Abstract
To combat the spread of coronavirus disease 2019 (COVID-19), significant measures were enacted including school and business closures, social distancing, and facial coverings. We hypothesized that this would have an impact on all respiratory infections in children. Using nasopharyngeal panel test results of children in the emergency department, we evaluated cross-sectional data from February to May in both 2019 and 2020. Respiratory panel testing included 11 common respiratory viruses and bacteria. After the restrictions were enacted, we observed a large drop in the number and percentage positive of all common respiratory viral infections in 2020 compared with the same time in 2019. When analyzing data from children <2 years old, a similar decrease was seen. Restrictions enacted to prevent the spread of COVID-19 were associated with a significant decrease in respiratory viral infections in children of all ages. This association could guide future public health recommendations and guidelines.
Keywords: respiratory infections, COVID-19 restrictions, pandemic, viral testing
Introduction
As coronavirus disease 2019 (COVID-19) began to spread rapidly throughout the world, extreme efforts were made to slow the spread of the pandemic. This led to the introduction of public health mandates including social distancing, masking, hand washing, school closures, cancellation of mass events, and overall reduction of population movement. Studies from the beginning of the pandemic and from past respiratory epidemics have shown that distancing and facial coverings are associated with a decrease in the prevalence of respiratory illnesses including influenza, respiratory syncytial virus (RSV), parainfluenza, and adenovirus.1-8 Studies of pediatric emergency department visits in the United Kingdom and Singapore showed that during lockdown, respiratory illnesses and breathing problems decreased significantly.9-11 No studies have yet looked at the impact of COVID-19 restrictions on the incidence of all common respiratory infections in children. In the counties surrounding our hospital in California in the United States, restrictions were enacted beginning the second week of March of 2020. We theorized that these measures would lead to a drop in some if not all respiratory infections. With the increased use of multiplex nucleic acid amplification swabs, we were able to perform this study evaluating the effect of COVID-19 restrictions on all common respiratory infections in our population.
Materials and Methods
We performed a retrospective study of all nasopharyngeal respiratory panel results from patients <18 years of age in the pediatric emergency department between February 1 to May 31, 2019, and February 1 to May 31, 2020. The respiratory panel used is a nucleic acid amplification test that detects multiple pathogens in a single test. It includes the following respiratory infections: adenovirus, coronaviruses HKU1, NL63, 229E, OC43, metapneumovirus, rhinovirus or enterovirus, influenza A and B, parainfluenza virus types 1-4, RSV, Bordetella pertussis, Bordetella parapertussis, Chlamydophila pneumoniae, and Mycoplasma pneumoniae. In our department, the test is performed on all patients admitted to the hospital for respiratory complaints. For patients who are discharged home, the test is performed at the discretion of the provider. We analyzed the data by weeks, with February 1 to 7 representing week 1, with a total of 17 weeks of data in both 2019 and 2020. This study was approved by our institutional review board.
Results
A total of 1321 respiratory panels (22 457 individual tests) were ordered between February 1 and March 31 in 2019 versus 930 panels (15 810 individual tests) ordered during the same weeks in 2020. There were 931 positive tests in 2019 versus 599 positive tests in 2020.
The number of positive tests in February and early March of 2020 mirrored or exceeded those in the same weeks of 2019. However, from late March onward, after the state restrictions were placed, the number of positive tests in 2020 were lower than in 2019 (Figure 1). The percentage of positive tests also decreased significantly after the middle of March in 2020 (Figure 2).
Figure 1.
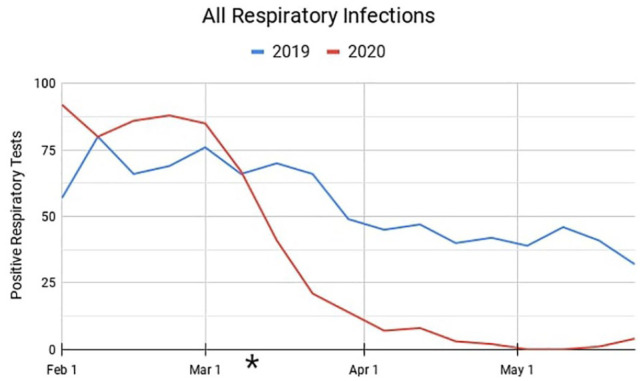
The number of respiratory infections by week in 2019 compared with 2020. The asterisk denotes the time when coronavirus disease 2019 restrictions were begun.
Figure 2.
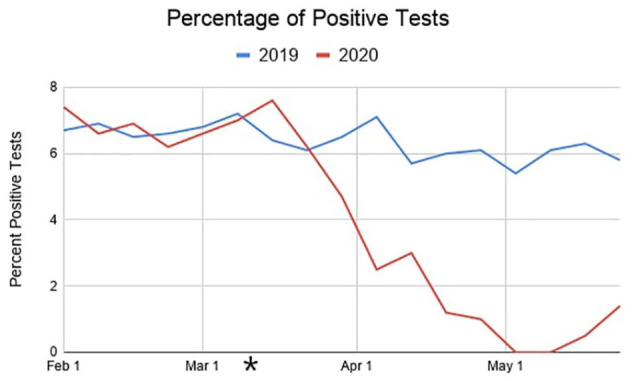
The percentage of positive tests by week in 2019 compared with 2020. The asterisk denotes the time when coronavirus disease 2019 restrictions were begun.
The number of bacterial infections (Bordetella pertussis, Bordetella parapertussis, Chlamydophila pneumoniae, and Mycoplasma pneumoniae) was low during both years with a total of 12 infections in 2019 and 10 infections in 2020 during the study period.
When analyzing patients <2 years of age only, we observed a decrease in positive tests after the middle of March in 2020 compared with the same time in 2019 (Figure 3). The percentage of positive tests also decreased in this age group in 2020 compared with 2019 (Figure 4).
Figure 3.
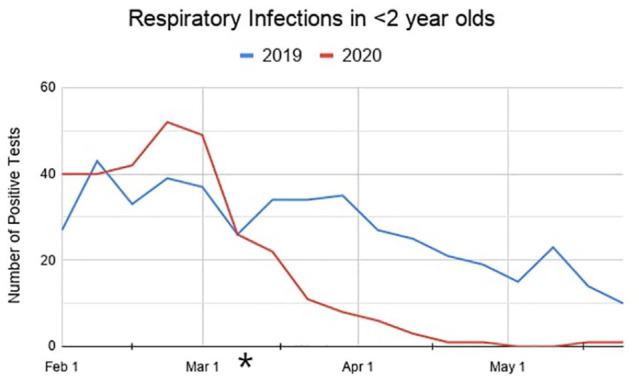
The number of respiratory infections in <2 year olds by week in 2019 compared with 2020. The asterisk denotes the time when coronavirus disease 2019 restrictions were begun.
Figure 4.
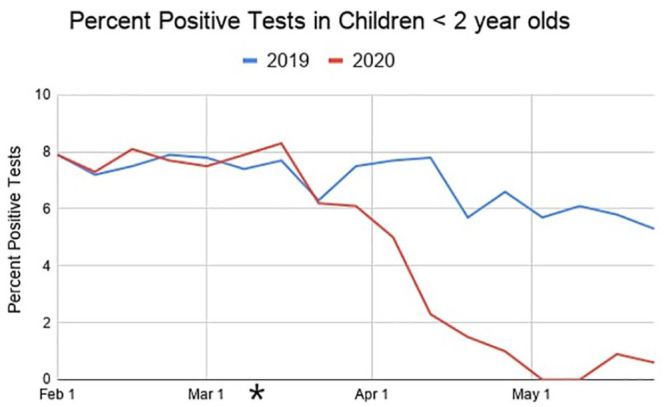
The percentage of positive tests in <2 year olds by week in 2019 compared with 2020. The asterisk denotes the time when coronavirus disease 2019 restrictions were begun.
Comparison of weekly positive tests for adenovirus, non-COVID-19 coronaviruses, metapneumovirus, rhinovirus and enterovirus, influenza A and B, parainfluenza viruses, and RSV all showed decreases in 2020 after the COVID-19 restrictions were begun, compared with 2019 (online Supplementary File).
Discussion
This study shows the association between the COVID-19 restrictions and a significant drop in all respiratory viral infections in children. With the concern that this finding could have been related to fewer tests being ordered, we also performed an analysis of the percentage of positive tests, which showed a similar decrease. We conclude that the findings are a significant change, likely the product of some or all the pandemic measures and less likely a result of yearly seasonal variation or decreased visits after lockdown. The same findings were also seen in the youngest children. Since it is less common for this age group to wear facial coverings, the observed drop in infections may be explained by social distancing alone versus the overall measures taken by older children and adults around them.
This information can influence public health measures in future pandemics, with early action potentially mitigating the impact of a global health crisis. These measures would be especially important in countries with limited resources where tenuous medical systems can be easily overwhelmed, and where there is more limited access to treatments and vaccines. Further studies are needed to decide which actions are most effective in stopping infectious spread: hand washing, facial coverings, social distancing, or school and business closures.
The information from this article can make significant impacts even during nonpandemic periods. Upper respiratory infections (URIs) have a significant negative economic impact, accounting for millions of missed work and school days due to illness.12,13 RSV alone results yearly in 58 000 hospitalizations, 500 000 emergency department visits, and 2.1 million outpatient clinic visits in the United States.14 URIs are also a significant cause of asthma exacerbations worldwide with asthma peaking yearly according to predictable patterns depending on the climate.15,16 The annual cost of asthma care in the United States is estimated at >$81 billion.17 Changes to normal behavior such as enhanced handwashing, facial coverings in public spaces, and social distancing during the highest respiratory infectious seasons could significantly decrease the negative effects of frequent URIs and associated illnesses.
One question that remains unanswered is how this decrease in infections may influence the next few years. There is concern that with restrictions being eased, along with less infectious exposure this year with resulting lower population immunity, the following seasons may show a vulnerability to severe infections.8
A limitation to this study is that respiratory panel testing is not performed on every patient with respiratory or infectious symptoms in our emergency department. This study may represent patients that overall are sicker who may have different infection patterns than patients who did not receive testing. It is also possible that once restrictions were in place, physicians might have been motivated to order more respiratory testing than usual to find non-COVID-19 explanations for respiratory symptoms. This could have affected the percentage of positive respiratory testing; however, we feel that any effect was likely small.
Another limitation is that the numbers of bacterial infections were too low in both 2019 and 2020 to measure a difference. Further dedicated studies are needed to define the effect restrictions have on bacterial pneumonia.
Conclusion
Restrictions enacted to prevent the spread of COVID-19 were associated with a significant decrease in respiratory viral infections in children of all ages. These findings should influence public health measures in future pandemics. Seasonal measures could also make a significant impact on the negative effects of respiratory infections during nonpandemic times. Further studies are needed to determine which measures make the most impact.
Author Contributions
MMR analyzed the data, edited and wrote the manuscript, and formatted the figures.
FDH assisted with editing and writing the manuscript.
JRN assisted with formatting the figures.
BGC assisted with editing the manuscript.
MC assisted with editing the manuscript.
LAB: supervised the project and edited the manuscript.
Supplemental Material
Supplemental material, sj-pdf-1-cpj-10.1177_00099228211044842 for COVID-19 Restrictions Are Associated With a Significant Decrease of All Common Respiratory Viral Illnesses in Children by Melanie M. Randall, Fairuz Despujos Harfouche, Jennifer Raae-Nielsen, Brian G. Chen, Miryah Chen and Lance A. Brown in Clinical Pediatrics
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Melanie M. Randall  https://orcid.org/0000-0002-8432-7689
https://orcid.org/0000-0002-8432-7689
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Britton PN, Hu N, Saravanos G, et al. COVID-19 public health measures and respiratory syncytial virus. Lancet Child Adolesc Health. 2020;4:e42-e43. doi: 10.1016/S2352-4642(20)30307-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cauchemez S, Valleron AJ, Boëlle PY, Flahault A, Ferguson NM.Estimating the impact of school closure on influenza transmission from Sentinel data. Nature. 2008;452:750-754. doi: 10.1038/nature06732 [DOI] [PubMed] [Google Scholar]
- 3.Cowling BJ, Ali ST, Ng TWY, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5:e279-e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang QS, Wood T, Jelley L, et al. Impact of the COVID-19 nonpharmaceutical interventions on influenza and other respiratory viral infections in New Zealand. Nat Commun. 2021;12:1001. doi: 10.1038/s41467-021-21157-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuo SC, Shih SM, Chien LH, Hsiung CA.Collateral benefit of COVID-19 control measures on influenza activity, Taiwan. Emerg Infect Dis. 2020;26:1928-1930. doi: 10.3201/eid2608.201192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olsen SJ, Azziz-Baumgartner E, Budd AP, et al. Decreased influenza activity during the COVID-19 pandemic—United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1305-1309. doi: 10.15585/mmwr.mm6937a6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soo RJJ, Chiew CJ, Ma S, Pung R, Lee V. Decreased influenza incidence under COVID-19 control measures, Singapore. Emerg Infect Dis. 2020;26:1933-1935. doi: 10.3201/eid2608.201229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yeoh DK, Foley DA, Minney-Smith CA, et al. The impact of COVID-19 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis. 2021;72:2199-2202f. doi: 10.1093/cid/ciaa1475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chong SL, Soo JSL, Allen JC, Jr, et al. Impact of COVID-19 on pediatric emergencies and hospitalizations in Singapore. BMC Pediatr. 2020;20:562. doi: 10.1186/s12887-020-02469-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDonnell T, Nicholson E, Conlon C, et al. Assessing the impact of COVID-19 public health stages on paediatric emergency attendance. Int J Environ Res Public Health. 2020;17:6719. doi: 10.3390/ijerph17186719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shanmugavadivel D, Liu JF, Gilhooley C, Elsaadany L, Wood D.Changing patterns of emergency paediatric presentations during the first wave of COVID-19: learning for the second wave from a UK tertiary emergency department. BMJ Paediatr Open. 2021;5:e000967. doi: 10.1136/bmjpo-2020-000967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fendrick AM, Monto AS, Nightengale B, Sarnes M.The economic burden of non-influenza-related viral respiratory tract infection in the United States. Arch Intern Med. 2003;163:487-494. doi: 10.1001/archinte.163.4.487 [DOI] [PubMed] [Google Scholar]
- 13.Bramley TJ, Lerner D, Sames M.Productivity losses related to the common cold. J Occup Environ Med. 2002;44:822-829. doi: 10.1097/00043764-200209000-00004 [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Respiratory syncytial virus infection (RSV): trends and surveillance. Accessed March, 2020. https://www.cdc.gov/rsv/research/us-surveillance.html
- 15.Busse WW, Lemanske RF, Jr, Gern JE.Role of viral respiratory infections in asthma and asthma exacerbations. Lancet. 2010;376:826-834. doi: 10.1016/S0140-6736(10)61380-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wisniewski JA, McLaughlin AP, Stenger PJ, et al. A comparison of seasonal trends in asthma exacerbations among children from geographic regions with different climates. Allergy Asthma Proc. 2016;37:475-481. doi: 10.2500/aap.2016.37.3994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nurmagambetov T, Kuwahara R, Garbe P.The economic burden of asthma in the United States, 2008-2013. Ann Am Thorac Soc. 2018;15:348-356. doi: 10.1513/AnnalsATS.201703-259OC [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-cpj-10.1177_00099228211044842 for COVID-19 Restrictions Are Associated With a Significant Decrease of All Common Respiratory Viral Illnesses in Children by Melanie M. Randall, Fairuz Despujos Harfouche, Jennifer Raae-Nielsen, Brian G. Chen, Miryah Chen and Lance A. Brown in Clinical Pediatrics


