Abstract
Aim
The aim of this study was to describe the overall sleep quality, sleep patterns and severity of sleep difficulties among nursing faculty using the Pittsburgh Sleep Quality Index (PSQI).
Design
Cross‐sectional descriptive and correlational study.
Methods
A survey of faculty recruited from Texas Board of Nursing approved colleges/schools was used. A purposive, convenience sample of 105 faculty completed the PSQI, a reliable and valid instrument, in an online setting. Data was collected from January 2019 through April 2019.
Results
Nursing faculty reported sleep difficulty across all components, with more problems in sleep latency, sleep disturbances and subjective sleep quality. Overall, 70.5% of participants were reportedly “poor” sleepers, a salient finding. Faculty experienced poor sleep quality across all academic ranks and age groups. Sleep latency and subjective sleep quality were components that presented higher in severity for the youngest faculty.
Keywords: evidence‐based practice, lifestyle, nurses, nursing, nursing faculty, Pittsburgh Sleep Quality Index, sleep, sleep quality, wellness
1. INTRODUCTION
Restorative sleep is a basic condition for enhanced well‐being through the renewal of the body, mind and soul (Helvig et al., 2016). The Sleep Quality Consensus Panel agreed that sleep latency, number of awakenings >5 min, wake after sleep onset and sleep efficiency were appropriate indicators of sleep quality across the life‐span (Ohayon et al., 2017) while Buxton et al. (2009) identified sufficient sleep duration and quality as key components of adequate sleep practices. Epidemiological and laboratory evidence has found that decreased sleep duration and poor sleep quality are associated with several negative health outcomes, such as obesity and chronic disease (Bowman et al., 2019; Chouchou et al., 2013; Zuraikat et al., 2020). Among health science students, healthcare workers and emergency personnel, poor sleep quality and sleep deficiencies have been linked to decreased work performance, poor decision‐making, medical errors, personal health challenges and burnout (Greeson et al., 2015; Melnyk, 2020; Wolkow et al., 2015; Xu et al., 2016). There has been some research on sleep quality among nurses (Fang & Li, 2015) and nursing professors’ quality of life (Cruz et al., 2015), but very little research about nursing faculty.
2. BACKGROUND
There has been a significant amount of research on the impact of irregular work schedules, such as shiftwork, on sleep among nurses. Several studies using the Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1989) in nurses reported poor quality of sleep for shift workers in the USA (Colditz et al., 2016), Taiwan (Lee et al., 2015), Turkey (Baskent et al., 2017), Ankara (Karahan et al., 2020), and Italy (Giorgi et al., 2017). Poor sleep quality has been associated with insomnia and emotional disturbances (Huang & Zhu, 2020; Lee et al., 2015), and sleep deprivation, irregular sleep patterns and sleepiness were significant issues for shiftwork nurses (Debbia et al., 2021; Zhang et al., 2016). In a systematic review, longer shift patterns, such as consecutive night shifts, were associated with poor sleep quality and fatigue (Querstret et al., 2020). Melnyk’s et al. (2018) study also reported poorer mental and physical health in nurses who work longer shifts. Research has also shown that shiftwork is associated with sleep deprivation and a decrease in psychomotor skills, attention, concentration, processing speed and quality of performance (Kaliyaperumal et al., 2017; Karahan et al., 2020). Medical errors have been linked to sleep disturbances and fatigue (Karahan et al., 2020) and hypersomnolence, excessive daytime sleepiness, have been associated with increased risk of accidents (Garbarino et al., 2016).
The work of nursing faculty involves clinical practice, academic responsibilities and a heavy workload, all likely to impact their work‐life balance and sleep (Fang & Li, 2015; Santos et al., 2019). Mintz‐Binder and Sanders (2012) described the workload demands of 242 associate degree nursing program directors in the USA and their association with sleep problems, decreased overall physical health and burnout. A study of non‐nursing university professors working full time found that females and faculty between ages 45 and 54 reported more frequent fatigue, inability to sleep and poor concentration than males and those 35–44 years old (Tacca Huamán & Tacca Huamán, 2019). These few studies indicate the need to examine sleep quality and the extent of sleep difficulties among nursing faculty. The significance of this study was to address this gap and contribute to building an evidence base that will guide future research and interventions to mitigate potential negative implications of sleep difficulties among nursing faculty. This study was conducted to be the foundational work in evaluating sleep quality among nursing faculty leading to a larger study with a more diverse population.
2.1. Research question
The purpose of this study was to describe the overall sleep quality, sleep patterns and severity of sleep difficulties among nursing faculty using the PSQI and examine demographic factors. The study aims were to (a) describe the overall sleep quality and sleep patterns of nursing faculty using the component scores of the PSQI and (b) describe the severity of sleep difficulties in this sample (in terms of poor and good sleepers).
3. THE STUDY
3.1. Design
The study design was a cross‐sectional descriptive and correlational study of sleep quality.
3.2. Methods
3.2.1. Participants
A survey of nursing faculty recruited from Texas Board of Nursing approved colleges or schools of nursing was used to conduct a cross‐sectional descriptive and correlational study of sleep quality. The Institutional Review Board from the University approved the study, which was conducted between January and April of 2019. Inclusion criteria were the following: (a) nursing faculty who worked in a Texas Board of Nursing approved college or school of nursing, (b) 21 years of age or older and (c) able to read and understand English. Pregnant women were also eligible.
Recruitment to participate in the nursing faculty sleep quality study began with development of a purposive sampling of nursing faculty emails from accredited schools and colleges in Texas. Processes in developing the list included email requests sent to deans and directors of accredited Texas Board of Nursing programs and direct email invitations to faculty. This procedure yielded 681 nursing faculty email addresses. A cover letter and consent were sent by the researcher via email to eligible faculty. Among the 681 targeted faculty, 126 accessed the survey using a Survey Monkey password protected account. Electronic consent had to be provided before the online survey would advance. Of the 126 respondents, 21 did not complete all components required for data inclusion, resulting in a final sample of 105 (15.42% response rate). This study was motivated by the lack of information surrounding sleep habits in nursing faculty to eventually study health consequences of nursing faculty. We had ample sample size to estimate response rates in this study and will be able to use results from this study to aid in designing a future hypothesis‐driven study.
3.3. Data collection
3.3.1. Procedures and instruments
The study used Survey Monkey software to collect nursing faculty data on basic demographics and a validated measure of sleep quality. A secure, reliable and encrypted website was used to host the survey and collect the data. After consent was obtained, a greeting script from the researcher was presented which contained instructions for filling out the survey. The greeting script was followed by the Demographic Form, and PSQI survey. Each subject created their own five‐digit self‐assigned identification number, which appeared at the top of the demographic form. The study data were encrypted for added security. The survey allowed only one attempt. A final page displayed a thank you message for completing the survey with an option for eligibility to receive one of eight $25 Visa gift cards upon completion. All survey questions had to be completed to be eligible for a gift card. Two‐week and 3‐day reminders were sent after the beginning of the study, and again at the 1‐day mark for completion of the survey. Gift cards were not issued until the study was completed.
3.3.2. Demographic form
Participants filled out basic demographic information including their gender, age range, race/ethnicity, employment status and academic rank.
3.3.3. Pittsburgh Sleep Quality Index
The PSQI (Buysse et al., 1989) is a widely used self‐report questionnaire that assesses overall sleep quality and sleep components along seven domains based on the past month: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication and daytime dysfunction. The PSQI consists of 19 items, most of them with a Likert response format. Items are combined to produce the component scores using authors’ recommended formulas. Each derived component has a range from 0–3 whereby “0” indicates no sleep difficulties and “3” represents more severe sleep problems. For instance, the daytime dysfunction score is the sum score on two items (how often taking medication to help sleep; how often having trouble staying awake during daily activities such as driving and eating), coded on the 0–3 scale (0 = 0, 1–2 = 1, 3–4 = 2, and 5–6 = 3). The subjective sleep quality component (1 item) refers to the person's rating of their overall sleep quality on a scale of 0 (very good) to 3 (very bad). Sleep latency represents how long it takes for the person to go to sleep, whereas sleep duration refers to how many hours of sleep a person actually gets at night. Habitual sleep efficiency is calculated as a ratio of number of hours slept/number of hours spent in bed multiplied by 100, which translates into a percentage (˃85% indicates no sleep problems, scored as “0”; <65% indicates more severe sleep problems, scored as “3”). The sleep disturbances component is derived from the sum of eight item scores indicating how often the person had trouble sleeping (e.g., waking up during the night, having pain or feeling too cold/hot). The global PSQI score is the sum of the seven components and ranges from 0–21, with a total score above 5 indicating a “poor” sleeper. The PSQI also includes an open question on “other reasons” for having trouble sleeping. The original authors found a diagnostic sensitivity of 89.6% and specificity of 86.5% in differentiating poor and good sleepers; a sensitivity of 98% and specificity of 55% were found in the Chinese population (Tsai et al., 2005).
The PSQI has been used in numerous studies of adult populations internationally to assess sleep quality and its relation to a variety of outcomes (Bowman et al., 2019; Huang & Zhu, 2020; Karahan et al., 2020). For instance, the PSQI was used as part of the Midlife in the United States (MIDUS) study, which includes the general adult population. A higher global PSQI score was associated with a higher risk of depressive symptoms (Huang & Zhu, 2020). Baseline data for the American Heart Association (AHA) Go Red Women prospective cohort study (Zuraikat et al., 2020) also included the PSQI, and results indicated that poor sleep quality was associated with greater food intake and lower quality diet, which are risk factors for cardiovascular disease. The PSQI was also used in a large cross‐sectional community‐based study of the Korean Medicine Data Center which showed an association between sleep problems and digestive symptoms (Hyun et al., 2019). In academic populations, the PSQI has been primarily utilized in studies with students, including nursing students (Liu et al., 2021). A recent literature review of determinants of sleep quality in college students (Wang & Biro, 2021) found that physical activity and healthy social relations related to improved sleep quality, while caffeine intake, stress and irregular sleep‐wake patterns were associated with decreased sleep quality.
A comprehensive meta‐analysis of observational studies of sleep quality among medical students in four continents (Rao et al., 2020) found a pooled prevalence of poor sleep quality of 52.7% using the PSQI and a mean PSQI score of 6.1. Sleep quality was more prevalent in Europe and the Americas. Very few studies have examined sleep quality among university faculty using the PSQI. A few studies have been conducted in Brazil and Portugal, which investigated contributing factors to sleep quality among university professors and related poor sleep quality to physical and emotional symptoms (Crepaldi & Carvalhais, 2020; Santos et al., 2019; Silva et al., 2018; Sousa et al., 2018).
3.4. Analysis
Overall sleep quality as measured by the global PSQI score was assessed numerically and nominally (“good” vs. “poor” sleeper) in terms of severity of sleep difficulties. Numerical data for PSQI and its component scores were presented as means (M), standard deviations (SD), and quartiles and ranges. Component scores (0–3) are ordinal categories; thus, quartiles, 25th, 50th (median) and 75th percentiles, and/or interquartile ranges (IQR = 75th percentile–25th percentiles) are appropriate to report measures of central tendency and spread. Overall sleep quality was defined based on a cut‐off of 5 on the global PSQI score (poor sleepers: >5; good sleepers: ≤5). Spearman correlation was used to assess the relationship between component scores and overall PSQI. From the demographic questionnaire, age was reported in six categorical ranges (under 25; 26–35; 36–45; 46–55; 56–65; and >66 years) and further collapsed into the following four age groups deemed meaningful for analysing sleep patterns in this population: ≤45; 46–55; 56–65, and ≥66 years. Among relevant demographic populations, Kruskal–Wallis test was used to evaluate PSQI scores (numerical) and Fisher's exact test was used to evaluate severity of sleep difficulties (nominal). Overall differences in severity of sleep difficulties among all nursing faculty were analysed using the binomial test of proportions. All statistical tests were conducted using an alpha level of 0.05. Statistical analysis was performed using Stata statistical software, version 14.0 (StataCorp., 2015).
3.5. Validity and reliability
Buysse et al. (1989) report an internal consistency reliability (Cronbach's alpha) of 0.83 for the seven components. A recent study conducted among 923 Chinese nurses found a Cronbach's alpha reliability coefficient of 0.73 (Li et al., 2019). In the current sample of nursing faculty, the estimated Cronbach's alpha coefficient was 0.68, with domain by overall score correlations ranging from 0.446–0.736.
4. RESULTS
4.1. Characteristics of sample
Nursing faculty demographics and characteristics are presented in Table 1. The majority of the nursing faculty was female (97%), white (82.9%) and worked full time (93%). Among the faculty sampled, the represented age groups consisted of ≤45 years (21.9%) up to ≥66 years (18.1%), with 56–65 year olds representing the majority of the sample (37.1%). The distribution of academic rank was as follows: assistant or associate professor (48%); professor (20%); clinical assistant or clinical associate professor (20%); clinical professor (~4%); and instructor or lecturer (8%). Among the faculty surveyed, 54% were reportedly non‐tenure track; 22% tenure track and 24% tenured. Among this sample of faculty, 29% (N = 30/105) reported a workload of more than 40 hr per week; 55% (N = 59) reported working 5–15 or more hours on the weekend on work‐related expectations; and 15% reportedly work 40–50 hr/week and 5–15 or more hours on the weekend. Further, among those working >40 hr, 53% (16/30) reported spending 5–15 or more hours on the weekend working.
TABLE 1.
Characteristics of the nursing faculty sample (N = 105)
| Characteristics | N (%) |
|---|---|
| Gender | |
| Female | 102 (97.1) |
| Male | 3 (2.9) |
| Age (years) | |
| <45 | 23 (21.9) |
| 46–55 | 24 (22.9) |
| 56–65 | 39 (37.1) |
| >66 | 19 (18.1) |
| Race | |
| White | 87 (82.9) |
| Hispanic/Latino | 8 (7.6) |
| African American | 4 (3.8) |
| Asian | 2 (1.9) |
| Other | 4 (3.8) |
| Work status | |
| Full time | 99 (94.3) |
| Part time | 2 (1.9) |
| Adjunct faculty | 4 (3.8) |
| Academic rank | |
| Assistant Professor | 36 (34.3) |
| Associate Professor | 15 (14.3) |
| Professor | 17 (16.2) |
| Clinical Assistant Professor | 3 (2.8) |
| Clinical Associate Professor | 4 (3.8) |
| Clinical Professor | 7 (6.7) |
| Instructor | 2 (1.9) |
| Lecturer | 21 (20.0) |
4.2. Overall sleep quality and patterns
The global PSQI score for sleep quality among nursing faculty was on average 8.14 (SD = 3.81) (range: 1–17), with a median score of 7 and IQR: six points (Table 2). While sleep quality components range from 0–3, not all values were represented across all components. Median (IQR) for each domain is estimated as: subjective sleep quality: 1 (1); sleep latency: 1 (2); sleep duration: 1 (2); habitual sleep efficiency: 0 (1); sleep disturbances: 2 (1); use of sleep medication: 1 (3); and daytime dysfunction: 1 (0). These scores indicate some level of sleep difficulty across all components in this study population, with the exception of habitual sleep efficiency.
TABLE 2.
Overall sleep quality and components among nursing faculty (N = 105)
| PSQI component/Domain | M (SD) | Mdn (25th, 75th) a | Range (min, max) |
|---|---|---|---|
| Global PSQI score | 8.14 (3.81) | 7 (5,11) | 1, 17 |
| Subjective sleep quality | 1.24 (0.66) | 1 (1,2) | 0, 3 |
| Sleep latency | 1.56 (1.06) | 1 (1,3) | 0, 3 |
| Sleep duration | 0.92 (1.01) | 1 (0,2) | 0, 3 |
| Habitual sleep efficiency | 0.67 (0.94) | 0 (0,1) | 0, 3 |
| Sleep disturbance | 1.54 (0.56) | 2 (1,2) | 1, 3 |
| Use of sleep medication | 1.15 (1.29) | 1 (0, 3) | 0, 3 |
| Daytime dysfunction | 1.06 (0.74) | 1 (1,1) | 0, 3 |
Abbreviation: PSQI, Pittsburgh Sleep Quality Index.
25th and 75th percentile.
Figure 1 displays the proportion of responses (0–3) for each domain, with “0” denoting lack of sleep problems in that domain and “3” highly problematic. Nursing faculty were observed to self‐report varying levels of sleep problems across all sleep domains. The proportion of nursing faculty reporting any indication of sleep problems (at least somewhat) was significantly higher than those not likely to have sleep difficulty (p < .05) for components of subjective sleep quality (89.2%), sleep latency (80%) and daytime dysfunction (79%), with 100% of nursing faculty reporting problems in sleep disturbance. Sleep components that had a larger proportion of higher scores were sleep latency (24%) and likely to use sleep medication (30%).
FIGURE 1.
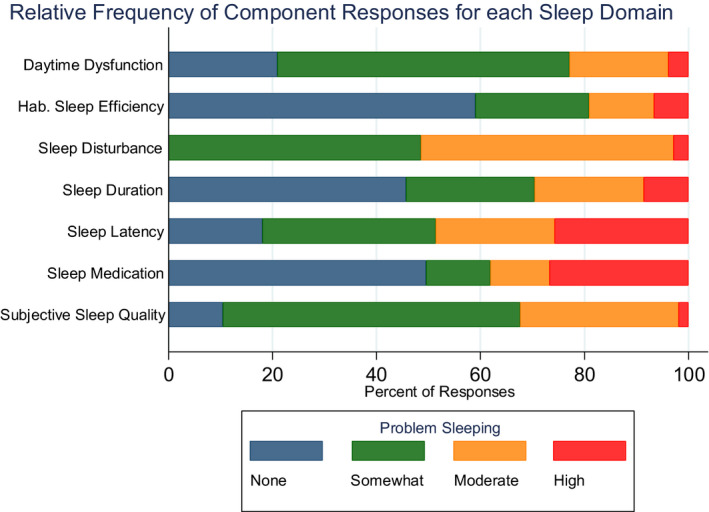
Relative Frequency of Component Responses for each Sleep Domain among Nursing Faculty (N = 105). Note. Figure 1 displays the proportion of response categories (0–3) for each sleep domain, with ‘0’ representing no sleep problems and ‘3’ indicating highly problematic in that domain. Across each domain (y axis), the stacked bars represent each response added up to 100%, and the width of each colour/bar represents the proportion of responses
Global PSQI scores were lower among the middle age groups (46–55 and 56–65 year olds) and, on average, were worse among the youngest and oldest age groups (Table 3). However, there was not a statistically significant difference in global PSQI scores across age groups (p = .204). Similar results were found when analysing sleep components across age groups (p > .05), but there tended to be a marginal relationship between subjective sleep quality and age (p = .053).
TABLE 3.
Distribution of Pittsburgh Sleep Quality Index component and global PSQI scores by age groups among nursing faculty (N = 105)
| PSQI |
<45 N = 23 |
46–55 years N = 24 |
56–65 years N = 39 |
>66 years N = 19 |
p |
|---|---|---|---|---|---|
|
M (SD) Mdn (IQR) |
M (SD) Mdn (IQR) |
M (SD) Mdn (IQR) |
M (SD) Mdn (IQR) |
||
| Subjective sleep quality |
1.52 (0.73) 2 (1) |
1.21 (0.51) 1 (0.5) |
1.05 (0.65) 1 (0) |
1.32 (0.67) 1 (1) |
.053 |
| Sleep latency |
1.91 (1.08) 2 (2) |
1.25 (1.11) 1 (2) |
1.51 (1.02) 1 (1) |
1.63 (1.01) 2 (1) |
.198 |
| Sleep duration |
1.13 (1.18) 1 (2) |
0.75 (0.90) 0.5 (1) |
0.79 (0.98) 0 (1) |
1.16 (0.96) 1 (2) |
.363 |
| Habitual sleep efficiency |
0.83 (1.23) 0 (2) |
0.83 (0.87) 1 (1) |
0.51 (0.85) 0 (1) |
0.58 (0.77) 0 (1) |
.398 |
| Sleep disturbance |
1.39 (0.50) 1 (1) |
1.67 (0.48) 2 (1) |
1.46 (0.55) 1 (1) |
1.74 (0.65) 2 (1) |
.118 |
| Use of sleep medication |
1.30 (1.30) 1 (3) |
1.25 (1.36) 1 (3) |
(1.32) 0 (3) |
1.16 (1.21) 1 (2) |
.748 |
| Daytime dysfunction |
1.22 (0.67) 1 (1) |
1.08 (0.78) 1 (0.5) |
0.87 (0.73) 1 (1) |
1.21 (0.79) 1 (1) |
.196 |
| Global PSQI score |
9.30 (4.44) 9 (8) |
8.04 (3.58) 7 (6) |
7.21 (3.65) 7 (5) |
8.79 (3.38) 9 (6) |
.204 |
Abbreviation: PSQI, Pittsburgh Sleep Quality Index.
4.3. Severity of sleep difficulties
Study results demonstrated that a large percentage (70.5%) of the nursing faculty reported as poor sleepers (total PSQI>5) (p < .05) (Figure 2). No significant effects of age group were found to be associated with severity of sleep difficulties (“poor” vs. “good” sleepers; p = .835) as depicted in Figure 2. Severity of sleep difficulties did not significantly differ across gender, race, work status or academic rank (p > .05).
FIGURE 2.
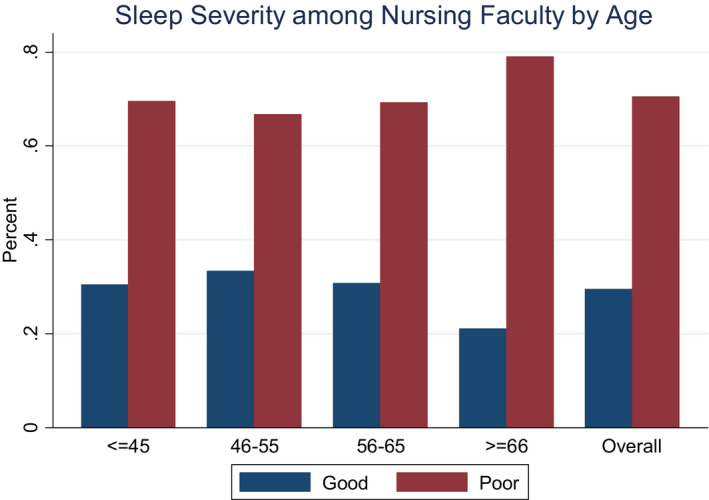
Severity of Sleep Difficulties among Nursing Faculty by Age (N = 105). Note. Global PSQI score is displayed nominally into sleep severity groups: Good sleeper ‐ global PSQI ≤ 5; Poor sleeper ‐ global PSQI > 5. Bar graphs represent the distribution of severity of sleep difficulties across age groups as well as among all nursing faculty
5. DISCUSSION
The aim of this study was to describe the overall sleep quality, sleep patterns and severity of sleep difficulties among nursing faculty using the PSQI. Our results showed that over 70.5% of nursing faculty reported poor sleep quality (“poor sleepers”) as compared to 51% of nursing students (Aung et al., 2016) and 37% of an urban adult population using the PSQI (Asghari et al., 2012). A possible contributing factor to the overall poor sleep is the 6%–8% of full‐time vacant faculty positions in Texas resulting in a faculty shortage during 2015–2016 (American Association of Colleges of Nursing [AACN], 2019; Texas Team Education Committee Taskforce Membership, 2017). The mean global PSQI score of 8.14 (SD = 3.81) found for the current sample of nursing faculty is similar to the night shift nurses’ global PSQI score of 8.28 (SD = 3.04) in Baskent et al.’s study (2017). We found that the majority of faculty reported sleep problems in each component of the PSQI, similar to nurses working irregular shifts (Querstret et al., 2020).
Sleep patterns, based on PSQI component scores, provide evidence that sleep latency (how long to fall asleep), sleep disturbance (things that cause trouble sleeping) and subjective sleep quality (good or bad) were “more severe” compared to the other component scores. Item level responses provided some explanation. For sleep latency, faculty reported a median of 20 min to fall asleep with a range of 0–150 min. Respondents wrote: “Anxiety ‐ can't shut down my list of things to do,” “too much thinking, worrying about work,” “constantly thinking of ‘life’ and everything I need to do,” and “my mind was busy with responsibilities.” For sleep disturbances, respondents wrote: “mind wakes me up – thinking,” “awake and cannot fall back asleep,” “pets in room, spouse snores, mind is racing,” and “children or pets waking me up.” The nursing faculty's comments seem to indicate that both work stress and family issues are interfering with their ability to fall asleep and stay asleep which impacts their subjective assessment of their sleep quality.
Biological, physiological, physical, psychological, social relationships and sleeping environment are confounding factors associated with poor quality of sleep, as reported by participant comments. Circadian rhythm sleep disorders, such as shift work type, jet lag and sleep–wake disorders related to medical conditions, are a few factors impacting quality sleep (Sadock et al., 2015). Moreover, sleep‐related movement disorders, parasomnias and environmental sleep disorders can impede restorative sleep. Sadock et al. (2015) report noise, heat, cold, light, bed partner noise and activity, or perceived danger have been identified as contributory to sleep disorder secondary to environmental factors.
Our findings showed no significant differences across gender or ethnicity, although replication of these findings with more diverse samples is warranted. Although the associations between age and the global PSQI score or its components were not statistically significant, there are some noteworthy patterns that merit future exploration. The sleep duration (actual sleep at night) ranged from 3–10 hr for all groups. The ≤45 age group reported a median of 6 hr falling short of the National Sleep Foundation’s (2015) recommended 7–9 hr of sleep. They reported the most severe global PSQI score of 9.30 compared to 7.21–8.79 global PSQI in the other age groups.
Similar to our faculty in this age group, Lee et al. (2017) found that adults (mean age of 45 years) with children slept an average of 6.4 hr a night and experienced sleep latency due to daily stressors of work–family balance. Sleep restrictions, less than the usual sleep recommendations for a specific age group, were linked to inflammatory, hormonal, mood states/psychological responses and psycho‐physiological stress responses (Lee et al., 2017; Wolkow et al., 2015). Therefore, our youngest faculty members may be at increased risk of cumulative effects harmful to their health. Finding the aetiologies and targeted interventions of the nursing faculty's poor sleep quality must be individualized.
5.1. Implications for nursing education
Melnyk (2020) reported burnout, depression and suicide are a public health epidemic worldwide. Nursing faculty are a subset of the larger nursing healthcare profession who experience job‐related stress and burnout in their dual roles as clinicians and academicians. It is suggested that faculty working at a university are at risk of poor sleep due to the psychological demands of the job, such as workload, and compensations, such as job instability (contract work) and undesirable changes (Tacca Huamán & Tacca Huamán, 2019). Emotional influences, such as mood changes, and social influences, i.e., the levels of empathy and personal distress, have been associated with the quality of sleep (Wu et al., 2020). Some possible causes from the literature are irregular schedules, mental health issues, such as, anxiety and depression, chronic health conditions, such as, a respiratory condition, gastroesophageal reflux disease, or pain, and sleep apnea.
5.2. Implications for future research
The results of this study brought attention to the overall poor sleep quality reported by nursing faculty which merits further research, especially in the USA where research on this topic is scarce. Research in South America and Europe suggests that poor sleep quality among faculty is a global problem (Amaro & Dumith, 2018). However, sleep problems with faculty may vary in different parts of the world based on the country's culture, academic culture, healthcare system and individual characteristics. More research is needed to explore these differences cross‐culturally. In order to produce more generalizable findings in the USA, exploration of the differences in the academy of nursing, and expansion of the study outside Texas and the USA are needed.
Increased knowledge is needed in several areas of sleep quality research among nursing faculty. Research that examines predictors of sleep quality among nursing faculty is crucial to developing mitigation strategies that address their unique needs and promote sleep health and well‐being. Future research is needed to address the health implications of sleep quality or lack thereof in this study population that addresses a more diverse demographic and rigorous biological data to relate sleep and health outcomes in a diverse sample of nursing faculty.
Organizational and academic predictors of sleep quality among nursing faculty need to be identified in order to develop and test systems‐level occupational health interventions and academic policies that foster nursing faculty well‐being. There has been an increased awareness among nursing scientists of the need to emphasize occupational factors in their nursing research on work and health (Castro et al., 2017). Potential predictors are faculty workload, including the balance among teaching, research and service, variations in sleep quality according to academic position (tenure, non‐tenure and clinical tracks), flexibility of schedules, organizational climate, mentoring support, promotion policies and availability of employee well‐being programs (Sousa et al., 2018; Ujvarine et al., 2020). At the individual level, physical activity, eating habits, social support, coping style and resilience are factors that have been associated with sleep quality in nurses and healthcare students, and can be examined about nursing faculty (Wang & Biro, 2021). More knowledge is also needed in terms of the impact of sleep quality of nursing faculty on teaching and performance outcomes.
In terms of research methodology, most studies on sleep quality among nurses and nursing faculty have relied on self‐report measures such as the PSQI. Although these measures have proved validity, several studies have demonstrated that estimates based on self‐reports of sleep quality may differ from more objective measures, such as via polysomnography and actigraphy (Mathews et al., 2018), the combination of objectively and subjectively assessed sleep being recommended (Bowman et al., 2019).
5.3. Limitations
This study has limitations that may affect generalizability of findings including a homogenous sampling of white, females, working full‐time as faculty members, although it reflects the basic demographics of nursing faculty. There is possible selection bias with using a purposive sampling from schools of nursing in Texas and with invitations being forwarded by a person holding a position of authority, such as a Dean or Director of a nursing program. PSQI is a well‐validated measure of sleep quality, but may be limited by retrospective self‐report biases. The response rate was low at 15% for the online survey which is slightly below the 20%–30% expected rate (Sauermann & Roach, 2013). Self‐selection bias could also have inflated the results by respondents that were interested in reporting their sleep problems. No definitive conclusions can be drawn from this study without a larger sample of faculty with more diversity.
6. CONCLUSION
Nursing faculty in this study reported poor sleep quality, which is likely to compromise their health and well‐being. Work–family conflict was identified by faculty as interfering with their sleep and is important factors to address in intervention development. Evidence‐based interventions to balance personal and work life, as described by Melnyk (2020), are needed. Developing a culture of wellness in academia, which promotes self‐care and sleep health, is essential to sustaining healthy nursing faculty and academic programs.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
AUTHOR CONTRIBUTIONS
SC involved in study design and acquisition of data; SC, JB, CB and TM took part in analysis and interpretation of data; SC, JB, CB and TM participated in drafting of the manuscript; SC, JB, CB and TM involved in critical revisions of the manuscript for important intellectual content. All authors read and approved the final manuscript.
ETHICAL APPROVAL
This study was reviewed and approved by the University's Institutional Review Board (IRB). The greeting script, demographic form, data collection procedures and questionnaire were approved by the IRB. The IRB identification number STUDY00001376 was approved. Participation in the study was voluntary. Each study participant self‐selected their own participant identification number. There were no foreseeable risks related to the procedures conducted as part of this study. Data were encrypted for additional security.
ACKNOWLEDGMENTS
This work was supported by a grant from the Phi Chi Chapter of Sigma. We wish to thank the Nursing faculty who participated in this study, Earline Moreland from the University of Houston College of Nursing who assisted with data management, Rachel Helbing and Stefanie Lapka with the University of Houston Libraries.
Cox, S. D. , Benoit, J. S. , Brohard, C. L. , & McIntyre, T. M. (2022). Evaluation of sleep quality among nursing faculty: Application of the Pittsburgh Sleep Quality Index—A descriptive correlational study. Nursing Open, 9, 339–348. 10.1002/nop2.1067
Funding information
The annual research award by Phi Chi Chapter of Sigma Theta Tau International Honor Society of Nursing provided funding support for this study. Grant award number 000178275
DATA AVAILABILITY STATEMENT
Research data are not shared. The data are not publicly available due to privacy and compliance with the Institutional Review Board protocol approval.
REFERENCES
- Amaro, J. , & Dumith, S. (2018). Sonolência diurnal excessiva e qualidade de vida relacionada à saúde dos professores universitários [Diurnal somnolence and quality of life associated with the health of university professors]. Jornal Brasileiro De Psiquiatria, 67(2), 94–100. 10.1590/0047-2085000000191 [DOI] [Google Scholar]
- American Association of Colleges of Nursing . (2019). Special survey on vacant faculty positions for academic year 2018‐2019. 2018 Faculty Vacancy Survey Report. Retrieved from https://www.aacnnursing.org/Portals/42/News/Surveys‐Data/Vacancy18.pdf [Google Scholar]
- Asghari, A. , Farhadi, M. , Kamrava, S. K. , Ghalehbaghi, B. , & Nojomi, M. (2012). Subjective sleep quality in urban population. Archives of Iranian medicine, 15(2), 95–98. [PubMed] [Google Scholar]
- Aung, K. T. , Nurumal, M. S. , SitiNurhizwany, Z. (2016). Sleep quality and academic performance of nursing students. Journal of Nursing and Health Science, 5(6), 145–149. 10.9790/1959-050601145149 [DOI] [Google Scholar]
- Baskent, G. , Keskin, N. O. , & Gokçay, G. (2017). The quality of sleep in nurses. European Respiratory Society, 3, 1–5. 10.1183/23120541 [DOI] [Google Scholar]
- Bowman, M. , Duggan, K. , Brindle, R. , Kline, C. , Krafty, R. , Thayer, J. , & Hall, M. (2019). Prospective associations among objectively and subjectively assessed sleep and the metabolic syndrome. Sleep Medicine, 58, 1–6. 10.1016/j.sleep.2019.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buxton, O. , Quintiliani, L. , Yang, M. , Ebbeling, C. , Stoddard, A. , Pereira, L. , & Sorensen, G. (2009). Association of sleep adequacy with more healthful food choices and positive workplace experiences among motor freight workers. American Journal of Public Health, 99(s3), s636–s643. 10.2105/AJPH.2008.158501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse, D. J. , Reynolds, C. F. III , Monk, T. H. , Berman, S. R. , & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Journal of Psychiatric Research, 28(2), 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Castro, A. , McCauley, L. , & Hong, O. (2017). Work, health, and nursing research. Nursing Research, 66(6), 417–418. 10.1097/NNR.0000000000000246 [DOI] [PubMed] [Google Scholar]
- Chouchou, F. , Pichot, V. , Pepin, J. L. , Tamisier, R. , Celle, S. , Maudoux, D. , Garcin, A. , Levy, P. , Barthelemy, J. C. , & Roche, F. (2013). Sympathetic overactivity due to sleep fragmentation is associated with elevated diurnal systolic blood pressure in healthy elderly subjects: The PROOF‐SYNAPSE study. European Heart Journal, 34(28), 2122–2131, 2131a. 10.1093/eurheartj/eht208 [DOI] [PubMed] [Google Scholar]
- Colditz, G. , Philpott, S. E. , & Hankinson, S. E. (2016). The impact of the nurses’ health study on population health: Prevention, translation, and control. American Journal of Public Health, 106, 1540–1545. 10.2105/AJPH.2016.303343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crepaldi, T. , & Carvalhais, J. (2020). A contribuição da má qualidade do sono na qualidade de vida no trabalho de professores: Uma revisão [The contribution of bad sleeping quality on professors work life: A review]. Brazilian Journal of Development, 6(10), 75044–75057. 10.34117/bjdv6n10-070 [DOI] [Google Scholar]
- Cruz, A. , Almeida, N. , Fialho, A. , Rodrigues, D. , Figueiredo, J. , & Oliveira, A. (2015). Perception of female nursing professors about their quality of life. Revista Da Rede De Enfermagem do Nordeste, 16(3), 382–390. 10.15253/2175-6783.2015000300011 [DOI] [Google Scholar]
- Debbia, F. , Medina‐Valverde, M. , García‐Arcos, A. , Garrido‐Gutiérrez, A. , Rodríguez‐Borrego, M. , & López‐Soto, P. (2021). Chronotype, general health and quality of sleep in a population of Spanish nurses. Revista Da Escola De Enfermagem USP, 55, e03752. 10.1590/S1980-220X2020010903752 [DOI] [PubMed] [Google Scholar]
- Fang, R. , & Li, X. (2015). A regular yoga intervention for staff nurse sleep quality and work stress: A randomised controlled trial. Journal of Clinical Nursing, 24, 3374–3379. 10.1111/jocn.12983 [DOI] [PubMed] [Google Scholar]
- Garbarino, S. , Lanteri, P. , Durando, P. , Magnavita, N. , & Sannita, W. (2016). Co‐morbidity, mortality, quality of life and the healthcare/welfare/social costs of disordered sleep: A rapid review. International Journal of Environmental Research and Public Health, 13(8), 1–15. 10.3390/ijerph13080831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giorgi, F. , Mattei, A. , Notanicola, I. , Petrucci, C. , & Lancis, L. (2017). Can sleep quality and burnout affect the job performance of shift‐work nurses? A hospital cross‐sectional study. Journal of Advanced Nursing, 74, 698–708. 10.1111/jan.13484 [DOI] [PubMed] [Google Scholar]
- Greeson, J. M. , Toohey, M. J. , & Pearce, M. J. (2015). An adapted, four‐week mind‐body skills group for medical students: Reducing stress, increasing mindfulness, and enhancing self‐care. Explore, 11(3), 186–192. 10.1016/j.explore.2015.02.003 [DOI] [PubMed] [Google Scholar]
- Helvig, A. , Wade, S. , & Hunter‐Eades, L. (2016). Rest and the associated benefits in restorative sleep: A concept analysis. Journal of Advanced Nursing, 72(1), 62–72. 10.1111/jan.12807 [DOI] [PubMed] [Google Scholar]
- Huang, Y. , & Zhu, M. (2020). Increased global PSQI score is associated with depressive symptoms in an adult population from the United States. Nature and Science of Sleep, 12, 487–549. 10.2147/NSS.S256625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyun, M. , Baek, Y. , & Lee, S. (2019). Association between digestive symptoms and sleep disturbance: A cross‐sectional community‐based study. BMC Gastroenterology, 19, 34. 10.1186/s12876-019-0945-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaliyaperumal, D. , Elango, Y. , Alagesan, M. , & Santhanakrishanan, I. (2017). Effects of sleep deprivation on the cognitive performance of nurses working in shift. Journal of Clinical and Diagnostic Research, 11(8), CC01–CC03. 10.7860/JCDR/2017/26029.10324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karahan, A. , Abbasoğlu, A. , Uğurlu, Z. , Işık, S. , Kılıç, G. , & Elbaş, N. (2020). Determination of sleep quality, fatigue, and concentration in nurses according to their shifts and chronotype. Journal of Psychiatric Nursing, 11(2), 98–105. 10.14744/phd.2019.90277 [DOI] [Google Scholar]
- Lee, C. Y. , Chen, H. C. , Tseng, M. C. , Lee, H. C. , & Huang, L. H. (2015). The relationships among sleep quality and chronotype, emotional disturbance, and insomnia vulnerability in shift nurses. The Journal of Nursing Research, 23(3), 225–235. 10.1097/jnr.0000000000000095 [DOI] [PubMed] [Google Scholar]
- Lee, S. , Crain, T. L. , McHale, S. M. , Almeida, D. , & Buxton, O. M. (2017). Daily antecedents and consequences of nightly sleep. Journal of Sleep Research, 26, 498–502. 10.1111/jsr.12488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Y. , Fang, J. , & Zhou, C. (2019). Work‐related predictors of sleep quality in Chinese nurses: Testing a path analysis model. Journal of Nursing Research, 27(5), 1–10. 10.1097/jnr.0000000000000319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, D. , Kahathuduwa, C. , & Vazsonyi, A. T. (2021). The Pittsburgh Sleep Quality Index (PSQI): Psychometric and clinical risk score applications among college students. Psychological Assessment, 33(9), 816–826. Advance online publication. 10.1037/pas0001027 [DOI] [PubMed] [Google Scholar]
- Matthews, K. , Patel, S. , Pantesco, E. , Buysse, D. , Kamarck, T. , Lee, L. , & Hall, M. (2018). Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self‐reported habitual sleep in a community sample. Sleep Health, 4(1), 96–103. 10.1016/j.sleh.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnyk, B. M. (2020). Burnout, depression and suicide in nurses/clinicians and learners: An urgent call for action to enhance professional well‐being and healthcare safety. Worldviews on Evidence‐Based Nursing, 17(1), 2–5. 10.1111/wvn.12416 [DOI] [PubMed] [Google Scholar]
- Melnyk, B. M. , Orsolini, L. , Tan, A. , Arslanian‐Engoren, C. , Melkus, G. D. , Dunbar‐Jacob, J. , Rice, V. H. , Millan, A. , Dunbar, S. B. , Braun, L. T. , Wilbur, J. E. , Chyun, D. A. , Gawlik, K. , & Lewis, L. M. (2018). A national study links nurses’ physical and mental health to medical errors and perceived worksite wellness. Journal of Occupational & Environmental Medicine, 60(2), 126–131. 10.1097/JOM.0000000000001198 [DOI] [PubMed] [Google Scholar]
- Mintz‐Binder, R. D. , & Sanders, D. L. (2012). Workload demand: A significant factor in the overall well‐being of directors of associate degree nursing programs. Teaching and Learning in Nursing, 7(1), 10–16. 10.1016/j.teln.2011.07.001 [DOI] [Google Scholar]
- National Sleep Foundation (2015). National Sleep Foundation recommends new sleep times. Retrieved from https://www.sleepfoundation.org/press‐release/national‐sleep‐foundation‐recommends‐new‐sleep‐times [Google Scholar]
- Ohayon, M. , Wickwire, E. M. , Hirshkowitz, M. , Albert, S. M. , Avidan, A. , Daly, F. J. , Dauvilliers, Y. , Ferri, R. , Fung, C. , Gozal, D. , Hazen, N. , Krystal, A. , Lichstein, K. , Mallampalli, M. , Plazzi, G. , Rawding, R. , Scheer, F. A. , Somers, V. , & Vitiello, M. V. (2017). National Sleep Foundation’s sleep quality recommendations: First report. Sleep Health, 3(1), 6–19. 10.1016/j.sleh.2016.11.006 [DOI] [PubMed] [Google Scholar]
- Querstret, D. , O’Brien, K. , Skene, D. J. , & Maben, J. (2020). Improving fatigue risk management in healthcare: A systematic scoping review of sleep‐related/fatigue‐management interventions for nurses and midwives. International Journal of Nursing Studies, 106, 1–16. 10.1016/j.ijnurstu.2019.103513 [DOI] [PubMed] [Google Scholar]
- Rao, W. , Li, W. , Qi, H. , Hong, L. , Chen, C. , Li, C. , Ng, C. , Ungvari, G. , & Xiang, Y. (2020). Sleep quality in medical students: A comprehensive meta‐analysis of observational studies. Sleep and Breathing, 24, 1151–1165. 10.1007/s11325-020-02020-5 [DOI] [PubMed] [Google Scholar]
- Sadock, B. , Sadock, V. , & Ruiz, P. (2015). Normal sleep and sleep‐wake disorders: Sleep‐wake disorders. In Pataki C. S. & Sussman N. (Eds.), Kaplan & synopsis of psychiatry: Behavioral sciences/clinical psychiatry, 11th ed. (pp. 536–563). Wolters Kluwer. [Google Scholar]
- Santos, F. , Viana, C. , Melo, L. , Costa, P. , & Ykeda, D. (2019). Sono e fatores de estresse de professores do ensino superior da área da saúde [Sleep and stress in high education teachers of health courses]. ASSOBRAFIR Ciência, 10(1), 21–30. 10.47066/2177-9333.AC.2019.0003 [DOI] [Google Scholar]
- Sauermann, H. , & Roach, M. (2013). Increasing web survey response Increasing web survey response rates in innovation research: An experimental study of static and dynamic contact design features. Research Policy, 42, 273–286. 10.1016/j.respol.2012.05.003 [DOI] [Google Scholar]
- Silva, K. , Marques, A. , Aragão, A. , Gonçalves, A. , Feitosa, A. , Araújo, W. , Custódio, P. , & Assis, E. (2018). Fatores de Risco para as Doenças Cardiovasculares e Qualidade do Sono [Risk Factors for Cardiovascular Diseases and Sleep Quality]. Revista De Enfermagem UFPE Online, 12(10), 2573–2582. 10.5205/1981-8963-v12i10a237489p2573-2582-2018 [DOI] [Google Scholar]
- Sousa, A. , Santos, R. , Silva, R. , Santos, C. , Lopes, V. , & Mussi, F. (2018). Estresse ocupacional e qualidade do sono em docentes da área da saúde [Occupational stress and sleep quality in professors of the health area]. Revista Rene, 19, e33088. 10.15253/2175-6783.20181933088 [DOI] [Google Scholar]
- StataCorp . (2015). Stata statistical software: Release 14. StataCorp LP. [Google Scholar]
- Tacca Huamán, D. R. , & Tacca Huamán, A. L. (2019). Psychosocial risk factors and perceived stress in university professors. Journal of Educational Psychology, 7(3), 339–354. 10.20511/pyr2019.v7n3.304 [DOI] [Google Scholar]
- Texas Team Education Committee Taskforce Membership (2017). The nursing faculty shortage: What is being done in Texas?. Texas Nursing Magazine, 12‐14. Retrieved from https://cdn.ymaws.com/www.texasnurses.org/resource/resmgr/tnm‐pdfs/FacultyShortage_Sum17.pdf [Google Scholar]
- Tsai, P. S. , Wang, S. Y. , Wang, M. Y. , Su, C. T. , Yang, T. T. , Huang, C. J. , & Fang, S. C. (2005). Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Quality of Life Research, 14(8), 1943–1952. 10.1007/s11136-005-4346-x [DOI] [PubMed] [Google Scholar]
- Ujvarine, A. , Gal, M. , Jacabne, E. , Sarvary, A. , Zrinyi, M. , Fuller, N. , & Olah, A. (2020). Staying with nursing: The impact of conflictual communication, stress and organizational problem‐solving. International Nursing Review, 64, 495–500. 10.1111/inr.12619 [DOI] [PubMed] [Google Scholar]
- Wang, F. , & Biro, E. (2021). Determinants of sleep quality in college students: A literature review. Explore, 17, 170–177. 10.1016/j.explore.2020.11.003 [DOI] [PubMed] [Google Scholar]
- Wolkow, A. , Ferguson, S. , Aisbett, B. , & Main, L. (2015). Effects of work‐related sleep restriction on acute physiological and psychological stress responses and their interactions: A review among emergency service personnel. International Journal of Occupational Medicine and Environmental Health, 28(2), 183–208. 10.13075/ijomeh.1896.00227 [DOI] [PubMed] [Google Scholar]
- Wu, J. W. , Yan, D. , Xue‐rong, Z. , Shu‐chang, H. , & Xiang‐Yang, Z. (2020). Burnout in university faculty: An interaction between subjective sleep quality and the OXTR rs2268498 polymorphism. Journal of Affective Disorders, 276, 927–935. 10.1016/j.jad.2020.07.094 [DOI] [PubMed] [Google Scholar]
- Xu, J. , Zhu, Y. , Fu, C. , Sun, J. , Li, H. , Yang, X. , Li, W. , Qin, W. , Shi, D. , & Tian, J. (2016). Frontal metabolic activity contributes to individual differences in vulnerability toward total sleep deprivation‐induced changes in cognitive function. Journal of Sleep Research, 25, 169–180. 10.1111/jsr.12354 [DOI] [PubMed] [Google Scholar]
- Zhang, L. I. , Sun, D. , Li, C. , & Tao, M. (2016). Influencing factors for sleep quality among shift‐working nurses: A cross‐sectional study in china using 3‐factor Pittsburgh Sleep Quality Index. Asian Nursing Research, 10, 277–282. 10.1016/j.anr.2016.09.002 [DOI] [PubMed] [Google Scholar]
- Zuraikat, F. , Makarem, N. , Liao, M. , St‐Onge, M. , & Aggarwal, B. (2020). Measures of poor sleep quality are associated with higher energy intake and poor diet quality in a diverse sample of women from the Go Red for Women Strategically Focused Research Network. Journal of the American Heart Association, 9, e014587. 10.1161/JAHA.119.014587 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared. The data are not publicly available due to privacy and compliance with the Institutional Review Board protocol approval.


