 2019;38(2):166–178. doi: 10.1097/HCM.0000000000000258 [DOI] [PubMed] [Google Scholar]