Abstract
Background & Aims
Though viewed as a critical measure to prevent the spread of the virus, a prolonged homestay may result in unfavourable sedentary behaviour and chronic disease risk. This systematic review focuses on sedentary behaviour resulting from this quarantine period which may elevate the cardiovascular disease risk, obesity, hypertension, cancer and mental health illness.
Methods
Evidence of breaking sedentary behaviour and global recommendations were investigated. Potential unanswered questions regarding sedentary behaviour and physical activity during lockdown were explored.
Results
Five systematic reviews and six prospective trials explored the effect of sedentarism affecting chronic disease through potential pathophysiological mechanisms. Sedentary behaviour especially prolonged sitting is found to be a pleiotropic risk factor with altered energy expenditure, adipogenic signalling, immunomodulation, autonomic stability and hormonal dysregulation perpetuating underlying chronic diseases such as obesity, cardiovascular disease, cancer and mental health disorders.
Conclusion
Breaking sitting and physical activity are found to reverse the adverse effects associated with excessive sitting during the lockdown.
Keywords: Sitting, physical activity, exercise, chronic disease, obesity, cardiovascular disease
Introduction
Though Chinese origin, Coronavirus disease (COVID-19) has become the global concern and public health emergency as declared by the World Health Organization (WHO). With 1st case reported on 4 March, cases are increasing at an alarming rate. As of 22 May 2020, WHO situation report-123 reveals 4993470 confirmed cases and 327738 deaths globally.1 The extent, prognosis of the COVID-19 and lockdown remains mostly unknown.
National lockdown and sedentary behaviour
The public has been advised by various health authorities to reduce travelling and stay at home as an essential means of limiting people's exposure to the virus as the virus transmission is continued to outgrow.2 Our government has implemented several mitigating measures such as travel bans, shutting more significant industries and institutions, essential commodities at the doorsteps and work from home for employees. Further implementing restrictions on necessary commodities such as groceries, medical shops, etc. has reduced the commute in the community. Shutting down schools and colleges, playgrounds, ban on outdoor games have reduced the quality of activity from toddlers till young adults substantially. Though unarguably a safety measure against the virus, lockdown or quarantine may have negative consequences, especially on increasing sedentary behaviour and may pave the way for chronic diseases. Prolonged stay at home was found to be substantially spent on lying and sitting in front of electronic gadgets (television, social network through smartphones, laptops for educational and work). This prolonged sedentary behaviour may increase cardiometabolic risks such as hyperglycemia, hyperinsulinemia, autonomic instability, altered immune markers expression, especially interleukins (IL 6), cytokines and tumor necrosis factor (TNF). Further hormonal dysfunction, including leptin, thyroxine which may potentially worsen underlying chronic diseases.3 This systematic review would demonstrate the possible molecular mechanisms of sedentary behaviour, especially uninterrupted sitting and chronic diseases, its evidence and physical measures administered to curb sedentary behaviour during the quarantine. This review may potentially improve the reader's awareness of sedentary behaviour during the self-quarantine period and how to maintain fitness to overcome the negative consequences.
Sedentary behaviour and chronic diseases
Sedentary behaviour (defined as any awakened activity such as lying or sitting characterized by the energy expenditure of fewer than 1.5 METS) is found to be one of the prime risk factors for onset and worsening of chronic diseases such as obesity, hypertension, coronary artery diseases and cancer.4 Further early cognitive decline, including worsening of memory, reaction times and implicit association is strongly associated with inactivity.5 Human evolution survived through ages because of our “hunter-gatherer” genes which are now being adapted for sedentary lifestyle due to technology spur and in turn leading to chronic disease.6 In a recent cross-sectional survey from a National Family Health survey, the prevalence of overweight and obesity was found to be doubled between 1998 and 2016. Total disability-adjusted life years have increased by 170% from 1990 to 2016 due to diabetes,7 but survey considered only socioeconomic status not considered the physical activity as a contributing risk to chronic diseases. Bountiful western literature is available that identified sedentary behaviour especially excessive sitting as the independent risk factor for the incidence or worsening of cardiometabolic and other chronic diseases.8 The following search and subsequent literature summary may reinforce the importance of curbing sedentary behaviour and its adverse effects during the lockdown period
Methods
Literature search
Scopus, Web of Science, PubMed and Ovid Medline databases were searched until 23 April 2020, with the following MeSH term “Sedentary behavio?r”, “Sitting”, “Physical inactivity”, “chronic diseases”, “Non communicable diseases”, “obesity”, cardiovascular diseases”, “cardiometabolic”, “cancer”, “diabetes”, “hypertension”. Boolean operators such as AND, OR and wild cards *,? were used as necessary. We limited our search to full text and English only. Observational studies, randomized trials, systematic reviews, narrative reviews that have identified sedentary behaviour as the independent risk factor for chronic diseases. We synthesized the retrieved results to data extraction table that included author, year, country, objective, study design, participants, method, sedentary behaviour measurement, key findings, possible physiology mechanisms (Table 1).
Table 1.
Table showing the studies included in the systematic review and the key findings.
| References | Country | Objective | Design | Participants | Method | Sedentary behaviour measurement | Key findings | Physiology |
|---|---|---|---|---|---|---|---|---|
| Obesity | ||||||||
| Megan Crowe et al.9 | Canada | To find out the risk associated with combined MVPA and screen time on overweight or obesity | Cross-sectional study | 9913 students of 7–12 grades | MVPA (active >60 min/day; inactive <60 min/day) and sedentary (>2 h of screen time; not sedentary (<2 h of screen time) were related with overweight and obesity | Sedentary > 2 h screen time/day; not sedentary < 2 h/day (questionnaire) | The inactive and sedentary the group was likely to have overweight or obesity than the active and not sedentary group (OR = 1.71; 95% CI, 1.26–2.32) | The body composition and energy expenditure were the possible reasons |
| Saeidifard et al.10 | USA | To find out the differences in EE between sitting and standing | Systematic review and meta-analysis | 46 studies (1184 participants) | The literature was searched until June 2017 for studies involving EE between sitting and standing in non-pregnant adults | EE was measured using accelerometers and indirect calorimeters | The mean difference in EE between standing and standing was 0.15 kcal/min (95% confidence interval (CI) 0.12–0.17) | Sitting reduces muscle recruitment and reduces the EE. Postures other than sitting improves NEAT and reduces obesity |
| Henson et al.11 | United Kingdom | To examine associations between sedentary time and adiposity | A nested study from a large RCT | 124 participants at the risk of diabetes | Accelerometers objectively measured sedentary time and MRI measured adiposity | Accelerometer (Actigraph) | Sixty minutes of sedentary time was adversely associated with 1.74 L higher total abdominal fat, 0.62 L higher visceral fat, 1.14 L higher subcutaneous fat, and 1.86% higher liver fat. | Partially explained by excess visceral fat, in which non-esterified fatty acids (NEFA), glycerol, and hormones released from adipose tissue |
| Cardiovascular diseases | ||||||||
| Lavie et al.12 | USA | To establish the relationship between cardiovascular outcomes and physical inactivity | Scoping review | Heterogenous population. 15 studies (4,58,879 men & 4,66,106 women) | The study reviewed several studies and elaborated the physiological mechanisms relating to chronic diseases and physical inactivity | Heterogenous measurement: subjective and objective measures | • Fit men were found to have reduced mortality by 52% then unfit men • everyone estimated MET increase in CRF was associated with 13% and 15% reductions in all-cause and CVD |
Reduced mitochondrial content and respiration, increased inflammation in skeletal muscles, β adrenergic receptor desensitization |
| Carter et al.13 | Netherlands | To review the studies establishing the relation between cardiometabolic risk and prolonged sitting | Scoping review | Eight studies(198 participants) | Several studies were reviewed. The cardiometabolic outcomes were associated with the physical inactivity or prolonged sitting bouts | Not mentioned | Sitting reduces flow-mediated dilatation by 2.2%; inflammatory cytokines increased, endothelial shear 2.2% ± 2.15% | Endothelial stress, cardiac remodelling and endurance, inflammatory markers (IL-6, IL-12), adiposity and atherogenesis |
| Cancer | ||||||||
| Rangul et al.15 | Norway | To examine the association between physical activity and sitting time with cancer incidence | Prospective study | 8,154 healthy participants from the Norwegian community | adults in the Nord-Trøndelag Health Study (HUNT) followed up for 17–19 years for cancer incidence | Sitting time was measured subjectively through the questionnaire | • sitting ≥eight hr/day was associated with 22% (95% CI, 1.05–1.42) higher risk of prostate cancer compared to sitting <8 h/day. • low physical activity (≤8.3 MET-h/week) had 31% (95% CI, 1.00–1.70) increased risk of colorectal cancer (CRC) and 45% (95% CI, 1.01–2.09) increased risk of lung cancer |
Possibly attributed to insulin resistance, adiponectin levels, insulin-like growth factors testosterone, muscle- and fat-related proteins as follistatin, myostatin, activin and inhibin. |
| Nguyen et al.17 | USA | To see whether sedentary behaviour related to colorectal cancer incidence | Cross-sectional study | 89,278 women in the Nurses' Health Study II ages 25–42 years | The participants from Nurses' Health Study II ages 25–42 years (1991–2011) were assessed for sedentary behaviour and colorectal cancer | TV viewing time through the questionnaire | If TV viewing hours is more than 7 hours increased the risk of colorectal cancer (RR:1.25). If more than 14 hours of RR increased by 1.69. Inspite of cumulative exercise, prolonged sitting time increases the risk of colorectal cancer | unbroken sitting results in extended exposure to faecal carcinogens, such as secondary bile acids, impair glucose homeostasis and decrease vitamin D levels |
| Lynch et al.16 | Canada | To systematically review studies examining associations of sedentary behaviourwith cancer risk | Systematic review and meta-analysis | 176 studies were retrieved investigating the effect on adiposity, sex hormones, inflammation and metabolic function | Literature search on peer-reviewed databases with SB and cancer risk. Also, the study investigated other health risks in cancer survivors. | 95% of the studies measured SB through subjective measures | A significant association between SB time and cancer risk factors (OR 1.02 – 1.17). TV times were found significantly related to cancer risk and early mortality | SB increases adiposity, sex hormones, inflammation and metabolic dysfunction predisposing to cancer |
| Diabetes | ||||||||
| Asvold et al.14 | Norway | To find whether prolonged sitting is a risk for diabetes | Prospective trial | 28,051 adult participants of the Nord-Trøndelag Health Study (the HUNT Study) were followed for diabetes incidence from 1995–1997 to 2006–2008 (11 years) | The trial used the HUNT2 Survey as the baseline risk factor examination. Diabetes risk was assessed at 11 years follow-up Self-reported sitting time | Sitting time was estimated from the questionnaires | • Sitting ≥ eight hr/day was associated with a 17% higher risk of developing diabetes compared with sitting ≤four hr/day. • Without leisure-time physical activity, this risk becomes 30% in participants sitting <8 h/day |
Hyperinsulinemia, postprandial hyperglycaemia, impaired glucose tolerance was observed. |
| Yates et al.18 | United Kingdom | To investigate whether prolonged sitting or any interruption alter the postprandial glycemia | Cross over randomized trial | 60 participants (30 south Asians and 30 Europeans) | Sitting, sitting with interruptions was administered and postprandial blood glucose was measured | Objective measure through accelerometer (ActivPAL) | insulin response was reduced by 22.4 (12.4, 32.4) mU/L (27%) during walking breaks compared to prolonged sitting | Possible mechanisms were insulin sensitivity and GLUT4 transporters sensitivity |
| Anxiety and depression | ||||||||
| Dale et al.19 | Canada | To examine the relationship between physical activity and mental health outcomes | Systematic review | 32 studies were included | Studies were searched until 2017 relating physical activity and self-esteem, anxiety and depression | Included both subjective and objective measures of physical activity included | Studies showed physical activity is inversely related to depression, anxiety and directly related to self-esteem | Self-esteem has found to reduce anxiety and depression. Possibly by endorphins and autonomic stability |
Supplementary file: Table 2. Breaking Sitting Behavior through Exercises during COVID-19 lockdown.
Results
Five systematic reviews and six prospective trials explored the effect of sedentarism affecting chronic disease through potential pathophysiological mechanisms (Table 1). The research articles included in both systematic reviews and included trials were heterogeneous in intervention, participants and outcome measure assessments. Hence qualitative synthesis of the researches was established.
Myriad of cardiometabolic risks, alterations in physiological systems determining future chronic diseases were found.9–14 Four reviews9,10,12,13 and two randomized controlled trials11,15 have established cardiometabolic risks such as hyperglycemia, hypertension, altered triglycerides and body mass index due to sedentary behaviour.
Further elevated cancer risk is identified from three articles (one prospective,15 one systematic review16 and one cross-sectional trial17) with altered immune functions, especially on proinflammatory cytokines such as interleukin and tumor necrosis factors. Most of the studies administered the physical activity interventions in the sedentary participants (self reported or accelerometer based activity of >6 h/day).16,18,20
Most of the studies, including systematic reviews, are found to originate from the United States of America, Australia and the United Kingdom. It's not surprising fact that there is a lack of evidence linking sedentary behaviour and chronic diseases in low and middle-income countries. Observed low physical activity in lower middle-income countries (16.6%) compared to Western countries (25.4%) probably speculated to be the reason for the poor evidence for the less research and lack of evidence in low-middle income countries.21 We found a significant difference in measurement techniques of sedentary behaviour ranging from questionnaires to accelerometers which might have facilitated a significant measurement bias in the studies. Further chronic disease risks, gender, nationality posed a significant heterogeneity in the studies. However, the possible associations between sedentary behaviour and possible pathophysiological mechanisms behind cardiometabolic risk were illustrated and discussed later.
Discussion
Sedentary behaviour and physiological mechanisms behind chronic diseases
Obesity
Sedentary behaviour is found to elevate the positive energy balance through reduced energy expenditure. Non-exercise activity thermogenesis plays a crucial role in elevating daily energy metabolism and found to be lowered with uninterrupted prolonged sitting bouts.22 Further sitting time is found to be adversely related to increased body mass index and waist circumference.23 The possible physiological mechanisms by which sitting causes overweight and obesity are leptin and ghrelin dysregulation, increased IL-6, thyroid dysregulation, adiponectin signalling, adipose tissue morphology, adipogenic signalling and poor gastrointestinal metabolism.24
Cardiovascular diseases
Sedentary behaviour is found to adversely associated with increased cardiometabolic risk. Atherogenesis through inadequate endothelial response to stress, inflammatory markers such as IL-6, reactive oxygen species (ROS), adiponectin and leptin dysregulation, reduced nitric oxide production and cascading atherosclerosis is postulated to enhance underlying coronary artery diseases.12 Prolonged sitting bouts increase postprandial hyperglycemia, triglyceridemia, hyperlipidemia and hypertension, which may further increase the risk of fat deposition and thrombotic nature of the blood vessels and increasing the risk of coronary artery diseases.25
Diabetes
Sedentary behaviour, especially uninterrupted sitting, is associated with reduced insulin sensitivity and GLUT 4 transporters, which in turn results in diabetes risk. Further increased inflammatory markers expression such as IL-6, cytokines, ROS causes damage to β cell damage further compounding the problem. Increased insulin resistance is found significantly associated with uninterrupted sitting.25
Cancer
Prolonged sitting is associated with increased inflammatory markers (C-reactive protein, leptin and adiponectin), increased adiposity, sex hormones such as poor androgen status and Vitamin C which are presumed to be the risk factors for cancer.16
Mental health
Sedentary behaviour is found to be adversely affecting mental health, especially anxiety and depression. Dale et al. recently established excessive sitting increase the risk of depression and anxiety from the 32 studies and physical activity reverses the effect on depression and anxiety.19 The pooled risk ratios of depression for sedentary behaviour were 1.31 (95% CI = 1.16–1.48) in 13 cross-sectional studies and 1.14 (95% CI = 1.06–1.21) in 11 longitudinal studies.26 Sedentary behaviour especially prolonged interrupted sitting causes depression and anxiety through potential physiological mechanisms: altered 5HT synthesis, lower serotonin, BDNF and depletion of tryptophan.27 Even lower self-esteem is found to be associated with increased sedentary behaviour leading isolation and depression.
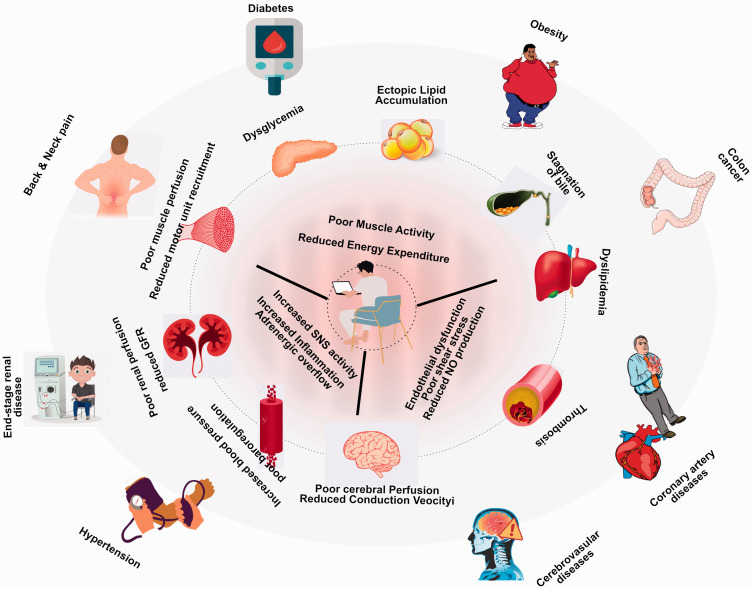
The overall physiological mechanisms of chronic disease and sedentary behaviour impact are depicted in the infographic (Figure 1).
Figure 1.
An infographic showing the relation between excessive sitting and possible biological mechanisms of chronic diseases. The inner dotted circle shows the potential physiology behind sitting leads to chronic diseases. The outer coloured circle shows the possible chronic diseases associated with excessive sitting.29
With all the above plausible biological mechanisms with the sedentary behaviour as elucidated above, it is speculated that breaking sitting with exercises or scheduled exercises may reverse the biological mechanisms and thus may improve or halt the progression of chronic diseases.
Breaking sedentary behaviour while staying at homes
Critical restriction measures for societal mobility as proclaimed by the government doesn't mean that exercises should also be ceased. Exercise at home with safe, simple, and easily implementable exercises is well suited to maintain fitness levels during the lockdown period. These exercises may include but are not limited to, aerobic exercises, strengthening exercises, activities for balance and control and stretching exercises. Examples of home exercises may include walking in the house, alternating leg lunges, stair climbing, stand-to-sit and sit-to-stand using a chair and from the floor, chair squats, and sit-ups and push-ups.28 Table 2 demonstrates sample exercises that are found to be safe and straightforward and can be done in-home without expensive equipment (supplementary file). The use of eHealth and mHealth videos, which focuses on encouraging and delivering physical activity through the smartphone applications and television should be done with precautions (based on underlying fitness & chronic diseases), and dosage should be considered after appropriate advice from exercise professional during this critical period.
Recommendation for breaks and exercises
Global guidance for preventing chronic diseases and maintain general fitness is to exercise for at least 30 minutes every day at least five days a week.30 In this central lockdown period, it is recommended to do exercise for 30 minutes all days of a week. Further, the prolonged sitting bouts (sitting >30 minutes) should be limited to a maximum of 2 per day and a mandatory break for 2 minutes every 30 minutes of sitting.31 Sleep is not added to the sedentary behaviour.
Staying active throughout the day
Apart from exercises mentioned above, it is recommended that every citizen should be active throughout the day by lifting and carrying groceries from neighbourhood groceries with necessary protective equipment, stair climbing even though not mandatory, using smartphone applications for a scheduled walk and step count, playing with children, gardening and standing while watching television. These simple measures, when cumulated over a while, may serve as potential measures for preventing and managing chronic disease risks.
Questions remaining unanswered?
The following questions remain unanswered: (1) whether sedentary behaviour during quarantine or homestay alters the Coronavirus disease risk and prognosis? (2) Whether patients with underlying coronavirus and known cardiovascular diseases suffer more significant coronary events than patients without coronavirus? (3) Whether immune responses boost up with the moderate or high intensity of exercise during the quarantine to prevent coronavirus? (4) Whether hospital stay, the cost differs among patients who exercised regularly or sedentary.
Conclusion
Though a fundamental safety step to limit infections from spreading widely in the Indian community, prolonged home stays can increase sedentary behaviours and may increase chronic disease risks. During the Coronavirus crisis, maintaining a regular physical activity and routinely exercising in homes is an essential strategy for happy and healthy lives. Future trials should focus on the questions remaining unanswered to emphasize physical activity and reducing sedentary behaviour as an essential measure to combat cardiometabolic disease risk during such future pandemics.
Supplemental Material
Supplemental material, sj-pdf-1-scm-10.1177_0036933020946336 for Sedentarism and chronic disease risk in COVID 19 lockdown – a scoping review by Baskaran Chandrasekaran and Thiru Balaji Ganesan in Scottish Medical Journal
Acknowledgements
The authors wish to thank Dr Fiddy Davis PhD, Head of the Department, Department of Exercise and Sports Sciences, Manipal Academy of Higher Education, Manipal, Karnataka, India for his continuous support and motivation for the research and article.
Footnotes
Authors’ contribution: BC conceived and designed the literature review, TBG carried out data analysis. BC interpreted the findings and drafted the article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Baskaran Chandrasekaran https://orcid.org/0000-0003-1439-9158
Supplemental Material: Supplemental material for this article is available online.
References
- 1.WHO. Coronavirus disease 2019. (COVID-19) Situation Report – 95, www.who.int/docs/default-source/coronaviruse/situation-reports/20200424-sitrep-95-covid-19.pdf?sfvrsn=e8065831_4. (accessed 25 April 2020).
- 2.Pulla P.Covid-19: India imposes lockdown for 21 days and cases rise. BMJ 2020; 368: m1251. [DOI] [PubMed] [Google Scholar]
- 3.Benatti FB, Ried-Larsen M.The effects of breaking up prolonged sitting time: a review of experimental studies. Med Sci Sports Exerc 2015; 47: 2053–2061. [DOI] [PubMed] [Google Scholar]
- 4.Gibbs B, Hergenroeder A, Katzmarzyk P, et al. Definition, measurement, and health risks associated with sedentary behavior. Med Sci Sports Exerc 2015; 47: 1295–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magnon V, Vallet GT, Auxiette C. Sedentary Behavior at Work and Cognitive Functioning: A Systematic Review. Front Public Health 2018; 6: 239. DOI: 10.3389/fpubh.2018.00239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Speakman JR.An evolutionary perspective on sedentary behavior. Bioessays 2020; 42: e1900156. [DOI] [PubMed] [Google Scholar]
- 7.Corsi DJ, Subramanian SV.Socioeconomic gradients and distribution of diabetes, hypertension, and obesity in India. JAMA Netw Open 2019; 2: e190411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wijndaele K, Healy GN.Sitting and chronic disease: where do we go from here? Diabetologia 2016; 59: 688–691. [DOI] [PubMed] [Google Scholar]
- 9.Crowe M, Sampasa-Kanyinga H, Saunders TJ, et al. Combinations of physical activity and screen time recommendations and their association with overweight/obesity in adolescents. Can J Public Health. Epub ahead of print 13 April 2020. DOI: 10.17269/s41997-020-00313-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saeidifard F, Medina-Inojosa JR, Supervia M, et al. Differences of energy expenditure while sitting versus standing: a systematic review and Meta-analysis. Eur J Prev Cardiol 2018; 25: 522–538. [DOI] [PubMed] [Google Scholar]
- 11.Henson J, Edwardson CL, Morgan B, et al. Sedentary time and MRI-Derived measures of adiposity in active versus inactive individuals. Obesity (Silver Spring) 2018; 26: 29–36. [DOI] [PubMed] [Google Scholar]
- 12.Lavie CJ, Ozemek C, Carbone S, et al. Sedentary behavior, exercise, and cardiovascular health. Circ Res 2019; 124: 799–815. [DOI] [PubMed] [Google Scholar]
- 13.Carter S, Hartman Y, Holder S, et al. Sedentary behavior and cardiovascular disease risk: mediating mechanisms. Exerc Sport Sci Rev 2017; 45: 80–86. [DOI] [PubMed] [Google Scholar]
- 14.Åsvold BO, Midthjell K, Krokstad S, et al. Prolonged sitting may increase diabetes risk in physically inactive individuals: an 11 year follow-up of the HUNT study, Norway. Diabetologia 2017; 60: 830–835. [DOI] [PubMed] [Google Scholar]
- 15.Rangul V, Sund ER, Mork PJ, et al. The associations of sitting time and physical activity on total and site-specific cancer incidence: results from the HUNT study, Norway. PLoS One 2018; 13: e0206015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lynch BM.Sedentary behavior and cancer: a systematic review of the literature and proposed biological mechanisms. Cancer Epidemiol Biomarkers Prev 2010; 19: 2691–2709. [DOI] [PubMed] [Google Scholar]
- 17.Nguyen LH, Liu PH, Zheng X, et al. Sedentary behaviors, TV viewing time, and risk of young-onset colorectal cancer. JNCI Cancer Spectr 2018; 2: pky073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yates T, Edwardson CL, Celis-Morales C, et al. Metabolic effects of breaking prolonged sitting with standing or light walking in Older South Asians and White Europeans: a randomized acute study. J Gerontol A Biol Sci Med Sci 2020; 75: 139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dale LP, Vanderloo L, Moore S, et al. Physical activity and depression, anxiety, and self-esteem in children and youth: an umbrella systematic review. Mental Health Physical Activity 2019; 16: 66–79. [Google Scholar]
- 20.Carter SE, Draijer R, Holder SM, et al. Effect of different walking break strategies on superficial femoral artery endothelial function. Physiol Rep 2019; 7: e14190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ranasinghe CD, Ranasinghe P, Jayawardena R, et al. Physical activity patterns among South-Asian adults: a systematic review. Int J Behav Nutr Phys Act 2013; 10: 116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chung N, Park MY, Kim J, et al. Non-exercise activity thermogenesis (NEAT): a component of total daily energy expenditure. J Exerc Nutrition Biochem 2018; 22: 23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta N, Hallman DM, Mathiassen SE, et al. Are temporal patterns of sitting associated with obesity among blue-collar workers? A cross sectional study using accelerometers. Bmc Public Health 2016; 16: 148. DOI:10.1186/s12889-016-2803-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Betts JA, Smith HA, Johnson-Bonson DA, et al. The energy cost of sitting versus standing naturally in man. Med Sci Sports Exerc 2019; 51: 726–733. [DOI] [PubMed] [Google Scholar]
- 25.Saunders TJ, Atkinson HF, Burr J, et al. The acute metabolic and vascular impact of interrupting prolonged sitting: a systematic review and meta-analysis. Sports Med 2018; 48: 2347–2366. [DOI] [PubMed] [Google Scholar]
- 26.Vancampfort D, Hallgren M, Schuch F, et al. Sedentary behavior and depression among community-dwelling adults aged ≥50 years: Results from the Irish longitudinal study on ageing. J Affect Disord 2020; 262: 389–396. [DOI] [PubMed] [Google Scholar]
- 27.Höglund E, Øverli Ø, Winberg S.Tryptophan metabolic pathways and brain serotonergic activity: a comparative review. Front Endocrinol (Lausanne) 2019; 10: 158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen P, Mao L, Nassis GP, et al. Wuhan coronavirus (2019-nCoV): the need to maintain regular physical activity while taking precautions. J Sport Health Sci 2020; 9: 103–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dempsey PC, Matthews CE, Dashti SG, et al. Sedentary Behavior and Chronic Disease: Mechanisms and Future Directions. J Phys Act Health 2020; 17: 52-61. DOI:10.1123/jpah.2019-0377 [DOI] [PubMed] [Google Scholar]
- 30.Golightly YM, Allen KD, Ambrose KR, et al. Physical activity as a vital sign: a systematic review. Prev Chronic Dis 2017; 14: E123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henson J, Davies MJ, Bodicoat DH, et al. Breaking up prolonged sitting with standing or walking attenuates the postprandial metabolic response in postmenopausal women: a randomized acute study. Dia Care 2016; 39: 130–138. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-scm-10.1177_0036933020946336 for Sedentarism and chronic disease risk in COVID 19 lockdown – a scoping review by Baskaran Chandrasekaran and Thiru Balaji Ganesan in Scottish Medical Journal