Abstract
Background
Modern, specialised care for children with inflammatory bowel disease [IBD] may have resulted in changes in health services use. We report trends over time in health services utilisation and surgery for children with IBD and children without IBD.
Methods
Children aged <18 years, diagnosed with IBD between 1994 and 2013 [n = 5518] and followed until 2015 in Ontario, Canada, were identified from health administrative data and matched to children without IBD on age, sex, rural/urban household, and income [n = 26,677]. We report the annual percentage change [APC] with 95% confidence intervals [CI] in the rate of outpatient visits, emergency department [ED] visits, and hospitalisations, using negative binomial regression for events within 5 years from the diagnosis/index date. We used Cox proportional hazards regression models to report APC in hazards of intestinal resection [Crohn’s disease; CD] and colectomy [ulcerative colitis; UC].
Results
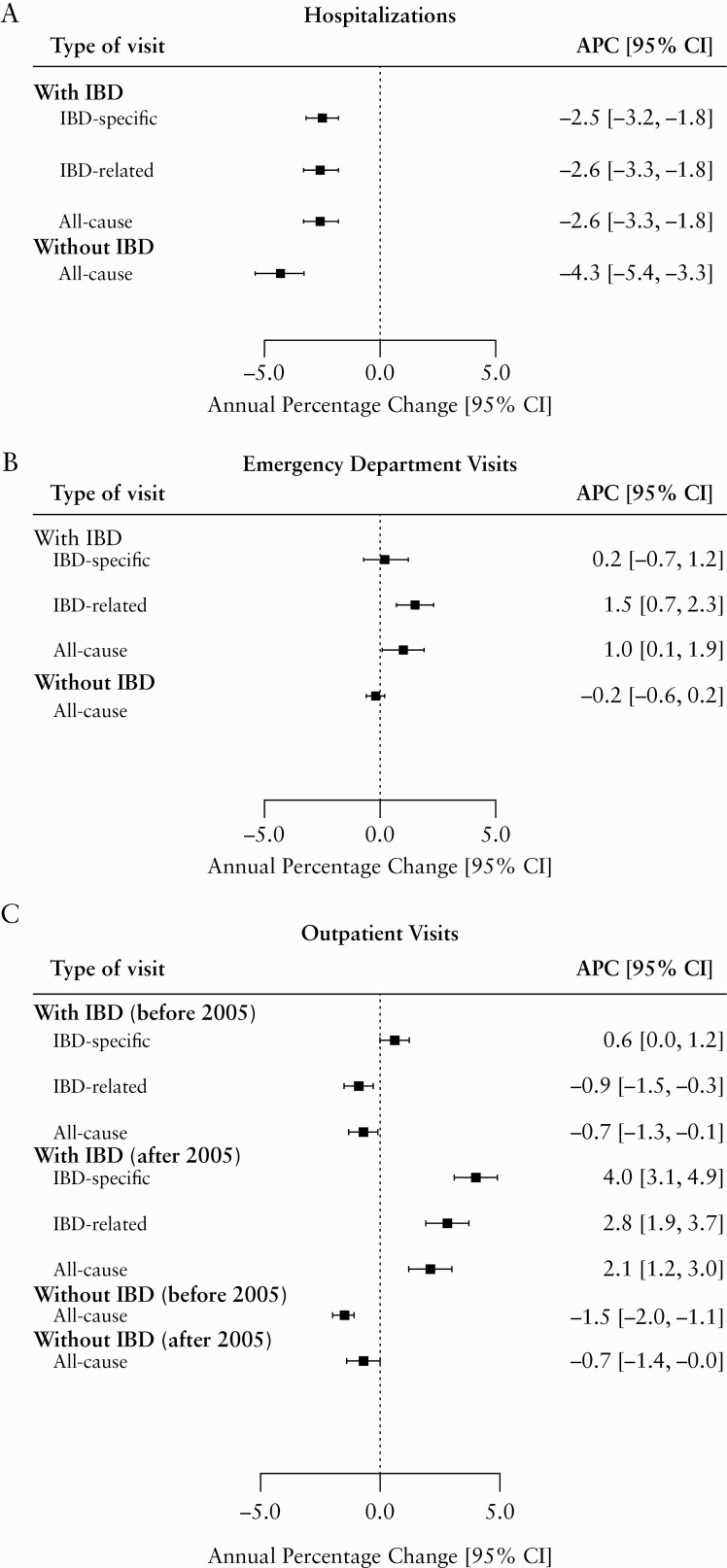
IBD-specific hospitalisation rates decreased by 2.5% [95% CI 1.8–3.2%] annually, and all-cause hospitalisation rates in children without IBD decreased by 4.3% [95% CI 3.5–5.1%] annually. Intestinal resection risk in CD decreased by 6.0% [95% CI 4.6–7.3%] annually and colectomy risk in UC decreased by 3.0% [95% CI 0.7–5.2%] annually. In contrast, IBD-specific outpatient visit rates increased after 2005 by 4.0% [95% CI 3.1–4.9%] annually. Similar trends in outpatient visits were not observed in children without IBD.
Conclusions
Hospitalisations and surgeries decreased over time while outpatient visits increased after 2005. Decreasing hospitalisations were mirrored in children without IBD, likely resulting from a combination of changes in disease management and health system factors.
Keywords: Inflammatory bowel disease, Crohn’s disease, ulcerative colitis, paediatrics, health services research, routinely collected health data, health administrative data
1. Introduction
Childhood-onset inflammatory bowel disease [IBD] presents unique challenges including delayed growth, increased school absenteeism, and impaired psychosocial well-being.1–6 The direct costs of care for children and adolescents with IBD are considerable and include the costs of medication, hospitalisations, surgeries, outpatient visits, and emergency department visits.7 Furthermore, the incidence of childhood-onset IBD, including Crohn’s disease [CD] and ulcerative colitis [UC], is rising globally.8 Because mortality from IBD is low, children with IBD live with their disease for longer than those with adult-onset disease and therefore will likely require more care over the course of their lives, resulting in greater overall costs to the health care system over their lifespan compared with individuals diagnosed at older ages.9,10
Current disease management strategies aim to minimise inflammation and decrease complications. The numerous changes in the care of paediatric IBD patients include increased specialist care,11 the widespread use of biologic therapies, and improvements in diagnostic capabilities. The impact of these improvements on health care use among children with IBD is poorly defined but of great importance. A previous study comparing children diagnosed before and after the introduction of biologics found that the likelihood of being admitted to hospital increased in children with IBD in Ontario, Canada, but the frequency of hospitalisations remained stable.12 Further, the frequency of outpatient visit rates remained stable in those diagnosed between 1994 and 2004,12 but temporal trends in emergency department [ED] visits have not been well documented.13 A systematic review reported decreasing surgery rates among IBD patients over the past half-century.14 Decreasing rates of intestinal resection among children with CD have also been reported, whereas rates of colectomy in children with UC were stable in Ontario12 but decreased in other Canadian provinces.15,16
As the prevalence of IBD among children continues to rise,8,17,18 the care of these children will place an increasingly heavy burden on health care systems, and an understanding of time trends in how these children use health services is needed for health care decision makers to effectively plan for the oncoming health services needs in paediatric IBD. We assessed the temporal trends of health services use and surgeries among children with IBD in Ontario, Canada’s most populous province.
2. Methods
This study was approved by the Children’s Hospital of Eastern Ontario [CHEO] Research Ethics Board.
2.1. Data sources
We used population-level health administrative datasets hosted at ICES. Health administrative data are routinely collected by the Province of Ontario’s Ministry of Health [MOH] and Ministry of Long-Term Care [MLTC] in the process of administering the universal publicly funded health care system, providing a wealth of information on health services use. ICES is a not-for-profit research institute that holds Ontario health data and other population data, in compliance with legal and privacy requirements. Data include information on demographics, outpatient visits, hospitalisations, outpatient procedures [e.g., colonoscopy], and ED visits. Patients are deterministically linked across databases using an encrypted unique identifier, enabling longitudinal tracking of patients over time and cross-sectional tracking of patients across databases.
Office-based outpatient visit records were acquired from the Ontario Health Insurance Plan [OHIP] physician claims database. OHIP is the publicly funded universal provincial health care plan provided to all legal Ontario residents [>99% of the population]. The OHIP database collects fee-for-service and shadow billing records from physicians and nurse practitioners, and therefore provides an accurate representation of health services use. Physician billings for medical procedures [e.g., colonoscopy] are also included in the OHIP physician claims database. The ICES Emergency Claims database [ERCLAIM] includes physician billings for patients seen in the ED and is derived from the OHIP physician claims data. For OHIP and ERCLAIM data, one diagnostic code is assigned per patient visit, using an abbreviated 3-digit version of the International Classification of Disease, 9th Revision [ICD-9] coding system.19
Data on hospitalisations and surgeries were obtained from the Canadian Institute for Health Information Discharge Abstract Database [CIHI-DAD], which collects data abstracted from patients’ medical charts at discharge by professional, certified medical coders. This database includes up to 25 diagnostic codes and 20 intervention codes related to the hospitalisation. Medical diagnoses are coded using the International Classification of Disease [ICD], 9th Revision [ICD-9] system before April 1, 2002, and the ICD 10th revision [ICD-10] system thereafter.19 The reason for admission [most responsible or contributing], comorbidity, and any additional diagnoses made while in hospital are also captured within the data. Interventions are coded using the Canadian Classification of Diagnostic, Therapeutic, and Surgical Procedures [CCP] before April 1, 2002, and the Canadian Classification of Health Interventions [CCI] thereafter, and include any diagnostic or therapeutic interventions that occurred during the hospitalisation, such as endoscopic procedures and surgeries.
Children with IBD were identified from the Ontario Crohn’s and Colitis Cohort [OCCC], which is a database of all children in Ontario with IBD, derived from health administrative data using age-stratified algorithms based on health services use.17,20
Sociodemographic data were derived from the Registered Persons Database [RPDB], which includes date of birth, sex, postal code, and eligibility for OHIP [updated bi-monthly].
2.2. Study design and setting
We conducted: [1] a population-based retrospective cohort study using health administrative data hosted at ICES, to determine changes in rates of IBD-specific and IBD-related hospitalisations, ED visits, outpatient visits, and hazard of surgery over time in children newly diagnosed with IBD between April 1, 1994, and March 31, 2013, (fiscal years [FY] 1994 to 2012) in Ontario, Canada; and [2] a population-based retrospective matched cohort study to compare all-cause health services [hospitalisations, ED visits, and outpatient visits] use between children newly diagnosed with IBD and children without IBD over the same time period in Ontario, Canada.
We identified all children aged from 6 months to <18 years and diagnosed with IBD, from the OCCC. The OCCC identified children with IBD using a validated two-step algorithm.17 Children who underwent endoscopic evaluation [sigmoidoscopy or colonoscopy] were considered to have IBD if they also had four physician contacts or two hospitalisations with an associated diagnostic code for IBD [CD: ICD-9 555.x, ICD-10 K50.x; UC: ICD-9 556.x, ICD-10 K51.x] within 3 years. Children who did not undergo endoscopy were classified as having IBD if they had seven outpatient physician contacts or three hospitalisations with associated IBD diagnosis codes within 3 years. Date of diagnosis was assigned as the date of the first health care contact with an IBD diagnostic code. The algorithm17 identified IBD in Ontario children with the following diagnostic accuracies: sensitivity 89.6–91.1%, specificity 99.5–100%, positive predictive value [PPV] 59.2–76.0%, and negative predictive value [NPV] 99.9–100%. The validated algorithm further differentiated CD and UC based on the last five of seven outpatient visits, with diagnostic accuracies of: sensitivity 95.1%, specificity 86.0%, PPV 92.0%, and NPV 91.2%.17 When the algorithm could not identify the IBD subtype [CD or UC], the patient was assigned a category of IBD type unclassifiable [IBD-U]. This does not reflect the Montreal classification system of IBD type unclassified, but instead reflects the inability to classify the patient as having CD or UC based on administrative data codes. To distinguish incident from prevalent cases, patients required a 3-year look-back period in which they had no health care contacts with an IBD diagnostic code.17 Children born after April 1, 1991, with continuous OHIP eligibility from birth, did not require a look-back period because their full health administrative data were available for analysis.
Children with IBD and aged from 6 months to <18 years at diagnosis were matched to up to five children without IBD from the general population registry [RPDB] on the date of the IBD diagnosis, based on age, sex, rural/urban household, and mean neighbourhood income quintile at the time of IBD diagnosis. Children without IBD were required to be eligible for OHIP for at least as long as their matched IBD patient. A total of 6.9% of children with IBD did not have five matched children without IBD, and 23 [0.4%] children with IBD were unmatched to any children without IBD. Children with IBD who matched to at least one child without IBD were included in all analyses, whereas children with IBD who had no matches to children without IBD were included in the analyses of IBD patients only [i.e., for IBD-specific and IBD-related health services use] but excluded from the analyses comparing children with and without IBD [i.e., all-cause health services use outcomes].
Children were followed from their date of diagnosis to either [a] death, [b] end of follow up [March 1, 2016], [c] migration out of Ontario, or [d] end of OHIP eligibility. OHIP eligibility is not age- or income-based and ends when patients are no longer Canadian citizens or hold immigration status, or are Ontario residents and physically live in Ontario for 153 days in a 12-month period. Children diagnosed after FY 2012 could not be included because a 3-year look-forward period was required for the algorithm to accurately identify an IBD diagnosis in children,17 and data were only available until March 31, 2016, at the time of study.
Children with and without IBD were excluded from the sample if they were missing information on date of birth, sex, and postal codes [Supplementary Figure 1, available as Supplementary data at ECCO-JCC online]. Patients who lived in the South East Local Health Integration Network [Kingston, Ontario region] at any point during OHIP eligibility were excluded because OHIP shadow-billings were inconsistently collected during the study period in this region. Shadow billings are physician tariff submissions used to track services provided by physicians who are compensated using an alternative funding plan [i.e., salaried]. Just as fee-for-service physicians submit tariffs and are paid according to the code submitted, salaried physicians submit the same fee codes but are not compensated for the service. Both types of billings are processed and filed for their accounting purposes and can be subsequently used to track health services use.
2.3. Exposure
The exposure was the year of IBD diagnosis [FY 1994–2012]. The non-IBD controls [children without IBD] were assigned an index date corresponding to the date their matched IBD patient was diagnosed with IBD.
2.4. Outcomes
The outcomes analysed are summarised in Table 1. For the first part of our study, we described the number of each type of encounter per person per year [i.e., rates] of IBD-specific and IBD-related hospitalisations, ED visits, and outpatient visits among IBD patients only. We also described the hazard of surgery as intestinal resection [in CD patients]21 or colectomy [in UC patients]22 using previously validated codes to identify surgeries [Supplementary Material 1, available as Supplementary data at ECCO-JCC online]. Only health services and surgeries occurring on or after the diagnosis or index date were included. IBD-specific visits were those with an associated diagnosis code of IBD [ICD-9: 555, 556; ICD-10: K50, K51]. IBD-related visits included visits with IBD-specific diagnoses, in addition to those with diagnoses of signs, symptoms, and extra-intestinal manifestations of IBD [Supplementary Material 2, available as Supplementary data at ECCO-JCC online].12,13,23 In the analyses evaluating hospitalisation admissions for IBD-specific or IBD-related diagnoses, the hospitalisation encounter was only included if: the IBD-specific or IBD-related diagnosis code was the most responsible for the hospitalisation, or the first, second, or third transfer between hospitalisations, or services within the same hospital; or if it was a contributing diagnosis, such as if the diagnosis was a pre-admit or post-admit comorbidity.
Table 1.
The multivariable regression models used to assess time trends in health services and surgical outcomes among children with inflammatory bowel disease in Ontario.
| Type of data | Regression model | Effect estimate | Reported measure | Population | Exposure | Outcome |
|---|---|---|---|---|---|---|
| Study 1: Trends in health service use in IBD patients | ||||||
| Count [number of events per person per year] | Negative binomiala | IRR | APC | IBD, CD, UC | Year of diagnosis [linear] | IBD-specific hospitalisations, IBD-related hospitalisations |
| APC | IBD-specific ED visits, IBD-related ED visits | |||||
| APC | Year of diagnosis [knot at 2005] | IBD-specific outpatient visits, IBD-related outpatient visits | ||||
| Time to first event | Cox proportional hazarda | HR | APC | IBD, CD, UC | Year of diagnosis [linear] | IBD-specific hospitalisations, IBD-related hospitalisations |
| APC | IBD-specific ED visits, IBD–related ED visits | |||||
| APC | CD | Year of diagnosis [linear] | Intestinal resection | |||
| APC | UC | Year of diagnosis [linear] | Colectomy | |||
| Study 2: Comparison of trends in health service use among children with and without IBD | ||||||
| Count [number of events per person per year] | Negative binomialb | IRR | APC | With and without IBD | Year of diagnosis or index date [linear] | All-cause hospitalisations |
| All-cause ED visits | ||||||
| Year of diagnosis or index date [knot at 2005] | All-cause outpatient visits |
APC, average annual percentage change; CD, Crohn’s disease; ED, emergency department visits; HR, hazard ratio; IBD, inflammatory bowel disease; IRR, incidence rate ratio; OR, odds ratio; UC, ulcerative colitis; y, years’
aAll models adjusted for age [10 y or older versus <10 y], sex [female versus male], rural/urban residency, and mean neighbourhood income quintile.
bAll models adjusted for IBD diagnosis [Yes/no] and included an interaction term between year of diagnosis and IBD diagnosis to compare trends in children with and without IBD. Autocorrelation was accounted for using an unstructured covariance.
In the second part of our study, we compared rates of all-cause health services use, including hospitalisations, ED visits, and outpatient visits separately, between children with and without IBD as a control analysis. These were encounters for any reason [i.e., had any diagnostic code].
We included only hospitalisations with a length of stay ≥48 h because hospitalisations for <48 h may have represented a hospitalisation for the sole purpose of facilitating bowel preparation for colonoscopy or to facilitate rapid access to biologic medication in these children, and not hospitalisation for disease activity and management. In addition, we counted only one hospitalisation per episode of care, and therefore a transfer between hospitals was considered a single hospitalisation.
Only one ED visit was counted when a child had multiple ED visit claims on a given day. Likewise, only one outpatient visit was counted when a child had multiple outpatient visit claims on a given day. Only office-based outpatient visits were included. Outpatient visits with an associated infusion, telephone, or tele-medicine code were excluded [<2.2% of outpatient visits] to ensure only true outpatient encounters were counted and that trends were not influenced by encounters solely for the purposes of administering an infusion or due to the increased availability of tele-medicine.
2.5. Statistical analysis
We reported the characteristics of children included in the study as means with standard deviations [SD], medians with interquartile range [IQR], or proportions, where appropriate. We determined the associations between year of diagnosis and health services use using multivariate maximum-likelihood regression models for counts of hospitalisations, ED visits, and outpatient visits using Poisson, or negative binomial regression and time to first intestinal resection and colectomy using Cox proportional hazards regression. We used these models to: [a] determine trends over time of surgeries and health services use for IBD-specific and IBD-related reasons in children with IBD overall [including IBD-U] and stratified by disease type [CD and UC, excluding IBD-U]; and [b] compare the trends in all-cause health services use in IBD children to matched children without IBD, who served as the reference population. A summary of the statistical analyses conducted in children with IBD and comparing children with and without IBD is provided in Table 1. Patients were followed for 5 years from the date of diagnosis or index in all models. We also censored patients at 1-year of follow-up from date of diagnosis or index in Poisson/negative binomial regression models, but patients were not censored at 1 year for surgical outcomes in Cox proportional hazards regression models.
Since most Poisson regression models were over-dispersed [Pearson χ2 statistic >1.5],24 negative binomial regression models were used instead. Follow-up time was accounted for by setting the offset equal to the natural log of the follow-up. The unstructured covariance structure was used to account for correlation within matched sets [i.e., children with and without IBD] in general estimating equation models for only the analyses of all-cause health services use [hospitalisations, ED visits, and outpatient visits]. The Cox proportional hazard assumption was assessed by visual inspection of plots and hypothesis testing using time-varying covariates; ties were handled using the exact method because we expected a relatively large number of ties. Patients were censored for either incomplete follow-up or end of study period in Cox proportional hazards regression models.
Fiscal year of diagnosis, or index, was modelled as a linear continuous variable, except when the data suggested an inflection point in the preliminary plots [Supplementary Figures 2 and 3, available as Supplementary data at ECCO-JCC online]. We assessed temporal trend linearity using two methods. The first was a hypothesis test [Kolmogorov-type supremum test of the cumulative martingale residuals at α = 5%] in Cox proportional hazards regression models. We also generated plots to visually assess if the association between fiscal year and the outcomes was linear [i.e., increased or decreased consistently over time]. When plots appeared to deviate from linearity, we identified any statistically significant inflection points [α = 5%] using Joinpoint Regression Program, Version 4.6.0.0 – April 2018 [Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute]. Preliminary plots of outpatient visit counts per person per year were the only plots suggesting that changes over time were non-linear [i.e., that there were inflection points]. These inflection points mostly occurred around 2005 in children with IBD, which was a notable time in the changes to care in paediatric IBD patients because it was when the first paediatric clinical trial of infliximab was published,25 and Health Canada subsequently approved infliximab for use in children. Therefore, we restricted analyses of outpatient visit rates to splines with a knot at 2005 and reported APC in outpatient visit rates in children diagnosed with IBD in or before 2005 and after 2005 separately. That is, time was modelled as a linear exposure with a split at 2005, allowing for different rates of change before and after this point. For all other outcomes, time was modelled as a linear exposure.
For all models [Table 1], effect estimates [incidence rate ratios or hazard ratios] were considered statistically significant if their 95% confidence intervals did not cross the null value of one. The results from the models are reported as the average APC, which is the change in the outcomes for every 1-year increase in diagnosis [or index] date and was calculated by subtracting 1 from the exponentiated beta-coefficient [eβ − 1].
Independent variables with potential confounding effects on the association between the exposure and outcome were chosen a priori due to their known associations with IBD17,18,26,27 or health services use.13,23,28 These variables were: age [dichotomous; <10 and ≥10],29 sex [male versus female], rural/urban residence [urban versus rural, according to the Canadian Census definition], and mean neighbourhood income quintile [a validated proxy for household income]30 at the date of IBD diagnosis or index date. In the analyses evaluating IBD-specific and IBD-related events in IBD patients [as well as CD and UC subgroups], these confounding variables were included as covariates in each regression model. In the analyses comparing trends in overall health services use between children with and without IBD, the confounding variables were not included since the two populations had been matched on those variables. However, a variable indicating whether the patient had an IBD diagnosis [present versus absent] was included as an additional independent predictor in the analyses of all-cause health services use in children with and without IBD. To determine if the trends between children with and without IBD were different from each other, we included an interaction term in the model [tested at α = 5%] between the fiscal year of diagnosis [or index date in children without IBD] and IBD diagnosis [present or absent].
Effect measure modification between predictors and covariates was assessed at a 5% significance level using interaction terms. Inconsistent statistically significant effect measure modification terms within and across outcomes and models were determined to be a result of random chance due to the large number of analyses conducted. Effect measure modification terms that were consistently statistically significant within or across outcomes and models were investigated by plotting average annual event rates against time and were determined to have been driven by small cells. As a result, no additional effect measure modification terms were included in the models.
All statistical analyses were conducted using SAS Enterprise Guide version 7.1 [SAS Institute, Cary, NC, USA].
3. Results
3.1. Descriptive statistics
Our cohort included 5518 children with IBD matched to 26 677 children without IBD [Table 2; Supplementary Figure 1]. Of included IBD patients, the mean [SD] age at diagnosis was 13.1 [3.6] years, 3122 [56.6%] were male, 58.2% had CD, 35.3% had UC, and 6.5% had IBD-U. The median length [Q1, Q3] of follow-up was 10.1 [6.5, 15.3] years for children with IBD and 10.4 [6.6, 15.7] years for children without IBD. Health services use rates are reported in Supplementary Figure 2, and survival curves of risk of surgery based on year of diagnosis are reported in Supplementary Figure 3.
Table 2.
Characteristics of children with and without IBD included in the study
| Characteristics | IBD [n = 5518] | Non-IBD [n = 26 677]a | |
|---|---|---|---|
| Sex | Females | 2396 [43.4%] | 11,573 [43.4%] |
| Males | 3122 [56.6%] | 15,104 [56.6%] | |
| Age at IBD diagnosis or index dateb [years] | Mean [SD] | 13.1 [3.6] | 13.1 [3.6] |
| Median [Q1, Q3] | 14.0 [11.0, 16.0] | 14.0 [11.0, 16.0] | |
| Diagnosis | CD | 3212 [58.2%] | N/A |
| UC | 1945 [35.3%] | N/A | |
| IBD-U | 361 [6.5%] | N/A | |
| Rural residence at diagnosis | Urban | 4929 [89.3%] | 24,630 [92.3%] |
| Rural | 583 [10.6%] | 2041 [7.7%] | |
| Missing | 6 [0.1%] | 6 [0.02%] | |
| Neighbourhood income quintile at diagnosis | First [lowest] | 714 [12.9%] | 3412 [12.8%] |
| Second | 928 [16.8%] | 4467 [16.7%] | |
| Third | 1092 [19.8%] | 5256 [19.7%] | |
| Fourth | 1285 [23.3%] | 6275 [23.5%] | |
| Fifth [highest] | 1487 [27.0%] | 7258 [27.2%] | |
| Unknown | 12 [0.2%] | 9 [0.03%] | |
| Length of follow-up [years] | Mean [SD] | 11.0 [5.4] | 11.3 [5.4] |
| Median [Q1, Q3] | 10.1 [6.5, 15.3] | 10.4 [6.6, 15.7] | |
| Minimum | 0.4 | 2.1 | |
| Maximum | 22.0 | 22.0 |
CD, Crohn’s disease; IBD, inflammatory bowel disease; IBD-U, IBD type unclassifiable; N/A, not applicable; Q1, first quartile; Q3, third quartile; SD, standard deviation; UC, ulcerative colitis.a6.9% of children with IBD were matched to fewer than five controls.
bDate of diagnosis in IBD patients, and the same date in matched non-IBD patients.
3.2. Hospitalisation rates
The rate of hospitalisations significantly declined for both IBD-specific [APC -2.5%, 95% CI -3.2 to -1.8%] and IBD-related [APC -1.7%, 95% CI -2.4 to -1.0%] admissions in IBD patients [Figure 1]. Similar decreases were observed in children with CD [Supplementary Figure 4, available as Supplementary data at ECCO-JCC online]. In children with UC, the rate of hospitalisations for IBD-specific reasons did not decrease significantly [APC -1.1%, 95% CI -0.25 to +0.003%], but the rate of IBD-related hospitalisations decreased [APC -1.4%, 95% CI -2.8 to -0.0004%] [Supplementary Figure 4].
Figure 1.
Forest plots of the annual percentage change [95% confidence intervals] in rates of health services for a 1-year increase in year of diagnosis/index in children with and without inflammatory bowel disease. The difference in all-cause rates between children with and without IBD were statistically significant [p <0.05] for hospitalisations, emergency department visits, and outpatient visits both before and after 2005. APC, average annual percentage change; 95% CI, 95% confidence interval; IBD, inflammatory bowel disease.
The rate of all-cause hospitalisations decreased by 2.6% [95% CI -3.3 to -1.8%] per year in children with IBD and by 4.3% [95% CI -5.4 to -3.3%] per year in children without IBD. Compared with children with IBD, children without IBD experienced a larger magnitude of decrease in rates of hospitalisations [p = 0.01].
Time trends in hospitalisation rates within 1 year of diagnosis generally followed trends similar to the rates within 5 years of diagnosis and are provided in Supplementary Material 3, available as Supplementary data at ECCO-JCC online.
3.3. Emergency department visit rates
In children with IBD, IBD-specific ED visit rates did not change over time [APC +0.2%, 95% CI -0.7 to 1.2%], but IBD-related ED visit rates increased by 1.5% [95% CI +0.7 to +2.3%] per year [Figure 1]. These trends were similarly observed in CD and UC subgroups [Supplementary Figure 4].
Rates of all-cause ED visits increased among IBD patients by 1.0% [95% CI +0.1 to +1.9%] per year. In children without IBD, the rate of all-cause ED visits remained unchanged [APC -0.2%, 95% CI -0.6 to +0.2%]. The differences in the rates between children with and without IBD were statistically significant [p = 0.01].
Time trends in ED visit rates within 1 year of diagnosis generally followed trends similar to the rates within 5 years of diagnosis and are provided in Supplementary Material 3.
3.4. Outpatient visit rates
Outpatient visit rates were found to differ before and after a 2005 diagnosis date and are reported separately before and after this inflection point. In children diagnosed with IBD in 2005 or earlier, rates of IBD-specific outpatient visit rates did not significantly change [APC +0.6%, 95% CI -0.04 to +1.2%], but IBD-related outpatient visits decreased by 0.9% [95% CI -1.5 to -0.3%] per year [Figure 1]. Similar trends were also generally observed in children with CD [Supplementary Figure 4]. Children diagnosed with UC in 2005 or earlier had increasing rates of IBD-specific outpatient visits [APC +1.1%, 95% CI +0.1 to +2.1%]; the rate of IBD-related outpatient visits remained unchanged [APC -0.7%, 95% CI -1.7 to +0.3%] [Supplementary Figure 4].
Among children diagnosed with IBD after 2005, IBD-specific outpatient visit rates increased by 4.0% [95% CI +3.1 to +4.9%] per year. IBD-related visits increased by 2.8% [95% CI +1.9 to +3.7%] per year. Similar trends were observed in children with CD and UC [Supplementary Figure 4].
In children with a diagnosis or index date in or before 2005, the frequency of all-cause outpatient visits within 5 years decreased for both children with [APC -0.7%, 95% CI -1.3 to -0.1%] and without [APC -1.6%, 95% CI -1.9 to -1.2%] IBD. The difference in these rates between children with and without IBD was statistically significant [p = 0.03].
In children diagnosed with IBD after 2005, there was an annual increase of 2.1% [95% CI +1.2 to +3.0%] in the rates of all-cause outpatient visits. The frequency of all-cause outpatient visits among children without IBD with an index date after 2005 decreased by 0.7% [95% CI -1.4 to -0.0002%] per year. The time trends in the frequency of outpatient visits were statistically different between children with and without IBD [p <0.0001].
Time trends in outpatient visit rates within 1 year of diagnosis generally followed trends similar to the rates within 5 years of diagnosis and are provided in Supplementary Material 3.
3.5. Surgery risk
The hazard of first intestinal resection within 5 years of diagnosis in CD patients decreased by 6.0% [95% CI -7.3 to -4.6%] per year. The hazard of colectomy within 5 years of diagnosis in UC patients decreased by 3.0% [95% CI -5.2 to -0.7%] per year.
4. Discussion
There have been significant changes in the management of paediatric IBD over the past three decades, and we observed changing trends in health services use in children with IBD living in Ontario, Canada. Although the incidence of IBD has increased in Ontario children,17,18 hospitalisations became less frequent with each passing year in Ontario among children newly diagnosed with IBD between fiscal years 1994 to 2012. During this same period, decreases in the frequency of hospitalisations were more pronounced among children without IBD than among children with IBD, suggesting health care system changes may have contributed significantly to the trends in hospitalisation rates among IBD patients. Surgeries also decreased in children with IBD in this time frame. However, stable rates of IBD-specific ED visits, but increasing IBD-related ED visits, were observed in contrast to decreasing all-cause ED visits in children without IBD. Furthermore beyond 2005, which corresponds to the time of marketplace introduction of biologics to treat children with IBD in Ontario, the frequency of outpatient visits increased in children with IBD but decreased in the same time frame in children without IBD. These results imply that the management of paediatric IBD has shifted from in-patient hospital care towards greater ambulatory care.
Our findings of decreasing surgeries and hospitalisations are consistent with most previous studies reporting decreasing trends in these same outcomes among Canadian children and adults with IBD.31–33 Another study found no changes or increasing need for surgery and hospitalisation over time but did not follow patients beyond the approval of infliximab for paediatric IBD and likely missed more recent trends.12 Decreasing hospitalisations have also been reported among all Ontario children,34 children and adults with other chronic diseases,35–40 and for medical events requiring acute care.41–43 Internationally, hospitalisations have increased in children with IBD,44–46 though these studies typically reported absolute values or were cross-sectional, and therefore may have been unable to distinguish trends in health services from trends in disease incidence.
Data on trends in ED visits among children and adults with IBD are sparse. A Canadian study previously reported decreasing ED visits among children and adults with IBD.32 This study included prevalent IBD cases, whereas we limited our analysis to incident cases; longer disease duration is associated with decreased rates of ED use.47 Internationally, increases in ED visits have been observed among children and adults with IBD.48–50 However, studies either report absolute numbers of visits49 or are cross-sectional in nature,48,50 where patients could not be followed after visiting the ED. Therefore, trends in ED visits seen in these studies may reflect either true changes in health services use or changes in disease prevalence. In children with other chronic diseases, ED visit use has either decreased51,52 or remained stable.53
Our analysis identified different trends in the frequency of outpatient visits before and after 2005. This coincides with the Health Canada approval of infliximab for paediatric CD in 2005.25 The increasing trends in outpatient visits in children with IBD have not been observed in children with other chronic diseases53–55 or among the overall population of children.56
The trends in health services use and surgery are inter-related. Decreases in hospitalisations and surgery among children with IBD likely arose from a combination of improving IBD care [e.g., through increased use of biologic therapies and adoption of a treat-to-target approach25 requiring closer monitoring by specialised paediatric gastroenterologists] and health system factors [e.g., decreased funding/capacity for hospital admissions]. Insufficient specialist care in outpatient settings has been associated with higher ED visit use in Ontario patients with IBD,47,57 whereas early use of specialist gastroenterology care reduces the risk of surgery.58 If increases in the prevalence of IBD among Ontario children are outpacing growth in the availability of paediatric gastroenterologists, lack of access to specialist care may drive growth in ED use.
The need for surgery is less influenced by patient and health system factors that influence health services use and, therefore, may better reflect improvement in the quality of IBD care and disease control. For example, despite associations between biologic therapy and decreased IBD surgeries,14,59–62 an Ontario study found that the introduction of anti-tumour necrosis factor therapy did not lower health services use or surgeries among adults with IBD beyond what was expected based on trends in these outcomes before its introduction.33 A systematic review additionally reported decreasing surgery rates long before biologic therapy was a treatment option for IBD.14 Thus, trends in health services use are multifaceted, and the observed decreases in surgeries and hospitalisations may result from multiple or a combination of factors, such as the increasing outpatient visit and IBD-related ED visits rates observed in the present study.
The strengths of the present study include its large sample size and the use of population-based data comprising all children in Ontario with IBD, to reduce selection bias. Another strength is the inclusion of a matched reference cohort of children without IBD, selected at random from the population, to determine overall systemic changes in health services use at the time of the study. By comparing trends in children with and without IBD, we distinguished between trends specific to the care of IBD and trends universal to all Ontario children.
There are limitations to this study. We did not look for direct associations between IBD care and time trends in health services use. Ontario health administrative data do not include information on clinical characteristics [e.g., disease phenotype or severity] or medications for individuals <65 years. As a result, we could not draw conclusions on the reasons these trends were observed, and our results may have been biased due to unmeasured confounding. In the absence of better indicators we used mean neighbourhood income quintile as a proxy for household income, and although it was validated in Ontario to reflect individual household income, we acknowledge it may not be a precise measure of individual household income. In addition, we excluded patients who ever had OHIP eligibility in LHIN [South East] 10, primarily comprising people who lived in Kingston, Ontario, who may have differed in demographic make-up compared with the rest of Ontario. However, we expected some level of demographic heterogeneity across LHINs. Furthermore, LHIN 10 residents could not be included because of inconsistencies in shadow billings in this region at the time of the study, which would have resulted in false event counts for residents of LHIN 10.
We did not conduct analyses stratified by factors previously associated with health services use in paediatric IBD [e.g., age and sex].13,28 However, we did not identify any clinically significant effect measure modification associated with these factors. As with studies conducted using routinely collected health administrative data, our study may have been subject to misclassification bias. To mitigate this risk, we used previously validated algorithms demonstrated to have high degrees of accuracy in identifying children with IBD and classifying IBD sub-type.17 The codes for surgery were validated in adults outside Ontario in the same hospitalisation database used in our study.21,22 However, the accuracy of these codes is uncertain among children in Ontario. Further, the codes used to identify IBD-related visits and hospitalisations were not validated. However, a panel of IBD experts chose and agreed upon these codes, and they have been used in previous studies.12,13,28 We continued to follow patients into adulthood, but did not evaluate the impact of transition from paediatric care to adult care [typically around the 18th birthday in Ontario]. Differences in paediatric and adult care may affect how patients use the health care system and may have led to differences in health services use in a way we were not able to capture in this study.
Although we were able to compare all-cause health services use between children with and without IBD, we were unable to compare surgical outcomes between these two populations. A non-IBD tracer surgery must be one that is not affected by having IBD or increased in IBD patients [e.g., appendectomy], and should have sufficient frequency in both children with and those without IBD to draw meaningful comparisons. We attempted to compare the frequency of orthopaedic surgery as a tracer event, but the frequency of events in IBD patients was insufficient to draw meaningful conclusions [data not shown]. However, IBD surgeries are performed only when there is a need [i.e., medical treatment has failed or complications arise], and changes in surgery rates should therefore reflect changes in IBD care, and not in the overall health system.
Although changing trends were commonly observed in children with CD and the overall IBD population, these trends were sometimes diminished or not replicated in children with UC. There are fewer children in Ontario with UC, and we may have been underpowered to detect significant trends. Alternatively, newer therapies [biologics] may not work as well in children with UC, or their use may not have been optimal in UC patients at the time of the study [e.g., less use of high-dose, rapid induction with infliximab in acute severe UC patients].63 Furthermore, since the biologics were approved later for use in children with UC, trends of decreasing health services use may not yet be apparent. Future studies assessing differences in the impact of biologics on health services use in UC compared with CD are needed.
In summary, we report decreasing hospitalisations and surgeries but increasing ED and outpatient visits in a population-based cohort of children with IBD. As the prevalence of paediatric-onset IBD continues to grow, IBD will place an increasing burden on health systems. Thus, it is important for health care management and policy makers to understand the evolving care needs of this population, ensuring patients receive best possible care and outcomes—with the goal of reducing the need for expensive hospitalisations and surgeries. Future studies identifying reasons for these observed trends are needed for continued improvement in care.
The data from this study are held securely in coded form at ICES. Data-sharing agreements prohibit ICES from making the dataset publicly available, but access may be granted to those who meet pre-specified criteria for confidential access, available at [www.ices.on.ca/DAS]. The full dataset creation plan and underlying analytical code are available from the authors upon request, understanding that the programs may rely upon coding templates or macros that are unique to ICES.
Funding
This work was supported by a Foundation Grant from the Canadian Institutes of Health Research [grant number 201409FDN-333131-FDN-CECC-164898]. MEK was supported by a Post-Doctoral Fellowship Award from the Canadian Institutes of Health Research [CIHR], Canadian Association of Gastroenterology [CAG], Crohn’s and Colitis Canada, and Mitacs Canada. DM is supported in part through a University of Ottawa, Faculty of Medicine, Distinguished Clinical Research Chair in Pediatric IBD. SM was supported by the Department of Medicine and Division of Gastroenterology and by a Tier 2 Clinical Research Chair in Inflammatory Bowel Diseases from the Faculty of Medicine at the University of Ottawa. EIB was supported by a New Investigator Award from the CIHR, CAG, and Crohn’s and Colitis Canada, and also by the Career Enhancement Program of the Canadian Child Health Clinician Scientist Program. This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health [MOH] and Ministry of Long-Term Care [MLTC]. The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOH and MLTC is intended or should be inferred.
Conflicts of Interest
GGK has received honoraria for speaking or consultancy from Abbvie, Janssen, Pfizer, and Takeda, and research support from Janssen, Abbvie, GlaxoSmith Kline, Merck, and Shire; he shares ownership of a patent: TREATMENT OF INFLAMMATORY DISORDERS, AUTOIMMUNE DISEASE, AND PBC. UTI Limited Partnership, assignee, Patent 62/ 555,397. EIB has acted as a legal consultant for Hoffman La-Roche Ltd and Peabody & Arnold LLP for matters unrelated to a medication used to treat inflammatory bowel disease.
Author Contributions
AKD: study concept, design, statistical analysis and interpretation of data, manuscript drafting. MEK: study concept, design, statistical analysis and interpretation of data, manuscript drafting and editing, supervision. DRM: study concept, design, interpretation of data, manuscript review and editing, supervision. SKM: study concept, design, interpretation of data, manuscript review and editing, supervision. GGK: study concept and design, manuscript review and editing. JD: study design, data support. GS: study design, data support. EIB: study concept, design, statistical analysis and interpretation of data, manuscript drafting and editing, supervision, data acquisition, obtained funding. Conference presentations: Canadian Digestive Diseases Week [Research Topics], Montreal, QC, Canada, 2020.
Supplementary Material
Acknowledgements
Parts of this material are based on data and/or information compiled and provided by Canadian Institute for Health Information [CIHI]. However, the analyses, conclusions, opinions and statements expressed in the material are those of the author[s], and not necessarily those of CIHI.
References
- 1. Walters TD, Griffiths AM. Mechanisms of growth impairment in pediatric Crohn’s disease. Nat Rev Gastroenterol Hepatol 2009;6:513–23. [DOI] [PubMed] [Google Scholar]
- 2. Malmborg P, Mouratidou N, Sachs MC, et al. Effects of childhood-onset inflammatory bowel disease on school performance: a nationwide population-based cohort study using Swedish Health and Educational Registers. Inflamm Bowel Dis 2019;25:1663–73. [DOI] [PubMed] [Google Scholar]
- 3. Szigethy EM, Youk AO, Benhayon D, et al. Depression subtypes in pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2014;58:574–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Clark JG, Srinath AI, Youk AO, et al. Predictors of depression in youth with Crohn disease. J Pediatr Gastroenterol Nutr 2014;58:569–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Reigada LC, Bruzzese JM, Benkov KJ, et al. Illness-specific anxiety: implications for functioning and utilization of medical services in adolescents with inflammatory bowel disease. J Spec Pediatr Nurs 2011;16:207–15. [DOI] [PubMed] [Google Scholar]
- 6. Carroll MW, Kuenzig ME, Mack DR, et al. The impact of inflammatory bowel disease in Canada 2018: children and adolescents with IBD. J Can Assoc Gastroenterol 2019;2:49–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kuenzig ME, Benchimol EI, Lee L, et al. The impact of inflammatory bowel disease in Canada 2018: direct costs and health services utilization. J Can Assoc Gastroenterol 2019;2:S17–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Benchimol EI, Fortinsky KJ, Gozdyra P, Van Den Heuvel M, Van Limbergen J, Griffiths AM. Epidemiology of pediatric inflammatory bowel disease: a systematic review of international trends. Inflamm Bowel Dis 2011;17:423–39. [DOI] [PubMed] [Google Scholar]
- 9. Kappelman MD, Rifas-Shiman SL, Porter CQ, et al. Direct health care costs of Crohn’s disease and ulcerative colitis in US children and adults. Gastroenterology 2008;135:1907–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. El-Matary W, Kuenzig ME, Singh H, et al. Disease-associated costs in children with inflammatory bowel disease: a systematic review. Inflamm Bowel Dis 2020;26:206. [DOI] [PubMed] [Google Scholar]
- 11. Benchimol EI, Manuel DG, Mojaverian N, et al. Health services utilization, specialist care, and time to diagnosis with inflammatory bowel disease in immigrants to Ontario, Canada: a population-based cohort study. Inflamm Bowel Dis 2016;22:2482–90. [DOI] [PubMed] [Google Scholar]
- 12. Benchimol EI, Guttmann A, To T, Rabeneck L, Griffiths AM. Changes to surgical and hospitalisation rates of pediatric inflammatory bowel disease in Ontario, Canada [1994–2007]. Inflamm Bowel Dis 2011;17:2153–61. [DOI] [PubMed] [Google Scholar]
- 13. Benchimol EI, Mack DR, Nguyen GC, et al. Incidence, outcomes, and health services burden of very early onset inflammatory bowel disease. Gastroenterology 2014;147:803–13.e7; quiz e14–5. [DOI] [PubMed] [Google Scholar]
- 14. Frolkis AD, Dykeman J, Negrón ME, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology 2013;145:996–1006. [DOI] [PubMed] [Google Scholar]
- 15. Targownik LE, Singh H, Nugent Z, Bernstein CN. The epidemiology of colectomy in ulcerative colitis: results from a population-based cohort. Am J Gastroenterol 2012;107:1228–35. [DOI] [PubMed] [Google Scholar]
- 16. Kaplan GG, Seow CH, Ghosh S, et al. Decreasing colectomy rates for ulcerative colitis: a population-based time trend study. Am J Gastroenterol 2012;107:1879–87. [DOI] [PubMed] [Google Scholar]
- 17. Benchimol EI, Guttmann A, Griffiths AM, et al. Increasing incidence of paediatric inflammatory bowel disease in Ontario, Canada: evidence from health administrative data. Gut 2009;58:1490–7. [DOI] [PubMed] [Google Scholar]
- 18. Benchimol EI, Bernstein CN, Bitton A, et al. Trends in epidemiology of pediatric inflammatory bowel disease in Canada: distributed network analysis of multiple population-based provincial health administrative databases. Am J Gastroenterol 2017;112:1120–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Institute for Clinical Evaluative Sciences. ICES Data Dictionary. Version 3.0.12. https://datadictionary.ices.on.ca/Applications/DataDictionary/Default.aspx Accessed June 1, 2018.
- 20. Benchimol EI, Guttmann A, Mack DR, et al. Validation of international algorithms to identify adults with inflammatory bowel disease in health administrative data from Ontario, Canada. J Clin Epidemiol 2014;67:887–96. [DOI] [PubMed] [Google Scholar]
- 21. Ma C, Moran GW, Benchimol EI, et al. Surgical rates for Crohn’s disease are decreasing: a population-based time trend analysis and validation study. Am J Gastroenterol 2017;112:1840–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ma C, Crespin M, Proulx MC, et al. Postoperative complications following colectomy for ulcerative colitis: a validation study. BMC Gastroenterol 2012;12:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Benchimol EI, Kuenzig ME, Bernstein CN, et al. ; Canadian Gastro-Intestinal Epidemiology Consortium. Rural and urban disparities in the care of Canadian patients with inflammatory bowel disease: a population-based study. Clin Epidemiol 2018;10:1613–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Payne EH, Gebregziabher M, Hardin JW, Ramakrishnan V, Egede LE. An empirical approach to determine a threshold for assessing overdispersion in Poisson and negative binomial models for count data. Commun Stat Simul Comput 2018;47:1722–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hyams J, Crandall W, Kugathasan S, et al. ; REACH Study Group. Induction and maintenance infliximab therapy for the treatment of moderate-to-severe Crohn’s disease in children. Gastroenterology 2007;132:863–73; quiz 1165–6. [DOI] [PubMed] [Google Scholar]
- 26. Benchimol EI, Kaplan GG, Otley AR, et al. Rural and urban residence during early life is associated with a lower risk of inflammatory bowel disease: a population-based inception and birth cohort study. Am J Gastroenterol 2017;112:1412–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sonnenberg A. Disability from inflammatory bowel disease among employees in West Germany. Gut 1989;30:367–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Benchimol EI, To T, Griffiths AM, Rabeneck L, Guttmann A. Outcomes of pediatric inflammatory bowel disease: socioeconomic status disparity in a universal-access healthcare system. J Pediatr 2011;158:960–7.e1–4. [DOI] [PubMed] [Google Scholar]
- 29. Levine A, Griffiths A, Markowitz J, et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis 2011;17:1314–21. [DOI] [PubMed] [Google Scholar]
- 30. Glazier RH, Creatore MI, Agha MM, Steele LS; Inner City Toronto Time Trends Working Group . Socioeconomic misclassification in Ontario’s Health Care Registry. Can J Public Health 2003;94:140–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Singh H, Nugent Z, Targownik LE, El-Matary W, Brownell M, Bernstein CN. Health care use by a population-based cohort of children with inflammatory bowel disease. Clin Gastroenterol Hepatol 2015;13:1302–9.e3. [DOI] [PubMed] [Google Scholar]
- 32. Rahman A, Jairath V, Feagan BG, et al. Declining hospitalisation and surgical intervention rates in patients with Crohn’s disease: a population-based cohort. Aliment Pharmacol Ther 2019;50:1086–93. [DOI] [PubMed] [Google Scholar]
- 33. Murthy SK, Begum J, Benchimol EI, et al. Introduction of anti-TNF therapy has not yielded expected declines in hospitalisation and intestinal resection rates in inflammatory bowel diseases: a population-based interrupted time series study. Gut 2020;69:274–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. To T, Guttmann A, Dick PT.. Inpatient and Day Surgery Use by Children in Ontario: ICES Research Atlas. Toronto, ON: Institute for Clinical Evaluation Studies [ICES]; 2001. [Google Scholar]
- 35. Evans C, Kingwell E, Zhu F, Oger J, Zhao Y, Tremlett H. Hospital admissions and MS: temporal trends and patient characteristics. Am J Manag Care 2012;18:735–42. [PubMed] [Google Scholar]
- 36. Marrie RA, Elliott L, Marriott J, et al. Dramatically changing rates and reasons for hospitalisation in multiple sclerosis. Neurology 2014;83:929–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rai SK, Antonio J, Na-Zubieta A, et al. Trends in gout and rheumatoid arthritis hospitalisations in Canada from 2000 to 2011. Arthritis Care Res 2017;69:758–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Canadian Institute for Health Information. Asthma Hospitalisations Among Children and Youth in Canada: Trends and Inequalities. Ottawa, ON: CIHI; 2018. [Google Scholar]
- 39. Crighton EJ, Mamdani MM, Upshur RE. A population based time series analysis of asthma hospitalisations in Ontario, Canada: 1988 to 2000. BMC Health Serv Res 2001;1:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Curtis JR, To T, Muirhead S, Cummings E, Daneman D. Recent trends in hospitalisation for diabetic ketoacidosis in Ontario children. Diabetes Care 2002;25:1591–6. [DOI] [PubMed] [Google Scholar]
- 41. Colantonio A, Croxford R, Farooq S, Laporte A, Coyte PC. Trends in hospitalisation associated with traumatic brain injury in a publicly insured population, 1992–2002. Trauma 2009;66:179–83. [DOI] [PubMed] [Google Scholar]
- 42. Fu TS, Jing R, McFaull SR, Cusimano MD. Recent trends in hospitalisation and in-hospital mortality associated with traumatic brain injury in Canada: a nationwide, population-based study. J Trauma Acute Care Surg 2015;79:449–54. [DOI] [PubMed] [Google Scholar]
- 43. Checchin D, Freeman M, Terres JAR. Temporal trends and regional variation in hospitalisation rates for stroke in Canada, 2002–2009 [Abstract 331]. Can J Cardiol 2012;28:S220. [Google Scholar]
- 44. Pant C, Anderson MP, Deshpande A, et al. Trends in hospitalisations of children with inflammatory bowel disease within the United States from 2000 to 2009. J Investig Med 2013;61:1036–8. [DOI] [PubMed] [Google Scholar]
- 45. Meregaglia M, Banks H, Fattore G. Hospital burden and gastrointestinal surgery in inflammatory bowel disease patients in Italy: a retrospective observational study. J Crohns Colitis 2015;9:853–62. [DOI] [PubMed] [Google Scholar]
- 46. Sandberg KC, Davis MM, Gebremariam A, Adler J. Increasing hospitalisations in inflammatory bowel disease among children in the United States, 1988–2011. Inflamm Bowel Dis 2014;20:1754–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Nugent Z, Singh H, Targownik LE, Strome T, Snider C, Bernstein CN. Predictors of emergency department use by persons with inflammatory bowel diseases: a population-based study. Inflamm Bowel Dis 2016;22:2907–16. [DOI] [PubMed] [Google Scholar]
- 48. Pant C, Deshpande A, Fraga-Lovejoy C, et al. Emergency department visits related to inflammatory bowel disease: results from nationwide emergency department sample. J Pediatr Gastroenterol Nutr 2015;61:282–4. [DOI] [PubMed] [Google Scholar]
- 49. Huh G, Yoon H, Choi YJ, et al. Correction: trends in emergency department visits and hospitalisation rates for inflammatory bowel disease in the era of biologics. PLoS One 2019;14:e0216768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ma C, Smith M, Guizzetti L, et al. Assessing national trends and disparities in ambulatory, emergency department, and inpatient visits for inflammatory bowel disease in the United States [2005–2016]. Clin Gastroenterol Hepatol 2020;18:2500–09.e1.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Booth GL, Hux JE, Fang J, Chan BT. Time trends and geographic disparities in acute complications of diabetes in Ontario, Canada. Diabetes Care 2005;28:1045–50. [DOI] [PubMed] [Google Scholar]
- 52. Nakhla M, Rahme E, Simard M, Guttmann A. Outcomes associated with a pediatric clinical diabetes network in Ontario: a population-based time-trend analysis. CMAJ Open 2017;5:E586–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sullivan PW, Ghushchyan V, Kavati A, et al. Trends in asthma control, treatment, health care utilization, and expenditures among children in the United States by place of residence: 2003–2014. J Allergy Clin Immunol Pract 2019;7:1835–42. [DOI] [PubMed] [Google Scholar]
- 54. Marrie RA, O’Mahony J, Maxwell CJ, et al. ; Canadian Pediatric Demyelinating Disease Network. High rates of health care utilization in pediatric multiple sclerosis: a Canadian population-based study. PLoS One 2019;14:e0218215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Akinbami LJ, Schoendorf KC. Trends in childhood asthma: prevalence, health care utilization, and mortality. Pediatrics 2002;110:315–22. [DOI] [PubMed] [Google Scholar]
- 56. Guttmann A, Lam K, Schultz S, et al., editors. Primary Care in Ontario: ICES Atlas. Toronto, ON: Institute for Clinical Evaluative Sciences; 2006. [Google Scholar]
- 57. Nguyen GC, Bouchard S, Diong C; Promoting Access and Care through Centres of Excellence [PACE] Network . Access to specialists and emergency department visits in inflammatory bowel disease: a population-based study. J Crohns Colitis 2019;13:330–6. [DOI] [PubMed] [Google Scholar]
- 58. Nguyen GC, Nugent Z, Shaw S, Bernstein CN. Outcomes of patients with Crohn’s disease improved from 1988 to 2008 and were associated with increased specialist care. Gastroenterology 2011;141:90–7. [DOI] [PubMed] [Google Scholar]
- 59. Adler J, Lin CC, Gadepalli SK, Dombkowski KJ. Association between steroid-sparing therapy and the risk of perianal fistulizing complications among young patients with Crohn disease. JAMA Netw Open 2020;3:e207378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ashton JJ, Borca F, Mossotto E, et al. Increased prevalence of anti-TNF therapy in paediatric inflammatory bowel disease is associated with a decline in surgical resections during childhood. Aliment Pharmacol Ther 2019;49:398–407. [DOI] [PubMed] [Google Scholar]
- 61. Lichtenstein GR, Yan S, Bala M, Blank M, Sands BE. Infliximab maintenance treatment reduces hospitalisations, surgeries, and procedures in fistulizing Crohn’s disease. Gastroenterology 2005;128:862–9. [DOI] [PubMed] [Google Scholar]
- 62. Costa J, Magro F, Caldeira D, Alarcão J, Sousa R, Vaz-Carneiro A. Infliximab reduces hospitalisations and surgery interventions in patients with inflammatory bowel disease: a systematic review and meta-analysis. Inflamm Bowel Dis 2013;19:2098–110. [DOI] [PubMed] [Google Scholar]
- 63. Rosen MJ, Minar P, Vinks AA. Review article: applying pharmacokinetics to optimise dosing of anti-TNF biologics in acute severe ulcerative colitis. Aliment Pharmacol Ther 2015;41:1094–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.