Abstract
Background and aims
Our departmental planning for COVID-19 was actioned a week before the lockdown (13th March 2020). We look at a 7- week lockdown activity for all scheduled outpatient clinics and urgent procedures.
Methods and results
A total of 2361 outpatient clinic slots (52.6% oncology slots and 47.4% benign urology slots) were scheduled during this period. The oncology slots included 330 (26.5%) flexible cystoscopy, 555 (44.7%) prostate cancer and 357(28.8%) non-prostate cancer slots. The benign urology slots included 323 (28.8%) andrology, 193 (17.2%) stones and 603 (54%) lower urinary tract symptoms (LUTS) slots. Of the total oncology outpatient slots (n = 1242), 66.3% were virtual consultations, 20% were face-to-face and 13.6% were cancelled. Of the total benign outpatient slots (n = 1119), 81% were virtual consultations, 9.7% were face-to-face and 9.3% were cancelled. A total of 116 anaesthetic surgical procedures were carried out, of which 54 (46.5%) were oncological procedures, 18 (15.5%) were benign urological procedures, and 44 (38%) were diagnostic procedures.
Conclusions
Hospitals and urologists can benefit from the model used by our hospital to mitigate the impact and prioritise patients most in need of urgent care. Reorganisation and flexibility of healthcare delivery is paramount in these troubled times and will allow clinical activity without compromising patient safety.
Keywords: Telemedicine, COVID-19, urgent, urology, clinics
The severe acute respiratory syndrome coronavirus-2(SARS-CoV-2) has rapidly spread around the world affecting all inhabited continents.1 As of the 28th July 2020, >16 million people have been infected with approximately 650,000 deaths globally. Coronavirus-2019 (COVID-19) was declared a public health emergency and a pandemic on the 11th March 2020 by the World Health Organisation (WHO).2 United Kingdom (UK) is one of the most affected countries in Europe with an estimated 300,000 people infected and approximately 46,000 deaths.3
On 23rd March 2020 a general lockdown was started in the UK to avoid the spread of infection. British Association of Urological Surgeons (BAUS) recommended guidelines for the management of clinical activities and urological procedures.4 Hospitals in the National Health Service (NHS) reorganised and redeployed services to prioritise and strengthen frontline staff. Routine outpatient clinics and elective surgery were cancelled to allocate resources, with risk stratified approach to cater urgent and high-risk cancer procedures only. Telemedicine was adopted for outpatient clinics to avoid the risk of transmission, and face-to-face clinics were minimised to performing outpatient procedures such as flexible cystoscopy and shock wave lithotripsy (SWL). A proportion of patients needing routine follow-up for check flexible cystoscopy, SWL and lower urinary tract symptoms (LUTS) were cancelled, wherein a follow-up planned after the normal services resume.
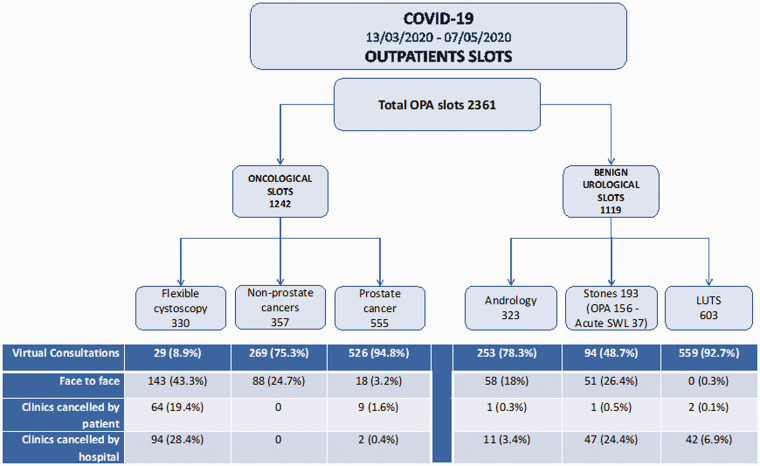
Our departmental planning for COVID-19 was actioned a week before the lockdown (13th March 2020). We look at a 7-week lockdown activity (till 7th May 2020) for all scheduled outpatient clinics and urgent procedures. A total of 2361 outpatient clinic slots (52.6% oncology slots and 47.4% benign urology slots) were scheduled during this period (Figure 1). The oncology slots included 330 (26.5%) flexible cystoscopy, 555 (44.7%) prostate cancer and 357 (28.8%) non-prostate cancer slots. The benign urology slots included 323 (28.8%) andrology, 193 (17.2%) stones and 603 (54%) LUTS slots.
Figure 1.
Outcomes of outpatient clinic slots during the 7 weeks of COVID-19 lockdown.
Where possible, all face-to-face slots were changed to virtual telephone or video clinic slots, although patients did attend for flexible cystoscopy and SWL procedures. Of the total oncology outpatient slots(n = 1242), 66.3% were virtual consultations, 20% were face-to-face, 5.9% were cancelled by the hospital and 7.7% was cancelled by the patient. Over half of the face-to-face (57%) consultations were related to flexible cystoscopy, and of the cancellations, 90% were related to diagnostic flexible cystoscopy which we electively triaged and deferred. Of the total benign outpatient slots (n = 1119), 81% were virtual consultations, 9.7% were face-to-face, 0.4% were cancelled by the hospital and 8.9% were cancelled by the patient. Of 193 stone patients, 37 (19%) had acute SWL for ureteric stones. Of these, 15 treatments for ureteric stones were done for patients from nearby hospitals where they would otherwise undergo emergency stent or ureteroscopy under a general anaesthetic.
A total of 116 anaesthetic surgical procedures were carried out, of which 54 (46.5%) were oncological procedures, 18 (15.5%) were benign urological procedures, and 44 (38%) were diagnostic procedures. The oncological procedures included transurethral resection of bladder tumour (n = 18), radical cystectomy (n = 15), radical prostatectomy (n = 6), radical nephrectomy(n = 5), and others including RPLND, penile cancer and radical orchidectomy (n = 10). The benign procedures included ureteroscopy for acute stones(n = 10), percutaneous nephrolithotomy for obstructing stones(n = 4), and others (n = 4). The diagnostic procedures were all risk stratified and on cancer pathways including template biopsy (n = 33), cystoscopy +/− biopsy(n = 7) and others (n = 4). The oncology and benign stone multidisciplinary meetings (MDT) were done virtually via ‘Microsoft Teams’ app(Microsoft, USA) and patients were discussed using electronic notes, with screen share to view images.
According to WHO, telemedicine involves ‘The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies’. This approach of communication and consultation was more pragmatic then cancelling their slots. It can be used for majority of oncological and non-oncological consultations except where a physical examination is paramount or an outpatient procedure such as flexible cystoscopy is necessary. Although virtual consultations cannot always replace their face-to-face counterparts, it can be helpful in most scenarios. However, there is a risk of loss of vital clinical information, and hence accurate and up-to-date electronic patient notes must be available.
For their surgical procedures, all patients were asked to self-isolate a week prior to their surgery and a negative COVID-19 swab was mandatory to proceed. Adequate protocol based personal protective equipment (PPE) was mandatory for anaesthetic and surgical staff based on the Royal College of Surgeons (RCS) guidance.5 All procedures were carried out at Spire Southampton Hospital or the Royal Southhants Hospital, which served as an NHS cold site with no COVID-19 patients. Over 7 weeks, 116 procedures were carried out and none of the patients developed symptoms or complications related to COVID-19.
Our model shows that despite the adversities caused from the COVID-19, virtual outpatient clinics and urgent urological surgery can be carried out to minimise disruption. Using a mixture of telemedicine and face-to-face consultations, 86% of oncological and 91% of benign urological outpatient activities were carried out. A risk stratified approach is however necessary to continue to deliver urological services and potentially mitigate the impact of delaying patients most in need. Operative procedures need to be based on clinical urgency and should be clinician led with appropriate patient counselling regarding the risk and benefit of intervention and match the resources available to carry them out. While social distancing lasts, it is in the best interest for patients and healthcare providers to use telehealth where possible. It would be especially useful when physical examination or office based diagnostic procedure is not necessary. While the use of telemedicine has risen steeply during COVID-19, it is likely to stay and become a reality even in non-pandemic times and healthcare systems should try and adopt this in future. However, clinicians and healthcare professionals need to be trained in telemedicine before its widespread uptake and use.
Healthcare systems worldwide have been forced to postpone treatment for urological conditions and surgical practice is changing due to risks posed by COVID-19. Hospitals and urologists can benefit from the model used by our hospital to mitigate the impact and prioritise patients most in need of urgent care. Reorganisation and flexibility of healthcare delivery is paramount in these troubled times and will allow clinical activity without compromising patient safety.
Acknowledgements
The urology department staff including all consultants and nurses who helped during COVID-19.
Authors’ contribution
BS and AP designed the study. AP collected and analysed the data. BS wrote the manuscript and JS revised the final manuscript.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Bhaskar K Somani https://orcid.org/0000-0002-6248-6478
References
- 1.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395: 507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus, www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed 28 July 2020).
- 3.COVID-19 daily deaths. NHS England, www.england.nhs.uk/statistics/statistical-work-areas/covid-19-daily-deaths/ (accessed 28 July 2020).
- 4.BAUS Coronavirus & COVID-19. British Association of Urological Surgeons (BAUS), www.baus.org.uk/about/coronavirus_covid-19.aspx (accessed 19 May 2020).
- 5.Royal College of Surgeons information hub COVID-19. Royal College of Surgeons, www.rcseng.ac.uk/coronavirus/ (accessed 19 May 2020).