Abstract
Aim
The aim of this study was to determine the prevalence and correlates of anaemia among postnatal women.
Design
A cross‐sectional survey was conducted from April–July, 2020, at a healthcare facility in Dodoma City.
Methods
Haemoglobin concentration was measured by using HemoCue Hb 201+ analyser machine. Anaemia was defined as haemoglobin concentration of <11 g/dl. Chi‐square test and logistic regression analysis were conducted to identify the correlates of anaemia.
Results
The overall prevalence of postpartum anaemia was found to be 21.6% (83). Correlates of anaemia were found to be multiple birth (AOR = 4.97), consumption of pulses (AOR = 2.07), normal BMI (AOR = 2.28) and perception of insufficient milk supply (AOR = 3.05).
Conclusion
The prevalence of postpartum anaemia found in this study is high. Iron and folic acid supplementation, promotion of dietary diversification practices and screening women higher risk for anaemia may be feasible interventions.
Keywords: anaemia, Dodoma city, haemoglobin, postnatal women, postpartum, Tanzania
1. INTRODUCTION
Anaemia is a global public health problem that affects both developed and developing countries. It is associated with adverse effects on the population health and social and economic development (World Health Organization [WHO], 2018). While anaemia affects people of all groups, children and women of reproductive age are most vulnerable because of their higher physiological iron needs due to growth, menstruation and pregnancy. In order to prevent anaemia and iron deficiency among the adult women and adolescent female population, the WHO guideline recommends daily oral iron and folic acid supplementation as a public health intervention among menstruating adult women and adolescent girls and routinely during pregnancy. Furthermore, the WHO guideline recommends that where the prevalence of anaemia in pregnant women is high (40% or more), supplementation should continue for at least 3 months postpartum (WHO, 2018). Tanzania has adopted the WHO’s iron–folic acid supplementation guideline, and the antenatal care guideline of the Tanzania, Ministry of Health, Community Development, Gender, Elderly and Children (Ministry of Health, Community Development, Gender, & Children [MoHCDGEC], 2018) clearly indicates every pregnant woman should take 200 mg of ferrous sulphate and 0.4 mg of folic acid tablet daily and continue for 3 months after delivery (MoHCDGEC, 2018). The supplements are free for pregnant clients and usually dispensed monthly during antenatal visits. Despite the current government efforts, the compliance of iron–folic acid uptake remains low (<30%) (Ministry of Health, Community Development, Gender, Elderly and Children ‐ MoHCDGEC/Tanzania Mainland, Ministry of Health ‐ MoH/Zanzibar, National Bureau of Statistics ‐ NBS/Tanzania, Office of Chief Government Statistician ‐ OCGS/Zanzibar, and ICF. 2016. Tanzania Demographic and Health Survey and Malaria Indicator Survey 2015‐2016. Dar es Salaam, Tanzania: [TDHS ‐ MIS, 2016]).
2. BACKGROUND
Globally, inadequate dietary iron is the leading factor associated with anaemia (Gebre & Mulugeta, 2015
; McClure et al., 2014; Ononge et al., 2014). Generally, this accounts for more than 50% of all anaemia cases (WHO, 2011), although this proportion may vary according to population groups and settings. In sub‐Saharan Africa, the prevalence is much higher due to the burden of infectious diseases such as malaria, helminthes infestations, schistosomiasis, cancer and human immunodeficiency virus (Balarajan et al., 2011; Black et al., 2013; McClure et al., 2014; Msuya et al., 2011; Okube et al., 2016; Ononge et al., 2014; Tolentino & Friedman, 2007).
Anaemia is a public health problem associated with negative health outcomes including: increased risk of maternal and perinatal mortality, increased numbers of preterm birth and/or low birth weight, impaired cognitive and physical development in children and reduced adult work productivity (Black et al., 2013; Okube et al., 2016; WHO, 2014). Although many scholars have put more emphasis on anaemia during pregnancy (Black et al., 2013; Gebre & Mulugeta, 2013; Msuya et al., 2011; Okube et al., 2016; Ononge et al., 2014; WHO, 2018), anaemia also affects other groups of women including adolescent girls and postpartum mothers.
Postpartum refers to the period from child birth to 6 weeks after delivery. The WHO describes postpartum as a critical and often forgotten phase in the lives of women and newborn (Garrido et al., 2017). Postpartum mothers are at higher risk of anaemia because of maternal iron depletion due to pregnancy (physiological anaemia of pregnancy), exposure to pre‐partum anaemia, blood losses during (Bergmann et al., 2010; Lakew et al., 2015) and after delivery, lacerations/tears and episiotomy (Kavle et al., 2008). Studies show that most maternal and newborn deaths occur during postpartum period (Black et al., 2013; Gebre & Mulugeta, 2013). Furthermore, anaemia during the postpartum period is associated with depressive symptoms, deficits in cognitive function, fatigue, lower work performance, impaired immune function and insufficient breast milk (Bhagwan et al., 2016; Bodnar et al., 2005; Milman, 2011; Rakesh et al., 2014). Other effects of anaemia during the postpartum period include: poorer functioning of mother–child interaction and even delayed infant development (Perez et al., 2005).
Despite the fact that the prevalence of postpartum anaemia is considerable and its effects are significant in many places worldwide, the problem has not received adequate attention even in developed countries (Garrido et al., 2017; Milman, 2011). Lack of standardized practice for diagnosis and management of anaemia during postpartum period is a challenge that has resulted in limited information on postpartum anaemia worldwide (Garrido et al., 2017; Ghadeeret al., 2019; Kofie et al., 2019; Petraro et al., 2013). For instance, in Tanzania, prevalence of postpartum anaemia was reported in a study conducted some 20 years ago. (Petraro et al., 2013). However, in order to plan for appropriate interventions, local and current evidence is crucial to inform relevant stakeholders on the situation and guide healthcare professionals to ensuring optimal health for postnatal women and infants. Therefore, this study was designed to assess the prevalence and factors associated with anaemia among postnatal women in Dodoma City, Tanzania.
The research questions in this study are as follows:
-
1. What is the prevalence of postpartum anaemia in Dodoma City?
This will help the stakeholders to know how big the problem is.
-
2. What are the factors associated with postpartum anaemia in Dodoma City?
This will give room for stakeholders to plan for appropriate interventions by addressing the factors identified
3. METHODS
3.1. Study design and population
This study was a cross‐sectional survey conducted from April–July, 2020. Eligible participants were all postnatal women within 6 weeks after birth attending postnatal clinics at healthcare facilities in Dodoma City. Based on ethical, medical and data quality issues, the following were excluded from the study: women aged <18 years, women who were ill at the time of data collection, women with a history of blood transfusion during postpartum period, women with sickle cell disorder and women who did not have a Reproductive and Child Health card 4 (client card RCH 4 opened and given to the pregnant woman at the first antenatal visit to collect and monitor information on pregnancy to postpartum period). Screening for eligible participants was performed by using RCH card 4 and the information obtained from the healthcare provider (HCP) at the postnatal clinic.
3.2. Study area
This study was conducted in Dodoma City, Central Tanzania. Dodoma City is the capital of Dodoma Region and the home of the national capital. The city has an estimated population of 459,350 people (National Bureau of Statistics, 2017). According to the information obtained on March, 2020, from the office of regional medical in‐charge, the city has 84 health facilities, including 66 dispensaries, 11 health centres and 7 hospitals. Reproductive and child health services are normally provided at the dispensaries and health centres. The average number of births per month from all health facilities is 2011.
3.3. Sample size and sampling procedures
The sample size (N) for this study was calculated using the formula, , whereby N = sample size, z = 1.96 and e = 5%. An arbitrary of 50% prevalence of anaemia among women during postpartum was employed to compute for the required minimum sample size of 384 respondents. A total of 398 postnatal women were selected for this study.
Simple random sampling by using Microsoft excel random number generator was used to select nine healthcare facilities for the study. Participants were selected by simple random sampling technique using rotary method. In this method, we prepared equal number of “Yes” and “No” pieces of paper. The papers were folded and placed in a container. During participant selection, the container was thoroughly shaken to ensure randomization. The participants were then allowed to pick one piece of paper from the container. A participant who picked “Yes” paper was enrolled for the study.
3.4. Data collection procedures
Data were collected using a pre‐tested semi‐structured questionnaire. Respondents’ information was obtained through a face‐to‐face interview. Socio‐demographic characteristics were assessed, including age, marital status, highest level of education attained, employment status and place of residence. Twenty‐four‐hour dietary recall was performed by using a standard dietary assessment tool adapted from the Food and Agricultural Organization (Food & Agriculture Organization, 2016). Breastfeeding‐related complications were explored through participants' self‐reporting based on their past 7 days experience. Obstetric characteristics and Vitamin A supplementation were obtained by using the client RCH card 4. Body weight and height were measured without shoes and with minimal clothing by using a SECCA® scale. One drop of capillary blood via finger prick was used to estimate haemoglobin concentration by using HemoCue Hb 201+ analyser machine. Respondents found to have anaemia were assisted to see a clinician at the respective health facility for further evaluation and management.
3.5. Definition of variables
Socio‐demographic variables were categorized into groups for clear definition of variables. Two age categories were created: older and younger than age 35. Marital status was either currently married or not married. Education categories included a range of options to reflect no formal education (did not attend/completed the 7 years of primary school education), primary education (completed 7 years school education), secondary education (completed 4–6 years secondary education) and tertiary education (attended college‐/university‐level education). Employment status categories reflected a range from formal employment where a person receives a regular monthly wage with a permanent or temporary contract to non‐formal employment where a person may be involved in other income‐generating activities such as casual labourer, small business or farming. Place of residence was determined using current municipal ward categories. For obstetrics characteristics, parity was categorized into three groups as follows: primiparous, multiparous and grand multiparous for a woman who has given birth once, two to four births and five or more births respectively.
The 24‐hr dietary recall history was categorized into 10 groups of foods for the assessment of women's dietary diversity. These included: 1. grains, roots, tubers and plantains; 2. pulses (beans, peas and lentils); 3. nuts and seeds; 4. dairy; 5. meat, poultry and fish; 6. eggs; 7. dark green vegetables; 8. other vitamin A–rich fruits and vegetables; 9. other vegetables and 10. other fruits. The food groups consumed were used to determine the minimum dietary diversity for women (MDD‐W). The MDD‐W is defined as whether women 15–49 years of age have consumed at least 5 of 10 defined food groups the previous day or night. The proportion of women 15–49 years of age who reach this minimum in a population can be used as a proxy indicator for higher micronutrient adequacy, one important dimension of diet quality (FAO, 2016). Body weight and height were used to calculate the body mass index (BMI) and categorized as normal (<25 kg/m2) or overweight (≥25kg/m2). Anaemia was defined as haemoglobin concentration of <11 g/dl (WHO, 2011).
3.6. Data analysis
Data collected were coded, cleaned and transformed by using the SPSS version 22 for WINDOWS computer program (SPSS Inc). Descriptive analysis was carried out to present frequency distributions for socio‐demographic characteristics, obstetric characteristics, dietary intakes, breastfeeding‐related complications and prevalence of anaemia. To compare prevalence of anaemia according to respondents' characteristics, chi‐square test for independence was conducted. Thereafter, binary and multivariable logistic regressions were conducted to determine the associates of anaemia. All independent variables with p‐value ≤.05 at binary logistic regression models were included in the multivariable logistic regression model to evaluate the correlates of anaemia among the postnatal women. All probabilities were two‐tailed and independent variables with p values <.05 were regarded as statistically significant.
4. RESULTS
4.1. Socio‐demographic and obstetrics characteristics of the respondents
A total of 384 (96.5% response rate) respondents participated in this study. Reasons for dropouts/decline included lack of enough time for the interview, not feeling well and ethical issues. The mean age of respondents was 27.17 ± 5.85 years. One hundred and eighty (46.9%) respondents had completed primary education only. A majority (328 [85.4%]) of the respondents were currently married and approximately two‐third of the respondents were living in urban areas. The majority of the respondents (274 [71.4%]) and about 236 (61.5%) of spouses were employed at non‐formal employment sector. The majority (239 [62.2%]) of the respondents were multiparous. About last pregnancy; the majority (373 [97.1%]) of the respondents had delivered a singleton baby and 334 (87.0%) respondents had spontaneous vaginal delivery. About half of the respondents (196 [51.0%]) had completed ≥4 antenatal care (ANC) visits during their pregnancy and 99 (25.8%) respondents had the history of anaemia during the last pregnancy (Table 1).
TABLE 1.
Socio‐demographic and obstetrics characteristics of the respondents (N = 384)
| Frequency | Percent | |
|---|---|---|
| Age group (years) | ||
| <35 | 335 | 87.5 |
| 35 years and above | 49 | 12.8 |
| Higher education level attained | ||
| Non‐formal | 36 | 9.4 |
| Primary | 180 | 46.9 |
| Secondary | 134 | 34.9 |
| Tertiary | 34 | 8.8 |
| Marital status | ||
| Currently married | 328 | 85.4 |
| Not married | 56 | 14.6 |
| Employment status of the participant | ||
| Formal employment | 52 | 13.5 |
| Non‐formal employment | 332 | 86.5 |
| Employment status of the spouse | ||
| Formal employment | 88 | 22.9 |
| Non‐formal employment | 276 | 77.1 |
| Place of residence | ||
| Urban | 250 | 65.1 |
| Peri‐urban | 134 | 34.9 |
| Parity | ||
| Primiparous | 123 | 32.0 |
| Multiparous | 239 | 62.2 |
| Grand multiparous | 22 | 5.7 |
| Number of babies born in last pregnant | ||
| Singleton | 373 | 97.1 |
| Multiple | 11 | 2.9 |
| Delivery mode in the last pregnant | ||
| Spontaneous vaginal delivery | 334 | 87.0 |
| Caesarean section | 50 | 13.0 |
| Number of ANC visits attended during last pregnant | ||
| 1–3 | 72 | 18.8 |
| 4 | 116 | 30.2 |
| >4 | 196 | 51.0 |
| History of anaemia during the last pregnancy | ||
| Yes | 99 | 25.8 |
| No | 285 | 74.2 |
4.2. Postpartum anaemia, BMI and breastfeeding complications
The prevalence of postpartum anaemia was 21.6% (83). More than three‐quarters of the respondent were either overweight or obese. About breastfeeding complications; about 37 (9.6%) had a perception of insufficient breast milk supply, and 25 (6.5%) respondents reported that they had initiated other foods with their newborns. A total of sixteen (4.2%) respondents reported experiencing nipple cracking, 24 (6.2%) reported breast engorgement and 13 respondents (3.4%) reported breast swelling (Figure 1).
FIGURE 1.
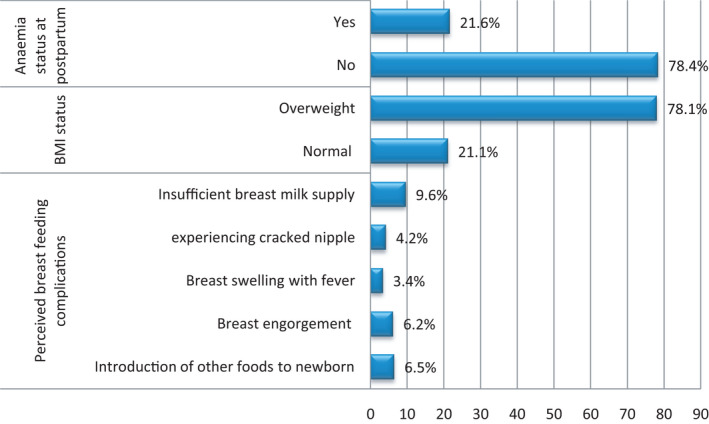
Postpartum anaemia, BMI and breast feeding complications
4.3. Dietary intakes for the past 24 hr
The majority of the respondents (345/89.5%) did not meet the minimum dietary diversity for women during the past 24 hr before the interview. Food groups mostly consumed were as follows: grains, roots, tubers and plantains (100%); meat, poultry, sardine and fish (79.4%) and other vegetables (79.7%). Eggs, nuts and seeds were food groups consumed less (<10%) by all respondents. More than half of the respondents (56%) consumed dark green leafy vegetables (Table 2).
TABLE 2.
Dietary intakes for the past 24 hr (N = 384)
| Yes – n (%) | No –n (%) | |
|---|---|---|
| Minimum dietary diversity for women | 39 (10.2) | 345 (89.8) |
| Grains, roots, tubers and plantains | 384 (100) | 0 (0) |
| Pulses (beans, peas and lentils) | 147 (38.3) | 237 (61.7) |
| Nuts and seeds | 24 (6.3) | 360 (93.7) |
| Dairy (milk, cheese and butter) | 32 (8.3) | 352 (91.7) |
| Meat, poultry, sardine and fish | 305 (79.4) | 79 (20.6) |
| Eggs | 16 (4.2) | 308 (95.8) |
| Dark green leafy vegetables | 215 (56.0) | 169 (44.0) |
| Vitamin A–rich fruits and vegetable | 81(21.1) | 303 (78.9) |
| Other vegetables | 306 (79.7) | 78 (20.3) |
| Other fruits | 36 (9.4) | 348 (90.6) |
4.4. Prevalence and correlates of postpartum anaemia among respondents
The chi‐square test for independence was conducted to assess the prevalence of anaemia according to respondents' characteristics. With respect to background characteristics, the results show that prevalence of postpartum anaemia was statistically significant by age, marital status, parity and number of babies born in the last pregnancy. About dietary intake and other maternal factors, prevalence of anaemia was also statistically significant by minimum dietary diversity for women, consumption of pulses and green leafy vegetables, introduction of other foods to the newborn, experience of cracked nipples, having normal BMI and perceived insufficient milk supply
Of note, the prevalence of anaemia was statistically significantly higher among respondents aged <35 years (23.6%), not married (32.1%) and respondents with multiple babies (54.5%). About the past 24‐hr dietary history, prevalence of anaemia was higher among respondents who consumed pulses (27.2%), those who did not consume dark green vegetables (26.6%) and those who did not meet minimum dietary diversity for women (23.2%). Furthermore, the prevalence of anaemia was higher among respondents with normal BMI (39.5%), experiencing cracked nipple (50.0%), primiparous (32.6%), respondents with the perception of insufficient milk supply (48.6%) and those who introduced other foods to their newborn (40.0%; Table 3).
TABLE 3.
Prevalence and correlates of postpartum anaemia among the respondents (N = 384)
| Postpartum anaemia | OR (95% CI) | AOR (95%CI) | p value | |
|---|---|---|---|---|
| Age of respondents | ||||
| <35 | 79 (23.6)** | 1 | 1 | .141 |
| ≥35 years | 4 (8.2) | 0.29 (0.10–0.83) | 0.40 (0.12–1.41) | |
| Marital status | ||||
| Currently married | 65 (19.8)** | 1 | 1 | .827 |
| Not married | 18 (32.1) | 1.92 (1.028–3.57) | 1.09 (0.52 –2.29) | |
| Employment status of the husband | ||||
| Currently employed | 14 (15.9)* | 1 | ‐ | ‐ |
| Not employed | 69 (23.3) | 1.61 (0.85–3. 02) | ‐ | ‐ |
| Type of residence | ||||
| Peri‐urban | 22 (16.4)* | 1 | ‐ | ‐ |
| Urban | 61 (24.4) | 1.64 (0.96–2.82) | ‐ | ‐ |
| Parity | .070 | |||
| Primiparous | 40 (32.5)*** | 1 | 1 | |
| Multiparous | 41 (17.2) | 0.43 (0.26–0.71) | 0.47 (0.25–0.89) | .957 |
| Grand multiparous | 2 (9.1) | 0.21 (0.45–0.93) | 0.48 (0.09–2.57) | .858 |
| Number of babies born in last pregnancy | ||||
| Singleton | 77 (20.6)** | 1 | 1 | .024 |
| Multiple | 6 (54.5) | 4.61 (1.37–15.52) | 4.97 (1.24–19.93) | |
| Consumption of pulses (beans, peas, etc.) | ||||
| No | 43 (18.1)** | 1 | 1 | .013 |
| Yes | 40 (27.2) | 1.69 (1.03–2.76) | 2.07 (1.17–3.69) | |
| Consumption of dark green leafy vegetables | ||||
| No | 45 (26.6)** | 1 | 1 | .261 |
| Yes | 38 (17.7) | 0.59 (0.39–0.97) | 0.73 (0.41–1.27) | |
| Minimum dietary diversity for women | ||||
| Yes | 3 (7.7)** | 1 | 1 | 0.063 |
| No | 80 (23.2) | 3.62 (1.09 – 12.08) | 3.44 (0.93–12.67) | |
| Introduction of other foods to the newborn | ||||
| No | 73 (20.3)** | 1 | 1 | .661 |
| Yes | 10 (40.0) | 2.61 (1.13 – 6.05) | 1.31 (0.34 – 5.02) | |
| BMI status | ||||
| Overweight | 51 (16.8)*** | 1 | 1 | .009 |
| Normal | 32 (39.5) | 3.23 (1.89 – 5.52) | 2.28 (1.22 – 4.22) | |
| Experiencing cracked nipple | ||||
| No | 75 (20.4)** | 1 | 1 | .267 |
| Yes | 8 (50.0) | 3.91 (1.42–10.75) | 1.92 (0.61–6.05) | |
| Perception of insufficient milk supply | ||||
| No | 65 (18.7)*** | 1 | 1 | .049 |
| Yes | 18 (48.6) | 4.11 (2.04–8.27) | 3.05 (1.00–9.29) | |
***p < .001, **p < .05, *p ≥ .05.
Simple logistic regression was conducted for all variables with p value of ≤.25 at the chi‐square test. The results of a simple logistic regression model show that respondent's age, marital status, parity, number of babies born in the last pregnant, BMI status, experience of cracked nipples and perception of insufficient milk supply were statistically significantly associated with postpartum anaemia (p < .05). Furthermore, introduction of other foods to the newborn, consumption of pulses, dark green leafy vegetables and minimum dietary diversity for women were also statistically significantly associated with postpartum anaemia (Table 3).
All variables with p‐value of <.05 from simple regression analysis were fitted into a multivariable logistic model to determine the associates of postpartum anaemia. After adjusting for the potential confounder, correlates of anaemia were found to be multiple birth in the last pregnancy (AOR = 4.97, 95% CI = 1.24–19.93), consumption of pulses (AOR = 2.07, 95% CI = 1.17–3.69), normal BMI (AOR = 2.28, 95% CI = 1.22–4.22) and perception of insufficient milk supply (AOR = 3.05, 95% CI 1.00–9.29; Table 3).
5. DISCUSSION
This study demonstrates that prevalence of anaemia among postpartum women attending postnatal clinics in Dodoma City is a public health problem (WHO, 2011) as one of every five postnatal women has anaemia in this setting. This prevalence is statistically significantly high and stakeholders are urged to plan for possible interventions to curb the situation. The current finding is similar to previous studies conducted in both developed (Bergmann et al., 2010; Bodnar et al., 2001; Garrido et al., 2017) and developing countries (Ghadeer et al., 2019; Kofie et al., 2019). However, the current prevalence is far less than what was reported from a study conducted in Uganda (64.4%) (Sserunjogiet al., 2003) and India (76.2%; Selvaraj et al., 2019). Possible explanations for this difference might be attributed to differences in study populations and definitions of anaemia used between the current study and the previous studies (Selvaraj et al., 2019; Sserunjogiet al., 2003). Unlike the current study, the former studies conducted among postnatal women with older children aged between 6 weeks–12 months used the higher haemoglobin cut‐off point of <12 g/dl to define anaemia. Despite the higher cut‐off point used to define anaemia in the former studies, the differences in prevalence observed is still high by considering the fact that the current study population was relatively at higher risk of anaemia compared to that of the former studies. Furthermore, time factor and study settings may also explain the current observed differences. About the time factor, the current study has been conducted 20 years after that of Uganda. Since Tanzania and Uganda are both in East Africa, they share many issues including cultural, lifestyle and developmental issues. Improved health services over time might explain the current lower prevalence relative to that of Uganda. Comparing with the finding from India, the current study was conducted at the healthcare facility, whereas the study from India was conducted at a community setting. Postnatal women found at the healthcare facility may not be a good representation of all postnatal women at the community. The current study population may constitute postnatal women who had received and adhered to standards of healthcare services, and hence, less risk of anaemia compared to those who are found at the general community.
Consistent with the previous studies done in Germany (Bergmannet al., 2010) and United States (Bodnar et al., 2001), this study showed that women with multiple birth had more than four chances of having anaemia. The possible explanations for this finding could be the increased risk of high blood loss during delivery and sometimes operative delivery due to multiple births (Bergmann et al., 2010). In addition, the iron requirements for the multiple pregnancy is much higher compared to singleton pregnancy. Therefore, the mother with multiple pregnancy is likely to deplete her iron stores much more during pregnancy in order to support foetal development and, hence, more at risk of developing anaemia later, particularly during postpartum period.
Inadequate intake of dietary iron is said to be the leading cause of anaemia worldwide, (Ononge et al., 2014). The current study noted that consumption of pulses was statistically significantly associated with anaemia during postpartum. Logically, pulses provide non‐haem iron that requires presence of either haem iron or ascorbic acid or both to enhance its bioavailability. The current finding suggests that pulses might have been consumed without other dietary sources for haem iron and/or ascorbic acid as it has been demonstrated by low proportion of the respondents who were able to consume minimum dietary diversity for women and higher consumption of single food group among the current respondents. The currently observed dietary practice is not surprising in this community as previous studies conducted in Dodoma have reported low food diversity and dietary intake characterized by only single food group (Ngilangwa, 2019), particularly dark green vegetable and low consumption of meat and meat products among women (Huang et al., 2018). Additionally, although the results were not statistically significant, the current findings showed that consumption of dark green vegetables and meeting minimum dietary diversity for women were found to reduce the prevalence of anaemia among postpartum women. Dark green vegetables and minimum dietary diversity ensure availability of non‐haem iron, haem iron and ascorbic acid. This mixture constitutes all the necessary conditions for enhancing the bioavailability of iron. These findings suggest that, food diversification may help to reduce the risk of anaemia. Therefore, health promotion that emphasizes dietary diversity practices by eating foods from at least five different groups should be given priority in order to reduce anaemia and other forms of malnutrition.
Surprisingly, the current study showed that normal BMI was statistically significantly associated with anaemia during postpartum. This is contrary to the findings from previous studies which showed that obesity was associated with anaemia (Bodnar et al., 2001; Sal et al., 2018; Tan et al., 2018). The current finding might suggest that BMI in this setting may not be necessarily a reflection of diet quality (Hotzel, 1986; Moss et al., 1989). This observation could be explained by the obesity patterns in developing and developed countries. In developing countries, including Tanzania, overweight and obesity are common among people with higher socioeconomic status (Maletnlema, 2002). These are the people who are also more likely to afford a variety of foods including iron‐rich food relative to those with normal BMI. Despite the possible explanations for this finding, we recommend more studies since the current study was a cross‐sectional design which limits analysis on causal–effect relationship.
The current study has demonstrated that anaemia was associated with a perception of inadequate breast milk supply among the postnatal women. This finding is similar to the previous study which showed that insufficient milk supply was statistically significantly higher among women with anaemia (Henley et al., 1995). The possible explanation for this finding may be due to the body fatigue experienced by women with anaemia, and hence, fail to breastfeed properly. Fatigue has been said to be the major factor affecting milk supply during postpartum (Lawrence, 1994). The noted association between anaemia and inadequate breast milk supply should be given required attention especially in settings like Tanzania where anaemia is a public health concern as this condition is likely to impair the breastfeeding practices, particularly exclusive breastfeeding.
5.1. Implications
The need to monitor postnatal health is crucial in order to ensure optimal health of the mother and the infant. Standard postnatal guideline is important to help healthcare provider give adequate care and monitoring of postnatal women. Implementation of WHO guideline (WHO, 2016) to continue daily supplementation of oral iron and folic acid for 3 months in the postpartum period is indispensable to our settings. More researches to provide evidences that will help in planning cost‐effective interventions to this problem are vital. Emphasis and strengthening of maternal nutritional education may help to reduce problem.
5.2. Strengths and limitations
This study will add to the limited available evidence on anaemia during postpartum in Tanzania. Also, the study was conducted in Dodoma City where there is limited information on anaemia. Anaemia was estimated based on primary data measured by a qualified laboratory technician during the survey. However, this study had a number of limitations. The study was a cross‐sectional study conducted at the healthcare facility level. This may limit generalization of the findings. Also, information on socio‐demographic characteristics and other factors assessed are self‐reported by the respondents, which may be subject to information bias.
6. CONCLUSION
The prevalence of anaemia among postnatal women found in this study is high. Short‐term interventions may include anaemia screening for women with higher risk(s) including women with multiple birth, women aged <35 years, women with history of anaemia during pregnant and primiparous after delivery before they are discharged home and during postnatal visits. The modifiable correlates of anaemia found in this study, particularly those associated with dietary intake, enable healthcare stakeholders to plan for appropriate nutritional interventions for this group, including promotion of dietary diversification practices that enhance iron bioavailability. Strategies should be therefore put in place to encourage frequent antenatal and postnatal visits to ensure many women get screening services and key nutritional education and treatment. This could be achieved through standard postnatal guideline, maternal health education and promotion programmes.
CONFLICT OF INTEREST
Authors declare that there is no competing interest.
AUTHOR CONTRIBUTIONS
Sophia Rogasian Tairo: Study conceptualization, data acquisition and prepared the first draft of the manuscript. Mariam John Munyogwa: Data analysis, interpretation and manuscript revision. Sophia Rogasian Tairo and Mariam John Munyogwa: Designed the study, read the final version and approved of its publication.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Research Review Committee of the University of Dodoma on March 27th, 2020, Ref: MA.84/261/02/03. Permission to conduct the study at the site was obtained from the city council and respective offices. Prior to data collection, the aim and objectives of the study were explained to the participants. A verbal and written consent was sought from respondents before data collection. All data collected during the study were treated with confidentiality. Questionnaires were assigned unique identification numbers, and no names were used during data collection.
ACKNOWLEDGEMENTS
Authors would like to acknowledge the followings for their contributions: Healthcare providers, specifically those working at postnatal units in Dodoma City, for their corporation. Colleagues at the College of Health Sciences – University of Dodoma; Postnatal women who participated in this study and Ms. Elisa Brettler Vandervort for her critical review and language editing.
Tairo, S. R. , & Munyogwa, M. J. (2022). Maternal anaemia during postpartum: Preliminary findings from a cross‐sectional study in Dodoma City, Tanzania. Nursing Open, 9, 458–466. 10.1002/nop2.1085
DATA AVAILABILITY STATEMENT
The data set that supports the current findings is available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Balarajan, Y. , Ramakrishnan, U. , Özaltin, E. , Shankar, A. H. , & Subramanian, S. V. (2011). Anaemia in low‐income and middle‐income countries. The Lancet, 378(9809), 2123–2135. 10.1016/S0140-6736(10)62304-5 [DOI] [PubMed] [Google Scholar]
- Bergmann, R. L. , Richter, R. , Bergmann, K. E. , & Dudenhausen, J. W. (2010). European Journal of Obstetrics & Gynecology and Reproductive Biology Prevalence and risk factors for early postpartum anemia. European Journal of Obstetrics and Gynecology, 150(2), 126–131. 10.1016/j.ejogrb.2010.02.030 [DOI] [PubMed] [Google Scholar]
- Bhagwan, D. , Kumar, A. , Rao, C. R. , & Kamath, A. (2016). Prevalence of anaemia among postnatal mothers in coastal Karnataka. Journal of Clinical and Diagnostic Research, 17–20, 10.7860/JCDR/2016/14534.7086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black, R. E. , Victora, C. G. , Walker, S. P. , Bhutta, Z. A. , Christian, P. , De Onis, M. , Ezzati, M. , Grantham‐McGregor, S. , Katz, J. , Martorell, R. , & Uauy, R. (2013). Maternal and child undernutrition and overweight in low‐income and middle‐income countries. The Lancet, 382(9890), 427–451. 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- Bodnar, L. M. , Cogswell, M. E. , & McDonald, T. (2005). Have we forgotten the significance of postpartum iron deficiency? American Journal of Obstetrics and Gynecology, 193(1), 36–44. 10.1016/j.ajog.2004.12.009 [DOI] [PubMed] [Google Scholar]
- Bodnar, L. M. , Scanlon, K. S. , Freedman, D. S. , Siega‐Riz, A. M. , & Cogswell, M. E. (2001). High prevalence of postpartum anemia among low‐income women in the United States. American Journal of Obstetrics and Gynecology, 185(2), 438–443. 10.1067/mob.2001.115996 [DOI] [PubMed] [Google Scholar]
- FAO and FHI 360 (2016) Minimum Diet Diversity for Women: A Guide for Measurement. Food and Agriculture Organization. Available at: http://www.fao.org/3/i5486e/i5486e.pdf. Accessed 5 December, 2020 [Google Scholar]
- Garrido, C. M. , Garrido, C. M. , León, J. , & Vidal, A. R. (2017). Maternal anaemia after delivery : Prevalence and risk factors Maternal anaemia after delivery : Prevalence and risk factors. Journal of Obstetrics and Gynaecology, 2017(8), 1–5. [DOI] [PubMed] [Google Scholar]
- Gebre, A. , & Mulugeta, A. (2015). Prevalence of anemia and associated factors among pregnant women in North Western zone of Tigray, Northern Ethiopia: A cross‐sectional study. Journal of Nutrition and Metabolism, 2015, 10.1155/2015/165430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghadeer, M. , Alsahafi, N. , Shami, B. , Abulkhair, S. , Alhazmi, N. , & Alsaleh, R. (2019). Incidence of Postpartum Anaemia among Postpartum Patients in East Jeddah Hospital. International Journal of Life Science and Pharma Research, 9(2), 39–46. [Google Scholar]
- Henley, S. J. , Anderson, C. M. , Avery, M. D. , Hills‐Bonczyk, S. G. , Potter, S. , & Duckett, L. J. (1995). Anemia and insufficient milk in first‐time mothers. Birth, 22, 86–92. 10.1111/j.1523-536X.1995.tb00565.x [DOI] [PubMed] [Google Scholar]
- Hotzel, D. (1986). Suboptimal nutritional status in obesity (selected nutrients). Bibliotheca Nutritio Et Dieta, 21, 36–41. [PubMed] [Google Scholar]
- Huang, M. , Sudfeld, C. , Ismail, A. , Vuai, S. , Ntwenya, J. , Mwanyika‐Sando, M. , & Fawzi, W. (2018). Maternal dietary diversity and growth of children under 24 months of age in rural Dodoma. Tanzania. Food and Nutrition Bulletin, 39(2), 219–230. 10.1177/0379572118761682 [DOI] [PubMed] [Google Scholar]
- Kavle, J. A. , Stoltzfus, R. J. , Witter, F. , Tielsch, J. M. , Khalfan, S. S. , & Caulfield, L. E. (2008). Association between anaemia during pregnancy and blood loss at and after delivery among women with vaginal births in Pemba Island, Zanzibar, Tanzania. Journal of Health, Population, and Nutrition, 26(2), 232. [PMC free article] [PubMed] [Google Scholar]
- Kofie, P. , Tarkang, E. E. , Manu, E. , Amu, H. , Ayanore, M. A. , Aku, F. Y. , Komesuor, J. , Adjuik, M. , Binka, F. , & Kweku, M. (2019). Prevalence and associated risk factors of anaemia among women attending antenatal and post‐natal clinics at a public health facility in Ghana. BMC . Nutrition, 1–9. 10.1186/s40795-019-0303-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakew, Y. , Biadgilign, S. , & Haile, D. (2015). Anaemia prevalence and associated factors among lactating mothers in Ethiopia : Evidence from the 2005 and 2011 demographic and health surveys. British Medical Journal Open, 5, 1–7. 10.1136/bmjopen-2014-006001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence, R. A. (1994). Breast‐feeding. A Guide for the Medical Profession. , 4th ed. Mosby. [Google Scholar]
- Maletnlema, T. N. (2002). A Tanzanian perspective on the nutrition transition and its implications for health. Public Health Nutrition, 5(1a), 163–168. 10.1079/PHN2001289 [DOI] [PubMed] [Google Scholar]
- McClure, E. M. , Meshnick, S. R. , Mungai, P. , Malhotra, I. , King, C. L. , Goldenberg, R. L. , Hudgens, M. G. , Siega‐Riz, A. M. , & Dent, A. E. (2014). The association of parasitic infections in pregnancy and maternal and fetal anemia: A cohort study in coastal Kenya. PLoS Neglected Tropical Diseases, 8(2), e2724. 10.1371/journal.pntd.0002724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milman, N. (2011). Postpartum anemia I: Definition, prevalence, causes, and consequences. Annals of Hematology, 90(11), 1247–1253. 10.1007/s00277-011-1279-z [DOI] [PubMed] [Google Scholar]
- Ministry of Health, Community Development, Gender and Children, The URT Antenatal Care Guidelines (2018). Ministry of health, Community Development, Gender and Children. Dar es Salaam, Tanzania. Available at: http://repository.out.ac.tz/2490/1/ANC%20Guidelines_Final%20Aproved%20%281%29.pdf. Accessed 13 February, 2021 [Google Scholar]
- Ministry of Health, Community Development, Gender, Elderly and Children – MoHCDGEC/Tanzania Mainland, Ministry of Health – MoH/Zanzibar, National Bureau of Statistics – NBS/Tanzania, Office of Chief Government Statistician – OCGS/Zanzibar, and ICF (2016). Tanzania Demographic and Health Survey and Malaria Indicator Survey 2015‐2016. Dar es Salaam, Tanzania: MoHCDGEC, MoH, NBS, OCGS, and ICF. Available at: http://dhsprogram.com/pubs/pdf/FR321/FR321.pdf. Accessed 5 May, 2021 [Google Scholar]
- Moss, A. J. , Levy, A. S. , Kim, I. , & Park, Y. K. (1989). Use of vitamin and mineral supplements in the United States: current users, types of products, and nutrients. National Center for Health Statistics. Advance Data from Vital and Health Statistics, No. 174. [Google Scholar]
- Msuya, S. E. , Hussein, T. H. , Uriyo, J. , Sam, N. E. , & Stray‐Pedersen, B. (2011). Anaemia among pregnant women in northern Tanzania: Prevalence, risk factors and effect on perinatal outcomes. Tanzania Journal of Health Research, 13(1), 33–39. 10.4314/thrb.v13i1.60881 [DOI] [PubMed] [Google Scholar]
- National Bureau of Statistics (2017). The United Republic of Tanzania; Tanzania Total Population by District – Regions – 2016‐2017. https://www.nbs.go.tz/index.php/en/census‐surveys/population‐and‐housing‐census/178tanzania‐total‐population‐by‐district‐regions‐2016‐201727 [Google Scholar]
- Ngilangwa, J. N. (2019). The contribution of women to household food and nutrition security in Chamwino District, Dodoma, Tanzania (Doctoral dissertation, Sokoine University of Agriculture). [Google Scholar]
- Okube, O. T. , Mirie, W. , Odhiambo, E. , Sabina, W. , & Habtu, M. (2016). Prevalence and Factors Associated with Anaemia among Pregnant Women Attending Antenatal Clinic in the Second and Third Trimesters at Pumwani Maternity Hospital, Kenya. Open Journal of Obstetrics and Gynecology, 06(01), 16–27. 10.4236/ojog.2016.61003 [DOI] [Google Scholar]
- Ononge, S. , Campbell, O. , & Mirembe, F. (2014). Haemoglobin status and predictors of anaemia among pregnant women in Mpigi, Uganda. BMC Research Notes, 7(1), 712. 10.1186/1756-0500-7-712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez, E. M. , Hendricks, M. K. , Beard, J. L. , Murray‐Kolb, L. E. , Berg, A. , Tomlinson, M. , Irlam, J. , Isaacs, W. , Njengele, T. , Sive, A. , & Vernon‐Feagans, L. (2005). Mother‐Infant Interactions and Infant Development Are Altered by Maternal Iron Deficiency Anemia. Journal of Nutrition, 135(4), 850–855. 10.1093/jn/135.4.850 [DOI] [PubMed] [Google Scholar]
- Petraro, P. , Duggan, C. , Urassa, W. , Msamanga, G. , Makubi, A. , Spiegelman, D. , & Fawzi, W. W. (2013). Determinants of anemia in postpartum HIV‐negative women in Dar es Salaam, Tanzania. European Journal of Clinical Nutrition, 67, 708–717. 10.1038/ejcn.2013.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakesh, P. S. , Gopichandran, V. , Jamkhandi, D. , Manjunath, K. , George, K. , & Prasad, J. (2014). Determinants of postpartum anemia among women from a rural population in southern India. International Journal of Women’s Health, 6(1), 395–400. 10.2147/IJWH.S58355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sal, E. , Yenicesu, I. , Celik, N. , Pasaoglu, H. , Celik, B. , Pasaoglu, O. T. , Kaya, Z. , Kocak, U. , Camurdan, O. , Bideci, A. , & Cinaz, P. (2018). Relationship between obesity and iron deficiency anemia: Is there a role of hepcidin? Hematology, 23(8), 542–548. 10.1080/10245332.2018.1423671 [DOI] [PubMed] [Google Scholar]
- Selvaraj, R. , Ramakrishnan, J. , Sahu, S. , Kar, S. , Laksham, K. , Premarajan, K. , & Roy, G. (2019). High prevalence of anemia among postnatal mothers in urban Puducherry: A community‐based study. Journal of Family Medicine and Primary Care, 8(8), 2703–2707. 10.4103/jfmpc.jfmpc_386_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sserunjogi, L. , Scheutz, F. , & Whyte, S. R. (2003). Postnatal anaemia: Neglected problems and missed opportunities in Uganda. Health Policy and Planning, 18(2), 225–231. 10.1093/heapol/czg027 [DOI] [PubMed] [Google Scholar]
- Tan, J. , Qi, Y. N. , He, G. L. , Yang, H. M. , Zhang, G. T. , Zou, K. , Luo, W. , Sun, X. , & Liu, X. H. (2018). Association between Maternal Weight Indicators and Iron Deficiency Anemia during Pregnancy: A Cohort Study. Chinese Medical Journal, 131(21), 2566–2574. 10.4103/0366-6999.244109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolentino, K. , & Friedman, J. F. (2007). An update on anemia in less developed countries. The American Journal of Tropical Medicine and Hygiene, 77(1), 44–51. 10.4269/ajtmh.2007.77.44 [DOI] [PubMed] [Google Scholar]
- WHO (2011). Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System. World Health Organization; (WHO/NMH/NHD/MNM/11.1) http://www.who.int/vmnis/indicators/haemoglobin.pdf [Google Scholar]
- Guideline: Daily iron supplementation in adult women and adolescent girls. World Health Organization; 2016. [PubMed] [Google Scholar]
- World Health Organization (WHO) (2018). WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience: Summary. World Health Organization, 10(January), 1–10. 10.1186/1742-4755-10-19.5 [DOI] [Google Scholar]
- World Health Organization (2014). Micronutrient deficiencies. IDA. WHO. Available at: http://www.who.int/nutrition/topics/ida/en/ [Google Scholar]
- Worldwide prevalence of anaemia 1993–2005 (2008). WHO Global Database on Anaemia. https://www.who.int/health‐topics/anaemia#tab=tab_ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data set that supports the current findings is available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


