Abstract
Background
Acute exacerbations (AEs) and disease progression in interstitial lung disease (ILD) pose important challenges to clinicians and patients. AEs of ILD are variable in presentation but may result in rapid progression of ILD, respiratory failure and death. However, in many cases AEs of ILD may go unrecognised so that their true impact and response to therapy is unknown. The potential for home monitoring to facilitate early, and accurate, identification of AE and/or ILD progression has gained interest. With increasing evidence available, there is a need for a systematic review on home monitoring of patients with ILD to summarise the existing data. The aim of this review was to systematically evaluate the evidence for use of home monitoring for early detection of exacerbations and/or progression of ILD.
Method
We searched Ovid-EMBASE, MEDLINE and CINAHL using Medical Subject Headings (MeSH) terms in accordance with the PRISMA guidelines (PROSPERO registration number CRD42020215166).
Results
13 studies involving 968 patients have demonstrated that home monitoring is feasible and of potential benefit in patients with ILD. Nine studies reported that mean adherence to home monitoring was >75%, and where spirometry was performed there was a significant correlation (r=0.72–0.98, p<0.001) between home and hospital-based readings. Two studies suggested that home monitoring of forced vital capacity might facilitate detection of progression in idiopathic pulmonary fibrosis.
Conclusion
Despite the fact that individual studies in this systematic review provide supportive evidence suggesting the feasibility and utility of home monitoring in ILD, further studies are necessary to quantify the potential of home monitoring to detect disease progression and/or AEs.
Short abstract
First systematic review that provides supportive evidence for the feasibility and utility of home monitoring in ILD; further studies are necessary to evaluate approaches to detect exacerbation and/or progression https://bit.ly/2Y8OCJL
Introduction
Interstitial lung disease (ILD) is a general term for approximately 200 different diseases that may result in inflammation and scarring of the lung [1]. ILD is characterised by progressive dyspnoea, inflammation, fibrosis and reduced quality of life [1]. Most cases of ILD result from an aetiological factor, such as exposure to allergens, toxins or drugs or from an underlying autoimmune disease, with a modifying influence of genetics and exogenous factors such as air pollution [2–4]. In many cases the aetiology is unclear [5]. The most severe form of ILD is idiopathic pulmonary fibrosis (IPF) [1, 6], for which there is no cure [2]. The median survival time after diagnosis of untreated IPF is 2–5 years [2, 7, 8]. The considerable variability seen between patients makes individual outcome prediction difficult. In addition, there is a lack of validated biomarkers of disease progression [6, 9]. Forced vital capacity (FVC) is one possible biomarker of disease progression and is usually measured intermittently. There are currently two anti-fibrotic drugs approved for use in IPF, nintedanib and pirfenidone, which have been demonstrated to slow the rate of FVC decline [10–13] and may increase median survival [10, 12, 14]. There is an urgent unmet need for better treatments. Currently all clinical trials of novel therapies for IPF have used the established end-point of rate of decline in FVC and have required large patient cohorts followed for a significant length of time (years) to identify meaningful treatment responses [15, 16]. More frequent measures, such as the use of home spirometry, may reduce the size, length of time and cost of clinical trials [17–20]. Ineffective drug treatments could also be identified at an earlier stage. More regular monitoring of physiological parameters in ILD might be of benefit in clinical practice and in research.
Patients with ILD may experience acute deteriorations (“exacerbations” or “acute exacerbations” (AEs)) of their condition, and there is a growing body of research into the detection of exacerbation in ILD [21, 22]. AEs of ILD (AE-ILD) are highly variable but may result in rapid respiratory deterioration, alveolar abnormalities, and in severe cases death [21–23]. This rapid progression can cause severe distress to patients and burden healthcare systems. The potential for home monitoring to identify progression, including AE, at an early stage is of significant interest. Supporting evidence exists in other respiratory diseases. It has been demonstrated that early detection of exacerbations in COPD speeds recovery time [24, 25]. Home monitoring has thus been recommended in lung diseases such as COPD to support earlier detection of exacerbation [26, 27]. It is suggested that similar technology may benefit patients with ILD [20, 28–32].
Another challenge in ILD is the marked inter-patient heterogeneity which makes it very difficult to accurately predict life expectancy and so to provide a reliable prognosis to individual patients and their families [22]. A benefit of home monitoring may be that more frequent monitoring of individual patients may allow prediction of a patient's personal trajectory that can inform prognostication and decisions of future care [31, 32].
The potential role for home monitoring in ILD has been amplified by the coronavirus disease 2019 (COVID-19) pandemic. The guidance from the British Lung Foundation and UK National Health Service for patients with ILD has been to “shield”, to reduce the risk of contracting COVID-19 [33]. Home monitoring could arguably decrease the inherent risk in physical attendance at outpatient clinics [26, 30]. This may also prove useful beyond the COVID-19 pandemic, given that ILD can limit patient mobility and care is often centralised at tertiary centres [34, 35].
There is no existing systematic synthesis of the literature to examine the role of home monitoring to detect ILD exacerbation and/or disease progression. Thus, we aimed to systematically gather, summarise and evaluate the evidence not just for feasibility and reliability, but also on detection of AE-ILD and/or disease progression in this systematic review.
Search methods
Protocol and registration
We undertook a systematic review of the literature using a protocol in accordance with the preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P 2015) [36, 37]. We prospectively registered this systematic review at PROSPERO (protocol registration number CRD42020215166).
Eligibility criteria
We utilised the PICO framework (participants/population, intervention(s)/exposure(s), comparator(s)/ control, main outcome(s)) as a search strategy. We systematically searched for studies on home monitoring and interstitial lung disease published worldwide with no restriction on date of publication. Home monitoring was defined as the regular use of any home-based technology and spirometry to monitor symptoms and/or physiological parameters (such as vital signs and spirometry) over a period of at least 3 weeks. The selected papers met the following inclusion criteria: 1) patients with confirmed diagnoses of ILD determined by the authors’ local criteria; 2) written in English; 3) focus on home monitoring to detect exacerbations and/or progression in patients with ILD; 4) detected ILD exacerbations and progression; and 5) randomised controlled trials (RCTs), prospective or retrospective cohort observational studies or case–control studies. Studies were excluded if the following criteria were met: 1) studies that were conference abstracts, theses and book chapters; or 2) systematic reviews and meta-analyses (we screened the bibliography), literature reviews or qualitative studies.
Search strategy
Between October and November 2020, we searched electronic databases for published articles at any date prior to this, and then updated the search in February 2021 to identify further relevant publications on ILD and home monitoring. We developed a search strategy with medical library staff and extensively searched the following databases: Ovid-EMBASE, Ovid-MEDLINE, Cumulative Index to Nursing and Allied Health Literature (supplementary tables S1 to S5). We also searched the references of studies thoroughly for any eligible articles. We searched the above electronic databases for Medical Subject Headings (MeSH) terms, and the main terms classified into three groups that describe ILD, home monitoring and progression. Further detailed related terms to this systematic review are included in supplementary tables S1 to S5.
Data collection
All studies found to be potentially eligible were retrieved from the electronic databases and stored for de-duplicating in the reference management software package EndNote. We exported the results, after removing duplicates, to the online software Rayyan, where the title and abstract of potential studies were screened by two independent reviewers (M.A. Althobiani and R.A. Evans). The software allows the two reviewers to include and exclude studies blindly, and when completed, disagreements were resolved by reading the full text and discussion. We exported the included studies to a new EndNote library, where the articles were read in full.
Quality assessment
Two authors (M.A. Althobiani and J.S. Alqahtani) conducted detailed quality assessment using the Cochrane risk of bias tool for the assessment of the included RCT studies, and the Newcastle–Ottawa tool was used in regard to the observational studies. The Cochrane risk of bias tool comprises seven domains. The Newcastle–Ottawa tool consists of three broad perspectives used to assess the quality of non-randomised studies included in this systematic review. The quality of the cohort studies is based upon a “star” system with a total possible score of nine stars. Study ratings are indicated with the following: 7–9 stars=good, 4–6 stars=fair, 1–3 stars=poor (tables 1 and 2).
TABLE 1.
Use of Cochrane risk of bias tool to assess quality of randomised controlled trials
TABLE 2.
Use of Newcastle–Ottawa tool to assess the quality of cohort studies
| Study | Representativeness of exposed cohort | Selection of non-exposed cohort | Ascertainment of all-cause | Outcome not present at the start of study | Comparability of cohort | Assessment of outcome | Adequate follow-up duration | Adequate follow-up rate | Score | Quality |
| Russell et al. (2016) [31] | 1 | 0 | 1 | 1 | 2 | 0 | 1 | 1 | 7 | Good |
| Johannson et al. (2017) [20] | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | Good |
| Veit et al. (2020) [32] | 1 | 0 | 1 | 1 | 2 | 1 | 1 | 1 | 8 | Good |
| Edwards et al. (2020) [39] | 0 | 0 | 1 | 1 | 2 | 1 | 1 | 1 | 7 | Good |
| Moor et al. (2019) [45] | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 6 | Fair |
| Moor et al. (2018) [40] | 1 | 0 | 1 | 1 | 2 | 1 | 1 | 1 | 8 | Good |
| Moor et al. (2020) [46] | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 6 | Fair |
| Broos et al. (2017) [41] | 1 | 0 | 1 | 1 | 2 | 1 | 1 | 1 | 8 | Good |
| Marcoux et al. (2019) [28] | 1 | 0 | 1 | 1 | 2 | 1 | 1 | 1 | 8 | Good |
| Noth et al. (2021) [43] | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | Good |
| Moor et al. (2020) [42] | 1 | 0 | 1 | 1 | 2 | 1 | 1 | 1 | 8 | Good |
Synthesis of results
Narrative synthesis was undertaken according to outcomes that were reported in the included studies with more emphasis given to studies of higher quality. We considered how differences in design, outcomes, intervention, population and setting may have contributed to any differences in observed results.
Results
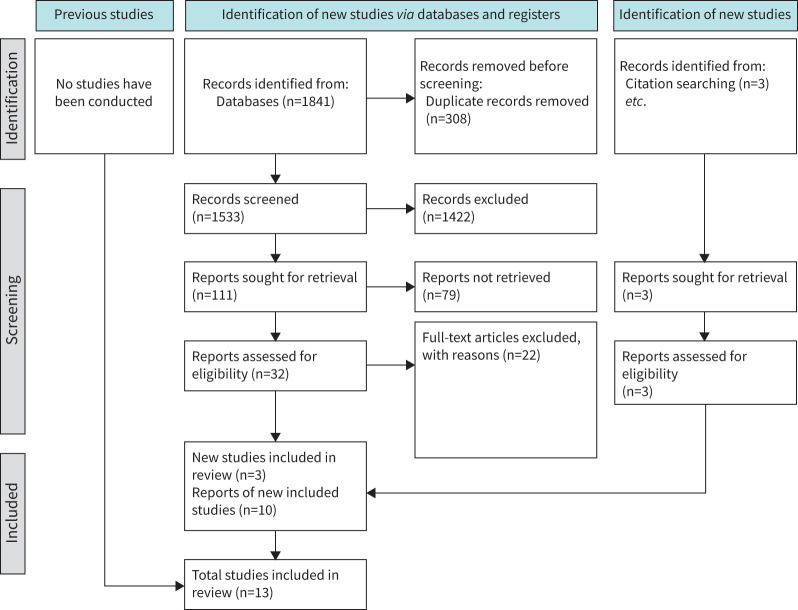
The original search across five databases identified 1841 publications; 1533 articles remained after duplicates were manually reviewed and removed. A total of 1422 articles were excluded using title-only screening, followed by 79 exclusions after title and abstract screening. A total of 32 articles remained for full-text screening, 22 of which were excluded. Three articles were included as relevant from searching the references. Thus, 13 studies were considered for inclusion in this systematic review as depicted in the PRISMA flow diagram (figure 1).
FIGURE 1.
PRISMA flow diagram.
Description of the included studies
11 prospective cohort studies and two RCTs were identified and included by the systematic search. The RCTs were conducted in the Netherlands and in multiple centres internationally. Seven cohort studies were conducted in the Netherlands, one in the UK, one in the USA, one in Germany, and one across the USA and Ireland.
General description
Characteristics of the included studies are summarised in table 3. The studies were published between 2016 and 2021 and involved a total of 968 recruited patients with ILD. The sample size for these studies ranged from 10 to 346 patients, with ages ranging from 31 to 73 years. The majority of the patients were male. The RCT duration was 24 weeks, and the prospective cohort studies ranged from 2 to 70 weeks.
TABLE 3.
Characteristics of included studies on home monitoring in interstitial lung disease (ILD) patients
| Study | Setting/design | Sample size and characteristics | Disease group | Clinic measures/frequency | Home measures/frequency | Study length | Outcome | Quality | Results |
| Moor et al. (2020) [30] | NL/RCT | n=90 Age (mean±sd): 71±6.9 years Intervention (n=46) Male: 39 (85%) Age (mean): 70 years Control (n=44) Male: 43 (98%) Age (mean): 72 years |
IPF | Spirometry, K-BILD, PESaM, EQ-5D-5L, HADS, VAS, GRC, EQ-VAS (baseline, and at 12 and 24 weeks) | FVC (Once daily) K-BILD, PESaM, EQ-5D-5L, HADS, VAS, GRC, EQ-VAS (weekly) |
24 weeks | Investigate whether a home monitoring programme improves HRQOL and medication use for patients with IPF | Moderate | (1) Improved psychological well-being compared to standard care alone (mean difference 1.04 points; 95% CI 0.09–2.00; p=0.032) (2) Mean change in FVC was not significantly different between hospital-based group (−87.9 mL; range −209 to 33.2 mL) and home monitoring group (−7.9 mL; range −96 to 69.4 mL; p=0.25) (3) Correlation between home and hospital spirometry was high at all time-points (r=0.97, p<0.001 at baseline and 12 weeks; r=0.96, p<0.001 at 24 weeks) (4) Correlation between slopes was moderately strong (r=0.58; p<0.001) |
| Maher et al. (2020) [38] | RCT | n=253 Intervention (n=127) Age (mean): 70 years (range 61.0–76.0) Male: 70 (55%) Placebo (n=126) Age (mean): 69 years (range 63.0–74.0) Male: 69 (55%) |
Unclassifiable ILD | Spirometry 6MWD, UCSD-SOBQ, Leicester Cough Questionnaire, SGRQ (baseline and at 24 weeks) |
FVC (once daily) | 24 weeks | The mean change in FVC measured by daily home-based spirometry, change in FVC measured by site spirometry, change in 6MWD, change in UCSD-SOBQ | Good | (1) The primary end-point was not adequately analysed due to technical issues resulting in variability in home-based spirometry measurements (2) Mean FVC decline measured by clinic spirometry was less in pirfenidone than placebo group (treatment difference 95.3 mL; 95% CI 35.9–154.6, p=0.002) |
| Russell et al. (2016) [31] | UK/PCS | n=50 Male: 45 (90%) Age (mean±sd): 66.7±7.9 years |
IPF | Spirometry baseline, and at 3, 6 and 12 months | FEV1, FVC (once daily) | Median: 279 days, range 13–490 days | Feasibility and reliability of measuring daily FVC | Good | (1) Daily FVC measurement was most predictive for disease progression and mortality when measured at 3 months (hazard ratio 1.04; 95% CI 1.02–1.06; p≤0.001), 6 months (HR 1.02; 95% CI 1.01–1.03; p<0.001), and 12 months (HR 1.012; 95% CI 1.007–1.01; p=0.001); 28 days did not yield a positive correlation (2) Regular home measurement of FVC is feasible and reliable (3) Home spirometry showed high correlation with hospital-based spirometry |
| Johannson et al. (2017) [20] | USA/PCS | n=25 Male: 21 (84%) Age (mean±sd): 73.6±7.5 years |
IPF | Spirometry baseline and at 24 weeks | FEV1, FVC (three times per week) UCSD-SOBQ (weekly), dyspnoea-VAS (weekly) | 24 weeks | Feasibility and reliability of measuring FVC and dyspnoea | Good | (1) Weekly home measurement of FVC and dyspnoea in patients with IPF is reliable and feasible over 24 weeks (2) Mean adherence to weekly home spirometry >90% |
| Veit et al. (2020) [32] | DE/PCS | n=47 Male: 28 (59.6%) Age (mean±sd): 62.7 ±11.5 years |
ILD | Spirometry, 6MWD, DLCO, FVC, K-BILD, SGRQ, VAS Cough (baseline, at 3 and 6 months) | FVC (three times per day) | 6 months | Determine feasibility in different types of fibrotic non-IPF ILD and investigate the clinical impact of daily home spirometry in patients with progressive ILD with respect to disease progression | Good | (1) Adherence was higher within the first 3 months compared to the second 3 months (83.5±19.6% versus 78.4±22.3% of the days; p=0.0086) (2) Correlation between hospital FVC values and the mean of the home FVC measurements was similarly strong at 3-month (r=0.95; p<0.0001) and 6-month visits (r=0.93; p<0.0001) |
| Edwards et al. (2020) [39] | IE/USA/PCS | n=36 USA: Age (mean): 62 years Ireland: Age (mean): 66 years |
PF | FVC (once daily) mMRC (once daily) IPF-PROM (weekly) |
1 year | Acceptability and utility of patientMpower | Fair | (1) 93% of respondents reported a positive impact on their well-being (2) Good correlation between hospital-based and home-based spirometry |
|
| Moor et al. (2019) [45] | NL/PCS | n=10 Male: 6 (60%) Age (mean): 53 years |
Sarcoidosis | Spirometry, activity, PROM (baseline and at 1 month), patients’ KSQ, EQ-5D-5L, HADS, FAS Satisfaction (interview) |
PEF, FEV1, FVC (daily) VAS fatigue, dyspnoea, cough, well-being (weekly) |
4 weeks | Evaluate feasibility of home monitoring programme and patient satisfaction programme | Fair | (1) Home spirometry measurements highly correlated with in-hospital measurements of FVC (r=0.97, p<0.001) and FEV1 (r=0.96, p<0.001) (2) Mean adherence to daily spirometry was 94.6%; it was measured by dividing the total number of measurements by the total numbers of days |
| Moor et al. (2018) [40] | NL/PCS | n=10 Male: 9 (90%) Age (mean): 71 years |
IPF | Spirometry, patient-reported outcome (baseline and at 1 month), patients’ K-BILD, HADS, EuroQoL 5D-5 L | Home spirometry (daily) Patient-reported outcome (weekly) |
4 weeks | Feasibility of a pre-developed home monitoring programme in IPF (home spirometry) | Fair | (1) Home-based spirometry showed similar results to hospital-based spirometry; measurements of home and hospital FVC were correlated (r=0.94; p<0.001) and FEV1 (r=0.97; p<0.001) were highly correlated (2) Feasibility and potential barriers of home spirometry: 80% of patients reported easy to use and 90% said it was not burdensome; mean adherence was 98.8% to home monitoring programme |
| Moor et al. (2020) [46] | NL/PCS | n=50 (n=44 acceptable data) Age range: 43–79 years Male: 68% |
IPF | Questionnaire (baseline and at 6 weeks) | FVC (twice daily) Patient-reported K-BILD online |
6 weeks | Measure diurnal variation in FVC in patients with f-ILD using home spirometry, evaluate the relationship between FVC and activity, home-based FVC, home and hospital-based correlation | Fair | (1) Morning FVC was significantly higher than afternoon FVC (mean difference 36 mL, p<0.001); the mean difference between morning and afternoon FVC was similar for patients with IPF compared with all f-ILDs (2) Daily step correlated with FVC (r=0.32, p=0.028, K-BILD total score (r=0.5, p<0.001)) (3) Home and hospital-based spirometry were correlated (r=0.98, p<0.0001) |
| Broos et al. (2017) [41] | NL/PCS | n=21 Male: 13 Female: 8 Age (mean±sd): 43±11 years 76% diagnosed with Scadding stage II sarcoidosis |
Sarcoidosis | Clinic spirometry, SGRQ, SF-36, KSQ, MRC, FAS at baseline, 1 and 3 months | FVC (daily) MRC, FAS (weekly) |
3 months | Detect early steroid treatment effects in newly treated pulmonary sarcoidosis |
Good | (1) Home spirometry in sarcoidosis is reliable (2) Home and hospital spirometry were correlated (r=0.98; p<0.001) |
| Marcoux et al. (2019) [28] | NL/PCS | n=20 Male: 16 (80%) Age (mean±sd): 73±6.9 years |
IPF | Clinic spirometry at baseline, 4 and 23 weeks 6MWD (baseline and at 12 weeks) |
FVC (3 manoeuvres daily) | 12 weeks | Test the 12-week feasibility of blinded daily handheld spirometry and physical activity monitoring in patients with IPF | Good | (1) The correlation for office-based and handheld FVC measurements was 0.99 (95% CI 0.97–0.99) and 0.95 (95% CI 0.91–0.98), respectively (2) Mean adherence to home spirometry was 84% |
| Noth et al. (2021) [43] | NL/PCS | n=346 diagnosed with IPF in the previous 3 years and had an FVC ≥80% predicted; 116 randomised to nintedanib, 230 randomised to placebo for 12 weeks, followed by an open-label period in which all subjects received nintedanib 150 mg twice daily for 40 weeks |
IPF | Clinic spirometry at baseline and weeks 4, 8, 12, 16, 20, 24, 36 and 52 | FVC (weekly) | 1 year | Investigate the feasibility and validity of home spirometry as a measure of lung function decline in patients with IPF | Good | (1) Over 52 weeks, mean adherence was 86% (2) Strong correlations were observed between home- and clinic-measured FVC at all time-points (r=0.72 to 0.84), but correlations between home- and clinic-measured rates of change in FVC were weak (r=0.26 for rate of decline in FVC over 52 weeks); the correlations were weaker in subjects who provided more FVC readings per week, due to variability in change in FVC measured at home (greater number of outliers) and errors in measurements |
| Moor et al. (2020) [42] | NE/PCS | n=10 Female: 60% Age (mean±sd): 60.3±9.9 years |
Systemic sclerosis-associated ILD | Spirometry at baseline and 3 months K-BILD, HADS, EQ-5D-5L (baseline and at 6 weeks) |
FVC (once daily) | 3 months | Investigate the feasibility of an online home monitoring application, and spirometry | Good | (1) Mean±sd adherence was 98.8±1.5% (2) Strong adherence and acceptability; 90% found home monitoring pleasant and wanted to continue to use home monitoring application daily |
IPF: idiopathic pulmonary fibrosis; CAT: COPD Assessment Test; EQ-5D-5L: EuroQoL Five-Dimensions Questionnaire; FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity; GRC: Global Rating Change; HRQOL: health-related quality of life; ILD: interstitial lung disease; 6MWD: 6-min walk distance; HADS: Hospital Anxiety and Depression Scale; IE: Ireland; K-BILD: The King's Brief Interstitial Lung Disease; NL: Netherlands; PESaM: Patient Experiences and Satisfaction with Medication questionnaire; PCS: prospective cohort study; RCT: randomised controlled trial; SGRQ: St George's Respiratory Questionnaire; UK: United Kingdom; US: United States; VAS: visual analogue scale; mMRC: Modified Medical Research Council; EQ-VAS: EuroQol-visual analogue scales; IPF-PROM: Idiopathic Pulmonary Fibrosis (IPF) Patient Reported Outcome Measure; KSQ: King's Sarcoidosis Questionnaire; PEF: peak expiratory flow; f-ILD: fibrosing interstitial lung disease; SF36: 36-Item Short Form; UCSD-SOBQ: The University of California, San Diego, Shortness of Breath Questionnaire.
A variety of types of home monitoring techniques, including but not limited to spirometry, weekly symptom reporting through electronic means, wearable devices to track/monitor vitals and activity, were used. Table 4 summarises the techniques and tools used in the included studies.
TABLE 4.
The components and outcomes measured in the home monitoring intervention in this systematic review
| Study | Measurement parameters | Data transmission | Online platform/app | ||||||
| Spirometer | Quality check | Oximetry | Step count/6MWD | Symptom report | Downloaded by staff | Real-time | Diary card | ||
| Moor et al. (2020) [30] | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Russell et al. (2016) [31] | ✓ | ✓ | |||||||
| Johannson et al. (2017) [20] | ✓ | ✓ | ✓ | ✓ | |||||
| Moor et al. (2019) [45] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Veit et al. (2020) [32] | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Moor et al. (2018) [40] | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Edwards et al. (2020) [39] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Noth et al. (2020) [43] | ✓ | ✓ | |||||||
| Moor et al. (2020) [42] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Broos et al. (2017) [41] | ✓ | ✓ | ✓ | ||||||
| Marcoux et al. (2019) [28] | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Moor et al. (2020) [46] | ✓ | ✓ | ✓ | ✓ | |||||
| Maher et al. (2020) [38] | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
Feasibility
Feasibility
A recent study by Maher et al. [38] raised some concerns related to the data integrity of home-based spirometry in patients with pulmonary fibrosis due to high variability and technical problems. However, 13 studies support the feasibility and utility of home-based spirometry in patients with ILD [20, 28, 30–32, 38–43, 45, 46]. Moor et al. [30] reported that the slopes of home- and clinic-based FVC over time were comparable. The rate of discontinuation was not dissimilar to the rates seen in other clinical trials. Most participants were able to provide daily readings, with at least four every 5 days, for up to 1 year [30, 31, 39, 42]. In contrast, Veit et al. [32] and Marcoux et al. [28] required patients to perform three spirometry manoeuvres every day and found it feasible. In summary, regular home measurement of FVC in the context of a clinical study was found to be feasible. Johannson et al. [20] and Noth et al. [43] showed feasibility and reliability of weekly spirometry in patients with ILD. Two studies in sarcoidosis [41, 45] and one in IPF [29] included 121 patients who performed daily home spirometry, and completed patient-reported outcomes at baseline, weekly and at the end of the studies. The articles concluded that a home monitoring programme for IPF and sarcoidosis was indeed feasible, and was well tolerated by most of the patients [29, 30, 41].
In general, all the included studies presented a positive experience in relation to acceptance of home monitoring programmes by patients. Edwards et al. [39] demonstrated acceptability of home monitoring to patients at 6 weeks, and the majority of patients wished to continue with home monitoring beyond this time-point. Patients showed a positive attitude towards home monitoring techniques despite differences in age and the size of studies. Ease of use and friendliness of technology contributed to good compliance among patients and their acceptance of the home monitoring systems [34].
Adherence
Adherence was calculated by the number of home measurements divided by the number of weeks enrolled in the study for weekly measurements, and number of home measurements divided by the number of days enrolled in the study for daily measurements [20, 32]. In the study by Johannson et al. [20] mean adherence to three times weekly home FVC monitoring over 24 weeks was 90.5% (sd=18.3%). The Veit et al. [32] study reported that adherence to three times daily home spirometry decreased over time. Median adherence dropped within the first 28 days and decreased from 90% to 81% over 6 months. Acceptance, however, was high; only four patients discontinued within the first week as dyspnoea made it too difficult to perform daily measurements. Noth et al. [43] demonstrated that adherence to weekly home spirometry decreased with time but remained over 75% throughout the entirety of the study. Studies by Moor et al. [29, 30, 40, 42, 45] demonstrated that mean adherence to once daily home FVC ranged from 90.5% to 98.8%. In summary, adherence to a home monitoring programme varied depending on study duration, frequency of measurement and transmission. However, nine studies [20, 28, 30, 32, 39, 40, 42, 43, 45] reported that mean adherence to home spirometry was >75%. Veit et al. [32] reported that the decrease in adherence with time might be due to lack of reminders to perform spirometry. Moor et al. [30] found good adherence that did not decrease with time and suggested that in other studies such challenges with home spirometry might have arisen because patients were blinded from their results and had no technical helpdesk.
Utility
Prediction of disease progression and mortality
Only Russell et al. [31] and Veit et al. [32] reported information describing whether home-based monitoring was able to detect disease progression. Russell et al. [31] reported 18 deaths out of 50 subjects during the 490-day study of patient-recorded daily spirometry. The study compared the rate of change in FVC between baseline to 28 days, 3 months, 6 months and 12 months. It demonstrated that the rate of change in FVC was more predictive for disease progression and mortality when measured at 3 months (hazard ratio (HR) 1.04; 95% CI 1.02–1.06; p≤0.001), 6 months (HR 1.02; 95% CI 1.01–1.03; p<0.001) and 12 months (HR 1.012; 95% CI 1.007–1.01; p=0.001); 28 days did not yield a significant correlation [31].
Veit et al. [32] included 47 patients and provided reliable daily measurements of spirometry for the cohort study. The study defined disease progression as death due to respiratory failure, lung transplantation, AE or hospital-based relative FVC decline >10% at 3 or 6 months [32]. During the 6 months, 12 of these 40 participants experienced disease progression [32]. A group of patients displayed high daily variability in FVC during the initial 28 days of the study; 60.0% showed a variation ≥5%. FVC variability over 28 days was independently associated with disease progression (HR 1.20; 95% CI 1.05–1.3; p=0.007). FVC variability over 3 months was also a significant predictor for disease progression (HR 1.2; 95% CI 1.01–1.64; p=0.03). It is possible that individual techniques for performing daily spirometry could cause the variation seen in FVC results early on. This study examined results prior to and post the 3-month hospital FVC check and saw no significant variations. This helps eliminate individual technique as a contributor to varied results, and so the correlation between results of 28 days and 3 months being strong, significantly supports the relationship between change in FVC and disease progression. The 6-min walk distance (6MWD) (301±140 m versus 433±89 m; p=0.009) and the King's Brief Interstitial Lung Disease questionnaire (K-BILD) total score (46.3±8.1 versus 55.8±12.7; p=0.004) were lower in the progressive group, indicating more limitation of physical and subjective well-being [34].
Correlation between home-based spirometry and hospital-based monitoring
Nine studies [28, 30–32, 39, 41, 42, 45, 46] confirmed strong correlation between home and hospital-based spirometry readings of FVC. Six studies [30, 36, 41, 42, 45, 46] showed a significant positive correlation with a p-value <0.001 and r=0.93–0.98. Noth et al. [43] reported strong correlations between home- and clinic-measured FVC at all time-points (r=0.72 to 0.84), but correlations between home- and clinic-measured rates of change in FVC were weak (r=0.26 for rate of decline in FVC over 52 weeks). The correlations were weaker in subjects who provided more FVC readings per week. This was due to variability in change in FVC measured at home (greater number of outliers) and errors in measurements [43]. Variability in change from baseline in FVC was greater when measured by home rather than clinic spirometry [43]. However, Johannson et al. [20] and Maher et al. [50] report studies that had problems with measurement variability, and the quality assurance of home-based spirometry is a major consideration. Johannson et al. [20] showed that home-based monitoring of FVC value was variable and hence suggested hospital-based confirmation of FVC decline to prevent error, defeating the object of home monitoring. Similarly, Maher et al. [50] recommended further research before home measurements of FVC be used as a primary end-point in clinical trials and in particular, a need for a priori consideration of how the planned statistical analysis will handle data from patients with missing or variable spirometry values, so as not to affect planned statistical analyses [40, 43]. Variability might also have been caused by limited adherence, training, technical problems and lack of reminders [19, 29, 40]. Marcoux et al. [28] reported that correlation between home spirometer and office-based measurements declined at week 12.
Home versus hospital monitoring of medication use
Two studies by Moor et al. [30, 45] used an online eHealth application developed for patients with sarcoidosis and IPF. Patients kept track of their own health-related data, such as lung function, symptoms, medication and side-effects, and were provided with a graphical overview of their data. It was found that patients reported better insights into the effects of medication by seeing a daily overview of their lung function and potential disease progression. This suggests that patients with ILD had better-tailored treatment decisions during home monitoring programmes [30, 45]. Moreover, Broos et al. [41] suggest that home monitoring of physiological parameters could help physicians not only to detect disease progression but also to evaluate response to therapy.
Home versus hospital monitoring of well-being and health-related quality of life
Moor et al. [30] assessed health-related quality of life in patients with IPF using the K-BILD questionnaire in a 24-week randomised controlled trial. K-BILD is a validated, 15-item self-rated questionnaire, and an interstitial lung disease-specific, health-related quality of life questionnaire [30]. Home monitoring was not associated with a statistically significant improvement in K-BILD (mean difference 2.67 points; 95% CI −1.85–7.17; p=0.24). The RCT consisted of 90 patients; 46 out of 90 received home monitoring services. It was found that both the mean K-BILD score and the K-BILD psychological domain score was greater in the home monitoring group indicating improved general psychological well-being. The results of the RCT showed that the anxiety scores were low in both groups, improved psychological well-being and allowed for individually tailored treatment adjustments.
Discussion
We have conducted the first systematic review examining home monitoring of lung function and symptoms to detect ILD exacerbations and progression. 13 studies utilised home monitoring to measure feasibility and utility with two studies including disease progression as an outcome. The included studies provide evidence to support the feasibility and utility of home-based monitoring in patients with ILD [20, 28, 30–32, 38–43, 45, 46]. However, the included studies varied in their primary outcome, and were heterogeneous with respect to duration, measurements, and the type of technology and questionnaires used.
ILD relies on regular pulmonary function testing to guide management [6, 47–50]. Among the tools used for home-based monitoring, comparison of spirometry before and after an exacerbation and/or progression demonstrated that FVC decline reflects the severity of disease progression [2, 42, 51]. At present, spirometry is the primary test used to detect exacerbation and/or progression in ILD [52–54]. FVC variability was addressed in two of the included studies in patients with ILD. Veit et al. [32] and Russell et al. [31] demonstrated a link between variability of FVC and ILD disease progression [31, 32]. Veit et al. [32] found that FVC variability was a statistically significant predictor for disease progression [53, 55, 56]. Moreover, Russell et al. [31] confirmed that the rate of change in FVC was most predictive for disease progression and mortality when measured over 3, 6 and 12 months. Risk of variation can be mitigated by providing training, a technical helpdesk and real-time monitoring with reminders [30].
Early detection of disease progression and AE has been a focus for several diseases, especially in COPD [57]. Home monitoring of heart rate and oxygen saturation has been shown to result in early detection of exacerbation in COPD [26]. Similarly, previously studies reported exacerbation and/or progression in patients with ILD [6, 21, 22, 23]. Most studies until recently have only focused on the feasibility and reliability of home monitoring. However, the potential for home monitoring to facilitate early identification of AE-ILD has gained increasing interest during the past years. Recently, Moor et al. [40] reported that FVC decline could be detected 2 days before symptoms of infection began. Although it is possible to continuously monitor heart rate and oxygen saturation, the included studies in this review did not examine data for heart rate and oxygen saturation. Monitoring heart rate, 6MWD, activity and oxygen saturation remotely might contribute to a more precise prediction of disease exacerbation and/or progression [50, 53, 58–65].
Other factors to be considered are potential use of real-time monitoring and artificial intelligence to predict exacerbation and/or progression [60, 66–68]. Artificial intelligence is now adapted to interpret complex data in COPD to predict acute respiratory events [60, 69–73]. Artificial intelligence could allow monitoring of a large number of patients continuously and simultaneously. Utilising machine learning via an online platform with real-time data transmission could allow real-time detection of exacerbation and/or progression [53, 58, 74]. Predictors of disease exacerbation and/or progression have already been published but not specifically for patients with ILD [69, 75–77]. The ability to accurately detect rare occurrences, such as AE-IPF, offers the potential for clinical trials to assess early treatments for these, often devastating, events. We believe that machine learning and the use of an online platform with direct data transmission, of proven value in other diseases [69, 72], has promising potential in the field of ILD.
Encouraging findings were the high level of adherence and that patients were generally satisfied with home monitoring [29, 30, 39, 40]. Nevertheless, some studies showed that adherence to home-based monitoring decreased over time [20, 32, 78]. It is suggested that involving patients in monitoring their own condition would give some feeling of being in control and managing the condition [20, 79, 80]. This aligns with what has been suggested in respect to patients’ increase in adherence to, and satisfaction with, home-based monitoring [20, 39, 81, 82]. Another reason for patients to remain adherent might be the ability of home monitoring to generate early alerts of deterioration with the potential for early interventions [30].
In recent assessments of home monitoring for patients with ILD, healthcare providers were interested to use home monitoring for regular care and research purposes [83]. Although these findings are encouraging, further studies considering clinician perspectives are necessary. It is important to consider that the total number of participants was fewer than one thousand, and all were patients. This is not a complete representation of real-world clinical experience. Both patients and clinicians could benefit from effective home monitoring for patients with ILD to detect exacerbations and/or progression and to allow timelier intervention; for closer monitoring of therapeutic interventions; and to assess novel medications in clinical trials. The potential cost reduction on both patient and clinician sides could also be explored.
The potential of home monitoring of ILD patients was a consistent focus of the included studies, but the challenge of providing effective detection of exacerbation and/or progression has yet to be addressed. The published trials were mostly feasibility studies with a few ongoing studies [56, 84–86] focusing on detection of AE-ILD using home spirometry. Researchers should conduct longitudinal studies of physiological parameters and symptoms with real-time feedback from integrated spirometry, pulse oximetry and wearable devices and smartphone applications to assess their ability to detect exacerbation and/or progression in patients with ILD.
Conclusion
Although there were no studies reporting conclusively on the ability of home monitoring to detect deteriorations of ILD and AE-ILD, this systematic review suggests good adherence and feasibility of home monitoring. Home monitoring presents an opportunity for earlier detection of exacerbation and/or progression in ILD and examining this question should be the focus of future research.
Footnotes
Provenance: Submitted article, peer reviewed.
This article has supplementary material available from openres.ersjournals.com
Conflict of interest: M.A. Althobiani has nothing to disclose.
Conflict of interest: R.A. Evans has nothing to disclose.
Conflict of interest: J.S. Alqahtani has nothing to disclose.
Conflict of interest: A.M. Aldhahir has nothing to disclose.
Conflict of interest: A-M. Russell reports speaker fees, conference support, research support and consultancy fees from Boehringer Ingelheim, and speaker fees from Hoffman La Roche, outside the submitted work. A-M. Russell is a NIHR 70@70 Senior Research Fellow. The views expressed in this publication are those of the author(s) and not necessarily those of the National Institute for Health Research or the Dept of Health and Social Care.
Conflict of interest: J.R. Hurst has nothing to disclose.
Conflict of interest: J.C. Porter has nothing to disclose.
Support statement: This study was supported by Dept of Respiratory Therapy, Faculty of Medical Rehabilitation Sciences, King Abdulaziz University, Jeddah, Saudi Arabia through the Saudi Arabian Cultural Bureau in London.
References
- 1.Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011; 183: 788–824. doi: 10.1164/rccm.2009-040GL [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seibold MA, Wise AL, Speer MC, et al. A common MUC5B promoter polymorphism and pulmonary fibrosis. N Engl J Med 2011; 364: 1503–1512. doi: 10.1056/NEJMoa1013660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kropski JA, Pritchett JM, Zoz DF, et al. Extensive phenotyping of individuals at risk for familial interstitial pneumonia reveals clues to the pathogenesis of interstitial lung disease. Am J Respir Crit Care Med 2015; 191: 417–426. doi: 10.1164/rccm.201406-1162OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marshall RP, Puddicombe A, Cookson WO, et al. Adult familial cryptogenic fibrosing alveolitis in the United Kingdom. Thorax 2000; 55: 143–146. doi: 10.1136/thorax.55.2.143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Thoracic Society/European Respiratory Society. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med 2002; 165: 277–304. doi: 10.1164/ajrccm.165.2.ats01 [DOI] [PubMed] [Google Scholar]
- 6.Ley B, Collard HR, Talmadge E, et al. Clinical course and prediction of survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2011; 183: 431–440. doi: 10.1164/rccm.201006-0894CI [DOI] [PubMed] [Google Scholar]
- 7.British Lung Foundation. Lung disease in the UK – big picture statistics. https://statistics.blf.org.uk/ Date last accessed: 11 November 2020.
- 8.Lederer DJ, Martinez FJ. Idiopathic pulmonary fibrosis. N Engl J Med 2018; 378: 1811–1823. doi: 10.1056/NEJMra1705751 [DOI] [PubMed] [Google Scholar]
- 9.Lee SH, Kim SY, Kim DS, et al. Predicting survival of patients with idiopathic pulmonary fibrosis using GAP score: a nationwide cohort study. Respir Res 2016; 17: 131. doi: 10.1186/s12931-016-0454-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Noble PW, Albera C, Bradford WZ, et al. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): two randomised trials. Lancet 2011; 377: 1760–1769. doi: 10.1016/S0140-6736(11)60405-4 [DOI] [PubMed] [Google Scholar]
- 11.King TE, Bradford WZ, Castro-Bernardini S, et al. A Phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med 2014; 370: 2083–2092. doi: 10.1056/NEJMoa1402582 [DOI] [PubMed] [Google Scholar]
- 12.Richeldi L, du Bois RM, Raghu G, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med 2014; 370: 2071–2082. doi: 10.1056/NEJMoa1402584 [DOI] [PubMed] [Google Scholar]
- 13.Maher TM, Strek ME. Antifibrotic therapy for idiopathic pulmonary fibrosis: time to treat. Respir Res 2019; 20: 205. doi: 10.1186/s12931-019-1161-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raghu G, Chen SY, Yeh WS, et al. Idiopathic pulmonary fibrosis in US Medicare beneficiaries aged 65 years and older: incidence, prevalence, and survival, 2001–11. Lancet Respir Med 2014; 2: 566–572. doi: 10.1016/S2213-2600(14)70101-8 [DOI] [PubMed] [Google Scholar]
- 15.Win T, Screaton NJ, Porter JC, et al. Pulmonary (18)F-FDG uptake helps refine current risk stratification in idiopathic pulmonary fibrosis (IPF). Eur J Nucl Med Mol Imaging 2018; 45: 806–815. doi: 10.1007/s00259-017-3917-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karimi-Shah BA, Chowdhury BA. Forced vital capacity in idiopathic pulmonary fibrosis: FDA review of pirfenidone and nintedanib. N Engl J Med 2015; 372: 1189–1191. doi: 10.1056/NEJMp1500526 [DOI] [PubMed] [Google Scholar]
- 17.Spagnolo P, Maher TM. Clinical trial research in focus: why do so many clinical trials fail in IPF? Lancet Respir Med 2017; 5: 372–374. doi: 10.1016/S2213-2600(17)30122-4 [DOI] [PubMed] [Google Scholar]
- 18.Gross TJ, Hunninghake GW. Idiopathic pulmonary fibrosis. N Engl J Med 2001; 345: 517–525. doi: 10.1056/NEJMra003200 [DOI] [PubMed] [Google Scholar]
- 19.Wells AU, Behr J, Costabel U, et al. Hot of the breath: mortality as a primary end-point in IPF treatment trials: the best is the enemy of the good. Thorax 2012; 67: 938–940. doi: 10.1136/thoraxjnl-2012-202580 [DOI] [PubMed] [Google Scholar]
- 20.Johannson KA, Vittinghoff E, Morisset J, et al. Home monitoring improves endpoint efficiency in idiopathic pulmonary fibrosis. Eur Respir J 2017; 50: 1602406. doi: 10.1183/13993003.02406-2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Collard HR, Ryerson CJ, Corte TJ, et al. Acute exacerbation of idiopathic pulmonary fibrosis. An international working group report. Am J Respir Crit Care Med 2016; 194: 265–275. doi: 10.1164/rccm.201604-0801CI [DOI] [PubMed] [Google Scholar]
- 22.Song JW, Hong SB, Lim CM, et al. Acute exacerbation of idiopathic pulmonary fibrosis: incidence, risk factors and outcome. Eur Respir J 2011; 37: 356–363. doi: 10.1183/09031936.00159709 [DOI] [PubMed] [Google Scholar]
- 23.Leuschner G, Behr J. Acute exacerbation in interstitial lung disease. Front Med (Lausanne) 2017; 4: 176. doi: 10.3389/fmed.2017.00176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hurst JR, Donaldson GC, Quint JK, et al. Domiciliary pulse-oximetry at exacerbation of chronic obstructive pulmonary disease: prospective pilot study. BMC Pulm Med 2010; 10: 52. doi: 10.1186/1471-2466-10-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilkinson TMA, Donaldson GC, Hurst JR, et al. Early therapy improves outcomes of exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2004; 169: 1298–1303. doi: 10.1164/rccm.200310-1443OC [DOI] [PubMed] [Google Scholar]
- 26.Al Rajeh AM, Aldabayan YS, Aldhahir A, et al. Once daily versus overnight and symptom versus physiological monitoring to detect exacerbations of chronic obstructive pulmonary disease: pilot randomized controlled trial. JMIR Mhealth Uhealth 2020; 8: e17597. doi: 10.2196/17597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Denis F, Basch E, Septans A-L, et al. Two-year survival comparing web-based symptom monitoring vs routine surveillance following treatment for lung cancer. JAMA 2019; 321: 306–307. doi: 10.1001/jama.2018.18085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marcoux V, Wang M, Burgoyne SJ, et al. Mobile health monitoring in patients with idiopathic pulmonary fibrosis. Ann Am Thorac Soc 2019; 16: 1327–1329. doi: 10.1513/AnnalsATS.201904-335RL [DOI] [PubMed] [Google Scholar]
- 29.Moor CC, van Manen MJG, Tak NC, et al. Development and feasibility of an eHealth tool for idiopathic pulmonary fibrosis. Eur Respir J 2018; 51: 1702508. doi: 10.1183/13993003.02508-2017 [DOI] [PubMed] [Google Scholar]
- 30.Moor CC, Mostard RLM, Grutters JC, et al. Home monitoring in patients with idiopathic pulmonary fibrosis. A randomized controlled trial. Am J Respir Crit Care Med 2020; 202: 393–401. doi: 10.1164/rccm.202002-0328OC [DOI] [PubMed] [Google Scholar]
- 31.Russell AM, Adamali H, Molyneaux PL, et al. Daily home spirometry: an effective tool for detecting progression in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2016; 194: 989–997. doi: 10.1164/rccm.201511-2152OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Veit T, Barnikel M, Crispin A, et al. Variability of forced vital capacity in progressive interstitial lung disease: a prospective observational study. Respir Res 2020; 21: 270. doi: 10.1186/s12931-020-01524-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.British Lung Foundation. Coronavirus and COVID-19. Coronavirus and living with a lung condition. https://www.blf.org.uk/support-for-you/coronavirus/people-living-with-lung-condition Date last accessed: 24 March 2021.
- 34.Nakshbandi G, Moor CC, Wijsenbeek MS. Home monitoring for patients with ILD and the COVID-19 pandemic. Lancet Respir Med 2020; 8: 1172–1174. doi: 10.1016/S2213-2600(20)30452-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Antoniou KM, Raghu G, Tzilas V, et al. Management of patients with interstitial lung disease in the midst of the COVID-19 pandemic. Respiration 2020; 99: 625–627. doi: 10.1159/000509523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009; 339: b2535. doi: 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Med 2021; 18: e1003583. doi: 10.1371/journal.pmed.1003583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maher TM, Corte TJ, Fischer A, et al. Pirfenidone in patients with unclassifiable progressive fibrosing interstitial lung disease: a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Respir Med 2020; 8: 147–157. doi: 10.1016/S2213-2600(19)30341-8 [DOI] [PubMed] [Google Scholar]
- 39.Edwards C, Costello E, Cassidy N, et al. Use of the patientMpower app with home-based spirometry to monitor the symptoms and impact of fibrotic lung conditions: longitudinal observational study. JMIR Mhealth Uhealth 2020; 8: e16158. doi: 10.2196/16158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moor CC, Wapenaar M, Miedema JR, et al. A home monitoring program including real-time wireless home spirometry in idiopathic pulmonary fibrosis: a pilot study on experiences and barriers. Respir Res 2018; 19: 105. doi: 10.1186/s12931-018-0810-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Broos CE, Wapenaar M, Looman CWN, et al. Daily home spirometry to detect early steroid treatment effects in newly treated pulmonary sarcoidosis. Eur Respir J 2018; 51: 1702089. [DOI] [PubMed] [Google Scholar]
- 42.Moor CC, van Leuven SI, Wijsenbeek MS, et al. Feasibility of online home spirometry in systemic sclerosis-associated interstitial lung disease: a pilot study. Rheumatology (Oxford) 2020; 60: 2467–2471. doi: 10.1093/rheumatology/keaa607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Noth I, Cottin V, Chaudhuri N, et al. Home spirometry in patients with idiopathic pulmonary fibrosis: data from the INMARK trial. Eur Respir J 2021; 58: 2001518. doi: 10.1183/13993003.01518-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moor K, Visser L, Aerts J, et al. Diurnal variation in forced vital capacity in patients with fibrotic interstitial lung disease using home spirometry: the DIVA study. Eur Respir J 2019; 54: Suppl. 63, PA2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moor CC, Gür-Demirel Y, Wijsenbeek MS. Feasibility of a comprehensive home monitoring program for sarcoidosis. J Pers Med 2019; 9: 23. doi: 10.3390/jpm9020023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Moor CC, van den Berg CAL, Visser LS, et al. Diurnal variation in forced vital capacity in patients with fibrotic interstitial lung disease using home spirometry. ERJ Open Res 2020; 6: 00054-2020. doi: 10.1183/23120541.00054-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martinez FJ, Flaherty K. Pulmonary function testing in idiopathic interstitial pneumonias. Proc Am Thorac Soc 2006; 3: 315–321. doi: 10.1513/pats.200602-022TK [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.du Bois RM, Nathan SD, Richeldi L, et al. Idiopathic pulmonary fibrosis: lung function is a clinically meaningful endpoint for phase III trials. Am J Respir Crit Care Med 2012; 186: 712–715. doi: 10.1164/rccm.201206-1010PP [DOI] [PubMed] [Google Scholar]
- 49.Erbes R, Schaberg T, Loddenkemper R. Lung function tests in patients with idiopathic pulmonary fibrosis: are they helpful for predicting outcome? Chest 1997; 111: 51–57. doi: 10.1378/chest.111.1.51 [DOI] [PubMed] [Google Scholar]
- 50.Maher TM, Corte TJ, Kreuter M, et al. Home spirometry as a primary endpoint in clinical trials: sensitivity analyses of a randomized controlled trial of pirfenidone in patients with unclassifiable interstitial lung disease (UILD). Am J Respir Crit Care Med 2020; 201: A2575. doi: 10.1164/ajrccm-conference.2020.201.1_MeetingAbstracts.A2575 [DOI]
- 51.du Bois RM, Weycker D, Albera C, et al. Ascertainment of individual risk of mortality for patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2011; 184: 459–466. doi: 10.1164/rccm.201011-1790OC [DOI] [PubMed] [Google Scholar]
- 52.Bois R, Weycker D, Albera C, et al. Forced vital capacity in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2011; 184: 1382–1389. doi: 10.1164/rccm.201105-0840OC [DOI] [PubMed] [Google Scholar]
- 53.Collard HR, King TE, Bartelson BB, et al. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2003; 168: 538–542. doi: 10.1164/rccm.200211-1311OC [DOI] [PubMed] [Google Scholar]
- 54.Zappala CJ, Latsi PI, Nicholson AG, et al. Marginal decline in forced vital capacity is associated with a poor outcome in idiopathic pulmonary fibrosis. Eur Respir J 2010; 35: 830–836. doi: 10.1183/09031936.00155108 [DOI] [PubMed] [Google Scholar]
- 55.Flaherty KR, Andrei A-C, Murray S, et al. Idiopathic pulmonary fibrosis: prognostic value of changes in physiology and sixminutewalk test. Am J Respir Crit Care Med 2006; 174: 803–809. doi: 10.1164/rccm.200604-488OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wijsenbeek M, Bendstrup E, Valenzuela C, et al. Design of a study assessing disease behaviour during the peri-diagnostic period in patients with interstitial lung disease: the STARLINER Study. Adv Ther 2019; 36: 232–243. [DOI] [PMC free article] [PubMed]
- 57.Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010; 363: 1128–1138. doi: 10.1056/NEJMoa0909883 [DOI] [PubMed] [Google Scholar]
- 58.Swigris JJ, Swick J, Wamboldt FS, et al. Heart rate recovery after 6-min walk test predicts survival in patients with idiopathic pulmonary fibrosis. Chest 2009; 136: 841–848. doi: 10.1378/chest.09-0211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Seemungal TAR, Donaldson GC, Paul EA, et al. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998; 157: 1418–1422. doi: 10.1164/ajrccm.157.5.9709032 [DOI] [PubMed] [Google Scholar]
- 60.Shah SA, Velardo C, Farmer A, et al. Exacerbations in chronic obstructive pulmonary disease: identification and prediction using a digital health system. J Med Internet Res 2017; 19: e69. doi: 10.2196/jmir.7207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wu W, Jordan S, Becker MO, et al. Prediction of progression of interstitial lung disease in patients with systemic sclerosis: the SPAR model. Ann Rheum Dis 2018; 77: 1326–1332. doi: 10.1136/annrheumdis-2018-213201 [DOI] [PubMed] [Google Scholar]
- 62.Bahmer T, Kirsten AM, Waschki B, et al. Clinical correlates of reduced physical activity in idiopathic pulmonary fibrosis. Respiration 2016; 91: 497–502. doi: 10.1159/000446607 [DOI] [PubMed] [Google Scholar]
- 63.Wallaert B, Monge E, Le Rouzic O, et al. Physical activity in daily life of patients with fibrotic idiopathic interstitial pneumonia. Chest 2013; 144: 1652–1658. doi: 10.1378/chest.13-0806 [DOI] [PubMed] [Google Scholar]
- 64.Root ED, Graney B, Baird S, et al. Physical activity and activity space in patients with pulmonary fibrosis not prescribed supplemental oxygen. BMC Pulm Med 2017; 17: 154. doi: 10.1186/s12890-017-0495-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bahmer T, Kirsten A-M, Waschki B, et al. Prognosis and longitudinal changes of physical activity in idiopathic pulmonary fibrosis. BMC Pulm Med 2017; 17: 104. doi: 10.1186/s12890-017-0444-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jha S, Topol EJ. Adapting to artificial intelligence: radiologists and pathologists as information specialists. JAMA 2016; 316: 2353–2354. doi: 10.1001/jama.2016.17438 [DOI] [PubMed] [Google Scholar]
- 67.Dilsizian SE, Siegel EL. Artificial intelligence in medicine and cardiac imaging: harnessing big data and advanced computing to provide personalized medical diagnosis and treatment. Curr Cardiol Rep 2014; 16: 441. doi: 10.1007/s11886-013-0441-8 [DOI] [PubMed] [Google Scholar]
- 68.Neill DB. Using artificial intelligence to improve hospital inpatient care. IEEE Intell Syst 2013; 28: 92–95. doi: 10.1109/MIS.2013.51 [DOI] [Google Scholar]
- 69.Esteban C, Moraza J, Esteban C, et al. Machine learning for COPD exacerbation prediction. Eur Respir J 2015; 46: Suppl. 59, OA3282. [Google Scholar]
- 70.Topalovic M, Das N, Burgel P-R, et al. Artificial intelligence outperforms pulmonologists in the interpretation of pulmonary function tests. Eur Respir J 2019; 53: 1801660. doi: 10.1183/13993003.01660-2018 [DOI] [PubMed] [Google Scholar]
- 71.Sanchez-Morillo D, Fernandez-Granero MA, Leon-Jimenez A. Use of predictive algorithms in-home monitoring of chronic obstructive pulmonary disease and asthma: a systematic review. Chron Respir Dis 2016; 13: 264–283. doi: 10.1177/1479972316642365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Finkelstein J, Jeong IC. Machine learning approaches to personalize early prediction of asthma exacerbations. Ann N Y Acad Sci 2017; 1387: 153–165. doi: 10.1111/nyas.13218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Orchard P, Agakova A, Pinnock H, et al. Improving prediction of risk of hospital admission in chronic obstructive pulmonary disease: application of machine learning to telemonitoring data. J Med Internet Res 2018; 20: e263. doi: 10.2196/jmir.9227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Darcy AM, Louie AK, Roberts LW. Machine learning and the profession of medicine. JAMA 2016; 315: 551–552. doi: 10.1001/jama.2015.18421 [DOI] [PubMed] [Google Scholar]
- 75.Janson C, Johansson G, Larsson K, et al. Use of Machine learning to predict asthma exacerbations. Eur Respir J 2020; 56: Suppl. 64, 4802. [Google Scholar]
- 76.Peng J, Chen C, Zhou M, et al. A machine-learning approach to forecast aggravation risk in patients with acute exacerbation of chronic obstructive pulmonary disease with clinical indicators. Sci Rep 2020; 10: 3118. doi: 10.1038/s41598-020-60042-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Young AL, Bragman FJS, Rangelov B, et al. Disease progression modeling in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2019; 201: 294–302. doi: 10.1164/rccm.201908-1600OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Noth I, Maher TM, Johannson KA, et al. Adherence to home spirometry among patients with IPF: results from the INMARK trial. Eur Respir J 2019; 54: Suppl. 63, PA2241. doi: 10.1183/13993003.01797-2018 [DOI] [Google Scholar]
- 79.Velardo C, Shah SA, Gibson O, et al. Digital health system for personalised COPD long-term management. BMC Med Inform Decis Mak 2017; 17: 19. doi: 10.1186/s12911-017-0414-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Swigris J, Nathan S, Tighe R, et al. STARMAP: an observational study to assess disease-relevant outcomes using home-monitoring devices in patients with idiopathic pulmonary fibrosis (IPF). Eur Respir J 2019; 54: Suppl. 63, PA1333. [Google Scholar]
- 81.Lenferink A, Brusse-Keizer M, van der Valk P, et al. Self-management interventions including action plans for exacerbations versus usual care in patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2017; 8: CD011682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wijsenbeek MS, Bendstrup E, Valenzuela C, et al. Interim analysis of patients with ILD enrolled in the STARLINER study. Eur Respir J 2019; 54: Suppl. 63, PA1335. [Google Scholar]
- 83.Nakshbandi G, Moor CC, Johannson KA, et al. Worldwide experiences and opinions of healthcare providers on eHealth for patients with interstitial lung diseases in the COVID-19 era. ERJ Open Res 2021; 7: 00405-2021. doi: 10.1183/23120541.00405-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. https://clinicaltrials.gov/ct2/show/NCT04304898 ClinicalTrials.gov Identifier NCT04304898. An International Patient-led Registry in Fibrotic Interstitial Lung Diseases Using eHealth Technology (I-FILE).
- 85. https://clinicaltrials.gov/ct2/show/NCT03979430 ClinicalTrials.gov Identifier NCT03979430. Early Detection of Acute Exacerbation in Patients with Idiopathic Lung Fibrosis - a Pilot Study.
- 86.Ranjan Y, Althobiani M, Jacob J, et al. Remote assessment of lung disease and impact on physical and mental health (RALPMH): protocol for a prospective observational study. JMIR Res Protoc 2021; 10: e28873. [DOI] [PMC free article] [PubMed] [Google Scholar]