Abstract
Background
Our aim was to present data on the prevalence of probable depression and anxiety and to determine their correlates during the COVID-19 pandemic in seven European countries using a longitudinal approach.
Methods
Longitudinal data (wave 4 in November 2020: n = 7,115; wave 5 in January 2021: n = 7,068; wave 6 in April 2021: n = 7,204) were taken from the European COvid Survey (ECOS), a representative sample of non-institutionalized inhabitants from Germany, United Kingdom, Denmark, Netherlands, France, Portugal and Italy aged 18+. Probable depression and anxiety were quantified using the established and validated PHQ-4 (2-item depression scale, PHQ-2 / 2-item anxiety scale, GAD-2).
Results
In wave 4 (wave 5; wave 6), 26.6% (25.5%; 23.8%) of all respondents had probable depression and 25.7% (23.6%; 22.1%) had probable anxiety. Prevalence rates for probable depression and probable anxiety differed significantly between countries. Among all countries and waves, particularly high prevalence rates were found among individuals aged 18 to 29 years. Longitudinal analysis showed that the likelihood of probable depression was positively associated with increasing age, great income difficulties and lower health-related quality of life. The likelihood of probable anxiety was positively associated with income difficulties, and lower health-related quality of life.
Limitations
Screening tool was used to quantify the outcomes.
Conclusion
The magnitude of probable depression and anxiety during the COVID-19 pandemic in European countries was highlighted. Moreover, determining the factors associated with probable depression or anxiety (e.g., income difficulties, worse health-related quality of life) may assist in identifying individuals at increased risk.
Keywords: Prevalence, Depression, Anxiety, Patient Health Questionnaire (PHQ), Mental disorders, SARS-CoV-2, Coronavirus, COVID-19, Mental illness
1. Introduction
In the past decades high prevalence rates of depression and anxiety have been reported for various countries (Investigators et al., 2004b; Kessler et al., 2003). During the current COVID-19 pandemic, various challenges for mental health arise such as temporary social isolation or loneliness (Stolz et al., 2021) as well as economic risks (such as unemployment, loss of income particularly for self-employed individuals). In line with this, a meta-analysis published in July 2020 identified a prevalence of anxiety (n = 17 studies) of about 32% (95% CI: 28–37) and a prevalence of depression (n = 14 studies) of about 34% (95% CI: 28–41) among general populations during the COVID-19 pandemic (Salari et al., 2020). However, it should be noted that the great majority of the existing studies are based on convenience samples (e.g., (Banna et al., 2020)), and only few studies were based on nationally representative samples during the pandemic (Brunoni et al., 2021; Budimir et al., 2021; Czeisler et al., 2021; Daly and Robinson, 2021; Hou et al., 2021a, 2021b; Hubbard et al., 2021; Hyland et al., 2020, 2021; Röhr et al., 2020; Twenge and Joiner, 2020; Wang et al., 2020b; Winkler et al., 2020). Thereof, nine studies examined depression or anxiety in specific countries (such as Ireland or the Czech Republic (Hyland et al., 2020; Winkler et al., 2020)), whereas only two studies compared representative data from two countries (United Kingdom and Austria (Budimir et al., 2021); Australia and United States (Czeisler et al., 2021)). Moreover, there is limited evidence based on representative longitudinal studies during the COVID-19 pandemic (Daly and Robinson, 2021; Hou et al., 2021b; Hyland et al., 2021; Twenge and Joiner, 2020; Winkler et al., 2020) and none of the existing studies compared more than two countries.
Therefore, our aim was to present data on the prevalence of probable depression and anxiety and to determine their correlates during the COVID-19 pandemic in several European countries using a longitudinal approach. To this end, longitudinal data were taken from the European COvid Survey (ECOS) covering Germany, United Kingdom, Denmark, Netherlands, France, Portugal and Italy. Knowledge about the factors longitudinally associated with depression and anxiety during the COVID-19 pandemic may help health professionals to identify individuals at risk for these mental disorders. This may assist in mitigating the expected increase in mental disorders (Riedel-Heller and Richter, 2020).
2. Methods
2.1. Sample
Longitudinal data were taken from wave 4 (November 2020, n = 7115), wave 5 (January 2021: n = 7068), and wave 6 (April 2021, n = 7204) from the European COvid Survey (ECOS) including Germany, United Kingdom, Denmark, Netherlands, France, Portugal and Italy. In each country, data from a sample of about 1000 adult individuals were recruited via the market research company Dynata. To reach the general population several recruiting techniques were used (open recruitment, affiliate networks, mobile apps or loyalty programs). Quotas were used to ensure the representativeness (in terms of gender, age, region and education - based on the national census statistics) within each country. Further details are given by Sabat et al. (Sabat et al., 2020).
Written informed consent was obtained from individual participants by Dynata. Confidentiality and anonymity of the participants were ensured. Ethical approval for this study was provided by the University of Hamburg, Germany (umbrella project “Countering COVID-19: A European survey on the acceptability of and commitment to preventive measures”). It was not required to obtain ethical approval from all countries because, among other things, patients were not involved.
2.2. Dependent variables
Probable depression and anxiety were quantified using the validated PHQ-4 (2-item depression scale, PHQ-2 (Kroenke et al., 2003; Löwe et al., 2005), and 2-item anxiety scale, GAD-2 (Kroenke et al., 2007)). While the PHQ-2 includes the two DSM-V diagnostic main criteria for depressive disorders (Association, 2013), the GAD-2 includes the two main criteria for GAD. It has been shown that the GAD-2 is a screening tool for post-traumatic stress disorder (specificity: 0.81; sensitivity: 0.59), social anxiety (specificity: 0.81; sensitivity: 0.70), and panic disorder (specificity: 0.81; sensitivity: 0.76) (Kroenke et al., 2007). The PHQ-2 is a screening tool for major depressive disorder (specificity: 0.78; sensitivity: 0.87) and any depressive disorders (specificity: 0.86; sensitivity: 0.79) (Löwe et al., 2005).
The Patient Health Questionnaire-4 (PHQ-4) combines these two measures into a four item scale. In accordance with previous recommendations (Kroenke et al., 2007; Löwe et al., 2005), sum scores of ≥ 3 (for both tools, PHQ-2 and GAD-2), were used as cut-off points for probable depression and anxiety, respectively. Additional details are given elsewhere (Kroenke et al., 2009; Löwe et al., 2010).
In our study, Cronbach's alpha for PHQ-4 was 0.89 (GAD-2: 0.88; PHQ-2: 0.79) in wave 4. In wave 5, it was 0.91 (GAD-2: 0.88; PHQ-2: 0.82). In wave 6, it was also 0.91 (GAD-2: 0.88; PHQ-2: 0.83). This indicates a good internal consistency of these instruments.
2.3. Independent variables
In regression analysis, factors were included as follows: age (years), marital status (married/registered partnership; living together (relationship); living alone (single); living alone (in a relationship); widowed; other), educational level (low education; medium education; high education; defined based on country specific education system, please see Varghese et al. for further details (Varghese et al., 2021)), perceived difficulties with income (exact wording: “Thinking of your household's total monthly income, would you say that your household is able to make ends meet…“: with great difficulty; with some difficulties; fairly easily; easily), infection with the novel coronavirus (no; yes, confirmed; yes, but not yet confirmed; don't know), and health-related quality of life (EQ-VAS (EuroQol Group, 1990), ranging from 0 (worst) to 100 (best)).
The time-constant variables (i.e., these variables are constant within individuals over time) country (Germany; United Kingdom; Denmark; Netherlands; France; Portugal; Italy) and gender (men; women) were additionally used for descriptive purposes.
2.4. Statistical analysis
Prevalence rates for probable depression and anxiety are shown (total and stratified by sex, country, age group, educational level and infection with the novel coronavirus). Thereafter, correlates of probable depression and anxiety were estimated using conditional FE logistic regressions (at individual level) to exploit the longitudinal data structure (Cameron and Trivedi, 2005). In contrast to logistic RE regressions, conditional FE logistic regressions provide consistent estimates when time-constant factors (observed and unobserved) are associated with the time-varying explanatory variables (when the exogeneity assumption is fulfilled) (Cameron and Trivedi, 2005).
Our choice was supported by Hausman-tests (with probable depression as outcome measure: Chi²=223.82, p<.001; with probable anxiety as outcome measure: Chi² = 267.52, p < .001). It is worth noting that conditional FE logistic regressions solely use changes within individuals over time (e.g., intraindividual changes from absence of probable depression to presence of probable depression or intraindividual changes in health-related quality of life from wave 4 to wave 6).
It should be noted that the analytical samples solely refer to individuals with intraindividual changes in probable depression or probable anxiety from wave 4 to wave 6. Therefore, the two analytical samples are much smaller than the original samples in wave 4 to wave 6. However, this is not a shortcoming of the FE strategy. It solely reflects the fact that a subset of individuals had such changes over time.
The level of significance was set at α = 0.05. Stata 16.1 was used to conduct statistical analysis.
3. Results
3.1. Prevalence of probable depression and anxiety stratified by sex, age, education, country, and infection with the novel coronavirus
Prevalence rates of probable depression and probable anxiety are shown in Table 1 . In wave 4 (wave 5; wave 6), 26.6% (25.5%; 23.8%) of the individuals had probable depression and 25.7% (23.6%; 22.1%) of the individuals had probable anxiety based on the PHQ-4 cut-off values. Moreover, 17.7% (18.2%; 16.7%) of the individuals had both probable depression and probable anxiety. Overall, there was a slight trend of decreasing prevalence rates in both probable depression and probable anxiety from November 2020 to April 2021.
Table 1.
Prevalence rate for probable depression and probable anxiety stratified by sex, country, age group, education and infection with the novel coronavirus in wave 4 (November 2020), wave 5 (January 2021) and wave 6 (April 2021) (N and%).
| Wave 4 | Wave 5 | Wave 6 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Sample size | Presence of probable depression | Presence of probable anxiety | Sample size | Presence of probable depression | Presence of probable anxiety | Sample size | Presence of probable depression | Presence of probable anxiety | |
| Total sample | N = 7115 | 26.6% | 25.7% | N = 7068 | 23.8% | 23.6% | N = 7110 | 23.8% | 22.1% |
| Gender | |||||||||
| Male | N = 3416 | 23.1% | 20.9% | N = 3415 | 21.3% | 20.2% | N = 3456 | 21.3% | 18.7% |
| Female | N = 3699 | 30.0% | 30.2% | N = 3653 | 26.2% | 26.7% | N = 3654 | 26.2% | 25.3% |
| Country | |||||||||
| Germany | N = 1043 | 21.1% | 21.0% | N = 1008 | 23.7% | 21.6% | N = 1013 | 23.7% | 22.3% |
| United Kingdom | N = 1006 | 30.2% | 30.1% | N = 1016 | 29.5% | 30.1% | N = 1024 | 29.5% | 27.1% |
| Denmark | N = 1012 | 41.1% | 21.2% | N = 1012 | 27.0% | 20.8% | N = 1023 | 27.0% | 17.7% |
| Netherlands | N = 1020 | 17.5% | 17.0% | N = 1006 | 20.2% | 17.3% | N = 1024 | 20.2% | 17.9% |
| France | N = 1017 | 25.3% | 28.5% | N = 1012 | 16.3% | 24.4% | N = 970 | 16.3% | 14.7% |
| Portugal | N = 1015 | 22.8% | 29.1% | N = 1005 | 23.8% | 26.0% | N = 1032 | 23.8% | 25.9% |
| Italy | N = 1002 | 28.8% | 33.6% | N = 1009 | 25.7% | 24.9% | N = 1024 | 25.7% | 28.5% |
| Age group | |||||||||
| 18–29 | N = 1201 | 39.9% | 39.5% | N = 1130 | 40.3% | 41.9% | N = 1180 | 40.3% | 40.2% |
| 30–49 | N = 2652 | 28.9% | 30.0% | N = 2644 | 26.1% | 28.6% | N = 2643 | 26.1% | 23.9% |
| 50–64 | N = 1799 | 22.5% | 20.5% | N = 1817 | 16.9% | 16.2% | N = 1820 | 16.9% | 14.8% |
| 65–74 | N = 1241 | 17.3% | 13.3% | N = 1269 | 10.5% | 9.8% | N = 1076 | 10.5% | 10.6% |
| 75+ | N = 218 | 13.8% | 11.9% | N = 208 | 12.1% | 9.6% | N = 214 | 12.1% | 8.0% |
| Education | |||||||||
| Low education | N = 1098 | 24.7% | 24.4% | N = 1171 | 22.5% | 22.0% | N = 1160 | 22.5% | 20.5% |
| Middle education | N = 3045 | 26.8% | 24.8% | N = 2919 | 23.7% | 23.3% | N = 2920 | 23.7% | 22.7% |
| High education | N = 2275 | 27.2% | 27.2% | N = 2978 | 24.4% | 24.5% | N = 3030 | 24.4% | 22.1% |
| Infection with the novel coronavirus | |||||||||
| Yes, confirmed | N = 227 | 52.0% | 52.4% | N = 366 | 40.4% | 42.9% | N = 450 | 40.4% | 40.3% |
| Yes, but not yet confirmed | N = 134 | 45.5% | 40.3% | N = 154 | 48.8% | 53.9% | N = 121 | 48.8% | 37.5% |
| No | N = 6127 | 25.0% | 24.1% | N = 6044 | 21.6% | 21.2% | N = 6112 | 21.6% | 20.0% |
| Don't know | N = 627 | 29.2% | 29.3% | N = 504 | 30.7% | 28.6% | N = 427 | 30.7% | 28.3% |
Notes: In bivariate (cross-sectional) analysis, probable depression and probable anxiety were associated with gender, country, age group and infection with the novel coronavirus in each of the three waves (each case: p < .001), whereas they were not associated with educational level (probable depression, wave 4: 0.286, wave 5: 0.143, wave 6: 0.432; probable anxiety, wave 4: 0.095, wave 5: 0.224, wave 6: 0.320).
In each wave, the prevalence rates of both probable depression and probable anxiety significantly differed between the countries (wave 4, probable depression: Chi²=185.77, p < .001; probable anxiety: Chi²=116.79, p < .001; wave 5, probable depression: Chi²=42.96, p < .001; probable anxiety: Chi²=56.94, p < .001; wave 6, probable depression: Chi²=63.45, p < .001; probable anxiety; Chi²=99.91, p < .001).
In all three waves, individuals aged 18 to 29 years and particularly individuals with an infection with the novel coronavirus (both: ‘yes, confirmed’ and ‘yes, but not yet confirmed’) had high prevalence rates for probable depression and probable anxiety. For example, 40.3% of the individuals aged 18 to 29 years had probable depression (probable anxiety: 40.2%) and 48.8% of the individuals with an unconfirmed infection with the novel coronavirus had probable depression (probable anxiety: 37.5%) in wave 6. In bivariate (cross-sectional) analysis, it may be worth noting that both outcome measures were associated with gender, country, age group and infection with the novel coronavirus in each of the three waves, whereas they were not associated with educational level. Additional details are given in Table 1.
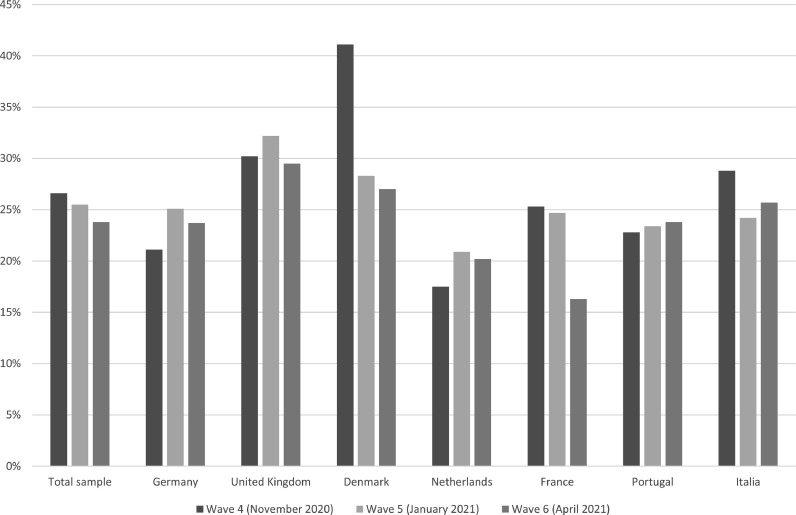
The prevalence rates of probable depression and probable anxiety among the seven European countries from wave 4 to wave 6 are displayed in Fig. 1, Fig. 2 , respectively. With regard to the prevalence rates of probable depression (Fig. 1), while there was some trend of decreasing prevalence rates in Italy and particularly in France (wave 4: 25.3%; wave 6: 16.3%) and Denmark (wave 4: 41.1%; wave 6: 27.0%) with time, no clear trend or slightly increasing prevalence rates were present in the other countries. For example, in the United Kingdom the prevalence rate was 30.2% in wave 4 and 29.5% in wave 6, and in Germany, the prevalence rate was 21.1% in wave 4 and 23.7% in wave 6.
Fig. 1.
Prevalence of probable depression among European countries.
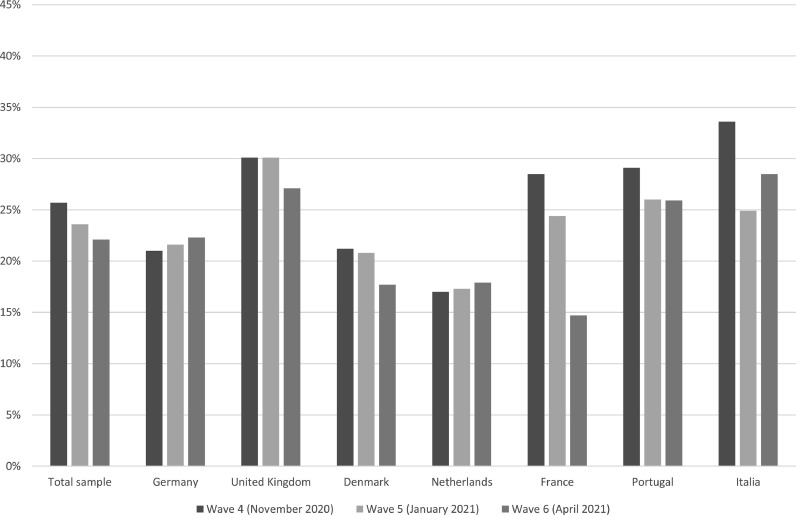
Fig. 2.
Prevalence of probable anxiety among European countries.
With regard to the prevalence rates of probable anxiety (Fig. 2), while there were slightly decreasing prevalence rates in the United Kingdom, Denmark, Portugal, and Italy over time, the prevalence rate sharply decreased in France (wave 4: 28.5%; wave 6: 14.7%) over time. In contrast, almost constant or slightly increasing prevalence rates over time were identified in Germany and the Netherlands.
3.2. Longitudinal regression analysis
Findings of conditional FE logistic regressions are shown in Table 2 . Regressions revealed that the likelihood of probable depression was positively associated with increasing age (OR: 1.02, 95% CI: 1.00–1.04), great income difficulties (OR: 2.31, 95% CI: 1.38–3.87) and lower health-related quality of life (OR: 0.99, 95% CI: 0.98–0.99), whereas it was not associated with other sociodemographic factors and an infection with the novel coronavirus. Moreover, the likelihood of probable anxiety was only positively associated with income difficulties (e.g., great difficulties, OR: 2.39, 95% CI: 1.39–4.10), and lower health-related quality of life (OR: 0.99, 95% CI: 0.98–0.99).
Table 2.
Determinants of probable depression (0 = absence of probable depression, 1 = presence of probable depression) and probable anxiety (0 = absence of probable anxiety, 1 = presence of probable anxiety).
| Independent variables | Probable depression | Probable anxiety |
|---|---|---|
| Age | 1.02* | 1.00 |
| (1.00–1.04) | (0.98–1.03) | |
| Marital status:–Living together (relationship) (Ref.:–married / registered partnership) | 1.05 | 1.12 |
| (0.65–1.71) | (0.69–1.81) | |
| - Living alone (single) | 1.68 | 1.68 |
| (0.87–3.27) | (0.84–3.36) | |
| - Living alone (in a relationship) | 0.85 | 0.83 |
| (0.41–1.74) | (0.39–1.78) | |
| - Widowed | 3.37+ | 3.43 |
| (0.95–11.98) | (0.35–33.93) | |
| - Other | 1.82 | 1.45 |
| (0.87–3.81) | (0.69–3.07) | |
| Education:–Middle (Ref.: low education) | 1.10 | 0.83 |
| (0.79–1.52) | (0.59–1.17) | |
| - High | 0.85 | 1.03 |
| (0.57–1.28) | (0.66–1.60) | |
| Income (ability to make ends meet):–With great difficulty (Ref.: easily) | 2.31⁎⁎ | 2.39⁎⁎ |
| (1.38–3.87) | (1.39–4.10) | |
| - With some difficulty | 1.33 | 1.79⁎⁎ |
| (0.88–2.00) | (1.15–2.77) | |
| - Fairly easily | 1.15 | 1.33 |
| (0.82–1.62) | (0.91–1.95) | |
| Infection with the novel coronavirus:–Yes, confirmed (Ref.: no) | 0.88 | 0.68+ |
| (0.56–1.37) | (0.43–1.08) | |
| - Yes, but not yet confirmed | 1.17 | 0.61 |
| (0.64–2.13) | (0.32–1.18) | |
| - Don't know | 1.23 | 1.06 |
| (0.89–1.69) | (0.77–1.47) | |
| Health-related quality of life (EQ-VAS, ranging from 0 (worst) to 100 (best)) | 0.99⁎⁎⁎ | 0.99⁎⁎⁎ |
| (0.98–0.99) | (0.98–0.99) | |
| Observations | 3683 | 3319 |
| Number of Individuals | 1457 | 1299 |
| Pseudo R² | 0.03 | 0.02 |
Comments: Odds Ratios were reported; 95% confidence intervals in parentheses;.
p < .001.
p < .01.
p < .05.
p < .10.
4. Discussion
4.1. Main findings
Using longitudinal data from the established representative European COvid Survey (ECOS), the main aim of this study was to present data on the prevalence of probable depression and probable anxiety–and to determine their correlates in several European countries during the COVID-19 pandemic. Our study highlighted the magnitude of probable depression and anxiety in November 2020, January 2021 and April 2021 in several European countries. Particularly, individuals in specific countries (e.g., United Kingdom or Italy), individuals aged 18 to 29 years and individuals with an infection with the novel coronavirus (both: ‘yes, confirmed’ and ‘yes, but not yet confirmed’) had high prevalence rates for probable depression and probable anxiety across all waves. Longitudinal regression analysis showed that income difficulties as well as lower health-related quality of life were associated with both the likelihood of probable depression and probable anxiety. The current longitudinal study adds knowledge on the prevalence and correlates of probable depression and probable anxiety in several European countries during the course of the COVID-19 pandemic.
4.2. Previous research and possible explanations
We demonstrated that probable depression and anxiety are frequent in the general adult population in several European countries. Compared to the time prior to the COVID-19 pandemic in Europe, prevalence rates were actually markedly higher in our study taking place during the COVID-19 pandemic (e.g., (Hajek and König, 2020; Investigators et al., 2004a)). For example, based on the PHQ-4 cut-off values, a previous study using nationally representative data from the adult population in Germany showed that about 10.4% of the individuals had probable depression and 9.8% of the individuals had probable anxiety almost ten years ago (Hajek and König, 2020). However, this is in contrast to results from a Brazilian study (Brunoni et al., 2021) showing no significant changes in depressive disorders from 2008 to 2020 and a slight decrease in anxiety disorders in the same period. These differences may be partly explained by differences in the time of data collection also regarding the conditions of the pandemic in the respective countries (May-July 2020 vs. November 2020-April 2021) and cultural differences.
Our findings are rather unsurprising and in accordance with other recent nationally representative studies (Budimir et al., 2021; Czeisler et al., 2021; Daly and Robinson, 2021; Hou et al., 2021a, 2021b; Hubbard et al., 2021; Hyland et al., 2020, 2021; Röhr et al., 2020; Twenge and Joiner, 2020; Winkler et al., 2020) which were conducted during the COVID-19 pandemic. Common explanations include factors such as health worries, loneliness due to social distancing as well as financial hardships. For example, Wang et al. (Wang et al., 2021a) showed that physical symptoms were associated with the need for health information which in turn is linked to a higher perceived impact of the pandemic. This in turn is related to, among other things, anxiety and depression. Another study from Vietnam also showed that about two out of three individuals reported household income loss due to the COVID-19 pandemic (Tran et al., 2020).
There were large cross-country differences regarding probable depression and probable anxiety in our study (e.g., between France and United Kingdom). It should be noted that remarkable differences in prevalence rates between European countries have been reported already prior to the pandemic . Factors such as intensity of restrictions during the pandemic might explain these differences. Apart from that, general explanations commonly cover cultural differences between the countries as main source for such differences (Simon et al., 2002). Besides ethnic differences in vulnerability to these mental illnesses, factors such as socioeconomic deprivation or cultural changes within countries have been discussed in the literature as possible causes (Juhasz et al., 2012). Moreover, differences in social support or locus of control between the countries could explain such findings (Steptoe et al., 2007; Steptoe and Wardle, 2001). Moreover, differences in optimism (i.e., positive outlook on life) may also partly explain such differences in probable depression and anxiety (Chang, 1996, 2001). Additionally, cultural variations in the clinical presentation of depression and anxiety may be present (Kirmayer, 2001). This means that culture-specific symptoms could contribute to underrecognition or misidentification of psychological distress (Kirmayer, 2001) – which could also explain the differences in prevalence rates between the countries. Furthermore, a recent study showed that the proportion of individuals wearing face masks was higher in Chinese individuals than in Spanish individuals based on an online sample (using a snowball sampling strategy) (Wang et al., 2021b). Similar results were found comparing the use of face masks between Chinese and Polish individuals (Wang et al., 2020a). Such precautionary measures (e.g., washing hands with soap and water) were also associated with a lower likelihood of both anxiety and depression (Wang et al., 2020b). Similar differences in precautionary measures may also exist between the European countries examined in this study. This could also explain the differences in prevalence rates. However, future research is required in this area.
Overall, it should be noted that prevalence rates across countries slightly decreased during the course of the COVID-19 pandemic in our study (November 2020 to April 2021). We assume that this general decrease may be mainly explained by the advancements in vaccinations against COVID-19 in Europe in the past few months in 2021. Given the fact that vaccination rates have been rather high in the United Kingdom compared to various other European countries by April 2021, it is quite surprising that prevalence rates only slightly decreased in the United Kingdom. Possible explanations for the high prevalence rates in the United Kingdom in January 2021 may cover high incidence rates in Winter 2020/2021, the identification of the variant of SARS-CoV-2 (B.1.1.7) in December 2020 and the partial lockdown in January 2021. Moreover, possible explanations for the slight decrease in prevalence rates in the United Kingdom from January 2021 to April 2021 include particularly the ongoing partial lockdown which was only eased in mid-April 2021.
At the same time, it should be highlighted that the prevalence rates of both probable depression and probable anxiety markedly decreased in France from November 2020 to April 2021. These are quite surprising findings (which differs from results published by the Sante Publique France (France, 2021) – most likely due to differences in assessment of probable depression and anxiety) given the fact that there were very high COVID-19 incidence rates in France in autumn 2020 resulting in a partial lockdown (including curfews in various high risk areas) which was intensified over the following months. It may be the case that adaptation effects (e.g., individuals lower their expectations) may occur or they are looking forward to the end of the pandemic. However, future research is required to clarify why these prevalence rates markedly dropped particularly in France between November 2020 and April 2021.
In line with previous research prior to the pandemic (Investigators et al., 2004a), the highest prevalence rates for both probable depression and probable anxiety have been determined among young adults in our study. Young adults may face multiple challenges (e.g., getting into working life, financial hardships, fears for the future, fulfilling multiple roles such as raising children while working full-time) which may explain their considerably high prevalence rates. Another speculative explanation may be that young individuals experienced more life-shaping events that have been negatively affected by the pandemic (such as exams and applications for a study program or job) which in turn may have an impact on probable depression and probable anxiety.
Given the fact that a recent meta-analysis identified young people most susceptible to suicide ideation during the pandemic (Dubé et al., 2021), these findings are quite alarming. However, it should be acknowledged that based on an interrupted time-series analysis (and examining various European countries) Pirkis et al. concluded that even higher depression and anxiety level during the early phase of the pandemic do “not appear to have translated into increases in suicides, at least in the countries in our study” (Pirkis et al., 2021). They noted that governments in several countries implemented approaches like extending mental health services (Pirkis et al., 2021). A recent meta-analysis also showed that the prevalence of clinically significant depressive symptoms was lower in countries wherein governments implemented stringent policies immediately (Lee et al., 2021). Thus, encouraging immediate governmental actions may be beneficial for mental health also in European countries.
Furthermore, individuals with an infection with the novel coronavirus reported high prevalence rates for both probable depression and probable anxiety in our study. Fears of health consequences (e.g. Post-COVID syndrome) and fear of infecting family, friends or other individuals as well as COVID-19 related stigma and discrimination (Bagcchi, 2020; Duan et al., 2020) could lead to depression and anxiety–which could explain our findings. Moreover, feelings of guilt (when presumably infecting others) could decrease their mental health.
In regression analysis, we found that decreases in health-related quality of life were associated with an increased likelihood of probable depression and probable anxiety. Similar findings have been made in several past studies (e.g., (Kroenke, 2003; Wong et al., 2008)). Moreover, we found that increasing income difficulties also increased the likelihood of probable depression and probable anxiety. This confirms previous research conducted prior to the pandemic (Heflin and Iceland, 2009; Kiely et al., 2015). These findings can be explained by worsening basic living conditions, nutritional shortfalls or unhealthy housing conditions associated with these income difficulties (Heflin and Iceland, 2009)–or by factors such as economic comparisons (e.g., with neighbors who are better off) which could decrease their well-being (Clark et al., 2009; Ferrer-i-Carbonell, 2005).
It should be noted that there was no significant association between the onset of infection with the novel coronavirus and changes in both probable depression and probable anxiety. This is in contrast to the “Neuro-Covid” hypothesis (Fotuhi et al., 2020). One possible explanation for our findings may be that most of these individuals had an asymptomatic or mild course of the disease. However, only a rather small proportion of individuals reported such Covid-19 infections from wave 4 to wave 6 (i.e., from not having an infection with the novel coronavirus to having a confirmed infection with the novel coronavirus over time, n = 155). Thus, these findings should be interpreted with great caution and future research is required to confirm our findings.
4.3. Strengths and limitations
This study builds upon our knowledge about the prevalence of probable depression and anxiety during the course of the COVID-19 pandemic in European countries. Longitudinal data were taken from the widely acknowledged representative ECOS. Using panel regression models can assist in mitigating the problem of unobserved heterogeneity – which is a key challenge when dealing with observational data. Several previous studies demonstrated good psychometric properties of the 4-item screening tool for depression and anxiety (PHQ-4) (Kroenke et al., 2003, 2009, 2007; Löwe et al., 2005, 2010). Kroenke et al. also stated that “because of its excellent operating characteristics, the PHQ–4 may well substitute for its parent scales (the GAD–7 and PHQ–9)” (Kroenke et al., 2009). Nevertheless, studies based on clinical interviews (e.g., Composite International Diagnostic Interview or Structured Clinical Interview for DSM-5 Disorders or neuroimaging techniques (Husain et al., 2020)) are desirable to validate our findings. Moreover, this study refers to the community-dwelling population in Europe. Upcoming studies should clarify the prevalence rates of mental disorders among individuals residing in institutionalized settings during the COVID-19 pandemic.
5. Conclusion
The magnitude of probable depression and anxiety during the COVID-19 pandemic in several European countries was highlighted. Prevalence rates for both probable depression and probable anxiety markedly differed between the countries (often with the Netherlands at the lower and United Kingdom at the upper end). Moreover, determining the factors associated with probable depression or anxiety (e.g., income difficulties or worse health-related quality of life) may assist in identifying individuals at increased risk.
Funding
This project has received funding from theGerman Research Foundation (DFG) under project number 466310,982 and the European Union's Horizon 2020 research and innovation program under the Marie Skłodowska-Curie grant agreement No 721402, the work was supported by funding under the Excellence Strategy by the German federal and state governments, as well as by the University of Hamburg, Erasmus School of Health Policy & Management and Nova School of Business and Economics Lisbon–Chair BPI | “Fundação La Caixa” on Health Economics.
Role of the funding source
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
CRediT authorship contribution statement
André Hajek: Conceptualization, Data curation, Writing – original draft. Iryna Sabat: Conceptualization, Data curation, Writing – review & editing. Sebastian Neumann-Böhme: Conceptualization, Data curation, Writing – review & editing. Jonas Schreyögg: Conceptualization, Data curation, Writing – review & editing. Pedro Pita Barros: Conceptualization, Data curation, Writing – review & editing. Tom Stargardt: Conceptualization, Data curation, Writing – review & editing. Hans-Helmut König: Conceptualization, Data curation, Writing – review & editing, Supervision.
Declaration of Competing Interest
All authors declare that they have no conflicts of interest.
Acknowledgements
None.
References
- Association A.P. American Psychiatric Association; Washington DC: 2013. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) [Google Scholar]
- Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect. Dis. 2020;20:782. doi: 10.1016/S1473-3099(20)30498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banna M.H.A., Sayeed A., Kundu S., Christopher E., Hasan M.T., Begum M.R., Kormoker T., Dola S.T.I., Hassan M.M., Chowdhury S. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: a nationwide cross-sectional study. Int. J. Environ. Health Res. 2020:1–12. doi: 10.1080/09603123.2020.1802409. [DOI] [PubMed] [Google Scholar]
- Brunoni A.R., Suen P.J.C., Bacchi P.S., Razza L.B., Klein I., dos Santos L.A., de Souza Santos I., da Costa Lane Valiengo L., Gallucci-Neto J., Moreno M.L., Pinto B.S., de Cássia Silva Félix L., de Sousa J.P., Viana M.C., Forte P.M., de Altisent Oliveira Cardoso M.C., Bittencourt M.S., Pelosof R., de Siqueira L.L., Fatori D., Bellini H., Bueno P.V.S., Passos I.C., Nunes M.A., Salum G.A., Bauermeister S., Smoller J.W., Lotufo P.A., Benseñor I.M. Prevalence and risk factors of psychiatric symptoms and diagnoses before and during the COVID-19 pandemic: findings from the ELSA-Brasil COVID-19 mental health cohort. Psychol. Med. 2021:1–12. doi: 10.1017/S0033291721001719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budimir S., Pieh C., Dale R., Probst T. Healthcare. Multidisciplinary Digital Publishing Institute; 2021. Severe Mental Health Symptoms during COVID-19: A Comparison of the United Kingdom and Austria; p. 191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron A.C., Trivedi P.K. Cambridge University Press; New York: 2005. Microeconometrics: Methods and Applications. [Google Scholar]
- Chang E.C. Cultural differences in optimism, pessimism, and coping: predictors of subsequent adjustment in Asian American and Caucasian American college students. J. Couns. Psychol. 1996;43:113. [Google Scholar]
- Chang E.C. American Psychological Association; Washington, DC, US: 2001. Cultural Influences On Optimism and pessimism: Differences in Western and Eastern construals of the self, Optimism & pessimism: Implications for theory, research, and Practice; pp. 257–280. [Google Scholar]
- Clark A.E., Westergård-Nielsen N., Kristensen N. Economic satisfaction and income rank in small neighbourhoods. J. Eur. Econ. Assoc. 2009;7:519–527. [Google Scholar]
- Czeisler M.É., Howard M.E., Robbins R., Barger L.K., Facer-Childs E.R., Rajaratnam S.M., Czeisler C.A. Early public adherence with and support for stay-at-home COVID-19 mitigation strategies despite adverse life impact: a transnational cross-sectional survey study in the United States and Australia. BMC Public Health. 2021;21:1–16. doi: 10.1186/s12889-021-10410-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Robinson E. Anxiety reported by US adults in 2019 and during the 2020 COVID-19 pandemic: population-based evidence from two nationally representative samples. J. Affect. Disord. 2021;286:296–300. doi: 10.1016/j.jad.2021.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan W., Bu H., Chen Z. COVID-19-related stigma profiles and risk factors among people who are at high risk of contagion. Soc. Sci. Med. 2020;266 doi: 10.1016/j.socscimed.2020.113425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubé J.P., Smith M.M., Sherry S.B., Hewitt P.L., Stewart S.H. Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res. 2021;301 doi: 10.1016/j.psychres.2021.113998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EuroQolGroup EuroQol–a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- Ferrer-i-Carbonell A. Income and well-being: an empirical analysis of the comparison income effect. J. Public Econ. 2005;89:997–1019. [Google Scholar]
- Fotuhi M., Mian A., Meysami S., Raji C.A. Neurobiology of COVID-19. J. Alzheimers Dis. 2020;76:3–19. doi: 10.3233/JAD-200581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- France, S.p., 2021. CoviPrev: une enquête pour suivre l’évolution des comportements et de la santé mentale pendant l'épidémie de COVID-19.
- Hajek A., König H.-.H. Prevalence and Correlates of individuals screening positive for depression and anxiety on the PHQ-4 in the german general population: findings from the nationally representative German socio-economic panel (GSOEP) Int. J. Environ. Res. Public Health. 2020;17:7865. doi: 10.3390/ijerph17217865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heflin C.M., Iceland J. Poverty, material hardship, and depression. Soc. Sci. Q. 2009;90:1051–1071. doi: 10.1111/j.1540-6237.2009.00645.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou W.K., Lee T.M.-C., Liang L., Li T.W., Liu H., Ettman C.K., Galea S. Civil unrest, COVID-19 stressors, anxiety, and depression in the acute phase of the pandemic: a population-based study in Hong Kong. Soc. Psychiatry Psychiatr. Epidemiol. 2021:1–10. doi: 10.1007/s00127-021-02037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou W.K., Lee T.M.-c., Liang L., Li T.W., Liu H., Tong H., Ben-Ezra M., Goodwin R. Psychiatric symptoms and behavioral adjustment during the COVID-19 pandemic: evidence from two population-representative cohorts. Transl. Psychiatry. 2021;11:1–11. doi: 10.1038/s41398-021-01279-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard G., den Daas C., Johnston M., Dixon D. Sociodemographic and psychological risk factors for anxiety and depression: findings from the Covid-19 health and adherence research in Scotland on mental health (CHARIS-MH) cross-sectional survey. Int. J. Behav. Med. 2021:1–13. doi: 10.1007/s12529-021-09967-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husain S.F., Yu R., Tang T.-.B., Tam W.W., Tran B., Quek T.T., Hwang S.-.H., Chang C.W., Ho C.S., Ho R.C. Validating a functional near-infrared spectroscopy diagnostic paradigm for Major Depressive Disorder. Sci. Rep. 2020;10:9740. doi: 10.1038/s41598-020-66784-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland P., Shevlin M., McBride O., Murphy J., Karatzias T., Bentall R.P., Martinez A., Vallières F. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020;142:249–256. doi: 10.1111/acps.13219. [DOI] [PubMed] [Google Scholar]
- Hyland P., Shevlin M., Murphy J., McBride O., Fox R., Bondjers K., Karatzias T., Bentall R.P., Martinez A., Vallières F. A longitudinal assessment of depression and anxiety in the Republic of Ireland before and during the COVID-19 pandemic. Psychiatry Res. 2021 doi: 10.1016/j.psychres.2021.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Investigators E.M., Alonso J., Angermeyer M., Bernert S., Bruffaerts R., Brugha T., Bryson H., de Girolamo G., de Graaf R., Demyttenaere K. 12-Month comorbidity patterns and associated factors in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr. Scand. 2004;109:28–37. doi: 10.1111/j.1600-0047.2004.00328.x. [DOI] [PubMed] [Google Scholar]
- Investigators E.M., Alonso J., Angermeyer M., Bernert S., Bruffaerts R., Brugha T., Bryson H., de Girolamo G., de Graaf R., Demyttenaere K. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr. Scand. 2004;109:21–27. doi: 10.1111/j.1600-0047.2004.00327.x. [DOI] [PubMed] [Google Scholar]
- Juhasz G., Eszlari N., Pap D., Gonda X. Cultural differences in the development and characteristics of depression. Neuropsychopharmacol. Hung. 2012;14:259–265. [PubMed] [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Koretz D., Merikangas K.R., Rush A.J., Walters E.E., Wang P.S. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kiely K.M., Leach L.S., Olesen S.C., Butterworth P. How financial hardship is associated with the onset of mental health problems over time. Soc. Psychiatry Psychiatr. Epidemiol. 2015;50:909–918. doi: 10.1007/s00127-015-1027-0. [DOI] [PubMed] [Google Scholar]
- Kirmayer L.J. Cultural variations in the clinical presentation of depression and anxiety: implications for diagnosis and treatment. J. Clin. Psychiatry. 2001;62:22–30. [PubMed] [Google Scholar]
- Kroenke K. Patients presenting with somatic complaints: epidemiology, psychiatric co-morbidity and management. Int. J. Methods Psychiatr. Res. 2003;12:34–43. doi: 10.1002/mpr.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The patient health questionnaire-2: validity of a two-item depression screener. Med. Care. 2003:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. 2009;50:613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Monahan P.O., Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Lee Y., Lui L.M.W., Chen-Li D., Liao Y., Mansur R.B., Brietzke E., Rosenblat J.D., Ho R., Rodrigues N.B., Lipsitz O., Nasri F., Cao B., Subramaniapillai M., Gill H., Lu C., McIntyre R.S. Government response moderates the mental health impact of COVID-19: a systematic review and meta-analysis of depression outcomes across countries. J. Affect. Disord. 2021;290:364–377. doi: 10.1016/j.jad.2021.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Kroenke K., Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2) J. Psychosom. Res. 2005;58:163–171. doi: 10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Löwe B., Wahl I., Rose M., Spitzer C., Glaesmer H., Wingenfeld K., Schneider A., Brähler E. A 4-item measure of depression and anxiety: validation and standardization of the patient health questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 2010;122:86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- Pirkis J., John A., Shin S., DelPozo-Banos M., Arya V., Analuisa-Aguilar P., Appleby L., Arensman E., Bantjes J., Baran A., Bertolote J.M., Borges G., Brečić P., Caine E., Castelpietra G., Chang S.S., Colchester D., Crompton D., Curkovic M., Deisenhammer E.A., Du C., Dwyer J., Erlangsen A., Faust J.S., Fortune S., Garrett A., George D., Gerstner R., Gilissen R., Gould M., Hawton K., Kanter J., Kapur N., Khan M., Kirtley O.J., Knipe D., Kolves K., Leske S., Marahatta K., Mittendorfer-Rutz E., Neznanov N., Niederkrotenthaler T., Nielsen E., Nordentoft M., Oberlerchner H., O'Connor R.C., Pearson M., Phillips M.R., Platt S., Plener P.L., Psota G., Qin P., Radeloff D., Rados C., Reif A., Reif-Leonhard C., Rozanov V., Schlang C., Schneider B., Semenova N., Sinyor M., Townsend E., Ueda M., Vijayakumar L., Webb R.T., Weerasinghe M., Zalsman G., Gunnell D., Spittal M.J. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8:579–588. doi: 10.1016/S2215-0366(21)00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riedel-Heller S., Richter D. CoViD-19 pandemic and mental health of the general public: is there a tsunami of mental disorders? Psychiatr. Prax. 2020;47:452–456. doi: 10.1055/a-1290-3469. [DOI] [PubMed] [Google Scholar]
- Röhr S., Reininghaus U., Riedel-Heller S.G. Mental wellbeing in the German old age population largely unaltered during COVID-19 lockdown: results of a representative survey. BMC Geriatr. 2020;20:1–12. doi: 10.1186/s12877-020-01889-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabat I., Neuman-Böhme S., Varghese N.E., Barros P.P., Brouwer W., van Exel J., Schreyögg J., Stargardt T. United but divided: policy responses and people's perceptions in the EU during the COVID-19 outbreak. Health Policy. 2020;124:909–918. doi: 10.1016/j.healthpol.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health. 2020;16:1–11. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon G.E., Goldberg D., Von Korff M., Üstün T. Understanding cross-national differences in depression prevalence. Psychol. Med. 2002;32:585–594. doi: 10.1017/s0033291702005457. [DOI] [PubMed] [Google Scholar]
- Steptoe A., Tsuda A., Tanaka Y. Depressive symptoms, socio-economic background, sense of control, and cultural factors in university students from 23 countries. Int. J. Behav. Med. 2007;14:97–107. doi: 10.1007/BF03004175. [DOI] [PubMed] [Google Scholar]
- Steptoe A., Wardle J. Health behaviour, risk awareness and emotional well-being in students from Eastern Europe and Western Europe. Soc. Sci. Med. 2001;53:1621–1630. doi: 10.1016/s0277-9536(00)00446-9. [DOI] [PubMed] [Google Scholar]
- Stolz E., Mayerl H., Freidl W. The impact of COVID-19 restriction measures on loneliness among older adults in Austria. Eur J Public Health. 2021;31:44–49. doi: 10.1093/eurpub/ckaa238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran B.X., Nguyen H.T., Le H.T., Latkin C.A., Pham H.Q., Vu L.G., Le X.T.T., Nguyen T.T., Pham Q.T., Ta N.T.K., Nguyen Q.T., Ho C.S.H., Ho R.C.M. Impact of COVID-19 on economic well-being and quality of life of the vietnamese during the national social distancing. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.565153. -565153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge J.M., Joiner T.E. US Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress. Anxiety. 2020;37:954–956. doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varghese N.E., Sabat I., Neumann-Böhme S., Schreyögg J., Stargardt T., Torbica A., van Exel J., Barros P.P., Brouwer W. Risk communication during COVID-19: a descriptive study on familiarity with, adherence to and trust in the WHO preventive measures. PLoS One. 2021;16 doi: 10.1371/journal.pone.0250872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Chudzicka-Czupała A., Grabowski D., Pan R., Adamus K., Wan X., Hetnał M., Tan Y., Olszewska-Guizzo A., Xu L., McIntyre R.S., Quek J., Ho R., Ho C. The association between physical and mental health and face mask use during the COVID-19 pandemic: a comparison of two countries with different views and practices. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.569981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Chudzicka-Czupała A., Tee M.L., Núñez M.I.L., Tripp C., Fardin M.A., Habib H.A., Tran B.X., Adamus K., Anlacan J., García M.E.A., Grabowski D., Hussain S., Hoang M.T., Hetnał M., Le X.T., Ma W., Pham H.Q., Reyes P.W.C., Shirazi M., Tan Y., Tee C.A., Xu L., Xu Z., Vu G.T., Zhou D., Chan N.A., Kuruchittham V., McIntyre R.S., Ho C.S.H., Ho R., Sears S.F. A chain mediation model on COVID-19 symptoms and mental health outcomes in Americans. Asians Eur. Sci. Rep. 2021;11:6481. doi: 10.1038/s41598-021-85943-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., López-Núñez M.I., Pan R., Wan X., Tan Y., Xu L., Choo F., Ho R., Ho C., Aparicio García M.E. The impact of the COVID-19 pandemic on physical and mental health in China and Spain: cross-sectional study. JMIR Form. Res. 2021:e27818. doi: 10.2196/27818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkler P., Formanek T., Mlada K., Kagstrom A., Mohrova Z., Mohr P., Csemy L. Increase in prevalence of current mental disorders in the context of COVID-19: analysis of repeated nationwide cross-sectional surveys. Epidemiol. Psychiatr. Sci. 2020;29 doi: 10.1017/S2045796020000888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong S.Y., Mercer S.W., Woo J., Leung J. The influence of multi-morbidity and self-reported socio-economic standing on the prevalence of depression in an elderly Hong Kong population. BMC Public Health. 2008;8:119. doi: 10.1186/1471-2458-8-119. [DOI] [PMC free article] [PubMed] [Google Scholar]