Abstract
Objective:
Shortened life expectancy of people with mental disorders has been attributed to medical comorbidities, yet these conditions remain under-recognized and under-treated. This study characterizes the medical demands placed on inpatient psychiatric units to help guide medical assessment and management practices in these settings.
Methods:
Medicaid claims records and clinician data were linked with hospital and regional data for individuals with a principal diagnosis of any mental disorder admitted to psychiatric inpatient units in New York State from 2012–2013. A modified Elixhauser Comorbidity Index (ECI) score was calculated for each unique individual (n=14,458). Adjusted odds ratios (AORs) of having a medical comorbidity were calculated using logistic regression analyses.
Results:
74.9% of psychiatric inpatients had at least one medical comorbidity, including 57.5% of people ages 18–24. Higher rates of medical comorbidity were associated with older age, female gender, non-schizophrenia diagnoses, and engagement in care prior to hospitalization. Patients with medical comorbidities had lower odds (AOR 0.54; 99% CI 0.35–0.83) of being treated in hospitals with 100 or more total beds compared to smaller hospitals.
Conclusions:
A high prevalence of common medical diagnoses among psychiatric inpatients underscores the importance of adequate detection and medical treatment of medical comorbidities in psychiatric inpatient settings.
Keywords: Inpatient Psychiatric Care, Medical Comorbidity
1. Introduction
Premature mortality is significantly higher for people with any mental illness compared to the general population,1 with even earlier mortality for those with serious mental illnesses such as schizophrenia,2 bipolar disorder,3 and severe depression.4 Shortened life expectancy in people with mental disorders has been primarily attributed to common medical comorbidities such as cardiovascular disease and cancer.1,5
Systematic reviews have described the prevalence of comorbid medical conditions in people with mental disorders compared to the general population, including high rates of obesity, diabetes, hypertension, hyperlipidemia, coronary heart disease, congestive heart failure, cerebrovascular disease, pulmonary disease, renal disease, and infectious diseases such as hepatitis and HIV.6,7 Diagnoses such as diabetes are even more common among racial and ethnic minority groups with serious mental illness.8,9 Nevertheless, people with mental disorders receive infrequent screenings for medical conditions like diabetes,10 cardiovascular disease,10 cervical and breast cancer,11,12 and HIV,13 among others.
Psychiatric inpatients with medical comorbidities also have higher utilization of acute care services and health care costs.14 People with mental disorders who also have medical comorbidities are more likely to have psychiatric hospital readmissions compared to those who do not have medical comorbidities.15 Though there is limited evidence for a synergistic effect between mental and physical illness on increased costs of care,16 it has been estimated that increasing access to care via adoption of evidence-based models for integrated behavioral and physical health care could yield as much as $67.8 billion in savings in the US.17
Better understanding factors related to prevalence of medical disorders in psychiatric populations has important clinical implications. Hospital settings have been proposed as an ideal environment for universal screening and engagement in treatment for common medical conditions in people with mental disorders.18 Approximately 3.3% of American adults with any mental illness are hospitalized annually, including 7.3% of adults with serious mental illnesses.19 As many as 84.2% of hospital stays for mental and substance use disorders already address at least one co-occurring physical health conditions.20 While medical comorbidity in inpatients with mental disorders has been previously described,21 there is less research specific to Medicaid beneficiaries who have been admitted for psychiatric inpatient care, a group that tends to have higher rates of medical comorbidity and severity of illness.22 The population insured by Medicaid is of particular interest given the prominent role that Medicaid plays in funding mental health services in the U.S.23
By using Medicaid claims and clinician data linked with hospital- and systems-level data, this study is able to describe the prevalence of medical diagnoses among admitted individuals with a principal psychiatric diagnosis. Based on the background described above, the analysis evaluates patient-level variables hypothesized to be associated with higher medical burden among psychiatric inpatients. The analysis also includes variables related to hospital and regional characteristics given hypothesized variations in medical burden depending on the complexity of patients that might be accepted by different types of hospitals or in different regions. Understanding medical demands that are placed on inpatient psychiatric units and how they vary across hospital settings and patient populations may help guide medical assessment and management practices of teams working in these settings.
2. Methods
2.1. Data Sources
Data for this study were obtained from four primary sources: (1) New York State (NYS) Medicaid claims records and clinician data; (2) the 2012–2013 American Hospital Association Annual Survey for NYS hospitals;24 (3) the 2012–2013 Health Resources and Human Services Administration Area Resource File for NYS;25 and (4) a 2012–2013 NYS Managed Behavioral Healthcare Organizations (MBHOs) Discharge File created during a statewide quality assurance program in which NYS contracted with five MBHOs in geographically distinct regions to review fee-for-service inpatient psychiatric admissions.26
The study was reviewed and determined to be exempt from human subject review by the New York State Psychiatric Institute Institutional Review Board.
2.2. Sample Selection
Eligibility criteria for the present analysis included: 1) age 18 to 64 years; 2) admitted to an inpatient psychiatric unit during 2012–2013 with a primary mental health diagnosis (not including substance use disorders); 3) discharged to the community; 4) Medicaid eligibility for at least 11 of the 12 months prior to admission; 5) no Medicare eligibility; and 6) inpatient length of stay of 60 days or less. For patients with more than one inpatient psychiatric admission during 2012–2013, only the patient’s initial admission during that period was included in the analysis.
2.3. Dependent Variables
We used an established algorithm to calculate Elixhauser Comorbidity Index (ECI) scores based on clinical diagnoses recorded in inpatient or outpatient records during the 12 months prior to inpatient admission.27,28 These claims included inpatient and outpatient services and used 5-digit ICD-9 codes.29 We excluded ECI mental disorder categories (depression, psychosis, alcohol use, and drug use) because all of the individuals in our study population had a mental disorder diagnosis and we wished to have a measure capturing only non-psychiatric medical comorbidity. We also excluded cardiac arrhythmias from the analysis due concerns about its reliability as a comorbidity in prior studies.29 There were therefore 26 total ECI categories (see Table 1). The score used as the dependent variable was the sum of all categories for which each inpatient had an eligible diagnosis.
Table 1.
Frequencies of comorbid medical conditions in 14,458 inpatient psychiatric admissions.1
| Elixhauser Comorbidity Index Category | N (%) |
|---|---|
| Hypertension without complications | 5615 (38.8) |
| Chronic Pulmonary Disease | 4798 (33.2) |
| Obesity | 3515 (24.3) |
| Diabetes without complications | 3012 (20.8) |
| Fluid and Electrolyte Disorders | 2357 (16.3) |
| Other Neurological Disorders | 2199 (15.2) |
| Liver Disease | 1572 (10.9) |
| Hypothyroidism | 1502 (10.4) |
| Diabetes with complications | 998 (6.9) |
| Deficiency Anemia | 921 (6.4) |
| Peripheral Vascular Disorders | 812 (5.6) |
| HIV/AIDS | 741 (5.1) |
| Weight Loss | 728 (5.0) |
| Valvular Disease | 696 (4.8) |
| Congestive Heart Failure | 632 (4.4) |
| Hypertension with complications | 622 (4.3) |
| Renal Failure | 533 (3.7) |
| Rheumatoid Arthritis/Collagen | 466 (3.2) |
| Coagulopathy | 458 (3.2) |
| Solid Tumor without Metastasis | 326 (2.3) |
| Pulmonary Circulation Disorders | 276 (1.9) |
| Peptic Ulcer Disease excluding bleeding | 259 (1.8) |
| Paralysis | 214 (1.5) |
| Blood Loss Anemia | 126 (0.9) |
| Metastatic Cancer | 62 (0.4) |
| Lymphoma | 43 (0.3) |
Data obtained from New York State Medicaid claims records and clinician data for patients ages 18–64 admitted to an inpatient psychiatric unit during 2012–2013 with a principal diagnosis of any mental disorder; Elixhauser Comorbidity Index (ECI) scores based on clinical diagnoses during the 12 months prior to each unique individual’s initial inpatient admission.
An additional analysis used specific Elixhauser categories as the dependent variable to examine factors related to the presence of medical conditions that were found to occur at higher rates in the study population (see Supplemental Table 1) and are described in the literature as occurring at high rates among people with serious mental illness and substance use disorders, including hypertension with and/or without complications (combined two categories), chronic pulmonary disease, obesity, diabetes with and/or without complications (combined two categories), other neurological disorders, liver disease, and HIV/AIDS (see Supplemental Tables 2a–g).
2.4. Patient-Level Variables
Patient-level variables from the Medicaid claims files included demographic characteristics (age group, gender, and race/ethnicity), primary inpatient discharge diagnosis, homelessness at admission, and co-occurring substance use diagnosis at discharge. A categorical variable on engagement in outpatient mental health services in the period preceding admission (active, recent, or none) was included to account for differences in those with medical diagnoses captured from outpatient mental health records in the 12 months prior to the initial psychiatric inpatient episode.
2.5. Hospital-Level Variables
Hospitals were characterized based upon size (total beds), provision of outpatient psychiatric services (yes or no), hospital ownership (public, private not-for-profit, or private for-profit), percentage of total annual discharges of patients enrolled in Medicaid, and by medical resident teaching status (teaching or nonteaching). Information from NYS administrative databases including the NYS Medicaid Program, the NYS Department of Health Statewide Planning and Research Cooperative System-SPARCS, and the NYS Office of Mental Health’s Mental Health Automated Record System (MHARS) were used to create additional variables characterizing hospitals during the 2012–2013 period including the percentage of psychiatric discharges that had a substance use disorder diagnosis and percentage of psychiatric patients who had two or more psychiatric hospitalizations.
2.6. System-Level Variables
Area Resource File data characterized counties in which patients resided with respect to regional mental health resources, poverty, and urban/rural classification. We also included a Managed Behavioral Health Organization variable to distinguish among the five different MBHOs contracted to perform the utilization review activities in distinct NYS regions.
2.7. Analytic Plan
Using the ECI score variable as described above, we first examined how many unique individuals in the dataset were identified within each of the 26 ECI categories (Table 1) and stratified these findings by age band (supplemental materials). We also examined the composite ECI scores by age group (Figure 1).
Figure 1. Distribution of Elixhauser Comorbidity Index (ECI) score by age group among Medicaid beneficiaries with mental disorders admitted to inpatient psychiatry.2.
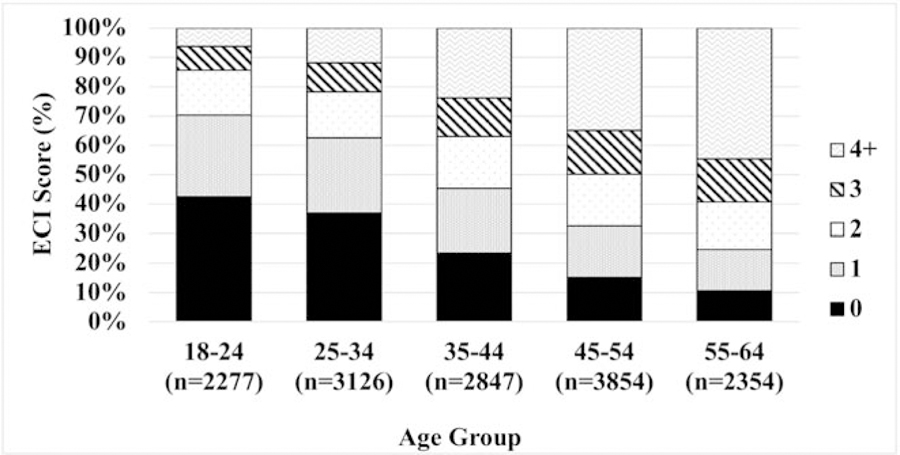
2 Source: New York State Medicaid claims records and clinician data for patients ages 18–64 admitted to an inpatient psychiatric unit during 2012–2013 with a principal diagnosis of any mental disorder; Elixhauser Comorbidity Index (ECI) scores based on clinical diagnoses during the 12 months prior to each unique individual’s initial inpatient admission.
The percentages of individuals with ECI score equal to zero (meaning no medical comorbidities) versus those with ECI of one or more (meaning any medical comorbidity) were determined overall and stratified by each patient, hospital and service system characteristic (Tables 2 and 3). Unadjusted odds ratios with 99% confidence intervals (CIs) were calculated for each characteristic to evaluate their associations with ECI of one or more. Adjusted odds ratios with 99% CIs were calculated for each characteristic using logistic regression analyses to measure the association of each variable with the probability of having a medical comorbidity, controlling for all other patient, hospital and service system characteristic variables. The following variables served as covariates: hospital provision of outpatient psychiatric services, percent of hospital discharges with substance use disorder diagnosis, NYS MBHO, and regional mental health workforce. Because of the nesting of patients within different hospitals, the observations are non-independent given that detection of comorbid medical diagnoses may vary by setting-specific screening protocols. Accordingly, generalized estimating equations were used to adjust all standard errors and confidence intervals for the clustering of observations within hospitals. Given that these analyses of a large sample were exploratory in nature, we used 99% CIs. We consider odds ratios with 99% CIs that do not include 1.0 to be statistically significant and odds ratios greater than 1.20 or less than 0.80 to be potentially substantial from a clinical or policy perspective. In this large, exploratory study, no adjustments have been made to the many P values for the multiple comparisons. Therefore, the P values should be interpreted with caution.
Table 2.
Patient-level factors associated with Elixhauser Comorbidity Index scores in 14,458 inpatient psychiatric admissions.3
| Variable | Total N (col %) (N=14458) | ECI ≥ 1 (row %) (N=10834) | Unadjusted OR (99% CI) | Adjusted OR (99% CI) |
|---|---|---|---|---|
| Age | ||||
| 18–24 | 2277 (15.8) | 57.5 | Reference | Reference |
| 25–34 | 3126 (21.6) | 63.1 | 1.26 (1.06–1.50) | 1.30 (1.09–1.55) |
| 35–44 | 2847 (19.7) | 76.5 | 2.40 (2.04–2.83) | 2.41 (2.01–2.88) |
| 45–54 | 3854 (26.7) | 84.8 | 4.12 (3.36–5.06) | 4.08 (3.29–5.06) |
| 55–64 | 2354 (16.3) | 89.4 | 6.21 (4.89–7.89) | 6.34 (4.91–8.19) |
| Gender | ||||
| Male | 7627 (52.8) | 69.3 | Reference | Reference |
| Female | 6831 (47.3) | 81.2 | 1.91 (1.71–2.14) | 1.66 (1.48–1.86) |
| Race/ethnicity | ||||
| Non-Hispanic White | 6118 (42.3) | 75.4 | Reference | Reference |
| Non-Hispanic Black | 4783 (33.1) | 74.0 | 0.93 (0.82–1.05) | 1.02 (0.89–1.17) |
| Puerto Rican-Hispanic | 1609 (11.1) | 77.1 | 1.10 (0.93–1.30) | 1.13 (0.94–1.36) |
| Other | 1248 (8.6) | 76.7 | 1.07 (0.89–1.29) | 1.11 (0.93–1.32) |
| Unknown | 700 (4.8) | 69.7 | 0.75 (0.59–0.96) | 0.88 (0.70–1.11) |
| Primary diagnosis at discharge | ||||
| Schizophrenia disorders | 5016 (34.7) | 70.7 | Reference | Reference |
| Schizoaffective disorders | 1887 (13.1) | 77.7 | 1.44 (1.22–1.70) | 1.47 (1.23–1.76) |
| Bipolar disorders | 3651 (25.3) | 75.1 | 1.25 (1.04–1.50) | 1.40 (1.15–1.70) |
| Depressive disorders | 2974 (20.6) | 80.4 | 1.70 (1.40–2.07) | 1.65 (1.37–2.00) |
| Other mental health disorders | 930 (6.4) | 73.7 | 1.16 (0.91–1.47) | 1.58 (1.25–2.01) |
| Co-occurring substance use diagnosis at discharge | ||||
| No | 7705 (53.3) | 75.6 | Reference | Reference |
| Yes | 6753 (46.7) | 74.2 | 0.93 (0.84–1.03) | 0.97 (0.87–1.08) |
| Length of stay | ||||
| 0–4 days | 2631 (18.2) | 75.6 | Reference | Reference |
| 5–14 days | 7575 (52.4) | 75.4 | 0.99 (0.85–1.14) | 0.91 (0.78–1.06) |
| 15–30 days | 3198 (22.1) | 74.7 | 0.95 (0.80–1.13) | 0.83 (0.67–1.02) |
| 31–60 days | 1054 (7.3) | 70.8 | 0.78 (0.64–0.95) | 0.67 (0.52–0.87) |
| Homeless at admission | ||||
| No | 12378 (85.6) | 74.7 | Reference | Reference |
| Yes | 1302 (9.0) | 75.2 | 1.03 (0.85–1.24) | 1.08 (0.90–1.28) |
| Prior engagement in psychiatric outpatient services | ||||
| Active (past month) | 7162 (49.5) | 77.3 | Reference | Reference |
| Recent (past 12 months, but not past month) | 3248 (22.5) | 74.4 | 0.85 (0.74–0.99) | 0.86 (0.74–1.00) |
| None (none in past 12 months) | 4048 (28.0) | 71.3 | 0.73 (0.63–0.85) | 0.70 (0.60–0.82) |
Sources: (1) Medicaid claims records and clinician data; (2) the 2012–2013 American Hospital Association Annual Survey; (3) the 2012–2013 Health Resources and Human Services Administration Area Resource File; and (4) a 2012–2013 New York State (NYS) Managed Behavioral Healthcare Organizations (MBHOs) Discharge File created during a statewide quality assurance program in which NYS contracted with five MBHOs in geographically distinct regions to review fee-for-service inpatient psychiatric admissions. Data includes patients ages 18–64 admitted to an inpatient psychiatric unit during 2012–2013 with a principal diagnosis of any mental disorder; Elixhauser Comorbidity Index (ECI) scores based on clinical diagnoses during the 12 months prior to each unique individual’s initial inpatient admission.
Table 3.
Hospital- and system-level factors associated with Elixhauser Comorbidity Index scores in 14,458 inpatient psychiatric admissions.4
| Variable | Total N (col %) (N=14458) | ECI ≥ 1 (row %) (N=10834) | Unadjusted OR (99% CI) | Adjusted OR (99% CI) |
|---|---|---|---|---|
| Hospital-level variables | ||||
|
| ||||
| Number of hospital beds | ||||
| Small: less than 100 | 177 (1.2) | 76.3 | Reference | Reference |
| Medium: 100–499 | 7587 (52.5) | 75.1 | 0.94 (0.40–2.19) | 0.54 (0.35–0.83) |
| Large: 500 or more | 6694 (46.3) | 74.7 | 0.92 (0.39–2.15) | 0.54 (0.34–0.86) |
| Hospital ownership | ||||
| Public | 3986 (27.6) | 74.8 | Reference | Reference |
| Private not-for-profit | 10387 (71.8) | 75.2 | 1.02 (0.83–1.25) | 1.03 (0.85–1.24) |
| Private for-profit | 85 (0.6) | 52.9 | 0.38 (0.26–0.56) | 0.67 (0.38–1.16) |
| Psychiatric discharges that were Medicaid, % | ||||
| Low: less than 49% (Q1) | 1865 (12.9) | 73.3 | Reference | Reference |
| Medium: 49–71% | 7857 (54.3) | 74.4 | 1.06 (0.87–1.28) | 1.01 (0.83–1.24) |
| High: over 71% (Q3) | 4736 (32.8) | 76.5 | 1.18 (0.95–1.47) | 1.08 (0.77–1.53) |
| Teaching hospital | ||||
| No | 925 (6.4) | 72.8 | Reference | Reference |
| Yes | 13533 (93.6) | 75.1 | 1.13 (0.87–1.47) | 1.06 (0.77–1.46) |
| Population w/ ≥ 2 psych discharges, % | ||||
| Low: less than 24.5% (Q1) | 1273 (8.8) | 70.2 | Reference | Reference |
| Medium: 24.5–35% | 8021 (55.5) | 74.7 | 1.25 (0.98–1.60) | 0.93 (0.69–1.25) |
| High: over 35% (Q3) | 5164 (35.7) | 76.5 | 1.38 (1.06–1.79) | 1.00 (0.70–1.43) |
|
| ||||
| System-level variables | ||||
|
| ||||
| County population in poverty, % | ||||
| Low: less than 15% | 4552 (31.7) | 73.7 | Reference | Reference |
| Medium: 15–19% | 5666 (39.5) | 74.0 | 1.02 (0.86–1.20) | 1.00 (0.78–1.28) |
| High: 20% or higher | 4134 (28.8) | 77.5 | 1.23 (1.02–1.49) | 1.14 (0.83–1.55) |
| Urban/rural classification | ||||
| Large central metro | 8169 (56.9) | 75.6 | Reference | Reference |
| Large fringe metro | 2478 (17.3) | 72.6 | 0.86 (0.72–1.02) | 0.96 (0.74–1.24) |
| Medium metro | 1495 (10.4) | 74.8 | 0.96 (0.81–1.14) | 1.14 (0.85–1.54) |
| Small metro | 832 (5.8) | 73.3 | 0.89 (0.75–1.06) | 1.16 (0.85–1.56) |
| Micropolitan | 1072 (7.5) | 75.6 | 1.00 (0.76–1.32) | 1.24 (0.85–1.82) |
| Noncore | 306 (2.1) | 77.8 | 1.130 (0.82–1.56) | 1.25 (0.83–1.88) |
Sources: (1) Medicaid claims records and clinician data; (2) the 2012–2013 American Hospital Association Annual Survey; (3) the 2012–2013 Health Resources and Human Services Administration Area Resource File; and (4) a 2012–2013 New York State (NYS) Managed Behavioral Healthcare Organizations (MBHOs) Discharge File created during a statewide quality assurance program in which NYS contracted with five MBHOs in geographically distinct regions to review fee-for-service inpatient psychiatric admissions. Data includes patients ages 18–64 admitted to an inpatient psychiatric unit during 2012–2013 with a principal diagnosis of any mental disorder; Elixhauser Comorbidity Index (ECI) scores based on clinical diagnoses during the 12 months prior to each unique individual’s initial inpatient admission.
In addition to conducting the analysis with the dichotomous ECI variable (0 or ≥ 1), we also conducted these analyses using a continuous ECI variable as well as a categorical variable breaking ECI into quartiles (0, 1, 2–3, and ≥4) and found that associations were consistent between the dichotomous, continuous, and quartile categorical analyses.
3. Results
A total of 14,458 unique Medicaid beneficiaries between ages 18 and 64 were identified as meeting eligibility criteria.
3.1. Medical Comorbidity Across Age Groups
A vast majority of individuals had significant comorbidity, including among young people (Figure 1). The portion of psychiatric inpatients with at least one comorbid medical diagnosis was 74.9% overall, including 57.5% for people ages 18–24, 63.1% for people ages 25–34, 76.5% for people ages 35–44, 84.8% of people ages 45–54, and 89.4% of people ages 55–64. Thirty percent of 18- to 24-year-olds had an ECI of two or more, and the most common disorder in this age group was pulmonary disease (see supplemental appendix). Among 55 to 64-year-olds, three quarters had an ECI of two or more and nearly half had four or more medical comorbidities.
3.2. Types of Medical Comorbidities
An analysis of ECI categories shows that serious chronic health conditions were highly prevalent in the study population (Table 1). Metabolic conditions such as hypertension (43.1%), diabetes (27.7%) and obesity (24.3%) were most frequently observed, in addition to chronic pulmonary disease (33.2%). Neurologic disorders, including traumatic and degenerative disorders of the brain and spinal cord, affected 16.7% of the population. Additional disorders affecting renal (16.3%), hepatic (10.9%), endocrine (10.4%), hematologic (10.4%), and cardiac (9.2%) systems were also common. Of note, 5.1% were identified as having been diagnosed with HIV or AIDS, and oncologic conditions were detected in 3.0% of the sample.
3.3. Patient-Level Factors
Consistent with the descriptive trends of increasing comorbidity with older age presented above, when comparing individuals without medical comorbidities (ECI = 0) to those with comorbidities (ECI ≥ 1), older age was the strongest effect observed, with higher odds of medical comorbidities in older age groups (Table 2). The 55 to 64 age group had 6.34 times the odds (99% CI: 4.91–8.19) of having at least one medical comorbidity compared to 18 to 24-year-olds in the adjusted analysis.
In addition to older age, female gender was associated with 1.66 greater odds (99% CI: 1.48–1.86) of having medical comorbidities. When compared to schizophrenia, a primary diagnosis of schizoaffective disorder (Adjusted Odds Ratio [AOR] 1.47; 99% CI: 1.23–1.76), bipolar disorders (AOR 1.40; 99% CI: 1.15–1.7), depressive disorders (AOR 1.65; 99% CI: 1.37–2.00), and other mental health disorders (AOR 1.58; 99% CI: 1.25–2.01) had increased odds of having a medical comorbidity.
Having a length of stay between 31 and 60 days compared to 4 or fewer days was associated with lower odds of medical comorbidity (AOR 0.67; 99% CI: 0.52–0.87). Additionally, lack of prior engagement in psychiatric outpatient services was associated with lower odds of having a medical comorbidity (AOR 0.70; 99% CI: 0.60–0.82).
Factors such as race and ethnicity, homelessness, and co-occurring substance use disorders did not have significant associations with the overall ECI score. However, there were some notable findings when analyzing factors associated with specific Elixhauser categories. People with race or ethnicity described as Puerto Rican-Hispanic had higher rates of chronic pulmonary disease, people who were non-Hispanic black had significantly higher rates of HIV/AIDS, and both groups had higher rates of hypertension and diabetes. Rates of chronic pulmonary disease were significantly higher in psychiatric inpatients identified as homeless at admission. Finally, patients with co-occurring substance use diagnosis at discharge had significantly higher rates of chronic pulmonary disease, liver disease, and HIV/AIDS, and lower rates of obesity and diabetes. rates of hypertension, obesity, and diabetes were significantly lower in people who had less prior engagement in psychiatric outpatient services. Additional findings are presented in Supplemental Tables 2a–g.
3.4. Hospital-Level Factors
The adjusted odds of medical comorbidity were significantly lower among individuals admitted to medium (AOR 0.54; 99% CI: 0.35–0.83) or large (AOR 0.54; 99% CI: 0.34–0.86) hospitals, as compared to small hospitals (Table 3). The unadjusted model showed that patients whose inpatient stays were at private for-profit hospitals had significantly lower odds of having a medical comorbidity compared to patients at public hospitals (OR 0.38; 99% CI: 0.26–0.56), though this finding was not statistically significant after controlling for other variables. The unadjusted odds of having medical comorbidities was higher for patients admitted to hospitals with high rates of readmissions compared to hospitals with lower readmission rates (OR 1.38; 99% CI: 1.06–1.79), though this too was not statistically significant in the adjusted model. Hospital-level factors such as percent of patients insured by Medicaid, percent of patients with substance use disorder diagnoses, provision of outpatient psychiatric services, and teaching hospital status did not have significant associations with medical comorbidities.
3.5. System-Level Factors
People admitted to hospitals located in higher poverty areas had higher odds of having medical comorbidity (OR 1.23; 99% CI: 1.02–1.49), though this finding did not remain statistically significant after controlling for other variables (Table 3). Urban/rural classifications were not associated with medical comorbidity.
4. Discussion
This statewide analysis of Medicaid beneficiaries with psychiatric hospitalizations demonstrates high rates of medical comorbidity in this vulnerable population, particularly among young people. In fact, 57.5% of psychiatric inpatients aged 18–24 had one or more medical comorbidity and 30% had two or more.14 The ECI categories described in this report represent serious chronic medical conditions that are associated with significant morbidity and mortality. Psychiatric inpatients who were more likely to have higher ECIs include older adults, females, people with shorter lengths of stay, people with non-schizophrenia diagnoses, and people who have been actively engaged in care. Hospitals that are smaller, publicly operated, have higher rates of readmissions, and are located in regions with higher rates of poverty may be more likely to treat patients with more medical comorbidities.
When compared with prevalence in the general U.S. household population as described by the National Health and Nutrition Examination Survey (NHANES), this sample had higher rates of diagnosed comorbid medical illnesses: hypertension 43.1% vs. 29.0%, pulmonary disease 33.2% vs. 13.5%, diabetes 27.7% vs. 7.7%, hypothyroidism 10.4% vs. 1.3%, and HIV/AIDS 5.1% vs. 1.3%.30 The one exception was obesity, with a rate of 24.3% in this sample compared to 33.8% in the general population according to NHANES,30 though this finding may be due to the fact that obesity is inconsistently coded in administrative claims data31,32 and measured directly in NHANES. Also worth noting are the low rates of nonmalignant tumors and malignancies observed in the inpatient study population, which may be partially explained by inadequate cancer screenings in people with mental disorders.33,11,34
Of note is the degree to which young people in this study were diagnosed with medical comorbidities—a key demographic for engaging early on in medical care so as to prevent future complications. Even in the youngest age groups, a majority had at least one medical comorbidity diagnosis and a third had two or more, which is consistent with previous findings in diabetes8,9 but has not been previously described across multiple medical illnesses. The fact that chronic pulmonary disease diagnoses were the most common medical diagnosis in younger people with psychiatric admissions is likely related to high rates of cigarette smoking in this population.35 Also highly concerning is prevalence of HIV among these young people with mental disorders. This finding is not only troubling because it is higher than the general young adult population (1.2% vs. 0.1%),36 but also because it is likely lower than the true prevalence in this population given poor HIV testing practices.13 We believe that addressing HIV testing and care in inpatient psychiatric settings is an opportunity to work towards national Getting to Zero HIV reduction efforts.37–39
This study also helps identify attributes of hospitals, whether because of treatment seeking patterns or hospital admission and screening practices, that were more likely to have a case mix of patients with higher rates of medical conditions. Hospitals located in regions with higher rates of poverty may treat psychiatric inpatients with greater medical burden due to socioeconomic risk factors for poor health,9 while settings with higher rates of readmissions may treat patients with more complex presentations that put them at greater risk for medical comorbidities.15 Hospitals with more than 100 beds may treat psychiatric inpatients with less medical burden due to selective admission practices, while patients admitted for over 30 days may have fewer medical comorbidities due to selective discharge practices. We believe it is critical to leverage population health approaches to universally screen and then provide evidence-based treatment across settings.
While higher rates of comorbid medical diagnoses among females may be due to gender differences in the prevalence of the Elixhauser disease categories, as has been described in studies showing higher rates of metabolic disorders among women with schizophrenia,40 this finding may also be attributed to detection bias resulting from higher rates of health care seeking among women.41 The opposite may be true for people with schizophrenia, who as compared to people with other serious mental illnesses may have lower detected rates of comorbid medical diagnoses related to their less frequent medical care seeking behavior.42,43 Of note, race/ethnicity, homelessness and co-occurring substance use disorders were not found to be associated with higher ECI in this analysis, nor was a hospital’s percentage of Medicaid beneficiaries, teaching hospital status or urban/rural classification, which suggests more equitable medical disease burden across these populations and settings. Future studies should continue to explore the prevalence of comorbidity in vulnerable populations.
In light of these high rates of comorbid medical diagnoses across ECI categories detected in the 12 months prior to psychiatric admission, there is a compelling need for workflows that link these patients to medical services. Prior studies have examined outcomes associated with integration of physical healthcare into outpatient mental health settings,44,45 but less attention has been paid to psychiatric hospitalizations as an important opportunity to help stabilize and connect patients to care from both a mental and physical health perspective. As a first step, clinicians working in inpatient psychiatric settings should consider implementing the following measures:
Medical screening for Medicaid-insured psychiatric inpatients, which constitutes a targeted public health approach given that this population is at high-risk for medical comorbidity;
When positive screens are detected, evidence-based treatments that can be feasibly initiated in inpatient settings, including with input from medical consultants; and
If medical issues are identified, discharge planning requirements that include a scheduled appointment with medical providers.
While ideally these interventions would be extended to all psychiatric inpatients, the findings of this study suggest that priority populations include women and young patients as well as older age groups. Small and publicly operated hospitals in poorer regions are more likely to have a higher case mix of people with medical comorbidities and should be proactive in implementing these measures. Expansion of reimbursement policies and medical outcome quality measurement can help hospitals to overcome resource constraints and staff shortages that may interfere with improving medical care workflows for psychiatric inpatients. Hospitals may also consider the implementation of ―medical psychiatry units,‖ which have been described in the Netherlands but have been minimally studied in the US.46 Additional research into each of these interventions in inpatient settings is critical to inform their use in clinical practice.
This study has some limitations. First, the medical conditions are limited to those captured by the ECI and do not represent all medical comorbidity in the population. Second, the medical conditions are derived from claims data and do not include clinically unrecognized and therefore undiagnosed conditions, particularly given the literature on under-screening for medical conditions in people with mental disorders.10,11,13,34 Third, in interpreting the raw rates of medical illness in this population compared to the general population, rates of medical illness may be higher in a Medicaid-eligible population simply due to income and disability that determine eligibility. Fourth, the generalizability of study results are constrained by exclusion of people under age 18 and over age 64, payment sources other than Medicaid, and dual Medicare and Medicaid coverage, a group with disproportionately high use of acute mental health services.47 Fifth, the analysis does not include laboratory or prescription claims data that could have been used to measure engagement in medical care prior to the index psychiatric admission. Finally, these data were collected from a single state and may not generalize to Medicaid beneficiaries throughout the nation.
Overall, the results presented here highlight significant medical comorbidity among psychiatric inpatient populations. Though several barriers impede access to physical health care for people with mental disorders, attention to comorbid medical illness is important given the decreased lifespans of this population. Novel approaches such as integrating physical health care into specialty behavioral health settings have begun to show promise and require further research and evaluation.48–51
5. Conclusion
Medicaid beneficiaries admitted for inpatient psychiatric care have high rates of medical comorbidity. Young people in this population have particularly high rates of comorbid medical illnesses. A high prevalence of common medical diagnoses among psychiatric inpatients underscores the importance of adequate detection and medical treatment of medical comorbidities in this patient population. Further research is needed to examine the extent to which medical conditions are recognized during psychiatric admissions as well as specific protocols for screening and follow-up that can be implemented in these settings.
Supplementary Material
Highlights:
74.9% of psychiatric inpatients on Medicaid have at least one medical comorbidity
Among psychiatric inpatients aged 18–24, 30% have 2 or more medical diagnoses
HIV and pulmonary disease disproportionately affect younger psychiatric inpatients
Women psychiatric inpatients have greater medical burden than men
Hospitals with <100 beds are more likely to admit patients with medical diagnoses
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Walker ER, McGee RE, Druss BG. Mortality in Mental Disorders and Global Disease Burden Implications: A Systematic Review and Meta-analysis. JAMA Psychiatry 2015;72(4):334–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Olfson M, Gerhard T, Huang C, Crystal S, Stroup TS. Premature Mortality Among Adults With Schizophrenia in the United States. JAMA Psychiatry 2015;72(12):1172–81. [DOI] [PubMed] [Google Scholar]
- 3.Roshanaei-Moghaddam B, Katon W. Premature Mortality From General Medical Illnesses Among Persons With Bipolar Disorder: A Review. Psychiatr Serv 2009;60(2):147–56. [DOI] [PubMed] [Google Scholar]
- 4.Cuijpers P, Vogelzangs N, Twisk J, Kleiboer A, Li J, Penninx BW. Differential mortality rates in major and subthreshold depression: meta-analysis of studies that measured both. Br J Psychiatry J Ment Sci 2013;202(1):22–7. [DOI] [PubMed] [Google Scholar]
- 5.Piotrowski P, Gondek TM, Królicka-Deręgowska A, Misiak B, Adamowski T, Kiejna A. Causes of mortality in schizophrenia: An updated review of European studies. Psychiatr Danub 2017;29(2):108–20. [DOI] [PubMed] [Google Scholar]
- 6.Osborn DP, Wright CA, Levy G, King MB, Deo R, Nazareth I. Relative risk of diabetes, dyslipidaemia, hypertension and the metabolic syndrome in people with severe mental illnesses: Systematic review and metaanalysis. BMC Psychiatry 2008;8:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janssen EM, McGinty EE, Azrin ST, Juliano-Bult D, Daumit GL. Review of the Evidence: Prevalence of Medical Conditions in the United States Population with Serious Mental Illness. Gen Hosp Psychiatry 2015;37(3):199–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mangurian C, Keenan W, Newcomer JW, Vittinghoff E, Creasman JM, Schillinger D. Diabetes Prevalence Among Racial-Ethnic Minority Group Members With Severe Mental Illness Taking Antipsychotics: Double Jeopardy? Psychiatr Serv 2017;68(8):843–6. [DOI] [PubMed] [Google Scholar]
- 9.Mangurian CV, Schillinger D, Newcomer JW, et al. Diabetes and Prediabetes Prevalence by Race and Ethnicity Among People With Severe Mental Illness. Diabetes Care 2018;41(7):e119–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mangurian C, Newcomer JW, Modlin C, Schillinger D. Diabetes and Cardiovascular Care Among People with Severe Mental Illness: A Literature Review. J Gen Intern Med 2016;31(9):1083–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.James M, Thomas M, Frolov L, et al. Rates of Cervical Cancer Screening Among Women With Severe Mental Illness in the Public Health System. Psychiatr Serv 2017;68(8):839–42. [DOI] [PubMed] [Google Scholar]
- 12.Thomas M, James M, Vittinghoff E, Creasman JM, Schillinger D, Mangurian C. Mammography Among Women With Severe Mental Illness: Exploring Disparities Through a Large Retrospective Cohort Study. Psychiatr Serv Wash DC 2018;69(1):48–54. [DOI] [PubMed] [Google Scholar]
- 13.Mangurian C, Cournos F, Schillinger D, et al. Low Rates of HIV Testing Among Adults With Severe Mental Illness Receiving Care in Community Mental Health Settings. Psychiatr Serv 2017;68(5):443–8. [DOI] [PubMed] [Google Scholar]
- 14.Jansen L, van Schijndel M, van Waarde J, van Busschbach J. Health-economic outcomes in hospital patients with medical-psychiatric comorbidity: A systematic review and meta-analysis. PloS One 2018;13(3):e0194029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Šprah L, Dernovšek MZ, Wahlbeck K, Haaramo P. Psychiatric readmissions and their association with physical comorbidity: a systematic literature review. BMC Psychiatry 2017;17(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaplan RM, Glassman JR, Milstein A. Effects of Mental Health on the Costs of Care for Chronic Illnesses. Psychiatr Serv 2019;70(11):1013–9. [DOI] [PubMed] [Google Scholar]
- 17.Melek SP, Norris DT, Paulus J, Matthews K, Weaver A, Davenport S. Potential economic impact of integrated medical-behavioral healthcare: Updated projections for 2017 [Internet]. Denver, CO: Milliman Inc.; 2018. Available from: https://www.milliman.com/uploadedFiles/insight/2018/Potential-Economic-Impact-Integrated-Healthcare.pdf [Google Scholar]
- 18.Rothbard AB, Blank MB, Staab JP, et al. Previously Undetected Metabolic Syndromes and Infectious Diseases Among Psychiatric Inpatients. Psychiatr Serv 2009;60(4):534–7. [DOI] [PubMed] [Google Scholar]
- 19.Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18–5068, NSDUH Series H-53). [Internet]. Rockville, MD: 2018. [cited 2018 Oct 16]. Available from: https://www.samhsa.gov/data [Google Scholar]
- 20.Owens PL, Heslin KC, Fingar KR, Weiss AJ. Co-occurrence of Physical Health Conditions and Mental Health and Substance Use Conditions Among Adult Inpatient Stays, 2010 Versus 2014 - HCUP Statistical Brief #240 [Internet]. Rockville, MD: Agency for Healthcare Research and Quality; 2018. [cited 2019 Dec 1]. Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb249-Mental-Substance-Use-Disorder-Hospital-Stays-2016.pdf [PubMed] [Google Scholar]
- 21.Weber NS, Cowan DN, Millikan AM, Niebuhr DW. Psychiatric and General Medical Conditions Comorbid With Schizophrenia in the National Hospital Discharge Survey. Psychiatr Serv 2009;60(8):1059–67. [DOI] [PubMed] [Google Scholar]
- 22.Razzano LA, Cook JA, Yost C, et al. Factors associated with co-occurring medical conditions among adults with serious mental disorders. Schizophr Res 2015;161(2):458–64. [DOI] [PubMed] [Google Scholar]
- 23.Garfield RL. Mental Health Financing in the United States: A Primer [Internet]. Kaiser Commission on Medicaid and the Uninsured; 2011. Available from: http://kff.org/medicaid/report/mental-health-financing-in-the-united-states/
- 24.AHA Annual Survey DatabaseTM Fiscal Year 2012 [Internet]. 2013. [cited 2019 Nov 21];Available from: http://www.ahadataviewer.com/book-cd-products/aha-survey/
- 25.US Department of Health and Human Services, Health Resources and Human Services Administration, Bureau of Health Professions. Area Health Resources Files [database on the Internet] [Internet]. 2012. [cited 2019 Nov 21];Available from: https://data.hrsa.gov/topics/health-workforce/ahrf
- 26.Haselden M, Corbeil T, Tang F, et al. Family Involvement in Psychiatric Hospitalizations: Associations With Discharge Planning and Prompt Follow-Up Care. Psychiatr Serv 2019;appi.ps.201900028. [DOI] [PMC free article] [PubMed]
- 27.Quan H, Sundararajan V, Halfon P, et al. Coding Algorithms for Defining Comorbidities in ICD-9-CM and ICD-10 Administrative Data. Med Care 2005;43(11):1130–9. [DOI] [PubMed] [Google Scholar]
- 28.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A Modification of the Elixhauser Comorbidity Measures Into a Point System for Hospital Death Using Administrative Data. Med Care 2009;47(6):626. [DOI] [PubMed] [Google Scholar]
- 29.Policy MCfH. Elixhauser Comorbidity Index: Concept Description and SAS Code [Internet]. [cited 2019 Nov 21];Available from: http://mchp-appserv.cpe.umanitoba.ca/viewConcept.php?printer=Y&conceptID=1436
- 30.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey (NHANES) [Internet]. [cited 2019 Nov 21];Available from: https://wwwn.cdc.gov/nchs/nhanes/Default.aspx
- 31.Quan H, Li B, Duncan Saunders L, et al. Assessing Validity of ICD-9-CM and ICD-10 Administrative Data in Recording Clinical Conditions in a Unique Dually Coded Database. Health Serv Res 2008;43(4):1424–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stephens MB. Coding and Obesity: Room to Grow. J Am Board Fam Med 2011;24(3):329– 30. [DOI] [PubMed] [Google Scholar]
- 33.Woodhead C, Cunningham R, Ashworth M, Barley E, Stewart RJ, Henderson MJ. Cervical and breast cancer screening uptake among women with serious mental illness: a data linkage study. BMC Cancer 2016;16(1):819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hwong A, Wang K, Bent S, Mangurian C. Breast Cancer Screening in Women With Schizophrenia: A Systematic Review and Meta-Analysis. Psychiatr Serv 2019;appi.ps.201900318. [DOI] [PMC free article] [PubMed]
- 35.Dickerson F, Schroeder J, Katsafanas E, et al. Cigarette Smoking by Patients With Serious Mental Illness, 1999–2016: An Increasing Disparity. Psychiatr Serv 2017;69(2):147–53. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention (CDC). Estimated HIV incidence and prevalence in the United States, 2010–2016: HIV Surveillance Supplemental Report [Internet]. 2019. [cited 2019 Dec 21];Available from: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-24-1.pdf
- 37.Shumway M, Mangurian C, Carraher N, et al. Increasing HIV Testing in Inpatient Psychiatry. Psychosomatics 2018;59(2):186–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Katz I, Jha AK. HIV in the United States: Getting to Zero Transmissions by 2030. JAMA 2019;321(12):1153–4. [DOI] [PubMed] [Google Scholar]
- 39.Carrico AW. Getting to Zero: Targeting Psychiatric Comorbidities as Drivers of the HIV/AIDS Epidemic. Int J Behav Med 2019;26(1):1–2. [DOI] [PubMed] [Google Scholar]
- 40.McEvoy JP, Meyer JM, Goff DC, et al. Prevalence of the metabolic syndrome in patients with schizophrenia: Baseline results from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial and comparison with national estimates from NHANES III. Schizophr Res 2005;80(1):19–32. [DOI] [PubMed] [Google Scholar]
- 41.Thompson AE, Anisimowicz Y, Miedema B, Hogg W, Wodchis WP, Aubrey-Bassler K. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract 2016;17:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Farasatpour M, Janardhan R, Williams CD, Margenthaler JA, Virgo KS, Johnson FE. Breast cancer in patients with schizophrenia. Am J Surg 2013;206(5):798–804. [DOI] [PubMed] [Google Scholar]
- 43.Tsay J-H, Lee C-H, Hsu Y-J, et al. Disparities in appendicitis rupture rate among mentally ill patients. BMC Public Health 2007;7:331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scharf DM, Eberhart NK, Schmidt N, et al. Integrating Primary Care Into Community Behavioral Health Settings: Programs and Early Implementation Experiences. Psychiatr Serv 2013;64(7):660–5. [DOI] [PubMed] [Google Scholar]
- 45.Wells R, Kite B, Breckenridge E, Sunbury T. Community Mental Health Center Integrated Care Outcomes. Psychiatr Q 2018;89(4):969–82. [DOI] [PubMed] [Google Scholar]
- 46.Caarls PJ, van Schijndel MA, Kromkamp M, et al. Need analysis for a new high acuity medical psychiatry unit: which patients are considered for admission? BMC Health Serv Res 2019;19(1):139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schroeder SM, Peterson M-L. Identifying Variability in Patient Characteristics and Prevalence of Emergency Department Utilization for Mental Health Diagnoses in Rural and Urban Communities. J Rural Health 2018;34(4):369–76. [DOI] [PubMed] [Google Scholar]
- 48.Scharf DM, Schmidt Hackbarth N, Eberhart NK, et al. General Medical Outcomes From the Primary and Behavioral Health Care Integration Grant Program. Psychiatr Serv 2016;67(11):1226–32. [DOI] [PubMed] [Google Scholar]
- 49.Murphy KA, Daumit GL, Stone E, McGinty EE. Physical health outcomes and implementation of behavioural health homes: a comprehensive review. Int Rev Psychiatry 2018;30(6):224–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mangurian C, Niu G, Schillinger D, Newcomer JW, Gilmer T. Understanding the Cost of a New Integrated Care Model to Serve CMHC Patients Who Have Serious Mental Illness. Psychiatr Serv 2017;68(10):990–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mangurian C, Schillinger D, Newcomer JW, et al. Comorbid Diabetes and Severe Mental Illness: Outcomes in an Integrated Health Care Delivery System. J Gen Intern Med [Internet] 2019. [cited 2019 Nov 21];Available from: 10.1007/s11606-019-05489-3 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


