Abstract
Background
HIV testing among men is paramount in the prevention, diagnosis, and treatment of HIV. There is limited literature in understanding the socio-economic and demographic factors associated with never having tested for HIV among sexually active men aged 15 – 54 across the four administrative regions of Uganda. The purpose of this study is to investigate the socio-economic and demographic factors associated with never having tested for HIV among sexually active men aged 15 – 54 across the four administrative regions in the country.
Methods
The study used a cross-sectional research design to examine factors associated with never having tested for HIV among 4,168 sexually active men (15 – 54 years) across four administrative regions of Uganda using data from 2016 Uganda Demographic and Health Survey (UDHS). Frequency distributions, Pearson chi-square tests, and multivariable logistic regression were used to establish the association between never having tested for HIV among sexually active men (15 – 54 years) and selected independent variables across regions.
Results
About 20% of sexually active men (15 – 54 years) never tested for HIV across regions of the country. The major correlates amidst variability of never testing for HIV among sexually active men across regions were; educational level and marital status. Age, religious status, wealth quintile, worked in the last 12 months, circumcised, and one sexual partner in the last 12 months were only correlates of never having tested for HIV among respondents in particular regions of the country.
Conclusion
Findings in the study suggest promotion of male education, and suggest further investigation into the relationship between HIV non-testing among sexually active men (15 – 54 years) and being married across regions of the country. The study also proposes appreciation of regional differences in the outcome of HIV non-testing and suggests that efforts be focused on addressing regional differences in order to attain high HIV testing among sexually active men (15 – 54 years) across regions of Uganda, and thus reduce HIV related morbidity and mortality.
Keywords: Never tested, sexually active men, HIV, regional, Uganda
Background
Human Immunodeficiency Virus (HIV) remains a major global health concern that weakens body immunity, and causes many HIV related deaths [1]. HIV/AIDS is a main cause of morbidity and mortality in sub-Saharan Africa [2, 3]. Regardless of rise in uptake of Anti-Retroviral Therapy (ART) in the mid-2000s and the consequent decline in mortality within sub-Saharan Africa, eastern and southern Africa is the hardest hit region by HIV, with more than 54% (20.7 million) of the total number of people living with the disease, including 7.3 million HIV positive males [4, 5]. Men and women in the region are prone to contracting HIV, however men are less likely to test for HIV, more likely to be diagnosed with advanced stages of the disease and more likely to be associated with HIV related deaths because of their poorer testing uptake and treatment [6–12]. HIV testing is a crucial approach in reducing HIV associated morbidity and mortality outcomes [13–15]. According to the World Health Organization (WHO) and Center for Disease Control (CDC), HIV testing is an essential pathway to prevention and management of HIV [16, 17]. It equips individuals with the knowledge to evade infection, as well as a prerequisite to initiate ART [18]. Notably, differences in HIV prevalence and proportion of never having tested for HIV among men in sub-Saharan Africa exist, even within countries [12, 19].
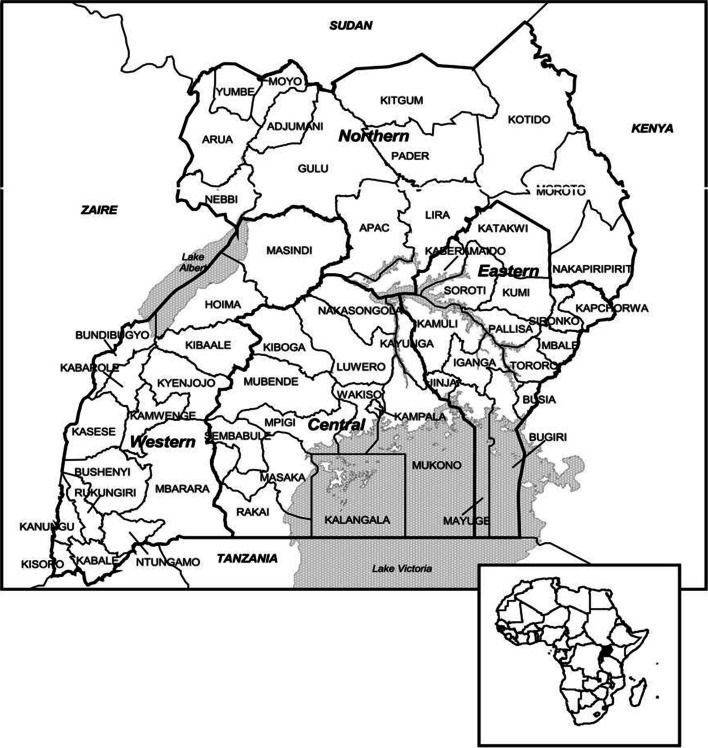
Uganda has four administrative regions which include; eastern, western, northern and central regions [20]. These regions differ in relation to social context, poverty share, and health infrastructure. For example; northern region is the least economically and socially developed region of Uganda, central and western regions have better health infrastructure compared to other regions [21, 22]. Historically, central region was the path of social services into the country due to earlier contact with western influences [23]. Consequently, most social services first became rooted in the area before spreading out to other regions of the country [23–25]. Central region also hosts the national capital, Kampala, and is the most urbanized [26, 27]. Systems of education, health, and communication are better in central region than in other regions [21]. In contrast, northern region has gone through over two decades of insurgency [28, 29] which has adversely affected the ability to manage health challenges [30]. Literature shows that social context, poverty, and health infrastructure have an impact on never having tested for HIV among men [31–36].
In Uganda, the proportion of men who have never tested for HIV is high (27%), yet over 80% of all men across the country have knowledge on where to obtain HIV testing services [37, 38] amidst availability of free HIV testing [39, 40]. Men’s HIV testing coverage in the country is a major hindrance to HIV decline [32, 41], and achievement of the global commitment to reduce and end the epidemic by 2030 [42, 43]. Consequently, emphasis ought to be placed in understanding the challenges men face in testing for HIV. Studies on drivers of never having tested for HIV among men in Uganda indicate among others; fear of being tested, older age, fear of knowing HIV status, absence of testing interest, men’s view of clinics as places for females, culture, facilities, fear of testing-related gossip, distrust of HIV testing methods, peer and economic influence [10, 32, 44–56], without examining determinants of never having tested for HIV among sexually active men (15 -54 years) across regions of Uganda. In Uganda, regional differences in never having tested for HIV among men exist, for instance; highest in Karamoja region (60%), trailed by Bukedi region (42%) and lowest in Greater Kampala (14%), betwixt availability of HIV testing services [20, 57]. These variations in never having tested for HIV among men across regions of the country signify a possibility of regional differences in determinants of never having tested for HIV.
Methods
Study design, data sources and population
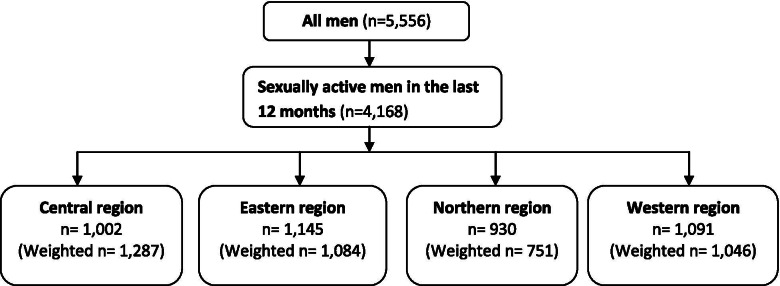
The present study used a cross-sectional research design. The 2016 Uganda Demographic and Health Survey (UDHS) was the premise of the present study. The 2016 UDHS was a national cross-sectional survey that captured the socio-economic, and demographic related issues concerning men aged 15 - 54. A two-stage cluster sampling was used in acquiring a representative sample of 5,336 men (15 – 54 years). Selection of clusters was undertaken in the first stage, whilst selection of the households was handled in the second stage of cluster sampling. The present study only selected 4,168 men who reported to have had sexual intercourse in the last 12 months. Notably, sexual activity is a key aspect through which HIV is transmitted [58]. Out of the 15 regions that were captured in the 2016 UDHS, the present study grouped the regions into four (4) administrative regions of Uganda; central, eastern, northern and western region (10). Study approval by the Institutional Review Board (IRB) was not applicable, since the research utilized secondary data. While using STATA 13.1, this study weighted and adjusted the 2016 UDHS dataset for non-responses in order to ascertain sample representativeness. These weighted counts can and usually will be non-integers. In order to address multicollinearity, a variance inflation factor (VIF) test was undertaken [59]. In the test, we examined our data and omitted extremely correlated covariates from the models. We as well did a multiple regression analysis including religion for sensitivity analysis. For additional information on the sampling procedures, exhaustive clarification can be obtained elsewhere [38]. Figure 1 is a flow chart that demonstrates how the study sample was obtained. Figure 2 is a map of Uganda showing the four administrative regions and their respective districts [60].
Fig 1.
Origin of the sample used for the study
Fig. 2.
Regions of Uganda and their respective districts (Source: UBOS and ORC Macro, 2001)
Study variables
Outcome variable
The outcome variable in this present study was self-reported lifetime history of HIV testing among men aged 15 – 54. The 2016 UDHS men’s questionnaire, asked respondents whether they have ever tested for HIV (‘have you ever tested for HIV?’). From the question, a binary outcome variable was produced, and coded: ‘1’ never tested for HIV and ‘0’ ever tested for HIV (yes =1, no = 0).
Explanatory variable
This study selected explanatory variables of HIV non-tested among sexually active men (15 – 54 years) based on literature review [12, 61–65] and the range of the 2016 UDHS variables [38]. The chosen explanatory variables are; age (grouped into four distinct categories; 15 – 24, 25 – 34, 35 – 44, and 45 – 54), education status (no education, primary, secondary, and higher), residence (categorized as: urban, and rural), religious status (Catholic, Anglican, Muslim, Pentecostal, and others), wealth quintile (poorest, poorer, middle, richer, and richest), worked in the last 12 months (yes/ no), ever given gifts or other goods to have sex in the last 12 months (no/yes), marital status (never married, married, widowed, and separated), circumcised (no/yes), and number of sexual partners, excluding spouse in the last 12 months (No sexual partner, 1 sexual partner, 2 and above sexual partners).
Ethical considerations
Demographic and Health Survey (DHS) dataset can freely be accessed by the public upon submission of a formal request. Therefore, as a pre-requisite, authors submitted a proposal to DHS Program/ICF International which later approved the download and use of the 2016 UDHS dataset. Further information on ethical concerns is elucidated elsewhere [38].
Statistical analysis
This study utilized STATA 13.1 in executing the three stages of statistical analyses. In the first stage, characteristics of study respondents across regions of the country were presented using descriptive statistics. In the second stage of the analysis, associations between each explanatory variable and outcome variable across regions of the country were evaluated with the Pearson chi-square test (x2). In the third stage of analysis, the study used multivariable logistic regression to model the associations between lifetime HIV testing history and the explanatory variables among sexually active men, across regions. At the second stage of analysis (bivariate), some variables were not statistically significant across regions (residence, religious status, wealth quintile, worked in the last 12 months, ever given gifts or other goods to have sex in the last 12 months, and number of sexual partners in the last 12 months), however, they were retained for further analysis due to their published associations with HIV testing history [12, 64–68]. Odds ratios (ORs) and 95% confidence intervals were measured and adopted at the multivariable logistic regression. Further, p-values less than 0.001 reported very strong relationship between variables, p-values less than 0.01 showed a strong relationship between variables, and p-values less than 0.05 demonstrated moderate relationship between variables [69].
Results
Descriptive findings
Results in Table 1 show that 19.8% of respondents in Uganda have never tested for HIV, with variations across regions; eastern region (23.6%) had the largest proportion of respondents who have never tested for HIV, unlike northern region (15.1%). In Table 1, central, eastern, northern and western regions, had the largest proportion of respondents with primary education (44.8%, 54.8%, 56.8%, and 60.3%, respectively). Majority of the respondents in the country were catholics (39.9%) and anglicans (34.5%), with the largest proportion of respondents in central (39.1%) and northern regions (61.5%), whereas in eastern and western regions, the largest proportion of respondents were anglicans (41.8% and 42.6%, respectively). Results (Table 1) show that majority of the respondents in the country were in the richest wealth quintile (24.6%); however, differences across regions indicated that central region (41.3%) had the largest proportion of respondents in the richest wealth quintile category, while northern region had the largest proportion in the poorest wealth quintile (45.1%). Across the four regions, over three-quarters had ever been married; the largest proportion married at least once were in northern region (82.7%) (Table 1). Results in Table 1 show that 53.8% of the respondents reported not have been circumcised in the entire country, with the largest proportion in eastern (57.1%) and central region (52.5%), and lowest in northern region (24.1%). Besides, results in Table 1 also indicate that majority of respondents in the country had no sexual partner in the last 12 months (62.3%), followed by respondents with 1 sexual partner in the last 12 months (29.4%), and least are those who had 2 and more sexual partners in the last 12 months (8.3%). Notable, regional variations indicate that the highest proportion of the respondents with no sexual partner, 1 sexual partner, and 2 and more sexual partners in the last 12 months were in northern (66.8%), central (34.4%), and central region (11.0), respectively.
Table 1.
Lifetime HIV testing history, socio-economic and demographic characteristics of sexually active men (15 – 54 years) across regions of Uganda
| Characteristics | Regions | Uganda (n=4,168) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Central (n=1,002) |
Eastern (n=1,145) |
Northern (n=930) |
Western (n=1,091) |
|||||||
| n | % | n | % | n | % | n | % | n | % | |
| HIV testing status | ||||||||||
| Never tested | 187 | 18.7 | 271 | 23.6 | 140 | 15.1 | 223 | 20.4 | 823 | 19.8 |
| Ever tested | 815 | 81.3 | 875 | 76.4 | 790 | 84.9 | 868 | 79.6 | 3345 | 80.2 |
| Age | ||||||||||
| 15 – 24 | 292 | 29.2 | 348 | 30.4 | 250 | 26.9 | 321 | 29.4 | 1214 | 29.1 |
| 25 – 34 | 361 | 36.0 | 358 | 31.3 | 331 | 35.5 | 360 | 33.0 | 1415 | 33.9 |
| 35 – 44 | 232 | 23.2 | 281 | 24.6 | 200 | 21.5 | 249 | 22.8 | 966 | 23.2 |
| 45 – 54 | 116 | 11.6 | 158 | 13.8 | 149 | 16.0 | 161 | 14.8 | 574 | 13.8 |
| Education level | ||||||||||
| No education | 47 | 4.6 | 46 | 4.0 | 38 | 4.0 | 59 | 5.4 | 191 | 4.6 |
| Primary | 449 | 44.8 | 628 | 54.8 | 528 | 56.8 | 658 | 60.3 | 2228 | 53.5 |
| Secondary | 309 | 30.9 | 353 | 30.8 | 205 | 22.1 | 268 | 24.6 | 1154 | 27.7 |
| Higher | 197 | 19.7 | 118 | 10.3 | 159 | 17.1 | 106 | 9.7 | 595 | 14.3 |
| Residence | ||||||||||
| Urban | 460 | 45.9 | 174 | 15.2 | 120 | 12.9 | 239 | 21.9 | 1081 | 25.9 |
| Rural | 542 | 54.1 | 971 | 84.8 | 810 | 87.1 | 852 | 78.1 | 3087 | 74.1 |
| Religious status | ||||||||||
| Catholic | 391 | 39.1 | 330. | 25.5 | 573 | 61.5 | 440 | 40.3 | 1664 | 39.9 |
| Anglican | 274 | 27.4 | 478 | 41.8 | 231 | 24.8 | 464 | 42.6 | 1437 | 34.5 |
| Muslim | 202 | 20.1 | 221 | 19.3 | 55 | 5.9 | 62 | 5.7 | 572 | 13.7 |
| Pentecostal | 113 | 11.2 | 134 | 11.7 | 60 | 6.5 | 65 | 5.9 | 382 | 9.2 |
| Others | 22 | 2.2 | 20 | 1.7 | 12 | 1.3 | 60 | 5.5 | 114 | 2.7 |
| Wealth quintile | ||||||||||
| Poorest | 27 | 2.7 | 241 | 21.0 | 420 | 45.1 | 82 | 7.5 | 681 | 16.3 |
| Poorer | 71 | 7.1 | 281 | 24.5 | 218 | 23.4 | 205 | 18.8 | 729 | 17.5 |
| Middle | 154 | 15.3 | 258 | 22.6 | 97 | 10.5 | 314 | 28.7 | 821 | 19.7 |
| Richer | 261 | 26.1 | 216 | 18.9 | 109 | 11.7 | 296 | 27.1 | 912 | 21.9 |
| Richest | 489 | 48.8 | 149 | 13.0 | 86 | 9.3 | 195 | 17.8 | 1025 | 24.6 |
| Worked in the last 12 months | ||||||||||
| No | 21 | 2.1 | 17 | 1.5 | 13 | 1.4 | 34 | 3.1 | 87 | 2.1 |
| Yes | 981 | 97.9 | 1128 | 98.5 | 917 | 98.6 | 1057 | 96.9 | 4081 | 97.9 |
| Marital status | ||||||||||
| Never married | 307 | 30.6 | 237 | 20.7 | 173 | 18.6 | 246 | 22.6 | 994 | 23.8 |
| Ever married | 695 | 69.4 | 908 | 79.3 | 757 | 81.4 | 845 | 77.4 | 3174 | 76.2 |
| Ever given gifts or other goods to have sex in the last 12 months | ||||||||||
| No | 875 | 87.3 | 1080 | 94.3 | 917 | 98.6 | 1006 | 92.2 | 3851 | 92.4 |
| Yes | 127 | 12.7 | 65 | 5.7 | 14 | 1.4 | 85 | 7.8 | 317 | 7.6 |
| Circumcised | ||||||||||
| No | 476 | 47.5 | 492 | 42.9 | 706 | 75.9 | 622 | 57.0 | 2243 | 53.8 |
| Yes | 526 | 52.5 | 653 | 57.1 | 224 | 24.1 | 469 | 43.0 | 1925 | 46.2 |
| Number of sexual partners in the last 12 months | ||||||||||
| No sexual partner | 548 | 54.6 | 791 | 69.1 | 621 | 66.8 | 669 | 61.3 | 2595 | 62.3 |
| 1 sexual partner | 345 | 34.4 | 293 | 25.6 | 254 | 27.3 | 313 | 28.7 | 1226 | 29.4 |
| 2 & above sexual partners | 110 | 11.0 | 61 | 5.3 | 54 | 5.8 | 109 | 10.0 | 347 | 8.3 |
Appropriate weights were used for the analyses.
An assessment of variations in socio-economic and demographic factors by HIV testing status among sexually active men (15 – 54 years) across regions of Uganda
In Table 2, results show an assessment of socio-economic and demographic factors by HIV testing status among sexually active men (15 – 54 years) across regions of the country. Table 2 shows results at bivariate level of analysis; herein, Pearson’s Chi-square tests (x2) were performed, specifically highlighting the relationship between respondents’ socio-economic and demographic factors and HIV testing status across regions. In Table 2, results show that age, education level, residence, wealth quintile, worked in the last 12 months, and marital status were significantly associated with HIV testing status among sexually active men (15 – 54 years) in Uganda, with variations across region; age, educational level, and marital status were the only variables that were significantly associated with HIV testing status among sexually active men (15 – 54 years) across regions (p-value < 0.001). Nevertheless, this study adopted all the variables at the multivariable level of analysis because of their importance in explaining HIV non-testing among sexually active men [12, 61–65].
Table 2.
Distribution of socio-economic and demographic factors by HIV testing status among sexually active men aged 15 – 54 across regions
| Characteristics | Regions | Uganda | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Central | Eastern | Northern | Western | |||||||
| Ever tested n (%) |
Never tested n (%) |
Ever tested n (%) |
Never tested n (%) |
Ever tested n (%) |
Never tested n (%) |
Ever tested n (%) |
Never tested n (%) |
Ever tested n (%) |
Never tested n (%) |
|
| Age | ||||||||||
| 15 – 24 | 217 (74.3) | 75 (25.7) | 237 (68.2) | 110 (31.8) | 191 (76.2) | 60 (23.8) | 217 (67.6) | 104 (32.4) | 865 (71.3) | 349 (28.7) |
| 25 – 34 | 314 (87.0) | 47 (13.0) | 282 (78.7) | 76 (21.3) | 307 (93.0) | 23 (7.0) | 316 (87.8) | 44 (12.2) | 1222 (86.3) | 193 (14.7) |
| 35 – 44 | 187 (80.6) | 45 (19.5) | 226 (80.4) | 55 (19.6) | 178 (88.8) | 23 (11.2) | 213 (85.3) | 37 (14.7) | 802 (83.1) | 164 (16.9) |
| 45 – 54 | 97 (83.0) | 20 (17.0) | 130 (82.1) | 28 (17.9) | 114 (76.5) | 35 (23.5) | 123 (76.2) | 38 (23.8) | 457 (79.6) | 117 (20.4) |
| χ2= 3.5524, p=0.0142 | χ2= 4.2277, p≤0.0064 | χ2= 11.8350, p≤0.001 | χ2= 13.4259, p≤0.001 | χ2= 21.4522, p≤0.001 | ||||||
| Education level | ||||||||||
| No education | 25 (53.9) | 22 (46.1) | 29 (61.9)) | 18 (38.1) | 13 (33.3) | 25 (66.7) | 43 (71.5) | 17 (28.5) | 110 (57.7) | 81(42.3) |
| Primary | 338 (75.3) | 111 (24.7) | 441 (70.3) | 187 (29.7) | 430 (81.3) | 99 (18.7) | 507 (77.3) | 150 (22.7) | 1686 (75.7) | 543 (24.4) |
| Secondary | 261 (84.3) | 48 (15.7) | 294 (83.5) | 58 (16.5) | 195 (94.8) | 11 (5.2) | 219 (81.8) | 49 (18.2) | 981 (85.0) | 173 (15.0) |
| Higher | 191 (96.9) | 6 (3.1) | 110 (93.3) | 8 (6.7) | 153 (96.6) | 5 (3.4) | 99 (93.0) | 7 (7.0) | 568 (95.5) | 27 (4.5) |
| χ2= 16.6242, p≤0.001 | χ2= 11.0568, p≤0.001 | χ2= 39.2516, p≤0.001 | χ2= 5.1079, p=0.0018 | χ2= 46.9833, p≤0.001 | ||||||
| Residence | ||||||||||
| Urban | 404 (88.0) | 55 (12.0) | 141 (80.9) | 33 (19.1) | 107 (89.2) | 13 (10.8) | 191 (80.0) | 48 (20.0) | 923 (85.3) | 159 (14.7) |
| Rural | 410 (75.7) | 132 (24.3) | 734 (75.6) | 237 (24.4) | 683 (84.3) | 127 (15.7) | 677 (79.5) | 175 (20.5) | 2423 (78.5) | 665 (21.5) |
| χ2= 15.5287, p≤0.001 | χ2= 1.0799, p=0.2991 | χ2= 1.9159, p=0.1668 | χ2= 0.0210, p=0.8848 | χ2= 12.5572, p=0.004 | ||||||
| Religious status | ||||||||||
| Catholics | 311 (79.6) | 80 (20.4) | 225 (76.8) | 68 (23.2) | 486 (84.9) | 86 (15.1) | 337 (76.6) | 103 (23.4) | 1329 (79.9) | 335 (20.1) |
| Anglican | 230 (83.9) | 44 (16.1) | 371 (77.5) | 108 (22.5) | 200 (86.7) | 31 (13.3) | 375 (80.7) | 90 (19.3) | 1167 (81.2) | 270 (18.8) |
| Muslim | 153 (76.2) | 48 (23.8) | 153 (69.4) | 68 (30.6) | 44 (81.0) | 10 (19.0) | 53 (86.2) | 9 (13.8) | 429 (75.1) | 142 (24.9) |
| Pentecostal | 100 (88.3) | 13 (11.7) | 111 (83.0) | 23 (17.0) | 55 (90.6) | 6 (9.4) | 55 (85.2) | 10 (14.8) | 330 (86.3) | 52 (13.7) |
| Others | 20 (93.3) | 2 (6.7) | 15 (76.4) | 5 (23.6) | 5 (40.2) | 7 (59.8) | 48 (79.8) | 12 (20.2) | 90 (79.2) | 24 (20.8) |
| χ2= 2.2809, p=0.0639 | χ2=1.6889, p=0.1516 | χ2= 4.1604, p=0.037 | χ2= 1.0481, p=0.3765 | χ2= 3.3290, p=0.0105 | ||||||
| Wealth quintile | ||||||||||
| Poorest | 19 (69.5) | 8 (30.5) | 178 (73.8) | 63 (26.3) | 343 (81.7) | 77 (18.3) | 50 (60.7) | 32 (39.3) | 517 (76.0) | 163 (24.0) |
| Poorer | 44 (62.4) | 27 (37.6) | 210 (74.9) | 70 (25.1) | 188 (86.3) | 30 (13.7) | 158 (76.9) | 47 (23.1) | 559 (76.7) | 170 (23.3) |
| Middle | 109 (71.0) | 44 (29.0) | 184 (71.1) | 75 (28.9) | 81 (83.1) | 17 (16.9) | 254 (81.0) | 60 (19.0) | 623 (75.8) | 199 (24.2) |
| Richer | 195 (74.5) | 67 (25.5) | 179 (82.9) | 37 (17.1) | 97 (88.6) | 13 (11.4) | 236 (79.7) | 60 (20.3) | 724 (79.4) | 188 (20.6) |
| Richest | 448 (91.6) | 41 (8.4) | 124 (83.1) | 25 (16.9) | 81 (94.6) | 5 (5.4) | 171 (87.9) | 24 (12.1) | 923 (90.0) | 103 (10.0) |
| χ2= 12.0630, p≤0.001 | χ2= 2.0527, p=0.0935 | χ2= 2.1795, p=0.0725 | χ2= 5.9923, p≤0.001 | χ2= 13.5046, p≤0.001 | ||||||
| Worked in the last 12 months | ||||||||||
| No | 12 (57.0) | 9 (43.0) | 8 (49.0) | 9 (51.0) | 7 (55.8) | 6 (44.2) | 23 (67.3) | 11 (32.7) | 51 (59.2) | 35 (40.8) |
| Yes | 803 (81.9) | 178 (18.1) | 866 (76.8) | 262 (23.2) | 783 (85.4) | 134 (14.6) | 845 (80.0) | 212 (20.0) | 3294 (80.7) | 788 (19.3) |
| χ2= 6.2645, p=0.0125 | χ2= 6.0192, p=0.0144 | χ2= 12.7655, p≤0.001 | χ2= 1.7484, p=0.1865 | χ2= 16.2038, p≤0.001 | ||||||
| Marital status | ||||||||||
| Never married | 229 (74.8) | 77 (25.2) | 148 (62.5) | 89 (37.5) | 128 (74.0) | 45 (26.0) | 155 (63.0) | 91 (37.0) | 687 (69.1) | 307 (30.9) |
| Ever married | 586 (84.2) | 110 (15.8) | 727 (80.0) | 182 (20.0) | 662 (87.4) | 95 (12.6) | 713 (84.4) | 132 (15.6) | 2658 (83.7) | 516 (16.3) |
| χ2= 6.5313, p=0.0108 | χ2= 16.1246, p≤0.001 | χ2=12.7302, p≤0.001 | χ2= 34.7689, p≤0.001 | χ2= 53.1542, p≤0.001 | ||||||
| Ever given gifts or other goods to have sex in the last 12 months | ||||||||||
| No | 717 (82.0) | 158 (18.0) | 831 (76.9) | 249 (23.1) | 781 (85.2) | 136 (14.8) | 800 (79.5) | 206 (20.5) | 3105 (80.0) | 746 (19.4) |
| Yes | 98 (77.0) | 29 (23.0) | 43 (66.9) | 22 (33.1) | 9 (68.7) | 4 (31.3) | 69 (80.7) | 16 (19.3) | 240 (75.7) | 77 (24.3) |
| χ2= 1.4311, p=0.2320 | χ2= 3.7218, p=0.0541 | χ2= 2.7495, p=0.0977 | χ2= 0.0388, p=0.8439 | χ2= 3.2888, p=0.0702 | ||||||
| Circumcised | ||||||||||
| No | 369 (77.5) | 107 (22.5) | 379 (77.1) | 113 (22.9) | 606 (85.8) | 100 (14.2) | 473 (76.0) | 149 (24.0) | 1775 (79.1) | 469 (20.9) |
| Yes | 446 (84.8) | 80 (15.2) | 496 (75.9) | 158 (24.1) | 184 (82.2) | 40 (17.8) | 396 (84.3) | 73 (15.7) | 1570 (81.6) | 354 (18.4) |
| χ2= 5.0290, p=0.0252 | χ2= 0.1328, p=0.7157 | χ2=1.0156, p=0.3139 | χ2= 8.7932, p=0.0031 | χ2= 2.4351, p=0.1191 | ||||||
| Number of sexual partners in the last 12 months | ||||||||||
| No sexual partner | 448 (81.8) | 99 (18.2) | 625 (79.0) | 166 (21.0) | 536 (86.2) | 86 (13.8) | 548 (82.0) | 120 (18.0) | 2126 (81.9) | 469 (18.1) |
| 1 sexual partner | 281 (81.5) | 64 18.5) | 205 (69.7) | 89 (30.3) | 212 (83.2) | 43 (16.8) | 247 (79.0) | 66 (21.0) | 962 (78.5) | 264 (21.5) |
| 2 & above sexual partners | 86 (78.4) | 24 (21.6) | 45 (73.9) | 16 (26.1) | 43 (78.2) | 12 (21.8) | 73 (66.5) | 37 (33.5) | 257 (74.1) | 90 (25.9) |
| χ2= 0.2288, p=0.7738 | χ2= 4.0041, p=0.0192 | χ2= 1.3207, p=0.2672 | χ2= 5.9696, p=0.0029 | χ2= 5.3051, p=0.0054 | ||||||
Weighted proportions; ever tested (ever tested for HIV); never tested (never tested for HIV).
Socio-economic and demographic factors associated with never having tested for HIV among sexually active men aged (15 – 54 years) across regions in Uganda
Results in Table 3 reveal the socio-economic and demographic factors associated with never having tested for HIV among sexually active men aged 15 – 54 across regions in Uganda, premised on adjusted multivariable logistic regression. The results (Table 3) indicate that age, education level, religious status, wealth quintile, worked in the last 12 months, marital status, circumcised, and number of sexual partners in the last 12 months were factors associated with never having tested for HIV among sexually active men (15 – 54 years) in Uganda, with variations in impact of the variables across regions. For instance, educational level and marital status were the only factors associated with never having tested for HIV amongst respondents amidst variation in effect across all the regions. Age, religious status, wealth quintile, worked in the last 12 months, circumcised, and number of sexual partners in the last 12 months were only predictors of never having tested for HIV among respondents in particular regions.
Table 3.
Multivariable logistic regression analysis on the net-impact of factors associated with never having tested for HIV among sexually active men (15 – 54 years) across regions
| Characteristics | Regions | Uganda | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Central | Eastern | Northern | Western | |||||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Age | ||||||||||
| 15 – 24† | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . |
| 25 – 34 | 0.82 | 0.44-1.53 | 1.00 | 0.63-1.61 | 0.47* | 0.23-0.97 | 0.49* | 0.28-0.87 | 0.72* | 0.54-0.96 |
| 35 – 44 | 1.34 | 0.63-2.84 | 0.87 | 0.51-1.48 | 0.63 | 0.29-1.36 | 0.62 | 0.33-1.16 | 0.86 | 0.62-1.18 |
| 45 – 54 | 0.90 | 0.39-2.07 | 0.77 | 0.42-1.43 | 1.72 | 0.81-3.65 | 1.16 | 0.60-2.25 | 1.02 | 0.73-1.44 |
| Education level | ||||||||||
| No education† | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . |
| Primary | 0.32** | 0.16-0.66 | 0.61 | 0.25-1.48 | 0.10*** | 0.04-0.24 | 0.69 | 0.36-1.32 | 0.38*** | 0.26-0.54 |
| Secondary | 0.19*** | 0.08-0.44 | 0.26** | 0.10-0.66 | 0.02*** | 0.01-0.06 | 0.45* | 0.22-0.95 | 0.19*** | 0.12-0.28 |
| Higher | 0.06*** | 0.02-0.23 | 0.12** | 0.04-0.41 | 0.01*** | 0.003-0.05 | 0.26* | 0.09-0.77 | 0.07*** | 0.04-0.13 |
| Residence | ||||||||||
| Rural† | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . |
| Urban | 1.31 | 0.72-2.37 | 0.99 | 0.55-1.79 | 1.32 | 0.61-2.86 | 1.28 | 0.83-1.97 | 1.15 | 0.88-1.54 |
| Religious status | ||||||||||
| Catholics† | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . |
| Anglican | 0.87 | 0.51-1.49 | 0.91 | 0.61-1.35 | 0.99 | 0.58-1.69 | 0.95 | 0.65-1.37 | 0.97 | 0.78-1.21 |
| Muslim | 2.22* | 1.17-4.21 | 1.46 | 0.88-2.43 | 1.06 | 0.39-2.88 | 0.93 | 0.35-2.48 | 1.73** | 1.25-2.39 |
| Pentecostal | 0.56 | 0.26-1.19 | 0.78 | 0.41-1.47 | 0.91 | 0.33-2.52 | 0.49 | 0.24-1.03 | 0.70 | 0.48-1.02 |
| Others | 0.45 | 0.09-2.27 | 0.93 | 0.23-3.77 | 2.70 | 0.37-19.47 | 0.80 | 0.37-1.71 | 0.91 | 0.55-1.53 |
| Wealth quintile | ||||||||||
| Poorest† | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . |
| Poorer | 1.22 | 0.37-4.02 | 1.06 | 0.67-1.67 | 1.01 | 0.56-1.78 | 0.39** | 0.20-0.77 | 1.05 | 0.79-1.39 |
| Middle | 0.89 | 0.27-2.90 | 1.19 | 0.75-1.89 | 1.19 | 0.57-2.49 | 0.28*** | 0.15-0.53 | 0.99 | 0.75-1.32 |
| Richer | 0.87 | 0.28-2.75 | 0.72 | 0.39-1.30 | 0.85 | 0.40-1.83 | 0.27*** | 0.14-0.52 | 0.90 | 0.67-1.21 |
| Richest | 0.22* | 0.06-0.75 | 0.89 | 0.43-1.85 | 0.49 | 0.11-2.14 | 0.17*** | 0.08-0.37 | 0.42*** | 0.29-0.62 |
| Worked in the last 12 months | ||||||||||
| Yes† | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . |
| No | 2.65 | 0.79-8.94 | 2.22 | 0.84-5.89 | 3.15* | 1.18-8.42 | 1.21 | 0.45-3.29 | 2.09** | 1.22-3.60 |
| Marital status | ||||||||||
| Ever married† | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . |
| Never married | 4.52*** | 2.12-9.63 | 2.50** | 1.42-4.38 | 4.50*** | 2.01-10.03 | 3.69*** | 2.00-6.79 | 3.46*** | 2.46-4.89 |
| Ever given gifts or other goods to have sex in the last 12 months | ||||||||||
| No† | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Yes | 0.98 | 0.53-1.78 | 1.12 | 0.60-2.07 | 3.25 | 0.72-14.76 | 0.69 | 0.35-1.36 | 0.99 | 0.70-1.41 |
| Circumcised | ||||||||||
| No† | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . |
| Yes | 0.58* | 0.35-0.98 | 0.99 | 0.68-1.46 | 1.25 | 0.69-2.26 | 0.51** | 0.35-0.76 | 0.81* | 0.65-1.00 |
| Number of sexual partners in the last 12 months | ||||||||||
| No sexual partner† | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . |
| 1 sexual partner | 0.55* | 0.31-0.98 | 1.10 | 0.69-1.76 | 0.81 | 0.42-1.58 | 0.73 | 0.44-1.19 | 0.75* | 0.57-0.98 |
| 2 & above sexual partners | 0.53 | 0.23-1.22 | 0.70 | 0.32-1.54 | 0.70 | 0.27-1.83 | 1.28 | 0.68-2.42 | 0.81 | 0.54-1.21 |
Abbreviations: †Reference category. Significant (P < 0.05), *P < 0.05 (Moderate), **P < 0.01 (Strong) ***P < 0.001 (very strong), OR Odds ratio, CI Confidence Interval
Notably, in Uganda (Table 3), amidst very strong significance (P < 0.001), increase in educational level was associated with reduced odds of never to have tested for HIV among respondents amid variations across regions; a very strong significance of education level was reported only in northern (primary, secondary, and higher vs no education), and central region (secondary and higher vs no education). Results in Table 3 show that, with a very strong significance, never married respondents were 3.46 times (OR= 3.46; 95% CI = 2.46-4.86) more likely to have never tested for HIV in Uganda amidst regional variations; never married respondents were 4.52 times with a very strong significance (OR = 4.52; 95% CI = 2.12-9.63), 2.50 times with a strong significance (OR = 2.50; CI = 1.42-4.38), 4.50 times with a very strong significance (OR = 4.50; CI = 2.01-10.03), and 3.69 times with a very strong significance (OR = 3.69; CI = 2.00-6.79), in central, eastern, northern and western region respectively, more likely to have never tested for HIV compared with their counterparts who have ever married.
Results in Table 3 show that amidst moderate significance (P < 0.05), respondents aged 25 – 34 were less likely (OR = 0.72; CI = 0.54-0.96) to have ever tested for HIV compared to the respondents aged 15 – 24 in Uganda. However, only respondents aged 25 – 34 in northern and western region demonstrated less likelihoods of never having tested for HIV amidst moderate significance (OR = 0.47; CI = 0.23-0.97, and OR = 0.49; CI = 0.28-0.87 respectively) compared with their counterparts aged 15 – 24.
In addition, results (Table 3) indicate that muslim respondents were 1.78 times amidst a strong significance (OR = 1.78; CI = 1.25-2.39), more likely never to have tested for HIV compared with the catholics in Uganda. However, with scrutiny of effect across regions, Table 3 shows that only muslim respondents in central region were 2.21 times amidst moderate significance (OR = 2.21; CI = 1.16-4.21), more likely to have never tested for HIV compared with their counterparts the catholics.
Results in Table 3 reveal that respondents in the richest wealth quintile were 0.42 times, amidst very strong significance (OR = 0.42; CI = 0.29-0.62), less likely never to have tested for HIV compared with the respondents in the poorest wealth quintile in Uganda. However, analysis on wealth quintile across regions in Table 3 demonstrated differences in effect across regions; in western region amidst strong (poorer) and very strong associations (middle, richer, and richest), an increase in wealth quintile among sexually active men (15-54 years) was associated with reduced odds of never to have tested for HIV amongst respondents. In addition, with a moderate association in central region, sexually active men in the richest wealth quintile had reduced odds of never to have tested for HIV (OR = 0.22; CI = 0.06-0.75) compared with the respondents in the poorest wealth quintile.
Besides, results in Table 3 demonstrate that, with a strong significance, respondents who did not work in the last 12 months were more likely (OR = 2.09; CI = 1.22-3.60) to have never tested for HIV compared with their counterparts who worked in the last 12 months in Uganda. However, analysis across regions (Table 3) shows that, with moderate significance, respondents in northern region who did not work in the last 12 months, had increased odds of never to have tested for HIV (OR = 3.15; CI = 1.18-8.42), compared with the respondents who worked in the last 12 months.
Further, results in Table 3 reveal that respondents who reported to have been circumcised in Uganda were less likely (OR = 0.81; CI = 0.65-1.00) to have never tested for HIV compared with their counterparts who reported not to be circumcised, amid strong significance. However, analysis across regions only indicated variation in association (moderate and strong in central and western region, respectively); where sexually active circumcised men in central and western regions were 0.58 times (OR = 0.58; CI = 0.35-0.98) and 0.51 times (OR = 0.51; CI = 0.35-0.76) respectively, less likely to have never tested for HIV compared with their counterparts the uncircumcised.
Results in Table 3 demonstrate that respondents who reported to have had 1 sexual partner amid moderate significance were less likely (OR = 0.75; CI = 0.57-0.98) to have never tested for HIV compared with respondents who reported to have had no sexual partner in the last 12 months in Uganda. Analysis across regions (Table 3), indicates significance (moderate) in only central region, with respondents in central region who had one sexual partner were 0.55 times (OR = 0.55; CI = 0.31-0.98) less likely to have never tested for HIV compared with the sexually active men (15 – 54 years) who reported not to have had a sexual partner in the last 12 months.
Discussion
The present study aimed at understanding the factors associated with never having tested for HIV among sexually active men (men who have had sexual intercourse in the last 12 months) aged 15 – 54 across regions of Uganda. Across regions of the country, about 20% of sexually active men aged 15 – 54 have never been tested for HIV. Findings established that in Uganda, age (25 – 34 years vs 15 – 24 years), education level (primary, secondary, and higher vs no education), religious status (muslim vs catholics), wealth quintile (richest vs poorest), worked in the last 12 months, marital status, circumcised, and number of sexual partners in the last 12 months (1 sexual partner vs no sexual partner), were associated with never to have tested for HIV among respondents; with analysis across regions of Uganda demonstrating amidst variations that, education level and marital status were the only factors associated with never to have tested for HIV among sexually active men (15 – 54 years). Conspicuously, age, religious status, wealth quintile, worked in the last 12 months, circumcised, and number of sexual partners in the last 12 months (excluding their spouses) were associated with never to have tested for HIV among respondents in particular regions.
Specifically, we found that amid variations in effect, an increase in education level (primary, secondary, and higher vs no education) was associated with reduced odds of never to have tested for HIV among respondents across regions. Our study agrees with findings in Uganda, and elsewhere that found increase in education level associated with HIV testing status [12, 32, 49, 63, 70, 71]. The most conceivable reason for this association could be that possessing secondary or higher education level can influence an individual’s desire for health, knowledge on access and uptake of health care services, including HIV testing services [71–78]. Consequently, the study finding stresses the need to promote men with no education to attain at least secondary educational level as a pathway to promote HIV testing among sexually active men aged 15 – 54 across the four administrative regions.
In addition, we found that never-married respondents were more likely not to have ever tested for HIV compared with the ever-married respondents, amid very strong significance across regions, except for eastern region that had a strong significance. There are limited studies done in Uganda that justify this significance; our study finding is in agreement with some studies in Uganda, and elsewhere [12, 32, 79–82]. The possible explanation for this association could be linked to the influence of the spouse, and or fathering of children which triggers behavioral change that is skewed towards improving health care seeking and service uptake, and cultural reforms [47, 55, 75, 83, 84]. Therefore, further examination should be done to understand the influence of marital status on HIV non-testing among respondents across the four administrative regions of Uganda.
Our study established that respondents in the richest wealth quintile (poorer, middle, richer, richest vs poorest) amidst very strong significance predicted HIV never testing among respondents. However, an analysis across regions demonstrated that wealth quintile was a major influence of HIV never testing only among respondents in western region, with moderate significance among respondents in the richest wealth quintile. There are limited studies that justify this difference in association and significance in central and western regions of Uganda. Available literature demonstrates that men who reported to have never tested for HIV belonged to the lower wealth quintile [12, 63], different from their counterparts in wealthier quintile [49, 70, 85]. The most plausible explanation for this association could be that less affluent men are taken-up most by economic opportunities that assist them meet the needs of their families [86]. Nevertheless, more research should be directed towards understanding this association in Central and Western region.
Furthermore, findings in the present study demonstrate that circumcised sexually active men (15 – 54 years) in central and western region amidst variations were less likely to have never been tested for HIV. Conversely, although a study in central region of Uganda and elsewhere in sub-Saharan Africa demonstrate that unlike HIV never tested men, ever tested men were more likely to be circumcised men [12, 32]. Limited studies explain this result, which therefore prompts further examination. However, it could be attributed to better health infrastructure in central and western regions [22], and medical male circumcision which is a means of preventing HIV contraction among men and its capacity to decrease the risk of HIV transmission by 60% [7]. Notably, before the procedure of medical male circumcision, a person is first supposed to test in order to obtain sero-status results that guide safety measures undertaken in the surgical procedure [7].
On the other hand, data used in this present study had some limitations. Firstly, the data was basically restricted to only variables captured in the 2016 UDHS. Therefore, an interrogation of crucial variables was limited, for instance; the data excluded respondents above the age of 54. Lastly, the cross-sectional kind of data used in the present study frustrated the capability to scrutinize casual relationships.
Conclusions
Across regions of Uganda, about 20% of respondents never tested for HIV. Socio-economic and demographic factors associated with never having tested for HIV among sexually active men aged 15 – 54 across regions were; educational level and marital status. Age, religious status, wealth quintile, worked in the last 12 months, circumcised, number of sexual partners in the last 12 months (excluding spouses) were only correlates of never having tested for HIV among respondents in particular regions of the country. Therefore, deliberate efforts by the government of Uganda and relevant stakeholders need to be channeled towards the promotion of male education, and further examination into the association of HIV never testing among sexually active men (15 – 54 years) and being married across regions of the country. Also, efforts should be geared towards addressing regional variations in order to maximize HIV testing among sexually active men (15 – 54 years) across regions of Uganda, as well reduce on HIV related morbidity and mortality.
Acknowledgements
We thank MEASURE DHS for offering us the permission to download and use the 2016 Uganda Demographic and Health Survey dataset.
Consent to publish
Not applicable
Abbreviations
- HIV
Human Immunodeficiency Virus
- UDHS
Uganda Demographic and Health Survey
- AIDS
Acquired immunodeficiency Syndrome
- MSM
Men who have Sex with Men
- UNAIDS
United Nations Programme on HIV/AIDS
- WHO
World Health Organization
Authors’ contributions
JO and NO conceptualized and designed the study. Acquisition of data: JO. Analysis and interpretation of data: JO and IK. Drafting of the manuscript: JO. We therefore, approve the final manuscript.
Funding
The current study did not receive any funding.
Availability of data and materials
The dataset that was used in the present study is available on rational request from the corresponding author. Authorization would as well be required from MEASURE DHS.
Declarations
Ethics approval and consent to participate
This study obtained authorization to use the 2016 Uganda Demographic and Health Survey (UDHS) dataset from MEASURE DHS. All respondents in the 2016 UDHS provided written and verbal informed consent. The 2016 UDHS was a non-experimental study.
Competing interests
The authors declare that there are no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Otim Jude, Email: otimjude18@gmail.com.
Otim Nelson, Email: nelsonotim2013@gmail.com.
Igeme Katagwa, Email: igemek@yahoo.com.
References
- 1.WHO. HIV/AIDS. Fact sheet. 2020. https://www.who.int/news-room/fact-sheets/detail/hiv-aids. Accessed 27 Jul 2020.
- 2.Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UNAIDS. Global factsheet 2019. AIDSinfo. 2020;:1–2. http://aidsinfo.unaids.org/. Accessed 10 Jul 2020.
- 5.UNAIDS. AIDSinfo | UNAIDS. 2019. http://aidsinfo.unaids.org/. Accessed 21 Jan 2021.
- 6.Cornell M, Schomaker M, Garone DB, Giddy J, Hoffmann CJ, Lessells R, et al. Gender differences in survival among adult patients starting antiretroviral therapy in South Africa: a multicentre cohort study. PLoS Med. 2012;9:e1001304. doi: 10.1371/journal.pmed.1001304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joint United Nations Programme on HIV/AIDS. Miles to go: closing gaps, breaking barriers, righting injustices. Geneva; 2018. https://www.unaids.org/sites/default/files/media_asset/miles-to-go_en.pdf. Accessed on 29-1-2021.
- 8.Kigozi IM, Dobkin LM, Martin JN, Geng EH, Muyindike W, Emenyonu NI, et al. Late disease stage at presentation to an HIV clinic in the era of free antiretroviral therapy in sub-Saharan Africa. J Acquir Immune Defic Syndr. 2009;52:280. doi: 10.1097/QAI.0b013e3181ab6eab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Novitsky V, Bussmann H, Okui L, Logan A, Moyo S, van Widenfelt E, et al. Estimated age and gender profile of individuals missed by a home-based HIV testing and counselling campaign in a Botswana community. J Int AIDS Soc. 2015;18:19918. doi: 10.7448/IAS.18.1.19918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dovel K, Yeatman S, Watkins S, Poulin M. Men’s heightened risk of AIDS-related death: the legacy of gendered HIV testing and treatment strategies. AIDS. 2015;29:1123. doi: 10.1097/QAD.0000000000000655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schell ES, Geoffroy E, Phiri M, Bvumbwe A, Weinstein J, Jere JM. Cracking the code: getting men tested in rural Africa. Aids. 2016;30:331–332. doi: 10.1097/QAD.0000000000000913. [DOI] [PubMed] [Google Scholar]
- 12.Quinn C, Kadengye DT, Johnson CC, Baggaley R, Dalal S. Who are the missing men? Characterising men who never tested for HIV from population-based surveys in six sub-Saharan African countries. J Int AIDS Soc. 2019;22:e25398. doi: 10.1002/jia2.25398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kagee A, Swartz A, Swartz L. Theorising beyond the individual: Adherence to antiretroviral therapy in resource-constrained societies. J Health Psychol. 2014;19:103–109. doi: 10.1177/1359105313500247. [DOI] [PubMed] [Google Scholar]
- 14.Li J, Gilmour S, Zhang H, Koyanagi A, Shibuya K. The epidemiological impact and cost-effectiveness of HIV testing, antiretroviral treatment and harm reduction programs. Aids. 2012;26:2069–2078. doi: 10.1097/QAD.0b013e3283574e54. [DOI] [PubMed] [Google Scholar]
- 15.Fonner VA, Denison J, Kennedy CE, O’Reilly K, Sweat M. Voluntary counseling and testing (VCT) for changing HIV-related risk behavior in developing countries. Cochrane database Syst Rev. 2012. [DOI] [PMC free article] [PubMed]
- 16.Woodring JV, Kruszon-Moran D, Oster AM, McQuillan GM. Did CDC’s 2006 revised HIV testing recommendations make a difference? Evaluation of HIV testing in the US household population, 2003–2010. J Acquir Immune Defic Syndr. 2014;67:331. doi: 10.1097/QAI.0000000000000303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization (WHO). Service delivery approaches to HIV testing and conselling (HTC): a strategic HTC programme framework. 2012.
- 18.UNAIDS. 90–90–90 - An ambitious treatment target to help end the AIDS epidemic. https://www.unaids.org/en/resources/documents/2017/90-90-90. Accessed 14 Apr 2021.
- 19.Hamilton A, Haider MR, Brown MJ, Conserve DF, Li X. Regional differences of self-reported HIV testing among men in Haiti: an analysis of the 2016–2017 Demographic and Health Survey. AIDS Care. 2020;1–5. 10.1080/09540121.2020.1801983. [DOI] [PMC free article] [PubMed]
- 20.Uganda Bureau of Statistics (UBOS) and ICF. Uganda Demographic and Health Survey. 2018;2016:85–102.
- 21.Uganda Bureau of Statistics (UBOS). Uganda National Household Survey 2019/2020. Kampala. Uganda; 2021. https://www.ubos.org/wp-content/uploads/publications/09_2021Uganda-National-Survey-Report-2019-2020.pdf. Accessed 15 Nov 2021.
- 22.Odokonyero T, Mwesigye F, Adong A, Mbowa S. Universal Health Coverage in Uganda: The critical health infrastructure, healthcare coverage and equity. 2017.
- 23.Golooba-Mutebi F. COLLAPSE, WAR AND RECONSTRUCTION IN UGANDA: AN ANALYTICAL NARRATIVE ON STATE-MAKING. 2008. https://www.lse.ac.uk/international-development/Assets/Documents/PDFs/csrc-working-papers-phase-two/wp27.2-collapse-war-and-reconstruction-in-uganda.pdf. Accessed on 16-11-21. Accessed 16 Nov 2021.
- 24.Byabazaire DM. The contribution of the Christian churches to the development of Western Uganda: 1894-1974. Eur Hochschulschriften/23. 1978.
- 25.Tiberondwa AK. Missionary teachers as agents of colonialism. National Educational Company of Zambia; 1978.
- 26.Kiggundu AT, Mukiibi S. Landuse and transport planning in the Greater Kampala. Uganda; 2011.
- 27.Uganda Bureau of Statistics (UBOS). 2019 Statistical abstract for Kampala city. Kampala; 2019. https://www.kcca.go.ug/media/docs/Statistical-Abstract-2019.pdf. Accessed on 16-11-21.
- 28.Branch A. Humanitarianism, violence, and the camp in Northern Uganda. Civ Wars. 2009;11:477–501. [Google Scholar]
- 29.Bongyereirwe H. Healing the wounds of the northern Uganda insurgency. J African Media Stud. 2010;2:193–208. [Google Scholar]
- 30.Refugee Law Project. Elevate regional referral hospitals in the newly created cities in post-conflict northern Uganda to support rehabilitation of war victims. reliefweb. 2021. https://reliefweb.int/report/uganda/elevate-regional-referral-hospitals-newly-created-cities-post-conflict-northern-uganda. Accessed 16 Nov 2021.
- 31.Okal J, Lango D, Matheka J, Obare F, Ngunu-Gituathi C, Mugambi M, et al. “It is always better for a man to know his HIV status” - A qualitative study exploring the context, barriers and facilitators of HIV testing among men in Nairobi, Kenya. PLoS One. 2020;15:e0231645–e0231645. 10.1371/journal.pone.0231645. [DOI] [PMC free article] [PubMed]
- 32.Nangendo J, Katahoire AR, Armstrong-Hough M, Kabami J, Obeng-Amoako GO, Muwema M, et al. Prevalence, associated factors and perspectives of HIV testing among men in Uganda. PLoS One. 2020;15:e0237402. doi: 10.1371/journal.pone.0237402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roger Pebody. Large HIV testing gap between rich and poor living in African countries | aidsmap. aidsmap. 2020. https://www.aidsmap.com/news/jun-2020/large-hiv-testing-gap-between-rich-and-poor-living-african-countries. Accessed 24 Jan 2021.
- 34.Hlongwa M, Mashamba-Thompson T, Makhunga S, Hlongwana K. Barriers to HIV testing uptake among men in sub-Saharan Africa: a scoping review. African J AIDS Res. 2020;19:13–23. doi: 10.2989/16085906.2020.1725071. [DOI] [PubMed] [Google Scholar]
- 35.Hamilton A, Shin S, Taggart T, Whembolua G-L, Martin I, Budhwani H, et al. HIV testing barriers and intervention strategies among men, transgender women, female sex workers and incarcerated persons in the Caribbean: a systematic review. Sex Transm Infect. 2020;96:189–196. doi: 10.1136/sextrans-2018-053932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ha JH, Van Lith LM, Mallalieu EC, Chidassicua J, Pinho MD, Devos P, et al. Gendered relationship between HIV stigma and HIV testing among men and women in Mozambique: a cross-sectional study to inform a stigma reduction and male-targeted HIV testing intervention. BMJ Open. 2019;9:e029748. doi: 10.1136/bmjopen-2019-029748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Uganda Bureau of Statistics (UBOS) and ICF. Uganda Demograpic and Health Survey 2011. ICF Int. 2012:1–461.
- 38.Uganda Bureau of Statistics (UBOS) and ICF. Uganda Demographic and Health Survey 2016. 2018;:85–102. https://www.dhsprogram.com/pubs/pdf/FR333/FR333.pdf. Accessed on 17-1-20.
- 39.Ministry of Health U. National HIV Testing Services Policy and Implementation Guidelines Uganda. Kampala; 2016.
- 40.Ochan B. Uganda to launch door to door anonymous testing for HIV. BMJ. 2003;327:1186. doi: 10.1136/bmj.327.7425.1186-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ministry of Health U. Uganda Population-based HIV Impact Assessment (UPHIA) 2016-2017: Final Report. Kampala, Uganda; 2019. https://phia.icap.columbia.edu/wp-content/uploads/2019/07/UPHIA_Final_Report_Revise_07.11.2019_Final_for-web.pdf. Accessed on 24-1-2021.
- 42.UNAIDS. Joint United Nations Programme on HIV/AIDS. Fast-Track - Ending the AIDS epidemic by 2030. 2014. https://www.unaids.org/en/resources/documents/2014/JC2686_WAD2014report. Accessed 13 Apr 2021.
- 43.United Nations. Transforming our World: The 2030 Agenda for Sustainable Development. 2015. https://sustainabledevelopment.un.org/post2015/transformingourworld/publication. Accessed 13 Apr 2021.
- 44.Tabana H, Doherty T, Swanevelder S, Lombard C, Jackson D, Zembe W, et al. Knowledge of HIV status prior to a community HIV counseling and testing intervention in a rural district of South Africa: results of a community based survey. BMC Infect Dis. 2012;12:73. doi: 10.1186/1471-2334-12-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.DiCarlo AL, Mantell JE, Remien RH, Zerbe A, Morris D, Pitt B, et al. ‘Men usually say that HIV testing is for women’: gender dynamics and perceptions of HIV testing in Lesotho. Cult Health Sex. 2014;16:867–882. doi: 10.1080/13691058.2014.913812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Byamugisha R, Tumwine JK, Semiyaga N, Tylleskär T. Determinants of male involvement in the prevention of mother-to-child transmission of HIV programme in Eastern Uganda: a cross-sectional survey. Reprod Health. 2010;7:1–9. doi: 10.1186/1742-4755-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Magala I, Tapati D, Nalubega R. Factors affecting utilization of HIV care services among men in TASO Masaka. Uganda: An exploratory study. J Clin Microbiol Infect Dis; 2018. p. 2. [Google Scholar]
- 48.Ssebunya RN, Wanyenze RK, Namale L, Lukolyo H, Kisitu GP, Nahirya-Ntege P, et al. Prevalence and correlates of HIV testing among adolescents 10–19 years in a post-conflict pastoralist community of Karamoja region. Uganda. BMC Public Health. 2018;18:1–8. doi: 10.1186/s12889-018-5544-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gage AJ, Ali D. Factors associated with self-reported HIV testing among men in Uganda. AIDS Care. 2005;17:153–165. doi: 10.1080/09540120512331325635. [DOI] [PubMed] [Google Scholar]
- 50.Arnesen R, Moll AP, Shenoi SV. Predictors of loss to follow-up among patients on ART at a rural hospital in KwaZulu-Natal. South Africa. PLoS One. 2017;12:e0177168. doi: 10.1371/journal.pone.0177168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Olakunde BO, Adeyinka DA, Olawepo JO, Pharr JR. HIV testing among men in Nigeria: a comparative analysis between young people and adults. AIDS Care. 2020;32:155–162. doi: 10.1080/09540121.2019.1622642. [DOI] [PubMed] [Google Scholar]
- 52.Zhao Y, Zhang L, Zhang H, Xia D, Pan SW, Yue H, et al. HIV testing and preventive services accessibility among men who have sex with men at high risk of HIV infection in Beijing, China. Medicine (Baltimore). 2015;94. [DOI] [PMC free article] [PubMed]
- 53.Skovdal M, Campbell C, Madanhire C, Mupambireyi Z, Nyamukapa C, Gregson S. Masculinity as a barrier to men’s use of HIV services in Zimbabwe. Global Health. 2011;7:13. doi: 10.1186/1744-8603-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.UNAIDS. Addressing a blind spot in the response to HIV—reaching out to men and boys. 2017;:10–58. https://www.unaids.org/sites/default/files/media_asset/blind_spot_en.pdf. Accessed on 11-7-2020.
- 55.Siu GE, Wight D, Seeley JA. Masculinity, social context and HIV testing: an ethnographic study of men in Busia district, rural eastern Uganda. BMC Public Health. 2014;14:1–11. doi: 10.1186/1471-2458-14-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Leichliter JS, Paz-Bailey G, Friedman AL, Habel MA, Vezi A, Sello M, et al. ‘Clinics aren’t meant for men’: sexual health care access and seeking behaviours among men in Gauteng province, South Africa. SAHARA-J J Soc Asp HIV/AIDS. 2011;8. [DOI] [PMC free article] [PubMed]
- 57.Uganda AIDS Commission. The Uganda HIV and AIDS Country Progress Report July 2017 - June 2018. 2018. https://www.unaids.org/sites/default/files/country/documents/UGA_2019_countryreport.pdf.
- 58.Baeten JM, Donnell D, Kapiga SH, Ronald A, John-Stewart G, Inambao M, et al. Male circumcision and risk of male-to-female HIV-1 transmission: A multinational prospective study in African HIV-1 serodiscordant couples. AIDS. 2010;24:737. doi: 10.1097/QAD.0b013e32833616e0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schroeder MA. Diagnosing and Dealing with Multicollinearity. West J Nurs Res. 1990;12:175–187. doi: 10.1177/019394599001200204. [DOI] [PubMed] [Google Scholar]
- 60.Uganda Bureau of Statistics (UBOS) and ORC Macro. Uganda 1995: Results from the Demographic and Health Survey. Calverton, Maryland, USA; 2001. 10.2307/2138118.
- 61.Mhlongo S, Dietrich J, Otwombe KN, Robertson G, Coates TJ, Gray G. Factors associated with not testing for HIV and consistent condom use among men in Soweto. South Africa. PLoS One. 2013;8:e62637. doi: 10.1371/journal.pone.0062637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hajabdolbaghi M, Ghafarzadeh M, Bayat Jozani Z, Mohraz M, Farrokhi M, Foroughi M, et al. Situational Analysis on Voluntary Counseling and Confidential Testing in HIV/AIDS Patients Referred to Behavioral Center in lmam Khomeini Hospital, Tehran. Iran. Int J Epidemiol Res. 2017;5:3–8. [Google Scholar]
- 63.Jean K, Anglaret X, Moh R, Lert F, Dray-Spira R. Barriers to HIV testing in Côte d’Ivoire: the role of individual characteristics and testing modalities. PLoS One. 2012;7:e41353. doi: 10.1371/journal.pone.0041353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Meyeyin-Bala K. Abstract HIV Testing and Multiple Sexual Partnerships Among Men in Nigeria. Walden University; 2019. https://scholarworks.waldenu.edu/cgi/viewcontent.cgi?article=8518&context=dissertations. Accessed on 29-1-2021.
- 65.Castle S. Doubting the existence of AIDS: a barrier to voluntary HIV testing and counselling in urban Mali. Health Policy Plan. 2003;18:146–155. doi: 10.1093/heapol/czg019. [DOI] [PubMed] [Google Scholar]
- 66.Wulandari LPL, Ruddick A, Guy R, Kaldor J. “Self-testing sounds more private, rather than going to the clinic and everybody will find out”: Facilitators and barriers regarding HIV testing among men who purchase sex in Bali. Indonesia. PLoS One. 2019;14:e0214987. doi: 10.1371/journal.pone.0214987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wulandari LPL, Kaldor J, Guy R. Uptake and acceptability of assisted and unassisted HIV self-testing among men who purchase sex in brothels in Indonesia: a pilot intervention study. BMC Public Health. 2020;20:1–14. doi: 10.1186/s12889-020-08812-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wringe A, Isingo R, Urassa M, Maiseli G, Manyalla R, Changalucha J, et al. Uptake of HIV voluntary counselling and testing services in rural Tanzania: implications for effective HIV prevention and equitable access to treatment. Trop Med Int Heal. 2008;13:319–327. doi: 10.1111/j.1365-3156.2008.02005.x. [DOI] [PubMed] [Google Scholar]
- 69.Acock AC. A Gentle Introduction to Stata, Second Edition. 2008. http://books.google.com/books?id=YZIQO0acuWwC&pgis=1.
- 70.Stephenson R, Elfstrom KM, Winter A. Community influences on married men’s uptake of HIV testing in eight African countries. AIDS Behav. 2013;17:2352–2366. doi: 10.1007/s10461-012-0223-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hensen B, Lewis JJ, Schaap A, Tembo M, Mutale W, Weiss HA, et al. Factors associated with HIV-testing and acceptance of an offer of home-based testing by men in rural Zambia. AIDS Behav. 2015;19:492–504. doi: 10.1007/s10461-014-0866-0. [DOI] [PubMed] [Google Scholar]
- 72.Nabukenya AM, Matovu JKB. Correlates of HIV status awareness among older adults in Uganda: results from a nationally representative survey. BMC Public Health. 2018;18:1–8. doi: 10.1186/s12889-018-6027-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mwangi M, Kellogg TA, Dadabhai SS, Bunnell R, Baltazar G, Ngare C, et al. Factors associated with uptake of HIV test results in a nationally representative population-based AIDS indicator survey. Open AIDS J. 2014;8:7. doi: 10.2174/1874613601408010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kong X, Kigozi G, Ssekasanvu J, Nalugoda F, Nakigozi G, Ndyanabo A, et al. Association of medical male circumcision and antiretroviral therapy scale-up with community HIV incidence in Rakai. Uganda. Jama. 2016;316:182–190. doi: 10.1001/jama.2016.7292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hensen B, Lewis JJ, Schaap A, Tembo M, Vera-Hernández M, Mutale W, et al. Frequency of HIV-testing and factors associated with multiple lifetime HIV-testing among a rural population of Zambian men. BMC Public Health. 2015;15:1–14. doi: 10.1186/s12889-015-2259-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ayenew A, Leykun A, Colebunders R, Deribew A. Predictors of HIV testing among patients with tuberculosis in North West Ethiopia: a case-control study. PLoS One. 2010;5:e9702. doi: 10.1371/journal.pone.0009702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bond L, Lauby J, Batson H. HIV testing and the role of individual-and structural-level barriers and facilitators. AIDS Care. 2005;17:125–140. doi: 10.1080/09541020512331325653. [DOI] [PubMed] [Google Scholar]
- 78.Shepler DK, Johnson KP, Width AA. Risky sexual behavior and knowledge of HIV/AIDS transmission in a community sample: Sexual orientation, race, and gender. J Soc Behav Heal Sci. 2017;11:10. [Google Scholar]
- 79.Narin P, Yamamoto E, Saw YM, Net N, Inthaphatha S, Kariya T, et al. Factors associated with HIV testing among the general male population in Cambodia: A secondary data analysis of the Demographic Health Survey in 2005, 2010, and 2014. PLoS One. 2019;14:e0219820. doi: 10.1371/journal.pone.0219820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mandiwa C, Namondwe B. Uptake and correlates of HIV testing among men in Malawi: evidence from a national population–based household survey. BMC Health Serv Res. 2019;19:203. doi: 10.1186/s12913-019-4031-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ziraba AK, Madise NJ, Kimani JK, Oti S, Mgomella G, Matilu M, et al. Determinants for HIV testing and counselling in Nairobi urban informal settlements. BMC Public Health. 2011;11:663. doi: 10.1186/1471-2458-11-663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Agha S. Factors associated with HIV testing and condom use in Mozambique: implications for programs. Reprod Health. 2012;9:20. doi: 10.1186/1742-4755-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Iwelunmor J, Sofolahan-Oladeinde Y, Airhihenbuwa CO. Sociocultural factors influencing HIV disclosure among men in South Africa. Am J Mens Health. 2015;9:193–200. doi: 10.1177/1557988314535235. [DOI] [PubMed] [Google Scholar]
- 84.Nyamhanga TM, Muhondwa EPY, Shayo R. Masculine attitudes of superiority deter men from accessing antiretroviral therapy in Dar es Salaam. Tanzania. Glob Health Action. 2013;6:21812. doi: 10.3402/gha.v6i0.21812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Staveteig S, Wang S, Head SK, Bradley SEK, Nybro E. Demographic patterns of HIV testing uptake in sub-Saharan Africa. MD: ICF International Calverton; 2013. [Google Scholar]
- 86.Sakala D, Kumwenda MK, Conserve DF, Ebenso B, Choko AT. Socio-cultural and economic barriers, and facilitators influencing men’s involvement in antenatal care including HIV testing: a qualitative study from urban Blantyre. Malawi. BMC Public Health. 2021;21:60. doi: 10.1186/s12889-020-10112-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset that was used in the present study is available on rational request from the corresponding author. Authorization would as well be required from MEASURE DHS.