Abstract
Background
Parent‐infant psychotherapy (PIP) is a dyadic intervention that works with parent and infant together, with the aim of improving the parent‐infant relationship and promoting infant attachment and optimal infant development. PIP aims to achieve this by targeting the mother’s view of her infant, which may be affected by her own experiences, and linking them to her current relationship to her child, in order to improve the parent‐infant relationship directly.
Objectives
1. To assess the effectiveness of PIP in improving parental and infant mental health and the parent‐infant relationship.
2. To identify the programme components that appear to be associated with more effective outcomes and factors that modify intervention effectiveness (e.g. programme duration, programme focus).
Search methods
We searched the following electronic databases on 13 January 2014: Cochrane Central Register of Controlled Trials (CENTRAL, 2014, Issue 1), Ovid MEDLINE, EMBASE, CINAHL, PsycINFO, BIOSIS Citation Index, Science Citation Index, ERIC, and Sociological Abstracts. We also searched the metaRegister of Controlled Trials, checked reference lists, and contacted study authors and other experts.
Selection criteria
Two review authors assessed study eligibility independently. We included randomised controlled trials (RCT) and quasi‐randomised controlled trials (quasi‐RCT) that compared a PIP programme directed at parents with infants aged 24 months or less at study entry, with a control condition (i.e. waiting‐list, no treatment or treatment‐as‐usual), and used at least one standardised measure of parental or infant functioning. We also included studies that only used a second treatment group.
Data collection and analysis
We adhered to the standard methodological procedures of The Cochrane Collaboration. We standardised the treatment effect for each outcome in each study by dividing the mean difference (MD) in post‐intervention scores between the intervention and control groups by the pooled standard deviation. We presented standardised mean differences (SMDs) and 95% confidence intervals (CI) for continuous data, and risk ratios (RR) for dichotomous data. We undertook meta‐analysis using a random‐effects model.
Main results
We included eight studies comprising 846 randomised participants, of which four studies involved comparisons of PIP with control groups only. Four studies involved comparisons with another treatment group (i.e. another PIP, video‐interaction guidance, psychoeducation, counselling or cognitive behavioural therapy (CBT)), two of these studies included a control group in addition to an alternative treatment group. Samples included women with postpartum depression, anxious or insecure attachment, maltreated, and prison populations. We assessed potential bias (random sequence generation, allocation concealment, incomplete outcome data, selective reporting, blinding of participants and personnel, blinding of outcome assessment, and other bias). Four studies were at low risk of bias in four or more domains. Four studies were at high risk of bias for allocation concealment, and no study blinded participants or personnel to the intervention. Five studies did not provide adequate information for assessment of risk of bias in at least one domain (rated as unclear).
Six studies contributed data to the PIP versus control comparisons producing 19 meta‐analyses of outcomes measured at post‐intervention or follow‐up, or both, for the primary outcomes of parental depression (both dichotomous and continuous data); measures of parent‐child interaction (i.e. maternal sensitivity, child involvement and parent engagement; infant attachment category (secure, avoidant, disorganised, resistant); attachment change (insecure to secure, stable secure, secure to insecure, stable insecure); infant behaviour and secondary outcomes (e.g. infant cognitive development). The results favoured neither PIP nor control for incidence of parental depression (RR 0.74, 95% CI 0.52 to 1.04, 3 studies, 278 participants, low quality evidence) or parent‐reported levels of depression (SMD ‐0.22, 95% CI ‐0.46 to 0.02, 4 studies, 356 participants, low quality evidence). There were improvements favouring PIP in the proportion of infants securely attached at post‐intervention (RR 8.93, 95% CI 1.25 to 63.70, 2 studies, 168 participants, very low quality evidence); a reduction in the number of infants with an avoidant attachment style at post‐intervention (RR 0.48, 95% CI 0.24 to 0.95, 2 studies, 168 participants, low quality evidence); fewer infants with disorganised attachment at post‐intervention (RR 0.32, 95% CI 0.17 to 0.58, 2 studies, 168 participants, low quality evidence); and an increase in the proportion of infants moving from insecure to secure attachment at post‐intervention (RR 11.45, 95% CI 3.11 to 42.08, 2 studies, 168 participants, low quality evidence). There were no differences between PIP and control in any of the meta‐analyses for the remaining primary outcomes (i.e. adverse effects), or secondary outcomes.
Four studies contributed data at post‐intervention or follow‐up to the PIP versus alternative treatment analyses producing 15 meta‐analyses measuring parent mental health (depression); parent‐infant interaction (maternal sensitivity); infant attachment category (secure, avoidant, resistant, disorganised) and attachment change (insecure to secure, stable secure, secure to insecure, stable insecure); infant behaviour and infant cognitive development. None of the remaining meta‐analyses of PIP versus alternative treatment for primary outcomes (i.e. adverse effects), or secondary outcomes showed differences in outcome or any adverse changes.
We used the Grades of Recommendation, Assessment, Development and Evaluation Working Group (GRADE) approach to rate the overall quality of the evidence. For all comparisons, we rated the evidence as low or very low quality for parental depression and secure or disorganised infant attachment. Where we downgraded the evidence, it was because there was risk of bias in the study design or execution of the trial. The included studies also involved relatively few participants and wide CI values (imprecision), and, in some cases, we detected clinical and statistical heterogeneity (inconsistency). Lower quality evidence resulted in lower confidence in the estimate of effect for those outcomes.
Authors' conclusions
Although the findings of the current review suggest that PIP is a promising model in terms of improving infant attachment security in high‐risk families, there were no significant differences compared with no treatment or treatment‐as‐usual for other parent‐based or relationship‐based outcomes, and no evidence that PIP is more effective than other methods of working with parents and infants. Further rigorous research is needed to establish the impact of PIP on potentially important mediating factors such as parental mental health, reflective functioning, and parent‐infant interaction.
Keywords: Female, Humans, Infant, Mental Health, Parent‐Child Relations, Depression, Depression/diagnosis, Depression/therapy, Family Therapy, Family Therapy/methods, Father‐Child Relations, Mental Disorders, Mental Disorders/therapy, Mother‐Child Relations, Mother‐Child Relations/psychology, Object Attachment, Randomized Controlled Trials as Topic, Spouse Abuse
Plain language summary
Parent‐infant psychotherapy for improving parent and infant well‐being
Background
Parent‐infant psychotherapy (PIP) is intended to address problems in the parent‐infant relationship, and problems such as excessive crying and sleeping/eating difficulties. A parent‐infant psychotherapist works directly with the parent and infant in the home or clinic, to identify unconscious patterns of relating and behaving, and influences from the past that are impeding the parent‐infant relationship. Parents may be referred to this service (e.g. by a general practitioner in the UK) or may self refer to privately run services. The intervention is delivered to individual dyads but can also be delivered to small groups of parents and infants.
Review question
This review examined whether PIP is effective in improving the parent‐infant relationship, or other aspects of parent or infant functioning, and to identify the programme components that appear to be associated with more effective outcomes and factors that modify intervention effectiveness (e.g. programme duration, programme focus).
Study characteristics
We searched electronic databases and identified randomised controlled trials (RCTs, where participants are randomly allocated to one of two or more treatment groups) and one cluster randomised trial (where prisons rather than participants were used as the unit of randomisation), in which participants had been allocated to a receive PIP versus a control group, and which reported results using at least one standard measure of outcome (i.e. an instrument which has been tested to ensure that it reliably measures the outcome under investigation).
Evidence is current to 13 January 2014.
We identified eight studies with 846 randomised participants comparing either PIP with a no‐treatment control group (four studies) or comparing PIP with other types of treatment (four studies).
Key results
The studies comparing PIP with a no‐treatment control group contributed data to 19 meta‐analyses of the primary outcomes of parental mental health (depression), parent‐infant interaction outcomes of maternal sensitivity (i.e. the extent to which the caregiver responds in a timely and attuned manner), child involvement and parent positive engagement, and infant outcomes of infant attachment category (the infant's ability to seek and maintain closeness to primary caregiver ‐ infant attachment is classified as follows: 'secure' infant attachment is a positive outcome, which indicates that the infant is able to be comforted when distressed and is able to use the parent as a secure base from which to explore the environment. Infants who are insecurely attached are either 'avoidant' (i.e. appear not to need comforting when they are distressed and attempt to manage the distress themselves); or 'resistant' (i.e. unable to be comforted when distressed and alternate between resistance and anger). Children who are defined as ‘disorganised’ are unable to produce a coherent strategy in the face of distress and produce behaviour that is a mixture of approach and avoidance to the caregiver); and the secondary outcomes of infant behaviour and infant cognitive development (i.e. intellectual development, including thinking, problem solving and communicating).
In our analyses, parents who received PIP were more likely to have an infant who was securely emotionally attached to the parent after the intervention; this a favourable outcome but there is very low quality evidence to support it.
The studies comparing PIP with another model of treatment contributed data to 15 meta‐analysis assessments of primary outcomes, including parental mental health, parent‐infant interaction (maternal sensitivity); infant attachment and infant behaviour, or secondary infant outcomes such as infant cognitive development. None of these comparisons showed differences that favoured either PIP or the alternative intervention.
None of the comparisons of PIP with either a control or comparison treatment group showed adverse changes for any outcome.
We conclude that although PIP appears to be a promising method of improving infant attachment security, there is no evidence about its benefits in terms of other outcomes, and no evidence to show that it is more effective than other types of treatment for parents and infants. Further research is needed.
Quality of the evidence
The included studies were unclear about important quality criteria, had limitations in terms of their design or methods, or we judged that there was risk of bias in the trial. This lower quality evidence gives us less confidence in the observed effects.
Summary of findings
Summary of findings for the main comparison. Parent‐infant psychotherapy versus control for improving parental and infant mental health: parent mental health and infant attachment.
| Comparison 1: parent‐infant psychotherapy intervention versus control: parental and infant mental health | ||||||
| Patient or population: participants with improving parental and infant mental health Settings: research clinic Intervention: parent‐infant psychotherapy intervention versus control | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Parent‐infant psychotherapy | |||||
| Parent mental health meta‐analysis: depression (dichotomous data) ‐ post‐intervention Number depressed | Study population | RR 0.74 (0.52 to 1.04) | 278 (3 studies) | ⊕⊕⊝⊝ low1,2 | There was no clear evidence of a difference between PIP and control | |
| 468 per 1000 | 346 per 1000 (243 to 487) | |||||
| Moderate | ||||||
| 481 per 1000 | 356 per 1000 (250 to 500) | |||||
| Parent mental health meta‐analysis: depression (continuous data) ‐ post‐intervention Validated assessment scales for depression, lower scores are less depressed | The mean depression scores in the control group ranged from 7.99 to 15.3 | The mean depression in the intervention groups was
0.22 standard deviations lower
(0.46 lower to 0.02 higher). The mean depression score in the intervention group was 1.1 lower (2.2 lower to 0.1 higher) |
‐ | 356 (4 studies) | ⊕⊕⊝⊝ low1,2 | Scores estimated using an SMD: SMD ‐0.22, 95% CI ‐0.46 to 0.02. There was no clear evidence of a difference between PIP and control |
| Infant attachment categories meta‐analysis: post‐intervention ‐ attachment category (SSP) secure Ainsworth Strange Situation | Study population | RR 8.93 (1.25 to 63.7) | 168 (2 studies) | ⊕⊝⊝⊝ very low1,2,3 | Favours PIP (more infants secure in PIP) | |
| 93 per 1000 | 827 per 1000 (116 to 1000) | |||||
| Moderate | ||||||
| 93 per 1000 | 830 per 1000 (116 to 1000) | |||||
| Infant attachment categories meta‐analysis: post‐intervention ‐ attachment category (SSP) disorganised Ainsworth Strange Situation | Study population | RR 0.32 (0.17 to 0.58) | 168 (2 studies) | ⊕⊕⊝⊝ low1,2 | Favours PIP (fewer infants disorganised in PIP) | |
| 593 per 1000 | 190 per 1000 (101 to 344) | |||||
| Moderate | ||||||
| 593 per 1000 | 190 per 1000 (101 to 344) | |||||
| Infant attachment categories meta‐analysis: follow‐up ‐ attachment category (SSP) secure Ainsworth Strange Situation | Study population | RR 3.3 (1.82 to 6) | 129 (2 studies) | ⊕⊕⊝⊝ low1,2 | Favours PIP (more infants secure in PIP) | |
| 146 per 1000 | 481 per 1000 (265 to 875) | |||||
| Moderate | ||||||
| 146 per 1000 | 482 per 1000 (266 to 876) | |||||
| Infant attachment categories meta‐analysis: follow‐up ‐ attachment category (SSP) disorganised Ainsworth Strange Situation | Study population | RR 0.8 (0.29 to 2.19) | 129 (2 studies) | ⊕⊝⊝⊝ very low1,2,3 | There was no clear evidence of a difference between PIP and control | |
| 344 per 1000 | 275 per 1000 (100 to 753) | |||||
| Moderate | ||||||
| 341 per 1000 | 273 per 1000 (99 to 747) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; PIP: parent‐infant psychotherapy; RR: risk ratio; SMD: standardised mean difference; SSP: Strange Situation Procedure. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Risk of bias due to study designs, randomisation and allocation concealment; and not possible to blind participants or personnel. 2 Relatively few participants and wide confidence intervals. 3 Moderate to high levels of statistical heterogeneity.
Summary of findings 2. Parent‐infant psychotherapy versus other (psychoeducational) parenting intervention: parent mental health and infant attachment.
| Comparison 2: parent‐infant psychotherapy versus other (psychoeducational) parenting intervention: parental and infant mental health | ||||||
| Patient or population: participants with improving parental and infant mental health Settings: research clinic Intervention: parent‐infant psychotherapy versus other (psychoeducational) parenting intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control (other (psychoeducational) parenting intervention) | Parent‐infant psychotherapy | |||||
| Parent mental health meta‐analysis: depression continuous data ‐ post‐intervention Validated assessment scales for depression, lower scores are less depressed | The mean depression scores in the non‐PIP group ranged from 6.9 to 9.57 | The mean depression scores in the intervention groups were
0.23 standard deviations higher
(0.49 lower to 0.95 higher). The mean depression score in the intervention group was 1.2 higher (2.6 lower to 5.1 higher) (Cohen 1999b used as a representative study) |
‐ | 172 (2 studies) | ⊕⊝⊝⊝ very low1,2,3 | Scores estimated using an SMD: SMD 0.23, 95% CI ‐0.49 to 0.95. There was no clear evidence of a difference between PIP and control |
| Parent mental health meta‐analysis: depression continuous data ‐ follow‐up (up to 18 months) Validated assessment scales for depression, lower scores are less depressed | The mean depression scores in the non‐PIP group ranged from 6.3 to 9.26 | The mean depression scores in the intervention groups were
0.13 standard deviations higher
(0.23 lower to 0.5 higher). The mean depression score in the intervention group was 0.70 higher (1.24 lower to higher) (Cohen 1999b used as a representative study) |
‐ | 160 (2 studies) | ⊕⊕⊝⊝ low1,2 | Scores estimated using an SMD: SMD 0.13, 95% CI ‐0.23 to 0.5. There was no clear evidence of a difference between PIP and control |
| Infant attachment categories meta‐analysis: post‐intervention ‐ attachment category secure Ainsworth Strange Situation | Study population | RR 0.83 (0.32 to 2.13) | 102 (2 studies) | ⊕⊝⊝⊝ very low1,2,3 | No statistically significant difference between groups | |
| 375 per 1000 | 311 per 1000 (120 to 799) | |||||
| Moderate | ||||||
| 405 per 1000 | 336 per 1000 (130 to 863) | |||||
| Infant attachment categories meta‐analysis: post‐intervention ‐ attachment category disorganised Ainsworth Strange Situation | Study population | RR 0.79 (0.34 to 1.82) | 36 (1 study) | ⊕⊕⊝⊝ low1,2 | There was no clear evidence of a difference between PIP and control | |
| 455 per 1000 | 359 per 1000 (155 to 827) | |||||
| Moderate | ||||||
| 455 per 1000 | 359 per 1000 (155 to 828) | |||||
| Infant attachment categories meta‐analysis: follow‐up ‐ attachment category secure Ainsworth Strange Situation | Study population | RR 1.61 (0.83 to 3.12) | 136 (2 studies) | ⊕⊝⊝⊝ very low1,2,3 | There was no clear evidence of a difference between PIP and alternative intervention | |
| 363 per 1000 | 584 per 1000 (301 to 1000) | |||||
| Moderate | ||||||
| 314 per 1000 | 506 per 1000 (261 to 980) | |||||
|
Infant attachment categories meta‐analysis: follow‐up ‐ attachment category disorganised Ainsworth Strange Situation |
Study population | RR 0.82 (0.3 to 2.22) | 136 (2 studies) | ⊕⊝⊝⊝ very low1,2,3 | There was no clear evidence of a difference between PIP and control | |
| 304 per 1000 | 249 per 1000 (91 to 675) | |||||
| Moderate | ||||||
| 408 per 1000 | 335 per 1000 (122 to 906) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; PIP: parent‐infant psychotherapy; RR: risk ratio; SMD: standardised mean difference. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Risk of bias due to study designs, including randomisation and allocation concealment; and not possible to blind participants or personnel. 2 Relatively few participants and wide confidence intervals. 3 Moderate to high levels of statistical heterogeneity.
Background
Description of the condition
Infant regulatory disturbances, such as excessive crying, feeding or sleeping difficulties, and bonding/attachment problems represent the main reasons for referral to infant mental health clinics (Keren 2001). The Copenhagen Child Cohort Study (6090 infants) found a population prevalence of such regulatory problems (including emotional and behavioural, eating and sleeping disorders) in children aged 1.5 years in the region of 18% (Skovgaard 2008; Skovgaard 2010). Some regulatory disturbances are stable over time with as many as 49.9% of infants and toddlers (aged 12 to 40 months) showing a continuity of emotional and behavioural problems one year after initial presentation (Briggs‐Gowan 2006). Problems of this nature are also significant predictors of longer‐term difficulties. For example, infant regulatory problems have a strong association with delays in motor, language and cognitive development, and continuing parent‐child relational problems (DeGangi 2000a; DeGangi 2000b). Difficult temperament, non‐compliance and aggression in infancy and toddlerhood (aged one to three years) are associated with internalising and externalising psychiatric disorders at five years of age (Keenan 1998). Insecure and disorganised attachment in infancy is also associated with poorer outcomes in childhood across a range of domains such as emotional, social and behavioural adjustment, scholastic achievement and peer‐rated social status (Berlin 2008; Granot 2001; Sroufe 2005a; Sroufe 2005b), particularly in the case of disorganised attachment, which is a significant predictor of significant later psychopathology (Green 2002).
Infant regulatory and attachment problems can best be understood in a relational context, and disturbances to the parent‐child relationship and parental psychosocial adversity are significant risk factors for infant emotional, behavioural, eating and sleeping disorders (Skovgaard 2008; Skovgaard 2010). Early research in the field of infant mental health and developmental psychology has highlighted the significant role that the infant's primary carer plays in regulating the infant (Beebe 2010; Sroufe 1997; Tronick 1989; Tronick 1997), but one systematic review found only modest correlations between 'maternal sensitivity' and infant attachment security (De Wolff 1997), prompting a search for more specific predictive factors. Research has focused on the specific nature or quality of the attunement or contingency between parent and infant (Beebe 2010), and the parent's capacity for what has been termed 'maternal mind‐mindedness' (Meins 2001) or 'reflective function' (Slade 2001).
Beebe developed the term 'mid‐range contingency' to refer to interaction in which both the parent's self regulation and the interactive regulation between parent and infant is in the mid‐range (Beebe 1988). Parents with low interactive tracking (e.g. resulting from withdrawal due to postnatal depression) are more likely to have infants who are insecurely attached, as are parents who have high interactive tracking (i.e. due to excessive vigilance resulting from anxiety) (Beebe 2010).
Parental reflective function refers to the parent's capacity to understand the infant's behaviour in terms of internal feeling states, and is strongly associated with maternal parenting behaviours, such as flexibility and responsiveness, while low maternal reflective function is associated with emotionally unresponsive maternal behaviours (withdrawal, hostility, intrusiveness) (Kelly 2005; Slade 2001; Slade 2005). Maternal reflective function is also associated with more optimal infant outcomes such as a greater use of the mother as a 'secure base' (i.e. the infant can be comforted by the primary carer when distressed, and able to explore the world in the presence of the carer when not distressed) (Kelly 2005). There is also a significant association between parental 'mind‐mindedness' (the parent's capacity to interpret what their child is thinking and feeling accurately) and later development, including attachment security at 12 months (Meins 2001).
Research has also highlighted a number of 'atypical' parenting behaviours that can be present during the postnatal period, including affective communication errors (e.g. mother positive while infant distressed), disorientation (frightened expression or sudden complete loss of affect) and negative‐intrusive behaviours (mocking or pulling infant's body) (Lyons‐Ruth 2005). A meta‐analysis of 12 studies found a strong association between disorganised attachment at 12 to 18 months of age and parenting behaviours characterised as 'anomalous' (i.e. frightening, threatening, looming), dissociative (haunted voice, deferential/timid) or disrupted (failure to repair, lack of response, insensitive/communication error) (Madigan 2006). These atypical parenting practices were identified in parents described as 'unresolved' with regard to previous trauma (Cicchetti 2006a; Cicchetti 2010; Jacobvitz 1997). However, disturbances to the mother‐infant relationship are common and are associated with a range of maternal problems, including postnatal depression (Murray 2003; Timmer 2011; Toth 2006), personality disorder (Crandell 2003; Newman 2008), psychotic disorders (Chaffin 1996), substance misuse (Suchman 2005; Tronick 2005), and domestic violence (Lyons‐Ruth 2003; Lyons‐Ruth 2005).
Description of the intervention
Since the mid‐1990s, a range of interventions (e.g. home visiting and parenting programmes) have been developed to address developmental problems in the infant, and problems in the parent‐infant relationship, with a view to promoting optimal infant development. These have mostly targeted the parent and used a range of techniques in their delivery (discussion, role play, watching video vignettes, and homework), with the aim of changing parenting behaviours and attitudes. Parent‐infant psychotherapy (PIP) in contrast is a dyadic intervention (or triadic if both parents are involved) that involves targeting the parent‐infant relationship (i.e. it is delivered to parent and infant together). A parent‐infant psychotherapist works by listening and observing the interaction, identifying the concerns and worries, and helping the parent observe and find different ways to relate to their baby. This work may take place in the home, clinic or hospital setting, and aims to address a wide range of problems that can arise during the antenatal and postnatal periods. The intervention is usually delivered to individual dyads but can also be delivered to small groups of dyads.
PIP focuses on improving the parent‐infant relationship and infant attachment security by targeting parental internal working models (i.e. representational world ‐ see below) and by working directly with the parent‐infant relationship in the room. The approach is essentially psychodynamic in that it involves identifying unconscious patterns of relating, and the earliest approach, developed by Selma Fraiberg (Fraiberg 1980), focused primarily on the mother's 'representational' world ('representation‐focused' approach) or the way in which the mother's current view of her infant was affected by interfering representations from her own history. The aim of such therapy was to help the mother to recognise the 'ghosts in the nursery' (i.e. the unremembered influences from her own past) and to link them to her current functioning, in order to improve the parent‐infant relationship directly, thereby facilitating new paths for growth and development for both mother and infant (Cramer 1988). Fraiberg's model has been further developed and evaluated by others (e.g. Lieberman 1991; Toth 2006), and representational and behavioural approaches have been combined (Cohen 1999a). For example, 'Watch, Wait and Wonder' (WWW) is an 'infant‐led' PIP that involves the mother spending time observing her infant's self initiated activity, accepting the infant's spontaneous and undirected behaviour, and being physically accessible to the infant (behavioural component). The mother then discusses her experiences of the infant‐led play with the therapist with a view to examining the mother's internal working models of herself in relation to her infant (representational component) (Cohen 1999a). PIP may also work with the father or other primary carer, or with two parents together.
The duration of the intervention depends on the presenting problems but typically ranges from five to 20 weeks, usually involving weekly sessions. Parents may be referred to this service by a clinician (e.g. general practitioner (GP) or health visitor in the UK) or may self‐refer to privately run services. PIP services typically target infants less than two years of age at the time of referral. This reflects the importance of the first two years of life in terms of children's later development (as described above).
How the intervention might work
The logic model underpinning representational forms of PIP is that changes to the mother's representations (internal working models) will improve the mother's sensitivity and behaviour towards her infant (e.g. Lieberman 1991), thereby reducing distorted projections and making it possible for her to see the infant as someone with a 'mind of their own'. Maternal sensitivity is strongly associated with more optimal parent‐infant interaction, which, in turn, is associated with infant attachment security (De Wolff 1997). Secure attachment is associated with resilience and optimal social functioning (Sroufe 2005a; Sroufe 2005b), while both insecure (Berlin 2008; Granot 2001; Lecce 2008; Sroufe 2005a; Sroufe 2005b), and disorganised attachment are associated with a range of compromised outcomes (Green 2002; Lyons‐Ruth 2005). The addition of behavioural components provides opportunities for parent and infant to interact, which then become the focus of exploratory discussions between therapist and parent, aimed once again at changing maternal representations about the infant (Cohen 1999a). The empathic relationship between the therapist and parent also plays a key role in helping parents to revise their internal working models (Toth 2006).
Why it is important to do this review
Parent‐infant interaction is a significant factor in infant mental health (Fonagy 2002), and problems with the parent‐infant relationship are common (Keren 2001). Government policy internationally is increasingly emphasising the importance of early intervention and the need to develop empirically derived models that can support vulnerable parents and their children, and this reflects an increased recognition at policy level that both health and social inequalities have their origins in early parent‐infant interaction (Field 2010), and that the social gradient in children's access to positive early experiences needs to be addressed (Marmot 2010).
There is a growing body of evidence pointing to the effectiveness of PIP in terms of improving both parental functioning (Cohen 1999a; Cohen 2002), and fostering secure attachment relationships in young children (Toth 2006), and there is some evidence to suggest that different forms of the therapy may be differentially effective for parents with different types of attachment insecurity (Bakermans‐Kranenburg 1998).
However, to date, there has been only one 'thematic' summary of the evidence about the effectiveness of PIP (Kennedy 2007), which did not involve a systematic search for evidence. As such, there is a need for a systematic review to identify whether this unique method of working has benefits for parents (both mothers and fathers) and infants, and whether the outcome is affected by the duration or content of the intervention.
Objectives
To assess the effectiveness of PIP in improving parental and infant mental health and the parent‐infant relationship.
To identify the programme components that appear to be associated with more effective outcomes and factors that modify intervention effectiveness (e.g. programme duration, programme focus).
Methods
Criteria for considering studies for this review
Types of studies
We pre‐specified our methods for this review in the protocol (Barlow 2013).
We included randomised controlled trials (RCTs) and quasi‐randomised controlled trials (quasi‐RCTs) in which participants had been randomly allocated to an experimental or a control group, the latter being a waiting‐list, no treatment, treatment‐as‐usual (normal service provision) or a placebo control group. We defined quasi‐RCTs as trials where allocation was done on the basis of a pseudo‐random sequence, for example, odd or even hospital number, date of birth or alternation (Higgins 2011). We also included studies comparing two different therapeutic modalities (i.e. without a control group).
Types of participants
We included studies involving parent‐infant dyads in which the parent was experiencing mental health problems, domestic abuse or substance dependency, with or without the infant showing signs of attachment or dysregulation problems, or both attachment and dysregulation problems. We included all infants irrespective of the presence of problems such as low birthweight, prematurity or disabilities. We included studies targeting infants and toddlers in which the mean age of the infant participants was 24 months or less at the point of referral. We included studies targeting all parents (i.e. including fathers, birth parents, adoptive and kinship parents, but not foster parents).
Types of interventions
We included studies that had evaluated the effectiveness of PIP programmes in which the intervention met all of the following criteria:
underpinned by a psychodynamic model that involved making unconscious patterns of relating by targeting the parent‐therapist transference; parental internal working models or representations (i.e. the way in which the mother's current view of her infant was affected by interfering representations or unremembered influences from her own history, and to link them to her current functioning, in order to improve the parent‐infant relationship directly, thereby facilitating new paths for growth and development for both mother and infant);
delivered jointly to both parent and infant with a focus on the parent‐infant relationship/interaction and aimed primarily at improving infant attachment security, socio‐emotional functioning, or both, via the parent‐infant relationship/interaction;
delivered by a parent‐infant psychotherapist/specialist on a dyadic basis or to dyads in groups, in any setting (clinic, hospital or home), over any period of time.
We also included studies of PIPs that used additional components (i.e. provided they still met the core inclusion criteria). We excluded studies of interventions that were delivered to the parent or parents alone (e.g. interpersonal psychotherapy (IPT) or that were dyadic but primarily psychoeducational or based on other therapeutic models (e.g. behavioural or cognitive behavioural therapy (CBT)). We excluded studies of stand‐alone video‐interaction guidance interventions but not studies in which video feedback had been incorporated into a PIP that met the above criteria.
Types of outcome measures
We extracted data for the following outcomes at both post‐intervention and follow‐up, provided they had been measured using a standardised parent‐report or independent observation of the type listed as examples for each outcome below.
Primary outcomes
Parent outcomes
Parental mental health including, for example, depression* (e.g. Beck Depression Inventory (BDI) (Beck 1961); anxiety (e.g. Beck Anxiety Inventory (BAI) (Beck 1988); parenting stress (e.g. Parenting Stress Index (PSI) (Abidin 1983).
Parent‐infant relationship outcomes
Parent‐infant interaction including, for example, Child‐Adult Relationship Experimental‐Index (CARE‐Index) (Crittenden 2001), Emotional Availability Scales (EAS) (Biringen 1993), Parent‐Child Early Relational Assessment (PC‐ERA) (Clark 1985), Dyadic Parent‐Child Interaction Coding System (DPICS) (Robinson 1981), Nursing Child Assessment of Feeding Scale (NCAFS) (Barnard 1978a), or the Nursing Child Assessment Teaching Scale (NCATS) (Barnard 1978b); Maternal Sensitivity Scale (MSS) (Ainsworth 1974), Atypical Maternal Behavior Instrument for Assessment and Classification (AMBIANCE) (Bronfman 1999), or Frightened/Frightening (FR) Coding System (Main 1992).
Infant outcomes
Infant emotional well‐being including, for example, infant attachment* measures such as the Strange Situation Procedure (SSP) (Ainsworth 1971), Preschool Measure of Attachment (PMA) (Crittenden 1992), or other measures of emotional and behavioural adjustment such as the Infant and Toddler Social and Emotional Assessment (ITSEA) (Carter 2000), Eyberg Child Behaviour Inventory (ECBI) (Eyberg 1978), Behaviour Screening Questionnaire (BSQ) (Richman 1971), and the Child Behaviour Questionnaire (CBQ) (Rutter 1970).
Adverse effects
Adverse effects of interventions were included as an outcome, including a worsening of outcome on any of the included measures.
Secondary outcomes
Parent outcomes
Parental reflective function including, for example, Parent Development Interview (PDI) (Slade 2004).
Infant outcomes
Infant stress including, for example, salivary or urinary cortisol measured in standardised units such as micrograms per decilitre (μg/dL) or nanograms per millilitre (ng/mL).
Infant development including, for example, social, emotional, cognitive and motor development using the Bayley Scales (Bayley 1969).
*For the comparison of PIP versus control, we used the primary outcomes of parental depression at post‐intervention and infant attachment at post‐intervention and follow‐up to complete Table 1. For the comparison of PIP versus alternate intervention in Table 2, we used the primary outcomes of parental depression at post‐intervention and follow‐up, and for infant attachment, we used outcomes from post‐intervention and follow‐up.
Search methods for identification of studies
Electronic searches
We searched the following databases on 13 January 2014 without restrictions on language, date or publication status. We applied RCT filters where appropriate (see Appendix 1).
Cochrane Central Register of Controlled Trials (CENTRAL) 2014 ( Issue 1), part of The Cochrane Library.
Ovid MEDLINE, 1950 to 10 January 2014.
EMBASE (Ovid), 1980 to January week 1 2014.
CINAHL (EBSCO), 1982 to current.
PsycINFO (Ovid), 1806 to January week 1 2014.
BIOSIS Citation Index (ISI), all available years.
SSCI (Web of Science), 1970 to current.
ERIC (ProQuest), 1966 to current.
Sociological Abstracts (ProQuest), 1952 to current.
We also searched the metaRegister of Controlled Trials (mRCT) on 20 January 2014 (Appendix 2).
Searching other resources
We contacted authors and experts in the field to identify unpublished studies. We handsearched reference lists of articles identified through database searches for further relevant studies. We also examined bibliographies of systematic and non‐systematic review articles to identify relevant studies.
Data collection and analysis
Selection of studies
Two review authors (CB and JB) screened the titles and abstracts of studies identified by the searches to assess whether they met the inclusion criteria and independently assessed full copies of papers that appeared to meet the inclusion criteria. We resolved any uncertainties by discussion with a third review author (NM).
Data extraction and management
Two review authors (CB and SL) independently extracted data using an identical data extraction form and entered the data into Review Manager 5 software (RevMan 2012). Where data were not available in the published trial reports, we contacted study investigators to supply missing information. We extracted information regarding: study design, measurement of delivery fidelity, participant characteristics, primary and secondary outcome measures, and data.
Assessment of risk of bias in included studies
Two review authors (CB, SL) carried out 'Risk of bias' assessments using The Cochrane Collaboration 'Risk of bias' assessment tool (Higgins 2011). We resolved differences by consultation with a third review author (JB or NM). We assessed each trial in the following areas: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective reporting and other sources of bias, including whether there was any assessment of the distribution of confounders. Where there was insufficient information in the trial report to make a judgement, we contacted trial investigators for further information.
We assessed all domains as being at low, high or unclear (uncertain) risk of bias.
We used 'Risk of bias' assessments in the synthesis of data, to interpret findings for specific outcomes and to comment on the quality of the evidence.
Sequence generation
We assessed the method used to generate the allocation sequence to identify whether it had produced comparable groups.
Allocation concealment
We assessed the method used to conceal allocation sequence to assess its adequacy in terms of whether the intervention schedules could have been foreseen in advance of, or during, recruitment.
Blinding
We assessed whether any steps were taken to blind participants and personnel, and to blind outcome assessors to the intervention that participants received.
Incomplete outcome data
We assessed whether incomplete data was dealt with adequately, and how data on attrition and exclusions were reported in comparison with the total number of participants randomised. Where studies did not report intention‐to‐treat (ITT) analyses, we attempted to obtain missing data by contacting the study authors.
Selective outcome reporting
We assessed whether any attempt had been made to reduce the possibility of selective outcome reporting.
Other sources of bias
We examined baseline or pre‐treatment means, where available, to assess whether there was any imbalance in terms of participant characteristics that were strongly related to outcome measures and that could cause bias in intervention effect estimates (Higgins 2011, Chapter 8.14.1.2).
We assessed whether the study was free of other problems that could have put it at a high risk of bias (e.g. contamination).
Measures of treatment effect
Dichotomous outcome data
For dichotomous endpoint measures, we present the number of parents or infants who showed an improvement as a proportion of the total number of parents/infants treated. We calculated risk ratios (RR) by dividing the risk in one group with the risk in the other group, and present these with 95% confidence intervals (CI) and standard deviations.
Not all dichotomous measures indexed relative risks of improvement over time and, for some measures, we provided the relative risk of a positive state (e.g. secure attachment) at post‐intervention.
Continuous outcome data
For the meta‐analyses of continuous outcomes, we estimated the mean differences (MDs) between groups. In the case of continuous outcome measures, where data were reported on different scales, we analysed data using the standardised mean difference (SMD), calculated by dividing the MD in post‐intervention scores between the intervention and control groups by the standard deviation. We presented the SMDs and 95% CIs for all meta‐analyses and individual outcomes from individual studies (i.e. where no meta‐analysis was undertaken).
Where the above data were not available, we present significance levels reported in the paper.
Unit of analysis issues
Cluster‐randomised trials
The randomisation of clusters can result in an overestimate of the precision of the results (with a higher risk of a Type I error) where their use has not been compensated for in the analysis. One study employed cluster‐randomisation (Sleed 2013a, mother and baby units in prisons). We explored the impact of the inclusion of data from this study in the meta‐analyses by imputing a set of intraclass correlation coefficients (ICC) (0.2, 0.4, 0.6, 0.8) (i.e. we were unable to identify external evidence for a reasonable ICC and for this reason, we selected multiple values for ICCs). We calculated the inflated standard errors that accounted for clustering by multiplying the original standard errors with the square root of the associated design effects (see Higgins 2011, Chapter 16.3.6).
Studies with multiple treatment groups
For studies where there was more than one active intervention and only one control group, we selected the intervention that most closely matched our inclusion criteria and excluded the others (see Higgins 2011, Chapter 16.5.4).
Dealing with missing data
We assessed missing data and attrition for each included study and reported them in the 'Risk of bias' tables. Where appropriate, we contacted authors to supply data missing from included studies. Where missing data could not be provided, we have reported this and the available data only (i.e. we used no imputation).
Assessment of heterogeneity
We assessed clinical heterogeneity by examining the extent of between‐trial differences, including methods, populations, interventions, whether the delivery of the intervention was monitored (to ascertain fidelity), and outcomes.
We assessed statistical heterogeneity using the I2 statistic. The importance of the observed I2 value is dependent on the magnitude and direction of effects and strength of evidence for heterogeneity (e.g. P value from the Chi2 test, or a CI for I2 statistic) (Higgins 2002), and we have interpreted an I2 greater than 50% as evidence of substantial heterogeneity.
Where we performed a Chi2 test of heterogeneity, we interpreted a significance level less than 0.10 as evidence of heterogeneity. We carried out the tau2 estimates for each meta‐analysis and presented Chi2 values, P values, tau2 statistic and I2 statistic.
Assessment of reporting biases
Due to the small number of included studies, we were unable to assess reporting biases. For more information on how we will assess reporting bias in future updates of this review, see Barlow 2013 and Appendix 3.
Data synthesis
We undertook meta‐analysis where there was sufficient clinical homogeneity in the intervention delivered, the characteristics of the study participants (e.g. age or the definition of 'at risk' participants), and the outcome measures. We made the decision about combining data post hoc based on the categories of interventions, participants, and outcomes identified in the reviewed literature. We combined data using a random‐effects model. We calculated overall effects using inverse variance methods.
All analyses included all participants in the treatment groups to which they were allocated, whenever possible.
While we attempted to combine data where at all possible, there were some circumstances where it was not possible; for example, where some studies reported the same outcome using different formats (e.g. dichotomous and continuous), we have carried out two separate analyses. For single outcomes, we presented the individual effect sizes and 95% CIs.
Subgroup analysis and investigation of heterogeneity
We explored possible reasons for heterogeneity by scrutinising the studies to assess the extent of between‐trial differences (e.g. age of infant, presenting problems, programme duration, programme focus, and whether or not the intervention was delivered as intended).
We had planned to carry out additional subgroup analyses (Barlow 2013), but there were too few included studies in each meta‐analysis to do this (see Appendix 3 for details).
Sensitivity analysis
We conducted a sensitivity analysis using a fixed‐effect model and a random‐effects model. We intended to re‐analyse the data excluding studies on the basis of design (Barlow 2013), but there were too few included studies in each meta‐analysis to do this (see Appendix 3 for details).
'Summary of findings' tables
We presented the findings of our review in 'Summary of findings' tables (Table 1; Table 2), which provide a transparent and simple tabular format of the review's primary outcomes that may be important to parents and decision makers. For the comparison of PIP versus control, we presented findings for the outcomes of parent mental health (depression) at post‐intervention, and infant attachment at post‐intervention and follow‐up. For PIP versus alternative intervention, we presented findings for the outcomes of parent mental health (depression) at post‐intervention and follow‐up, and infant attachment at post‐intervention and follow‐up. We used GRADEpro software to construct the tables (GRADEpro 2014). The tables present information about the body of evidence (e.g. number of studies), the judgements about the underlying quality of evidence, key statistical results, and a grade for the quality of evidence for each outcome. We used the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) system to describe the quality of the evidence and the strength of recommendation (GRADE 2013; Guyatt 2011). We expressed the quality of evidence on a four‐point adjectival scale from 'high' to 'very low'. We gave evidence from RCT data initially a high quality rating but downgraded it if there was unexplained clinically important heterogeneity, the study methodology had a risk of bias, the evidence was indirect, there was important uncertainty around the estimate of effect, or there was evidence for publication bias. Therefore, it was possible for RCT data to have a very low quality of evidence if several of these concerns were present.
Results
Description of studies
Results of the search
Electronic searches in February 2013 and updated in January 2014 identified 2604 records (for search results, see Appendix 4). The January 2014 search included a correction to the EMBASE search strategy. We identified 16 additional records through other sources. After we removed duplicates, we screened 1937 records. We obtained and scrutinised 85 potentially relevant records, and 61 of these reports (58 studies) did not meet the inclusion criteria and we excluded them (see Characteristics of excluded studies). We included eight studies (from 19 reports of trials) (see Characteristics of excluded studies), and identified five ongoing studies (see Characteristics of ongoing studies) (Figure 1).
1.
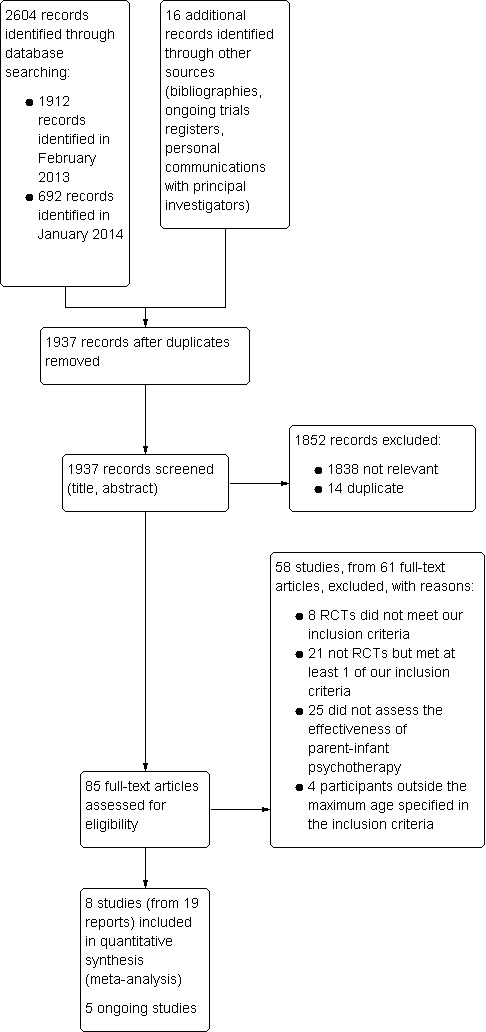
Study flow diagram
Our included studies were: Cicchetti 1999a; Cicchetti 2006b; Cohen 1999b; Cooper 2003a; Lieberman 1991; Robert‐Tissot 1996a; Salomonsson 2011a; and Sleed 2013a. These were grouped as follows:
Cicchetti 1999a comprised three reports (Cicchetti 1999b; Cicchetti 2000; Toth 2006);
Cicchetti 2006b comprised three reports (Cicchetti 2006a; Cicchetti 2011a; Stronach 2013);
Cohen 1999b comprised three reports (Cohen 1999a; Cohen 2000; Cohen 2002);
Cooper 2003a comprised two reports (Cooper 2003b; Murray 2003);
Lieberman 1991 was a single report;
Robert‐Tissot 1996a comprised two reports (Cramer 2002; Robert‐Tissot 1996b);
Salomonsson 2011a comprised three reports (Salomonsson 2011b; Salomonsson 2011c; Salomonsson 2011d); and
Sleed 2013a was a single published report; further details can be found on the Anna Freud Centre's website (Anna Freud 2014).
In both studies conducted by Cicchetti et al. (Cicchetti 1999a and Cicchetti 2006b), each subsequent publication reported on a subset of the main study for which data were available, therefore some details, such as participant demographics, were reported differently in each publication. We have summarised these differences in the Characteristics of included studies table.
Included studies
Three studies were conducted in the USA (Cicchetti 1999a; Cicchetti 2006b; Lieberman 1991), two in the UK (Cooper 2003a; Sleed 2013a); and one each in Canada (Cohen 1999b), Switzerland (Robert‐Tissot 1996a), and Sweden (Salomonsson 2011a).
Methods
All of the included studies were RCTs. Some of the studies also recruited or compared results from a non‐randomised control group (Cicchetti 1999a; Cicchetti 2006b; Robert‐Tissot 1996a); we have not included the results from these non‐randomised arms in this review.
Design
Three studies employed a two‐arm RCT design in which participants were randomised either to PIP or a control (treatment‐as‐usual) condition (Cicchetti 1999a; Lieberman 1991; Salomonsson 2011a), one other employed a cluster‐randomised trial design in which mother and baby units in UK prisons were allocated to either the treatment (PIP) or a control standard care condition (Sleed 2013a). We included these studies in analyses of PIP versus control (control being no intervention or treatment‐as‐usual).
Two studies compared PIP with another treatment: one compared PIP that followed Fraiberg's model (Fraiberg 1987), and hereafter referred to as psychodynamic psychotherapy (PPT), with an 'infant‐led' PIP called WWW (Cohen 1999b); and the second compared PIP with interaction guidance (Robert‐Tissot 1996a). We included these studies in analyses of PIP versus an alternative intervention.
One study employed a three‐arm parallel group design in which PIP (also called child‐parent psychotherapy (CPP)) was compared with a psychoeducational parenting intervention (PPI), derived from the preventive home visiting work of David Olds and colleagues (Olds 1998), and a control community standard care condition (Cicchetti 2006b). This three‐arm study contributed data to both analyses of PIP versus control and PIP versus an alternative intervention. To avoid double counting, we split the number of participants in the common group (i.e. the PIP group).
One study employed a randomised four‐arm comparison of routine primary care, non‐directive counselling, CBT, and psychodynamic (PIP) therapy (Cooper 2003a). For the purposes of this review, we aggregated data from the counselling and CBT arms and compared this with the PIP therapy arm, in analyses of PIP versus alternative intervention.
Participants
The eight included studies initially randomised 846 participants. The number of participants randomised in each trial ranged from 59 (Lieberman 1991) to 193 (Cooper 2003a) parent‐infant dyads. The intervention was directed at mothers in all of the included studies (fathers were not excluded in Robert‐Tissot 1996a, but no separate data for the intervention groups was included in the published report or available from the investigator).
In all eight included studies, the mean age of the infant participants was under 24 months at study enrolment. In one study, the infants were eight weeks old at study entry (Cooper 2003a). We included two studies which stated that the age of some the participating infants was 30 months at study entry but the mean age still met our inclusion criteria (in Cohen 1999b, the mean age in the two intervention groups was 21.5 months (SD = 6.5) in the WWW arm and 19.2 months (SD = 6.1) in the PIP ('PPT') arm, range 10‐30 months; in Robert‐Tissot 1996a the mean age at pretreatment assessment was 15.6 months and ranged from 2 to 30 months (SD = 8.4). The report of Lieberman 1991 stated that the intervention was delivered to infants aged 12 months with infants being 11 to 14 months old at study entry. Cicchetti 1999a stated that the mean age of all the infants in the study (i.e. both the intervention and the control groups) was 20.4 months (SD = 2.38); in Cicchetti 2006b the mean age was 13.31 months (SD = 0.81). In Salomonsson 2011a the mean age of the infants was 4.4 months (SD = 2.4) in the PIP group and 5.9 months (SD = 3.8) in the control group; the maximum age of the infants at study entry was less than < 18 months. In Sleed 2013a, infants were aged 1‐23 months in the intervention group with a mean age of 4.9 months (SD = 4.5; range = 0.2‐23.0 months); in the control group, the mean age was 4.4 months (SD = 4.6; range = 0.1‐18.5 months). Cicchetti 1999a, Cicchetti 2006b, and Cooper 2003a did not state the maximum age of the infants at enrolment.
The eight included studies investigated the effectiveness of PIP with a range of clinical groups, including depressed mothers (Cicchetti 1999a; Cooper 2003a); maltreating parents (Cicchetti 2006b); incarcerated mother‐infant dyads (Sleed 2013b); parents experiencing a range of infant problems (Cohen 1999b; Robert‐Tissot 1996a); mothers with concerns about their own role as mothers, well‐being of the infants, or the mother‐infant relationship (Salomonsson 2011a); and parents of infants at risk of anxious attachment because their mothers are emotionally unavailable (Lieberman 1991).
Two studies reported the population groups to be either Caucasians (94.5% Caucasian in Cicchetti 1999a) or European Caucasian infants (Robert‐Tissot 1996a); or in a third study, American Hispanic (recently immigrated from Mexico or Central America) (Lieberman 1999). Three studies reported the proportion of participants from a minority race or ethnicity: in Cicchetti 2006b, overall, 74.1% of the randomised participants were described as minority race or ethnicity (Cicchetti 2006a) and in Sleed 2013a over one‐half were white and the remaining "Asian, Mixed or other"; in Salomonsson 2011a, 11% in the PIP group and 22% in the control group were described as 'immigrant' (Salomonsson 2011a). Two studies did not report participant ethnicity (Cohen 1999b; Cooper 2003a).
Recruitment
Cicchetti 1999a recruited from a community sample of mothers with a history of depressive disorder via referrals from mental health professionals and through notices placed in the community. Cicchetti 2006b recruited maltreating mothers (i.e. child protection services identified infants known to have been maltreated or who were living in maltreating families with the biological mothers). Cooper 2003a recruited from hospital birth records and after screening for mood disturbances. Cohen 1999b and Robert‐Tissot 1996a used referrals made by the parents or by medical mental health and child welfare professionals for feeding, sleeping, and behaviour problems. Lieberman 1991 recruited dyads from paediatric clinics at large teaching hospitals and neighbourhood health clinics, targeting recent Latino immigrants at risk of anxious attachment due to parental unavailability. Sleed 2013a liaised with the mother and baby unit staff of the women's prisons to identify mother‐infant dyads who would be willing to take part. Salomonsson 2011a recruited mothers through information provided at the delivery ward of the hospital and at parenting internet sites.
Interventions
All included studies involved the delivery of PIP, which had its origins in the work of Selma Fraiberg (Fraiberg 1975; Fraiberg 1980), and was based on a psychodynamic model. Only three of the included studies used manualised programmes (Cicchetti 1999a; Cicchetti 2006b; Sleed 2013a).
Parent‐infant psychotherapy
Lieberman 1991 delivered PIP in unstructured weekly sessions. There was no didactic teaching and the therapists sought to alleviate the mothers' psychological conflicts about their children through observations.
Cicchetti 1999a and Cicchetti 2006b employed manualised infant‐parent psychotherapy. Mothers and their infants attended conjoint therapy sessions. Insights gained by the therapist were used to increase maternal sensitivity, responsivity, and attunement to the child.
In Cohen 1999b, in the PIP ('PPT') arm, the mother and infant played while the therapist's observations were used to draw the mother's attention to her infant's needs and signals. In the infant‐led psychotherapy (WWW), mothers and infants played on the floor, and mothers were instructed to interact only at the infant's initiative. The therapist engaged in a parallel process of 'watching, waiting, wondering' about the interactions between mother and infant and did not intervene.
Salomonsson 2011a also employed a form of infant‐led psychotherapy, in which the analyst received and emotionally processed the infant's distress and communicated it back to the infant in a form that the infant could assimilate, in the presence of the mother.
Robert‐Tissot 1996a employed a method of PIP that was explicitly based on the work of Fraiberg. The therapist listened to the mother's concerns, anxieties and narratives, and examined the relationship between the therapist, mother and infant in terms of the core conflictual relationship between the mother and infant. An emphasis was placed on fostering a positive therapeutic alliance.
Cooper 2003a employed brief psychodynamic parent‐infant therapy, which focused on the therapist exploring the mother's representations of the experience of motherhood in terms of her own experiences of being parented.
Only one study employed a group‐based therapy (Sleed 2013a). "New Beginnings" was conducted over eight sessions that were delivered over a four‐week period. The groups were comprised of up to six mother‐baby dyads and two parent‐infant psychotherapists as facilitators. The topics of each session were selected and examined in terms of their potential as triggers of the attachment relationship.
Further details about the specifics of the psychodynamic therapy, and intervention of all the included studies, can be found in the Characteristics of included studies table.
Duration of intervention
The duration of the therapies ranged from eight sessions (Sleed 2013a) to between 46 and 49 weeks (Cicchetti 2006b).
Site of delivery of intervention
Robert‐Tissot 1996a delivered the intervention and assessed outcomes in a research clinic. Cooper 2003a delivered the intervention in the participants' homes, and Cicchetti 2006b and Lieberman 1991 delivered the intervention in the client's home and the assessment of outcome in university research facilities. Cohen 1999b delivered the intervention in a playroom at a children's mental health centre. Sleed 2013a delivered the intervention in the mother and baby units of several women's prisons in the UK. It is unclear where Salomonsson 2011a and Cicchetti 1999a delivered the intervention, although outcome assessments were made in the research clinic setting.
Monitoring treatment fidelity
The delivery of the intervention was monitored in all included studies and therapists were highly trained and supervised during the intervention.
Comparisons
Four studies compared PIP with a treatment‐as‐usual control condition (Cicchetti 1999a; Lieberman 1991; Salomonsson 2011a; Sleed 2013a). The control condition in Cicchetti 1999a was not described but assumed to be treatment‐as‐usual in which all participants were able to access other mental health treatments; and in Lieberman 1991 was not described but assumed to be normal service provision. In Sleed 2013a, mothers and babies in both groups had access to standard health and social care provision as provided by the prison service. In Salomonsson 2011a, the control condition involved access to the local child health centre responsible for check‐ups from birth to six years of age, antidepressants, and brief psychotherapies.
Two studies compared PIP with alternative interventions, including a behavioural and infant‐led PIP (i.e. WWW) (Cohen 1999b); and Interaction Guidance (Robert‐Tissot 1996a).
One study employed a three‐arm trial design in which PIP was compared with a home visitation intervention delivered over 12 months (i.e. a preventive intervention, involving home visitations scheduled weekly over a 12‐month period) and a treatment‐as‐usual control (Cicchetti 2006b).
Cooper 2003a employed a four‐arm study in which PIP was compared with a control condition (i.e. routine primary care provided by the primary healthcare team), and two alternative interventions (CBT and non‐directive counselling).
Outcomes
Timing of outcome assessment
In Cicchetti 1999a, post‐intervention outcomes were assessed when the child was 36 months of age. In Cicchetti 2006b, all outcomes were assessed at post‐intervention (i.e. when the children were aged 26 months) (Stronach 2013), but cortisol levels were assessed at 12 months' follow‐up (when the children were approximately 38 months of age) (Cicchetti 2011a). Cohen 1999b reported outcomes at post‐intervention and six‐month follow‐up (Cohen 2002). Lieberman 1991 assessed outcomes at post‐intervention (24 months of age). Robert‐Tissot 1996a assessed outcomes immediately post‐intervention and at six‐month follow‐up (when the children were approximately 26 months of age). Long‐term follow‐up interviews at pre‐adolescence were also reported (Cramer 2002), but the results were not presented separately for the intervention groups and we were unable to obtain further information. Sleed 2013a assessed outcomes immediately post‐intervention (range one to 25 months of age) and two months after the end of treatment when the infants were three to 27 months of age. Cooper 2003a presented results immediately post‐intervention and at nine‐month, 18‐month and five‐year follow‐up. Salomonsson 2011a reported post‐intervention outcomes only.
Outcomes
The included studies reported a range of outcomes relating to parental mental health, parent‐infant interactions and infant development (i.e. attachment, behaviour, cognitive, and mental development).
Primary outcomes
Parent outcome
Five studies measured maternal depression using a number of self report measures (e.g. BDI; Beck 1978) (Cicchetti 1999a; Cohen 1999b), Edinburgh Postnatal Depression Scale (EPDS) (Salomonsson 2011a), and Center for Epidemiologic Studies Depression Scale (CES‐D) (Sleed 2013a). In two studies, the number of number of depressive episodes was reported using criteria from the Diagnostic and Statistical Manual of Mental Disorders ‐ Third Edition ‐ Revised (DSM‐III‐R) (Cohen 1999b; Cooper 2003a).
Cohen 1999b measured parent stress using the PSI (Abidin 1986), and parenting sense of competence using the Parenting Sense of Competence (PSOC) scale (Johnston 1989). Salomonsson 2011a reported scores on the Swedish equivalent of the PSI (the Swedish Parenting Stress Questionnaire; SPSQ) and a measure of general psychological stress, the General Severity Index (GSI) of the Symptom Checklist ‐ 90 (SCL‐90) (Derogatis 1994).
Parent‐infant relationship outcomes
Six studies measured mother‐infant interaction during play using video‐taped sessions, which were then analysed and coded. Cohen 1999b measured dyadic reciprocity, dyadic conflict, maternal intrusiveness, and maternal unresponsiveness using the Chatoor Play Scale (Chatoor 1986). Lieberman 1991 measured maternal initiation of interaction, behaviour on reunion (goal‐corrected partnership) and maternal child‐rearing attitudes (control aggression, encourage reciprocity and awareness of complexity in child rearing). Robert‐Tissot 1996a measured controlling or unresponsive behaviour using the CARE‐Index (Crittenden 1981). Sleed 2013a used the Coding Interactive Behavior (CIB) for parent positive engagement and child involvement. Cooper 2003a assessed maternal warmth, responsiveness, and acceptance using the Global Rating Scales (GRS; Murray 1996). Salomonsson 2011a assessed sensitivity, structuring, non‐intrusiveness and non‐hostility; and two infant dimensions: responsiveness and involvement using the EAS.
Robert‐Tissot 1996a measured maternal sensitivity using the CARE‐Index (Crittenden 1981); Lieberman 1991 measured maternal empathic responsiveness (sensitivity) coded from video‐taped free‐play measures; and Sleed 2013a used the CIB for dyadic attunement/maternal sensitivity. Cooper 2003a assessed maternal sensitivity using the GRS (Murray 1996). Salomonsson 2011a assessed sensitivity using the EAS.
Infant outcomes
Five studies measured infant attachment (Cicchetti 1999a; Cicchetti 2006b; Cohen 1999b; Cooper 2003a; Lieberman 1991). Cicchetti 1999a used the Attachment Q‐Set (AQS) (Waters 1995). Three studies assessed infant attachment using the SSP (Cicchetti 2006b; Cohen 1999b; Cooper 2003a). The SSP categorises infant attachment styles into one of four classifications: secure, insecure avoidant, insecure resistant or disorganised attachment (Ainsworth 1971). Secure attachment is a favourable outcome. Lieberman 1991 measured security of attachment using the 90‐item Attachment Q‐sort, which is a refinement of the original Q‐set (AQS) (Waters 1985), and is an observation‐based report, obtained by home visitors at follow‐up only. Lieberman 1991 also assessed dyadic behaviour on reunion, proximity avoidance and resistance, behaviour on reunion and goal‐corrected partnership, using the Ainsworth Interactive Behaviour Scales (modelled on the SSP but with 10‐minute episodes suitable for younger children; Ainsworth 1978).
One study assessed the mean number of angry or externalising behaviours and restriction of affect using a non‐standardised rating of video‐taped interactions (Lieberman 1999). One study used the Child Behaviour Checklist (CBCL; Achenbach 1992) (Cicchetti 2006b). One study measured infant behaviour using the Behavioural Screening Questionnaire (BSQ), and the Rutter Parent A2 Scale (maternal report) and Parent Behavior Checklist (PBCL ‐ teacher report) (Cooper 2003a).
Adverse effects
Three studies (Cicchetti 1999a; Cicchetti 2006b; Cohen 1999b) measured adverse effects in terms of the potential adverse impact of the intervention on attachment security (i.e. measured change from secure to insecure attachment).
Secondary outcomes
Parent outcomes
One study measured maternal representations using the Mother's Object Relations Scale (MORS) (Danis 2005; a self‐report measure) and the PDI (Slade 2004; a structured interview, objective report) (Sleed 2013a); and one study measured maternal attitudes using the Egeland 1979 abbreviated version of the Maternal Attitude Scale (MAS; Cohler 1970) (Lieberman 1991).
Infant outcomes
In one study, infant symptoms were obtained by asking the mother to list the primary problems present at the time of referral for help and to rate these on a 100‐point scale for severity, degree of difficulty, and perceptions of effectiveness and comfort in dealing with problems (Cohen 1999b).
Infant functioning and cognitive development were measured in Cohen 1999b using the Bayley Scales of Infant Development (BSID) I or II (Bayley 1969; Bayley 1993), to derive a Developmental Quotient (DQ); and the BSID Mental Development Index (MDI) (Bayley 1969) in Cooper 2003a. The infant's cognitive development (infant IQ) was assessed in Cicchetti 1999a using the Wechsler Preschool and Primary Scales of Intelligence (WPPSI‐R; Wechsler 1989). Salomonsson 2011a measured infant functioning using the Ages and Stages Questionnaire (ASQ).
Cicchetti 2006b measured infant stress using samples of morning salivary cortisol (expressed as micrograms per decilitre; μg/dL), but the results were aggregated for both intervention groups and we were unable to obtain disaggregated data.
Excluded studies
We formally excluded 58 studies, details of which can be found in the Characteristics of excluded studies table. Of these, eight were RCTs but did not fit our inclusion criteria. Twenty‐one were not RCTs but otherwise met at least one of our inclusion criteria. Twenty‐five studies did not assess the effectiveness of PIP. In three RCTs of PIP (Lieberman 2005; Smyrnios 1993; Toth 2002), the age of the children was outside the maximum age specified in the inclusion criteria for this review.
Risk of bias in included studies
We presented the 'Risk of bias' tables for each included study beneath the Characteristics of included studies table. Figure 2 shows a summary of risk of bias across all studies; Figure 3 shows the results as percentages. For all studies rated as unclear risk of bias, when contacted, the study investigators were unable to provide further details.
2.
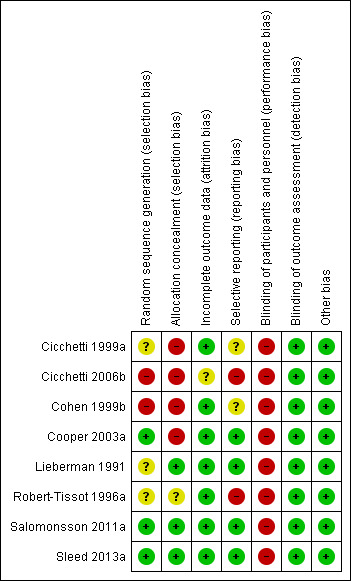
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
3.
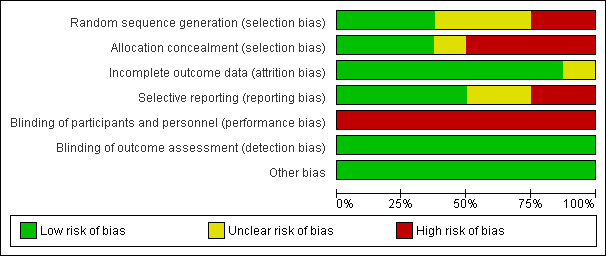
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Allocation
We judged three of the included studies as being at low risk of bias because adequate methods were used to generate the randomisation sequence (Cooper 2003a; Salomonsson 2011a; Sleed 2013a).
The method used to generate the randomisation sequence in Robert‐Tissot 1996a was unclear. Cicchetti 1999a and Lieberman 1991 used block randomisation procedures; they assigned infants to the intervention of control group by blocks stratified for infant sex and birth order (first, later), but the method of randomisation was unclear.
In Cicchetti 2006b, we judged the risk of bias due to randomisation methods as high because some of the control participants who were originally assigned to PPI or infant‐parent psychotherapy (IPP; also called CPP) declined, and the study investigators presented results for this group of decliners in the same group as the community standard care randomised group. We judged Cohen 1999b to be at high risk of bias for random sequence generation because randomisation was inadequate in one‐third of the cases in which assignment was dependent on therapist caseload and availability for time of treatment; in two‐thirds of the cases, assignment was done using a random numbers table.
Three studies concealed allocation sequence (Lieberman 1991; Salomonsson 2011a; Sleed 2013a). In one study, we could not obtain details about allocation concealment (Robert‐Tissot 1996a), and we rated this as unclear. We judged four studies to be at high risk of bias in terms of allocation concealment: Cicchetti 1999a and Cicchetti 2006b did not use a preset allocation sequence; Cohen 1999b did not provide details about allocation concealment, and allocation of one‐third of the participants was based on therapist availability (therefore, it could not have been concealed); and the allocation sequence was not concealed in Cooper 2003a.
Blinding
Performance bias
Due to the nature of the interventions, it was not possible to blind both the participants and personnel to group allocation.
Detection bias
We rated blinding of outcome assessment as low in all of the included studies. Although it is not possible to blind participants and personnel to the allocation given the nature of the treatment, the investigators of the included studies made efforts to ensure that, where possible, those who were involved in the measurement of outcomes were blind to the initial allocation. For four studies, the blinding of outcome assessors was complete. In Robert‐Tissot 1996a, the researchers who coded mother‐infant interactions and analysed and coded the responses to the different questionnaires were blind to the treatment condition. In Cooper 2003a, the outcome assessors were blinded to the allocation. In Sleed 2013a, coders were blind for PDI, and CIB coding was carried out by trained coders who were blind to both the group and time point. In Cicchetti 1999a, outcome assessment was conducted with toddlers, with their mothers present, by an experimenter unaware of experimental hypotheses and the diagnostic and intervention status of participants in the study.
In four studies, blinding of outcome assessment was carried out, but it may not have been possible to blind assessors to all of the outcomes. In these cases, where for example, maternal self reports were used or where outcome assessments were directly administered, we judged that the risk of bias was low. Cohen 1999b used a range of measures (SSP, Chatoor Play Scale, and Bayley Scales) that have proven reliability and validity and that were either scored independently from video‐tapes by raters blind to treatment group or administered directly to the child, which reduces the effects of reporter bias. In Cicchetti 2006b, two independent raters each coded all of the video‐tapes of the individual SSP sessions, and raters were unaware of the maltreatment status and group assignment of individual mother‐child dyads. It was unclear if the cortisol assays were blinded; however, as we were unable to obtain disaggregated data for this outcome, and did not use it in our analyses, we rated this study as low for blinding of outcome assessment risk of bias. In Lieberman 1991, the SSP was coded by fully trained and experienced judges. The home and laboratory measures were scored by coders who were blind to the 12‐month classification and group assignment of the dyads. Different coders scored the home and laboratory measures. In the 24‐month laboratory situation, the free‐play measures and reunion measures were scored by different coders. Intervention process raters had no access to other outcome data. These procedures were adopted to protect the independence of the different ratings. In Salomonsson 2011a, outcome assessors were not blinded for assessments of depression (EPDS), but this was a maternal self report and unlikely to introduce bias. Two raters with substantial clinical infant experience, blind to case history, interview content and assignments, rated EAS.
Incomplete outcome data
We judged seven of the eight included studies to be at low risk of attrition bias with attrition being well investigated and explained, and any effects on the balance of baseline characteristics in the intervention and control groups was not significant (Cicchetti 1999a; Cohen 1999b; Cooper 2003a; Lieberman 1991; Robert‐Tissot 1996a; Salomonsson 2011a; Sleed 2013a).
We rated Cicchetti 2006b, as unclear for attrition bias, as we were uncertain if the decision to aggregate those participants who were randomised to receive treatment but declined into the no treatment control group, introduced a source of bias.
Selective reporting
We judged two out of the eight included studies to be at high risk of selective outcome reporting (Cicchetti 2006b; Robert‐Tissot 1996a). In both studies, several outcomes were not reported for the intervention group; in some cases, two intervention groups were combined and compared with the control group or a non‐clinical sample (non‐clinical being a non‐randomised control group). In Cicchetti 2006b, pre‐specified outcomes were reported, but intervention group data were aggregated and presented alongside randomised control group and non‐maltreated non‐randomised comparison groups.
We rated the risk of bias from selective reporting in Cicchetti 1999a as unclear. Although some outcomes were reported selectively, it was unclear if this would have introduced bias. We also rated Cohen 1999b as unclear for selective outcome reporting because the number of participants in each attachment category was not reported (although the patterns of change were reported). We were unable to obtain the attachment category data from the principal investigator, as the records were no longer available.
We judged the remaining four studies as being at low risk of reporting bias because all pre‐specified outcomes were reported according to the group assignment (Cooper 2003a; Lieberman 1991; Salomonsson 2011a; Sleed 2013a).
Other potential sources of bias
We also examined baseline or pre‐treatment means where available, to assess whether there was any imbalance in terms of participant characteristics. Although there were some differences in the baseline demographics, this was not thought to introduce any additional sources of bias and we rated all studies as low risk.
Effects of interventions
We summarised the results of our meta‐analyses below. Data derived from single studies that could not be pooled in meta‐analyses are provided in the Data and analyses section, Comparison 3 and Comparison 4.
For effect sizes of SMD, values greater than 0.70 have been treated as large; values between 0.40 and 0.70 as moderate; and values less than 0.40 but greater than 0.10 as small (Higgins 2011).
We have summarised the results below under headings corresponding to the primary and secondary outcomes outlined in the Types of outcome measures section and in the Table 1 and Table 2.
In the text below, numbers given are the total number of participants randomised. Where it has been possible to calculate an effect size, we have reported this with 95% CIs. Where the calculated effect size was statistically significant (P value < 0.05), we stated whether the result favours the intervention (i.e. PIP) group.
We have indicated which outcome measures were derived from participant self reports.
Comparison 1. Parent‐infant psychotherapy versus control
Parent outcomes
Primary parent outcomes
1.1 Parent mental health: depression (dichotomous data) post‐intervention
One meta‐analysis of three studies reported the number of subsequent episodes of depression post‐intervention using the Diagnostic Interview Schedule ‐ Version III ‐ Revised (DIS‐III‐R; Cicchetti 1999a), DSM‐III‐R (Cooper 2003a), or CES‐D (Sleed 2013a). The results of one meta‐analysis using a random‐effects model showed no significant difference between PIP and control groups (RR 0.74, 95% CI 0.52 to 1.04, 278 participants, Analysis 1.1). Heterogeneity was low (Chi2 = 2.30; degree of freedom (df) = 2; P value = 0.32; tau2 = 0.01; I2 = 13%). We rated the overall quality of the evidence as low (Table 1).
1.1. Analysis.
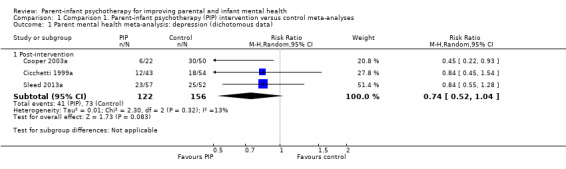
Comparison 1 Comparison 1. Parent‐infant psychotherapy (PIP) intervention versus control meta‐analyses, Outcome 1 Parent mental health meta‐analysis: depression (dichotomous data).
We assessed the impact of the inclusion of data from one cluster‐randomised trial (Sleed 2013a) in further sensitivity analyses (see 'Sensitivity analyses: parent‐infant psychotherapy versus control, sensitivity analyses assuming different values of intraclass correlation coefficient') .
1.2 Parent mental health: depression (continuous data) post‐intervention
Four studies reported a continuous measure of depression at post‐intervention, which was measured using the CES‐D Scale (Sleed 2013a), BDI (Cicchetti 1999a), and EPDS (Cooper 2003a; Salomonsson 2011a. The result shows no difference between PIP and control groups (SMD ‐0.22, 95% CI ‐0.46 to 0.02, 356 participants, Analysis 1.2). Heterogeneity was low (Chi2 = 3.75; df = 3; P value = 0.29; tau2 = 0.01, I2 = 20%). We rated the overall quality of the evidence as low for depression at post‐intervention (Table 1).
1.2. Analysis.
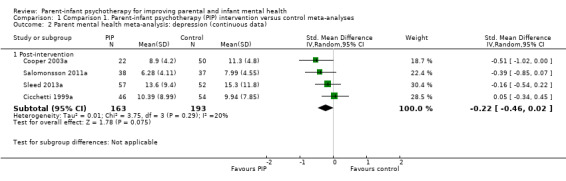
Comparison 1 Comparison 1. Parent‐infant psychotherapy (PIP) intervention versus control meta‐analyses, Outcome 2 Parent mental health meta‐analysis: depression (continuous data).
We assessed the impact of the inclusion of data from one cluster randomised trial (Sleed 2013a) in further sensitivity analyses (see 'Sensitivity analyses: parent‐infant psychotherapy versus control, sensitivity analyses assuming different values of intraclass correlation coefficient') .
Secondary parent outcomes
There were no studies comparing PIP and a control intervention reporting secondary parent outcomes that could be pooled in a meta‐analysis.
Parent‐infant relationship outcomes
Primary parent‐infant relationship outcomes
1.3 Maternal sensitivity meta‐analysis: post‐intervention
Four studies reported maternal sensitivity post‐intervention, which was measured using the CIB scale (dyadic attunement) (Sleed 2013a); EAS (sensitivity subscale) (Salomonsson 2011a); video‐taped interaction rated using the sensitivity dimension from the Murray 1996 scales (Cooper 2003a); and maternal empathic responsiveness/empathy post‐intervention, which was measured using video‐taped free play episodes and coded using a non‐standardised nine‐point scale based on body orientation, posture, facial expressions, and timing and content of responses to provide a measures of empathic responsiveness/empathy (Lieberman 1991). There was no statistically significant difference between PIP and control groups (SMD ‐0.13, 95% CI ‐0.64 to 0.38, 283 participants, Analysis 1.3). There were significant levels of heterogeneity (Chi2 = 13.00; df = 3; P value = 0.005; tau2 = 0.21; I2 = 77%). We assessed the impact of the inclusion of data from one cluster‐randomised trial (Sleed 2013a) in further sensitivity analyses (see 'Sensitivity analyses: parent‐infant psychotherapy versus control, sensitivity analyses assuming different values of intraclass correlation coefficient').
1.3. Analysis.
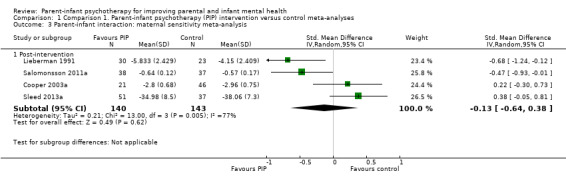
Comparison 1 Comparison 1. Parent‐infant psychotherapy (PIP) intervention versus control meta‐analyses, Outcome 3 Parent‐infant interaction: maternal sensitivity meta‐analysis.
1.4 Child involvement meta‐analysis: post‐intervention
Two studies reported child involvement post‐intervention, which used the CIB scales (i.e. involvement of the child subscale) (Sleed 2013a), and the EAS (i.e. infant involvement subscale) (Salomonsson 2011a). There was no statistically significant difference between intervention and control groups (SMD ‐0.01, 95% CI ‐0.32 to 0.30, 163 participants, Analysis 1.4). There was no evidence of heterogeneity (Chi2 = 0.39; df = 1; P value = 0.53; tau2 = 0, I2 = 0%).
1.4. Analysis.
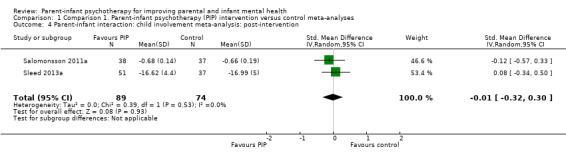
Comparison 1 Comparison 1. Parent‐infant psychotherapy (PIP) intervention versus control meta‐analyses, Outcome 4 Parent‐infant interaction: child involvement meta‐analysis: post‐intervention.
We assessed the impact of the inclusion of data from one cluster‐randomised trial (Sleed 2013a) in further sensitivity analyses (see 'Sensitivity analyses: parent‐infant psychotherapy versus control, sensitivity analyses assuming different values of intraclass correlation coefficient'). The impact of the inclusion of data from one cluster randomised trial was assessed following adjustment for clustering (i.e. using an imputed ICC: 0.2, 0.4, 0.6, 0.8), and the result remains largely unchanged (i.e. slightly wider 95% CIs due to the inflated standard errors). The results showed no significant difference between PIP and control groups (SMD ‐0.07, 95% CI ‐0.46 to 0.32 if ICC = 0.2; SMD ‐0.09, 95% CI ‐0.50 to 0.33 if ICC = 0.4; SMD ‐0.09, 95% CI ‐0.52 to 0.33 if ICC = 0.6; SMD ‐0.10, 95% CI ‐0.53 to 0.33 if ICC = 0.8, Analysis 5.4).
5.4. Analysis.
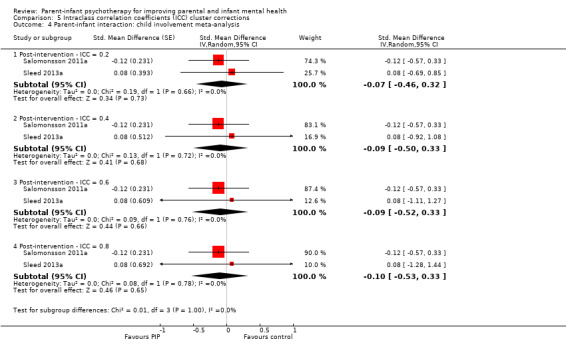
Comparison 5 Intraclass correlation coefficients (ICC) cluster corrections, Outcome 4 Parent‐infant interaction: child involvement meta‐analysis.
1.5 Maternal positive engagement meta‐analysis: post‐intervention
Three studies measured maternal positive engagement at post‐intervention, which used the CIB scale (i.e. interactions where the parent looked and talked to her baby positively, did not appear depressed, and was enthusiastic in engaging with her baby) (Sleed 2013a); the 'structuring' domain of the EAS (i.e. assesses the extent to which the mother provided appropriate guidance and suggestions during video‐taped mother and baby interactions) (Salomonsson 2011a), and maternal engagement using coded video‐taped free play sessions in a laboratory session rated on a seven‐point scale for frequency, quality and persistence of effort to initiate interaction with the child (Lieberman 1991). There was no statistically significant difference between PIP and control groups (SMD ‐0.16, 95% CI ‐0.46 to 0.15, 216 participants, Analysis 1.5). Heterogeneity was low (Chi2 = 2.53; df = 2; P value = 0.28; tau2 = 0.02; I2 = 21%).
1.5. Analysis.
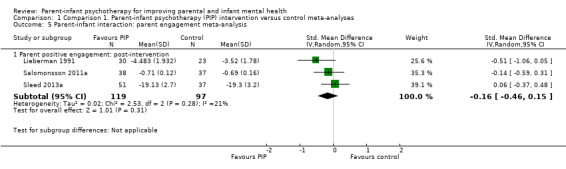
Comparison 1 Comparison 1. Parent‐infant psychotherapy (PIP) intervention versus control meta‐analyses, Outcome 5 Parent‐infant interaction: parent engagement meta‐analysis.
We assessed the impact of the inclusion of data from one cluster‐randomised trial (Sleed 2013a) in further sensitivity analyses (see 'Sensitivity analyses: parent‐infant psychotherapy versus control, sensitivity analyses assuming different values of intraclass correlation coefficient').
Infant outcomes
Primary infant outcomes
Infant emotional well‐being
1.6 Infant attachment category: post‐intervention
Two studies assessed attachment classification (i.e. secure, avoidant, resistant, disorganised) using the SSP at post‐intervention (Cicchetti 1999a; Cicchetti 2006b). We conducted meta‐analyses for each type of infant attachment style. The data showed a statistically significant difference favouring the PIP group for the outcome of secure attachment (RR 8.93, 95% CI 1.25 to 63.70; P value = 0.03, 168 participants, Analysis 1.6). There was substantial heterogeneity (Chi2 = 3.71; df = 1; P value = 0.05; tau2 = 1.54; I2 = 73%) and we rated the overall quality of the evidence as very low (Table 1).
1.6. Analysis.
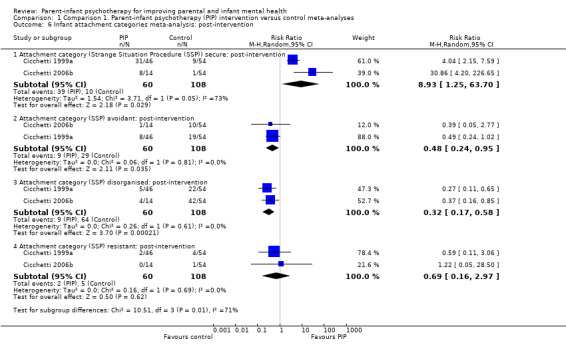
Comparison 1 Comparison 1. Parent‐infant psychotherapy (PIP) intervention versus control meta‐analyses, Outcome 6 Infant attachment categories meta‐analysis: post‐intervention.
We found that significantly fewer infants were avoidant in the PIP group compared with the control group (RR 0.48, 95% CI 0.24 to 0.95, P value = 0.03, 168 participants, Analysis 1.6). There was low heterogeneity (Chi2 = 0.06; df = 1; P value = 0.81; tau2 = 0; I2 = 0%). Significantly fewer infants in the PIP group compared with the control group were disorganised (RR 0.32, 95% CI 0.17 to 0.58, 168 participants, Analysis 1.6). We rated the overall quality of the evidence as low (Table 1). There was low heterogeneity (Chi2 = 0.26; df = 1; P value = 0.61; tau2 = 0; I2 = 0%). However, there were no statistically significant differences between the PIP group and the control group at post‐intervention for the resistant category (RR 0.69, 95% CI 0.16 to 2.97, 168 participants, Analysis 1.6). There was low heterogeneity (Chi2 = 0.16; df = 1; P value = 0.69; tau2 = 0, I2 = 0%).
1.7 Infant attachment category: follow‐up
Two studies reported attachment category (i.e. secure, avoidant, resistant, disorganised) using the SSP at follow‐up (Cicchetti 2006b; Cooper 2003a). There was a statistically significant difference favouring the PIP group compared with the control group for the number of infants securely attached, that is, more infants in the PIP group were securely attached by the end of the intervention (RR 3.30, 95% CI 1.82 to 6.00, P value < 0.0001, 129 participants, Analysis 1.7). We rated the overall quality of the evidence as low for secure infant attachment (Table 1). Significantly more infants in the control group were avoidant (RR 0.33, 95% CI 0.15 to 0.76, P value = 0.81, 129 participants, Analysis 1.7). However, there were no differences between the groups in the proportions of infants classified as resistant (RR 0.57, 95% CI 0.11 to 3.07, 129 participants, Analysis 1.7) or disorganised (RR 0.80, 95% CI 0.29 to 2.19, 129 participants, Analysis 1.7). We rated the overall quality of the evidence as very low for the disorganised infant attachment outcome (Table 1). There was low heterogeneity for the secure, avoidant and resistant categories (tau2 = 0.00; I2 = 0%, Analysis 1.7). There was substantial heterogeneity for the disorganised category (Chi2 = 2.04; df = 1; P value = 0.15; tau2 = 0.27; I2 = 51%, Analysis 1.7).
1.7. Analysis.
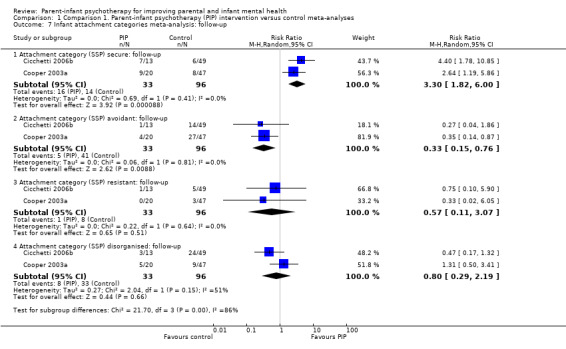
Comparison 1 Comparison 1. Parent‐infant psychotherapy (PIP) intervention versus control meta‐analyses, Outcome 7 Infant attachment categories meta‐analysis: follow‐up.
1.8 Infant attachment change: post‐intervention
Two studies reported whether participants had changed attachment category by the end of the intervention (i.e. immediately post‐intervention) (Cicchetti 1999a; Cicchetti 2006b). Significantly more infants in the PIP group had moved from insecure at pre‐intervention to secure at post‐intervention (RR 11.45, 95% CI 3.11 to 42.08; P value = 0.0002, 168 participants, Analysis 1.8). There were moderate levels of heterogeneity (Chi2 = 1.61; df = 1; P value = 0.21; tau2 = 0.39; I2 = 38%). There were more infants who were secure at pre‐intervention and remained secure at post‐intervention (stably secure) in the PIP groups, but this was not statistically significant (RR 2.28, 95% CI 0.41 to 12.56, 168 participants, Analysis 1.8). There were moderate levels of heterogeneity (Chi2 = 1.46; df = 1; P value = 0.23; tau2 = 0.66; I2 = 31%).
1.8. Analysis.
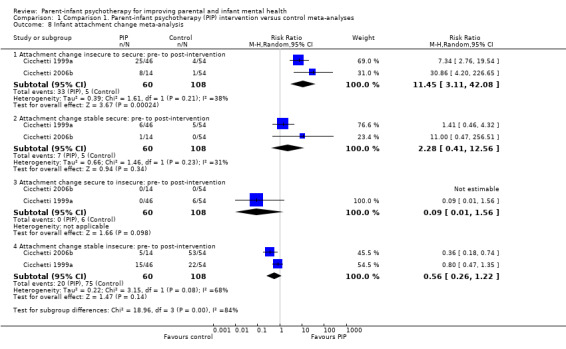
Comparison 1 Comparison 1. Parent‐infant psychotherapy (PIP) intervention versus control meta‐analyses, Outcome 8 Infant attachment change meta‐analysis.
There was no statistically significant difference between the number of participants whose attachment category changed from secure at pre‐intervention to insecure at post‐intervention (RR 0.09, 95% CI 0.01 to 1.56, 168 participants, Analysis 1.8). (Note: it was not possible to assess heterogeneity in this meta‐analysis because no participants changed from secure to insecure categories; therefore, statistical heterogeneity is not estimable.)
Although more infants in the control group were insecure at pre‐ and post‐intervention (stably insecure), there was no significant difference in children who were stably insecure (RR 0.56, 95% CI 0.26 to 1.22, 168 participants, Analysis 1.8). There were high levels of heterogeneity (Chi2 = 3.15; df = 1; P value = 0.08; tau2 = 0.22; I2 = 68%).
1.9 Infant problem behaviours, angry or externalising behaviours meta‐analysis: follow‐up
Two studies reported angry or externalising behaviour at follow‐up, which was measured using the CBCL (externalising subscale) (Cicchetti 2006b); and the BSQ, modified for use with this age group (Cooper 2003a). There was no statistically significant difference between the two groups (SMD 0.22, 95% CI ‐0.34 to 0.77, 131 participants, Analysis 1.9). There was substantial heterogeneity (Chi2 = 1.91; df = 1; P value = 0.17; tau2 = 0.08; I2 = 48%).
1.9. Analysis.
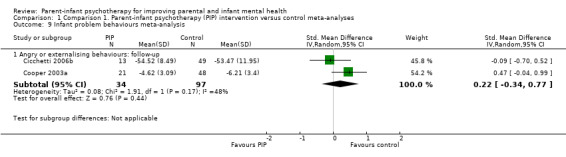
Comparison 1 Comparison 1. Parent‐infant psychotherapy (PIP) intervention versus control meta‐analyses, Outcome 9 Infant problem behaviours meta‐analysis.
Secondary infant outcomes
1.10 Infant cognitive development meta‐analysis: post‐intervention
Two studies measured infant cognitive development post‐intervention using the Weschler Preschool Scales of Intelligence (WPPSI; full scale) (Cicchetti 1999a); and the ASQ: SE (maternal report) (Salomonsson 2011a). There was no statistically significant difference between PIP and control groups (SMD ‐0.15, 95% CI ‐0.82 to 0.51, 172 participants, Analysis 1.10). There were significant levels of heterogeneity (Chi2 = 4.76; df = 1; P value = 0.03; tau2 = 0.18; I2 = 79%).
1.10. Analysis.
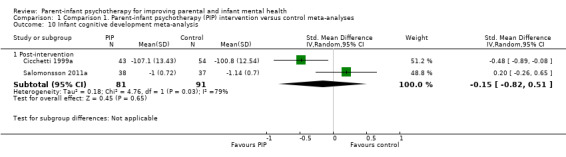
Comparison 1 Comparison 1. Parent‐infant psychotherapy (PIP) intervention versus control meta‐analyses, Outcome 10 Infant cognitive development meta‐analysis.
Adverse effects
Other than the potential for the therapy to have adverse effects on the attachment of the infant (see 1.6 Infant attachment category: post‐intervention; 1.7 Infant attachment category: follow‐up; and 1.8 infant attachment change: pre‐ to post‐intervention), no studies comparing PIP with a control group reported adverse effects.
Comparison 2. Parent‐infant psychotherapy versus alternative (non‐parent‐infant psychotherapy) intervention
Parent outcomes
Primary parent outcomes
2.1.1 Parent mental health: depression (continuous data): post‐intervention
Note: in Cohen 1999b, PPT refers to the standard PPT, that is, PIP and WWW to the infant‐led PIP.
Two studies reported continuous measures of depression post‐intervention, which was measured using the BDI (self report) (Cohen 1999b); and the EPDS (Cooper 2003a). There was no statistically significant difference between PPT and WWW (SMD 0.23, 95% CI ‐0.49 to 0.95, 172 participants, Analysis 2.1). There were significant levels of heterogeneity (Chi2 = 4.36; df = 1; P value = 0.04; tau2 = 0.21; I2 = 77%). We rated the quality of the evidence as very low (Table 2).
2.1. Analysis.
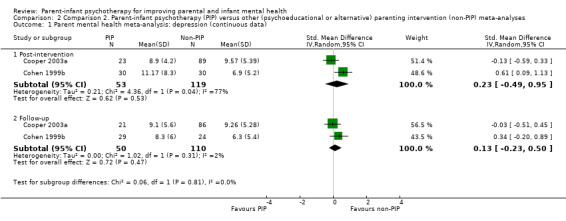
Comparison 2 Comparison 2. Parent‐infant psychotherapy (PIP) versus other (psychoeducational or alternative) parenting intervention (non‐PIP) meta‐analyses, Outcome 1 Parent mental health meta‐analysis: depression (continuous data).
2.1.2 Parent mental health: depression (continuous data): follow‐up
Two studies reported a continuous measure of depression at follow‐up, which was measured using the EPDS at follow‐up (Cooper 2003); and the BDI at six‐month follow‐up (Cohen 1999b). There was no statistically significant difference between PIP and non‐PIP at 18 months (SMD 0.13, 95% CI ‐0.23 to 0.5, 160 participants, Analysis 2.1) and levels of heterogeneity were low (I2 = 2%). We rated the quality of the evidence as low (Table 2).
Secondary parent outcomes
There were no studies comparing PIP and an alternative intervention reporting secondary parent outcomes that could be pooled in a meta‐analysis.
Parent‐infant relationship outcomes
Primary parent‐infant relationship outcomes
2.2.1 Maternal sensitivity: post‐intervention
Three studies reported maternal sensitivity post‐intervention, which was measured using the Chatoor Play Scale ‐ subscale dyadic reciprocity (Cohen 1999b), the Crittenden CARE‐Index (Robert‐Tissot 1996a), and the GRS of video‐taped mother‐infant interactions (Cooper 2003a). There was no statistically significant difference between PIP and non‐PIP groups (SMD 0.20, 96% CI ‐0.27 to 0.66, 248 participants, Analysis 2.2). There were marginally significant levels of heterogeneity (Chi2 = 5.81; df = 2; P value = 0.05; tau2 = 0.11; I2 = 66%).
2.2. Analysis.
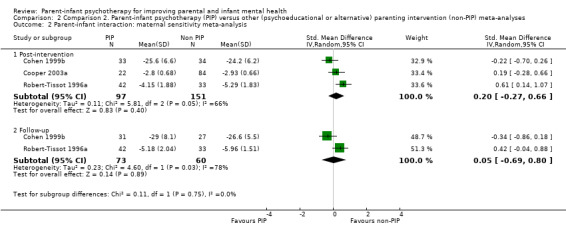
Comparison 2 Comparison 2. Parent‐infant psychotherapy (PIP) versus other (psychoeducational or alternative) parenting intervention (non‐PIP) meta‐analyses, Outcome 2 Parent‐infant interaction: maternal sensitivity meta‐analysis.
2.2.2 Maternal sensitivity: follow‐up
Two studies reported maternal sensitivity at six‐month follow‐up using the Chatoor Play Scale ‐ subscale dyadic reciprocity (Cohen 1999b), and the Crittenden CARE‐Index (Robert‐Tissot 1996a). There was no statistically significant difference between the PIP and the non‐PIP groups (SMD 0.05, 95% CI ‐0.69 to 0.80, 133 participants, Analysis 2.2). There were significant levels of heterogeneity (Chi2 = 4.6; df = 1; P value = 0.03; tau2 = 0.23; I2 = 78%).
Infant mental health and development
Primary infant outcomes
2.3 Infant attachment category: post‐intervention
2.3.1 Attachment category secure: post‐intervention
Two studies comparing PIP versus non‐PIP reported attachment status, which was measured using the SSP (Cicchetti 2006b; Cohen 1999b). There was no statistically significant difference in the numbers of infants categorised as having secure attachment between PIP and non‐PIP groups (RR 0.83, 95% CI 0.32 to 2.13, 102 participants, Analysis 2.3). There was a high level of heterogeneity (Chi2 = 2.6; df = 1; P value = 0.11; tau2 = 0.3; I2 = 62%) and we rated the overall quality of the evidence as very low (Table 2).
2.3. Analysis.
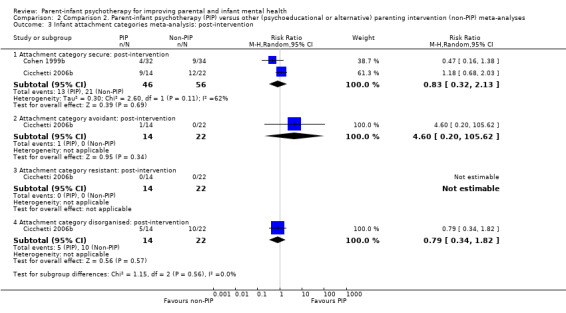
Comparison 2 Comparison 2. Parent‐infant psychotherapy (PIP) versus other (psychoeducational or alternative) parenting intervention (non‐PIP) meta‐analyses, Outcome 3 Infant attachment categories meta‐analysis: post‐intervention.
2.3.2 Attachment category avoidant/resistant/disorganised: post‐intervention
Only one study comparing PIP versus non‐PIP reported the proportion of infants with avoidant, resistant or disorganised attachment status at post‐intervention (Cicchetti 2006b). There was no statistically significant difference between PIP and non‐PIP groups in the numbers of infants categorised as avoidant (RR 4.60, 95% CI 0.20 to 105.62, 36 participants); or disorganised (RR 0.79, 95% CI 0.34 to 1.82, 36 participants, Analysis 2.3). No infants were categorised as resistant. We rated the overall quality of the evidence for the disorganised outcome as low (Table 2).
2.4 Infant attachment category: follow‐up
Two studies comparing PIP versus non‐PIP reported the proportion of children with secure, avoidant, resistant or disorganised attachment status at follow‐up (Cicchetti 2006b; Cooper 2003a). There was no significant difference between the groups for the secure category (RR 1.61, 95% CI 0.83 to 3.12, 136 participants, Analysis 2.4); this subgroup had moderate levels of heterogeneity (Chi2 = 1.79; df = 1; P value = 0.18; tau2 = 0.11; I2 = 44%) and we rated the overall quality of the evidence as very low. There was no significant difference between the groups for the avoidant category (RR 0.76, 95% CI 0.35 to 1.64, 136 participants, Analysis 2.4); resistant category (RR 1.48, 95% CI 0.32 to 6.98, 136 participants, Analysis 2.4) or disorganised category (RR 0.82, 95% CI 0.30 to 2.22, 136 participants, Analysis 2.4). There were high levels of heterogeneity for the disorganised category (Chi2 = 2.79; df = 1; tau2 = 0.33; P value = 0.09; I2 = 64%). For the disorganised infant attachment outcome, we rated the overall quality of the evidence as very low (Table 2).
2.4. Analysis.
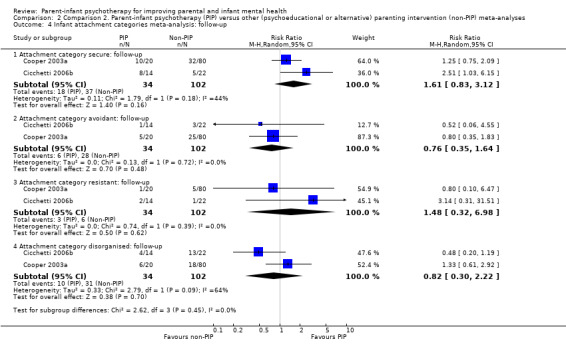
Comparison 2 Comparison 2. Parent‐infant psychotherapy (PIP) versus other (psychoeducational or alternative) parenting intervention (non‐PIP) meta‐analyses, Outcome 4 Infant attachment categories meta‐analysis: follow‐up.
2.5 Infant attachment category change: pre‐ to post‐intervention
2.5.1 Attachment change insecure to secure: pre‐ to post‐intervention
Two studies comparing PIP versus non‐PIP reported change in attachment category from insecure to secure pre‐ to post‐intervention, and from secure to insecure pre‐ to post‐intervention (Cicchetti 2006b; Cohen 1999b). There were no statistically significant differences between the PIP and non‐PIP groups for change from insecure to secure (RR 0.48, 95% CI 0.06 to 4.10, 102 participants; I2 = 76%, Analysis 2.5) or secure to insecure (RR 1.59, 95% CI 0.49 to 5.13, 102 participants, Analysis 2.5).
2.5. Analysis.
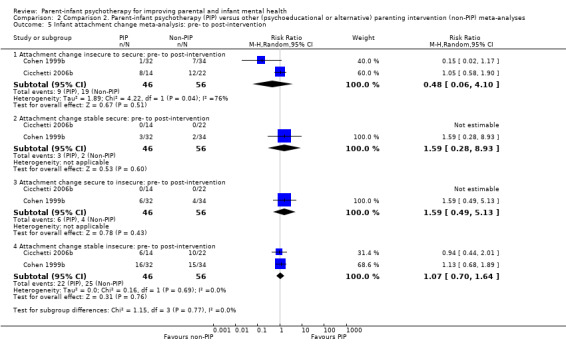
Comparison 2 Comparison 2. Parent‐infant psychotherapy (PIP) versus other (psychoeducational or alternative) parenting intervention (non‐PIP) meta‐analyses, Outcome 5 Infant attachment change meta‐analysis: pre‐ to post‐intervention.
2.5.2 Attachment change stable secure and stable insecure: pre‐ to post‐intervention
Two studies reported change in attachment from stable secure pre‐ to post‐intervention and from stable insecure pre‐ to post‐intervention (Cicchetti 2006b; Cohen 1999b). There were no significant differences between intervention groups for the proportion of children who were stably secure (RR 1.59, 95% CI 0.28 to 8.93, 102 participants, Analysis 2.5) or stably insecure (RR 1.07, 95% CI 0.70 to 1.64; tau2 = 0; I2 = 0%, Analysis 2.5).
2.6 Infant problem behaviours
2.6.1 Angry or externalising behaviours: follow‐up
Three studies comparing PIP versus non‐PIP reported angry or externalising behaviours at follow‐up, which was measured using the Mental Scales of the BSID (i.e. the Bayley Infant Behavior Rating Scale, subscale Emotion Regulation) at six‐month follow‐up (Cohen 1999b); the subscale of the CBCL for maternally reported externalising behaviours at 12‐month follow‐up (Cicchetti 2006b); and the BSQ, modified for use with the study's age group at six‐month follow‐up (Cooper 2003a). There was no statistically significant difference between groups (SMD ‐0.05, 95% CI ‐0.39 to 0.28,184 participants, Analysis 2.6). There was no evidence of heterogeneity (Chi2 = 1.07; df = 2; P value = 0.58; tau2 = 0; I2 = 0%).
2.6. Analysis.
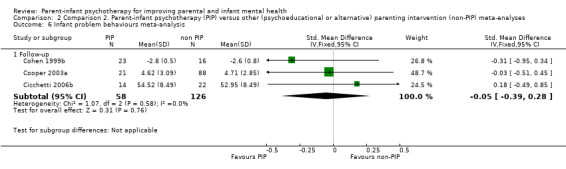
Comparison 2 Comparison 2. Parent‐infant psychotherapy (PIP) versus other (psychoeducational or alternative) parenting intervention (non‐PIP) meta‐analyses, Outcome 6 Infant problem behaviours meta‐analysis.
Secondary infant outcomes
2.7 Infant cognitive development: follow‐up
Two studies reported infant cognitive development at follow‐up, which was measured using the Mental Scales of the BSID I or II to derive a DQ (Cohen 1999b), and the BSID MDI (Bayley 1969) in Cooper 2003a. There was no statistically significant difference between PIP and non‐PIP groups (SMD 0.10, 95% CI ‐0.25 to 0.46, 162 participants, Analysis 2.7). There was no evidence of heterogeneity (Chi2 = 0; df = 1; P value = 0.95; tau2= 0; I2 = 0%).
2.7. Analysis.
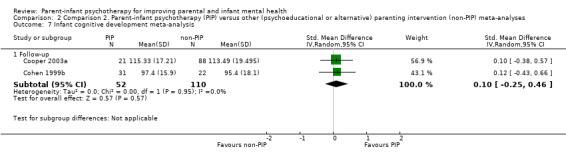
Comparison 2 Comparison 2. Parent‐infant psychotherapy (PIP) versus other (psychoeducational or alternative) parenting intervention (non‐PIP) meta‐analyses, Outcome 7 Infant cognitive development meta‐analysis.
2.8 Infant cortisol regulation; post‐intervention and follow‐up
Salivary cortisol samples were obtained by the principal investigators of Cicchetti 2006b and reported in Cicchetti 2011a, which described collection of morning saliva cortisol samples at pre‐intervention, mid‐intervention, post‐intervention (26 months of age) and 12‐month follow‐up (38 months of age). We were unable to obtain disaggregated data from the maltreated PIP and non‐PIP intervention groups. The study report stated that there were no differences in cortisol levels between the aggregated maltreated intervention groups (PIP and non‐PIP) versus the community standard control group. By 12‐month follow‐up, infants in the maltreated intervention group had normalised cortisol levels (i.e. they were not different from a normal community sample).
Adverse effects
Other than the potential for the therapy to have adverse effects on the attachment of the infant (i.e. the extent to which infants who were securely attached at baseline were categorised as insecure at post‐intervention or follow‐up) (see 2.3 Infant attachment category: post‐intervention; 2.4 Infant attachment category: follow‐up; and 2.5 infant attachment change: pre‐ to post‐intervention), none of the comparisons of PIP with a comparison treatment group reported adverse events.
Comparison 3. Parent‐infant psychotherapy versus control (single‐study results only)
We did not perform meta‐analyses for the following outcomes as each outcome was only reported by one study.
Parent outcomes
Primary parent outcomes
3.1 Parent mental health
There was no statistically significant difference between PIP and the control group for any dichotomous measure of parental mental health depression assessed at nine‐month, 18‐month or five‐year follow‐up (DSM‐III‐R interview, Analysis 3.1; Cooper 2003a); or for any continuous measure of parental mental health depression assessed using the EPDS at nine‐month, 18‐month or five‐year follow‐up (Analysis 3.2; Cooper 2003a); or for parental stress assessed using the SPSQ and general maternal psychological stress measured using the GSI (SCL‐90) at post intervention (Analysis 3.3; Analysis 3.4; Salomonsson 2011a).
3.1. Analysis.
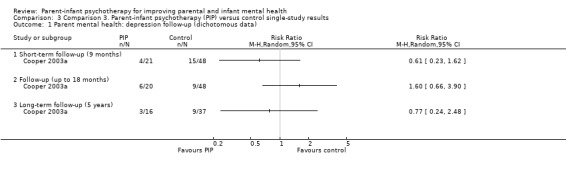
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 1 Parent mental health: depression follow‐up (dichotomous data).
3.2. Analysis.
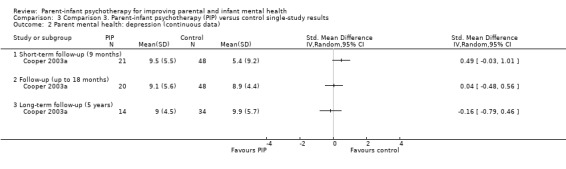
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 2 Parent mental health: depression (continuous data).
3.3. Analysis.
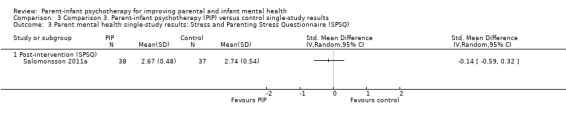
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 3 Parent mental health single‐study results: Stress and Parenting Stress Questionnaire (SPSQ).
3.4. Analysis.
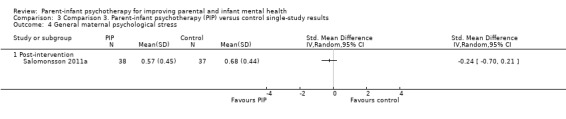
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 4 General maternal psychological stress.
3.2 Secondary parent outcomes
There was no statistically significant difference between PIP and the control group for parental reflective function at post‐intervention using the PDI (Analysis 3.5; Sleed 2013a); maternal representations at post‐intervention using the MORS object relations scale (Analysis 3.6; Sleed 2013a); or maternal attitudes using the maternal attitudes scale at post‐intervention (Analysis 3.7; Lieberman 1991).
3.5. Analysis.
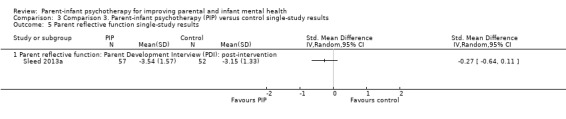
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 5 Parent reflective function single‐study results.
3.6. Analysis.
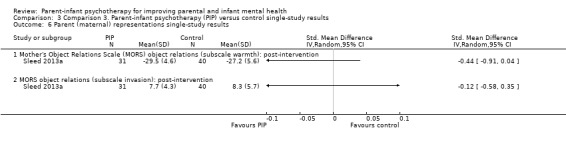
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 6 Parent (maternal) representations single‐study results.
3.7. Analysis.
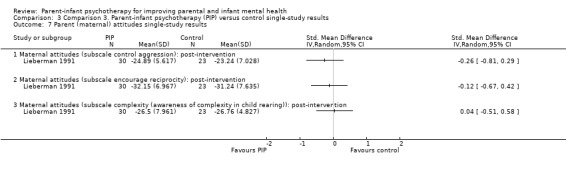
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 7 Parent (maternal) attitudes single‐study results.
Parent‐infant relationship outcomes
Primary and secondary parent‐infant relationship outcomes
3.3 Parent‐infant interaction
One trial assessed maternal reports of mother‐infant relationship problems and behaviour management problems at post‐intervention (Cooper 2003a). There were no statistically significant differences between the groups for either outcome, for the total number of mothers reporting problems, or of the mothers who had reported problems before treatment and who were still reporting problems after the treatment period (i.e. controlling for reported problems prior to treatment did not make a difference) (Analysis 3.8). There was no statistically significant difference for maternal intrusiveness post‐intervention between PIP and control groups using the EAS scales (Analysis 3.9; Salomonsson 2011a). However, there were statistically significant findings favouring the PIP group for a well‐adapted dyadic relationship using the Parent‐Infant Relationship Global Assessment Scale (PIR‐GAS) post‐intervention (SMD ‐0.58, 95% CI ‐1.05 to ‐0.12, P value = 0.01, Analysis 3.9; Salomonsson 2011a), and dyadic behaviour on reunion at post‐intervention (SMD ‐1.37, 95% CI ‐1.98 to ‐0.77, P value < 0.00001, Analysis 3.9; Lieberman 1991).
3.8. Analysis.
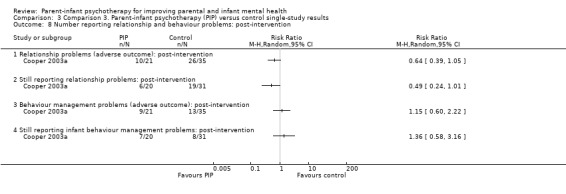
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 8 Number reporting relationship and behaviour problems: post‐intervention.
3.9. Analysis.
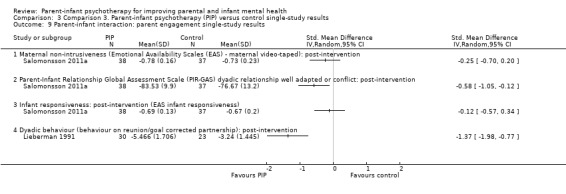
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 9 Parent‐infant interaction: parent engagement single‐study results.
Infant outcomes
Primary infant outcomes
3.4 Attachment security
There was a significant difference in the intervention group for stability in infants classified as disorganised at both pre‐ and post‐intervention using the SSP (RR 0.15, 95% CI 0.04 to 0.59, P value = 0.007) (note: disorganised attachment style is a negative outcome, this result favours the PIP group) and for infants who had changed to a secure attachment (RR 5.20, 95% CI 1.26 to 21.42, Analysis 3.10) (Cicchetti 1999a). There was no statistically significant difference between the groups for infants who changed from an initially disorganised classification to another insecure classification (Analysis 3.10). Using other measures of attachment security (Q‐sort) at post‐intervention, one study found that infants in the intervention group showed significantly less proximity avoidance (SMD ‐1.18, 95% CI ‐1.77 to ‐0.59, P value < 0.0001, Analysis 3.11), but no statistically significant difference for contact resistance (Lieberman 1991). There were no significant differences for attachment security between groups for the Q‐Scale reported at post‐intervention (Analysis 3.12; Cicchetti 1999a).
3.10. Analysis.
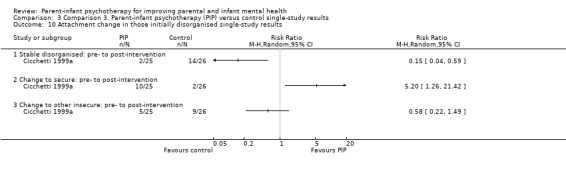
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 10 Attachment change in those initially disorganised single‐study results.
3.11. Analysis.
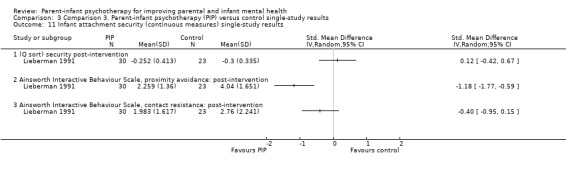
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 11 Infant attachment security (continuous measures) single‐study results.
3.12. Analysis.
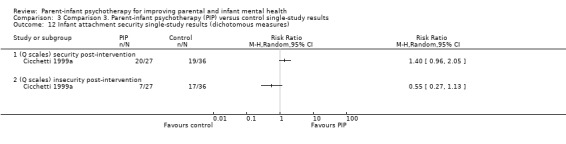
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 12 Infant attachment security single‐study results (dichotomous measures).
3.5 Infant problem behaviours
There was no statistically significant difference between PIP and control group at post‐intervention for any measure of infant problem behaviours (Analysis 3.13) at follow‐up using the scale for angry or externalising behaviours, that is the mean number of instances when a toddler hit, kicked, bit or yelled at mother (Lieberman 1991), or long‐term (five years) follow‐up based on maternal reports (Rutter A2 report) or teacher‐report (PBCL) (Cooper 2003a). There was no significant difference for restriction of affect measured on a seven‐point scale post‐intervention (Lieberman 1991), or total problem and internalising behaviours at 12‐month follow‐up using the CBCL total and internalising scales (Analysis 3.14; Cicchetti 2006b).
3.13. Analysis.
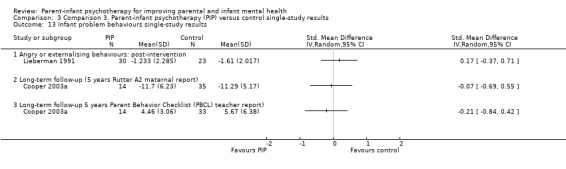
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 13 Infant problem behaviours single‐study results.
3.14. Analysis.
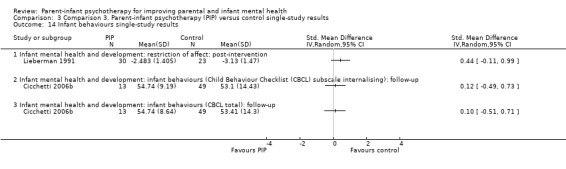
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 14 Infant behaviours single‐study results.
3.6 Infant cognitive development meta‐analysis
There were no statistically significant results for infant cognitive development at 18‐months follow‐up using the BSID MDI (Cooper 2003a), or long‐term follow‐up (measured at five years using the McCarthy Scales of Children's Abilities) (Analysis 3.15; Cooper 2003a). One study reported infant performance IQ and verbal IQ post‐intervention (Analysis 3.16; Cicchetti 1999a). The infants of mothers who had experienced a further episode of depression had significantly different full‐scale and verbal IQ scores at post‐intervention favouring the PIP group (using the WPPSI‐R, full scale IQ: SMD ‐0.99, 95% CI ‐1.77 to ‐0.22; verbal IQ: SMD ‐0.89; 95% CI ‐1.66 to ‐0.12, 30 participants, Analysis 3.17).
3.15. Analysis.
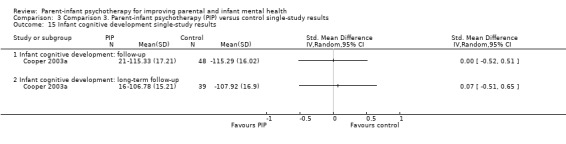
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 15 Infant cognitive development single‐study results.
3.16. Analysis.
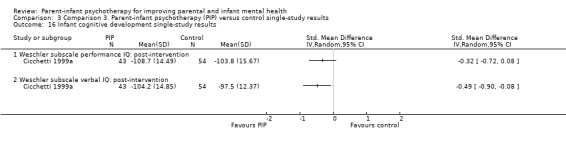
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 16 Infant cognitive development single‐study results.
3.17. Analysis.
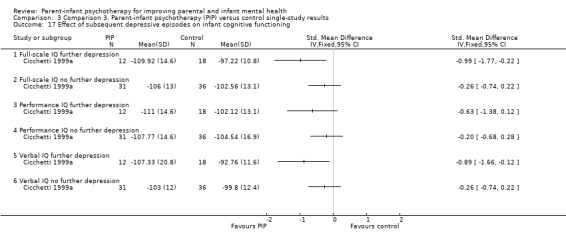
Comparison 3 Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results, Outcome 17 Effect of subsequent depressive episodes on infant cognitive functioning.
Adverse effects
None of the comparisons of PIP with a control group in the above single‐study analyses showed adverse changes attributable to PIP.
Comparison 4. Parent‐infant psychotherapy versus alternative (non‐parent‐infant psychotherapy) intervention (single‐study results only)
Note: in Cohen 1999b, PPT refers to the standard form, that is, PIP and WWW to the infant‐led PIP.
Parent outcomes
Primary parent outcomes
4.1 Parent mental health (depression)
There were no statistically significant results for any measures of parent mental health (depression) in any of our analyses of single‐study data at post‐intervention or follow‐up.
One study reported the number of mothers experiencing subsequent episodes of depression post‐intervention using the DSM‐III‐R at nine‐month follow‐up, 18‐month follow‐up and five‐year follow‐up (Analysis 4.1; Cooper 2003a).
4.1. Analysis.
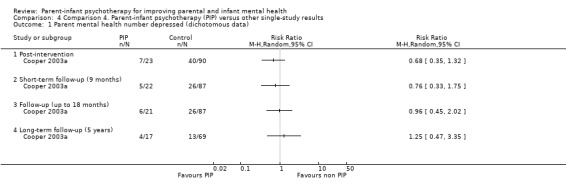
Comparison 4 Comparison 4. Parent‐infant psychotherapy (PIP) versus other single‐study results, Outcome 1 Parent mental health number depressed (dichotomous data).
One study assessed depression using the EPDS at nine‐month follow‐up and at long‐term follow‐up (five years) (Cooper 2003a). Neither analyses favoured PIP or alternative intervention (Analysis 4.2).
4.2. Analysis.
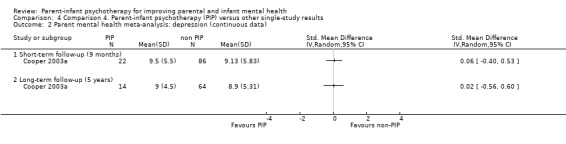
Comparison 4 Comparison 4. Parent‐infant psychotherapy (PIP) versus other single‐study results, Outcome 2 Parent mental health meta‐analysis: depression (continuous data).
4.2 Parenting stress
One study reported parenting stress using the PSI at post‐intervention and follow‐up (Cohen 1999b). None of the analyses for the parent or child domain of this scale showed a statistically significant difference between PIP and alternative intervention (Analysis 4.3).
4.3. Analysis.
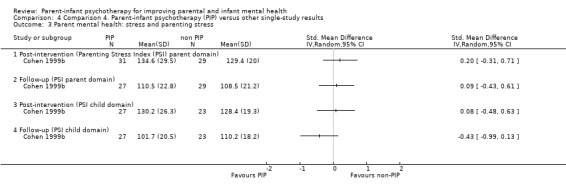
Comparison 4 Comparison 4. Parent‐infant psychotherapy (PIP) versus other single‐study results, Outcome 3 Parent mental health: stress and parenting stress.
Secondary parent outcomes
4.3 Parenting sense of competence
One study reported parent sense of competence using the PSOC scale at post‐intervention and follow‐up (Cohen 1999b). None of the analyses for total satisfaction or total lack of efficacy favoured either PIP or alternative intervention (Analysis 4.4).
4.4. Analysis.
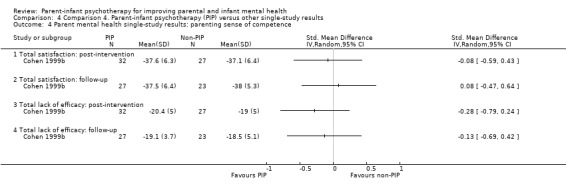
Comparison 4 Comparison 4. Parent‐infant psychotherapy (PIP) versus other single‐study results, Outcome 4 Parent mental health single‐study results: parenting sense of competence.
Parent‐infant interaction
Primary and secondary parent‐infant relationship outcomes
4.4 Parent‐infant interaction: ‐ maternal responsiveness, intrusiveness, and dyadic conflict
There were no statistically significant results for maternal responsiveness or intrusiveness measured at post‐intervention or follow‐up, using the Chatoor Play Scale (Cohen 1999b). However, there was a statistically significant difference for dyadic conflict measured by WWW that favoured the alternative intervention (SMD 0.54, 95% CI 0.01 to 1.07, P value = 0.04, 67 participants, Analysis 4.5).
4.5. Analysis.
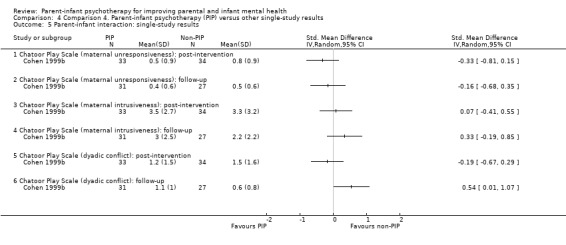
Comparison 4 Comparison 4. Parent‐infant psychotherapy (PIP) versus other single‐study results, Outcome 5 Parent‐infant interaction: single‐study results.
4.5 Mother‐infant relationship or infant behaviour management problems: post‐intervention and follow‐up
One study assessed maternal reports of mother‐infant relationship problems and behaviour management problems at post‐intervention (Cooper 2003a). There were no statistically significantly differences between the groups for the total number reporting problems and those who had initially reported problems and who were still reporting problems after therapy.
There was no statistically significant difference between the groups (WWW and PPT in Cohen 1999b) for maternal perception of problem severity, how effective the mothers felt in dealing with the problem or comfort in dealing with problems. There was no significant difference between PIP and non‐PIP groups for either outcome at post‐intervention or follow‐up (Analysis 4.6; Analysis 4.7).
4.6. Analysis.
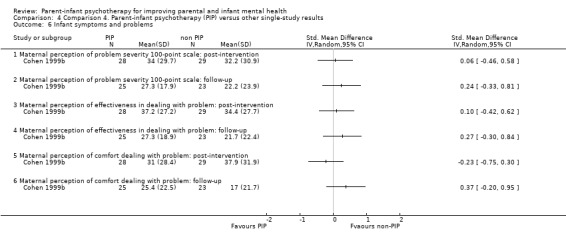
Comparison 4 Comparison 4. Parent‐infant psychotherapy (PIP) versus other single‐study results, Outcome 6 Infant symptoms and problems.
4.7. Analysis.
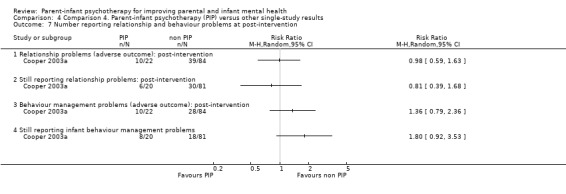
Comparison 4 Comparison 4. Parent‐infant psychotherapy (PIP) versus other single‐study results, Outcome 7 Number reporting relationship and behaviour problems at post‐intervention.
Infant mental health and development
Primary outcomes
4.6 Infant attachment category: change from initially insecure (avoidant ‐ A, resistant ‐ C or disorganised ‐ D): pre‐ to post‐intervention
Using data from Cohen 1999b, which assessed infant attachment category using the SSP, there were no statistically significant differences between the PIP or non‐PIP groups for: 1. the change from initially insecure avoidant or resistant to disorganised; or 2. infants who were initially categorised as disorganised and changed to avoidant or resistant (organised but insecure) (Analysis 4.8). However, 3. insecure (avoidant or resistant) or disorganised to secure and organised (resistant) significantly favoured the WWW group (RR 0.35, 95% CI 0.13 to 0.99, P value = 0.05, 66 participants, Analysis 4.8); and 4. no change or less secure, favoured the PPT group (RR 1.35, 95% CI 1.02 to 1.79, P value = 0.04, 66 participants, Analysis 4.8).
4.8. Analysis.
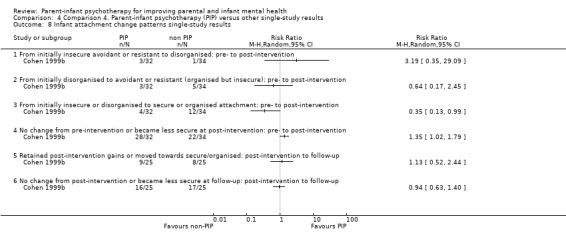
Comparison 4 Comparison 4. Parent‐infant psychotherapy (PIP) versus other single‐study results, Outcome 8 Infant attachment change patterns single‐study results.
There were no statistically significant differences between the groups for participants who had retained post‐intervention gains or moved to a secure or organised attachment (Analysis 4.8).
4.7 Infant behaviours
One study found no statistically significant differences between the groups for angry or externalising behaviours at post‐intervention, which was measured using the Mental Scales of the BSID (i.e. the Bayley Infant Behavior Rating Scale, subscale Emotion Regulation) (Cohen 1999b). In addition, there were no statistically significant differences between the groups in the total infant behaviour and internalising behaviour at six‐month follow‐up measured using the CBCL (Cicchetti 2006b), or for long‐term follow‐up using the PBCL teacher report at five years, or the Rutter A2 maternal report at five years (Cooper 2003a) (Analysis 4.9).
4.9. Analysis.
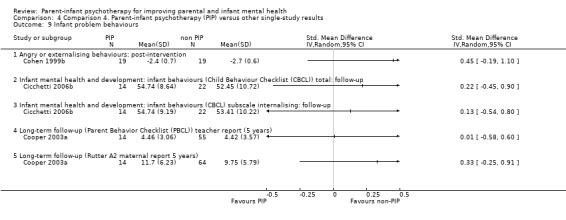
Comparison 4 Comparison 4. Parent‐infant psychotherapy (PIP) versus other single‐study results, Outcome 9 Infant problem behaviours.
Secondary outcomes
4.8 Infant cognitive development
There were no statistically significant differences between the groups for infant cognitive development (infant competence measured using the BSID MDI at post‐intervention (Cohen 1999b), or at long‐term (five‐year) follow‐up using the McCarthy General Cognitive Index (GCI) (Cooper 2003a) (Analysis 4.10), or when infant cognitive development was assessed in infants with and without developmental delay at post‐intervention using the BSID MDI (Cohen 1999b) (Analysis 4.11).
4.10. Analysis.
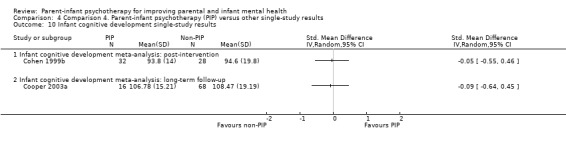
Comparison 4 Comparison 4. Parent‐infant psychotherapy (PIP) versus other single‐study results, Outcome 10 Infant cognitive development single‐study results.
4.11. Analysis.
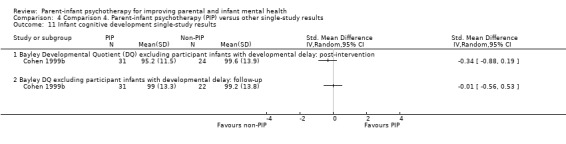
Comparison 4 Comparison 4. Parent‐infant psychotherapy (PIP) versus other single‐study results, Outcome 11 Infant cognitive development single‐study results.
Adverse effects
None of the comparisons of PIP with a treatment group in the above single study analyses showed adverse changes attributable to PIP, other than a difference between PIP ('PPT') and an alternative intervention (infant‐led WWW) for change in infant attachment (see 4.6 Infant attachment category: change from initially insecure). From pre‐ to post‐intervention, more infants in the PPT group stayed in the same attachment category or became less secure from pre‐ to post‐intervention (RR 1.35, 95% CI 1.02 to 1.79, P value = 0.04, 66 participants, Analysis 4.8; Cohen 1999b).
Sensitivity analyses: parent‐infant psychotherapy versus control, sensitivity analyses assuming different values of intraclass correlation coefficient
We conducted sensitivity analyses assuming different values of ICC (i.e. using an imputed ICC: 0.2, 0.4, 0.6, 0.8) in the cluster‐randomised trial (Sleed 2013a). The overall result of the analysis was robust to the use of imputed ICCs.
Parent outcomes
Primary parent outcomes
5.1 Parent mental health: depression (dichotomous data) post‐intervention
There were no significant differences between PIP and control groups (RR 0.69, 95% CI 0.46 to 1.03 if ICC = 0.2; RR 0.67, 95% CI 0.44 to 1.03 if ICC = 0.4; RR 0.67, 95% CI 0.43 to 1.03 if ICC = 0.6; RR 0.66, 95% CI 0.42 to 1.03 if ICC = 0.8, Analysis 5.1).
5.1. Analysis.
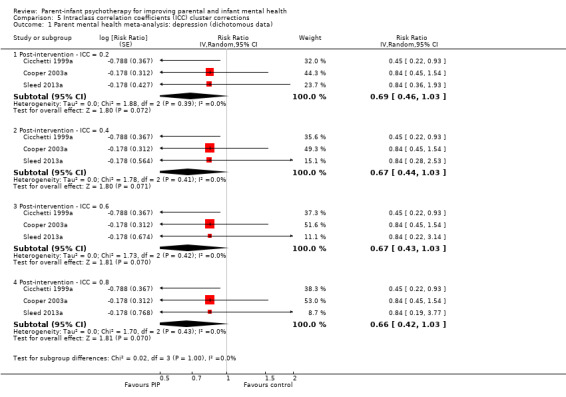
Comparison 5 Intraclass correlation coefficients (ICC) cluster corrections, Outcome 1 Parent mental health meta‐analysis: depression (dichotomous data).
5.2 Parent mental health: depression (continuous data) post‐intervention
There were no significant differences between PIP and control groups (SMD ‐0.22, 95% CI ‐0.47 to 0.03 if ICC = 0.2; SMD ‐0.24, 95% CI ‐0.52 to 0.05 if ICC = 0.4; SMD ‐0.24 with 95% CI ‐0.53 to 0.05 if ICC = 0.6; SMD ‐0.24 with 95% CI ‐0.53 to 0.05 if ICC = 0.8, Analysis 5.2).
5.2. Analysis.
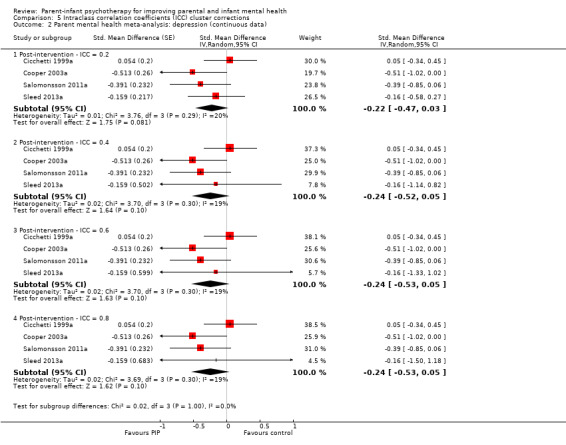
Comparison 5 Intraclass correlation coefficients (ICC) cluster corrections, Outcome 2 Parent mental health meta‐analysis: depression (continuous data).
Secondary parent outcomes
5.3 Maternal sensitivity meta‐analysis: post‐intervention
There were no significant differences between PIP and control groups (SMD ‐0.16, 95% CI ‐0.65 to 0.32 if ICC = 0.2; SMD ‐0.19, 95% CI ‐0.67 to 0.29 if ICC = 0.4; SMD ‐0.22, 95% CI ‐0.69 to 0.26 if ICC = 0.6; SMD ‐0.23, 95% CI ‐0.71 to 0.25 if ICC = 0.8, Analysis 5.3).
5.3. Analysis.
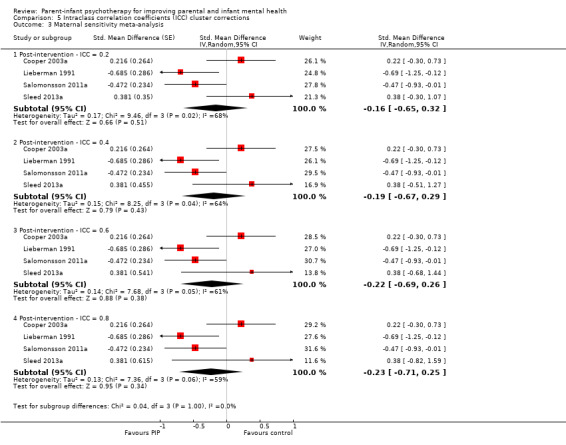
Comparison 5 Intraclass correlation coefficients (ICC) cluster corrections, Outcome 3 Maternal sensitivity meta‐analysis.
Parent‐infant relationship outcomes
Primary and secondary parent‐infant relationship outcomes
5.4 Child involvement meta‐analysis: post‐intervention
There were no significant differences between PIP and control groups (SMD ‐0.07, 95% CI ‐0.46 to 0.32 if ICC = 0.2; SMD ‐0.09, 95% CI ‐0.50 to 0.33 if ICC = 0.4; SMD ‐0.09, 95% CI ‐0.52 to 0.33 if ICC = 0.6; SMD ‐0.10, 95% CI ‐0.53 to 0.33 if ICC = 0.8, Analysis 5.4).
5.5 Maternal positive engagement meta‐analysis: post‐intervention
There were no significant differences between PIP and control groups (SMD ‐0.23, 95% CI ‐0.55 to 0.09 if ICC = 0.2; SMD ‐0.25, 95% CI ‐0.58 to 0.08 if ICC = 0.4; SMD ‐0.26, 95% CI ‐0.60 to 0.07 if ICC = 0.6; SMD ‐0.27, 95% CI ‐0.60 to 0.07 if ICC = 0.8, Analysis 5.5).
5.5. Analysis.
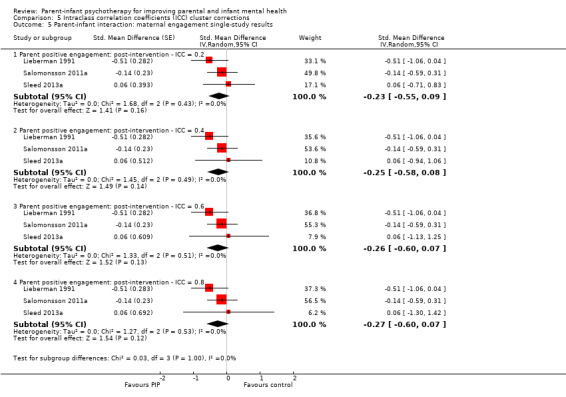
Comparison 5 Intraclass correlation coefficients (ICC) cluster corrections, Outcome 5 Parent‐infant interaction: maternal engagement single‐study results.
Sensitivity analyses: parent‐infant psychotherapy versus control, fixed‐effect versus random‐effects meta‐analyses
Overall, there was little difference between point estimates for analyses using fixed‐effect or random‐effects meta‐analyses with the exception of the following outcomes.
Parent outcomes
Primary parent outcomes
6.1 Parent mental health: depression (dichotomous data) post‐intervention
A fixed‐effect meta‐analysis found a statistically significant difference between PIP and control groups on the depression outcomes favouring PIP at post‐intervention (fewer depressed parents in PIP group: RR 0.72, 95% CI 0.53 to 0.99 for the dichotomous depression outcomes; lower depression scores in PIP group: SMD ‐0.21, 95% CI ‐0.42 to 0.00 for the continuous depression outcomes; analyses not shown).
Infant mental health and development
Primary outcomes
6.2 Infant attachment category: change from initially insecure
Using a fixed‐effect meta‐analysis, there was a statistically significant difference in children who remained stably insecure at post‐intervention favouring the control group (RR 0.57, 95% CI 0.38 to 0.87; analyses not shown).
Discussion
Summary of main results
Overall
We included eight studies (846 participants), four compared PIP with control groups only (Cicchetti 1999a; Lieberman 1991; Salomonsson 2011a; Sleed 2013a), and four compared PIP with another treatment. of the four comparing PIP with another treatment, one compared a representative PPT with an 'infant‐led' PIP (WWW) (Cohen 1999b); one compared PIP with interaction guidance (Robert‐Tissot 1996a); one comprised three arms permitting a comparison of PIP with both a no‐treatment community control group and a psychoeducational parent training programme (Cicchetti 2006b); and one employed a randomised four‐arm comparison of PIP, CBT, non‐directive counselling, and routine primary care (in which, for the purposes of this review, we aggregated data from the counselling and CBT arms (non‐psychodynamic interventions; Cooper 2003a).
All eight studies provided post‐intervention data. Three studies provided follow‐up data at six and 12 months (Cicchetti 2006b; Cohen 1999b; Cooper 2003a), and one study provided long‐term (five‐year) follow‐up data (Cooper 2003a).
When describing the null findings for most of the outcomes synthesised in the review, it should be noted that these provide no evidence of an effect (rather than evidence of no effect) and may be due to low statistical power given the small number of included studies and the imprecision in the random‐effects variance component. Where we report statistical significance, the statistic is reliable but it cannot be inferred that the finding is clinically important or that it should be the sole factor taken into account in decision‐making.
Parent‐infant psychotherapy versus control group
Six studies contributed data to the PIP versus control comparisons producing 19 meta‐analyses measuring the primary outcomes of: parental depression (both dichotomous and continuous data at post‐intervention); measures of the parent‐infant relationship, including the primary outcomes of maternal sensitivity, parent engagement and child involvement at post‐intervention; primary infant outcomes of attachment category at post‐intervention and follow‐up (secure, avoidant, disorganised, resistant), attachment change (insecure to secure, stable secure, secure to insecure, stable insecure); and infant behaviour at follow‐up. The studies also provided data for analyses of the secondary outcomes of infant cognitive development at post‐intervention.
The results showed no clear evidence of improvements in incidence of parental depression or parent‐reported levels of depression, and no clear evidence of a difference for parent‐infant interaction (i.e. maternal sensitivity, child involvement and parent engagement). There were improvements in the proportion of infants securely attached at post‐intervention and a reduction in the number of infants with an avoidant attachment at post‐intervention; there were also significantly fewer infants with disorganised attachment at post‐intervention. Four meta‐analyses were produced with follow‐up data and showed significantly more PIP infants who were categorised as secure, and significantly fewer infants who were avoidant. There was no clear evidence of a difference favouring either the intervention group or the controls group for resistant attachment, and no evidence of effectiveness in reducing the numbers of infants with a disorganised attachment style. There was an increase in the proportion of children moving from insecure at pre‐intervention to secure attachment at post‐intervention favouring PIP. There were no differences between the groups for infant behaviour, or infant cognitive development (see Table 1).
Parent‐infant psychotherapy versus alternative treatment
Four studies contributed data to the PIP versus alternative treatment analyses producing 15 meta‐analyses measuring the primary outcomes of parent mental health (depression); the parent‐infant interaction outcome of maternal sensitivity, and the primary infant outcomes of attachment category (secure, avoidant, resistant, disorganised) and attachment change (insecure to secure, stable insecure), although meta‐analysis was not possible for infants who were stable secure, or those who changed from secure to insecure (i.e. because no events occurred in the PIP group) or for infant behaviour. Meta‐analysis was possible for the secondary outcome of infant cognitive development. None of the meta‐analyses for primary or secondary outcomes of PIP versus alternative treatment at post‐intervention or follow‐up showed significant differences in outcome between PIP and alternative treatment interventions (see Table 2).
Adverse effects
Overall, this review found little evidence of adverse effects. Three of the included studies assessed whether PIP had adverse effects in terms of infant attachment security (i.e. the extent to which infants who were securely attached at baseline were categorised as insecure at post‐intervention or follow‐up) (Cicchetti 1999a; Cicchetti 2006b; Cohen 1999b). In our meta‐analyses, none of the comparisons of PIP with either a control or comparison treatment group showed adverse changes for infant attachment or any other outcome. However, results of an analysis from only one study showed a difference between PIP and an alternative intervention (infant‐led WWW) for adverse effects (Cohen 1999b). From pre‐ to post‐intervention, more infants in the PIP group stayed in the same attachment category or became less secure from pre‐ to post‐intervention.
Overall completeness and applicability of evidence
The data presented here are complete for the published studies that were identified. We were also able to identify five ongoing studies evaluating the effectiveness of PIPs that have not yet reported, and the results from these will be included at the next update.
In terms of the applicability of the evidence, there was some variation in the type of PIP being evaluated, including two types of infant‐led psychotherapy (Cohen 1999b; Salomonsson 2011a), in addition to the standard representational types of therapy. The duration of intervention also varied (i.e. ranging from eight sessions in Sleed 2013a to up to 49 weeks in Cicchetti 2006b), as did the content and focus. For example, the focus varied from child attachment in the context of maltreating families (Cicchetti 2006b), maternal depression or mothers' feelings of failure in bonding with their infant (Cicchetti 1999a; Cohen 1999b; Cooper 2003a), parental psychosocial functioning and the parent‐child relationship (e.g. Cooper 2003a; Lieberman 1991; Sleed 2013a), and functional and behavioural problems in children (Cohen 1999b; Robert‐Tissot 1996a). The target populations were diverse, including depressed women, anxiously attached dyads, maltreating parents and incarcerated women, and there was little consistency in the outcomes measured or clarity about the relationship between outcomes and programme mechanisms. This variability was manifest in high levels of statistical heterogeneity for some of the meta‐analyses that we conducted, including some of the measures of attachment that we found to be significant.
Quality of the evidence
We included eight studies comprising 846 initially randomised participants. Our risk of bias estimates show that overall the quality of the included studies was poor (Figure 2; Figure 3). Many studies had limitations in their design or implementation or were unclear about important quality criteria, including randomisation, and were at high risk for allocation concealment, sequence generation and blinding. It should be noted that all of the studies were judged at high risk of performance bias because it is not possible to blind participants and personnel in studies of this nature. Many studies did not provide adequate information for assessment of these domains. In two studies, the intervention groups were combined (Cicchetti 2006b; Robert‐Tissot 1996a). In all cases of uncertainly, we attempted to obtain further information or disaggregated data from the trial investigator, but, where this was not available, it was because the investigator no longer had access to historical trial data or was unable to provide additional information.
None of the included studies conformed with the CONSORT (Consolidated Standards of Reporting Trials) reporting requirements for an RCT (Schulz 2010). We rated the overall quality of the evidence as low or very low for the key outcomes of parental depression and secure or disorganised infant attachment (Table 1; Table 2), resulting in lower confidence in the estimate of effect for those outcomes. Where we downgraded the evidence, it was because there was risk of bias in the trial, out of six estimates of potential bias (random sequence generation, allocation concealment, incomplete outcome data, selective reporting, blinding of participants and personnel, blinding of outcome assessment), only two studies obtained scores of four or more. The included studies involved relatively few participants and wide CIs (imprecision), although it is accepted that large‐scale community studies of this type would be very difficult to perform due to the one‐to‐one nature of the intervention. The results of many meta‐analyses had moderate to high levels of statistical heterogeneity (inconsistency). One explanation for this may be the clinical heterogeneity between the trials, with trials having different aims, participants (depressed parent, infants at risk of abuse or insecure attachment, prison populations, community samples), methods of delivery (i.e. individual or group‐based), and primary outcome measures, for example, parent (maternal) mental health (depression) and infant attachment. This clinical heterogeneity that was present in the eight included studies, alongside the limited available evidence, precluded us from reaching any firm conclusions about the effectiveness of PIPs.
Potential biases in the review process
Potential biases in the review process were limited. We estimated the SMD by calculating the treatment effect for each outcome in each study by dividing the MD in post‐intervention scores for the intervention and treatment groups by the pooled standard deviation. However, it should be noted that random allocation does not guarantee equality of means between groups at pre‐test, and also that post‐test standard deviation may be inflated by a differential response to intervention, and may underestimate the effect size attributable to the intervention.
In addition, we did not take into account the possibility of ICC that can occur in group interventions. Although we corrected for unit analysis issues arising from cluster‐randomisation, we did not investigate further the clustering effect of individually randomised trials with group delivered therapies. This could mean that we have overestimated the significance of the findings.
We contacted the study investigators to provide missing data, but where this was not provided, we did not choose to impute missing data for two reasons. In terms of dichotomous data, there was no clear judgement about the value of performing sensitivity analyses based on best‐case/worst‐case scenarios or their alternative. For continuous data, we would have required access to the raw data (i.e. in order to impute missing data by using the last‐observation‐carried‐forward). Therefore, the analysis was limited to outcomes for which published data were available.
We had planned to carry out additional subgroup analyses to explore the programme components that appeared to be associated with more effective outcomes, and factors that modified intervention effectiveness, but there were too few included studies in each meta‐analysis to do this. There were similarly too few studies to conduct sensitivity analyses to examine the impact of study design or quality.
Agreements and disagreements with other studies or reviews
To date, there has been only two systematic reviews of parent‐infant (Singleton 2004) or attachment‐based (Bakermans‐Kranenburg 2003) therapies.
The first included 25 studies of parent‐infant therapies with children from birth to 36 months of age, but included studies that were not RCTs, alongside diverse populations (e.g. low birthweight babies, low‐income families, infants with cerebral palsy) and diverse interventions (e.g. infant massage, home visiting, PIP) (Singleton 2004). The results showed significant improvements in infant mental health (d = 0.28, where d is the effect size (Cohen 1977)), parent‐infant relationship (d = 0.56), parent ability (d = 1.65), but not infant development (d = ‐0.06) with significant heterogeneity for all meta‐analyses.
The second review included 70 studies assessing the effectiveness of a diverse range of attachment interventions, including PIP, video‐interaction guidance, social support, etc. (Bakermans‐Kranenburg 2003). The results showed that attachment‐based interventions appeared to be effective in reducing insensitive parenting (d = 0.33) and infant attachment insecurity (d = 0.20). The most effective interventions used a moderate number of sessions and a clear‐cut behavioural focus in families with, as well as without, multiple problems. Interventions that were more effective in enhancing parental sensitivity were also more effective in enhancing attachment security, which supports the notion of a causal role of sensitivity in shaping attachment. In our review, there was no difference in attachment outcomes between PIP versus alternative treatment group, and the reasons for this were unclear. Some non‐psychodynamic interventions are relationship‐based and it may be that interventions of any type that promote parental sensitivity result in more secure infant attachment without the need for further input that specifically targets infant attachment.
It is difficult to assess the degree of consistency between the findings of the current review and the two earlier reviews because neither review disaggregated the effects for different intervention types, and positive effects, therefore, may be due to intervention components other than PIP (Bakermans‐Kranenburg 2003;Singleton 2004).
Authors' conclusions
Implications for practice.
The results of this review suggest that parent‐infant psychotherapy (PIP) is a promising model in terms of improving infant attachment security in high‐risk populations, including maltreatment and prisons, but that there is currently limited evidence of benefit across many other outcomes measured, including maternal representations and parent‐infant interaction. Several studies were lacking in rigour, and there was significant statistical heterogeneity affecting some of the key outcomes, suggesting the need for caution when interpreting these findings.
With regard to the effectiveness of PIP relative to other methods of working, the evidence is again inconclusive, partly as a result of the diverse interventions with which PIP was compared. While early evidence suggested that interventions for parent mental health problems, such as depression, which did not contain specific components that explicitly target parent‐infant interaction were not effective, the data from this review have suggested that PIP has not yet been demonstrated to be superior to other methods of working with high‐risk groups of parents, for reasons that are unclear and that there is an urgent need for further high‐quality research.
None of the included studies provided data regarding the cost of implementing PIP or its cost‐effectiveness relative to other methods of intervening.
Implications for research.
Further rigorous research is needed in the form of high‐quality primary studies that make use of adequate methods of random allocation and that minimise bias in their conduct and reporting. There is also a need to establish whether the current findings can be replicated with other groups of parent‐infant dyads, and to identify the mechanisms of change. Existing research suggests that parental reflective functioning and interactive regulation are key to the development of attachment security in infants, but the limited data available in the current review found no evidence of an impact on mediatory factors such as parent‐infant interaction or reflective functioning. Future research should identify a set of core outcomes for both parents and infants that would facilitate comparisons between different studies, and that would improve our ability to assess whether this intervention has an impact in terms of key moderating variables. Further research is also needed to assess the impact of PIP on father‐infant dyads or mother‐father‐infant triads. The included studies in this review were all conducted in high‐income northern hemisphere countries, albeit with different population groups, and future studies should evaluate the impact of relationship‐based interventions in lower‐income countries.
There is a lack of consensus about what a core PIP model should involve, with considerable evolution of the basic model (e.g. introduction of video‐interaction guidance and infant massage, etc.) in the absence of evidence regarding the benefits of the core PIP model compared with treatment‐as‐usual.
Future studies should aim to identify the active components involved in PIP, and compare standard PIP models with variations on the core PIP model of working, including attachment‐based components for which there is already evidence of benefit with high‐risk groups (e.g. video‐interaction guidance).
Similarly, studies comparing alternative interventions should also include a control arm, and should focus on attachment‐based interventions for which there is already evidence of benefit with high‐risk groups (e.g. video‐interaction guidance), in addition to variations on the core PIP model of working.
Future comparative studies should also aim to address whether different forms of therapy may be differentially effective for parents with different types of attachment insecurity (Bakermans‐Kranenburg 1998), and provide cost‐effectiveness data.
Acknowledgements
We acknowledge the financial support provided by PIP UK (see below for further information) to undertake this review, and the administrative and research support of the Cochrane Developmental, Psychosocial and Learning Problems Group and the Campbell Collaboration in undertaking this review.
This review is co‐registered within the Campbell Collaboration and a version of it appears on The Campbell Library.
We gratefully acknowledge the additional data and information provided to us by the study investigators, Prof Christiane Robert‐Tissot, Prof Alice Lieberman, Prof Lynne Murray and Prof Peter Cooper, Prof Nancy Cohen, Prof Dante Cicchetti, Dr Fred Rogosch, and Dr Michelle Sleed.
Ms Soili Larkin provided additional data extraction and data entry support to the review.
Dr Yinghui Wei carried out intraclass correlation coefficient analyses and provided statistical advice.
Appendices
Appendix 1. Search strategies
Cochrane Central Register of Controlled Trials (CENTRAL)
#1 MeSH descriptor: [Psychotherapy] explode all trees
#2 MeSH descriptor: [Psychoanalytic Therapy] explode all trees
#3 MeSH descriptor: [Psychotherapeutic Processes] explode all trees
#4 MeSH descriptor: [Psychotherapy, Brief] explode all trees
#5 MeSH descriptor: [Psychotherapy, Multiple] this term only
#6 MeSH descriptor: [Psychotherapy, Rational‐Emotive] this term only
#7 MeSH descriptor: [Socioenvironmental Therapy] explode all trees
#8 MeSH descriptor: [Psychoanalytic Interpretation] this term only
#9 (psychotherap* or psycho‐therap* or psychoanalytic* or psycho‐analytic* or psychodynamic* or psycho‐dynamic*):ti,ab,kw (Word variations have been searched)
#10 MeSH descriptor: [Family Therapy] this term only
#11 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10
#12 MeSH descriptor: [Maternal Behavior] explode all trees
#13 MeSH descriptor: [Parent‐Child Relations] explode all trees
#14 MeSH descriptor: [Parenting] this term only
#15 MeSH descriptor: [Paternal Behavior] this term only
#16 MeSH descriptor: [Mothers] this term only and with qualifiers: [Psychology ‐ PX]
#17 MeSH descriptor: [Fathers] this term only and with qualifiers: [Psychology ‐ PX]
#18 MeSH descriptor: [Parents] this term only
#19 MeSH descriptor: [Object Attachment] this term only
#20 MeSH descriptor: [Reactive Attachment Disorder] this term only
#21 ((attachment near/3 disorder*) or (insecure near/3 attachment*) or (secure near/3 attachment*) or (dysregulation near/3 disorder*)):ti,ab,kw (Word variations have been searched)
#22 (parent* or mother* or maternal* or father* or paternal* or infant* or child*) near/3 (attachment* or bond* or interaction* or relationship* or dyad* or triad*):ti,ab,kw (Word variations have been searched)
#23 #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22
#24 MeSH descriptor: [Infant] explode all trees
#25 MeSH descriptor: [Infant Behavior] this term only
#26 (baby or babies or infant* or child* or toddler*):ti,ab,kw (Word variations have been searched)
#27 #24 or #25 or #26
#28 #11 and #23 and #27
#29 ((parent* or mother* or maternal* or father* or paternal*) near/3 (baby or babies or infant* or child* or toddler*) near/3 (psychother* or psycho‐therap* or psychodynamic* or psycho‐dynamic*)):ti,ab,kw (Word variations have been searched)
#30 ((parent* or mother* or maternal* or father* or paternal*) near/3 (baby or babies or infant* or child* or toddler*) near/3 (psychoanalytic* or psycho‐analytic* or psychodynamic* or psycho‐dynamic*)):ti,ab,kw (Word variations have been searched)
#31 #29 or #30
#32 #28 or #31
Ovid MEDLINE
1 psychotherapy/ or exp psychoanalytic therapy/ or exp psychotherapeutic processes/ or psychotherapy, brief/ or psychotherapy, multiple/ or psychotherapy, rational‐emotive/ or exp socioenvironmental therapy/
2 Psychoanalytic Interpretation/
3 (psychotherap$ or psycho‐therap$ or psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$).tw.
4 Family Therapy/
5 or/1‐4
6 exp maternal behavior/ or parent‐child relations/ or father‐child relations/ or mother‐child relations/ or parenting/ or paternal behavior/
7 Mothers/px or Fathers/px or Parents/px
8 Object Attachment/
9 Reactive Attachment Disorder/
10 ((attachment adj3 disorder$) or (insecure adj3 attachment$) or (secure adj3 attachment$) or (dysregulation adj3 disorder$)).tw.
11 ((parent$ or mother$ or maternal$ or father$ or paternal$ or infant$ or child$) adj3 (attachment$ or bond$ or interaction$ or relationship$ or dyad$ or triad$)).tw.
12 or/6‐11
13 exp infant/
14 infant behavior/
15 (baby or babies or infant$ or child$ or toddler$).tw.
16 or/13‐15
17 5 and 12 and 16
18 (parent$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw.
19 (mother$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw.
20 (maternal$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw.
21 (father$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw.
22 (paternal$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw.
23 (parent$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw.
24 (mother$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw.
25 (maternal$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw.
26 (father$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw.
27 (paternal$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw.
28 or/18‐27
29 17 or 28
30 randomized controlled trial.pt.
31 controlled clinical trial.pt.
32 randomized.ab.
33 placebo.ab.
34 drug therapy.fs.
35 randomly.ab.
36 trial.ab.
37 groups.ab.
38 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37
39 exp animals/ not humans.sh.
40 38 not 39
41 29 and 40
EMBASE (Ovid)
1. psychotherapy/ or exp psychoanalytic therapy/ or exp psychotherapeutic processes/ or psychotherapy, brief/ or psychotherapy, multiple/ or psychotherapy, rational‐emotive/ or exp socioenvironmental therapy/ 2. Psychoanalytic Interpretation/ 3. (psychotherap$ or psycho‐therap$ or psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$).tw. 4. Family Therapy/ 5. or/1‐4 6. exp maternal behavior/ or parent‐child relations/ or father‐child relations/ or mother‐child relations/ or parenting/ or paternal behavior/ 7. Object Attachment/ 8. Reactive Attachment Disorder/ 9. ((attachment adj3 disorder$) or (insecure adj3 attachment$) or (secure adj3 attachment$) or (dysregulation adj3 disorder$)).tw. 10. ((parent$ or mother$ or maternal$ or father$ or paternal$ or infant$ or child$) adj3 (attachment$ or bond$ or interaction$ or relationship$ or dyad$ or triad$)).tw. 11. or/6‐10 12. exp infant/ 13. infant behavior/ 14. (baby or babies or infant$ or child$ or toddler$).tw. 15. or/12‐14 16. 5 and 11 and 15 17. (parent$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw. 18. (mother$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw. 19. (maternal$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw. 20. (father$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw. 21. (paternal$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw. 22. (parent$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw. 23. (mother$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw. 24. (maternal$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw. 25. (father$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw. 26. (paternal$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw. 27. or/17‐26 28. 16 or 27 29. random$.tw. 30. factorial$.tw. 31. crossover$.tw. 32. cross over$.tw. 33. cross‐over$.tw. 34. placebo$.tw. 35. (doubl$ adj blind$).tw. 36. (singl$ adj blind$).tw. 37. assign$.tw. 38. allocat$.tw. 39. volunteer$.tw. 40. Crossover Procedure/ 41. double‐blind procedure.tw. 42. Randomized Controlled Trial/ 43. Single Blind Procedure/ 44. or/29‐43 45. (animal/ or nonhuman/) not human/ 46. 44 not 45 47. 28 and 46
CINAHL (EBSCO)
S24 S20 OR S23
S23 S21 OR S22
S22 ((parent* or mother* or maternal* or father* or paternal*) N3 (baby or babies or infant* or child* or toddler*) N3 (psychoanalytic* or psycho‐analytic* or psychodynamic* or psycho‐dynamic*))
S21 ((parent* or mother* or maternal* or father* or paternal*) N3 (baby or babies or infant* or child* or toddler*) N3 (psychother* or psycho‐therap* or psychodynamic* or psycho‐dynamic*))
S20 S4 AND S15 AND S19
S19 S16 OR S17 OR S18
S18 (baby or babies or infant* or child* or toddler*)
S17 (MH "Infant Behavior")
S16 (MH "Infant+")
S15 S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14
S14 (parent* or mother* or maternal* or father* or paternal* or infant* or child*) N3 (attachment* or bond* or interaction* or relationship* or dyad* or triad*)
S13 ((attachment N3 disorder*) or (insecure N3 attachment*) or (secure N3 attachment*) or (dysregulation N3 disorder*))
S12 (MH "Reactive Attachment Disorder")
S11 (MH "Parents")
S10 (MH "Fathers")
S9 (MH "Mothers")
S8 (MH "Paternal Behavior")
S7 (MH "Parenting")
S6 (MH "Parent‐Child Relations+")
S5 (MH "Maternal Behavior")
S4 S1 OR S2 OR S3
S3 (MH "Family Therapy")
S2 (psychotherap* or psycho‐therap* or psychoanalytic* or psycho‐analytic* or psychodynamic* or psycho‐dynamic*)
S1 (MH "Psychotherapy") OR (MH "Psychotherapeutic Processes+") OR (MH "Psychotherapy, Brief")
PsycINFO (Ovid)
1 psychotherapy/ or exp psychoanalytic therapy/ or exp psychotherapeutic processes/ or psychotherapy, brief/ or psychotherapy, multiple/ or psychotherapy, rational‐emotive/ or exp socioenvironmental therapy/ (104467)
2 Psychoanalytic Interpretation/ (9695)
3 (psychotherap$ or psycho‐therap$ or psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$).tw. (146964)
4 Family Therapy/ (17803)
5 or/1‐4 (198219)
6 exp maternal behavior/ or parent‐child relations/ or father‐child relations/ or mother‐child relations/ or parenting/ or paternal behavior/ (43042)
7 Attachment behavior/ (14546)
8 Reactive Attachment Disorder/ (432)
9 ((attachment adj3 disorder$) or (insecure adj3 attachment$) or (secure adj3 attachment$) or (dysregulation adj3 disorder$)).tw. (4317)
10 ((parent$ or mother$ or maternal$ or father$ or paternal$ or infant$ or child$) adj3 (attachment$ or bond$ or interaction$ or relationship$ or dyad$ or triad$)).tw. (57962)
11 [or/6‐11(0)] Error corrected in line 27
12 infant development/ (13025)
13 (baby or babies or infant$ or child$ or toddler$).tw. (545430)
14 or/12‐13 (545817)
15 [5 and 11 and 14 (0)] Error corrected in line 28
16 (parent$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw. (547)
17 (mother$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw. (184)
18 (maternal$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw. (16)
19 (father$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw. (19)
20 (paternal$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychother$ or psycho‐therap$ or psychodynamic$ or psycho‐dynamic$)).tw. (0)
21 (parent$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw. (121)
22 (mother$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw. (106)
23 (maternal$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw. (4)
24 (father$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw. (17)
25 (paternal$ adj3 (baby or babies or infant$ or child$ or toddler$) adj3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$)).tw. (1)
26 or/16‐25 (862)
27 or/6‐11 (87434)
28 5 and 27 and 14 (6395)
29 26 or 28 (6736)
30 clinical trials/ (6560)
31 (randomis* or randomiz*).tw. (41195)
32 (random$ adj3 (allocat$ or assign$)).tw. (27153)
33 ((clinic$ or control$) adj trial$).tw. (34970)
34 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw. (18319)
35 (crossover$ or "cross over$").tw. (6424)
36 random sampling/ (563)
37 Experiment Controls/ (649)
38 Placebo/ (3380)
39 placebo$.tw. (28872)
40 exp program evaluation/ (15216)
41 treatment effectiveness evaluation/ (14233)
42 ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw. (51687)
43 or/30‐42 (165354)
44 29 and 43 (202)
BIOSIS Citation Index and Social Science Citation Index (Web of Science)
#27 #26 AND #18
#26 #25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19
#25 Topic=(("random* allocat*") or ("random* assign*"))
#24 Topic=(crossover)
#23 Topic=(("tripl* blind*") or ("tripl* mask*"))
#22 Topic=(("trebl* blind*") or ("trebl* mask*"))
#21 Topic=(("doubl* blind*") or ("doubl* mask*"))
#20 Topic=(("singl* blind*") or ("singl* mask*"))
#19 Topic=(("clin* trial*"))
#18 #17 OR #6
#17 #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 OR #7
#16 Topic=(((parent* near/3 (baby or babies or infant* or child* or toddler*) near/3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$))))
#15 Topic=(((mother* near/3 (baby or babies or infant* or child* or toddler*) near/3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$))))
#14 Topic=(((maternal* near/3 (baby or babies or infant* or child* or toddler*) near/3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$))))
#13 Topic=(((father* near/3 (baby or babies or infant* or child* or toddler*) near/3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$))))
#12 Topic=(((paternal* near/3 (baby or babies or infant* or child* or toddler*) near/3 (psychoanalytic$ or psycho‐analytic$ or psychodynamic$ or psycho‐dynamic$))))
#11 Topic=(((paternal* near/3 (baby or babies or infant* or child* or toddler*) near/3 (psychother* or psycho‐therap* or psychodynamic* or psycho‐dynamic*))))
#10 Topic=(((father* near/3 (baby or babies or infant* or child* or toddler*) near/3 (psychother* or psycho‐therap* or psychodynamic* or psycho‐dynamic*))))
#9 Topic=((maternal* near/3 (baby or babies or infant* or child* or toddler*) near/3 (psychother* or psycho‐therap* or psychodynamic* or psycho‐dynamic*)))
#8 Topic=((mother* near/3 (baby or babies or infant* or child* or toddler*) near/3 (psychother* or psycho‐therap* or psychodynamic* or psycho‐dynamic*)))
#7 Topic=((parent* near/3 (baby or babies or infant* or child* or toddler*) near/3 (psychother* or psycho‐therap* or psychodynamic* or psycho‐dynamic*)))
#6 #5 AND #4 AND #1
#5 Topic=((baby or babies or infant* or child* or toddler*))
#4 #3 OR #2
#3 Topic=(((parent* or mother* or maternal* or father* or paternal* or infant* or child*) near/3 (attachment* or bond* or interaction* or relationship* or dyad* or triad*)))
#2 Topic=(((attachment near/3 disorder*) or (insecure near/3 attachment*) or (secure near/3 attachment*) or (dysregulation near/3 disorder*)))
#1 Topic=((psychotherap* or psycho‐therap* or psychoanalytic* or psycho‐analytic* or psychodynamic* or psycho‐dynamic* or "family therap*"))
ERIC (ProQuest)
(((all((((parent* OR mother* OR maternal* OR father* OR paternal*) NEAR/3 (baby OR babies OR infant* OR child* OR toddler*) NEAR/3 (psychother* OR psycho‐therap* OR psychodynamic* OR psycho‐dynamic*)))) OR all((((parent* OR mother* OR maternal* OR father* OR paternal*) NEAR/3 (baby OR babies OR infant* OR child* OR toddler*) NEAR/3 (psychoanalytic* OR psycho‐analytic* OR psychodynamic* OR psycho‐dynamic*))))) OR ((SU.EXACT.EXPLODE("Infants") OR all(((baby OR babies OR infant* OR child* OR toddler*)))) AND (all(((psychotherap* OR psycho‐therap* OR psychoanalytic* OR psycho‐analytic* OR psychodynamic* OR psycho‐dynamic*))) OR SU.EXACT("Parent Child Relationship") OR SU.EXACT("Mothers") OR SU.EXACT("Fathers") OR all((((attachment NEAR/3 disorder*) OR (insecure NEAR/3 attachment*) OR (secure NEAR/3 attachment*) OR (dysregulation NEAR/3 disorder*)))) OR all(((parent* OR mother* OR maternal* OR father* OR paternal* OR infant* OR child*) NEAR/3 (attachment* OR bond* OR interaction* OR relationship* OR dyad* OR triad*)))) AND SU.EXACT.EXPLODE("Psychotherapy"))) AND (SU.EXACT("Longitudinal Studies") OR SU.EXACT("Control Groups") OR SU.EXACT("Program Effectiveness"))) OR (((all((((parent* OR mother* OR maternal* OR father* OR paternal*) NEAR/3 (baby OR babies OR infant* OR child* OR toddler*) NEAR/3 (psychother* OR psycho‐therap* OR psychodynamic* OR psycho‐dynamic*)))) OR all((((parent* OR mother* OR maternal* OR father* OR paternal*) NEAR/3 (baby OR babies OR infant* OR child* OR toddler*) NEAR/3 (psychoanalytic* OR psycho‐analytic* OR psychodynamic* OR psycho‐dynamic*))))) OR ((SU.EXACT.EXPLODE("Infants") OR all(((baby OR babies OR infant* OR child* OR toddler*)))) AND (all(((psychotherap* OR psycho‐therap* OR psychoanalytic* OR psycho‐analytic* OR psychodynamic* OR psycho‐dynamic*))) OR SU.EXACT("Parent Child Relationship") OR SU.EXACT("Mothers") OR SU.EXACT("Fathers") OR all((((attachment NEAR/3 disorder*) OR (insecure NEAR/3 attachment*) OR (secure NEAR/3 attachment*) OR (dysregulation NEAR/3 disorder*)))) OR all(((parent* OR mother* OR maternal* OR father* OR paternal* OR infant* OR child*) NEAR/3 (attachment* OR bond* OR interaction* OR relationship* OR dyad* OR triad*)))) AND SU.EXACT.EXPLODE("Psychotherapy"))) AND (SU.EXACT("Experimental Groups") OR SU.EXACT("Followup Studies") OR SU.EXACT("Comparative Analysis"))) OR (((all((((parent* OR mother* OR maternal* OR father* OR paternal*) NEAR/3 (baby OR babies OR infant* OR child* OR toddler*) NEAR/3 (psychother* OR psycho‐therap* OR psychodynamic* OR psycho‐dynamic*)))) OR all((((parent* OR mother* OR maternal* OR father* OR paternal*) NEAR/3 (baby OR babies OR infant* OR child* OR toddler*) NEAR/3 (psychoanalytic* OR psycho‐analytic* OR psychodynamic* OR psycho‐dynamic*))))) OR ((SU.EXACT.EXPLODE("Infants") OR all(((baby OR babies OR infant* OR child* OR toddler*)))) AND (all(((psychotherap* OR psycho‐therap* OR psychoanalytic* OR psycho‐analytic* OR psychodynamic* OR psycho‐dynamic*))) OR SU.EXACT("Parent Child Relationship") OR SU.EXACT("Mothers") OR SU.EXACT("Fathers") OR all((((attachment NEAR/3 disorder*) OR (insecure NEAR/3 attachment*) OR (secure NEAR/3 attachment*) OR (dysregulation NEAR/3 disorder*)))) OR all(((parent* OR mother* OR maternal* OR father* OR paternal* OR infant* OR child*) NEAR/3 (attachment* OR bond* OR interaction* OR relationship* OR dyad* OR triad*)))) AND SU.EXACT.EXPLODE("Psychotherapy"))) AND (all(prospective) OR all("follow‐up") OR all(((experimental OR evaluat* OR compar* OR blind* OR "double‐blind*" OR placebo*) NEAR/5 (study OR studies OR research))))) OR (((all((((parent* OR mother* OR maternal* OR father* OR paternal*) NEAR/3 (baby OR babies OR infant* OR child* OR toddler*) NEAR/3 (psychother* OR psycho‐therap* OR psychodynamic* OR psycho‐dynamic*)))) OR all((((parent* OR mother* OR maternal* OR father* OR paternal*) NEAR/3 (baby OR babies OR infant* OR child* OR toddler*) NEAR/3 (psychoanalytic* OR psycho‐analytic* OR psychodynamic* OR psycho‐dynamic*))))) OR ((SU.EXACT.EXPLODE("Infants") OR all(((baby OR babies OR infant* OR child* OR toddler*)))) AND (all(((psychotherap* OR psycho‐therap* OR psychoanalytic* OR psycho‐analytic* OR psychodynamic* OR psycho‐dynamic*))) OR SU.EXACT("Parent Child Relationship") OR SU.EXACT("Mothers") OR SU.EXACT("Fathers") OR all((((attachment NEAR/3 disorder*) OR (insecure NEAR/3 attachment*) OR (secure NEAR/3 attachment*) OR (dysregulation NEAR/3 disorder*)))) OR all(((parent* OR mother* OR maternal* OR father* OR paternal* OR infant* OR child*) NEAR/3 (attachment* OR bond* OR interaction* OR relationship* OR dyad* OR triad*)))) AND SU.EXACT.EXPLODE("Psychotherapy"))) AND (all(((compar* OR control* OR placebo*) NEAR/5 group*)) OR all((random* OR intervention* OR experiment* OR trial*))))
Sociological Abstracts (ProQuest)
(((SU.EXACT.EXPLODE("Infants" OR "Premature Infants") OR all((baby OR babies OR infant* OR child* OR toddler*))) AND (SU.EXACT.EXPLODE("Parent Child Relations") OR SU.EXACT("Mothers") OR SU.EXACT("Fathers") OR SU.EXACT("Parents") OR all(((attachment NEAR/3 disorder*) OR (insecure NEAR/3 attachment*) OR (secure NEAR/3 attachment*) OR (dysregulation NEAR/3 disorder*))) OR all((parent* OR mother* OR maternal* OR father* OR paternal* OR infant* OR child*) NEAR/3 (attachment* OR bond* OR interaction* OR relationship* OR dyad* OR triad*))) AND (SU.EXACT.EXPLODE("Psychotherapy") OR all((psychotherap* OR psycho‐therap* OR psychoanalytic* OR psycho‐analytic* OR psychodynamic* OR psycho‐dynamic*)) OR SU.EXACT.EXPLODE("Family Therapy"))) OR (all(((parent* OR mother* OR maternal* OR father* OR paternal*) NEAR/3 (baby OR babies OR infant* OR child* OR toddler*) NEAR/3 (psychother* OR psycho‐therap* OR psychodynamic* OR psycho‐dynamic*))) OR all(((parent* OR mother* OR maternal* OR father* OR paternal*) NEAR/3 (baby OR babies OR infant* OR child* OR toddler*) NEAR/3 (psychoanalytic* OR psycho‐analytic* OR psychodynamic* OR psycho‐dynamic*))))) AND (SU.EXACT("Experimental Groups") OR SU.EXACT("Longitudinal Studies") OR SU.EXACT("Control Groups") OR SU.EXACT("Program Effectiveness") OR all(((experimental OR evaluat* OR compar* OR blind* OR "double‐blind*" OR placebo*) NEAR/5 (study OR studies OR research))) OR SU.EXACT("Followup Studies") OR SU.EXACT("Comparative Analysis") OR all(prospective) OR all("follow‐up") OR all((random* OR intervention* OR experiment* OR trial*)) OR all(((compar* OR control* OR placebo*) NEAR/5 group*)))
Appendix 2. metaRegister of Controlled Trials (mRCT)
We searched mRCT (www.controlled‐trials.com/mrct/search.htm) for ongoing trials using the terms "parent AND psychotherapy". We included reports from the following databases:
ISRCTN Register (International) ‐ copy of ISRCTN Register;
Action Medical Research (UK) ‐ subset from ISRCTN Register;
NIH ClinicalTrials.gov Register (International) ‐ subset of randomised trial records;
The Wellcome Trust (UK) ‐ subset from ISRCTN Register; and
UK trials (UK) ‐ subset from ISRCTN Register, UK trials only.
Appendix 3. Additional methods
| Analysis | Method |
| Assessment of reporting biases | Funnel plots (estimated differences in treatment effects against their standard error) were not drawn because there was an insufficient number of included studies (more than 10 are recommended), to identify asymmetry due to publication bias |
| Subgroup analysis and investigation of heterogeneity | We intended to explore the programme components that appeared to be associated with more effective outcomes and factors that modified intervention effectiveness, but there were too few included studies in each meta‐analysis to do this |
| Sensitivity analysis | We intended to reanalyse the data excluding studies on the basis of design (e.g. removing quasi‐randomised controlled trials (RCTs)) and risk of bias, but there were too few included studies in each meta‐analysis to do this. We conducted a sensitivity analysis using fixed‐effect and random‐effects models |
Appendix 4. Search results for each database up to January 2014
| Database searched | Last date searched | Number of results |
| CENTRAL Issue 12 of 12, 2013 (The Cochrane Library) | 13 January 2014 | 593 |
| MEDLINE (Ovid) 1950 up to 10 January 2014 | 13 January 2014 | 524 |
| EMBASE (Ovid) 1980 to January week 1 2014 | 13 January 2014 | 565 |
| CINAHL (EBSCOhost) 1982 to January 2014 | 13 January 2014 | 108 |
| PsycINFO (Ovid) 1806 to week 1 January 2014 | 13 January 2014 | 215 |
| BIOSIS Citation Index (ISI) to January 2014 | 13 January 2014 | 100 |
| SSCI (Web of Science ISI) to January 2014 | 13 January 2014 | 59 |
| ERIC (ProQuest) to January 2014 | 13 January 2014 | 428 |
| Sociological Abstracts (ProQuest) to January 2014 | 13 January 2014 | 12 |
| Total | 2604 | |
| After de‐duplication | 1921 | |
Data and analyses
Comparison 1. Comparison 1. Parent‐infant psychotherapy (PIP) intervention versus control meta‐analyses.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Parent mental health meta‐analysis: depression (dichotomous data) | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Post‐intervention | 3 | 278 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.52, 1.04] |
| 2 Parent mental health meta‐analysis: depression (continuous data) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Post‐intervention | 4 | 356 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.46, 0.02] |
| 3 Parent‐infant interaction: maternal sensitivity meta‐analysis | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Post‐intervention | 4 | 283 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.64, 0.38] |
| 4 Parent‐infant interaction: child involvement meta‐analysis: post‐intervention | 2 | 163 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.32, 0.30] |
| 5 Parent‐infant interaction: parent engagement meta‐analysis | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Parent positive engagement: post‐intervention | 3 | 216 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.46, 0.15] |
| 6 Infant attachment categories meta‐analysis: post‐intervention | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 Attachment category (Strange Situation Procedure (SSP)) secure: post‐intervention | 2 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 8.93 [1.25, 63.70] |
| 6.2 Attachment category (SSP) avoidant: post‐intervention | 2 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.24, 0.95] |
| 6.3 Attachment category (SSP) disorganised: post‐intervention | 2 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.17, 0.58] |
| 6.4 Attachment category (SSP) resistant: post‐intervention | 2 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.16, 2.97] |
| 7 Infant attachment categories meta‐analysis: follow‐up | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 Attachment category (SSP) secure: follow‐up | 2 | 129 | Risk Ratio (M‐H, Random, 95% CI) | 3.30 [1.82, 6.00] |
| 7.2 Attachment category (SSP) avoidant: follow‐up | 2 | 129 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.15, 0.76] |
| 7.3 Attachment category (SSP) resistant: follow‐up | 2 | 129 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.11, 3.07] |
| 7.4 Attachment category (SSP) disorganised: follow‐up | 2 | 129 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.29, 2.19] |
| 8 Infant attachment change meta‐analysis | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Attachment change insecure to secure: pre‐ to post‐intervention | 2 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 11.45 [3.11, 42.08] |
| 8.2 Attachment change stable secure: pre‐ to post‐intervention | 2 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 2.28 [0.41, 12.56] |
| 8.3 Attachment change secure to insecure: pre‐ to post‐intervention | 2 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 0.09 [0.01, 1.56] |
| 8.4 Attachment change stable insecure: pre‐ to post‐intervention | 2 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.26, 1.22] |
| 9 Infant problem behaviours meta‐analysis | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 Angry or externalising behaviours: follow‐up | 2 | 131 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.34, 0.77] |
| 10 Infant cognitive development meta‐analysis | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 Post‐intervention | 2 | 172 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.82, 0.51] |
Comparison 2. Comparison 2. Parent‐infant psychotherapy (PIP) versus other (psychoeducational or alternative) parenting intervention (non‐PIP) meta‐analyses.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Parent mental health meta‐analysis: depression (continuous data) | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Post‐intervention | 2 | 172 | Std. Mean Difference (IV, Random, 95% CI) | 0.23 [‐0.49, 0.95] |
| 1.2 Follow‐up | 2 | 160 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.23, 0.50] |
| 2 Parent‐infant interaction: maternal sensitivity meta‐analysis | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Post‐intervention | 3 | 248 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.27, 0.66] |
| 2.2 Follow‐up | 2 | 133 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.69, 0.80] |
| 3 Infant attachment categories meta‐analysis: post‐intervention | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Attachment category secure: post‐intervention | 2 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.32, 2.13] |
| 3.2 Attachment category avoidant: post‐intervention | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 4.6 [0.20, 105.62] |
| 3.3 Attachment category resistant: post‐intervention | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.4 Attachment category disorganised: post‐intervention | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.34, 1.82] |
| 4 Infant attachment categories meta‐analysis: follow‐up | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Attachment category secure: follow‐up | 2 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.61 [0.83, 3.12] |
| 4.2 Attachment category avoidant: follow‐up | 2 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.35, 1.64] |
| 4.3 Attachment category resistant: follow‐up | 2 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.48 [0.32, 6.98] |
| 4.4 Attachment category disorganised: follow‐up | 2 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.30, 2.22] |
| 5 Infant attachment change meta‐analysis: pre‐ to post‐intervention | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Attachment change insecure to secure: pre‐ to post‐intervention | 2 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.06, 4.10] |
| 5.2 Attachment change stable secure: pre‐ to post‐intervention | 2 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [0.28, 8.93] |
| 5.3 Attachment change secure to insecure: pre‐ to post‐intervention | 2 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [0.49, 5.13] |
| 5.4 Attachment change stable insecure: pre‐ to post‐intervention | 2 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.70, 1.64] |
| 6 Infant problem behaviours meta‐analysis | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Follow‐up | 3 | 184 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.39, 0.28] |
| 7 Infant cognitive development meta‐analysis | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Follow‐up | 2 | 162 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.25, 0.46] |
Comparison 3. Comparison 3. Parent‐infant psychotherapy (PIP) versus control single‐study results.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Parent mental health: depression follow‐up (dichotomous data) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Short‐term follow‐up (9 months) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Follow‐up (up to 18 months) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Long‐term follow‐up (5 years) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Parent mental health: depression (continuous data) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Short‐term follow‐up (9 months) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Follow‐up (up to 18 months) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Long‐term follow‐up (5 years) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Parent mental health single‐study results: Stress and Parenting Stress Questionnaire (SPSQ) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Post‐intervention (SPSQ) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 General maternal psychological stress | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Parent reflective function single‐study results | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Parent reflective function: Parent Development Interview (PDI): post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Parent (maternal) representations single‐study results | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Mother's Object Relations Scale (MORS) object relations (subscale warmth): post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 MORS object relations (subscale invasion): post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Parent (maternal) attitudes single‐study results | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 Maternal attitudes (subscale control aggression): post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Maternal attitudes (subscale encourage reciprocity): post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 Maternal attitudes (subscale complexity (awareness of complexity in child rearing)): post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Number reporting relationship and behaviour problems: post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 Relationship problems (adverse outcome): post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Still reporting relationship problems: post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Behaviour management problems (adverse outcome): post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Still reporting infant behaviour management problems: post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Parent‐infant interaction: parent engagement single‐study results | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Maternal non‐intrusiveness (Emotional Availability Scales (EAS) ‐ maternal video‐taped): post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Parent‐Infant Relationship Global Assessment Scale (PIR‐GAS) dyadic relationship well adapted or conflict: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 Infant responsiveness: post‐intervention (EAS infant responsiveness) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.4 Dyadic behaviour (behaviour on reunion/goal corrected partnership): post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Attachment change in those initially disorganised single‐study results | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 10.1 Stable disorganised: pre‐ to post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Change to secure: pre‐ to post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Change to other insecure: pre‐ to post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Infant attachment security (continuous measures) single‐study results | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 (Q sort) security post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Ainsworth Interactive Behaviour Scale, proximity avoidance: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.3 Ainsworth Interactive Behaviour Scale, contact resistance: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Infant attachment security single‐study results (dichotomous measures) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 12.1 (Q scales) security post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 (Q scales) insecurity post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Infant problem behaviours single‐study results | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 13.1 Angry or externalising behaviours: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Long‐term follow‐up (5 years Rutter A2 maternal report) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.3 Long‐term follow‐up 5 years Parent Behavior Checklist (PBCL) teacher report) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Infant behaviours single‐study results | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Infant mental health and development: restriction of affect: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Infant mental health and development: infant behaviours (Child Behaviour Checklist (CBCL) subscale internalising): follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.3 Infant mental health and development: infant behaviours (CBCL total): follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Infant cognitive development single‐study results | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 15.1 Infant cognitive development: follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 Infant cognitive development: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Infant cognitive development single‐study results | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16.1 Weschler subscale performance IQ: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Weschler subscale verbal IQ: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Effect of subsequent depressive episodes on infant cognitive functioning | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 17.1 Full‐scale IQ further depression | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 Full‐scale IQ no further depression | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.3 Performance IQ further depression | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.4 Performance IQ no further depression | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.5 Verbal IQ further depression | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.6 Verbal IQ no further depression | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 4. Comparison 4. Parent‐infant psychotherapy (PIP) versus other single‐study results.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Parent mental health number depressed (dichotomous data) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Short‐term follow‐up (9 months) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Follow‐up (up to 18 months) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Long‐term follow‐up (5 years) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Parent mental health meta‐analysis: depression (continuous data) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Short‐term follow‐up (9 months) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Long‐term follow‐up (5 years) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Parent mental health: stress and parenting stress | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Post‐intervention (Parenting Stress Index (PSI) parent domain) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Follow‐up (PSI parent domain) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Post‐intervention (PSI child domain) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Follow‐up (PSI child domain) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Parent mental health single‐study results: parenting sense of competence | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Total satisfaction: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Total satisfaction: follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Total lack of efficacy: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Total lack of efficacy: follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Parent‐infant interaction: single‐study results | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Chatoor Play Scale (maternal unresponsiveness): post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Chatoor Play Scale (maternal unresponsiveness): follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Chatoor Play Scale (maternal intrusiveness): post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.4 Chatoor Play Scale (maternal intrusiveness): follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.5 Chatoor Play Scale (dyadic conflict): post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.6 Chatoor Play Scale (dyadic conflict): follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Infant symptoms and problems | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Maternal perception of problem severity 100‐point scale: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Maternal perception of problem severity 100‐point scale: follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Maternal perception of effectiveness in dealing with problem: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 Maternal perception of effectiveness in dealing with problem: follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.5 Maternal perception of comfort dealing with problem: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.6 Maternal perception of comfort dealing with problem: follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Number reporting relationship and behaviour problems at post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 Relationship problems (adverse outcome): post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Still reporting relationship problems: post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 Behaviour management problems (adverse outcome): post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.4 Still reporting infant behaviour management problems | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Infant attachment change patterns single‐study results | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 From initially insecure avoidant or resistant to disorganised: pre‐ to post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 From initially disorganised to avoidant or resistant (organised but insecure): pre‐ to post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 From initially insecure or disorganised to secure or organised attachment: pre‐ to post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 No change from pre‐intervention or became less secure at post‐intervention: pre‐ to post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.5 Retained post‐intervention gains or moved towards secure/organised: post‐intervention to follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.6 No change from post‐intervention or became less secure at follow‐up: post‐intervention to follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Infant problem behaviours | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Angry or externalising behaviours: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Infant mental health and development: infant behaviours (Child Behaviour Checklist (CBCL)) total: follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 Infant mental health and development: infant behaviours (CBCL) subscale internalising: follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.4 Long‐term follow‐up (Parent Behavior Checklist (PBCL)) teacher report (5 years) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.5 Long‐term follow‐up (Rutter A2 maternal report 5 years) | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Infant cognitive development single‐study results | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 Infant cognitive development meta‐analysis: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Infant cognitive development meta‐analysis: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Infant cognitive development single‐study results | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Bayley Developmental Quotient (DQ) excluding participant infants with developmental delay: post‐intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Bayley DQ excluding participant infants with developmental delay: follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 5. Intraclass correlation coefficients (ICC) cluster corrections.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Parent mental health meta‐analysis: depression (dichotomous data) | 3 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Post‐intervention ‐ ICC = 0.2 | 3 | Risk Ratio (Random, 95% CI) | 0.69 [0.46, 1.03] | |
| 1.2 Post‐intervention ‐ ICC = 0.4 | 3 | Risk Ratio (Random, 95% CI) | 0.67 [0.44, 1.03] | |
| 1.3 Post‐intervention ‐ ICC = 0.6 | 3 | Risk Ratio (Random, 95% CI) | 0.67 [0.43, 1.03] | |
| 1.4 Post‐intervention ‐ ICC = 0.8 | 3 | Risk Ratio (Random, 95% CI) | 0.66 [0.42, 1.03] | |
| 2 Parent mental health meta‐analysis: depression (continuous data) | 4 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 2.1 Post‐intervention ‐ ICC = 0.2 | 4 | Std. Mean Difference (Random, 95% CI) | ‐0.22 [‐0.47, 0.03] | |
| 2.2 Post‐intervention ‐ ICC = 0.4 | 4 | Std. Mean Difference (Random, 95% CI) | ‐0.24 [‐0.52, 0.05] | |
| 2.3 Post‐intervention ‐ ICC = 0.6 | 4 | Std. Mean Difference (Random, 95% CI) | ‐0.24 [‐0.53, 0.05] | |
| 2.4 Post‐intervention ‐ ICC = 0.8 | 4 | Std. Mean Difference (Random, 95% CI) | ‐0.24 [‐0.53, 0.05] | |
| 3 Maternal sensitivity meta‐analysis | 4 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 3.1 Post‐intervention ‐ ICC = 0.2 | 4 | Std. Mean Difference (Random, 95% CI) | ‐0.16 [‐0.65, 0.32] | |
| 3.2 Post‐intervention ‐ ICC = 0.4 | 4 | Std. Mean Difference (Random, 95% CI) | ‐0.19 [‐0.67, 0.29] | |
| 3.3 Post‐intervention ‐ ICC = 0.6 | 4 | Std. Mean Difference (Random, 95% CI) | ‐0.22 [‐0.69, 0.26] | |
| 3.4 Post‐intervention ‐ ICC = 0.8 | 4 | Std. Mean Difference (Random, 95% CI) | ‐0.23 [‐0.71, 0.25] | |
| 4 Parent‐infant interaction: child involvement meta‐analysis | 2 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 4.1 Post‐intervention ‐ ICC = 0.2 | 2 | Std. Mean Difference (Random, 95% CI) | ‐0.07 [‐0.46, 0.32] | |
| 4.2 Post‐intervention ‐ ICC = 0.4 | 2 | Std. Mean Difference (Random, 95% CI) | ‐0.09 [‐0.50, 0.33] | |
| 4.3 Post‐intervention ‐ ICC = 0.6 | 2 | Std. Mean Difference (Random, 95% CI) | ‐0.09 [‐0.52, 0.33] | |
| 4.4 Post‐intervention ‐ ICC = 0.8 | 2 | Std. Mean Difference (Random, 95% CI) | ‐0.10 [‐0.53, 0.33] | |
| 5 Parent‐infant interaction: maternal engagement single‐study results | 3 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 5.1 Parent positive engagement: post‐intervention ‐ ICC = 0.2 | 3 | Std. Mean Difference (Random, 95% CI) | ‐0.23 [‐0.55, 0.09] | |
| 5.2 Parent positive engagement: post‐intervention ‐ ICC = 0.4 | 3 | Std. Mean Difference (Random, 95% CI) | ‐0.25 [‐0.58, 0.08] | |
| 5.3 Parent positive engagement: post‐intervention ‐ ICC = 0.6 | 3 | Std. Mean Difference (Random, 95% CI) | ‐0.26 [‐0.60, 0.07] | |
| 5.4 Parent positive engagement: post‐intervention ‐ ICC = 0.8 | 3 | Std. Mean Difference (Random, 95% CI) | ‐0.27 [‐0.60, 0.07] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cicchetti 1999a.
| Methods | Randomised, 2‐arm comparison of TPP for depressed mothers versus control Unit of allocation: participant Study dates: not reported |
|
| Participants |
Number randomised: n = 131 Number randomised to each group:
Participants: mothers and infants (dyads) received therapy Sex of infants:
Age of child:
Maximum age of child at entry: not stated Ethnicity:
Recruitment: a community sample of mothers with a history of depressive disorder recruited through referrals from mental health professionals and through notices placed in newspapers and community publications, in medical offices and on community bulletin boards Risk factors: mothers with history of depressive disorder within their toddlers' first 18 months. In Toth 2006 ‐ mothers with major depression ‐ co‐morbidities were also present, including anxiety, bulimia, alcohol disorder Social and economic status: not socio‐economically disadvantaged Country and setting: USA. Assessments in university research clinic, unclear where intervention delivered Child development: not stated, assumed to be typically developing Inclusion criteria: having a child approximately 20 months of age, diagnostic inclusion criteria for mothers in the depressed groups required mothers to meet the DSM‐III‐R criteria for major depression occurring at some period since the birth of their toddlers. Specifically, parents were required to have at least a high school education. Willing to accept random assignment Exclusion criteria: families could not be reliant on public assistance. In order to minimise co‐occurring risk factors that may accompany parental depression, families of low SES were excluded. Toth 2006 stated that participants with bipolar disorder, prior or current psychiatric disorder other than depression were excluded Comparability of randomised groups at baseline: intervention and control groups were comparable on a range of demographic characteristics. In Toth 2006, attachment security or disorganised attachment of infants was not significantly different in the intervention (TPP) and control groups. The retained sample (i.e. the infants who were assessed at post‐intervention) were not biased in terms of baseline attachment classifications |
|
| Interventions |
Duration of intervention:
Number of sessions and frequency: weekly sessions of mother and toddler with therapist
Intervention: manualised, TPP. The structure of TPP is unique in that mothers and their toddlers are seen in conjoint therapy sessions. Through joint observation of the mother and the child, opportunities arise to observe the influence of maternal representations on the character of interactions between mother and child, and therapeutic insights into the influence of maternal representation on parenting can be gained. Within the therapeutic sessions, the therapist strives to alter the relationship between mother and toddler. Toth 2006 specifies: "Through the use of observation and empathic comments, the therapist works toward assisting the mother in recognizing how she experiences and perceives her infant and herself, thereby allowing for correction of distorted perceptions and alterations in how the toddler and the self are experienced. The therapist also attends to the nature of the interactions that occur between the mother and the toddler, the mother and the therapist, and the therapist and the toddler. Interactions in one relationship pair tend to elicit parallel interactions in other relationship pairs, and attention to this parallel process in interactions across relationships and the influence of representations on these interactions provides templates for modifying maternal representations as they are enacted behaviorally in the mother–child relationship. In the course of this intervention, TPP is designed to provide the mother with a corrective emotional experience in the context of the relationship with the therapist. Through empathy, respect, concern, accommodation, and positive regard, the mother and child are provided with a context in which new experiences of self in relation to others—and, for the mother, in relation to the toddler—can be internalized. If mothers have a generalized negative representational model of self and relationships, then a therapeutic goal is to help them to use more specific representations with regard to various relationship partners, including the toddler. Evolving positive representations of the therapist can be contrasted with maternal representations of self in relation to parents. As the mother is able to reconstruct representations of self in relation to others through the therapeutic relationship, she also is able to reconstruct and internalize new representations of herself in relation to her child. Through highlighting, clarifying, and restructuring the dynamic balance between representational and interactional contributions to the quality of the mother– child relationship, improvement in the quality of maternal and child relationship capacities emerges. Moreover, the reorganization of maternal representations of self and of self in relation to others provides a framework for ongoing optimization of mother–child relationship functioning. Therapeutic change thus occurs through expansion of maternal understanding of the effects of prior relationships on current feelings and interactions. Through the development of more positive representational models of self and of self in relation to others, improvements in maternal sensitivity, responsivity, and attunement to the child are found to increase" (p. 1009) Type of psychodynamic model: TPP has its origins in the work of Selma Fraiberg, who described the pernicious influences that an unresolved parental past can exert on the evolving parent‐child relationship (Fraiberg 1975) Control: no details. Assumed to be TAU as all participants were not restricted from accessing other mental health treatments while in the study Therapist: Master's or PhD level therapists supervised during intervention Monitoring fidelity of the intervention: fidelity of TPP was monitored through weekly individual supervision, weekly group presentations and discussions of video‐taped cases, and monthly monitoring of video‐taped sessions for each case by 1 of the authors (DC), who was not providing supervision for the intervention therapists and, therefore, was able to assess objectively adherence to the parameters of the intervention. A checklist was utilised to assess adherence to the parameters of the intervention and if any concerns emerged they were brought to the immediate attention of the therapist's supervisor |
|
| Outcomes |
Timing of outcome assessment: post‐intervention (36 months of age) Outcomes Parent:
Parent/infant interaction: none Child:
Clinician or participant report of outcomes:
|
|
| Notes |
Note: each of the study publications reports on a subsets of participants from the same trial, therefore, the demographic characteristics and participant numbers vary in each report * Cicchetti 1999b employed the maternal report of attachment using the AQS. Attachment categories were re‐examined in Toth 2006: "In the prior investigation, which was an intervention evaluation, the maternal report attachment Q‐sort (AQS) methodology was used as the outcome measure. Although the AQS been shown to relate to attachment classifications derived from the Strange Situation ..... it is not considered to be the gold standard of the field. Therefore, further examination of the efficacy of the preventive intervention in fostering attachment security as assessed by the Strange Situation is warranted" (p. 1008). Thus, 2 separate measures of attachment security were reported in the publications of this study Adverse effects: no details given. Therapy did not alleviate depression (although the intervention was not designed to do so, so this is not an adverse effect per se) Funder: a grant and scientific MERIT award from the Child and Adolescent Prevention Research Branch (MH45027) of the NIMH Aim:
Study investigator's conclusion: the findings support the efficacy of an attachment‐theory‐based model of intervention for fostering developmental competence in the offspring of depressed mothers
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk |
Quote: "A randomised blocks procedure based on demographic characteristics of the depressed mothers" (Toth 2006, p. 1008). Because this was a preventive intervention RCT of a non‐treatment‐seeking sample, the study did not use a pre‐set allocation sequence, as might be the case in a treatment‐seeking sample from a clinic. Further information from study investigator: "NIMH had advised us to monitor demographic comparability of the intervention and control conditions over time, and adjust through the randomised blocking procedure over time, as needed". When mothers entered the study, they had to agree to random assignment Comment: further information obtained from study investigator (email 25 July 2013), method of randomisation unclear (also see below) |
| Allocation concealment (selection bias) | High risk |
Further information from study investigator: "Mothers were randomised during the baseline assessment wave, but mothers were not informed of their group assignment until completion of the baseline, pre‐intervention assessments" Comment: we obtained this further information from the study investigator by email on 25 July 2013, but concealment of the allocation sequence is only implied and we were unable to obtain further information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Although attrition levels were high, attrition was investigated and any effect on balance of demographics in the intervention and control groups was not significant:
|
| Selective reporting (reporting bias) | Unclear risk |
Comment: further information (disaggregated data) was requested but was not available from the study investigator |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No detail, but due to the nature of intervention blinding of participants not possible. In Cicchetti 2000: "Research staff working with the participating families were kept unaware of group status over the course of the study" (p. 1008) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk |
Comment: probably done
|
| Other bias | Low risk | No other sources of bias; no imbalance in terms of participant characteristics at baseline |
Cicchetti 2006b.
| Methods | Randomised, 3‐arm, parallel comparison of IPP (also called CPP in Cicchetti 2011a), PPI, and CS Unit of allocation: participant Study dates: not reported |
|
| Participants |
Number randomised: n = 137
Number randomised to each group:
Participants: mothers and infants (dyads) received therapy Sex:
Age of child: 13.31 months (SD 0.81) Maximum age of child at entry: not stated Ethnicity:
Recruitment: infants in maltreating families and their mothers were recruited. Quote: "A Department of Human Services (DHS) recruitment liaison was retained. As an employee of DHS, the liaison was able to access DHS Child Protective Service (CPS) and preventive service records to identify all infants known to have been maltreated and/or who were living in maltreating families with their biological mothers. The DHS liaison contacted eligible families and explained the project to mothers. Mothers who were interested in participating signed a release form for their names to be given to project staff. During the initial contact by project staff, the mothers provided informed consent and permission for their infant's participation. Mothers also signed a release allowing project staff to have access to DHS records regarding the family's CPS and preventive service involvement" (Cicchetti 2006a; p. 791) Risk factors: previous confirmed maltreatment that had occurred in the family or that the infant had experienced Social and economic status:
Setting: USA; university research, delivered in home‐based setting Child development: not stated. Assumed to be typically developing Inclusion criteria: infants in maltreating families and their mothers; child aged 12 months at recruitment. Maltreatment included all subtypes of maltreatment (i.e. neglect, emotional maltreatment, physical abuse, sexual abuse) Exclusion criteria: infants who had been placed in foster care because of limited ongoing contact with their mothers Comparability of randomised groups at baseline: all maltreatment groups comparable in terms of child gender, maternal age, minority race/ethnicity, education (Hollingshead level), and receiving assistance on the basis of need, total income, marital status. Quote: "At the onset of the intervention, groups did not differ on child gender, maternal age, maternal minority race/ethnicity, Temporary Assistance for Needy Families (TANF) receipt, income, or marital status" (Stronach 2013; p. 12 of unpublished manuscript) |
|
| Interventions |
Duration of intervention: mean duration 46.4 weeks (SD 7.36) for IPP group; 49.4 weeks (SD 4.81) for PPI group Number of sessions and frequency: mean 21.56 sessions (SD 9.60) in IPP group; 25.38 sessions (SD 9.65) in PPI group. Although intervention sessions in the home were scheduled weekly, fewer sessions were conducted as a result of cancellations and missed appointments Type of psychodynamic model: derived from the work of Selma Fraiberg (Fraiberg 1975) and Lieberman 1991 Intervention 1: IPP manualised, with central components and core principles of each approach specified. Quote: "Masters level therapists met weekly with mothers and their 12‐month‐old infants during sessions conducted in the home over the course of 1 year. The approach is supportive, nondirective, and non‐didactic, and includes developmental guidance based on the mother's concerns. During the sessions, the therapist and the mother engage in joint observation of the infant. The therapist's empathic responsiveness to the mother and the baby allows for expansion of parental understanding and exploration of maternal misperceptions of the infant. Therapists strive to allow distorted emotional reactions and perceptions of the infant as they are enacted during mother–infant interaction to be associated with memories and affects from the mother's prior childhood experiences. Through respect, empathic concern, and unfailing positive regard, the therapeutic relationship provides the mother with a corrective emotional experience, through which the mother is able to differentiate current from past relationships, form positive internal representations of herself and of herself in relationship to others, particularly her infant. As a result of this process, mothers are able to expand their responsiveness, sensitivity, and attunement to the infant, fostering security in the mother–child relationship and promoting emerging autonomy in the child" (Cicchetti 2011a; p. 793). Intervention 2: PPI. Quote: "This model of preventive intervention is derived from the ... work of David Olds and colleagues, in which nurses provided a home‐based education program on infant physical and psychological development and parenting, encouraged mothers to seek further education and employment, and enhanced informal social support. From this home‐based model, the PPI intervention was supplemented by a variety of cognitive and behavioural techniques in order to address parenting skill deficits and social‐ecological factors, such as limited personal resources, poor social support, and stresses in the home, associated with maltreatment. Masters level therapists, experienced in working with multi‐problem families, conducted home visits scheduled weekly over a 12‐month period (mean = 49.36 weeks, SD = 4.81 weeks). The PPI model was psychoeducationally based, striving to address current concerns, provide parental education and parenting skill training, reduce maternal stress, foster social support, and increase life satisfaction. The approach is didactic in nature, and involved training in parenting techniques, problem solving, and relaxation" (Cicchetti 2011a; p. 794) Control: services typically available to maltreating families in the community. CS: mothers and infants randomised to the CS group did not receive enhanced services. Rather, families continued to receive services that were typically available to maltreating families in the community. Families may have continued to be monitored by CPS and may have participated in other preventive services programmes. Quote: "families in the CS condition received case management from the DHS, according to their customary approach. Additionally, they received assistance in obtaining referrals to services and resources that may have been more difficult to access outside of the research trial. Service receipt within the CS condition varied from minimal contact to group parent skills training or individual counseling" (Stronach 2013, unpublished manuscript; p. 16) Therapist: for IPP, Master's level therapists met weekly with mothers and their infants during sessions. (For PPI, Master's level therapists, experienced in working with multi‐problem families, conducted home visits) Monitoring fidelity of the intervention: both the IPP/CPP and PPI interventions were manualised, with central components and core principles of each approach specified. Therapists participated in individual and group supervision on a weekly basis, and checks on the fidelity of the intervention implementation for each approach were conducted throughout the course of intervention. Extensive outreach was typically necessary to engage mothers in the interventions |
|
| Outcomes |
Timing of outcome assessment:
Outcomes Parent:
Parent/infant interaction:
Child:
Adverse effects: none reported Clinician or participant report of outcomes: clinician for outcomes other than the maternal‐reported child behaviour problems |
|
| Notes |
Note: each publication reported a subset that was followed up, thus the characteristics of each sample differs in each report. Results for both intervention groups were aggregated in the published report and we were unable to obtain further separate data from the study investigator. Some participants randomised to intervention declined treatment and their results were combined with the control (CS) group Funder: research supported by grants from the NIMH (MH54643), and the Spunk Fund, Inc. Aim:
Study investigator's conclusion:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Block randomisation procedures (further information obtained from investigator by email 24 July 2013). However, participants who declined treatment after assignment were aggregated with the randomised control (no treatment group). We judged the risk of bias as high |
| Allocation concealment (selection bias) | High risk |
Quote: "the study did not use a preset allocation sequence, as might be the case in a treatment‐seeking sample from a clinic" Comment: this further information was obtained from trial investigator by email 24 July 2013 |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Significant levels of attrition, but well‐investigated and explained. However, it was unclear if the decision to aggregate participants who were randomised to receive treatment but declined into the no treatment control group introduced a source of bias. Initially: IPP n = 53; PPI n = 49; CS n = 35. Participants who declined treatment were analysed in the control group (i.e. IPP n = 32; PPI n = 24; control n = 81). The following completed post‐intervention outcome assessments: IPP n = 28/32; PPI n = 22/24; control n = 54/81
|
| Selective reporting (reporting bias) | High risk |
|
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind personnel adequately. Unclear if participants blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk |
Comment: probably done
|
| Other bias | Low risk | No other sources of bias; no imbalance in terms of participant characteristics at baseline |
Cohen 1999b.
| Methods | Randomised, 2‐arm parallel group comparison of 2 psychodynamic psychotherapeutic interventions (MIP, PPT vs. infant‐led PIP WWW Unit of allocation: participant Study dates: not reported |
|
| Participants |
Number randomised: n = 67. Described as 67 mothers and their infants with clinical referrals. At follow‐up, the sample comprised 58 of the original 67 infants aged 10‐30 months old Number randomised to each group: PPT n = 33; WWW n = 34 Participants: mother and infants (dyads) received therapy (in addition to the sessions with the mother and infant, if indicated, the whole family could be included, or sessions might just involve the parents or the mother alone) Sex of infants:
Age of child: WWW 21.5 months (SD 6.5); PPT 19.2 months (SD 6.1); of the 58 dyads who were followed up in Cohen 2002: WWW 21.7 months (SD 6.7); PPT 19.4 months (SD 6.2); range 10‐30 months. Maximum age of child at entry: 30 months Ethnicity: not stated Recruitment: quote: "Referrals were made by parents themselves or by mental health, medical, and child welfare professionals. In some cases, presenting problems were manifested as functional problems in the infant involving feeding, sleeping, and behavioural regulation. In other cases, referrals were due to maternal depression and feelings of failure in bonding or attachment, all factors that impeded the mothers' ability to relate to their infants" (Cohen 1999a; p. 436) Risk factors: infant functional or behavioural problems, maternal depression and feelings of failure in bonding or attachment (impeding mother's ability to relate to infant) Social and economic status: table 1, p. 440 (Cohen 1999b). Not specifically recruited due to poverty, or other measures of SES. The groups were not different in low SES, poor or low education status Country and setting: Canada; intervention delivered in playroom set‐up at children's mental health centre funded by the Ontario Ministry of Community and Social Services Child development: normal length of pregnancy, labour, not premature, normal Apgar scores, birth weight reported in table 1 p. 440, therefore, assumed to be typically developing Inclusion criteria: quote: "To be included, mothers and infants had to be physically capable of participating in play" (Cohen 1999b; p. 436) Exclusion criteria: not stated Comparability of randomised groups at baseline: the 2 groups did not differ in the nature or number of presenting complaints. There were no significant difference in other demographic measures |
|
| Interventions |
Duration of intervention: approximately 5 months Number of sessions and frequency: weekly 1‐hour sessions for approximately 5 months. WWW: weekly sessions; PPT: weekly, with additional family or couple sessions at 3‐4 week intervals. The mean number of sessions for WWW was 13.8 and for PPT 14.9 . The mean length of time over which treatment occurred was 4.6 months for the WWW group and 5.4 months for the PPT group. Intervention 1 (PPT): quote: "PPT is the most common treatment offered in the Infant and Family Assessment and Treatment Team at the Hincks‐Dellcrest Centre, and represents what most families could expect to receive by way of infant‐parent treatment in this clinic. Typically, PPT involved discussion between the mother and therapist throughout the whole session while mother and infant played, but without any instructions. The only expectation was that “we will talk and play” and the sessions were not divided into two parts as was done in the WWW treatment. Unlike WWW, there was more flexibility so that in addition to the sessions with the mother and infant, if indicated, the whole family might be included, or just involve the parents or the mother alone. Nevertheless, the infant and mother were seen as the primary therapeutic unit in all but one case (a mother of twins was seen alone). Whereas the mother‐infant sessions were typically held weekly, family or couple sessions occurred at 3‐ to 4‐week intervals. The parent‐infant therapy was generally conducted as follows: The mother and infant were invited to play and the mother to talk. The mother was told that anything she talked about was okay, but that she and the therapist would also try to attend to the infant's activity. Generally, the therapist indicated by his/her demeanour that he/she would not take a primary role in playing with the child, but would try to help the mother to be with her child. As with other forms of psychodynamic psychotherapy, use was made of transference, repetition of the past, re‐experiencing of affect and interpretation. The therapist's observations made of the infant and the mother‐infant interaction were used to draw the mother's attention to her infant's needs and signals" (Cohen 1999a; p. 437) Intervention 2 (WWW): quote: "WWW. Following from Muir et al. (1989), each WWW session was divided into two parts. The first half hour consisted of the infant‐led activity. The critical procedural difference between this therapy and PPT was the instruction to the mother to get down on the floor with her infant, observe her infant, and follow his lead. She was encouraged to respond to the infant's initiations, but asked not to take over or guide the infant's activity or play in any way. The therapist's role was to engage in a parallel process of watching, waiting, and wondering about the interactions between mother and infant. The therapist also did not intervene by directing the mother, or by interpreting the infant's activity or the mother's comments. By structuring the session in this way, the space was created for the infant to use the mother for his own therapeutic purposes (i.e. to play out relational and developmental struggles). The second part of the session comprised a 20‐minute discussion between the mother and the therapist intended to explore what the mother observed about her infant, understood about her infant's experience, and how she experienced the session. It also provided an opportunity for working through inevitable anxieties and painful feelings the mothers experienced following their infants' lead. The therapist routinely asked the mother to make her own observations of her infant's activity and to reflect on her feelings during the session. The focus was on making it possible for the mother to follow her infant's lead over her gaining insight" (Cohen 1999a; p. 437) Type of psychodynamic model
Control: no control group Therapist: there were 4 therapists (1 man and 1 woman per treatment) who were infant mental health specialists with > 5 years of clinical experience as well as experience in applying the respective psychotherapies for a minimum of 3 years Monitoring fidelity of the intervention: no details given |
|
| Outcomes |
Timing of outcome assessment: at the end of treatment (post‐treatment), and follow‐up at 6 months after treatment ended (follow‐up) Outcomes Parent: PSI (Abidin 1986). Only the total scores for the parent and child domains were analysed for this paper. The PSI is standardised for ages ranging from 1 month to 19 years. PSOC scale (self esteem) specific to the parenting role (Johnston 1989). Depression (BDI; Beck 1978). PSI, PSOC, and BDI are self reported Parent/infant interaction: the Chatoor Play Scale (Chatoor 1986) was used to code 10 minutes of video‐taped free play between mothers and their infants. 4 dimensions were derived: dyadic reciprocity, dyadic conflict, maternal intrusiveness, and maternal unresponsiveness Child:
Adverse effects: none reported Clinician or participant report of outcomes: clinician with some participant symptom reporting (mothers self reported depression using the BDI, parenting stress using the PDI, and parenting sense of competence using the PSOC scale; parents reported severity of infant symptoms |
|
| Notes |
Funder: research supported by a grant from Health Canada National Health Research and Development Program (6606‐4431) and a postdoctoral award from the Ontario Mental Health Foundation to Mirek Lojkasek Aim: contrasted the relative effectiveness of infant‐led psychotherapy with an alternate form of PIP. It was hypothesised that mothers in the WWW group would report a greater decrease in parenting stress, a greater increase in their sense of parenting competence and satisfaction, and less depression than mothers in the PPT group at the end of treatment Study investigator's conclusion: quote: "A broad range of measures of attachment, qualities of the mother‐infant relationship, maternal perception of parenting stress, parenting competence and satisfaction, depression, and infant cognition and emotion regulation were used. The WWW group showed a greater shift toward a more organized or secure attachment relationship and a greater improvement in cognitive development and emotion regulation than infants in the PPT group" (Cohen 1999a; from abstract p. 429) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation in one‐third of cases was inadequate. In two‐thirds of cases, assignment was done using a table of random numbers. Otherwise, assignment was dependent on therapist caseload and available time for treatment. Further details from investigator: "A table of random numbers was used initially. However, because some therapists were paid from the research grant we did not have the luxury of leaving them idle. Therefore, some cases were referred to whatever therapist had time. This was done before reviewing the file for pertinent information that would be needed by the therapist and the people doing the assessment" (email 26 June 2013) |
| Allocation concealment (selection bias) | High risk | No details given, but unlikely to have been adequately concealed given that allocation of one‐third of the participants was on therapist availability |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 9/67 dropped out. 6 dyads who started treatment dropped out early in treatment, 3 because of life events (e.g. a move) and 3 because of ambivalence about treatment. These dyads are not included in the analyses. Of the 9 dyads lost to follow‐up in the report of the 6‐month follow‐up study, 7 were in the WWW group and 2 were in the PPT group. The report stated that "These dyads did not differ from the remainder of the sample on background measures or pre‐treatment scores on the dependent variables" (quote from Cohen 2002; p. 366) |
| Selective reporting (reporting bias) | Unclear risk | All pre‐specified outcomes reported, but further the numbers in each attachment category were not reported and we were unable to obtain further data, although we requested this, the investigator no longer had access to these data in a format that could be provided from incorporation into the review (email 27 November 2013) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Further information from investigator: participants were blinded to the intervention they received (email 26 June 2013) Comment: it is likely that therapists were aware which treatment was being delivered |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "(Strange Situation, Chatoor Play Scale, and Bayley Scales) are measures of proven reliability and validity that were either independently scored from videotapes by raters blind to treatment group or directly administered to the child, which reduces the effects of reporter bias" (p. 447) |
| Other bias | Low risk | No other sources of bias; no imbalance in terms of participant characteristics at baseline |
Cooper 2003a.
| Methods | Randomised, 4‐arm comparison of routine primary care, non‐directive counselling, CBT or psychodynamic therapy Unit of allocation: participant Study dates: screening took place between January 1990 and August 1992 |
|
| Participants |
Number randomised: n = 193 Number randomised to each group: counselling n = 48; CBT n = 43; PIP n = 50; control n = 52 Participants: mothers (depressed) and infants (dyads) received therapy. The mothers identified through birth records of Addenbrooke's Hospital, Cambridge were screened for mood disturbance in the early postpartum period by means of EPDS (Cox 1987). Mothers with suspected postpartum depression (EPDS score of ≥ 12) were assessed systematically and women found to have postpartum depression were invited to take part in the study. Any father or other family member participation was not stated in the report Sex of infants: not stated Age of child: 8 weeks at study entry Maximum age of child at entry: not stated Recruitment: quote: "A large consecutive series of primiparous women (i.e. n = 3222), identified through the birth records of Addenbrooke's Hospital, Cambridge, was screened ... for mood disturbance in the early post‐partum period by means of a postal administration of the Edinburgh Postnatal Depression Scale (EPDS; Cox 1987). Those with suspected post‐partum depression (EPDS score of 12 or more) were assessed systematically and those found to be suffering from post‐partum depression were invited." (Cooper 2003b; p. 412) Risk factors: depressed new mothers Social and economic status: high social disadvantage noted in each group: 30% in counselling; 24% in CBT; 10% in PIP; 35% in control Country and setting: UK; Cambridge University Department of Psychiatry. Intervention delivered in the community (home) Child development: assumed to be typically developing and with no gross congenital abnormalities Inclusion criteria: quote: "Women were considered eligible for the study if they fulfilled the following criteria: primiparous, living within a 15‐mile radius of the maternity hospital and with English as their first language" (Cooper 2003b; p. 412) Exclusion criteria: quote: "Women were excluded if they had delivered prematurely (before 36 weeks' gestation), if their infant had any gross congenital abnormality, if they had not had a singleton birth or if they were intending to move out of the area within the period of the intervention" (Cooper 2003b; p. 412) Comparability of randomised groups at baseline: comparable on all baseline factors, including negative orientation to motherhood. More women in the control group (35%) experienced social adversity compared with fewer women in the PIP group |
|
| Interventions |
Duration of intervention: 8‐18 weeks' postpartum Number of sessions and frequency: on a weekly basis from 8 to 18 weeks postpartum. Total number of sessions not stated, if given on a weekly basis from 8 to 18 weeks postpartum then ten sessions were delivered. Participants were considered to be completers if they attended more than 4 treatment sessions Interventions: details of the treatments were given in Cooper 2003b Intervention 1: brief psychodynamic PIP using the treatment techniques described by Cramer 1990, in which an understanding of the mothers representation of her infant and relationship was promoted by exploring aspects of the mothers and early attachment history Intervention 2: CBT. This is an appropriately modified form of interaction guidance (McDonough 1993) primarily directed, not at maternal depression, but the problems identified by the mother in the management of the infant concerning, e.g. feeding or sleeping, as well as observed problems in the quality of the mother‐infant interaction. In this context, the mother was provided with advice about managing infant problems and was helped to solve such problems in a systematic way, encouraged to examine her patterns of thinking about her infant and herself as a mother, and was helped through modelling and reinforcement of the aspects of interactional style Intervention 3: non‐directive counselling, in which women were provided with the opportunity to air their feelings about any current concerns, including marital problems or financial difficulties as well as concerns they might raise about the infant Control: routine primary care that involved the normal care provided by the primary healthcare team with no additional input from the research team Type of psychodynamic model: PIP based on Cramer 1990 using a range of techniques Therapist: 6 study therapists were involved, comprising a specialist in each of the 3 research treatments and 3 non‐specialists who included 2 seconded NHS health visitors who were trained in 2 of the treatments Monitoring fidelity of the intervention: the principal investigators ran weekly supervision sessions with the therapists during which the progress of each case was reviewed and adherence to treatment protocols was ensured. The content of therapy was also assessed to check the therapist adherence and 30 items from the therapist rating scale |
|
| Outcomes |
Timing of outcome assessment: maternal mental state assessments were made immediately post‐intervention (4.5 months' or 18 weeks' postpartum), at short‐term follow‐up when the infant was 9‐months old, at medium‐term follow‐up at 18‐months old, and at long‐term follow‐up at 5 years of age Outcomes Parent: maternal depression at 4.5 months, immediately post‐intervention, using EPDS and structured interview for DSM‐III‐R; and using EPDS at 9‐month follow‐up, at 18‐month follow‐up, and at 5‐year follow‐up Parent/infant interaction: quality of the mother‐infant relationship (maternal sensitivity, warmth, responsiveness and acceptance), assessed by mother and infant interacting in a 5‐minute face‐to‐face play session at 8 weeks' and 18 weeks' postpartum assessments (i.e. before treatment and immediately post‐intervention using global rating scales (Murray 1996)) Child: childhood cognitive and emotional development using the BSQ (Richman 1971) at 18‐month follow‐up; infant attachment at 18‐month follow‐up using the SSP (Ainsworth 1978); infant cognitive development at 18‐month follow‐up using the BSID MDI (Bayley 1969). At 5‐year follow‐up of the McCarthy Scales of Children's Abilities (McCarthy 1972), a general measure of children's cognitive development was administered. At 5‐year follow‐up, mothers completed a self report Rutter A2 scale (Rutter 1970) for child behaviour problems of clinical significance At 5‐year follow‐up, the children's teachers completed the PBCL (McGuire 1988) Clinician or participant report of outcomes: maternal depression self report (EPDS), the Rutter A2 scale was reported by mothers. The SSP was assessed by trained independent assessors, the BSID were assessed in the research unit by the study investigators, the PBCL was reported by the children's teachers, and the McCarthy Scale of Children's Abilities was administered in the research unit. The video‐taped interactions were assessed by the study investigators. The BSQ was obtained by interviewing the mothers (i.e. clinician report) |
|
| Notes |
Note: this study comprised Murray 2003 and Cooper 2003a Adverse effects: negative findings were reported in terms of in efficacy Funder: initial study funded by a grant from Birthright. The 5‐year follow‐up study was supported by the Medical Research Council Aim: to evaluate the effect of 3 psychological treatments in addition to routine primary care on maternal mood and the mother‐child relationship and child outcomes Study investigator's conclusion: psychological intervention for postpartum depression improves maternal mood in the short term; however, this benefit was not superior to spontaneous remission in the long term. Early intervention was of short‐term benefit to the mother‐child relationship and infant behaviour problems |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The women were allocated randomly to a treatment group by the study recruiter, who drew one of 4 coloured balls from a bag, the assignment of each therapy to a different coloured ball having been defined at the start of the study and maintained until the end of the recruitment period" (Cooper 2003b, p. 413) |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 170 completed therapy (89.5%) out of the 193 randomised; 41 in non‐directive counselling; 41 in CBT; 40 in psychodynamic PIP; 48 in control. Refusals to participate, drop‐outs or participants who had moved away during the intervention period were described: "No difference was found between the completers and non‐completers on the measures of maternal mood collected pre‐therapy and at 4.5, 9, and 18 months (p. 414). The women who did not complete therapy were younger (mean = 24 years, SD = 6.3) than those who did complete (mean = 28 years, SD = 5.1; t = 72.9, df = 186, P = 0.004). The non‐completer group also had a higher proportion of women who were single or separated (Fisher's exact test P = 0.05)" (p. 414) |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported; however, means and SD for all outcomes, where applicable, were not reported at each time point for each group. Instead, the results of statistical tests and their significance or median and interquartile ranges were reported in the published reports. We obtained further information from the study investigator who provided means and SD (email 13 December 2013) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unclear if the women participants were aware of which intervention they had been assigned to, but given the nature of the interventions it is unlikely that the personnel or participants were adequately blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The outcome assessors were blinded to the allocation |
| Other bias | Low risk | At baseline, more social adversity in control group |
Lieberman 1991.
| Methods | Randomised, 2‐arm comparison PIP of anxiously attached 12‐month‐old infants versus control Unit of allocation: participant Study dates: not reported |
|
| Participants |
Number randomised: n = 59 dyads randomised Number randomised to each group: intervention n = 34; control n = 25. Securely attached dyads formed a second non‐randomised control group (n = 34), not addressed in this review Participants: mother and infants (dyads) received therapy Sex of infants: intervention 52.9% boys; control 44% boys Age of child: 12 months (11‐14 months at entry) Maximum age of child at entry: up to 14 months Ethnicity: Hispanic Recruitment: the dyads were recruited from paediatric clinics at a large teaching hospital and neighbourhood health clinics Risk factors: at risk for disorders of attachment because quote: "recent Latino immigrants face a high incidence of depression and anxiety as a result of poverty, unemployment, and cultural uprootedness". "We surmised that the infants would be at risk for anxious attachment because their mothers might be relatively emotionally unavailable due to their circumstances" (p. 200) Social and economic status: economic hardship was reflected in the living conditions and parents' employment with 74.2% sharing living quarters and only 44.3% fathers and 8.2% mothers working full time in low‐paid service jobs. Most families shared living quarters with others (74.2%). Only 44.3% of fathers and 8.2% of mothers worked full‐time, mostly in low‐paying service jobs Country and Setting: USA; intervention delivered during home visits with laboratory outcome assessments Child development: no congenital birth defects; overall 29.6% of whole sample had some birth complication; assumed to be typically developing Inclusion criteria: children aged 12‐24 months at entry; at risk due to stressful life events. At 12 months of age, during a home visit, infants were assessed using the SSP (Ainsworth 1978). Infants classified as anxious‐avoidant or anxious‐resistant were randomised Exclusion criteria: > 5 children to each mother; flagrant psychological disorders Comparability of randomised groups at baseline: no differences except in unemployment rates: 15.0% anxious control; 53.8% anxious intervention; P value = 0.024 |
|
| Interventions |
Duration of intervention: 12 months Number of sessions and frequency: weekly sessions. Total number of sessions not stated. The study began when the infants were 12 months old and ended shortly after their second birthday Intervention: quote: "The intervention began immediately after research group assignment. The format was unstructured weekly sessions with mother and baby. Visits took place mostly in the home and lasted 1 1/2 hours. Each dyad had one intervenor during the entire intervention period. The main focus of the intervention was to respond to the affective experiences of mother and child, both as reported by the mother and as observed through the mother‐child interaction. There was no didactic teaching. Instead, the intervenors sought to alleviate the mothers' psychological conflicts about their children and to provide developmental information that was clinically timed and tailored to the child's temperament and individual style. The developmental information focused on areas relevant to quality of attachment, such as contingency to signals, availability of age‐appropriate opportunities for exploration, and negotiation of infant‐mother conflicts to promote a goal‐corrected partnership. In attachment theory language, this intervention approach intends to provide the mother with a corrective attachment experience. The intervenor spoke for the mother's affective experience, addressing the legitimacy of her longings for protection and safety both when she was a child and currently as an adult, and enabling her to explore unsettling feelings of anger and ambivalence toward others (including the child and the intervenor). The intervenor linked this process to the child through appropriately timed developmental information to reduce negative attributions and to support a benign perception of the child's motives. When feasible, the intervenor also tried to provide concrete elements of protection by helping to secure needed goods and services" (p. 201) Type of psychodynamic model: based on Fraiberg 1980 Therapist: the 4 intervenors were bicultural, bilingual women with Master's degrees in psychology or social work and with clinical experience Control: not stated, assumed to be TAU Monitoring fidelity of the intervention: each intervenor received weekly supervision by senior faculty |
|
| Outcomes |
Timing of outcome assessment: post‐intervention (24 months of age) Outcomes Parent: LEI (stressful life events) (Egeland 1979) at baseline Parent/infant interaction: free play measures; maternal empathic responsiveness/empathy (equivalent to the Home Observation for Measurement of the Environment (HOME) Inventory: maternal care, maternal responsiveness, and maternal involvement Bradley 1977); maternal initiation of interaction (7‐point scale); behaviour on reunion (goal‐corrected partnership, 9‐point scale); maternal child‐rearing attitudes (control aggression, encourage reciprocity, complexity) (Cohler 1970) Child: restriction of affect (7‐point scale); angry behaviour (frequency); security of attachment (Q‐sort) (Waters 1985). Avoidance and resistance, behaviour on reunion, and goal‐corrected partnership were measured using Ainsworth Interactive Behaviour Scales, which are modelled after the SSP, but with longer 10‐minute episodes suitable for younger children Ainsworth 1978) Adverse effects: none Clinician or participant report of outcomes: all outcomes reported objectively by clinician/investigators |
|
| Notes |
Funder: NIMH Prevention Research Branch grant 5 ROI MH39973 to AF Lieberman Aim: to test the hypothesis that PIP can improve quality of attachment and social‐emotional functioning Study investigator's conclusion: intervention group infants were significantly lower than anxious controls in avoidance, resistance, and anger. They were significantly higher than anxious controls in partnership with mother. Intervention mothers had higher scores than anxious controls in empathy and interactiveness with their children. The groups did not differ in maternal child‐rearing attitudes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Anxiously attached dyads were assigned to the intervention or the control group by block randomization for infant sex and birth order (first, later). Fifty‐nine dyads were randomly assigned (intervention group n = 34 and anxious control group n = 25)" (p. 201) |
| Allocation concealment (selection bias) | Low risk | Further details from investigator: allocation of participants was concealed up to the point where treatment began, the randomisation took place during the last assessment session after the SSP classification took place. At that time, the clinician opened an envelope in the mother's presence where a piece of paper stated which group the dyad would be assigned to: intervention or control. The clinician found out at the same time as the mother about the group assignment, which was done at random (email 3 June 2013) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 32/59 completed. 7 cases dropped out after the home visit but before the pre‐intervention SSP (12 months of age) and could not be assigned. Overall attrition was 18% and did not differ for the experimental groups. At the post‐intervention assessment (24 months of age), the randomised sample consisted of 82 dyads: 29 in the anxious‐intervention group and 23 in the anxious‐control group |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes are reported, but the LEI (parental stress) result at post‐intervention was presented only as a whole sample mean |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No details given. Judged as high risk after we obtained further information from the investigator as it is likely that given the nature of the intervention the participants or personnel would have been aware of their assignment to therapy and, at randomisation, the mothers were told if they had been assigned to intervention or control |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The Strange Situation was coded by fully trained and experienced judges. The home and laboratory measures were scored by coders who were blind to the 12‐month classification and group assignment of the dyads. Different coders scored the home and laboratory measures. In the 24‐month laboratory situation, the free‐play measures and reunion measures were scored by different coders. Intervention process raters had no access to other outcome data. These procedures were adopted to protect the independence of the different ratings" (p. 203) |
| Other bias | Low risk | No other sources of bias; no imbalance in terms of participant characteristics at baseline |
Robert‐Tissot 1996a.
| Methods | Randomised, 2‐arm parallel comparison of PPT and interaction guidance therapy Unit of allocation: participant Study dates: recruited between Autumn 1987 and Spring 1991 |
|
| Participants |
Number randomised: n = 75 (75 mothers took part (unclear how many were initially randomised or if the number randomised is different from the number taking part)) Number randomised to each group: PPT n = 42; interaction guidance therapy n = 33 Participants: mother and infants (dyads) received therapy. Fathers were not excluded but father data were not included in the published report. The study investigator collected and provided us with data from fathers but separate data were not available for each intervention group Sex of infants:
Age of child: mean 15.6 months (SD 8.4), range 2‐30 months with no difference between boys and girls Maximum age of child at entry: 30 months Ethnicity: (additional data from investigator): the clinical group was representative of the general population of the same age in the Geneva area according to the State statistics available for the years during which the study was conducted (% of Swiss and non‐Swiss, % of single parents, parental education and occupation). Mainly Caucasian European infants. The proportion of children with non‐Swiss citizenship was identical to the main population (34%) Recruitment: quote: "referred to the Child Guidance Clinic for sleep, feeding, and behavioural disorders (mostly crying fits, aggression, and temper tantrums)". Quote from p. 101: "Referred symptoms were sleep disorders (52%), eating disorders (12%), behaviour disorders (mostly crying fits, agitation, tantrums, and aggression; 21%); and parent‐infant interaction problems (i.e. separation and attachment problems; 15%). Most cases were referred by paediatricians (59%)." Quote from p. 103: "New cases were presented to the clinical team during regular weekly seminars. Marked developmental delay, pervasive disorder of the child, or a major personality disorder of the mother (i.e. psychosis, borderline, or major depression) constituted exclusion criteria for brief psychotherapy. If there was no contraindication, the case was randomly assigned to psychodynamic therapy or interaction guidance" (p. 101) Risk factors: no details other than with the problems detailed above. Depression not specifically targeted but scores on BDI (Beck 1961) were mild to severe (mean 11.67; SD 7.23). No other risks identified: "the clinical group was representative of the general population of the same age in the Geneva area according to the State statistics available for the years during which the study was conducted (the percentages of Swiss and non‐Swiss, of single parents, parental education and occupation)" (further information obtained from investigator by email on 23 May 2013) Social and economic status: not stated Country and setting: Switzerland; research clinic setting Child development: typically developing (children with developmental problems were excluded) Inclusion criteria: consenting and referred to clinic for sleep, feeding, and behavioural disorders (mostly crying fits, aggression, and temper tantrums) Exclusion criteria: a marked developmental delay, pervasive disorder of the child or a major personality disorder of the mother (i.e. psychosis, borderline or major depression) Comparability of randomised groups at baseline: group differences on the demographic variables were explored using Chi2 or ANOVAs as appropriate; no significant differences were found between the 2 intervention groups, except for the mean number of therapy sessions |
|
| Interventions |
Duration of intervention: mean duration 9.3 weeks (SD 4.6) Number of sessions and frequency: weekly sessions. Mean number of sessions for both treatments 6.1 (SD 2.5), range 1‐12. Mean number of sessions (n = 7) was significantly greater (P < 0.009) for interaction guidance than for PPT (n = 5.5) Intervention 1 (PPT): based on Fraiberg's pioneering work (Fraiberg 1980). It aims at uncovering the impact of maternal conflict on the perceptions the mother has of the child, with attendant distortions in the interactions. Mother and infant (more rarely mother, father, and infant) are seen on a once‐a‐week basis. The therapist listens to the mother's complaints, anxieties and narratives while remaining attentive to the ongoing interactions between the 3 protagonists. He or she searches actively for a focus of intervention in the relationship. The focus is composed of a core conflictual relationship within the child, of basic projections and maternal representations concerning the infant, of corresponding symptomatic interactions and of similar conflicts in the mother's past history. The therapist verbalises this core constellation in order to lessen projective distortions, with attendant anxieties and symptomatic interactions. A positive therapeutic alliance is fostered, while the transference is not interpreted Intervention 2 (interaction guidance): focusses on parent‐infant relationship, video‐assisted coaching methods during parent‐infant play. Quote: "Interaction guidance can be considered as a contrasting therapy, because several of its components are basically different from those in psychodynamic approaches. The main difference lies in the absence of references to the mother's past and to the process of projection. The therapist remains in the "here and now" frame and capitalizes on refined observations of interactional sequences that are problematic and that reveal maternal misperceptions of the child's signals. Moreover, the therapist will attempt to reinforce, with encouragement, interactions that are favourable (rather than look for and interpret negative patterns)" (p. 100) Type of psychodynamic model: PPT based on Fraiberg's pioneering work (Fraiberg 1980). A thorough description of the technique is presented in a book that serves as a primer for its teaching (Cramer 1993) Control: interaction guidance (McDonough 1995). Positive family interactions are encouraged through the use of video‐assisted coaching methods during parent infant play. The therapist empowers families by identifying positive carer behaviour and attends to problems by suggesting alternative interpretations of the infant's behaviour. In this approach, no explicit reference is made to the mother's past history Therapist: PPT was provided by 4 psychiatrists who were also practicing psychoanalysts; the interaction guidance therapy was practiced by a psychologist and by a speech therapist, who were trained by Susan McDonough, one of the leading experts in this technique Monitoring fidelity of the intervention: not mentioned specifically in the report |
|
| Outcomes |
Timing of outcome assessment: 1 week after the end of treatment (Evaluation 2), and 6 months later (Evaluation 3). There were no statistics available for the fourth time point at 1‐year follow‐up (Evaluation 4) due to sample attrition Outcomes Parent: maternal representations ('R'‐interview, a 28‐question checklist of representation of the infant, the mother in her mothering role, the mother as a person, her mother, the infant's father, and affects and self esteem) (Stern 1989b) Parent/infant interaction: maternal sensitivity (Ainsworth 1974), CARE‐Index (Crittenden 1981) Child: Symptom checklist to measure the frequency, duration, and intensity of disturbances in: sleep, feeding, digestion, breathing, skin and allergies; behaviour disorders (temper tantrums, negativism, crying spells, and aggression); fears and separation problems. The frequency, duration, and intensity of disturbance were evaluated by the mother on a 5‐point scale (ranging from 1 = never or non‐important, to 5 = nearly always or very important) (Robert‐Tissot 1989) (self report), KIA/KIDIES Profile was used to measure the following affects in the child's behaviour: joy, distress, sadness, anger, negativism, and fear (Stern 1989a) Adverse effects: none Clinician or participant report of outcomes: symptoms reported by mothers using a checklist. All other outcomes were reported objectively by the investigators |
|
| Notes |
Note: results for the PPT and interaction guidance groups were combined and differences over time were presented. We obtained further data from the study investigator but the intervention groups were combined and presented vs. a non‐clinical, non‐randomised normal community sample and no further data were available (email 23 May 2013). Follow‐up interviews on 53 of children at pre‐adolescence were reported in Cramer 2002 (no disaggregated data available for intervention groups) Funder: supported by Fonds National Suisse de la Recherche Scientifique (FNRS) grants No 3.830.0.86 and No 32‐8949.86/2 Aim: to treat many infant disorders and possibly for preventing the establishment of protracted mother‐infant conflictual relationships Study investigator's conclusion: results indicated a significant symptom reduction; dyadic interactions became more harmonious (mothers became less intrusive and infants more co‐operative). Maternal self esteem grew significantly and negative affects decreased Improvements lasted as least several months, with some positive improvement detected at follow‐up. No major difference in outcome was found between the effects of the 2 forms of intervention |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised. Further details from investigator: "As quoted in the 1996 paper, at the end of the weekly clinical meetings, the therapists were asked to decide if the case met the criteria for a brief mother‐infant psychotherapy (they responded individually and then as a group to an ad hoc indication questionnaire. If yes, they had to [precis whether therapy was indicated] in two or three sentences which were verbatim registered. Then, if they agreed [to] mother‐infant psychotherapy, a random assignment to treatment condition was done. Then, the case was attributed to a therapist of the treatment that had been chosen by random, according to the therapist's [availability]" (email 23 May 2013) |
| Allocation concealment (selection bias) | Unclear risk | No details given. Investigator contacted by email 21 May 2013, but no further details about allocation concealment provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 72/75 completed at 1‐week follow‐up, 64/75 completed follow‐up at 6 months' post‐intervention (38/75 were contacted after 1 year but results not included in study report). Drop‐out was mainly due to change of address or unavailability Quote: "Written consent was obtained from all parents enrolled in the study. An indication for brief psychotherapy was assigned, after a pretreatment assessment (Evaluation l), for 88 of the 103 mother‐infant dyads (85%). Treatment was refused by 4 mothers (4%) and 6 had an early termination (6%). Among the 78 remaining cases, 75 mothers agreed to take part in the follow‐up and were included in the study. Seventy‐two mothers (96%) took part in the posttest assessment 1 week after the end of treatment (Evaluation 2), 64 mothers (86%) returned 6 months later (Evaluation 3). Attrition was mainly due to changes of address or unavailability at assessment time. Only 38 mothers (51%) were contacted 1‐year after treatment termination (Evaluation 4). This article, therefore, reports on 75 treated subjects having participated at Evaluation 2, Evaluation 3, or both." (Robert‐Tissot 1996a, p. 101) Further details from investigator: "There are no statistics available for [Evaluation] 4 as the research only focused on the first 3 [evaluations] due to sample attrition" (email 23 May 2013) |
| Selective reporting (reporting bias) | High risk | Pre‐specified outcomes were reported but not in groups, only summary statistics of both intervention groups combined versus a matched non‐randomised control were reported, and significance levels. Also only Episode 1,2 of Ainsworth Scales reported. We requested further data but the investigator no longer had access to this. A follow‐up study was produced but again the intervention groups (clinic group) data were combined (extensive interviews with 53/75 previous infants of the clinic group at 11 years of age, and their parents, to study their cognitive development, mental health, school achievement, and risk factors. This study was published in Cramer 2002 |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not described in study report Further details from investigator: "Clinical Psychologists who met parents and child at Evaluation 2 (E2) and Evaluation 3 (E3) were not blind to the treatment condition, because they participated, after E1, to the meeting with psychotherapists where the clinical data were presented and the indication for a brief mother‐infant psychotherapy done. Therefore, we cannot exclude the fact that some of them might have remembered, at E2 and E3, the type of therapy provided to patients" (email, 23 May 2013) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Further details from investigator: "the researchers who coded mother‐infant interactions, analysed and coded the responses to the different questionnaires were blind to the treatment condition" (email, 23 May 2013) |
| Other bias | Low risk | No differences in baseline characteristics |
Salomonsson 2011a.
| Methods | Randomised, 2‐arm comparison of infant‐led PIP versus child health centre (TAU) control Unit of allocation: participant Study dates: recruitment interviews took place from October 2005 to January 2008 |
|
| Participants |
Number randomised: 80 dyads Number randomised to each group: n = 40 PIP; n = 40 TAU Participants: mothers and infants (dyads) received therapy. Data on fathers' demographics were collected but fathers did not take part Sex of infants: PIP 40% boys; control 43% boys Age of child: PIP: mean 4.4 months (SD 2.4); control: mean 5.9 months (SD 3.8) Maximum age of infant at entry: < 18 months Ethnicity: not stated explicitly. PIP 11% 'immigrant'; control 22% 'immigrant' Recruitment: quote: "Nurses at five child health care centres (CHCC) who were collaborating with the project and had detected mother–infant disturbances informed the mothers about the project. Mothers also were recruited through information provided at the delivery ward of the Karolinska University Hospital and at parenting Internet sites. All mothers were given a leaflet that mentioned the joys of parenthood, but also explained that babies sometimes seem to be unhappy and mothers worry. We stated our interest in interviewing mothers and babies, and informing them of treatment modalities and that if they consented, they could participate in a randomized study. A paediatric check‐up was offered. Mothers contacted the project, and a 15‐min telephone interview was conducted by the first author" (Salomonsson 2011b; p. 212) Risk factors: mothers had expressed concerns about themselves as mothers, their infant's well‐being or their relationship with the infant. The SES of the parent participants was not reported, but a high proportion had a psychiatric disorder in adulthood (PIP 51%; control 60%) Country and setting: Sweden; university research clinic, psychotherapy delivered at the analyst's private facilities Child development: assumed to be typically developing Inclusion criteria: quote: "Criteria were that the mother should express significant concerns regarding one or more of the following domains: (a) herself as a mother, (b) her infant's well‐being, or (c) their relationship. This was operationalized as ≤ 80 ("perturbed relation") between mother and child on the Parent‐Infant Relationship Global Assessment Scale (PIR‐GAS; Zero to Three 2005) or ≥ 2.5 on the SPSQ (Östberg, Hagekull, & Wettergren, 1997). In addition, the following criteria had to be met: (d) The age of the infant was less than 18 months, (e) the duration of the mother's concerns was longer than 2 weeks, (f) their domicile was in Stockholm, and (g) the mother had a reasonable mastery of the Swedish language" (Salomonsson 2011b; p. 213) Exclusions: quote: "Exclusion criteria were kept to a minimum: (a) maternal psychosis or (b) substance dependence according to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision (DSM‐IV‐TR, 2000), to an extent that would preclude collaboration. No mother met these criteria" (Salomonsson 2011b; p. 213) Comparability of randomised groups at baseline: there was a statistically significant difference. T tests indicated that the MIP children were 1.5 months younger (t = 2.22, P value = 0.030), and had more somatic Axis III child conditions (t = 2.15, P value = 0.035), than did the TAU children. The TAU mothers demonstrated more Axis IV stressors (t = 2.46, P value = 0.016) |
|
| Interventions |
Duration of intervention: mean 10 weeks Number of sessions and frequency: MIP dyads had mean duration of 29 (SD 24.5) treatment sessions (median 23, range 0‐101; the mean session frequency was 2.5 (SD 1.0) weekly sessions (median 3, range 1‐4), that is, session frequency was 2 to 3 times weekly. Sessions lasted 50 minutes, treatment duration frequency and content were left to the participant's discretion Intervention: included child health care as usual. Quote: "In MIP treatment, the analyst's containment…of the infant's distress is believed to bring about change. The analyst receives and emotionally processes within him‐/herself the infant's distress and communicates it back to the infant in a form that the infant can assimilate. Thus, the containment process takes place predominantly in the infant–analyst dialogue, based on the belief that the distressed infant seeks containment from the analyst. The aim is to liberate the infant's affects that are assumed to be expressed in his or her symptoms such as whining, fussiness, sleeping and feeding problems, mood disturbances, and attachment problems. In the MIP method, the mother is always present and is often affected by the infant‐analyst interchange. As she witnesses their interaction, she will understand more about the links between her baby's affects and symptoms, which enables her to resume maternal care. For this to occur, the analyst needs to pay close attention to her self‐esteem, which often vacillates" (Salomonsson 2011b; p. 209) Control: quote: "The local child health centre is responsible for check‐ups from birth to 6 years of age. Nurse calls follow a regular schedule; weekly during the first month, monthly at 4 months and every second month during the rest of the first year followed by check‐ups at 1 and a half, 3, 4, and 5 years. The CHCC aims at assisting parents concerning their children’s physical, psychological, and social development " (Salomonsson 2011b; p. 211). Quote: “For the child health care centre care (CHCC) dyads, the staff initiated brief psychotherapies in four cases. Furthermore, four mothers sought individual or marital psychotherapy, and 4 continued to take antidepressants. On average, the psychotherapies comprised four (±2) sessions. Some were cognitive behavioural, others were psychodynamic. Twelve mothers elected to take part in any of these treatments, which were considered part of the usual care at CHCs. Their outcome data were included in the outcome analyses as CHCC cases without any corrections" (Salomonsson 2011b; p. 219) Type of psychodynamic model: based on Norman 2001; Norman 2004 Therapist: 7 of the psychoanalysts were women, 1 was a man, and all were members of the Swedish Psychoanalytic Society, a branch of the International Psychoanalytical Association. 3 were Doctor of Medicines, and 5 had a Master of Science degree in Psychology. Their mean professional experience as analysts was 19 years (SD 7.4), with 12 of those years (SD 5.6) treating children and 3 years (SD 1.1) treating mothers and infants. Trained in the Mother‐Infant Psychoanalysis Project in Stockholm Monitoring fidelity of the intervention: analysts met on a weekly basis for supervision and to maintain treatment adherence. Adherence was checked after the end of treatment when the first author interviewed the analyst and the mother (with the infant present) on separate occasions |
|
| Outcomes |
Timing of outcome assessment: post‐intervention, i.e. at 6 months following the start of the project (so within 16 weeks of end of therapy). Infant age at follow‐up not stated Outcomes Parent: maternal postnatal depression: EPDS (Cox 1987); maternal stress: SPSQ (Östberg 1997), a Swedish‐language version of the PSI (Abidin 1990) with 35 items; maternal general psychological distress symptom report GSI SCL‐90 (Derogatis 1994), a self report questionnaire containing 90 items rated from 0 to 4 Parent/infant interaction: mother‐baby relationship. The PIR‐GAS (GAS (ZERO TO THREE 2005) is an observer‐rated scale ranging from 1 to 10 (documented maltreatment) to 91 to 100 (well‐adapted); EAS (Biringen 1998) assessed video‐taped mother‐baby interactions of 10‐minute durations Child: infant social and emotional functioning. ASQ: SE (Squires 2002); items are rated on a 4‐step scale, with the exception of 4 items rated on a 2‐step scale; CHC records. To assess healthcare utilisation, records were requested, and somatic or psychological concerns, or visits other than routine calls, received 1 point. Infant and maternal ideal types and suitability for psychoanalysis are discussed in Salomonsson 2011c Clinician or participant report of outcomes: clinician and maternal reports |
|
| Notes |
Note: study comprised Salomonsson 2011b; Salomonsson 2011c. This project was registered at Clinicaltrials.gov, MIPPS‐01. Statement on informed consent can be found in the Method section of the published reports Adverse effects: none Funder: article supported by the Ahren, Axson Johnson, Engkvist, Golden Wedding Memorial of Oscar II and Queen Sophia, Groschinsky, Jerring, Kempe‐Carlgren, Mayflower Charity, Solstickan and Wennborg Foundations, and the Research Advisory Board of the International Psychoanalytical Association Aim: to compare the efficacy of PIP treatment with the usual form of CHCC, the therapies address maternal depression, mother‐reported infant social and emotional functioning, and mother infant relations. Mother‐reported stress and general psychic distress were reported. 2 additional secondary outcomes evaluated video‐taped mother‐infant interactions and the level of healthcare consumption Study investigator's conclusion: effects were non‐significant on maternal stress, mother‐reported infant functional problems, general psychic distress, maternal interactive structuring and non‐intrusiveness, infant responsiveness and involvement, and healthcare consumption. PIP treatment improved mother‐infant relationships and maternal sensitivity and depression, all of which are known to influence child development |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate. Quote: "At the end of the first interview, each mother was informed of the treatment alternatives. If she consented to randomisation, she picked a sealed envelope from a bag containing 40 tickets for each treatment type (MIP or CHCC)." and "We randomized during the interviews to deal with maternal reactions to the assignment. This was ethically preferable and conducive to reducing dropout and refuser rates" (Salomonsson 2011b; p. 213) |
| Allocation concealment (selection bias) | Low risk | To conceal treatment allocation, an official outside the project placed the tickets in identical (sealed) envelopes before the project started |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | A flow chart of participants and randomisation provided in Figure 2 of Salomonsson 2011b (p. 212). 60/80 dyads who were randomised completed treatment. 75 participants were included in the ITT analyses in the report of the study. Reasons for drop‐out from treatment lost to follow‐up given at each stage of the process |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported, but post‐intervention scores for healthcare consumption were not reported numerically, only as moderator of other treatment effects. Healthcare consumption not reported by group: "In contrast to our original hypothesis, the consumption of CHCC did not decrease significantly for dyads in MIP treatment" (p. 222) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors not blinded for assessments of depression (using the EPDS) but this is a maternal self report and unlikely to introduce bias. 2 raters with substantial clinical infant experience, both blinded to case history, interview content and assignments, rated EAS |
| Other bias | Low risk | In terms of participant characteristics at baseline, slightly older in CHCC (control) group |
Sleed 2013a.
| Methods | Cluster‐randomised, 2‐arm comparison of 'New Beginnings' programme and standard care controls in UK prisons Unit of allocation: prison MBU (cluster) Study dates: not reported |
|
| Participants |
Number randomised: n = 163 (mother‐infant dyads) in 7 prisons. 88 dyads in intervention prisons and 75 dyads in control prisons. All 7 women's prisons in the UK that had MBUs took part. 3 prisons allocated to intervention and 4 to controls Number randomised to each group: 3 intervention prisons: n = 88 consenting participants; 4 control prisons: n = 75 consenting participants Participants: mother and infant (dyads) in small groups received therapy Sex: intervention: 38.6% boys; control: 40% boys Age of child: 1‐23 months; intervention: mean 4.9 months (SD 4.5), range 0.2‐23.0 months; control: mean 4.4 months (SD 4.6), range 0.1‐18.5 months Maximum age of child at entry: intervention: 18.5 months; control: 23 months Ethnicity: intervention: 43.2% white, 42% black, 14.5% other (Asian, mixed or other); controls: 68% white, 20% black, 12% other Recruitment: during the recruitment phase, the research team liaised regularly with the MBU staff to ascertain the numbers of new mothers and babies. As soon as there were sufficient numbers of new dyads in the intervention sites, a New Beginnings course was arranged and these mothers and babies were invited to participate in the intervention and research. In the control sites, the researcher paid regular visits to the prisons to recruit and interview new mothers who had entered the units Risk factors: prison population ‐ infants incarcerated with their mothers in prison MBUs. The environment may have consequences for the mother‐infant relationship Social and economic status: prisoners; no details given other than educational status. Intervention: 64.8% no qualifications or basic education only; control: 64% no qualifications or basic education only Setting: UK; female prisons with MBUs, conducted 2006‐2009. Intervention delivered in group session with baby mat on the floor Child development: not stated Inclusion criteria: mother‐baby dyads staying on MBUs in the participating prisons during the recruitment period were eligible to take part in the study Exclusions: dyads were excluded if the mother was not sufficiently fluent in English to be able to give informed consent or take part in the research, or if she and her baby were known to be due for release before the first follow‐up interview Comparability of randomised groups at baseline: the intervention and control groups were not perfectly matched at baseline. The study investigators stated that "This is likely to be the result of cluster randomization. The intervention prisons were geographically closer to the international airports and therefore may have included an over‐representative number of non‐national mothers and babies, leading to ethnic and language differences between the two groups" (p. 215). Mothers in the control group tended to have higher levels of reflective functioning and better quality interactions with their infants at baseline than those in the intervention group. Group differences tested by Chi2 test were not significant |
|
| Interventions |
Duration of intervention: 4 weeks Number of sessions and frequency: 8 sessions (2 sessions, each lasting 2 hours per day, 1 day per week) over 4‐week period. The mean number of clinical sessions attended was 7.1 (SD 1.6). Most (87%) of the mothers and babies attended at least half of the sessions offered Type of psychodynamic model: further information from study investigator (email 30 August 2013): "The New Beginnings programme would be classified as a group based PIP intervention. The programme is developed, facilitated and supervised by a team of experienced parent‐infant psychotherapists and very much informed by PIP principles and practice." Quote: "New Beginnings is a manualized attachment‐based intervention developed specifically for mothers and babies in prison (Baradon 2006). Details of the development and content of the intervention have been reported elsewhere (Baradon 2008)." In Baradon 2008, the intervention is described on p. 2443: "More specifically, the New Beginnings programme was geared towards making mothers more cognisant of their babies' intersubjective and attachment needs as separate from their own and, thus, towards increasing their range of contingent responses to the infant. Increasing the mothers' capacity for mentalisation (may be facilitated by the discussion of dedicated topics that link past and present patterns of relating, and by the careful observation of, and reflection on, non‐conscious behaviours between mother and baby. The mother's ability to produce a genuine narrative of the baby's thoughts, feelings, wishes and subjectivity in general has been demonstrated to be associated with secure attachment in a number of studies. The strongest evidence for this comes from observations that the inclination of mothers to take a psychological perspective on their child, including maternal mind‐mindedness and reflective function in interacting with or describing their infants, is associated with both secure attachment and mentalisation." The study investigator confirmed that: "The programme is developed, facilitated and supervised by a team of experienced parent‐infant psychotherapists and very much informed by parent‐infant psychotherapy principles and practice" (p. 3) Intervention: New Beginnings programme versus control receiving standard prison health and social care. New Beginnings is an attachment‐based, manualised group intervention developed specifically for mothers and babies in prison (see above). Each programme was carried out over 8 sessions over a 4‐week period. The groups were comprised of up to 6 mother‐baby dyads and 2 parent‐infant psychotherapists as facilitators. All sessions took place on a baby mat on the floor so that the babies were able to participate actively in the sessions. Specific topics were covered through group discussion, handouts, individual worksheets and homework tasks. The topics of each session were selected as potential triggers of the attachment relationship. These were explored through discussions of dedicated topics that link past and present patterns of relating, and by the careful observation of, and reflection on, non‐conscious behaviours between mothers and babies Control: quote: "The New Beginnings courses were not held in the control prisons during the study period. The MBU units were otherwise very similar for both the intervention and control groups. Mothers and babies in both groups had access to standard health and social care provision as provided by the prison service" (p. 7) Therapist: 2 parent‐infant psychotherapists as facilitators for each group session, no details about training Monitoring fidelity of the intervention: adherence checklist used, alongside regular clinical supervision (these details supplied by investigator email to Dr Nick Midgley 27 March 2013). Details of how the checklist was used or level/frequency of supervision not stated |
|
| Outcomes |
Timing of outcome assessment: at 5 weeks after baseline (i.e. immediately post‐intervention; intervention was 4 weeks' duration). Follow‐up at 2 months after end of treatment, but only for those dyads remaining in prison and no data were reported for this time point. Quote: "The very small number of dyads who were available for the second follow‐up did not allow for this data point to be reliably included in the analysis" (p. 9) Outcomes Parent: parental reflective functioning (PDI, Slade 2004), maternal depression, CES‐D (Radloff 1977), and maternal representations, MORS (Danis 2005). All self reported Parent/infant: mothers and their infants were video‐taped in free‐play for 10 minutes. Mothers were asked to "be with your baby as you usually are". These video‐taped interactions were coded using the CIB scales (Feldman 1998) for the subscales of dyadic attunement, parent positive engagement and child involvement) Child: none Adverse effects: none Clinician or participant report of outcomes: clinician for all outcomes except CES‐D and MORS, which were self reported by mothers |
|
| Notes |
Note: cluster randomised, group‐based intervention Funder: not stated Aim: to examine the impact and relative effects of this attachment based intervention on the mother‐infant relationship in a prison environment Study investigator's conclusion: mothers in the control group deteriorated in their level of reflective functioning and behavioural interaction with their babies over time, whereas the mothers in the intervention group did not. There were no significant group effects on levels of maternal depression or mothers' self reported representations of their babies over time. An attachment‐based intervention may mitigate some of the risks to the quality of the parent‐infant relationship for these dyads |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Cluster‐randomised. Prisons served as clusters and were randomly assigned to the intervention or control conditions. Computer randomisation (external to trial) |
| Allocation concealment (selection bias) | Low risk | No details given other than that randomisation was carried out by independent statistician Further details from principal investigator: "Random allocation was carried out by an external statistician in the US who had no knowledge of or affiliation with any of the UK prisons being allocated. The randomisation of all prisons was carried out at once and allocation sequence was therefore not an issue" (email, 13 December 2013) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 62/88 completed intervention. The attrition rates of the sample being lost to follow‐up at time 2 were 29% and at time 3 were 83%. Most dyads could not be followed up as they had been released from, or moved to, a different prison. There were no significant differences between drop‐outs and participants who were followed up. 88 started intervention, 62 were available for follow‐up at time 2, and 19 were available at time 3. In the control group, 75 started, 53 were available at time 2, and 8 at time 3 (mainly due to prison‐release or moving from prison). The very small number of dyads who were available for the second follow‐up did not allow for these data points to be included reliably in the analysis |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No details given. As this was a cluster‐randomised trial, participants would possibly be unaware that they had been assigned to the treatment arms but the personnel delivering the intervention would be aware of randomisation status Further information from trial investigator: "this was a cluster randomised controlled trial and it was not possible, for pragmatic and ethical reasons, to conceal allocation from the prison staff, researchers or participants prior to recruiting participants. To reduce selection bias, all eligible mothers in the MBU's at the time of recruitment were approached and invited to participate in the study. However, a slightly higher proportion of mothers in the control prisons chose not to participate in the research than in the intervention prisons, which may have introduced a selection bias" (email 5 December 2013) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Coders blind for PDI and CIB. Coding was carried out by trained coders who were blind to both the group and time point |
| Other bias | Low risk | At baseline, more white mothers in control group |
AAPI: Adult‐Adolescent Parenting Inventory; ANOVA: Analysis of Variance; AQS: Attachment Q‐Set; ASQ: SE: Ages and Stages Questionnaire: Social‐Emotional; BDI: Beck Depression Inventory; BSID: Bayley Scales of Infant Development; BSQ: Behavioural Screening Questionnaire; CARE‐Index: Child‐Adult Relationship Experimental Index; CBCL: Child Behavior Checklist; CBT: cognitive behavioural therapy; CES‐D: Center for Epidemiologic Studies Depression Scale; CHCC: Child Health Centre Care; CIB: Coding Interactive Behavior; CPP: Child‐Parent Psychotherapy; CPS: Child Protective Service; CS: Community Standard controls; CTQ: Childhood Trauma Questionnaire; DAS: Dyadic Adjustment Scale; df: degrees of freedom; DIS‐IV: Diagnostic Interview Schedule Version IV; DSM‐III‐R: Diagnostic and Statistical Manual of Mental Disorders ‐ Third Edition ‐ Revised (DSM‐III‐R); dyad: a mother and infant pair; EAS: Emotional Availability Scales; EPDS: Edinburgh Postnatal Depression Scale; FES: Family Environment Scale; GSI: General Severity Index; IPP: Infant‐Parent Psychotherapy; IQ: intelligence quotient; ISEL: Interpersonal Support Evaluation List; ITT: intention to treat; KIA/KIDIES Profile (Kiddie‐Infant Affect Profile of Child Mood and Affect; LEI: Life Event Inventory; MBQ: Maternal behaviour (Q set); MBUs: mother and baby units; MDI: Mental Development Index; MIP: mother‐infant psychotherapy; MORS: Mother's Object Relations Scales; NHS: National Health Service (UK); NIMH: National Institute of Mental Health (USA); n: number; p.: page; PAAS: Perceptions of Adult Attachment Scale; PDI: Parent Development Interview; PBCL: Preschool Behaviour Checklist; PhD: Doctor of Philosophy; PIP: parent‐infant psychotherapy; PIR‐GAS: Parent‐Infant Relationship Global Assessment Scale; PPI: psychoeducational parenting intervention; PPT: psychodynamic psychotherapy; PSI: Parenting Stress Index; PSOC: Parenting Sense of Competence; PSS: Perceived Stress Scale; RCT: randomised controlled trial; SCL‐90: Symptom Checklist ‐ 90; SD: standard deviation; SES: socioeconomic status; SPSQ: Stress and Parenting Stress Questionnaire; SSB: Social Support Behaviours; SSP: Strange Situation Procedure; TAU: treatment‐as‐usual; TPP: Toddler‐Parent Psychotherapy; WPPSI‐R: Wechsler Preschool and Primary Scales of Intelligence; WWW: Infant‐Led Parent‐Infant Psychotherapy 'Watch Wait and Wonder'.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bakermans‐Kranenburg 2008 | RCT, but not PIP |
| Baradon 2008 | Not RCT or quasi‐RCT. Controlled‐clinical trial. Pilot of method ‐ 'New Beginnings' ‐ cluster‐randomised trial. No data for randomised trial that followed (Sleed 2013b) |
| Barrera 1986 | RCT, but not PIP. Met inclusion criteria for age and randomisation. There was a parent‐infant group intervention that focused on improving interaction rather than teaching specific skills but this was not rooted in a psychodynamic tradition |
| Beeber 2013 | RCT, but not PIP. Age‐group met the inclusion criteria for this review, but treatment was IPT |
| Belt 2007 | Not RCT or quasi‐RCT, but PIP in substance‐abusing mothers |
| Belt 2013 | Not RCT or quasi‐RCT, but case study |
| Brisch 1996 | Not PIP |
| Brisch 2003 | Not PIP, but individual psychotherapy for the parent, and not PIP working with dyads |
| Brown 1998 | Not RCT or quasi‐RCT, but investigated the process of infant‐parent psychotherapy in a field setting |
| Carvalho 2009 | Not PIP |
| Cicchetti 2011b | Not PIP, but genetic study of research participants |
| Clark 2003 | Not RCT or quasi‐RCT. Controlled‐clinical trial using 'sequential allocation' i.e. group assignment as needed to fill each group. Summarised a trial of PIP. Mother‐infant therapy for women with moderate‐to‐severe depressive symptoms postpartum. Described an RCT in progress in 2008 (see Characteristics of ongoing studies table) |
| Compas 2011 | Not PIP |
| Cooper 2009 | Not PIP |
| Dawe 2007 | Not RCT or quasi‐RCT, but commentary on Cicchetti 1999a |
| Dozier 2008 | Not PIP |
| Fisher 1980 | Not PIP |
| Fraiberg 1981 | Not RCT or quasi‐RCT, but case history of an 'at‐risk' infant with anorexic depressed mother |
| Frisch 2013 | Not RCT or quasi‐RCT. Infant‐age greater than inclusion criteria. Not PIP |
| Gao 2012a | Not PIP |
| Gao 2012b | Not PIP |
| Ghosh 2011 | Child > 4 years of age, reanalysis of Lieberman 2005 |
| Goodman 2013 | Not RCT or quasi‐RCT, but reported a pilot use of perinatal dyadic psychotherapy with 6 acutely depressed postpartum women (see Characteristics of ongoing studies table) |
| Hayes 2008 | Not PIP |
| Herve 2009 | Not RCT or quasi‐RCT, but study of factors that were predictive of outcome for children and parents following a brief parent‐infant psychotherapy |
| Jardim 2007 | Not PIP |
| Kaplan 2011 | Not RCT or quasi‐RCT, but history of the PPP, its underlying assumptions, and case study of specific interventions with a family. |
| Lara 2010 | Not PIP, but RCT of antenatal psychotherapy for prevention of depression in at‐risk women |
| Lieberman 1999 | Not RCT, but overview of PIP. No additional outcome data or reports of trials not otherwise identified |
| Lieberman 2005 | RCT of child‐parent psychotherapy in at‐risk population (exposed to marital violence), participants were children and their mothers, but children do not fit age criteria for our review, i.e. too old (the participants were aged 3‐5 years (mean 4.06 years, SD 0.82) |
| Mays 2013 | Not RCT or quasi‐RCT, but case study |
| Meijer 2011 | Not PIP |
| Mulcahy 2010 | Not PIP |
| Pollock 1996 | Not PIP |
| Punamäki 2013 | Not RCT or quasi‐RCT. Probably PIP (although not clear if babies were included in intervention) |
| Ravn 2012 | RCT, age range met criteria for our review and was a dyadic intervention. Not PIP. This was a psychoeducational approach without any psychodynamic basis |
| Robert‐Tissot 1998 | Not RCT or quasi‐RCT, but study of effectiveness (maternal choices influence treatment) |
| Sadek 2013 | Not RCT or quasi‐RCT, but review article |
| Santelices 2011 | Not PIP |
| Santos 2006 | Not PIP |
| Sleed 2013b | Not RCT or quasi‐RCT, but controlled clinical trial of hostel‐based PIP (1 intervention hostel and 4 comparison hostels) |
| Smyrnios 1993 | RCT of PIP, but children did not fit age criteria for this review (i.e. too old, at least 7.5 years old) |
| Spinelli 2003 | Not PIP |
| Stoleru 1994 | Not RCT or quasi‐RCT, but 2 case reports of PIP |
| Svanberg 2010 | Not PIP |
| Swartz 2006 | Not PIP |
| Swartz 2008 | Not PIP |
| Torres 2011 | Not RCT or quasi‐RCT, but study of group intervention for infant‐mother attachment, spanned a period of 14 months starting from the 3rd quarter of pregnancy |
| Toth 2002 | RCT, but children did not fit age criteria for this review (i.e. too old, pre‐school children 4 years of age; mean = 48.18 months, SD = 6.88) |
| Toth 2011 | Not RCT or quasi‐RCT, but book chapter of relational interventions (including PIP) for young children who have been maltreated |
| Toth 2012 | PIP, overview of research and evidence base for relational interventions for maltreated children |
| Van Horn 2011 | Not RCT or quasi‐RCT, but book chapter, reports the evidence base (including PIP) for child‐parent psychotherapy with traumatised young children in kinship care. |
| Van Zeijl 2006 | Not PIP |
| Vliegen 2013 | Not RCT or quasi‐RCT, but naturalistic follow‐up of group PIP |
| Wan 2008 | Not RCT or quasi‐RCT, but review article. No additional reports of trials or outcome data |
| Woodhead 2006 | Not PIP |
| Yang 2009 | Not PIP |
| Zelkowitz 2008 | Not PIP |
IPT: interpersonal therapy; PIP: parent‐infant psychotherapy; RCT: randomised controlled trial; quasi‐RCT: quasi‐randomised controlled trial; SD: standard deviation
Characteristics of ongoing studies [ordered by study ID]
ISRCTN38741417.
| Trial name or title | Helping Parents with Mental Health Problems to Parent Young Infants: a Randomised Controlled Trial of Parent‐Infant Psychotherapy |
| Methods | RCT |
| Participants | Clinically referred mothers with identified mental health difficulties and infants < 12 months of age |
| Interventions | Open‐ended parent‐infant psychotherapy and treatment‐as‐usual |
| Outcomes | Parental mental health, parent‐infant interactions, parental reflective functioning, infant development and infant attachment |
| Starting date | June 2007 |
| Contact information | Peter Fonagy and Michelle Sleed (Michelle.Sleed@annafreud.org) |
| Notes | Completed, but no study results available as yet ISRCTN registration number 38741417 |
NCT00051246.
| Trial name or title | Group Therapy for Postpartum Depression |
| Methods | Randomised, parallel, 2‐arm |
| Participants |
Eligibility Age: ≥ 18 years Gender: female Accepts healthy volunteers: no Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Active comparator 1:
Behavioural:
Active comparator 2:
|
| Outcomes |
Primary outcome measures:
Secondary outcome measures:
|
| Starting date |
Study start date: January 2002 Estimated study completion date: July 2008. Completed, but no study results available as yet |
| Contact information | Please refer to this study by its ClinicalTrials.gov identifier: NCT00051246 Locations: Wisconsin, US University of Wisconsin, Department of Psychiatry, Madison, Wisconsin, US Sponsors and collaborators: National Institute of Mental Health (NIMH) Principal investigator: Roseanne Clark, PhD University of Wisconsin, Madison |
| Notes | 10‐20% of new mothers experience major depression in the postpartum period (i.e. PPD). This condition poses a risk for disturbances in the mother‐infant relationship as well as for developmental delays and subsequent psychopathology in their children. Thus, an investigation of the efficacy of a relational approach that focuses on improving the mother's sense of competence in the parenting role, and reducing depressive symptoms and social isolation through group therapy, is warranted. Participants are randomly assigned to either relational group treatment or to standard individual treatment. Assessments of maternal and infant functioning, mother‐infant and father‐infant relations, parenting stress and marital conflict, and conducted pre‐ and post‐treatment, at 12‐months post‐treatment, and when infants are 12 and 24 months of age |
NCT01744041.
| Trial name or title | Mommy‐Baby Treatment for Perinatal Depression |
| Methods | Allocation: randomised Intervention model: parallel assignment Masking: open label Primary purpose: treatment |
| Participants |
Enrolment: n = 40 Inclusion criteria:
Exclusion criteria:
|
| Interventions | Behavioural: dyadic IPT versus other: enhanced treatment‐as‐usual Experimental:
Active comparator:
|
| Outcomes | Change in EPDS from baseline:
|
| Starting date |
Study start date: November 2012 Study completion date: completing October 2015 (final data collection date for primary outcome measure) |
| Contact information |
Principal investigator: Shannon Lenze, PhD Washington University and National Institute of Mental Health (NIMH), USA |
| Notes | Perinatal depression is a major public health problem, affecting 15% of women during pregnancy through the postpartum period, with adverse consequences for the mother, fetus, infant, and family. Despite increasing evidence of the importance of this critical risk interval, little research has investigated the effects of depression treatment during pregnancy on infant outcomes. The purpose of this study is to test the feasibility, acceptability, and effectiveness of a new intervention: IPT for the mother‐infant dyad (IPT‐Dyad). This intervention begins during pregnancy and continues with the mother and infant until 1‐year postpartum. The investigators hypothesise that IPT‐Dyad will be better than treatment‐as‐usual in reducing depressive symptoms, improving psychosocial functioning, increasing parenting self efficacy, improving infant emotional development, and enhancing mother‐infant relationship quality |
NCT01888809.
| Trial name or title | Building Healthy Children (BHC): Evidence‐Based Home Visitation Integrated with Paediatric Medical Homes |
| Methods | Randomised trial combining 3 evidence‐based services versus screening and referral to community services only |
| Participants |
Enrolment:
Inclusion criteria:
Exclusion criteria:
|
| Interventions | Treatment families receive parents as teachers, child‐parent psychotherapy and IPT as needed. Outreach workers assist with concrete needs, including transportation to medical visits Experimental:
Active comparator: screening and referral to annual screening, referral for services as needed |
| Outcomes |
|
| Starting date |
Study start date: August 2007 Study completion date: August 2016 (final data collection date for primary outcome measure) |
| Contact information |
Principal investigator Heather Paradis (Heather_Paradis@URMC.Rochester.edu) Trial data handled by Dr Jody Todd Manly, publication in progress (jody.manly@rochester.edu) Sheree L Toth, PhD (sheree_toth@URMC.rochester.edu) |
| Notes | Separate data for child‐parent psychotherapy only participants requested "Building Healthy Children is a collaboration of social service and health care agencies, each providing evidence‐based services to intervention families in a seamless package. Low‐income parents who gave birth to their first child when they were under 21 and who were not involved in the child welfare system were targeted as an at‐risk group for whom home visitation services would offer optimal preventive and cost‐efficiency outcomes. Services include Interpersonal Psychotherapy [IPT] for maternal depression and Child Parent Psychotherapy [CPP] for maternal‐child relationship development and trauma treatment, and Parents As Teachers [PAT]. Families are provided a tiered complement of BHC services based upon risk and current need. Case management and outreach services are key to assure family engagement and full program participation. An assigned community outreach worker provides a consistent, nurturing relationship that helps retain families in the program and readies parents for the evidence‐based treatments, movement towards goals, and behavior change. Outreach workers help to stabilise families and ensure compliance with medical appointments and recommended care. Most importantly, BHC home‐based services are integrated with primary care practices: pediatric, family medicine, and federally qualified neighborhood health center. These comprehensive services are compared with a screening and referral only group in a randomized design. Integration with the child's medical home is an all‐inclusive approach to improve child health and well‐being and to achieve desired program outcomes. Building Healthy Children program, it is likely to be very difficult to analyze the data separately for parents who participate in CPP because of the integrated delivery model. The evaluation design was not set up to specifically evaluate CPP, but instead to evaluate the integration of CPP within the child's medical home and within a comprehensive service array of evidence‐based interventions tailored to the individual needs of the family. However, we have completed several evaluations of CPP in the past" |
NCT02057627.
| Trial name or title | Mother‐Infant Intervention for Postpartum Depression and Associated Mother‐Infant Relationship Dysfunction |
| Methods | RCT |
| Participants | Depressed new mothers |
| Interventions | Perinatal dyadic psychotherapy vs. control |
| Outcomes | Reduction of depression and anxiety symptoms |
| Starting date | June 2010. Completed July 2012, but no study results available as yet |
| Contact information | jgoodman@MGHIHP.edu |
| Notes | Referred to in Goodman 2013 |
BHC: Building Healthy Children; DD‐NOS: depressive disorder not otherwise specified; EPDS: Edinburgh Postnatal Depression Scale; ERA: Early Relational Assessment; HRSD: Hamilton Rating Scale for Depression; IPT: interpersonal psychotherapy; RCT: randomised control trial; MDD: major depressive disorder; PPD: postpartum depression; SCID‐IV: Structured Clinical Interview for DSM Disorders.
Differences between protocol and review
We modified the protocol as follows.
We stated that a systematic review of this topics is important as there is a need to develop empirically derived models that can support vulnerable parents and their children.
We provided further details in the 'Background' section of the review to differentiate parent‐infant psychotherapy (PIP) from other home visiting approaches. We clarified that we included interventions delivered to dyads in a small group setting; that psychotherapy focuses on improving infant attachment security by targeting parental internal working models (i.e. representational world) and working directly with the parent‐infant relationship; that focus on the parent‐infant relationship/interaction (not just maternal representations); and are aimed primarily at improving attachment security or infant socio‐emotional functioning, or both.
We clarified that we excluded interventions that were purely delivered to the parent (e.g. interpersonal psychotherapy), or which were primarily psycho‐educational, or which were primarily based on other therapeutic models (e.g. cognitive behavioural therapy) or were focused on parent‐infant interaction in a purely behavioural way. We excluded stand‐alone video‐interaction guidance interventions, but not studies in which video feedback was incorporated into a PIP that included the core components. We excluded psychotherapy working only with the parent.
We clarified that we included birth parents (mothers and fathers), adoptive and kinship parents, but did not include foster parents.
For the purposes of this review, we referred to the included children as infants irrespective of the term used to describe them in the study report (e.g. children, toddlers).
We included studies of PIPs that included additional components (i.e. provided they still met the core inclusion criteria).
We clarified that we recorded information about monitoring the fidelity of the intervention during the course of the trial, in order to ascertain whether or not the intervention was delivered as intended.
We previously specified in our protocol that the maximum age of the infants at entry into the study should be 24 months or less; it should have stated that the mean age of the infants should 24 months or less at the point of referral. In this review, we included two studies where the maximum age of the infants was 30 months at study entry, but the mean age of the infant participants at entry was below 24 months in keeping with our inclusion criteria (Cohen 1999b; Robert‐Tissot 1996a).
The decisions about combining data were made post hoc and based on the categories of interventions, participants, and outcomes identified in the reviewed literature.
For studies where there was more than one active intervention and only one control group, we had intended to select the intervention that most closely matched our inclusion criteria and exclude the others (see Higgins 2011, Chapter 16.5.4). However, because we found some head‐to‐head comparisons of PIP versus other interventions, we conducted analyses on intervention versus control and one intervention (PIP) versus another intervention, and we were able to include studies that used more than one intervention by splitting the participant numbers in the shared (PIP) intervention group. One study comprised three intervention arms and one control arm (Cooper 2003a). We combined the two non‐PIP intervention groups into one to create two pairwise comparisons (intervention versus control and PIP versus other intervention), using statistical methods to pool the mean and standard deviation for continuous outcomes where applicable.
We made a post‐hoc decision based on editorial comments to conduct sensitivity analyses for a fixed‐effect and a random‐effects model and intraclass correlation coefficient (ICC) imputations. There was little difference between point estimates for analyses using a random‐effects or a fixed‐effect model, with no impact on the overall conclusions of treatment effects with the exceptions of two outcomes. We added a new subsection of "sensitivity analyses" where we summarised the results from sensitivity analyses.
We included 'Summary of findings' tables for the outcomes of parental depression and infant attachment. We added a section to the methods of the review to describe how we constructed the 'Summary of finding' tables (GRADEpro 2014), and how we applied the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) system to rate the overall quality of evidence.
For statistical assessment of heterogeneity, we have added the tau2 estimates for each meta‐analysis. We now comment on the heterogeneity of each meta‐analysis by looking at and reporting all of the following statistics: Chi2, P value, tau2, and I2 statistic.
We edited the background text of this review after the publication of the protocol, in response to comments from Dr Aron Schlonsky, Campbell Collaboration Social Welfare Coordinating Group, and Dr Nick Midgley (review author).
Contributions of authors
JB secured funding for the review and is the contact author and guarantor of the review. JB drafted the text of the review with CB and NM.
CB screened studies with JB and NM, extracted data with JB and NM, entered data into Review Manager 5 (RevMan 2012), characteristics of studies tables and analyses, carried out 'Risk of bias' assessments, drafted the analysis and results sections, edited the review, provided support to the authors in the use of Review Manager 5, and maintained the review reference management databases. CB also contacted principal investigators for further details and study characteristics.
NM screened literature searches for potentially included studies, finalised the included studies lists, provided advice about outcomes, commented and edited the text. NM also obtained additional data about the included studies.
NM and CB provided additional references and comments on the text of the protocol.
SL extracted data for the 'Characteristics of included studies' tables and carried out 'Risk of bias' assessments.
YW conducted the intraclass correlation coefficient analyses, gave advice on statistical methods, and assisted with production of the 'Summary of findings' tables.
Sources of support
Internal sources
No sources of support supplied
External sources
-
PIP UK, UK.
Charitable organisation with a remit to establish parent‐infant psychotherapy services across England who provided financial support for the conduct of this review
Declarations of interest
Funding for this review has been received from PIP UK, a charitable organisation led by Andrea Leadsom (MP) to establish and evaluate parent‐infant psychotherapy programmes.
Jane Barlow ‐ editor with the Cochrane Developmental, Psychosocial and Learning Problems Group and Co‐Chair of the Campbell Social Welfare Group.
Cathy Bennett ‐ proprietor of Systematic Research Ltd, a company providing research services, and employee of that company; received a consultancy fee from the PIP UK grant for contribution to this review, as well as travel expenses for travel to work‐related meetings and conferences. Cathy also received consultancy fees for other Cochrane reviews and work in evidence‐based medicine. Cathy is a member of the data monitoring committee for the Barrett's Oesophagus Surveillance Study (BOSS), this work is not related to review writing.
Nick Midgley ‐ employed by Anna Freud Centre, which offers a parent‐infant psychotherapy service. One of the studies reviewed is based on work from this team; however, his role in the Centre is not connected with the parent‐infant psychotherapy service in any way. Nick is a recipient of funding to conduct the review from PIP UK.
Soili Larkin ‐ none known.
Yinghui Wei ‐ received a consultancy fee for her work on this review.
Cathy Bennett is a co‐first author with Jane Barlow on this review.
New
References
References to studies included in this review
Cicchetti 1999a {published data only}
- Cicchetti D, Rogosch FA, Toth SL. The efficacy of toddler‐parent psychotherapy for fostering cognitive development in offspring of depressed mothers. Journal of Abnormal Child Psychology 2000;28(2):135‐48. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL, Rogosch FA. The efficacy of toddler‐parent psychotherapy to increase attachment security in offspring of depressed mothers. Attachment & Human Development 1999;1(1):34‐66. [DOI] [PubMed] [Google Scholar]
- Toth SL, Rogosch FA, Manly JT, Cicchetti D. The efficacy of toddler‐parent psychotherapy to reorganize attachment in the young offspring of mothers with major depressive disorder: a randomized preventive trial. Journal of Consulting and Clinical Psychology 2006;74(6):1006‐16. [DOI] [PubMed] [Google Scholar]
Cicchetti 2006b {published data only}
- Cicchetti D, Rogosch FA, Toth SL. Fostering secure attachment in infants in maltreating families through preventive interventions. Development and Psychopathology 2006;18(3):623‐49. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL, Sturge‐Apple ML. Normalizing the development of cortisol regulation in maltreated infants through preventive interventions. Development and Psychopathology 2011;23(3):789‐800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stronach EP, Toth S, Rogosch F, Cicchetti D. Preventive interventions and sustained attachment security in maltreated children. Development and Psychopathology 2013;25(4 Pt 1):919‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen 1999b {published data only}
- Cohen NJ, Lojkasek M, Muir E, Muir R, Parker CJ. Six‐month follow‐up of two mother‐infant psychotherapies: convergence of therapeutic outcomes. Infant Mental Health Journal 2002;23(4):361‐80. [Google Scholar]
- Cohen NJ, Muir E, Lojkasek M, Muir R, Parker CJ, Barwick M, et al. Erratum. Watch, Wait, and Wonder: testing the effectiveness of a new approach to mother‐infant psychotherapy. Infant Mental Health Journal 2000;21(1‐2):131. [Google Scholar]
- Cohen NJ, Muir E, Lojkasek M, Muir R, Parker CJ, Barwick M, et al. Watch, Wait and Wonder: testing the effectiveness of a new approach to mother‐infant psychotherapy. Infant Mental Health Journal 1999;20(4):429‐51. [Google Scholar]
Cooper 2003a {published data only}
- Cooper PJ, Murray L, Wilson A, Romaniuk H. Controlled trial of the short‐ and long‐term effect of psychological treatment of post‐partum depression. I. Impact on maternal mood. British Journal of Psychiatry 2003;182(5):412‐9. [PubMed] [Google Scholar]
- Murray L, Cooper PJ, Wilson A, Romaniuk H. Controlled trial of the short‐ and long‐term effect of psychological treatment of post‐partum depression: 2. Impact on the mother‐child relationship and child outcome. British Journal of Psychiatry 2003; Vol. 182, issue 5:420‐7. [PubMed]
Lieberman 1991 {published data only}
- Lieberman AF, Weston DR, Pawl JH. Preventive intervention and outcome with anxiously attached dyads. Child Development 1991;62(1):199‐209. [PubMed] [Google Scholar]
Robert‐Tissot 1996a {published data only}
- Cramer B, Robert‐Tissot C, Rusconi Serpa S. Du Bébé au Préadolescent. Une Etude Longitudinale. Paris: Odile Jacob, 2002. [Google Scholar]
- Robert‐Tissot C, Cramer B, Stern DN, Serpa SR, Bachmann J‐P, Palacio‐Espasa F, et al. Outcome evaluation in brief mother‐infant psychotherapies: report on 75 cases. Infant Mental Health Journal 1996;17(2):97‐114. [Google Scholar]
Salomonsson 2011a {published data only}
- Salomonsson B, Sandell R. A randomized controlled trial of mother‐infant psychoanalytic treatment: I. Outcomes on self‐report questionnaires and external ratings. Infant Mental Health Journal 2011; Vol. 32, issue 2:207‐31. [DOI: 10.1002/imhj.20291] [DOI] [PubMed]
- Salomonsson B, Sandell R. A randomized controlled trial of mother‐infant psychoanalytic treatment: II. Predictive and moderating influences of qualitative patient factors. Infant Mental Health Journal 2011; Vol. 32, issue 3:377‐404. [DOI: 10.1002/imhj.20302] [DOI] [PubMed]
- Salomonsson B, Sandell R, Werbart A, Rydelius P‐A. Psychoanalytic treatment of problems in the mother‐child relation. A randomized controlled trial shows significant therapeutic effects. Lakartidningen 2011; Vol. 108, issue 18:984‐7. [PUBMED: 21809525] [PubMed]
Sleed 2013a {published data only}
- Anna Freud Centre. New Beginnings. www.annafreud.org/pages/new‐beginnings.html (accessed 20 November 2014).
- Sleed M, Baradon T, Fonagy P. New Beginnings for mothers and babies in prison: a cluster randomized controlled trial. Attachment & Human Development 2013; Vol. 15, issue 4:349‐67. [DOI] [PMC free article] [PubMed]
References to studies excluded from this review
Bakermans‐Kranenburg 2008 {published data only}
- Bakermans‐Kranenburg MJ, Ijzendoorn MH, Mesman J, Alink LR, Juffer F. Effects of an attachment‐based intervention on daily cortisol moderated by dopamine receptor D4: a randomized control trial on 1‐ to 3‐year‐olds screened for externalizing behavior. Development and Psychopathology 2008;20(3):805‐20. [DOI] [PubMed] [Google Scholar]
Baradon 2008 {published data only}
- Baradon T, Fonagy P, Bland K, Lenard K, Sleed M. New Beginnings ‐ an experience‐based programme addressing the attachment relationship between mothers and their babies in prisons. Journal of Child Psychotherapy 2008;34(2):240‐58. [Google Scholar]
Barrera 1986 {published data only}
Beeber 2013 {published data only}
- Beeber LS, Schwartz TA, Holditch‐Davis D, Canuso R, Lewis V, Hall HW. Parenting enhancement, interpersonal psychotherapy to reduce depression in low‐income mothers of infants and toddlers. Nursing Research 2013; Vol. 62, issue 2:82‐90. [PUBMED: 23458906] [DOI] [PMC free article] [PubMed]
Belt 2007 {published data only}
- Belt R, Punamaki R‐L. Mother‐infant group psychotherapy as an intensive treatment in early interaction among mothers with substance abuse problems. Journal of Child Psychotherapy 2007;33(2):202‐20. [Google Scholar]
Belt 2013 {published data only}
- Belt RH, Kouvo A, Flykt M, Punamäki R‐L, Haltigan JD, Biringen Z, et al. Intercepting the intergenerational cycle of maternal trauma and loss through mother–infant psychotherapy: a case study using attachment‐derived methods. Clinical Child Psychology and Psychiatry 2013; Vol. 18, issue 1:100‐20. [PUBMED: 22569679] [DOI] [PubMed]
Brisch 1996 {published data only}
- Brisch KH, Buchheim A, Kohntop B, Kunzke D, Schmucker G, Kachele H, et al. Early preventive psychotherapeutic intervention for parents of a premature infant with very low birth weight: the Ulm study [Praventives psychotherapeutisches interventionsprogramm fur eltern nach der geburt eines sehr kleinen fruhgeborenen ‐ ulmer modell. Randomisierte langsschnittstudie]. Monatsschrift Kinderheilkunde 1996; Vol. 144, issue 11:1206‐12.
Brisch 2003 {published data only}
- Brisch KH, Bechinger D, Betzler S, Heinemann H. Early preventive attachment‐oriented psychotherapeutic intervention program with parents of a very low birthweight premature infant: results of attachment and neurological development. Attachment & Human Development 2003;5(2):120‐35. [DOI] [PubMed] [Google Scholar]
Brown 1998 {published data only}
- Brown SR. Toward the integration of efficacy research and effectiveness research in infant mental health: processes of infant‐parent intervention. Dissertation Abstracts International: Section B: The Sciences and Engineering 1998;58(7‐B):3917. [Google Scholar]
Carvalho 2009 {published data only}
- Carvalho AE, Linhares MB, Padovani FH, Martinez FE. Anxiety and depression in mothers of preterm infants and psychological intervention during hospitalization in neonatal ICU. Spanish Journal of Psychology 2009;12(1):161‐70. [DOI] [PubMed] [Google Scholar]
Cicchetti 2011b {published data only}
Clark 2003 {published data only}
- Clark R, Tluczek A, Brown R. A mother‐infant therapy group model for postpartum depression. Infant Mental Health Journal 2008; Vol. 29, issue 5:514‐36. [DOI: 10.1002/imhj.20189] [DOI] [PubMed]
- Clark R, Tluczek A, Wenzel A. Psychotherapy for postpartum depression: a preliminary report. American Journal of Orthopsychiatry 2003; Vol. 73, issue 4:441‐54. [PUBMED: 14609406] [DOI] [PubMed]
Compas 2011 {published data only}
- Compas BE, Forehand R, Thigpen JC, Keller G, Hardcastle EJ, Cole DA, et al. Family group cognitive‐behavioral preventive intervention for families of depressed parents: 18‐ and 24‐month outcomes. Journal of Consulting and Clinical Psychology 2011;79(4):488‐99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 2009 {published data only}
- Cooper PJ, Tomlinson M, Swartz L, Landman M, Molteno C, Stein A, et al. Improving quality of mother‐infant relationship and infant attachment in socioeconomically deprived community in South Africa: randomised controlled trial. BMJ 2009;338:b974. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dawe 2007 {published data only}
- Dawe S. Toddler‐parent psychotherapy increases secure attachment between toddlers and mothers who have experienced major depressive disorder. Evidence‐Based Mental Health 2007;10(4):123. [DOI] [PubMed] [Google Scholar]
Dozier 2008 {published data only}
- Dozier M, Peloso E, Lewis E, Laurenceau J‐P, Levine S. Effects of an attachment‐based intervention on the cortisol production of infants and toddlers in foster care. Development and Psychopathology 2008;20(3):845‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fisher 1980 {published data only}
- Fisher SG. The use of time limits in brief psychotherapy: a comparison of six‐session, twelve‐session, and unlimited treatment with families. Family Process 1980; Vol. 19, issue 4:377‐92. [DOI] [PubMed]
- Fisher SG. Time‐limited brief therapy with families: a one‐year follow‐up study. Family Process 1984;23(1):101‐6. [DOI] [PubMed] [Google Scholar]
Fraiberg 1981 {published data only}
- Fraiberg S, Lieberman AF, Pekarsky JH, Pawl JH. Treatment and outcome in an infant psychiatry program: II. Journal of Preventive Psychiatry 1981;1(2):143‐67. [Google Scholar]
Frisch 2013 {published data only}
Gao 2012a {published data only}
- Gao LL, Chan SW, Sun K. Effects of an interpersonal‐psychotherapy‐oriented childbirth education programme for Chinese first‐time childbearing women at 3‐month follow‐up: randomised controlled trial. International Journal of Nursing Studies 2012;49(3):274‐81. [DOI] [PubMed] [Google Scholar]
Gao 2012b {published data only}
- Gao LL, Luo SY, Chan SW. Interpersonal psychotherapy‐oriented program for Chinese pregnant women: delivery, content, and personal impact. Nursing & Health Sciences 2012;14(3):318‐24. [DOI] [PubMed] [Google Scholar]
Ghosh 2011 {published data only}
- Ghosh Ippen C, Harris WW, Horn P, Lieberman AF. Traumatic and stressful events in early childhood: can treatment help those at highest risk?. Child Abuse & Neglect 2011;35(7):504‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goodman 2013 {published data only}
- Goodman JH, Guarino AJ, Prager JE. Perinatal dyadic psychotherapy: design, implementation, and acceptability. Journal of Family Nursing 2013;19(3):295‐323. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hayes 2008 {published data only}
- Hayes L, Matthews J, Copley A, Welsh D. A randomized controlled trial of a mother‐infant or toddler parenting program: demonstrating effectiveness in practice. Journal of Pediatric Psychology 2008;33(5):473‐86. [DOI] [PubMed] [Google Scholar]
Herve 2009 {published data only}
Jardim 2007 {published data only}
- Jardim FC, Zavaschi ML, Costa F, Perrone S, Zeni CP. Psychotherapeutic group intervention for parents and infants: a case report. Revista de Psiquiatria do Rio Grande do Sul 2007;29(3):321‐3. [Google Scholar]
Kaplan 2011 {published data only}
- Kaplan BA, Venza J. Changing what you know and do: The parent‐child psychotherapy program. Zero to Three 2011;31(4):45‐51. [Google Scholar]
Lara 2010 {published data only}
Lieberman 1999 {published data only}
- Lieberman AF, Zeanah CH. Contributions of attachment theory to infant‐parent psychotherapy and other interventions with infants and young children. Handbook of Attachment: Theory, Research, and Clinical Applications. New York, NY: Guilford Press US, 1999:555‐74. [Google Scholar]
Lieberman 2005 {published data only}
- Lieberman AF, Ghosh Ippen C, Horn P. Child‐parent psychotherapy: 6‐month follow‐up of a randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry 2006;45(8):913‐8. [DOI] [PubMed] [Google Scholar]
- Lieberman AF, Horn P, Ghosh Ippen C. Toward evidence‐based treatment: child‐parent psychotherapy with preschoolers exposed to marital violence. Journal of the American Academy of Child & Adolescent Psychiatry 2005;44(12):1241‐8. [DOI] [PubMed] [Google Scholar]
Mays 2013 {published data only}
- Mays M, Lieberman AF. Mommy hates daddy. Zero to Three 2013; Vol. 33, issue 6:4‐10. [0736‐8038]
Meijer 2011 {published data only}
- Meijer JL, Bockting CL, Beijers C, Verbeek T, Stant AD, Ormel J, et al. PRegnancy Outcomes after a Maternity Intervention for Stressful EmotionS (PROMISES): study protocol for a randomised controlled trial. Trials 2011;12:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mulcahy 2010 {published data only}
- Mulcahy R, Reay RE, Wilkinson RB, Owen C. A randomised control trial for the effectiveness of group interpersonal psychotherapy for postnatal depression. Archives of Women's Mental Health 2010;13(2):125‐39. [DOI] [PubMed] [Google Scholar]
Pollock 1996 {published data only}
- Pollock KL. The effectiveness of parent‐child interaction therapy conducted in a Head Start workshop. Dissertation Abstracts International: Section B: The Sciences and Engineering 1996;57(6‐B):4039. [Google Scholar]
Punamäki 2013 {published data only}
- Punamäki R‐L, Belt R, Posa T. Emotions during the transition to parenthood among substance‐abusing mothers: intensity, content and intervention effects. Journal of Reproductive and Infant Psychology 2013; Vol. 31, issue 3:222‐44. [DOI: 10.1080/02646838.2013.803046] [DOI]
Ravn 2012 {published data only}
- Ravn IH, Smith L, Smeby NA, Kynoe NM, Sandvik L, Bunch EH, et al. Effects of early mother‐infant intervention on outcomes in mothers and moderately and late preterm infants at age 1 year: a randomized controlled trial. Infant Behavior and Development 2012; Vol. 35, issue 1:36‐47. [PUBMED: 22024475] [DOI] [PubMed]
Robert‐Tissot 1998 {published data only}
- Robert‐Tissot C, Cramer B. When patients contribute to the choice of treatment. Infant Mental Health Journal 1998;19(2):245‐59. [Google Scholar]
Sadek 2013 {published data only}
- Sadek N. Using the parent‐child relationship as a platform for psychotherapeutic interventions with very young children... Part II of a two‐part series. Brown University Child and Adolescent Behavior Letter 2013; Vol. 29, issue 3:1‐5. [1058‐1073]
Santelices 2011 {published data only}
- Santelices MP, Guzmán GM, Aracena M, Farkas C, Armijo I, Pérez‐Salas CP, et al. Promoting secure attachment: evaluation of the effectiveness of an early intervention pilot programme with mother‐infant dyads in Santiago, Chile. Child: Care, Health and Development 2011;37(2):203‐10. [DOI] [PubMed] [Google Scholar]
Santos 2006 {published data only}
- Santos RG. Effectiveness of early intervention for infants and their families: relating the working alliance to program outcomes. Dissertation Abstracts International: Section B: The Sciences and Engineering 2006;66(10‐B):5714. [Google Scholar]
Sleed 2013b {published data only}
- Sleed M, James J, Baradon T, Newbery J, Fonagy P. A psychotherapeutic baby clinic in a hostel for homeless families: practice and evaluation. Psychology and Psychotherapy: Theory, Research and Practice 2013;86(1):1‐18. [DOI] [PubMed] [Google Scholar]
Smyrnios 1993 {published data only}
- Smyrnios KX, Kirkby RJ. Long‐term comparison of brief versus unlimited psychodynamic treatments with children and their parents. Journal of Consulting & Clinical Psychology 1993;61(6):1020‐7. [DOI] [PubMed] [Google Scholar]
Spinelli 2003 {published data only}
- Spinelli MG, Endicott J. Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. American Journal of Psychiatry 2003;160(3):555‐62. [DOI] [PubMed] [Google Scholar]
Stoleru 1994 {published data only}
- Stoleru S, Morales‐Huet M. Psychotherapy with mothers and infants in problem families [Psychotherapie mit Muttern und Sauglingen in Problemfamilien]. Psyche 1994;48(12):1123‐53. [PubMed] [Google Scholar]
Svanberg 2010 {published data only}
- Svanberg PO, Mennet L, Spieker S. Promoting a secure attachment: a primary prevention practice model. Clinical Child Psychology & Psychiatry 2010;15(3):363‐78. [DOI] [PubMed] [Google Scholar]
Swartz 2006 {published data only}
- Swartz HA, Zuckoff A, Frank E, Spielvogle HN, Shear MK, Fleming MAD, et al. An open‐label trial of enhanced brief interpersonal psychotherapy in depressed mothers whose children are receiving psychiatric treatment. Depression & Anxiety 2006;23(7):398‐404. [DOI] [PubMed] [Google Scholar]
Swartz 2008 {published data only}
- Swartz HA, Frank E, Zuckoff A, Cyranowski JM, Houck PR, Cheng Y, et al. Brief interpersonal psychotherapy for depressed mothers whose children are receiving psychiatric treatment. American Journal of Psychiatry 2008;165(9):1155‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Torres 2011 {published data only}
- Torres B, Alonso‐Arbiol I, Cantero MJ, Abubakar A. Infant‐mother attachment can be improved through group intervention: a preliminary evaluation in Spain in a non‐randomized controlled trial. Spanish Journal of Psychology 2011;14(2):630‐8. [DOI] [PubMed] [Google Scholar]
Toth 2002 {published data only}
- Toth SL, Maughan A, Manly JT, Spagnola M, Cicchetti D. The relative efficacy of two interventions in altering maltreated preschool children's representational models: implications for attachment theory. Development and Psychopathology 2002;14(4):877‐908. [DOI] [PubMed] [Google Scholar]
Toth 2011 {published data only}
- Toth SL, Manly JT, Hathaway A. Relational interventions for young children who have been maltreated. In: Osofsky JD editor(s). Clinical Work with Traumatized Young Children. New York: Guilford Press, 2011:96‐113. [Google Scholar]
Toth 2012 {published data only}
- Toth SL, Gravener J. Bridging research and practice: relational interventions for maltreated children. Child and Adolescent Mental Health 2012;17(3):131‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Horn 2011 {published data only}
- Horn P, Gray L, Pettinelli B, Estassi N. Child‐parent psychotherapy with traumatized young children in kinship care: adaptation of an evidence‐based intervention. Clinical Work with Traumatized Young Children. New York, NY: Guilford Press, 2011:55‐74. [Google Scholar]
Van Zeijl 2006 {published data only}
- Zeijl J, Mesman J, Ijzendoorn MH, Bakermans‐Kranenburg MJ, Juffer F, Stolk MN, et al. Attachment‐based intervention for enhancing sensitive discipline in mothers of 1‐ to 3‐year‐old children at risk for externalizing behavior problems: a randomized controlled trial. Journal of Consulting & Clinical Psychology 2006;74(6):994‐1005. [DOI] [PubMed] [Google Scholar]
Vliegen 2013 {published data only}
- Vliegen N, Casalin S, Luyten P, Docx R, Lenaerts M, Tang E, et al. Hospitalization‐based treatment for postpartum depressed mothers and their babies: rationale, principles, and preliminary follow‐up data. Psychiatry: Interpersonal & Biological Processes 2013; Vol. 76, issue 2:150‐68. [PUBMED: 23631545] [DOI] [PubMed]
Wan 2008 {published data only}
- Wan MW, Moulton S, Abel KM. A review of mother‐child relational interventions and their usefulness for mothers with schizophrenia. Archives of Women's Mental Health 2008;11(3):171‐9. [DOI] [PubMed] [Google Scholar]
Woodhead 2006 {published data only}
- Woodhead J, Bland K, Baradon T. Focusing the lens: the use of digital video in the practice and evaluation of parental infant psychotherapy. Infant Observation 2006;9(2):139‐50. [Google Scholar]
Yang 2009 {published data only}
- Yang J, Shi S‐X, Chen Y, Yu W, Zhu Y‐Y, Tang Y‐F, et al. Effect of maternal antepartum psychological therapy upon early infant temperament. Chinese Medical Journal 2009;89(29):2038‐41. [PubMed] [Google Scholar]
Zelkowitz 2008 {published data only}
- Zelkowitz P, Feeley N, Shrier I, Stremler R, Westreich R, Dunkley D, et al. The Cues and Care Trial: a randomized controlled trial of an intervention to reduce maternal anxiety and improve developmental outcomes in very low birthweight infants. BMC Pediatrics 2008;8:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
ISRCTN38741417 {unpublished data only}
- ISRCTN38741417. Helping parents with mental health problems to parent young infants: a randomised controlled trial of parent‐infant psychotherapy and counselling. www.isrctn.com/ISRCTN38741417 (accessed 20 January 2014). [DOI: 10.1186/ISRCTN38741417] [DOI]
NCT00051246 {unpublished data only}
- NCT00051246. Group therapy for postpartum depression. https://clinicaltrials.gov/ct2/show/NCT00051246 (accessed 20 January 2014).
NCT01744041 {unpublished data only}
- NCT01744041. Mommy‐baby treatment for perinatal depression. https://clinicaltrials.gov/ct2/show/NCT01744041 (accessed 20 January 2014).
NCT01888809 {published and unpublished data}
- NCT01888809. Building Health Children (BHC). https://clinicaltrials.gov/ct2/show/NCT01888809 (accessed 20 January 2014).
- Paradis HA, Sandler M, Manly JT, Valentine L. Building healthy children: evidence‐based home visitation integrated with pediatric medical homes. Pediatrics 2013; Vol. 132, issue Suppl 2:S174‐9. [DOI: 10.1542/peds.2013-1021R] [DOI] [PubMed]
- Toth SL, Manly JT, Hathaway A. Relational interventions for young children who have been maltreated. In: Osofsky JC editor(s). Clinical Work with Traumatized Young Children Clinical Work with Traumatized Young Children. New York: Guilford Press, 2011:96‐113. [Google Scholar]
NCT02057627 {unpublished data only}
- NCT02057627. Mother‐infant intervention for postpartum depression and associated mother‐infant relationship dysfunction. https://clinicaltrials.gov/ct2/show/NCT02057627 (accessed 20 January 2014).
Additional references
Abidin 1983
- Abidin RR. The Parenting Stress Index. Charlottesville, VA: Pediatric Psychology Press, 1983. [Google Scholar]
Abidin 1986
- Abidin RR. Parenting Stress Index. 2nd Edition. Charlottesville, VA: Pediatric Psychology Press, 1986. [Google Scholar]
Abidin 1990
- Abidin RR. Parenting Stress Index (PSI). Professional Manual. 3rd Edition. Odessa, FL: Psychological Assessment Resources, 1990. [Google Scholar]
Achenbach 1992
- Achenbach T. Manual for the Child Behavior Checklist/2‐3 and 1992 Profile. Burlington, VT: Department of Psychiatry, University of Vermont, 1992. [Google Scholar]
Ainsworth 1971
- Ainsworth MDS, Bell SM, Stayton DJ. Individual differences in strange situation behavior of one‐year‐olds. In: Schaffer HR editor(s). The Origins of Human Social Relations. New York: Academic Press, 1971:17‐57. [Google Scholar]
Ainsworth 1974
- Ainsworth MDS, Bell SM, Stayton DJ. Infant‐mother attachment and social development: socialization as a product of reciprocal responsiveness to signals. In: Richards MPM editor(s). The Integration of a Child into a Social World. London: Cambridge University Press, 1974:97‐119. [Google Scholar]
Ainsworth 1978
- Ainsworth MDS, Blehar MC, Waters E, Wall S. Patterns of Attachment: A Psychological Study of the Strange Situation. Hillsdale, NJ: Lawrence Erlbaum Associates, 1978. [ISBN: 0470265345] [Google Scholar]
Anna Freud 2014
- Anna Freud Centre. New Beginnings. www.annafreud.org/pages/new‐beginnings.html (accessed 20 November 2014).
Bakermans‐Kranenburg 1998
- Bakermans‐Kranenburg MJ, Juffer F, Ijzendoorn MH. Interventions with video feedback and attachment discussions: does type of maternal insecurity make a difference?. Infant Mental Health Journal 1998; Vol. 19, issue 2:202‐19.
Bakermans‐Kranenburg 2003
- Bakermans‐Kranenburg MJ, Ijzendoorn MH, Juffer F. Less is more: meta‐analyses of sensitivity and attachment interventions in early childhood. Psychological Bulletin 2003;129(2):195‐215. [DOI] [PubMed] [Google Scholar]
Baradon 2006
- Baradon T. New Beginnings for mothers and babies in prison. Unpublished manual, The Anna Freud Centre, London, UK 2006.
Barnard 1978a
- Barnard K. Nursing Child Assessment Feeding Scale. Seattle, WA: University of Washington, 1978. [Google Scholar]
Barnard 1978b
- Barnard K. Nursing Child Assessment Teaching Scale. Seattle, WA: University of Washington, 1978. [Google Scholar]
Bavolek 1984
- Bavolek SJ. Handbook of the AAPL‐Adult Adolescent Parenting Inventory. Park City, UT: Family Development Resources Inc, 1984. [Google Scholar]
Bayley 1969
- Bayley N. Bayley Scales of Infant Development. New York: Psychological Corporation, 1969. [Google Scholar]
Bayley 1993
- Bayley S. Bayley Scales of Infant Development ‐ 2. New York: Psychological Corporation, 1993. [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4(6):561‐71. [DOI] [PubMed] [Google Scholar]
Beck 1978
- Beck AT. Beck Depression Inventory. Philadelphia, PA: Centre for Cognitive Therapy, 1978. [Google Scholar]
Beck 1988
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology 1988;56(6):893‐7. [DOI] [PubMed] [Google Scholar]
Beebe 1988
- Beebe B, Lachmann FM. The contribution of mother‐infant mutual influence to the origins of self‐ and object representations. Psychoanalytic Psychology 1988; Vol. 5, issue 4:305‐37.
Beebe 2010
- Beebe B, Jaffe J, Markese S, Buck K, Chen H, Cohen P, et al. The origins of 12‐month attachment: a microanalysis of 4‐month mother‐infant interaction. Attachment & Human Development 2010;12(1‐2):3‐141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berlin 2008
- Berlin LJ, Cassidy J, Appleyard KC, Shaver PR. The influence of early attachments on other relationships. Handbook of Attachment: Theory, Research, and Clinical Applications. 2nd Edition. New York: Guilford Press, 2008:333‐47. [Google Scholar]
Bernstein 1994
Biringen 1993
- Biringen Z, Robinson JL, Emde RN. Emotional Availability Scales. Health Science Center, University of Colorado, Denver, USA 1993.
Biringen 1998
Bradley 1977
- Bradley RH, Caldwell B. Home observation for measurement of the environment: a validation study of screening efficiency. American Journal of Mental Deficiency 1977; Vol. 81, issue 5:417‐20. [PubMed]
Briggs‐Gowan 2006
Bronfman 1999
- Bronfman E, Parsons E, Lyons‐Ruth K. Atypical Maternal Behaviour instrument for assessment and classification. Harvard Medical School 1999.
Carter 2000
- Carter A, Briggs‐Gowan M. Manual of the Infant‐Toddler Social‐Emotional Assessment. New Haven, CT: Yale University, 2000. [Google Scholar]
Chaffin 1996
Chatoor 1986
- Chatoor I. Mother/Infant/Toddler Play Scale. Children's Hospital 1986.
Cicchetti 1999b
- Cicchetti D, Toth SL, Rogosch FA. The efficacy of toddler‐parent psychotherapy to increase attachment security in offspring of depressed mothers. Attachment & Human Development 1999;1(1):34‐66. [DOI] [PubMed] [Google Scholar]
Cicchetti 2000
- Cicchetti D, Rogosch FA, Toth SL. The efficacy of toddler‐parent psychotherapy for fostering cognitive development in offspring. Journal of Abnormal Child Psychology 2000;28(2):135‐48. [DOI] [PubMed] [Google Scholar]
Cicchetti 2006a
Cicchetti 2010
- Cicchetti D, Gunnar MR, Rogosch FA, Toth SL. The differential impacts of early physical and sexual abuse and internalizing problems on daytime cortisol rhythm in school‐aged children. Child Development 2010; Vol. 81, issue 1:252‐69. [DOI] [PMC free article] [PubMed]
Cicchetti 2011a
- Cicchetti D, Rogosch FA, Toth SL, Sturge‐Apple ML. Normalizing the development of cortisol regulation in maltreated infants through preventive interventions. Development and Psychopathology 2011;23(3):789‐800. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clark 1985
- Clark R. The parent‐infant early relational assessment: instrument and manual. Madison: Department of Psychiatry, University of Wisconsin Medical School 1985.
Cohen 1977
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc, 1977. [Google Scholar]
Cohen 1983a
- Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology 1983; Vol. 13, issue 2:99‐125. [DOI: 10.1111/j.1559-1816.1983.tb02325.x] [DOI]
Cohen 1983b
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior 1983; Vol. 24, issue 4:385‐96. [PubMed]
Cohen 1999a
- Cohen N, Muir E, Lojkasek M, Muir R, Parker CJ, Barwick M, et al. Watch, Wait and Wonder: testing the effectiveness of a new approach to mother‐infant psychotherapy. Infant Mental Health Journal 1999;20(4):429‐51. [Google Scholar]
Cohen 2000
- Cohen NJ, Muir E, Lojkasek M, Muir R, Parker CJ, Barwick M, et al. Erratum: "Watch, wait, and wonder: testing the effectiveness of a new approach to mother‐infant psychotherapy". Infant Mental Health Journal 2000;21(1‐2):131. [Google Scholar]
Cohen 2002
- Cohen NJ, Lojkasek M, Muir E, Muir R, Parker CJ. Six‐month follow‐up of two mother‐infant psychotherapies: convergence of therapeutic outcomes. Infant Mental Health Journal 2002;23(4):361‐80. [Google Scholar]
Cohler 1970
- Cohler BJ, Weiss JL, Grunebaum HU. Child‐care attitudes and emotional disturbance among mothers of young children. Genetic Psychology Monographs 1970; Vol. 82, issue 1:3‐47. [PubMed]
Cooper 2003b
Cox 1987
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10‐item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry 1987;150(6):782‐6. [DOI: 10.1192/bjp.150.6.782] [DOI] [PubMed] [Google Scholar]
Cramer 1988
- Cramer B, Stern DN. Evaluation of changes in mother–infant brief psychotherapy: a single case study. Infant Mental Health Journal 1988;9(1):20‐45. [Google Scholar]
Cramer 1990
- Cramer B, Robert‐Tissot C, Stern DN, Serpa‐Rusconi S, Muralt M, Besson G, et al. Outcome evaluation in brief mother‐infant psychotherapy: a preliminary report. Infant Mental Health Journal 1990; Vol. 11, issue 3:278‐300.
Cramer 1993
- Cramer B, Palacio Espasa C. The practice of mother infant psychotherapy [La pratique des psychothérapies mères‐bébés]. Études Cliniques et Techniques. Paris: Presses Universitaires de France, 1993. [Google Scholar]
Cramer 2002
- Cramer B, Robert‐Tissot C, Rusconi Serpa S. Du Bébé au Préadolescent. Une Etude Longitudinale. Paris: Odile Jacob, 2002. [Google Scholar]
Crandell 2003
Crittenden 1981
- Crittenden PM. Abusing, neglecting, problematic, and adequate dyads: differentiating by patterns of interaction. Merrill‐Palmer Quarterly of Behavior and Development 1981; Vol. 27, issue 3:201‐18.
Crittenden 1992
- Crittenden PM. Quality of attachment in the preschool years. Development and Psychopathology 1992; Vol. 4, issue 2:209‐41.
Crittenden 2001
- Crittenden PM. CARE‐Index: Coding Manual. Miami, FL 2001.
Crnic 1990
Danis 2005
- Danis I, Oates JM, Gervai J. Studying child‐parent relationships by questionnaires [A szülő‐gyermek kapcsolat kérdőíves felmérésének lehetőségei]. Applied Psychology 2005;7(4):27‐33. [Google Scholar]
De Wolff 1997
- Wolff MS, Ijzendoorn MH. Sensitivity and attachment: a meta‐analysis on parental antecedents of infant attachment. Child Development 1997;68(4):571‐91. [PubMed] [Google Scholar]
DeGangi 2000a
- DeGangi GA. Pediatric Disorders of Regulation in Affect and Behavior: A Therapist's Guide to Assessment and Treatment. New York: Academic Press, 2000. [Google Scholar]
DeGangi 2000b
- DeGangi GA, Breinbauer C, Roosevelt JD, Porges S, Greenspan S. Prediction of childhood problems at three years in children experiencing disorders of regulation during infancy. Infant Mental Health Journal 2000;21(3):156‐75. [Google Scholar]
Derogatis 1994
- Derogatis LR. Symptom Checklist‐90‐R: Administration, Scoring and Procedures Manual. Minneapolis, MN: National Computer Systems, 1994. [Google Scholar]
Egeland 1979
- Egeland B, Deinard A, Brunnquell D, Phipps‐Yonas S, Crichton L. Final report: a prospective study of the antecedents of child abuse. In: National Center on Child Abuse and Neglect, Administration for Children, Youth and Families. Washington, DC: Office of Child Development, HEW, 1979. [Google Scholar]
Eyberg 1978
- Eyberg SM, Ross AW. Assessment of child behavior problems: the validation of a new inventory. Journal of Clinical Child Psychology 1978;7(2):113‐6. [Google Scholar]
Feldman 1998
- Feldman R. Coding Interactive Behavior Manual. Israel: Bar‐llan University, 1998. [Google Scholar]
Field 2010
- Field F. The foundation years: preventing poor children becoming poor adults. In: The Report of the Independent Review on Poverty and Life Chances. London, UK: Stationery Office, 2010. [Google Scholar]
Fonagy 2002
- Fonagy P, Gergely G, Jurist E, Target M. Affect Regulation, Mentalization and the Development of the Self. New York: Other Press, 2002. [Google Scholar]
Fraiberg 1975
Fraiberg 1980
- Fraiberg SH. Clinical Studies in Infant Mental Health: The First Year of Life. Basic Books, 1980. [Google Scholar]
Fraiberg 1987
- Fraiberg S, Adelson E, Shapiro V. Ghosts in the nursery: a psychoanalytic approach to the problems of impaired infant–mother relationships. In: Fraiberg s editor(s). Selected Writings of Selma Fraiberg. Columbus, Ohio: Ohio State University Press, 1987:100‐36. [Google Scholar]
GRADE 2013
- Schünemann H, Brozek J, Guyatt G, Oxman A (editors). GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. Available from www.guidelinedevelopment.org/handbook.
GRADEpro 2014 [Computer program]
- McMaster University. GRADEpro.. Version 3.6. McMaster University, 2014.
Granot 2001
- Granot D, Mayseless O. Attachment security and adjustment to school in middle childhood. International Journal of Behavioral Development 2001;25(6):530‐41. [Google Scholar]
Green 2002
Guyatt 2011
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction ‐ GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383‐94. [PUBMED: 21195583] [DOI] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21(11):1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Howes 1999
Jacobvitz 1997
- Jacobvitz D, Hazen NL, Riggs S. Disorganized mental processes in mothers, frightened/frightening behavior in caregivers, and disoriented, disorganized behavior in infancy. Proceedings of the Biennial Meeting of the Society for Research in Child Development; Washington (DC). 1997; Vol. 17:329‐47.
Johnston 1989
- Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. Journal of Clinical Child Psychology 1989; Vol. 18, issue 2:167‐75.
Keenan 1998
Kelly 2005
- Kelly K, Slade A, Grienenberger JF. Maternal reflective functioning, mother‐infant affective communication, and infant attachment: exploring the link between mental states and observed caregiving behavior in the intergenerational transmission of attachment. Attachment & Human Development 2005;7(3):299‐311. [DOI: 10.1080/14616730500245963] [DOI] [PubMed] [Google Scholar]
Kennedy 2007
- Kennedy E, Midgley, N. Process and outcome research in child, adolescent and parent‐infant psychotherapy. North Central London Strategic Health Authority 2007.
Keren 2001
- Keren M, Feldman R, Tyano S. Diagnoses and interactive patterns of infants referred to a community‐based infant mental health clinic. Journal of the American Academy of Child and Adolescent Psychiatry 2001;40(1):27‐35. [DOI] [PubMed] [Google Scholar]
Lecce 2008
- Lecce S. Attachment and Subjective Well‐Being: The Mediating Role of Emotional Processing and Regulation [PhD thesis]. Canada: Toronto University, 2008. [Google Scholar]
Lichtenstein 1991
- Lichtenstein J, Cassidy J. The INVentory of Adult Attachment (INVAA): validation of a new measure of adult attachment. Proceedings of the Biennial Meeting of the Society for Research in Child Development; 1991 April 18‐20; Seattle (WA). 1991.
Lyons‐Ruth 2003
- Lyons‐Ruth K, Yellin C, Melnick S, Atwood G. Childhood experiences of trauma and loss have different relations to maternal unresolved and hostile‐helpless states of mind on the AAI. Attachment & Human Development 2003;5(4):409‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lyons‐Ruth 2005
- Lyons‐Ruth K, Yellin C, Melnick S, Atwood G. Expanding the concept of unresolved mental states: hostile/helpless states of mind on the Adult Attachment Interview are associated with disrupted mother‐infant communication and infant disorganization. Development and Psychopathology 2005;17(1):1‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Madigan 2006
- Madigan S, Bakermans‐Kranenburg MJ, Ijzendoorn MH, Moran G, Pederson DR, Benoit D. Unresolved states of mind, anomalous parental behavior, and disorganized attachment: a review and meta‐analysis of a transmission gap. Attachment & Human Development 2006;8(2):89‐111. [DOI] [PubMed] [Google Scholar]
Main 1992
- Main M, Hesse E. Frightening, frightened, dissociated or disorganised behaviour on the part of the parent: a coding system for parent‐infant interaction. Unpublished manuscript. University of California at Berkeley 1992.
Marmot 2010
- Marmot M. The Marmot Review. Fair society, healthy lives: a strategic review of health inequalities in England post‐2010. www.instituteofhealthequity.org/projects/fair‐society‐healthy‐lives‐the‐marmot‐review (accessed 3 December 2014).
McCarthy 1972
- McCarthy D. Manual for the McCarthy Scales of Children's Abilities. New York: Psychological Corporation, 1972. [Google Scholar]
McDonough 1993
- McDonough S. Interaction guidance: understanding and treating early infant‐caregiver relationship disturbances. In: Zeanah C editor(s). Handbook of Infant Mental Health. 3rd Edition. New York: Guilford Press, 1993:414‐26. [Google Scholar]
McDonough 1995
- McDonough SC. Promoting positive early parent‐infant relationships through interaction guidance. Child and Adolescent Psychiatric Clinics of North America 1995;12:237‐44. [Google Scholar]
McGuire 1988
- McGuire J, Richman NN. Pre‐School PBCL Behaviour Checklist Handbook. Slough, UK: NFER‐Nelson, 1988. [ISBN: 0700511466] [Google Scholar]
Meins 2001
- Meins E, Fernyhough C, Fradley E, Tuckey M. Rethinking maternal sensitivity: mothers' comments on infants' mental processes predict security of attachment at 12 months. Journal of Child Psychology and Psychiatry. 2001/07/24 2001; Vol. 42, issue 5:637‐48. [PubMed]
Moos 1974
- Moos RH. Family Environment Scale Preliminary Manual. Palo Alto, CA: Consulting Psychologists Press, 1974. [Google Scholar]
Murray 1996
- Murray L, Fiori‐Cowley A, Hooper R, Cooper P. The impact of postnatal depression and associated adversity on early mother‐infant interactions and later infant outcome. Child Development 1996; Vol. 67, issue 5:2512‐26. [PUBMED: 9022253] [PubMed]
Murray 2003
- Murray L, Cooper PJ, Wilson A, Romaniuk H. Controlled trial of the short‐ and long‐term effect of psychological treatment of post‐partum depression: 2. Impact on the mother‐child relationship and child outcome. British Journal of Psychiatry 2003; Vol. 182:420‐7. [PUBMED: 12724245] [PubMed]
Newman 2008
Norman 2001
Norman 2004
Olds 1998
- Olds D, Henderson C, Kitzman H, Eckenrode J, Cole R, Tatelbaum R. The promise of home visitation: results of two randomized trials. Journal of Community Psychology 1998;26(1):5‐21. [Google Scholar]
Pedersen 1995
- Pedersen DR, Moran G. A categorical description of infant‐mother relationships in the home and its relation to Q‐sort measures of infant–mother interaction. Monographs of the Society for Research in Child Development. Vol. 60, Canada: Monographs of the Society for Research in Child Development, 1995:111‐32. [DOI: ] [Google Scholar]
Radloff 1977
- Radloff LS. The CES‐D scale a self‐report depression scale for research in the general population. Applied Psychological Measurement 1977; Vol. 1, issue 3:385‐401. [0146‐6216]
RevMan 2012 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
Richman 1971
- Richman N, Graham PJ. A behavioural screening questionnaire for use with three‐year‐old children. Preliminary findings. Journal of Child Psychology and Psychiatry 1971;12(1):5‐33. [1469‐7610] [DOI] [PubMed] [Google Scholar]
Robert‐Tissot 1989
- Robert‐Tissot C, Serpa‐Rusconi S, Bachmann JP, Besson G, Cmer B, Knauer D, et al. The Symptom Checklist question: evaluation of psycho‐functional problems in early infancy [Le questionnaire "Symptom Check‐List": evaluation des troubles psychofonctionnels de la petite enfance]. In: Lebovici S, Mazet P, Visier JP editor(s). L'evaluation des Interactions Precoses Entre le Bebe et ses Partenaires. Paris; Geneva: Eshel; Medecine et Hygiene, 1989:179‐215. [Google Scholar]
Robert‐Tissot 1996b
- Robert‐Tissot C, Cramer B, Stern DN, Serpa SR, Bachmann J‐P, Palacio‐Espasa F, et al. Outcome evaluation in brief mother‐infant psychotherapies: report on 75 cases. Infant Mental Health Journal 1996;17(2):97‐114. [Google Scholar]
Robins 1985
- Robins L, Helzer J, Orvaschel H, Anthony J, Blazer D, Burnam A, et al. The Diagnostic Interview Schedule. In: Eaton W, Kessler L editor(s). Epidemiologic Field Methods in Psychiatry. New York: Academic Press, 1985:143‐70. [Google Scholar]
Robins 2000
- Robins L, Cottler L, Bucholz K, Compton W, North C, Rourke K. Diagnostic Interview Schedule for the DSM‐IV (DIS‐IV). St Louis, MO: Washington University School of Medicine, 2000. [Google Scholar]
Robinson 1981
- Robinson EA, Eyberg SM. The dyadic parent‐child interaction coding system: standardization and validation. Journal of Consulting and Clinical Psychology 1981;49(2):245‐50. [DOI: 10.1037/0022-006X.49.2.245] [DOI] [PubMed] [Google Scholar]
Rutter 1970
- Rutter M, Tizard J, Whitmore K. Appendix 6: a children's behavior questionnaire for completion by parents. Education, Health, and Behavior: Psychological and Medical Study of Childhood Development. New York: Wiley, 1970:412‐21. [Google Scholar]
Salomonsson 2011b
Salomonsson 2011c
Salomonsson 2011d
- Salomonsson B, Sandell R, Werbart A, Rydelius P‐A. Psychoanalytic treatment of problems in the mother‐child relation. A randomized controlled trial shows significant therapeutic effects. Lakartidningen 2011; Vol. 108, issue 18:984‐7. [PUBMED: 21809525] [PubMed]
Schulz 2010
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [PUBMED: 20332509] [DOI] [PMC free article] [PubMed] [Google Scholar]
Singleton 2004
- Singleton JL. Parent‐infant Interaction Interventions: A Meta‐Analysis [PhD thesis]. University of Northern Colorado 2004.
Skovgaard 2008
- Skovgaard AM, Olsen EM, Christiansen E, Houmann T, Landorph S, Jørgensen T. Predictors (0‐10 months) of psychopathology at age 1½ years ‐ a general population study in The Copenhagen Child Cohort CCC 2000*. Journal of Child Psychology and Psychiatry 2008; Vol. 49, issue 5:553‐62. [PUBMED: 18341552] [DOI] [PubMed]
Skovgaard 2010
- Skovgaard AM. Mental health problems and psychopathology in infancy and early childhood. An epidemiological study. Danish Medical Bulletin 2010; Vol. 57, issue 10:B4193. [PubMed]
Slade 2001
- Slade A, Grienenberger J, Bernbach E, Levy D, Locker A. Maternal reflective functioning and attachment: considering the transmission gap. Proceedings of the Biennial Meeting of the Society for Research on Child Development; 2001 April; Minneapolis, MN. 2001.
Slade 2004
- Slade AAJ, Berger B, Bresgi I, Kaplan M. The Parent Development Interview ‐ Revised. The City University of New York 2004.
Slade 2005
- Slade A, Grienberger J, Bernbach E, Levy D, Locker A. Maternal reflective functioning, attachment and the transmission gap: a preliminary study. Attachment & Human Development 2005;7(3):283‐98. [DOI] [PubMed] [Google Scholar]
Spanier 1989
- Spanier G. Manual for the Dyadic Adjustment Scale. Multi‐Health Systems: New York, 1989. [Google Scholar]
Squires 2002
- Squires J, Bricker D, Twombly E, Yockelson S, Davis MS, Younghee K, et al. Ages & Stages Questionnaires: Social‐Emotional: A Parent‐Completed, Child‐Monitoring System for Social‐Emotional Behaviors. Baltimore, MD: Brookes, 2002. [Google Scholar]
Sroufe 1997
- Sroufe LA. Emotional Development: The Organization of Emotional Life in the Early Years. Cambridge: Cambridge University Press, 1997. [Google Scholar]
Sroufe 2005a
- Sroufe LA, Egeland B, Carlson E, Collins WA. Placing early attachment experiences in developmental context: the Minnesota longitudinal study. Attachment from Infancy to Adulthood: The Major Longitudinal Studies. New York, NY: Guilford Publications, 2005:48‐70. [Google Scholar]
Sroufe 2005b
- Sroufe LA. Attachment and development: a prospective, longitudinal study from birth to adulthood. Attachment & Human Development 2005;7(4):349‐67. [DOI] [PubMed] [Google Scholar]
Stern 1989a
- Stern D, Robert‐Tissot C, Muralt M, Cramer B, Lebovici S, Mazet P, et al. KIA‐Profile: a tool for clinical research for evaluation of affective states of early childhood [Le KIA‐Profil: un instrument de recherche clinique pour l'evaluation des états affectifs du jeune enfant]. L'évaluation des Interactions Précoces Entre le Bébé et ses Partenaires 1989:131‐49.
Stern 1989b
- Stern D, Robert‐Tissot C, Muralt M, Cramer B, Lebovici S, Mazet P, et al. The R‐interview: a method for evaluation of maternal representations [L'entretien "R" une methode d'evaluation des representations maternelles]. In: Lebovici S, Mazet P, Visier JP editor(s). L'évaluation des Interactions Précoces Entre le Bébé et Ses Partenaires. Paris, Geneva: Eshel (Paris), Medecine et Hyiene (Geneva), 1989:151‐77. [Google Scholar]
Stronach 2013
- Stronach EP, Toth S, Rogosch F, Cicchetti D. Preventive interventions and sustained attachment security in maltreated children. Development and Psychopathology 2013;5(4 pt 1):919‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Suchman 2005
- Suchman NE, McMahon TJ, Slade A, Luthar SS. How early bonding, depression, illicit drug use, and perceived support work together to influence drug‐dependent mothers' caregiving. American Journal of Orthopsychiatry. 2005/08/03 2005; Vol. 75, issue 3:431‐45. [DOI] [PMC free article] [PubMed]
Timmer 2011
- Timmer SG, Ho LK, Urquiza AJ, Zebell NM, Fernandez YGE, Boys D. The effectiveness of parent‐child interaction therapy with depressive mothers: the changing relationship as the agent of individual change. Child Psychiatry and Human Development. 2011/04/12 2011; Vol. 42, issue 4:406‐23. [DOI] [PubMed]
Toth 2006
- Toth SL, Rogosch FA, Manly JT, Cicchetti D. The efficacy of toddler‐parent psychotherapy to reorganize attachment in the young offspring of mothers with major depressive disorder: a randomized preventive trial. Journal of Consulting and Clinical Psychology. 2006/12/13 2006; Vol. 74, issue 6:1006‐16. [DOI] [PubMed]
Tronick 1989
Tronick 1997
- Tronick EZ, Weinberg MK. Depressed mothers and infants: failure to form dyadic states of consciousness. In: Murray LCP editor(s). Post‐Partum Depression and Child Development. New York: Guilford, 1997:54‐85. [157230197X] [Google Scholar]
Tronick 2005
- Tronick EZ, Messinger DS, Weinberg MK, Lester BM, Lagasse L, Seifer R, et al. Cocaine exposure is associated with subtle compromises of infants' and mothers' social‐emotional behavior and dyadic features of their interaction in the face‐to‐face still‐face paradigm. Developmental Psychology 2005; Vol. 41, issue 5:711‐22. [DOI] [PubMed]
Vaux 1987
- Vaux A, Riedel S, Stewart D. Modes of social support: the social support behaviors (SS‐B) scale. American Journal of Community Psychology 1987; Vol. 15, issue 2:209‐32. [DOI: 10.1007/BF00919279] [DOI]
Waters 1985
- Waters E, Deane KE. Defining and assessing individual differences in attachment relationships: Q‐methodology and the organization of behavior in infancy and early childhood. Monographs of the Society for Research in Child Development 1985; Vol. 50, issue 1‐2:41‐65.
Waters 1995
- Waters E. Appendix A: the Attachment Q‐Set (version 3.0). Monographs of the Society for Research in Child Development 1995; Vol. 60, issue 2‐3:234‐46. [DOI: 10.1111/j.1540-5834.1995.tb00214.x] [DOI]
Wechsler 1989
- Wechsler D. WPPSI‐R, Manual: Wechsler Preschool and Primary Scale of Intelligence, Revised. Psychological Corporation New York, NY 1989.
Zero to Three 2005
- Zero to Three. Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood (DC 0‐3:R). Washington: DC: Zero to Three Press, 2005. [Google Scholar]
Östberg 1997
References to other published versions of this review
Barlow 2013
- Barlow J, Bennett C, Midgley N. Parent‐infant psychotherapy for improving parental and infant mental health. Cochrane Database of Systematic Reviews 2013, Issue 5. [DOI: 10.1002/14651858.CD010534] [DOI] [PMC free article] [PubMed] [Google Scholar]


