Abstract
Background:
Arthroscopy-assisted reduction percutaneous internal fixation (ARIF) has emerged recently as an alternative treatment method in treating lower-energy tibial plateau fractures. To date, the comparison of clinical efficacy between ARIF and open reduction internal fixation (ORIF) is limited, with divergent conclusions.
Purpose:
To review studies on the clinical efficacy of ARIF and ORIF in the treatment of tibial plateau fracture.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
A search was conducted using the PubMed, Web of Science, Cochrane Library, and EMBASE databases between inception and August 20, 2020, for retrospective and prospective studies evaluating ARIF versus ORIF in the treatment of tibial plateau fracture. We identified 6 clinical studies that met the inclusion criteria, with 231 patients treated with ARIF and 386 patients treated with ORIF. The risk of bias and the quality of evidence of the included studies were assessed. The 2 treatment types were compared in terms of clinical results and complications by using odds ratios (ORs), mean differences (MDs), or standardized mean differences (SMDs), with 95% confidence intervals (CIs). Heterogeneity among studies was quantified using the I 2 statistic.
Results:
The quality of the studies was high. Compared with ORIF, treatment with ARIF led to better clinical function (SMD = 0.31; 95% CI, 0.14 to 0.48; I 2 = 15%; P = .0005), shorter hospital stay (MD = –2.37; 95% CI, –2.92 to –1.81; I 2 = 0%; P < .001), and more intra-articular lesions found intraoperatively (OR = 3.76; 95% CI, 1.49 to 9.49; I 2 = 66%; P = .005). There were no complications or significant differences between the techniques in the radiological evaluation of reduction.
Conclusion:
Compared with ORIF, the ARIF technique for tibial plateau fractures led to faster postoperative recovery and better clinical function and the ability to find and treat more intra-articular lesions during the operation. However, the radiological evaluation of reduction and complications were not significantly different between the 2 groups.
Keywords: arthroscopy-assisted reduction percutaneous internal fixation (ARIF), open reduction internal fixation (ORIF), tibial plateau fracture, clinical function, faster recovery, intra-articular lesions, meta-analysis
Tibial plateau fractures, which are typically caused by high-energy trauma or osteoporosis in older adults, comprise approximately 1% of all fractures, 2,4,5 and many different surgical techniques and approaches have been described for the management of tibial plateau fractures. 18,42 There are 2 principles in the treatment of tibial plateau fractures: one is the anatomic reduction of the articular surface and reconstruction of the mechanical axis of the lower limb, and the other is to reconstruct the stability of the injured knee joint. Tibial plateau fractures are usually classified using Schatzker type (I-VI) or the 3-column system. 25,33 Traditionally, although displaced tibial plateau fractures are treated with open reduction internal fixation (ORIF), many surgical approaches and techniques have been developed, 37 such as the anterolateral approach and posteromedial inverted L-shape approach. However, complications after ORIF, such as infections, hematoma formation, surgical wound dehiscence, and knee stiffness, are common. 12,13
Recently, arthroscopy-assisted reduction percutaneous internal fixation (ARIF) has emerged as an alternative treatment method in treating lower-energy tibial plateau fractures. ARIF was first reported by Caspari et al 3 and Jennings 17 in patients with fractures of Schatzker types I to III. This method has the advantage of the minimally invasive operation damage without violating the intra-articular structures and the treatment of additional intra-articular lesions. A large number of studies have reported the satisfactory clinical and radiological results of ARIF in treating tibial plateau fracture. 6,31,34 Thus, it seems ARIF has advantages in the treatment of tibial plateau fracture; however, there has been little published meta-analysis of the comparison between ARIF and ORIF in tibial plateau fracture. 40
Since the differences between ARIF and ORIF in tibial plateau fracture were not very clear, this up-to-date meta-analysis study aimed to compare functional and radiological results, complication rates, and other clinical measurements of ARIF with those of traditional ORIF in the treatment of tibial plateau fractures. We hypothesized that ARIF would have a lower complication rate, faster postoperative recovery, and better functional and radiological results.
Methods
Search Strategy and Article Selection
A systematic search of the literature was performed on August 20, 2020, in the PubMed, Web of Science, Cochrane Library, and EMBASE databases with the following search string: ((tibial plateau fracture OR tibial platform fracture) AND (arthroscopy OR arthroscopic OR ARIF) AND (open OR operation OR surgery OR ORIF)). We supplemented the electronic database examination by searching the reference lists of selected articles manually. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were followed. 26 The article selection process was performed independently by 2 authors (L.J., E.C.). Any disagreement in the selection was resolved by consensus or by the intervention of a third author (L.H.).
Eligibility Criteria
The inclusion criteria were the following: (1) clinical studies comparing ARIF versus ORIF in treating acute tibial plateau fracture (3 weeks from injury to surgery), including randomized controlled trials (RCTs), cohort studies, and case-control studies; (2) published in English; (3) included functional outcomes; (4) follow-up time >12 months; and (5) full text of studies available. The exclusion criteria were the following: (1) letters, comments, case reports, reviews, animal studies, cadaveric studies, biomechanical studies, and study protocols; (2) only abstract available; (3) chronic tibial plateau fracture (3 weeks after trauma); and (4) duplicated studies and data.
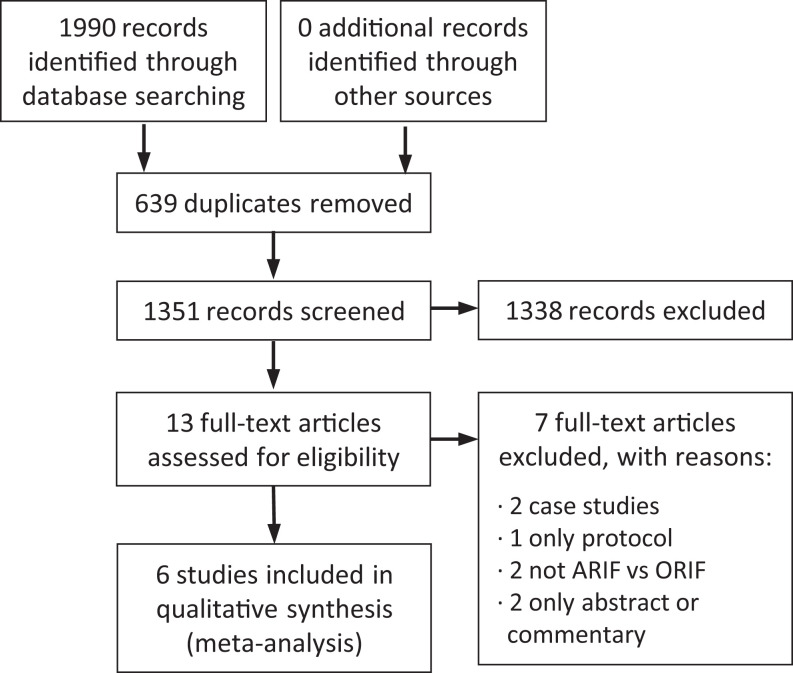
The database search resulted in 1990 records, 639 of which were duplicates. Of the remaining 1351 articles, after the title and abstract screening, 13 articles remained eligible for full-text screening. From these studies, 5 retrospective case-control studies and 1 prospective RCT met the inclusion criteria. 8,11,22,27,39,41 Figure 1 shows the flowchart of study inclusion.
Figure 1.
Flow diagram based on the PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) guidelines outlining the literature search, screening, and review. ARIF, arthroscopy-assisted reduction percutaneous internal fixation; ORIF, open reduction internal fixation.
Data Assessment
An electronic piloted form was created for data extraction. Data including study design, sample size, length of follow-up, patient sex and age at surgery, Schatzker tibial plateau fracture classification, hospital stay, and functional outcome parameters were extracted. The functional outcomes were evaluated in terms of the Rasmussen clinical score, 30 Knee Society Score (KSS), 16 Hohl and Delamarter scoring system, and Hospital for Special Surgery (HSS) score. 29 In addition, associated intra-articular injuries and complications as defined in each study were collected. Radiological outcomes were evaluated using the Rasmussen radiological score (excellent = 18, good = 12-17, fair = 6-11, and poor = 0-5), 30 in which the comparison was made using either the point score or the percentage of cases graded as excellent/good versus fair/poor, as provided.
Assessment of Risk of Bias and Quality of Evidence
The risk of bias for RCTs was assessed using the revised Cochrane risk-of-bias tool for randomized trials (RoB 2.0). 36 The overall quality of evidence for retrospective case-control studies or prospective cohort studies was graded according to the Newcastle-Ottawa Scale (NOS) guidelines. 24 All assessments were checked by 2 reviewers (L.J., C.W.), and any disagreements were resolved via discussion or the involvement of a third author (E.C.).
Statistical Analysis
Statistical analysis was performed using RevMan Version 5.3.5 (Cochrane Community) for outcome measurements. Estimations of the overall results are shown as forest plots. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated for dichotomous outcomes, and mean differences (MDs) with 95% CIs were used for continuous outcomes. When the same outcome was measured using different scales or the same data were calculated with either dichotomous or continuous outcomes, the standardized mean difference (SMD) was calculated. Heterogeneity among studies was quantified using the I 2 statistic, and substantial heterogeneity was represented by an I 2 value >50%. Random-effects models were used when significant heterogeneity was detected in the meta-analysis; otherwise, fixed-effects models were used. P <.05 was considered statistically significant.
Results
Study Characteristics
The quality of evidence for the 5 case-control studies was considered good according to the NOS, and the risk of bias of the RCT was considered low according to RoB 2.0. All studies were of high quality. Individual study characteristics are provided in Table 1. Among the 6 studies, a total of 617 patients participated (231 in the ARIF group, 386 in the ORIF group) with a follow-up rate of 100% and a frequency weighted mean follow-up time of 41.4 months (range, 12-116 months). The frequency-weighted mean age of participants was 48.4 years (range, 13-77 years); 364 were male and 253 were female. According to the Schatzker tibial plateau fracture classification, there were 123 cases of type I, 277 of type II, 179 of type III, 16 of type IV, 12 of type V, and 10 of type VI. The interval from injury to surgery was <3 weeks.
Table 1.
Study Characteristics a
| First Author (year) | Study Design | Sample Size, ARIF/ORIF | Sex, M/F | Age, y | Follow-up, mo | Schatzker Classification, I/II/III/IV/V/VI | Quality Score b |
|---|---|---|---|---|---|---|---|
| Verona (2019) 39 | Case-control | 19/21 | 21/19 | 48 ± 16 | 41.95 ± 28.85 | 5/16/19/0/0/0 | 9 (good) |
| Elabjer (2017) 11 | RCT | 40/35 | 58/17 | 47 | 13.5 | 19/33/23/0/0/0 | Low risk of bias |
| Ohdera (2003) 27 | Case-control | 19/9 | 9/19 | 48 | 31.5 | 0/15/13/0/0/0 | 7 (good) |
| Dall’oca (2012) 8 | Case-control | 50/50 | 54/46 | 51 | 73 ± 27 | 14/12/44/8/0/0 | 9 (good) |
| Wang (2017) 41 | Case-control | 26/31 | 36/21 | 46 | 44 ± 11.8 | 9/28/12/8/12/10 | 8 (good) |
| Le Baron (2019) 22 | Case-control | 77/240 | 186/131 | 48 ± 14 | 38 ± 23 | 76/173/68/0/0/0 | 9 (good) |
a Data are presented in M ± SD. ARIF, arthroscopy-assisted reduction percutaneous internal fixation; ORIF, open reduction internal fixation; RCT, randomized controlled trial.
b Study quality was assessed with the Newcastle-Ottawa Scale for case-control studies (good, fair, or poor) and the revised Cochrane risk-of-bias tool for randomized trials (low or high risk of bias).
Functional Outcomes
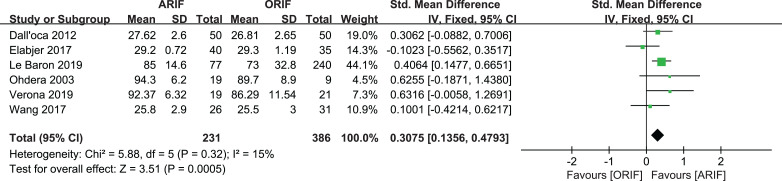
The Rasmussen clinical assessment score was used in 3 studies 8,11,41 ; the HSS score, in 1 study 22 ; the Hohl and Delamarter score, in 1 study 27 ; and the KSS, in 1 study. 39 The results indicated statistically significantly better postoperative functional outcomes for patients treated with ARIF compared with ORIF (SMD = 0.31; 95% CI, 0.14-0.48; I 2 = 15%; P = .0005) (Figure 2).
Figure 2.
Forest plot of postoperative patients’ clinical functional score. ARIF, arthroscopy-assisted reduction percutaneous internal fixation; IV, inverse variance; ORIF, open reduction internal fixation. Std., standard deviation.
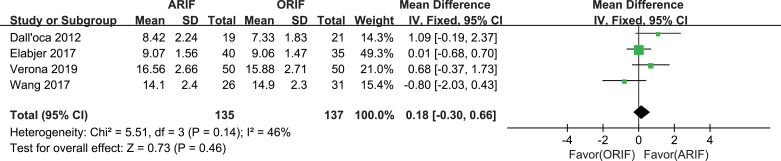
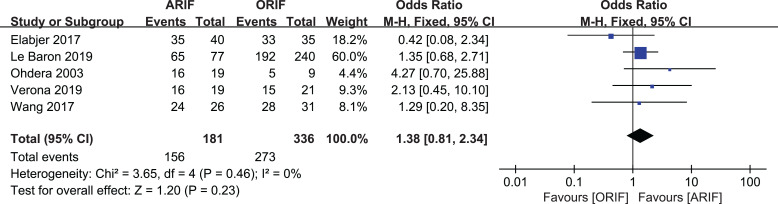
Regarding the Rasmussen radiological evaluation, the point score was reported in 4 studies comprising 135 patients with ARIF and 137 patients with ORIF 8,11,39,41 and ranged from 10 to 18. The mean score was 12.04 in the ARIF group and 11.79 in the ORIF group, with no statistically significant difference between groups (MD = 0.18; 95% CI, –0.30 to 0.66; I 2 = 46%; P = .46) (Figure 3). The Rasmussen evaluation was reported as a grade in 5 studies comprising 181 patients with ARIF and 336 patients with ORIF. 11,22,27,39,41 The percentage of fracture reductions graded as excellent/good was 86.2% in the ARIF and 81.3% in the ORIF group, with no significant between-group difference (OR = 1.38; 95% CI, 0.81 to 2.34; I 2 = 0%; P = .23) (Figure 4).
Figure 3.
Forest plot of postoperative patients’ Rasmussen radiological score. ARIF, arthroscopy-assisted reduction percutaneous internal fixation; IV, inverse variance; ORIF, open reduction internal fixation.
Figure 4.
Forest plot of postoperative patients’ Rasmussen radiological evaluation. ARIF, arthroscopy-assisted reduction percutaneous internal fixation; M-H, Mantel-Haenszel; ORIF, open reduction internal fixation.
Other Clinical Results
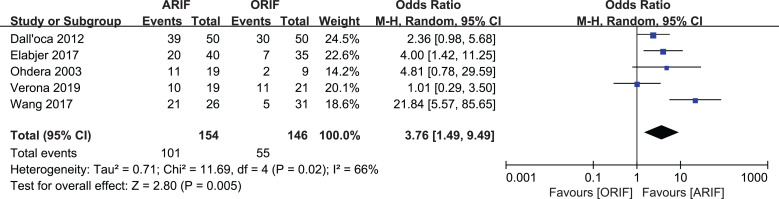
Associated intra-articular injuries found intraoperatively were reported in 5 studies, 8,11,27,39,41 of which 154 cases were patients with ARIF and 146 cases were patients with ORIF. Intra-articular injuries included meniscal tear, chondral damage, and ligament rupture. The rate of intra-articular injuries found was 65.6% in the ARIF group and 37.7% in the ORIF group, which was statistically significantly higher in favor of the ARIF technique (OR = 3.76; 95% CI, 1.49-9.49; I 2 = 66%; P = .005) (Figure 5). The intra-articular injuries were treated simultaneously using fracture management in all reports.
Figure 5.
Forest plot of rate of associated intra-articular injuries found intraoperatively. ARIF, arthroscopy-assisted reduction percutaneous internal fixation; M-H, Mantel-Haenszel; ORIF, open reduction internal fixation.
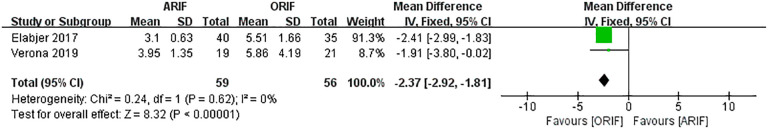
Hospital stay was reported in 2 studies comprising 59 patients with ARIF and 56 patients with ORIF. 11,39 The mean hospital stay in the ARIF group was 3.37 days as opposed to 5.64 days in the ORIF group. There was a statistically significant difference in favor of the ARIF technique (MD, –2.37; 95% CI, –2.92 to –1.81; I 2 = 0%; P < .001) (Figure 6).
Figure 6.
Forest plot of postoperative patients’ hospital stay. ARIF, arthroscopy-assisted reduction percutaneous internal fixation; IV, inverse variance; ORIF, open reduction internal fixation.
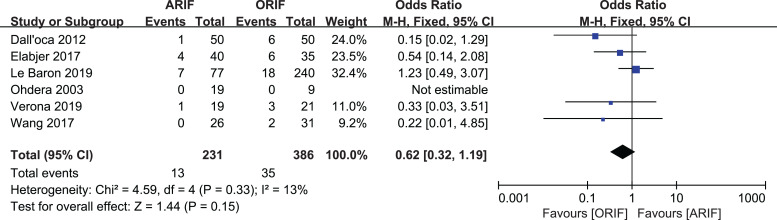
Complications
Complications were reported in all 6 studies. 8,11,22,27,39,41 The reported complication rate for the patients in the ARIF group was 5.6%, with 9.1% for the ORIF group. There was no statistically significant difference between the 2 groups (OR, 0.62; 95% CI, 0.32-1.19; I 2 = 13%; P = .15), but the ARIF group showed lower complication rates compared with the ORIF group (Figure 7).
Figure 7.
Forest plot of postoperative patients’ complications. ARIF, arthroscopy-assisted reduction percutaneous internal fixation; M-H, Mantel-Haenszel; ORIF, open reduction internal fixation.
Discussion
In this comprehensive meta-analysis, ARIF provided better clinical function and shorter hospital stays for patients and led to more intra-articular lesions found intraoperatively compared with ORIF. However, the fracture reduction evaluation and postoperative complication rate for ARIF and ORIF were similar.
There has been a limited number of published meta-analyses about ARIF compared with ORIF in treating tibial plateau fracture. Wang et al 40 reported their meta-analysis about ARIF and ORIF in 2018, but all trials included in their meta-analysis were conducted in China with small sample sizes, lacked diversity, and were written in Chinese. Thus, the results suggested in their meta-analysis, that the clinical function of ARIF is superior to that of ORIF and that the risk of perioperative complications in the ARIF group is statistically significantly lower than in the ORIF group, may not be conclusive. ARIF has features allowing minimally invasive operation damage without violating the intra-articular structures, 1,38 which could maintain the integrity of the lateral knee capsule. Further, avoidance of meniscal detachment preserves maximum function of the affected knees. According to the results of our meta-analysis, ARIF treatment in tibial plateau fracture could significantly shorten hospital stay, which means ARIF could promote patient recovery more than could the traditional ORIF technique. Although the radiological evaluation was similar between the 2 groups, patients in the ARIF group recovered from the operation more quickly and had better clinical function because of the minimally invasive damage during the operation.
A number of studies have demonstrated satisfactory short-term functional and radiological results of ARIF in the treatment of tibial plateau fracture. 8,7,9,19,23,32 There was no need to perform arthrotomy---a process that may induce stiffness, proprioceptive disorder, severe postoperative pain, and scar-related complications---during the operation. 15,32 As ARIF could avoid these drawbacks, it might have advantages in the functional recovery of patients. Tibial plateau fractures are often associated with intra-articular lesions such as chondral damage, meniscal tear, and ligament rupture. 2,28,35 ARIF allows the surgeon to treat additional intra-articular lesions, 21 which are easy to miss during the operation according to our meta-analysis results (65.6% vs 37.7%). A significant difference in intra-articular lesions between the ARIF and the ORIF group was found. Arthroscopy helped find and manage intra-articular injury during the operation. Finding intra-articular injuries during treatment for tibial plateau fracture is important. If a meniscal tear exists, we could perform a meniscal repair; if chondral damage exists, we could remove cartilage fragments from the articular space; and if anterior cruciate ligament or posterior cruciate ligament injury exists, the patient may need a brace and a second-stage operation. In ORIF, we may not recognize the details of these injuries and thus miss treatment opportunities. Thus, the advantages of ARIF in tibial plateau fracture are not only the minimally invasive damage during, and faster patient recovery after, the operation but also the treatment of additional intra-articular lesions during the operation.
The ARIF technique is used most commonly in the treatment of Schatzker types I to III tibial plateau fractures because complex tibial plateau fractures such as Schatzker types V to VI fracture are difficult to visualize using the arthroscopy monitor. 10 Schatzker types I to III fractures involve the lateral tibial plateau and have been treated traditionally with ORIF via an anterolateral approach. 37 Herbort et al 14 identified complex tibial plateau fracture as a contraindication for ARIF because of the high risk of iatrogenic compartment syndrome secondary to irrigation fluid extravasation. However, Krause et al 20 reported using “open fracturoscopy” compared with fluoroscopy to analyze the anatomic accuracy of fracture reduction in complex tibial plateau fractures (AO/OTA 41-C type fracture) during the operation. This latter study showed that subsequent “fracturoscopy” could find persistent fracture depression (≥2 mm; fracturoscopy group) with the need for intraoperative correction in most cases, meaning that ARIF also could have value in the treatment of complex tibial plateau fracture by the method of open fracturoscopy. Our meta-analysis included a total of 617 patients; of these, only 38 were in the complex tibial fracture category (types IV-VI). Wang et al 41 reported 8 cases of type IV, 12 of type V, and 10 of type VI, and Dall’oca et al 8 reported 8 cases of type IV but used the ARIF technique only in selected cases where a low degree of comminution was present, which could be recognized as a simple fracture. Overall, ARIF is currently used mostly in simple tibial plateau fracture, and there are still difficulties with ARIF use in complex tibial plateau fracture; however, open fracturoscopy may offer a new method of arthroscopy in the treatment of tibial plateau fracture.
The present study has several limitations and potential biases. First, only 6 studies with 617 patients were included; the limited number of studies and small sample size might reduce the precision of the pooled results. Second, there was only 1 RCT, which might reduce the strength of evidence. 11 Most of the reviewed studies were retrospective, so there may be a selection bias, with ARIF being chosen for less comminuted or less displaced fractures. Third, different clinical functional scores were used in these studies; the most commonly used method was the Rasmussen radiological score, and it was only used in 5 studies. 8,11,22,39,41 Other clinical outcomes were only included in 2 to 4 studies. The comparison of these 2 groups needs more consistent measurement methods. Fourth, these studies did not pay much attention to the advantages of ARIF of a minimally invasive operation and fast patient recovery from surgery. Hospital stay was reported in 2 studies, 11,39 and full weightbearing was reported in only 1 study. 27 Finally, the follow-up duration of the included studies was varied, and more clinical studies with long-term follow-up are required.
Conclusion
This meta-analysis demonstrated that the most important value of ARIF might be the faster postoperative recovery and better clinical function for patients, as well as the ability to find and treat additional intra-articular lesions during the operation. There were also fewer complications with the ARIF technique compared with ORIF, although this difference was not statistically significant. Thus, the current literature supports the view that ARIF is a beneficial and safe treatment method in tibial plateau fracture. However, more high-level evidence research should be carried out, and ARIF use in complex tibial plateau fracture should be explored further.
Acknowledgment
The authors thank the Orthopedics Department, 2nd Affiliated Hospital, Zhejiang University School of Medicine, for help with this study.
Footnotes
Final revision submitted February 21, 2021; accepted March 2, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References:
- 1. Benea H, Tomoaia G, Martin A, Bardas C. Arthroscopic management of proximal tibial fractures: technical note and case series presentation. Clujul Med. 2015;88(2):233–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Burdin G. Arthroscopic management of tibial plateau fractures: surgical technique. Orthop Traumatol Surg Res. 2013;99(1)(suppl):S208–S218. [DOI] [PubMed] [Google Scholar]
- 3. Caspari RB, Hutton PM, Whipple TL, Meyers JF. The role of arthroscopy in the management of tibial plateau fractures. Arthroscopy. 1985;1:76–82. [DOI] [PubMed] [Google Scholar]
- 4. Chan YS, Chiu CH, Lo YP, et al. Arthroscopy-assisted surgery for tibial plateau fractures: 2- to 10-year follow-up results. Arthroscopy. 2008;24:760–768. [DOI] [PubMed] [Google Scholar]
- 5. Chan YS, Yuan LJ, Hung SS, et al. Arthroscopic-assisted reduction with bilateral buttress plate fixation of complex tibial plateau fractures. Arthroscopy. 2003;19:974–984. [DOI] [PubMed] [Google Scholar]
- 6. Chen XZ, Liu CG, Chen Y, Wang LQ, Zhu QZ, Lin P. Arthroscopy-assisted surgery for tibial plateau fractures. Arthroscopy. 2015;31:143–153. [DOI] [PubMed] [Google Scholar]
- 7. Chiu CH, Cheng CY, Tsai MC, et al. Arthroscopy-assisted reduction of posteromedial tibial plateau fractures with buttress plate and cannulated screw construct. Arthroscopy. 2013;29:1346–1354. [DOI] [PubMed] [Google Scholar]
- 8. Dall’oca C, Maluta T, Lavini F, Bondi M, Micheloni GM, Bartolozzi P. Tibial plateau fractures: compared outcomes between ARIF and ORIF. Strategies Trauma Limb Reconstr. 2012;7(3):163–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Duan XJ, Yang L, Guo L, Chen GX, Dai G. Arthroscopically assisted treatment for Schatzker type I-IV tibial plateau fractures. Chin J Traumatol. 2008;11:288–292. [DOI] [PubMed] [Google Scholar]
- 10. Egol KA, Cantlon M, Fisher N, Broder K, Reisgo A. Percutaneous repair of a Schatzker III tibial plateau fracture assisted by arthroscopy. J Orthop Trauma. 2017;31(suppl 3):S12–S13. [DOI] [PubMed] [Google Scholar]
- 11. Elabjer E, Benčić I, Ćuti T, Cerovečki T, Ćurić S, Vidović D. Tibial plateau fracture management: arthroscopically-assisted versus ORIF procedure---clinical and radiological comparison. Injury. 2017;48(suppl 5):S61–S64. [DOI] [PubMed] [Google Scholar]
- 12. Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 1999;13:401–406. [DOI] [PubMed] [Google Scholar]
- 13. Frattini M, Vaienti E, Soncini G, Pogliacomi F. Tibial plateau fractures in elderly patients. Chir Organi Mov. 2009;93:109–114. [DOI] [PubMed] [Google Scholar]
- 14. Herbort M, Domnick C, Petersen W. Arthroscopic treatment of tibial plateau fractures. Oper Orthop Traumatol. 2014;26:573–588. [DOI] [PubMed] [Google Scholar]
- 15. Hung SS, Chao EK, Chan YS, et al. Arthroscopically assisted osteosynthesis for tibial plateau fractures. J Trauma. 2003;54:356–363. [DOI] [PubMed] [Google Scholar]
- 16. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 17. Jennings J. Arthroscopic management of tibial plateau fractures. Arthroscopy. 1985;1:160–168. [DOI] [PubMed] [Google Scholar]
- 18. Jiang L, Zheng Q, Pan Z. Comparison of extended anterolateral approach in treatment of simple/complex tibial plateau fracture with posterolateral tibial plateau fracture. J Orthop Surg Res. 2018;13(1):303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kayali C, Oztürk H, Altay T, Reisoglu A, Agus H. Arthroscopically assisted percutaneous osteosynthesis of lateral tibial plateau fractures. Can J Surg. 2008;51:378–382. [PMC free article] [PubMed] [Google Scholar]
- 20. Krause M, Preiss A, Meenen NM, Madert J, Frosch KH. “Fracturoscopy” is superior to fluoroscopy in the articular reconstruction of complex tibial plateau fractures—an arthroscopy assisted fracture reduction technique. J Orthop Trauma. 2016;30(8):437–444. [DOI] [PubMed] [Google Scholar]
- 21. Kumar A, Whittle AP. Treatment of complex (Schatzker type VI) fractures of the tibial plateau with circular wire external fixation: retrospective case review. J Orthop Trauma. 2000;14:339–344. [DOI] [PubMed] [Google Scholar]
- 22. Le Baron M, Cermolacce M, Flecher X, Guillotin C, Bauer T, Ehlinger M. SoFCOT. Tibial plateau fracture management: ARIF versus ORIF---clinical and radiological comparison. Orthop Traumatol Surg Res. 2019;105(1):101–106. [DOI] [PubMed] [Google Scholar]
- 23. Levy BA, Herrera DA, MacDonald P, Cole PA. The medial approach for arthroscopic-assisted fixation of lateral tibial plateau fractures: patient selection and mid- to long-term results. J Orthop Trauma. 2008;22:201–205. [DOI] [PubMed] [Google Scholar]
- 24. Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010;24(11):683–692. [DOI] [PubMed] [Google Scholar]
- 26. Moher D, Liberati A, Tetzlaff J, Altman DG; the PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. [DOI] [PubMed] [Google Scholar]
- 27. Ohdera T, Tokunaga M, Hiroshima S, Yoshimoto E, Tokunaga J, Kobayashi A. Arthroscopic management of tibial plateau fractures---comparison with open reduction method. Arch Orthop Trauma Surg. 2003;123(9):489–493. [DOI] [PubMed] [Google Scholar]
- 28. Prat-Fabregat S, Camacho-Carrasco P. Treatment strategy for tibial plateau fractures: an update. EFORT Open Rev. 2016;1:225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ranawat CS, Insall J, Shine J. Duo-condylar knee arthroplasty: hospital for special surgery design. Clin Orthop Relat Res. 1976;120:76–82. [PubMed] [Google Scholar]
- 30. Rasmussen PS. Tibial condylar fractures: impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am. 1973;55:1331–1350. [PubMed] [Google Scholar]
- 31. Rossi R, Bonasia DE, Blonna D, Assom M, Castoldi F. Prospective follow-up of a simple arthroscopic-assisted technique for lateral tibial plateau fractures: results at 5 years. Knee. 2008;15:378–383. [DOI] [PubMed] [Google Scholar]
- 32. Ruiz-Ibán MÁ, Diaz-Heredia J, Elías-Martín E, Moros-Marco S, Martinez Del Val L. Repair of meniscal tears associated with tibial plateau fractures: a review of 15 cases. Am J Sports Med. 2012;40:2289–2295. [DOI] [PubMed] [Google Scholar]
- 33. Schatzker J, McBroom R, Bruce D. The tibial plateau fracture: the Toronto experience 1968–1975. Clin Orthop Relat Res. 1979;138:94–104. [PubMed] [Google Scholar]
- 34. Siegler J, Galissier B, Marcheix PS, Charissoux JL, Mabit C, Arnaud JP. Percutaneous fixation of tibial plateau fractures under arthroscopy: a medium term perspective. Orthop Traumatol Surg Res. 2011;97:44–50. [DOI] [PubMed] [Google Scholar]
- 35. Stahl D, Serrano-Riera R, Collin K, Griffing R, Defenbaugh B, Sagi HC. Operatively treated meniscal tears associated with tibial plateau fractures: a report on 661 patients. J Orthop Trauma. 2015;29:322–324. [DOI] [PubMed] [Google Scholar]
- 36. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 37. Van Dreumel RLM, Van Wunnik BPW, Janssen L, Simons PCG, Janzing HMJ. Mid-to long-term functional outcome after open reduction and internal fixation of tibial plateau fractures. Injury. 2015;46:1608–1612. [DOI] [PubMed] [Google Scholar]
- 38. van Glabbeek F, van Riet R, Jansen N, D’Anvers J, Nuyts R. Arthroscopically assisted reduction and internal fixation of tibial plateau fractures: report of twenty cases. Acta Orthop Belg. 2002;68:258–264. [PubMed] [Google Scholar]
- 39. Verona M, Marongiu G, Cardoni G, Piras N, Frigau L, Capone A. Arthroscopically assisted reduction and internal fixation (ARIF) versus open reduction and internal fixation (ORIF) for lateral tibial plateau fractures: a comparative retrospective study. J Orthop Surg Res. 2019;14:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wang Y, Wang J, Tang J, Zhou F, Yang L, Wu J. Arthroscopy assisted reduction percutaneous internal fixation versus open reduction internal fixation for low energy tibia plateau fractures. Sci Rep. 2018;8:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wang Z, Tang Z, Liu C, Liu J, Xu Y. Comparison of outcome of ARIF and ORIF in the treatment of tibial plateau fractures. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):578–583. [DOI] [PubMed] [Google Scholar]
- 42. Xie X, Zhan Y, Wang Y, Lucas JF, Zhang Y, Luo C. Comparative analysis of mechanism-associated 3-dimensional tibial plateau fracture patterns. J Bone Joint Surg Am. 2020;102(5):410–418. [DOI] [PubMed] [Google Scholar]