Abstract
The transformation that COVID-19 has brought upon the world is unparalleled. The impact on mental health is equally unprecedented and yet unexplored in depth. An online-based survey was administered to 413 community-based adults during COVID-19 confinement to explore psychological impact and identify high risk profiles. Young females concerned about the future, expressing high COVID-related distress, already following psychological therapy and suffering from pre-existing chronic conditions, were those at highest risk of psychological impact due to the COVID-19 situation. Findings could be employed to design tailored psychological interventions in the early stages of the outbreak to avoid the onset/exacerbation of psychopathology.
Keywords: COVID-19, cross-sectional survey, non-pharmaceutical interventions, online survey, pandemic, population mental health, psychological impact, quarantine
Introduction
The world has faced a global threat in the last months from the Coronavirus disease 2019 (COVID-19) caused by the SARS-CoV-2, emerging into a pandemic with generalized health and socio-economic consequences. The transformation that this pandemic has brought upon the society is unparalleled, and the impact on mental health is equally unprecedented and therefore, unexplored. With huge contagion capacity, COVID-19 mortality around the world is up to 4% (lower than previous SARS, but not trivial), and directly related to age and immune-compromised states (Standl et al., 2020). Precisely, this extremely high infection rate and the relatively high mortality, causes the population to begin to worry about the COVID-19.
In the early stages of an infectious disease outbreak such as COVID-19, there is frequent uncertainty about the nature of the disease, its spread, scope, and potential impact. Indeed, fear and worry of contacting individuals who are possibly infected by COVID-19 has been reported as a common response pattern to the still developing COVID-19 crisis (Lin, 2020; Zysberg & Zisberg, 2020). Fear is directly associated with its transmission rate and medium (rapidly and invisibly), as well as its morbidity and mortality. This further leads to other psychosocial challenges including stigmatization and discrimination (Islam et al., 2020). Additionally, with high levels of fear, individuals may not think clearly and rationally when reacting to COVID-19 (Perini, 2012). Taken together, these factors (fear and COVID-related concerns) could contribute substantially to an individual profile that experiences greater psychological impact.
Due to the still lacking effective therapeutic remedies or vaccines guaranteeing protection to COVID negative consequences, the WHO Joint Mission on Coronavirus Disease 2019 has called for a worldwide response to draw on China’s extensive experience of non-pharmaceutical interventions (NPIs) aim to modify behavior to reduce the spread of infectious diseases (Brooks et al., 2020). In this sense, initially lockdown (social isolation or confinement) and quarantine have been one of the main measures to stop the spread of infection and related death toll. As happened in Wuhan, China, its role has been crucial in heavily affected countries like Spain or Italy (Ni et al., 2020; Rodríguez-Rey et al., 2020). Quarantine differs from lockdown since it entails the separation and restriction of movement of people who have potentially been exposed to a contagious disease to ascertain if they become unwell, so reducing the risk of them infecting others. COVID-19 social restriction measures efforts have ranged from the mass quarantine of entire cities, confinement in government-run facilities, to self-isolation at home. There are precedents for such measures. In 2003, citywide quarantines were also imposed in areas of China and Canada during the outbreak of Severe Acute Respiratory Syndrome (SARS), whereas entire villages in many West African countries were quarantined during the 2014 Ebola outbreak.
While all these non-pharmacological interventions (NPIs) can broadly serve the public good, they might cause significant disruption globally, and have been directly associated with psychological challenges for those isolated, their loved ones and the healthcare workers caring for them (Ni et al., 2020; Rodríguez-Rey et al., 2020). Besides, common psychological and behavioral responses from general population in front of health crises include several distress reactions (insomnia, anxiety, decreased perception of safety, anger, scapegoating, and increased recurrence to healthcare centers due to fears of illness), and health risk behaviors (i.e. increased use of alcohol, tobacco and/or drugs, altered work/life balance, increased family/social conflictivity); (Wang et al., 2020b). Moreover, imposed social distancing may cause or critically exacerbate existing loneliness and feeling alone is an independent risk factor for mood disorders and eventually, suicide (Hwang et al., 2020).
Despite the World Health Organization and other public health authorities’ actions to contain the COVID-19 outbreak, at this time of crisis, one of the highest tolls paid is at a psychosocial level, testing the resilience and adaptive resources of the population (World Health Organization [WHO], 2020). Therefore, to support mental and to favor psychosocial well-being in different target groups during this crisis seems mandatory. We must consider also as a special group of interest vulnerable populations, which include the economically disadvantaged or low-income individuals, racial and ethnic minorities, the elderly, the children, the homeless, those with human immunodeficiency virus (HIV), and those with other chronic health conditions, including severe mental illness. Each of them might endure different and additional psychological impacts depending on their characteristics and specific circumstances (Lurie, 1993; Wang et al., 2020a; Wu, 2020). The long-term psychosocial consequences are the key challenge for our healthcare system, where the importance of mental health prevention is not sufficiently recognized. Besides, it is worth noting that most mental health services were not active any longer in the midst of the outbreak (Marazziti et al., 2020)
Previous research, mostly based on SARS, Ebola and the H1N1 influenza found mixed evidence concerning whether demographics and population’s general health status are predictors of the psychological impact of quarantine (Brooks et al., 2020). However, several main stressors directly related to higher maladjustment and psychological impact have been outlined and appear related to COVID psychological impact. These include socio-economic inequities conducting to lower access to supplies or reliable information, and caring for a frail loved one or being oneself in a high risk health situation (Brooks et al., 2020). Similarly, recent surveys from the Census Bureau, the Centers for Disease Control and Prevention, and preliminary data from cross-sectional studies assessing COVID-19 psychological impact have pointed out that COVID crisis has been reported to be associated with rapid rises in psychological distress across many nations with female gender, the young, the less educated, those having lost their job during the health crisis, and those presenting physical and psychological comorbidities, reporting greater mental health strain (Resnick, 2020; Rodríguez-Rey et al., 2020).
To the best of our knowledge, there is an urgent need to deepen our understanding on the psychological impact of the general population living in Spain during the COVID-19 pandemic. This novel information will serve as a first ground to develop psychological interventions, so that the possible short and mid-long term and possible lasting psychological negative consequences of the pandemic can be diminished or reverted. Considering all this, this research has two main aims: (1) To explore and describe the mental health status and psychological impact of the general adult population in Spain during the COVID-19 confinement, and (2) to examine the existence of a possible high risk profile of psychological distress considering: demographics (age, gender), degree and type of concerns about the current COVID-19 pandemic, COVID-19 specific health data (i.e. close contact or suspicion of contact with the COVID-19 disease, death of loved ones by COVID-19, diagnosis and/or hospital admission by COVID-19), self-perceived health status, and other environmental conditions during the home confinement (i.e. number of cohabitants, taking care of vulnerable population).
Methods
Design
This study follows a cross-sectional population survey design, with a descriptive-correlational approach.
Participants
A sample of community-based adults were recruited for the study. Inclusion criteria required being ⩾18 years old. Exclusion criteria were not understanding Spanish well enough to complete the questionnaire. These criteria were stated in the informed consent presented before the survey.
A total of 413 adults from different Spanish provinces (Barcelona 82.57%, n = 341) filled the survey. Socio-demographic characteristics are comprehensively presented in Table 1. Most respondents were women (70.05%), young adults (age M = 37.62 years, SD = 13.96; range 18–73), with 9.2% (38/413) being older than 60 years old, married or cohabiting with a partner (54.70%) and children (35.80%) or with parents (mother: 34.10%, father: 25.40%). The majority of the sample lived in the region of Catalonia with just a few cases being abroad (0.73%, n = 3) at the moment of the study.
Table 1.
Participants’ demographics (N = 413).
| Variables | n (%) |
|---|---|
| Gender | |
| Male | 121 (29.30%) |
| Female | 291 (70.50%) |
| Prefer not to label | 1 (0.20%) |
| Country of origin | |
| Spain | 410 (99.27%) |
| Other | 3 (0.73%) |
| Cohabiting | |
| Yes | 386 (93.46%) |
| No | 27 (6.54%) |
| Age | |
| 18–35 | 192 (46.49%) |
| 36–59 | 183 (44.31%) |
| >60 | 38 (9.20%) |
| Occupation | |
| Healthcare professionals | 98 (23.73%) |
| Non-healthcare professionals | 315 (76.27%) |
Data collection
Between 14th May and 2nd of June 2020 -in a context of strict general population lockdown that started on 16th March-, a brief snowball survey entitled: “How am I coping with the situation that COVID-19 has generated?” was distributed via mailing lists and social media (Whatsapp). Participants were encouraged to distribute the survey. We selected an online survey as the lockdown and enrollment of participants precluded in-person surveys and random selection. We deployed an ad hoc multifactorial 34-item questionnaire using the Kwik surveys platform. A brief advertisement explaining the research objectives, usefulness of results and outlining main ethical and privacy details accompanied the survey link in both different distribution channels. The survey was available only in Spanish, as we aimed to reach as many respondents as possible in our country. We made the length of the survey short enough to not take more than 5 minutes to ensure a high completion rate. To compensate for the brevity of the survey, we included 4 open-answer boxes to specify some responses and 1 open-answer question asking respondents to offer more details concerning the topic assessed.
Sample size calculation was based on a margin of error and confidence level rather than prevalence or expected effect sizes. With a 5% margin of error and a confidence level of 95%, a minimum sample size of 384 was estimated to be sufficient to reveal differences in an average response to each survey question.
Outcomes and covariables
Based on previous research and the unavailability of a reliable and validated questionnaire to explore COVID-19 related psychosocial impact and distress, an ad hoc 34-item online survey was designed.
Participants provided information regarding their gender, age, residency, marital status, number of children, number of people living together and dependent cohabitants during the home confinement.
COVID-related distress and degree of concern was asked by means of a numeric scale ranging from 0 to 10 (not all distressed/concerned, to very distressed/concerned). Main worries were also collected by multiple choice and one open question to specify in case of not finding relevant categories to express their main worries related to COVID-19. Psychological symptoms were also screened in a multiple choice item collecting aspects such as anxiety, stress, depressive symptoms, panic attacks, fatigue, anhedonia, loss of interest in social contact, disturbances in eating or sleep patterns, irritability, intense fear, frequent and invasive concerns, general discomfort or other psychological symptoms.
Respondents were asked to declare if they have received psychological support during the confinement and, in affirmative cases, if it was due to COVID-19 situation, due to pre-existing psychological problems, or both. They were also asked to state if they believe they would need psychological support in a near future due to the experience (main outcome variable).
COVID-related data were also collected. Participants indicated whether they have been diagnosed of COVID-19, type of diagnostic test (rapid strep test, CRP or swab, if applicable), need for hospital admission (including ICU) and symptoms consistent with a diagnosis of COVID (fever, cough, sore throat, headaches, muscle or joint pain, dizziness, diarrhea, rhinitis, chills and respiratory distress) that they have experienced in the last two weeks. Participants were also asked about the degree to which they considered they could have been infected by COVID without knowing, or in close contact with people infected by COVID, if they have experienced the loss of a loved one due to COVID-19, and the degree of confidence in healthcare professionals to both, diagnosed COVID by just clinical criteria (history of symptoms) and by means of objective testing.
General self-perceived health status (based on item 1 from SF122: very good, good, regular, bad, very bad) and history of relevant health conditions were collected too.
Finally, an open question was offered to add any other relevant aspects they consider not being included or requested in the survey.
Ethics
Research ethics procedures of this study complied with European and national legislation (e.g. the Charter of Fundamental Rights of the EU, Directive 95/46/EC of the European Parliament and of the Council of 24 October 1995 on the protection of individuals with regard to the processing of personal data and on the free movement of such data). All data was collected and kept with all guarantees of confidentiality and codification procedures were employed to ensure the privacy and confidentiality of information. All participants were informed about study purposes and direct informed consent was requested to all respondents before sending their responses. Data were kept confidential and were not disclosed unless for study purposes.
Statistical analysis
Descriptive statistics were calculated for all baseline and final outcome variables using measures of central tendency (mean, standard deviation, range for continuous variables; frequencies and total percentages for categorical variables). For bivariate analysis, Kolmogorov-Smirnov test was used to determine whether parametric or non-parametric tests were indicated. Bivariate comparisons were performed through either t Student test and ANOVA for variables with more than two categories or levels, the Mann-Whitney U test for continuous variables or Chi-square test (and Fisher’s exact test when n < 5) for dichotomous variables. The correlation of two variables was compared using Pearson correlation. To analyze the predictors of psychological impact as the main outcome variable, contingency tables were performed with the Chi-Square test. Subsequently, a binary logistic regression analysis (forward stepwise conditional method) was performed with those variables that exhibited a statistically significant relationship with the main variable (need for psychological support in the future; yes vs. no), giving results as adjusted odds ratios (Exp (B)). This main outcome variable to describe the psychological burden of the COVID-19 pandemic and to determine high risk profiles, was measured using scores on item 29 of the survey, aimed at assessing need for psychological support in a near future due to COVID-19 health crises. The level of statistical significance was 5% (p ⩽ 0.05). In all cases, appropriate post hoc analyses were performed, and 95% confidence intervals were reported. All statistical analyses were performed using the SPSS version 25 (IBM Corp.).
Data sharing statement
The current article includes the complete raw data-set collected in the study including the participants’ data set, syntax file, and log files for analysis. Pending acceptance for publication, all of the data files will be automatically uploaded to the Figshare repository.
Results
The psychological and physical impact of COVID-19
Concerns and psychological symptoms
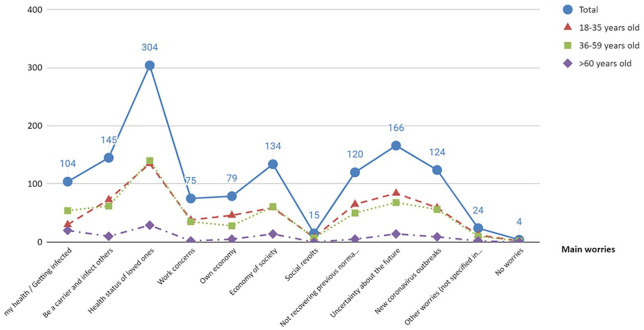
During confinement, most people reported concerns about different aspects (average worries per person = 3.12, SD = 1.05, range 0–9, >5 concerns n = 16). Main worries for different age groups are displayed in Figure 1. Table 2 shows main concerns according to each gender.
Figure 1.
Main worries in different age groups.
Table 2.
Worries expressed by each gender.
| Main worries (affirmative responses are presented) | Times reported (n = 413) | Women n = 291 | Men n = 121 | ||
|---|---|---|---|---|---|
| n (%)≀ | n (%)≀≀ | n (%)≀≀ | p | ||
| My health / Getting infected | 104 (25.18%) | 69 (23.71%) | 35 (28.93%) | 1.231 | 0.267 |
| Be a carrier and infect others | 145 (35.11%) | 103 (35.40%) | 42 (34.71%) | 0.018 | 0.895 |
| Health status of loved ones | 303 (73.36%) | 215 (73.88%) | 88 (72.73%) | 0.059 | 0.809 |
| Work concerns | 75 (18.16%) | 56 (19.24%) | 19 (15.70%) | 0.720 | 0.396 |
| Own economy | 79 (19.13%) | 55 (18.90%) | 24 (19.83%) | 0.048 | 0.826 |
| Economy of society | 133 (32.20%) | 95 (32.65%) | 38 (31.40%) | 0.060 | 0.806 |
| Social revolts | 15 (3.63%) | 11 (3.78%) | 4 (3.31%) | 0.055 | 1.000 |
| Not recovering previous normality (social & leisure life) | 120 (29.05%) | 90 (30.93%) | 30 (24.79%) | 1.558 | 0.212 |
| Uncertainty about the future | 166 (40.19%) | 127 (43.64%) | 39 (32.23%) | 4.626 | 0.031* |
| New coronavirus outbreaks | 123 (29.78%) | 88 (30.24%) | 35 (28.93%) | 0.071 | 0.791 |
| Other worries (not specified in the list) | 24 (5.81%) | 17 (5.84%) | 7 (5.79%) | 0.001 | 0.982 |
| No worries | 4 (0.97%) | 2 (0.69%) | 2 (1.65%) | 0.892 | 0.584 |
Statistical significant differences between genders according to the Chi squared test.
Number of times (%) reporting this concern on the survey.
Number of times (%) reporting this concern in the gender sub-sample.
For the whole sample, the degree of concern was medium-to-high (M = 7.01, SD = 1.89, range 0–10, 17.19% scoring ⩾9) without significant differences between genders, while the degree of emotional distress was medium (M = 5.61, SD = 2.44, range 0–10, 6.30% scoring ⩾9) with women reporting greatest emotional distress (t(410) = 2.858, p = 0.004, 95%CI [0.234, 1.264]). Older participants were more concerned about their own health when compared to younger adults (t(411) = −5.642, p < 0.001, 95%CI [−11.611, −5.611]). When asking about how much they care about being a carrier of COVID-19 and transmitting the virus to others, mean scores were also medium-to-high (M = 7.81, SD = 2.03, range 0–10, 39.47% scoring ⩾9) independently of gender, but with the oldest being significantly the most concerned about this risk (r = 0.103, p = 0.036).
Almost one third of the sample (23.73%, n = 98) work in healthcare settings. These professionals were significantly more concerned compared to general population about infecting others = 9.31, p = 0.002) and the uncertainty about the future = 3.92, p = 0.048). Similarly, they were very sensitized of the higher odds of being infected (t(146) = −3.315, p = 0.001, 95%CI [−1.467, −0.371]).
In the last 14 days, most referred psychological symptoms were apathy (n = 202, 48.91%), depressed mood (n = 183, 44.31%), fatigue (n = 177, 42.86%), stress (n = 169, 40.92%) and anxiety (n = 165, 39.95%), with women (t(410) = 3.292, p = 0.001, 95%CI [0.403, 1.599]) and the youngest respondents (r = −0.369, p < 0.001), those reporting a greater number of symptoms.
All these psychological symptoms revealed different associations with expressed concerns. First, concerns about one’s health was related to greater general physical discomfort = 4.34, p = 0.037), while concern about being a carrier and infecting others was associated with anxiety = 7.57, p = 0.006). Secondly, a higher degree of concern about one’s own work situation was related to depressed mood = 3.98, p = 0.046) and apathy = 4.51, p = 0.034), while concern about one"s own economy was related to anxiety = 4.65, p = 0.031), little desire to talk or contact friends = 6.71, p = 0.010) and intrusive worries = 9.71, p = 0.002). The latter, also related to those concerned about the economy of society = 6.21, p = 0.013). Finally, being worried about not being able to regain normality was associated with stress = 6.88, p = 0.009), depressed mood = 7.833, p = 0.005) and apathy = 11.01, p = 0.001).
Additionally, the number of psychological symptoms experienced correlated positively with the degree of concern (r = 0.245, p < 0.001), number of expressed concerns (r = 0.216, p < 0.001), emotional distress (r = 0.453, p < 0.001), the specific concern about being a carrier of COVID-19 and transmitting the virus to others (r =0.128, p = 0.009), number of physical symptoms endured during confinement (r = 0.397, p < 0.001), considering relevant to offer support to those affected by COVID-19 (r = 0.184, p < 0.001) and to healthcare professionals (r = 0.145, p = 0.003), and the probability of ask for psychological support in the future (r = 0.425, p < 0.001).
Self-perceived risk and confidence in healthcare system
For the whole sample, self-perceived risk of being infected was medium (M = 5.08, SD = 2.26, range 0–10, 34.87% scoring ⩽4) and self-perceived severity of possible consequences of being infected was also medium-to-low (M = 4.77, SD = 2.47, range 0–10, 42.37% scoring ⩽4). Similarly, only a few individuals believe that, with high probability (scoring 8 in a 0–10 probability scale) they might have been positive for COVID (n = 49, 11.86%). A similar proportion of subjects were doubtful (n = 76, 18.40%) while most of the sample reported that they did not believe they had been infected (n = 238, 57.63%, scoring <5).
A total of 47 individuals (11.38%) confirmed to have maintained close contact with people positive for COVID at less than 2 m, and 35 individuals (8.47%) expressed being suspicious of having maintained close contact with people probably positive for COVID. Those having had direct contact with a person infected with COVID-19 were more prone to consider themselves at risk (t(53.64) = −3.616, p = 0.001, 95%CI [−2.315, −0.663]) or even to have been already infected without knowing (t(63.33) = −3.386, p = 0.001, 95%CI [−2.893, −0.741]). Similarly, those considering that they might have been in contact with a possible COVID-19 positive individual, were also more prone to consider that they might have been infected for the virus (t(411) = −3.442, p = 0.001, 95%CI [−2.694, −0.735]) and will probable ask for psychological support in the future (t(411) = −2.140, p = 0.033, 95%CI [−1.959, −0.083]).
Confidence in healthcare professionals to detect COVID-19 from its symptoms (without using tests) was medium (M = 6.42, SD = 2.42) and negatively associated with the number of psychological symptoms experienced (r = −0.123, p = 0.012). This confidence increased when the diagnosis of the infection was made by using tests (i.e. rapid strep tests, CRP or swab) (M = 8.16, SD = 1.77). Only a few cases (3.60%, n = 15) admitted being tested for COVID with positive results obtaining this diagnosis in older participants (U = 2087.50, p = 0.048), by means of a CRP test (n = 11, 73.33%), a quick test (n = 3, 20%) or a swab (n = 1, 6.67%). Any of the respondents required ICU admission due to COVID-19 during the confinement. However, 20% (n = 3) of the individuals diagnosed of COVID-19 had to be admitted to a hospital ward and 60% (n = 9) were quarantined.
Health status and COVID-related physical symptoms
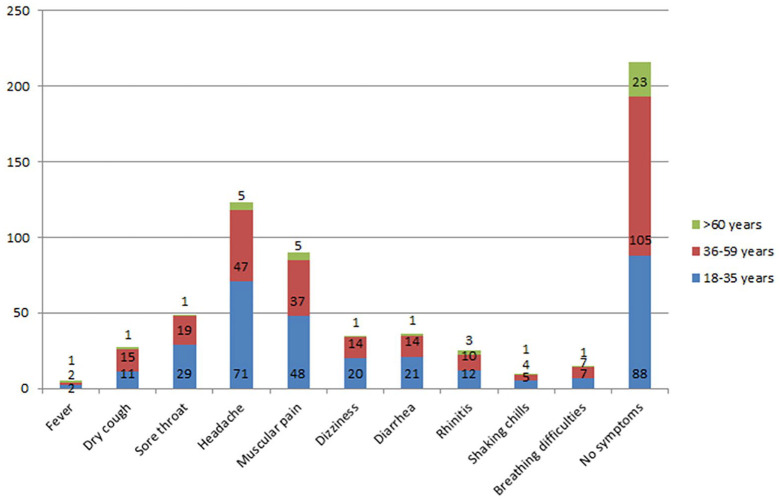
Despite this low prevalence of diagnosed individuals, within the immediate period before the study (two weeks), some of the participants had experienced a wide range of symptoms that have been associated with COVID-19 (see Figure 2). Globally, the most self-reported physical symptoms were headache (n = 123, 29.78%), muscular and joint pain (n = 90, 21.79%) and sore throat (n = 49, 11.86%). It is important to note that half of the sample (52.30%, n = 216) indicated that they had not experienced symptoms within the same time period.
Figure 2.
COVID-19 related symptoms experienced in different age groups.
A sizable proportion of participants (n = 70, 16.95%) affirmed to suffer from chronic conditions being the most prevalent asthma (n = 13), hypertension (n = 9) and allergies (n = 7).
Self-perceived health for the whole sample was “good” (n = 224, 54.24%) with the oldest (t(173.96) = −2.145, p = 0.033, 95%CI [−6.726, −0.279]), those suffering from chronic conditions = 9.809, p = 0.002) and those who received psychological support during the pandemic = 5.415, p = 0.020) reporting worse scores.
Health-care professionals reported better self-perceived health than non-healthcare professionals = 8.13, p = 0.004) and also, reported less number of physical symptoms (t(193.8) = 2.009, p = 0.046, 95%IC [0.011, 1.179]) and some psychological disturbances such as apathy = 6.34, p = 0.011) and changes in appetite = 5.74, p = 0.017).
For the whole sample, general self-perceived health was inversely related to degree of concern (t(411) = 3.186, p = 0.002, 95%CI [0.255, 1.077]), emotional distress (t(411) = 4.553, p < 0.001, 95%CI [0.689, 1.735]), self-perceived severity of COVID-19 in case of being infected (t(411) = 2.931, p = 0.004, 95%CI [0.264, 1.340]), degree of concern about being a carrier of the virus and infecting others (t(411) = 2.512, p = 0.012, 95%CI [0.123, 1.007]), number of psychological symptoms endured in the last 14 days (t(160.2) = 7.268, p < 0.001, 95%CI [1.734, 3.028]), physical symptoms related to COVID-19 (t(124.4) = 6.130, <0.001, 95%CI [0.654, 1.277]) and probability of needing psychological support in the future (t(411) = 4.375, p < 0.001, 95%CI [0.714, 1.879]).
COVID-19 consequences
A little but relevant percentage of the sample (12.59%, n = 52) experienced the loss of a family member or a close contact, which was related to greater degree of concern (t(411) = −2.224, p = 0.027, 95%CI [−1.171, −0.072]), risk of being infected (t(411) = −2.077, p = 0.038, 95%CI [−1.353, −0.037]), self-perceived severity in case of being infected (t(411) = −2.664, p = 0.008, 95%CI [−1.686, −0.254]), degree of concern of being a carrier and transmitting the virus (t(88.87) = −3.461, p = 0.001, 95%CI [−1.202, −0.325]) and older age (t(411) = 3.291, p = 0.001, 95%CI [10.755, 2.711]). Specifically, 31 individuals reported the loss of a relative (n = 6 first degree relative, n = 5 second degree, n = 14 third degree, n = 6 fourth degree) and 24 the loss of acquaintances and friends. Among those reporting the loss of a close one, 30.77% were unsure about the nature of the loss, not relating it directly to COVID.
A small percentage of the studied sample (9.20%, n = 38) revealed having received psychological support during the confinement period and just a minority of them (10.53%, n = 4) affirmed that this was related to the COVID situation. When asking about the importance of providing psychological support to face the health crises caused by COVID, mean score for those affected and their families were high (M = 8.92, SD = 1.43, range 2–10, 66.83% scoring ⩾9) and especially, for healthcare professionals working at front line (M = 9.20, SD = 1.28, range 2–10, 77.48% scoring ⩾9). Women turned out to be the most sensitized to this situation, showing greater importance of offering this type of support for both groups, general (t(175.61) = 3.936, p < 0.001, 95%CI [0.337, 1.014]) and healthcare professionals (t(172.02) = 3.546, p = 0.001, 95%CI [0.246, 0.865]), respectively. Similarly, they were the most likely to express the need for psychological support in the future (t(410) = 4.238, p < 0.001, 95%CI [0.654, 1.786]). Globally, the willingness or intention to ask for psychological support in the future was directly related to uncertainty about the future experienced during confinement (t(411) = −3.049, p = 0.002, 95%CI [−1.351, −0.292]).
High risk profile of psychological impact as a response to the COVID pandemic
A statistically significant model (χ2(7,N = 411) = 100.112; p < 0.001;Nagelkerke R2 = 0.308) predicting profiles of higher odds to experience persistent psychological was obtained for the studied sample, including the following factors: higher degree of distress (OR = 208, p < 0.001, 95%CI [1.089, 1.341]), reporting higher number of psychological symptoms during confinement (OR = 1.208, p < .001, 95%CI [1.089, 1.341]), suffering from chronic conditions (OR = 2.541, p = 0.006, 95%CI [1.313, 4.917], concerned about the uncertainty in the future (OR = 1.743, p = 0.027, 95%CI [1.065, 2.853), receiving psychological support during confinement (OR = 6.236, p < 0.001, 95%CI [2.736, 14.214]), being female (OR = 0.545, p = 0.033, 95%CI [.312, .952]) and younger (OR = 0.975, p = 0.019, 95%CI [0.955, 0.996]).
Discussion
The COVID-19 has led to dramatic changes worldwide in people’s everyday lives. To combat the pandemic, many governments have implemented social distancing, quarantine, and stay-at-home orders. Despite the urgent need claimed by several authors to systematically examine the psychological health of the population being most affected by the COVID-19 pandemic (Brooks et al., 2020; de Carvalho et al., 2020; Duan and Zhu, 2020; Zandifar and Badrfam, 2020), there is still limited scientific data on the impact of such extreme and extraordinary measures on mental health. To fill this gap in the literature, this online population survey study focused on exploring and describing data on the psychological impact that the first stages of COVID-19 crisis and confinement had on Spaniards’ psychological health.
Concerning the first objective of the study aimed at describing psychological impact, it has been found that main worries during confinement in the studied sample were the health status of the loved ones, uncertainty about the future and being a carrier and infecting others. There were no significant differences between genders or age. Nevertheless, the older reported to be equally worried about being infected and the economy of the society. Our results are in line with previous research that has outlined that the psychological impact of quarantine can vary from immediate effects - like irritability, fear of contracting and spreading infection to family members, anger, confusion, frustration, loneliness, denial, anxiety, depression, insomnia, despair to extremes of consequences, including suicide (Barbisch et al., 2015; Brooks et al., 2020; Liu et al., 2012).
Another very relevant aspect to be consider is fear, stigma and societal rejection regarding the quarantined cordon in forms of discrimination, suspicion and avoidance by neighborhood, workplace prejudice (i.e. among healthcare professionals quarantined) and withdrawal from social events even after containment of epidemics (Barbisch et al., 2015; Brooks et al., 2020; Liu et al., 2012); (Mertens et al., n.d.). In this sense, in our sample, health professionals were clearly more aware than the general population about the possibility of becoming transmitters of the virus, despite not being the subgroup that was worse off both physically and mentally. Nevertheless, their concern was also greater regarding the uncertainties of the future in relation to the evolution of this pandemic. Despite positive general health status among this population, healthcare professionals who are (or suspected to be) infected with COVID-19 and need isolation or quarantine might require special attention to meet their fear, anxiety and other psychological effects (Ruiz and Gibson, 2020; Sankhi and Marasine, 2020; Tan et al., 2020).
Half of the sample rates their self-perceived health as good despite the health crises. This could be explained because also, half of the sample did not report any symptoms compatible with a COVID-19 diagnosis. However, and as expected, health status was significantly related to mental health, including COVID-related distress and concerns, the specific worry of being a possible case and infecting others, and the expectancy of asking for psychological support in a near future. Likewise, despite being a clear minority in our sample (<10% of the whole sample), people receiving psychological support -related or not to COVID-, showed poorer self-perceived health, maybe due to a greater acceptance and/or insight about their suffering and general health. Often, therapeutic change involves a transition period in which, through work with the elements that cause discomfort, painful aspects of the individual are revealed and might temporarily decrease his/her well-being, to later give way to a level of superior performance. This is why sometimes the initiation and development of psychological therapy can translate into higher levels of emotional distress than those experienced by people who do not come into contact with this inner reality (Corey, 2008; Goldfried, 1980). In this study, people having received a positive diagnosis for COVID-19 claimed to be more predisposed to seek psychological help in the near future, possibly related to fear experienced and/or uncertainty about the future.
When analyzing variables related to psychological impact of COVID-19, it was found that, in accordance with other studies carried out in China (Liu et al., 2020a; Sun et al., 2020; Wang et al., 2020a; Wu, 2020), or other countries (Alkhamees et al., 2020; Varshney et al., 2020), our results suggest that women and vulnerable populations such as the youngest and the elderly, are the ones that suffered the greater psychological impact due to different factors.
Concerning gender, the study of Rodríguez and collaborators (Ni et al., 2020; Rodríguez-Rey et al., 2020), carried out in our own country, has already shown that it is women who experience the highest levels of discomfort, given all the stresses imposed by the COVID pandemic situation. This result should not come as a surprise if we consider the ways that gender roles differently affect women and men (Wenham et al., 2020). Likewise, in our cultural setting, women present a more externalizing pattern and are more open to sharing their emotional distress compared to men (Chaplin, 2015). However, results in this area are inconsistent and recent evidence shows that there are many nuances, especially with regard to non-verbal communication of emotions (McDuff et al., 2017). Despite the whole sample considered crucial to offer psychological support to any individual significantly affected by the virus or its consequences (specially, healthcare professionals), women were also those significantly more aware of the need of this service to cope with the situation and promote resilience among those affected. This is in line with previous research depicting gender differences in preferences for psychological treatment and triggers to help-seeking (Liddon et al., 2018).
As for age, some literature in the field of disaster and trauma indicates that the elderly are particularly vulnerable to the negative psychological sequelae of critical situations, such as PTSD (Ngo, 2001). However, in line with our results, most of the studies have found that age constitutes a protective effect (Jorm, 2000; Website, n.d.) that in our case had a medium effect size and the youngest have revealed as the collective more vulnerable to suffer more psychological symptoms (e.g. apathy, depressed mood, tiredness/fatigue, stress or irritability) (Mazza et al., 2020; Qiu et al., 2020). Contrary to what many of the messages that the media have shared throughout the COVID crisis, especially in periods of post-lockdown or de-escalation (El alegato de los mayores a los jóvenes que pasan del coronavirus: “Se acabó la fiesta,” 2020) (La OMS alerta a los jóvenes sobre el riesgo del ocio noct. . . - Consalud, 2020), young adults have turned out to be the most concerned group about being a possible carrier and transmitter of the virus. This might be explained because they are the ones who have had to go to work forcibly during confinement, or because they could be more aware of not having maintained strict social isolation and distancing, for whatever reason. In any case, future studies should explore the psychological impact of the COVID-19 pandemic in larger samples of both age-groups, analyzing how younger and older participants cope and recover differently from the psychological effects of the COVID-19 crisis. What is clear from our results is that the elderly are those with the greatest probability of suffering from chronic diseases and experiencing physical symptoms compatible with a COVID diagnosis and, perhaps for this reason, they are the ones that have been preferably tested for COVID in our country. It is important to bear in mind that during the time of execution of this survey, massive tests were not being carried out in our country. This has been largely due to lack of resources and/or poor planning. Therefore, and as our results have shown, there was a lot of uncertainty regarding the possibility of being infected or not, or having been in contact with other infected people, with the consequent chain of transmission of contagions that this could entail in the population. Thus, only 15 cases were tested and resulted positive for COVID-19 in our sample. They were precisely those older and reporting the worst self-perceived health.
So far, not only physical but also psychological mid and long-term effects of COVID-19 are still quite unknown to the scientific community. In a study examining the level of stress and distress one year after the outbreak among survivors (general population) of SARS, it was found that they still showed high levels of stress and worrying levels of psychological distress; recognising the importance of not ignoring the long-term psychological implications of the infectious diseases, mainly in healthcare professionals, specifying that mental health services could play an important role in the psychosocial rehabilitation (Brooks et al., 2020; Lee et al., 2007). In the current pandemic, a recent study in this line carried out in China, revealed that 54% of respondents showed moderate-to-severe persistent psychological impact, 16% and 29% moderate-to-high depressive or anxiety symptoms, respectively, and 8% moderate-to-high levels of stress (Wang et al., 2020b). Besides, anxiety and depression symptoms showed no decline four weeks after the COVID-19 pandemic (Wang et al., 2020a).
Finally, our results have revealed that the risk profile to suffer greater psychological impact and needing psychological support in the future as a consequence, are younger females worried about the future, experiencing higher degree of distress, psychological symptoms, already following psychological therapy and suffering from pre-existing chronic conditions. These results are in line with recent research (Barbisch et al., 2015; Brooks et al., 2020; Liu et al., 2012) but some factors such as gender or cohabiting still need to be further studied since mixed evidences have been reported (Vindegaard and Benros, 2020).
Implications
Getting people safe through the pandemic is the immediate aim. Subsequently, a major effort and targeted resources will be necessary to ensure services that will allow people to maintain or return to optimal functioning are quickly re-established (Milligan and McGuinness, 2009). Some of the issues that have been revealed as major concerns following quarantine are fears about becoming infected and then infecting others. The health status of loved ones and uncertainty about the future and possible new outbreaks are very prevalent in the studied sample. These stressors are likely to cause high levels of emotional distress and thus, worsen the psycho-affective state and the self-perceived health status of people (Perini, 2012; Wang et al., 2020b). Information and communication technologies could mitigate the mental health impact of COVID-19 and lockdowns by maintaining social contact during physical distancing, as well as providing health services including: information provision, telemedicine and/or online psychological counseling (Liu et al., 2020b; Wang et al., n.d.). Yet, it is also important to bear in mind that social and mass media can also spread fake news during an epidemic that might cause negative emotions and worsen the psychological impact (Grady et al., n.d.; Kadam and Atre, 2020; Kramer et al., 2014). During the COVID-19 crisis, digital technologies have become a major route for accessing remote care. Therefore, the need to ensure that these tools are safe and effective has never been greater (Inkster et al., 2020). Ecological Momentary Assessments (EMA) are a great opportunity in this context, to provide information and assessment at real time and in the real context, improving the ecological validity of assessment tools. In addition, because of the enormous advances in information and communication technologies (ICTs), nowadays it is possible to conduct tailored person-centered interventions in natural contexts, which can facilitate efficiency and efficacy and also, timely application and generalization of learned skills. These types of interventions, also known as Ecological Momentary Interventions (EMIs) are beginning to be used more and more in the field of health psychology with promising results (Heron and Smyth, 2010; Moskowitz and Young, 2006; Versluis et al., 2016). In this sense, Zhang et al. (2020) put forward a new psychological crisis intervention model by utilizing internet technology. This new model integrates physicians, mental health professionals and social workers into Internet platforms to carry out psychological intervention to patients, their families and medical staff. This is one very valuable model that could serve as a basis for developing a similar comprehensive psychological crisis intervention response system that is applicable for urgent social and psychological problems, such as this caused by the COVID-19 pandemic.
Limitations
This study has its limitations owing to a small sample size for exploratory factor analysis and for the time-sensitivity of the outbreak and with a curfew in place, we adopted a snowballing sampling strategy, which allows for studies to take place where otherwise it might be impossible to conduct because of a lack of participants. However, non-probabilistic sampling techniques make impossible to determine the sampling error or make solid inferences about populations. Also, the survey provides only a snapshot of psychological responses at a particular point in time, and therefore, a longitudinal study with larger sample size is required to provide information on whether the observed impact will last for longer periods. Similarly, self-reported psychological impact might not adequately represent the mental health status assessed by means of a full in depth clinical interview; thus, for the outcome to be determined, prospective studies are necessary to provide more accurate data to support the need for focused public mental health strategies. Lastly, the number of respondents who have been quarantined and tested for COVID-19, and had a contact history with infected persons was minimal, and our result could not be generalized to them. Despite all the above limitations, our study provides very relevant information about the immediate psychological responses of the general population on the COVID-19 pandemic, giving a clear idea about the magnitude of the psychological burden on the community during the COVID-19 outbreak. Besides, results cover many factors that can influence mental health, providing a broader vision of the issue for future research, aimed at minimizing the psychological impact of similar health crises.
Conclusions
During this time of global pandemic, it is so important to continue to advocate for those in the community who are particularly vulnerable in the context of considerable existing mental health and associated social challenges. Policy makers need to include specific sections on different COVID-19 management protocols, addressing how to handle the psychological impact of the pandemic on mental health, both by the virus itself and the emerging social situation. Special emphasis should be placed on health professionals who are one of the most vulnerable groups to suffer psychological disorders, along with hospitalized patients and people with pre-existing mental health conditions. Considering that we are still in the midst of an evolving situation that can unleash a deeper kind of unmoored experience of people’s life, we believe our results provide new insights on the psychological impact of COVID-19, and can help to design tailored person-centered interventions for those at higher risk, helping not only to adjust but also to thrive through the unknown times ahead.
Highlights
The transformation that coronavirus disease pandemic has brought upon the world and mental health is unparalleled.
Online-based surveys have revealed as suitable methods for gathering data on psychological impact during confinement.
It is crucial to leverage technologies for the most vulnerable, especially in extraordinary situations such as confinement.
Ecological Momentary Assessments/Interventions are a great opportunity in these contexts of lockdown and quarantine.
Acknowledgments
We gratefully acknowledge all participants for their contributions to the study and for circulating this survey during the process of data collection.
Footnotes
Authors’ contributions: CCT and AC were responsible for the study design and conducting. MTS and CCT analyzed data. CCT wrote the first draft of the manuscript. CCT, MTS, and AC participated in the following versions of the manuscript and made important contributions to its final version. All authors have read and have approved the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Informed consent was obtained from participants for publication of their results in combination with the rest of the participants’ results.
ORCID iD: Carmina Castellano-Tejedor  https://orcid.org/0000-0003-2335-8550
https://orcid.org/0000-0003-2335-8550
References
- Alkhamees AA, Alrashed SA, Alzunaydi AA, et al. (2020) The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Comprehensive Psychiatry 102: 152192. DOI: 10.1016/j.comppsych.2020.152192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbisch D, Koenig KL, Shih F-Y. (2015) Is there a case for quarantine? Perspectives from SARS to Ebola. Disaster Medicine and Public Health Preparedness 9(5): 547–553. DOI: 10.1017/dmp.2015.38. [DOI] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, et al. (2020) The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet 395(10227): 912–920. DOI: 10.1016/s0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaplin TM. (2015) Gender and emotion expression: A developmental contextual perspective. Emotion Review: Journal of the International Society for Research on Emotion 7(1): 14–21. DOI: 10.1177/1754073914544408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corey G. (2008) Theory and Practice of Counseling and Psychotherapy. Cengage Learning. Available at: http://perpus.univpancasila.ac.id/repository/EBUPT190498.pdf [Google Scholar]
- El alegato de los mayores a los jóvenes que pasan del coronavirus: “Se acabó la fiesta” (2020). Available at: https://www.lavanguardia.com/participacion/debates/20200802/482622885805/debate-mayores-jovenes-contagios-rebrotes-covid-19-ocio-nocturno.html (accessed 26 August 2020).
- Goldfried MR. (1980) Toward the delineation of therapeutic change principles. The American psychologist 35(11): 991–999. DOI: 10.1037//0003-066x.35.11.991. [DOI] [PubMed] [Google Scholar]
- Grady C, Feliciano JT, Kwon J, et al. (n.d.) Influence of news media and public health agencies during pre-pandemic COVID-19: Twitter analysis (Preprint). Avaialble at: https://preprints.jmir.org/preprint/19460
- Heron KE, Smyth JM. (2010) Ecological momentary interventions: Incorporating mobile technology into psychosocial and health behaviour treatments. British Journal of Health Psychology 15(Pt 1): 1–39. DOI: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang T-J, Rabheru K, Peisah C, et al. (2020) Loneliness and social isolation during the COVID-19 pandemic. International Psychogeriatrics: 1–4. Epub ahead of print 26May2020. DOI: 10.1017/S1041610220000988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inkster B, O’Brien R, Selby E, et al. (2020) Digital health management during and beyond the COVID-19 pandemic: Opportunities, barriers, and recommendations. JMIR Mental Health 7(7): e19246. DOI: 10.2196/19246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam MS, Sarkar T, Khan SH, et al. (2020) COVID-19-related infodemic and its impact on public health: A global social media analysis. The American Journal of Tropical Medicine and Hygiene 103(4): 1621–1629. DOI: 10.4269/ajtmh.20-0812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm AF. (2000) Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychological Medicine 30(1): 11–22. DOI: 10.1017/s0033291799001452. [DOI] [PubMed] [Google Scholar]
- Kadam AB, Atre SR. (2020) Negative impact of social media panic during the COVID-19 outbreak in India. Journal of Travel Medicine 27(3): taaa057. DOI: 10.1093/jtm/taaa057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer ADI, Guillory JE, Hancock JT. (2014) Experimental evidence of massive-scale emotional contagion through social networks. Proceedings of the National Academy of Sciences of the United States of America 111(24): 8788–8790. DOI: 10.1073/pnas.1320040111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La OMS alerta a los jóvenes sobre el riesgo del ocio noct. . . - Consalud (2020). Available at: https://www.consalud.es/pacientes/especial-coronavirus/oms-alerta-jovenes-riesgo-ocio-nocturno-realmente-necesitais-fiesta_83678_102.html (accessed 26 August 2020).
- Lee AM, Wong JG, McAlonan GM, et al. (2007) Stress and psychological distress among SARS survivors 1 year after the outbreak. The Canadian Journal of Psychiatry 52(4): 233–240. DOI: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- Liddon L, Kingerlee R, Barry JA. (2018) Gender differences in preferences for psychological treatment, coping strategies, and triggers to help-seeking. The British Journal of Clinical Psychology 57(1): 42–58. DOI: 10.1111/bjc.12147. [DOI] [PubMed] [Google Scholar]
- Lin C-Y. (2020) Social reaction toward the 2019 novel coronavirus (COVID-19). Journal of Health and Social Behavior 3(1): 1–2. DOI: 10.4103/SHB.SHB_11_20. [DOI] [Google Scholar]
- Liu N, Zhang F, Wei C, et al. (2020. a) Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Research 287: 112921. DOI: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S, Yang L, Zhang C, et al. (2020. b) Online mental health services in China during the COVID-19 outbreak. The Lancet Psychiatry 7(4): e17–e18. DOI: 10.1016/s2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Kakade M, Fuller CJ, et al. (2012) Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Comprehensive Psychiatry 53(1): 15–23. DOI: 10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie N. (1993) Book review at risk in America: The health and health care needs of vulnerable populations in the United States by Lu Ann Aday. 375 pp. San Francisco, Jossey-Bass, 1993. New England Journal of Medicine, 329(9): 671. DOI: 10.1056/nejm199308263290924. [DOI] [Google Scholar]
- Marazziti D., Pozza A., Di Giuseppe M., Conversano C. (2020). The psychosocial impact of COVID-19 pandemic in Italy: A lesson for mental health prevention in the first severely hit European country. Psychological Trauma: Theory, Research, Practice, and Policy, 12(5), 531. [DOI] [PubMed] [Google Scholar]
- Mazza C, Ricci E, Biondi S, et al. (2020) A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. International Journal of Environmental Research and Public Health 17(9): 3165. DOI: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDuff D, Kodra E, el Kaliouby R, et al. (2017) A large-scale analysis of sex differences in facial expressions. PloS One 12(4): e0173942. DOI: 10.1371/journal.pone.0173942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens G, Gerritsen L, Duijndam S, et al. (n.d.) Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March2020. Journal of Anxiety Disorders 74: 102258. DOI: 10.31234/osf.io/2p57j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milligan G, McGuinness TM. (2009) Mental health needs in a post-disaster environment. Journal of Psychosocial Nursing and Mental Health Services 36(3): 159–164. DOI: 10.3928/02793695-20090731-01. [DOI] [PubMed] [Google Scholar]
- Moskowitz DS, Young SN. (2006) Ecological momentary assessment: What it is and why it is a method of the future in clinical psychopharmacology. Journal of Psychiatry & Neuroscience 31(1): 13–20. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1325062/ [PMC free article] [PubMed] [Google Scholar]
- Ngo EB. (2001) When disasters and age collide: Reviewing vulnerability of the elderly. Natural Hazards Review 2(2): 80–89. DOI: 10.1061/(asce)1527-6988(2001)2:2(80). [DOI] [Google Scholar]
- Ni MY, Yang L, Leung CMC, et al. (2020) Mental health, risk factors, and social media use during the COVID-19 epidemic and Cordon Sanitaire among the community and health professionals in Wuhan, China: Cross-sectional survey. JMIR Mental Health 7(5): e19009. DOI: 10.2196/19009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perini M. (2012) Panic and pandemics: From fear of contagion to contagion of fear. In: Brunning H. (ed.) Psychoanalytic Reflections on a Changing World, 1st edition. London: Routledge. [Google Scholar]
- Qiu J, Shen B, Zhao M, et al. (2020) A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry 33(2): e100213. DOI: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick B. (2020) A third of Americans report anxiety or depression symptoms during the pandemic. Vox. Available at: https://www.vox.com/science-and-health/2020/5/29/21274495/pandemic-cdc-mental-health (accessed 25 July 2020). [Google Scholar]
- Rodríguez-Rey R, Garrido-Hernansaiz H, Collado S. (2020) Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Frontiers in Psychology 11: 1540. DOI: 10.3389/fpsyg.2020.01540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz MA, Gibson C-AM. (2020) Emotional impact of the COVID-19 pandemic on U.S. health care workers: A gathering storm. Psychological Trauma: Theory, Research, Practice, and Policy 12(S1): S153–S155. DOI: 10.1037/tra0000851. [DOI] [PubMed] [Google Scholar]
- Sankhi S, Marasine NR. (2020) Impact of COVID-19 pandemic on mental health of the general population, students, and health care workers. Europasian Journal of Medical Sciences 2 (COVID-19 special Issue): 1–9. DOI: 10.46405/ejms.v2i2.131 [Google Scholar]
- Standl F, Jöckel K-H, Brune B, et al. (2020) Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. The Lancet Infectious Diseases 20(9): E238–E244. DOI: 10.1016/S1473-3099(20)30648-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun L, Sun Z, Wu L, et al. (2020) Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. Psychiatry and Clinical Psychology medrxiv;2020.03.06.20032425v1. medRxiv. [Google Scholar]
- Tan BYQ, Chew NWS, Lee GKH, et al. (2020) Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Annals of Internal Medicine 173(4): 317–320. DOI: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varshney M, Parel JT, Raizada N, et al. (2020) Initial psychological impact of COVID-19 and its correlates in Indian Community: An online (FEEL-COVID) survey. PloS One 15(5): e0233874. DOI: 10.1371/journal.pone.0233874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Versluis A, Verkuil B, Spinhoven P, et al. (2016) Changing mental health and positive psychological well-being using ecological momentary interventions: A systematic review and meta-analysis. Journal of Medical Internet Research 18(6): e152. DOI: 10.2196/jmir.5642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N, Benros ME. (2020) COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity 89: 531–542. DOI: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, et al. (2020. a) A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity 87: 40–48. DOI: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, et al. (2020. b) Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health 17(5): 1729. DOI: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Li B, Liu L. (n.d.) Telemedicine for COVID-19 in China. JMIR Preprint. DOI: 10.2196/preprints.19010. [DOI] [Google Scholar]
- Wenham C, Smith J, Morgan R, et al. (2020) COVID-19: The gendered impacts of the outbreak. The Lancet 395(10227): 846–848. DOI: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Mental health and psychosocial considerations during the COVID-19 outbreak, 18March2020. (No. WHO/2019-nCoV/MentalHealth/2020.1). World Health Organization. [Google Scholar]
- Wu B. (2020) Social isolation and loneliness among older adults in the context of COVID-19: A global challenge. Global Health Research and Policy 5: 27. DOI: 10.1186/s41256-020-00154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Wu W, Zhao X, et al. (2020) Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: A model of West China Hospital. Precision Clinical Medicine 3(1): 3–8. DOI: 10.1093/pcmedi/pbaa006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zysberg L, Zisberg A. (2020) Days of worry: Emotional intelligence and social support mediate worry in the COVID-19 pandemic. Journal of Health Psychology 1359105320949935. Epub ahead of print 18August2020. DOI: 10.1177/1359105320949935. [DOI] [PubMed] [Google Scholar]