Abstract
Aim and objectives
To describe young children's experiences of valuable support in managing their fears about treatment for acute lymphoblastic leukaemia. The focus was specifically on support from parents and healthcare professionals.
Design
The study had a qualitative descriptive longitudinal design.
Methods
The study analysed 35 interviews with 13 children at three different times during their treatment period. Data were analysed using a matrix‐based method. The Consolidated criteria for reporting qualitative research (COREQ) guidelines have been followed.
Results
Parents and healthcare professionals provide important support to children undergoing treatment for acute lymphoblastic leukaemia, although their roles differ. Children valued their parents’ closeness and advocacy, being able to participate in their own care, and being given pain relief during procedures known to create pain. Valued support from healthcare professionals changed over time, from providing information and showing the tools that would be used in procedures, to paying attention to the child's needs and desires. It was more important for children to be able to choose between different alternatives in medical procedures than deciding on major treatment issues.
Keywords: acute lymphoblastic leukaemia, fear, health personnel, parents, qualitative studies, support
1. INTRODUCTION
Fear is common in sick children who interact with the healthcare system, and children with acute lymphoblastic leukaemia (ALL) are no exception. Perhaps their fear is unavoidable, yet all children have the right to adequate support in managing their situation. Such support can be especially important during a long, unpleasant course of treatment. This study focuses on the types of support from healthcare professionals and parents that 5‐to‐9‐year‐old children with ALL report as helping them when they feel scared. Age and development are associated with how children express hospital‐related experiences (Lindeke et al., 2006). Although older children might have better verbal skills, younger children can also express their fear in practice and in research (Kassa et al., 2017; Kleye et al., 2021; Leibring & Anderzén‐Carlsson, 2019; Zimmer‐Gembeck & Skinner, 2011). From a children's rights perspective (UNICEF, 1989), it is important to study and give voice to young children's experiences of support during their treatment for ALL.
As described in a previous study within the project (Leibring & Anderzén‐Carlsson, 2019), children in the Nordic countries were at the time of this study diagnosed and treated according to the Nordic Society of Paediatric Hematology and Oncology (NOPHO) 2008 treatment protocol. The treatment, which typically takes about 2.5 years, is initially intense and includes repeated hospitalizations for intrusive procedures, including intravenous and intrathecal therapy. After about a year, medication is typically given orally, and the treatment is less intense, with fewer hospitalizations (Toft et al., 2018). Nevertheless, Darcy et al. (2016) showed that although the treatment regimen is less challenging in the later stages, the children's problems are not all over. Instead, children with leukaemia may face problems with interpersonal relationships when they return to school after completing the more intense treatment.
Previous longitudinal research has identified fear in children during treatment for ALL (Dupuis et al., 2016; Leibring & Anderzén‐Carlsson, 2019; Myers et al., 2014). However, children's experiences of support in managing their fears have not been studied from their perspective. It is reasonable to believe that their needs for support change over time, as do their fears and their own abilities to cope (Leibring & Anderzén‐Carlsson, 2019).
2. BACKGROUND
2.1. Experiences of fear and coping
Needle‐related fear has been reported as common in children of various ages (Coyne, 2006; Leibring & Anderzén‐Carlsson, 2019; Lööf et al., 2019; Salmela et al., 2009; Taddio & McMurtry, 2015). In a group of healthy 4‐to‐6‐year‐olds recruited from kindergarten and a similar group recruited from a surgical ward, more than 90% of the children had at least one experience of fear in connection to a hospital visit. The children reported fears about pain, sample‐taking and injections; however, the healthy children reported fewer fears than those recruited from the hospital setting (Salmela et al., 2009). Similarly Lööf et al. (2019), reported that 4‐to‐13‐year‐olds recalled previous negative needle‐related experiences and were thus afraid of experiencing the same again during later hospitalizations. Coyne (2006) reported that somewhat older children (7–14 years) also had fears about blood tests and injections. Despite the similarities in their fears, children's hospital‐related experiences vary, as do their needs and wishes (Lindeke et al., 2006). Fear of needle‐related procedures such as immunizations and venous sample collection could have a long‐lasting impact on children, possibly resulting in their refusal of subsequent treatments (Taddio & McMurtry, 2015). Being hospitalized as a child also implies a changed life situation. Both the unfamiliar surroundings and the separation from their parents can cause anxiety and fear. Loss of autonomy is also common during hospitalization, which could further add to the experience of anxiety and fear (Coyne, 2006).
A diagnosis of ALL often causes anxiety and fear for the entire family (Muskat et al., 2017). Young children (5–9 years) with ALL, like other populations of children, have been found to be afraid of needles, feeding tubes, adhesive‐tape removal, having to swallow tablets and various physical changes caused by ALL. Their fears vary over the course of treatment (Leibring & Anderzén‐Carlsson, 2019), and early hospital experiences, age and individual traits all affect those fears (Han et al., 2011).
Children can, however, develop and use coping strategies, which have been classified differently by different researchers. Salmela et al. (2010) divided such strategies into problem‐oriented coping, emotional coping and function‐oriented coping; in children with ALL, Leibring and Anderzén‐Carlsson (2019) identified that cognitive, emotional and functional strategies developed during the course of treatment. Han et al. (2017) categorized the strategies of children with acute leukaemia as dependence on oneself, dependence on professionals and dependence on parents. Coping strategies in children develop with age and are often more differentiated in older children. Preschool age children often seek support from adults (Zimmer‐Gembeck & Skinner, 2011).
2.2. Support
Support and security from adults are generally important to a child under stress (Lööf et al., 2019). Thus, paediatric healthcare professionals have an important role in empowering fearful children (Kleye et al., 2021). Children can be reassured when healthcare professionals ask about and adapt to their preferences or offer them information (Kleye et al., 2021; Lööf et al., 2019). Humour and small gifts are valued rewards for undergoing surgery (Lööf et al., 2019), and children also like to be distracted (Kleye et al., 2021; Lööf et al., 2019) by games (Kleye et al., 2021), toys, films or social media interactions with friends (Lööf et al., 2019). Imaginal coping, in which the child interacts with the one providing the distraction, is another specific distraction technique (Rindstedt, 2014).
Healthcare professionals should be alert to the emotional and informational needs of hospitalized children (Coyne & Kirwan, 2012). Understanding information and having positive interactions with healthcare providers have been related to feelings of security and trust in children undergoing surgery (Lööf et al., 2019). Having good communications with the professionals helps the children ask about their condition and understand their illness and treatment regimens (Coyne & Kirwan, 2012; Pelander & Leino‐Kilpi, 2010). This, in turn, could result in less stress for the child (Coyne & Kirwan, 2012). Similarly, children's discomfort with medical procedures decreased when healthcare professionals listened to them, gave them information and acknowledged their individual needs (Kassa et al., 2017). In one study (Pelander & Leino‐Kilpi, 2010), children were reported to become less stressed when allowed to participate in their care and to feel respected and acknowledged; being separated from their family, however, was reported to be one of children's worst experiences of hospitalization. When healthcare professionals are entertaining and inventive, they can support children and decrease their hospital‐related distress (Pelander & Leino‐Kilpi, 2010). Opportunities to play are also important to children in the hospital environment (Coyne & Kirwan, 2012).
Children suffering from leukaemia, specifically, need support throughout (Han et al., 2014) and after termination of their treatment (Pålsson et al., 2017), including psychosocial support to endure both the illness itself and the treatment (Sitaresmi et al., 2008). The needs of children with cancer do not differ much from those described for other children in the healthcare system. Healthcare professionals are important for offering information and allowing children to participate in their own care (Darcy et al., 2014). Han et al. (2014) reported that children with ALL who were more communicative with their parents and healthcare professionals from the beginning received more information about their illness than less communicative children. They also found that healthcare professionals could offer support by listening to the child and being emotionally available (Han et al., 2014). Younger children with leukaemia need more parental support than older children (Han et al., 2017). Parents are important in improving children's negative experiences of hospitalization (Coyne, 2006; Kassa et al., 2017).
To summarize, children with ALL are known to experience fear during their treatment and to develop their own coping strategies. Nevertheless, like all children, they also need support from adults to manage their fears. What supports these children identify as beneficial have been less described, but such knowledge is important for healthcare professionals, who offer support both to children and help to parents in supporting their children during treatment.
3. AIM
The aim of the study was to describe the types of support young children experience as helpful in coping with their fears during treatment for ALL. We focused specifically on support from parents and healthcare professionals.
3.1. Research question
What do children aged 5–9 experience as supportive in managing fear at different time points during their treatment for ALL?
4. METHOD
4.1. Design
This study had a longitudinal descriptive qualitative design. Data were collected through one to three individual interviews and analysed using the matrix‐based qualitative analysis described by Miles et al. (2014). This study is part of a larger longitudinal project about fear in children aged 5–18 years being treated for ALL.
4.2. Sample and setting
Recruitment took place during 2011–2014 with the assistance of all six regional oncology centres for children in Sweden. In this study, one designated nurse was assigned to inform all newly diagnosed children aged 5–9 years about the study and invite them to participate. There were no exclusion criteria for this study. If both the child and parents consented, the nurse shared their contact details with one of the researchers. The last author contacted those families who had agreed, offered additional information, asked them to provide informed consent for the child to be interviewed and scheduled a time and place for the first interview. All children provided their written assent. In total, 13 children (10 boys, three girls) aged 5–9 years at the first interview agreed to participate. Three of the children had another first language, but spoke Swedish fluently and thus all interviews were conducted in Swedish.
The study was approved by the Regional Ethical Review Board in Uppsala (registration number: 2010/195).
4.3. Data collection
The children participated in one to three interviews during their treatment for ALL. The first interview was conducted approximately 2 months after diagnosis, the second after one year and the third at the end of treatment, about 2.5 years after diagnosis. In total, 35 interviews were performed by the last author, a paediatric nurse and experienced researcher with no previous professional contact with the children. The interviews were held at a setting chosen by the families (hospital, home or café), lasted from 5–72 min (mean: 35 min) and were digitally recorded and transcribed by an experienced secretary.
The interviews were adapted to the age and development of each child (Kortesluoma et al., 2003), but all asked about the children's fears, how they had coped with them (presented elsewhere) and what support helped them with those fears. During the interviews, the children were encouraged to draw pictures of the situations they described. This assignment was voluntary; the drawings were not subject to analysis, but helped the researcher to frame follow‐up questions and the child to keep focus. At the end of the first and second interviews, the children were asked whether the researcher could contact them again for the scheduled follow‐up interview. Data were collected from January 2011 to November 2016.
4.4. Data analysis
As the data were quite manifest and we wanted to present a longitudinal perspective, we used a qualitative matrix methodology inspired by that of Miles et al. (2014). First, all interviews were read in their entirety and the first author used different coloured markers to highlight excerpts answering the research question and distinguish the various actors. Case‐specific matrices were then created in which the first author inserted all of the text mentioning support from various actors during the three interview times. Text was inserted as either direct quotations or paraphrases. Cross‐case matrices were then created in which data from all children (from the case‐specific matrices) were inserted; see Figure 1 for an example of two children's reports of support from healthcare staff and their parents.
FIGURE 1.
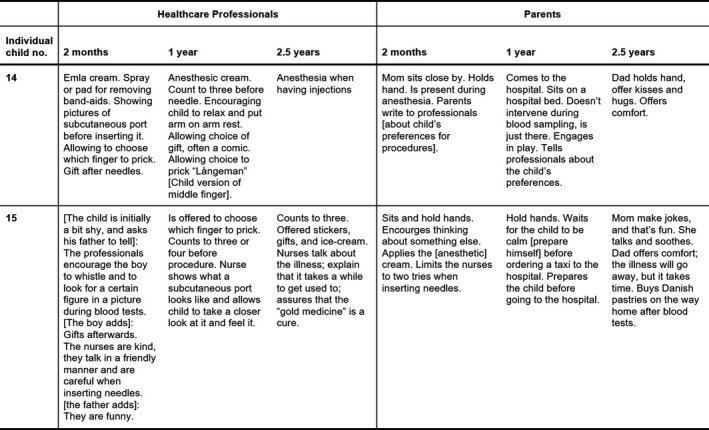
Examples of text from the cross‐case matrix. All supports mentioned in the interviews as decreasing fear, related to healthcare professionals and parents were inserted in the cross‐case matrix. The text was paraphrased or quoted directly
Through visual examination of the data, it was possible to identify some recurrent abstract patterns that were used as headings in two final matrices: one for support from parents, and one for support from healthcare professionals. Under each heading, we marked whether each child had mentioned each of the different aspects of support, which allowed us to count how many children had described each type of support over time (Table 1).
TABLE 1.
An example of a cross‐case summary matrix, illustrating the number of children reporting about the support of parental closeness and advocacy
| Closeness | Advocacy | |||||
|---|---|---|---|---|---|---|
| 2 months | 1 year | 2.5 years | 2 months | 1 year | 2.5 years | |
| Number of participants | 11 | 13 | 11 | 11 | 13 | 11 |
| Child no: 2 | 1 | 1 | 1 | |||
| Child no: 3 | 1 | 1 | 1 | |||
| Child no: 5 | 1 | 1 | 1 | 1 | ||
| Child no: 7 | 1 | 1 | 1 | 1 | ||
| Child no: 10 | 1 | 1 | 1 | |||
| Child no: 12 | 1 | 1 | — | 1 | — | |
| Child no: 13 | 1 | 1 | 1 | 1 | ||
| Child no: 14 | 1 | 1 | 1 | 1 | ||
| Child no: 15 | 1 | 1 | 1 | |||
| Child no: 16 | 1 | 1 | 1 | |||
| Child no: 18 | — | 1 | — | — | 1 | — |
| Child no: 21 | 1 | 1 | 1 | |||
| Child no: 22 | — | 1 | 1 | — | ||
| Total | 11 | 12 | 9 | 4 | 4 | 1 |
These matrices, together with the first cross‐case matrix, were used to write up the findings. The interview text was then used again to check the final accuracy of the findings. The first author was responsible for the analysis about the healthcare pofessionals; the second author validated all the text about this in the matrices and analysed parental support.
5. FINDINGS
The findings are presented below in terms of who offered various types support. We describe parental support first, then support from healthcare staff. We start each section with the support described most frequently, followed by the other supports in diminishing order of the number of children who reported them.
5.1. Parental support
An overview of the parental supports found to lessen fear is presented in Figure 2.
FIGURE 2.

Reported support from parents at different time points
5.1.1. Closeness (all 13 children)
All children‐reported feeling supported by their parents’ physical and emotional closeness. Their parents’ presence eased their fears about the medical procedures and their existential fears. The children mainly reported physical contact with parents, such holding hands during blood sampling, cuddling, sitting in their laps or being hugged when they were frightened. Physical contact was the most frequently reported aspect during the first interview and remained the most mentioned in later interviews. Children also reported feeling supported by having their parents in the same room during a procedure, keeping them company or sitting on a chair nearby. Parental presence, but not physical contact, was most frequently mentioned during the second interview. After 2.5 years, the majority of the children interviewed still found this a valuable source of support. Having parents present during anesthetization was found supportive by 3/11 children in the first interview and one child in each of the two later interviews: “Mom and Dad are always there when they put me to sleep [administer anesthesia]. They hold my hand and say ‘Sleep well,’ or something like that.” (13:2). Three children slept in the same bed as their parent to feel their supportive closeness. Having both parents stay at the hospital was also important.
Besides mentioning physical closeness, five of the children explicitly reported parents offering them comfort and security The children found it hard to elaborate on what they meant by comfort and security, but they used these words when describing the supportive actions of their parents.
5.1.2. Facilitating participation (10 children)
The second most reported support from parents was facilitating the child's participation in their own treatment and care. This was done in many ways, most often reported on the first occasion, but also in the two later interviews. The single most important aspect of facilitating participation, mentioned by nine of the 13 children, was helping the child find strategies to endure the procedures: “Mom usually says that I should try to calm down and relax.” (21:1).
Facilitating participation was also described in terms of allowing the child to decide on various matters (such as who would accompany them in the ambulance or at the hospital) and deferring to the children's wishes by providing asked‐for support or accepting their preferred way of doing things, such as removing an adhesive dressing.
Another way parents were regarded as supportive was in helping the child to prepare for treatment and care, for example by reading them a book about a certain examination or giving them a reward after treatment: “… afterward, Dad and I go and buy a Danish pastry.” (15:3). One child's parents played ‘hospital’ to support the child in processing their experience. Finally, one child reported their parent giving a blood sample before the child, and another reported their parent taking photographs so they could discuss what the child had undergone.
5.1.3. Advocacy (nine children)
The third most often mentioned parental support was advocacy, although it was less mentioned at each time point. Parents acted as their children's advocates by verbally expressing the child's fears, needs or wishes to healthcare staff, protecting the child from seeing the needle during injections and disallowing further blood sampling or injections after the first try or two did not succeed. “If they want to put a needle in my arm, then Mom says ‘no’. She wouldn't allow them to do that.” (16:3).
5.1.4. Distraction (six children) and talking about children's fears (six children)
An equal number of children reported feeling supported by parents distracting them or talking with them about their fears. Distraction was most often described as helpful during needle‐related procedures. At such times, parents could read a story, allow the child to play with their mobile phones, play a game or make the child laugh. “Mom and Dad usually talk to me and try to make me laugh [during needle‐related procedures].” (7:2).
5.1.5. Assisting healthcare staff to alleviate pain and fear (five children)
When describing parents assisting healthcare staff to alleviate their distress, four children mentioned parents’ applying the topical anaesthetic cream used before blood sampling. It was also supportive when a mother inserted a nasogastric tube at home instead of the child having to go to the hospital, when one father found a coating to put on tablets to make them easier to swallow and when one mother suggested the staff give her child Midozalam before needle‐related procedures.
5.1.6. Restraining the child (five children)
Five children reported feeling supported by parents who used physical or verbal force to make them comply with certain procedures. The children who reported physical restraint described parents who held one of the child's legs during an injection or held the child firmly in their lap during blood tests. Three of the children talked about this in the first interview, and one at each of the other time points:
#21:3: Well, they held me. Mom had to hold me. I sat on her lap, then they held me and sort of talked to me… …I mean, I guess she had to hold me… …She was sort of calm, and she did not hold very firmly, more like I was supposed to feel safe and secure, yet she also held me to stop me from running away… …Sort of firmly… I don't like being held against my will, but (laughter), but then they [the nurses] managed to draw some blood, and I didn't have to be horrified [at the idea of being given the needle] any more.
Interviewer: What would it have been like if it was a nurse who held you?
# 21:3: I would have been pissed off and told her to let go of me. It would have made me so angry. I would have yelled at her and said that she was not at all kind. It’s quite different if one’s parents are the ones holding. Because that’s better. They are my parents and they want what’s best for me. Well, the nurses do too, but it would be strange if they… One doesn’t know them as well.
5.1.7. Other forms of support mentioned by one to four children
Four children mentioned feeling supported when their parents played with them. This was mentioned only occasionally. The parents also assured the children that their treatment would cure them and that things would get better and they helped the children with practical issues. Three children reported feeling supported when parents provided information about the illness and its consequences to classmates at school and contacted teachers when the other children were too pushy or even teased the child. Providing information at school was mentioned only in the later interviews.
5.2. Support from healthcare professionals
A longitudinal overview of support from healthcare professionals found to lessen fear is presented in Figure 3.
FIGURE 3.

Reported support from professionals during the treatment period
5.2.1. Facilitating participation (all 13 children)
The children felt supported by healthcare professionals facilitating their participation in their own care or treatment. All children expressed in at least at one interview that they wanted to take an active role. This was most prominent at one year into treatment.
The healthcare professionals facilitated children's participation in care by informing them about the illness and treatment plan and asking questions to ensure the child understood, showing them the equipment that would be used and allowing the child to decide whether to proceed with painful and scary procedures: “She asked me every time she tried to get some blood [and was unsuccessful] if she could try again or if she had to stop.” (7:3). Another important aspect of participation was when the physician informed the child first, before turning to the parents: “… That's good, first talking to me, or rather the children, because they are the ones in focus, because they are the ones who are ill. That's what I like about him [a named physician].” (21:3).
Participation was encouraged when the healthcare professionals offered a choice between various alternatives. The children also felt supported in their wish to participate when the healthcare professionals told the truth. One child reported feeling betrayed when a nurse removed an intravenous catheter, having said that she should only wanted to look at it: “What she did was actually not good!” (10:1). Subsequently, this child was supported by his mother in writing a book telling the healthcare professionals about how he wished to be treated: “I don't want them to do this, and I want them to get to know me and my preferences….” (10:2). This further increased his participation in his own care. Another child found the healthcare professionals to be supportive when they allowed him to prick his own finger. The professionals informed the child how to do it and the boy succeeded despite feeling a bit hesitant and frightened: “… first I didn't want to do it. But then, I started to proceed, and said, ‘I will finger‐prick when I have counted to three.’” (3:2).
During the first interview, one child said it was supportive when healthcare professionals held his legs when inserting a nasogastric tube, which helped him to endure the procedure: “Then a nurse joined in and held my legs, so that I couldn't kick. And meanwhile, they managed to put the tube in place.” (3:1).
5.2.2. Relieving pain and fear with medication (10 children)
Most of the children discussed how the healthcare professionals had relieved their pain and/or fear during treatment through various medications. The children had experienced pain relief through nitrous oxide, topical anaesthetic cream (Emla), general anesthesia, Midozalam (which they called “dizzy medicine”) and undefined intravenous medication.
It was also supportive when healthcare professionals not only administered topical anaesthetic cream, but also monitored its effect: “Yes, they usually pinch me here [points to arm] and then here, and then I know it's working.” (3:3). Another child described his experience with nitrous oxide: “… and then they usually offer me some, well, some nitrous oxide, and then I’m totally lost.” (7:2).
5.2.3. Rewarding (nine children)
In total, nine children mentioned receiving a small token as a reward for enduring various treatments, for example blood sampling and injections. This support was especially appreciated at the beginning of treatment and after one year; it did not seem as important at the end of treatment. One boy reported being cheered up by being offered a small gift from the gift basket: “And then you feel a bit more happy.” (5:2). A negative aspect of having blood samples taken in the patient's room rather than the treatment room was that the healthcare professionals often forgot to bring such a gift.
5.2.4. Being careful and kind (nine children)
During the entire treatment period, the children mentioned that they felt supported when the healthcare professionals were kind to them. This was often regarded as a personal trait and was thus related to the importance of continuity. The children wanted the professionals to act carefully and not harshly when caring for them. They wanted the professionals to use care when removing adhesive dressings and be gentle when collecting blood samples or giving injections. At the first interview, one child said, “They talk to me… yes and they are gentle when injecting.” (15:1). Another child found it supportive when the nurses were kind and hid what they were doing during blood sampling, so that she did not have to see.
Being playful and permitting to the child to play tricks was another aspect of being kind, a professional trait the children mentioned as a supportive. It was equally appreciated throughout the entire illness trajectory and mentioned by about half the children. Children described “being playful” as staff joking with them, dressing up as different animals or played ball with the child. Two months into treatment, one child said: “Yes, she speaks silly… Once she said, when we were leaving, that I should stay with her. And once she dressed up like a giraffe.” (13:1). Even though this did not distract the child enough to ignore a needle‐related procedure, the child nevertheless viewed the occasion as somewhat positive. The same child, in the last interview, revealed longing for the fun nurses and experiencing it as positive to meet with them: “She [the nurse] says that she is a vampire, and that's why she collects blood… It makes me happy to see her.” (13:3). Yet another child revealed in his last interview that the professionals joked with him and added salt to his lemonade, and a girl said that she found it supportive when the healthcare professionals called her by a fun nick‐name and played football with her in the middle of the night. “Then, even in the middle of the night, at about 10.30, or 11.30 or something, he played ball with me.” (18:2).
5.2.5. Facilitating children's play (nine children)
Another action of healthcare professionals that children experienced as supportive was when they made it possible for the children to play. Play therapy was central to this support. The children described various activities, such as playing hospital, playing parlour games and enjoying free play in the play hall. The children appreciated the hospital clowns, and some liked playing with other children diagnosed with leukaemia. One girl reported her hospital stay as mostly boring, “…but at play therapy, one could play, and in one room one could color.” (16:1).
The children mentioned the importance of having a good environment to play in. They found that to be a support against boredom as well as fear. One young boy compared his experience of being in‐patient at two different hospitals. At one of the hospitals, children with leukaemia were allowed to move around and play anywhere, but at the other, they had to stay in their rooms. He thought that this was not good for him: “…. All the tummy flus [children with gastric flu] can move around freely and all children with leukaemia have to be locked in, in a very, very tiny room. And the best medication for me is surely to move around…” (3:1). Another child described being frustrated when the play therapy room was locked and healthcare professionals on the ward would not let her in.
Difficulties playing with classmates were also mentioned. One child described feeling supported when a contact nurse gave people at school, including the other children, information necessary to understand the implications of leukaemia. This allowed classmates to understand why the child could not run as fast as the others during play.
5.2.6. Distracting (seven children)
Especially at the beginning of treatment, the children felt supported when healthcare professionals distracted them from the various treatments and tests they were undergoing. One way of distraction was when the healthcare professionals told stories. One boy said, “Yes, there are usually two [nurses]. One tries to make me think of anything but the syringe, and the other is the one collecting blood. So, that's pretty good.” (7:2). Another child described being offered a lollipop while the nurse removed some adhesive tape: “I suck the lollipop, and she removes the adhesive. And it doesn't hurt as much.” (5:2). One child reported that the healthcare professionals had taught him to whistle, and they encouraged him to whistle to distract himself when undergoing a procedure.
Professionals could be helped by the environment to distract children during treatments and tests. The children described treatment rooms filled with enjoyable things that healthcare professionals encouraged them to look at or search for specific details. These could for example be trolls or hanging puzzles or pictures. One child, at his last interview, told about preferring procedures in the treatment room because of the various things to focus on: “Yes, they have, have some kind of a troll that you can look at, and there is a puzzle on the wall picturing a crazy hospital” (13:3).
5.2.7. Continuity of care (six children)
About half the children described feeling supported by seeing the same healthcare professionals each time they visited the hospital. Such continuity of care made the children feel safe and secure, and it decreased their fears. Furthermore, continuity enabled the children to establish relationships with the professionals. One child said, “It's the best if they [the professionals] are the same,” (16:1) and another, “When they know me, they know how I want things to be done… they are not strangers, no, I’ve known them for two and a half years. They are sort of friends.” (7:3).
One girl revealed that such continuity also made it easier for her to ask questions, because when she knew the healthcare professionals, she felt more secure. Knowing that the professionals were experienced and knowledgeable about the tasks they performed was another aspect of continuity, which was supportive to the children.
5.2.8. Encouraging the child (five children)
Children felt supported when healthcare professionals encouraged them. Most of the children who mentioned this did so during the last interview, as they looked back over their entire treatment period. Such encouragement helped the children endure needle‐related procedures, physiotherapy and individual training through reassurances that such measures would work to make them well and bring back the walking strength they had lost to the complications of treatment. General pep‐talks were also considered supportive. “When I am afraid and don't want to undergo the blood‐test, they encourage me, and says that it's easier to do it now, instead of postponing it, and so on.” (7:3). One nurse supported a boy by sharing her experience as a nurse: “…it will take some time, but finally you will get used to this [undergoing treatments and tests].” (15:3), and another boy felt supported when a professional said, “Only you can manage this, come on, you have to…,” (10:3).
One boy drew a picture during his first interview and said that the “gold‐medicine” would cure him. The healthcare professionals had told him so, and it encouraged him to believe that the medicine would beat the cancer cells. Another child shared what the physiotherapist and the physician had said to him about his walking difficulties: “If you keep on training, you will be able to walk again… after a little while.” (7:2). For children to be helped by these encouraging statements, however, they must be able to comprehend them. One child revealed some difficulties with that and said, “Sometimes, I cannot understand what he [the doctor] says, and he talks too fast.” (12:1).
6. DISCUSSION
The aim of the study was to describe young children's experiences of support related to their fears during treatment for ALL. The focus was specifically on support from parents and healthcare professionals. The results indicate that children's need for support varies during the treatment, as they highlight various beneficial measures at different time in the treatment period (Figures 2 and 3). However, having their parents close, being able to participate in their own care, and having pain relief were central support to the majority of the children. Closeness with parents was important from both an existential and a practical point of view, as they could soothe all types of fear as well as make treatments and tests endurable. Most of the support from healthcare professionals was related to treatment and tests, and less focused on existential issues, although the line between these two aspects is sometimes blurry and they can overlap. Some types of support were appreciated from both parents and healthcare professionals, such as facilitating participation, administrating medication to relieve fear, distraction, being playful and being encouraging.
6.1. Parental support
Parental support had an impact on the child's emotional, social and physical wellbeing, and in this study closeness seemed to be the most important aspect of parental support, and children preferred to have both parents present. Parental support has previously been identified as a very important factor in the psychological wellbeing of young children suffering from leukaemia (Enskär et al., 2014; Han et al., 2017). As the children wished to be able to have their family stay with them, it is important to have family rooms in paediatric departments, to allow siblings and parents to stay close to and support children during their hospital stays (Kassa et al., 2017). The finding about need for closeness is not unique, it has been identified also in previous studies (Björk et al., 2006; Enskär et al., 1997; Kars et al., 2008). However, this need changed somewhat over the treatment trajectory, from physical closeness to general proximity. The reasons for this pattern can be more than one; the child has grown older, developed coping strategies or has become used to procedures (Leibring & Anderzén‐Carlsson, 2019). It could also be that the treatment is less intense later into the treatment protocol, with less invasive hospitalizations and tests (Leibring & Anderzén‐Carlsson, 2019; Toft et al., 2018).
It is an obvious finding that facilitating participation in treatment and care is of major importance for supporting children by preventing and decreasing fear. The parents typically helped the children find strategies to endure frightening procedures and offered distraction during procedures and hospital stays. Previous literature on valuable parental support is sparse. Instead, parental support has been described in the light of children's coping. For example, Han et al. (2017) categorized it as children's dependence on parents and Zimmer‐Gembeck and Skinner (2011) concluded that preschool age children often seek support from adults.
For the parent to offer support to their child they need support themselves (Björk et al., 2006; Miller et al., 2009). For example, parents of sick children need emotional support and honest information (McGrath, 2002), which can be given through various modes. Wang et al. (2016) found that parents were helped by using a smartphone app that decreased their distress by offering knowledge and information about how to support a child with ALL. To the best of our knowledge, the literature on how to support parents to support their child with ALL is sparse. This should be considered when planning future studies within this context.
6.2. Professional support
To support children, healthcare professionals have to be sensitive to the individual child's preferred support (Harder et al., 2011). All children in this study expressed that it was supportive to participate in their care. What they found supportive about being able to participate in their care and treatment was not deciding on major treatment issues, but rather feeling informed enabled to choose between different alternatives regarding their treatments and tests, and neither forced nor deceived.
Medical procedures often created fear and yet, the children described their wish to be active agents and they wanted the healthcare professionals to be honest. Children can react to frightening procedures by becoming upset and showing resistance to what they are about to undergo (Bray et al., 2019). Maslak et al. (2019) found that 4‐to 7‐year‐olds experience greater distress during invasive procedures than both younger and older children. In line with the present findings, they concluded that allowing children to choose the type of support they wish to use in these situations decrease their distress (Maslak et al., 2019). The importance of listening to children's voices about treatment and care have also been highlighted by others (e.g., Anderzén‐Carlsson et al., 2007; Coyne et al., 2016; Kassa et al., 2017; Kleye et al., 2021; Lööf et al., 2019). However, Moore and Kirk (2010) and Coyne (2006) have concluded that evidence‐based guidelines for children's participation in their care are lacking, which is a potential threat for optimal support to children who are ill.
The findings reveal that what was found supportive with regard to participation in care varied. The professionals initially supported the children by informing them and showing what equipment would be used during the procedure. One tool found to decrease children's fear is the Interactive Communication Tool for Activities. This is a digital tool showing children various procedures or settings, such as a needle procedure or a waiting room (Stålberg et al., 2018). No such device was mentioned in the current study, instead non‐digital pedagogical devices were mentioned by the children. Digital tools might not have been as common during the data‐collection period as they are today.
Later in the treatment, the support children appreciated from healthcare professionals for facilitating participation was more related to their paying attention to the child's needs and wishes and ensuring that the child understood the information provided. However, the findings indicated that it sometimes could be hard for children to understand information given by the professionals. Therefore, to facilitate children in being active agents in their own care, there is a need to optimize communications by focusing on the child's perspective. A literature review identified that the psychological health of children with leukaemia worsens if they are unable to comprehend their illness and treatment (Willingham Piersol et al., 2008). Thus, it is important for the professionals to be attentive to whether the child understand given information. The fifth article of the European Association for Children in Hospital emphasizes the importance of healthcare professionals’ attentiveness to their patients and responsibility for building rapport and trust and states that children and their parents have the right to receive information before treatment and care (European Association for Children in Hospital). According to Hallström and Elander (2004), children are always able to participate in decisions, although they are not mature enough to do this independently as they cannot fully comprehend the consequences of care decisions. The ability to participate in decisions, despite young age was confirmed in the current study.
Another aspect that was supportive and increased the children's willingness to participate in care was healthcare professionals offering small rewards after a procedure. The importance of this gesture, however, decreased during the illness trajectory. We do not know why, but perhaps it was because the children got used to the treatment, and also because their coping strategies developed (Leibring & Anderzén‐Carlsson, 2019).
Being playful and offering distraction were two other aspects of support that could decrease children's fears. In the hospital environment, the children described these aspects in terms of play therapy, hospital clowns, distracting décor and professionals joking with them. Previous research has highlighted the benefit of distraction (Bray et al., 2019) as well as the importance of play for children who are ill (Depianti et al., 2018; Enskär et al., 1997; Gariépy & Howe, 2003; Karlsson et al., 2019; Lindeke et al., 2006). Play is important for children's general development and health (Rejane Rolim Gomes et al., 2018). Facilitating children's play in the hospital has been shown to decrease their negative experiences and offer them a sense of control. Healthcare professionals can facilitate play by initiating various activities (Depianti et al., 2018; Jones, 2018; Koukourikos et al., 2015), encouraging parents to engage in playful activities with their children and encouraging children to bring favourite toys to the hospital (Koukourikos et al., 2015). Along with being able to play, the children also wished to be able to move around the ward. Healthcare facilities need to allow personal space and dignity to patients and their families (Lambert et al., 2014). It is therefore important on an organizational level to listen to the voices of children when planning and developing paediatric in‐patient settings to provide a more child‐centred environment (Coyne, 2006). Children as young as 6 years old have been found able to participate in quality‐improvement measures related to the hospital environment if given the opportunity (Schalkers et al., 2015).
The literature on what young children find to be supportive when fearful under treatment for ALL is sparse. Nevertheless, much of the valued support have previously been described in the paediatric literature, from professionals’ perspective, when describing how to best care for ill children. What this study adds is that the children value this experience‐based support.
6.3. Restraining the child
The issue of physically restraining children during medical procedures has been discussed by scholars in previous literature. Therefore, we find it important to highlight the children's perspective on this topic. Bray et al. (2018) showed in their study that it is still common for healthcare professionals from Australia, New Zealand and UK to restrain children without their consent or that of their parents, but the issue of parental restraint was not studied there. However, in another study it was identified that parents first and foremost tried to maintain their children's wellbeing, but if children were too resistant, parents prioritized their physical health and could force a child to undergo a procedure against their will (Anderzén‐Carlsson et al., 2010). So, what did the children think about being restrained? Five of 13 children reported that on one or more occasions they had found it supportive when a parent had physically restrained them during a procedure or verbally forced them to accept it. Their opinions varied, however, on whether or not it was acceptable for a professional to restrain them. One child said specifically that it was good when the parent held firmly, but that it was not okay if a professional did. Another child, however, found it supportive to be held tight by healthcare professionals. Sahlberg et al. (2020) found that when it was necessary to physically restrain a child, only the healthcare professions should do so, not the parents. They also highlighted the importance of simultaneous distraction during such restraint and the necessity of a policy to stop any restraint that is not working. In another study, Bray et al. (2019) showed that healthcare professionals first try to persuade children to undergo procedures by distraction and information, but if this does not work, it is common to restrain the child to complete the procedure. They argue that it is a balancing act to decide what is the right thing to do in such a situation. There is a risk of overruling the child's voice and rights, so they suggest taking a clinical pause to allow the child to participate in deciding the best way to continue. An even better alternative is to discuss the procedure prior to attempting it.
The present findings show various preferences about being restrained, and we believe it is important to give voice to the children's preferences at various time points. The results show that being restrained when undergoing a frightening treatment could be regarded as positive by some children, who interpreted it as being in the safe haven of their parents.
6.4. The connection between support and coping
Reflecting on the findings in this study and the literature on coping (Han et al., 2017; Salmela et al., 2010), we recognize an obvious connection between the concepts of support and coping. In a previous study within the larger project (Leibring & Anderzén‐Carlsson, 2019), the same group of children described their fears and their ways of coping. There, the children described counting backward from three before allowing a procedure. In this current study, we viewed the same situation from a different perspective, the children's perceptions of parental and professional support as they suggested the child count backward when undergoing a procedure. We also recognize that the healthcare professionals adapt to the children's preferred strategies, which is supportive and in line with the child's coping strategy of requiring that professionals act in accordance with their wishes. Han et al. (2017) also acknowledge the connection between coping and support and highlight children's dependence on the support of their parents and the healthcare professionals. Delvecchio et al. (2019) determined that hospitalized children used more support‐seeking strategies than non‐hospitalized children. Likewise, hospitalized children reported a greater need of support than the non‐hospitalized children.
This connection between coping and support indicates that children's ability to use the coping strategies described by Han et al. (2017) depends on their interacting with another person who offers them support. This study shows that this other person could be either a parent or a healthcare professional, both of whom play important, but different, roles in supporting children in the hospital.
6.5. Strengths and limitations
The major strength of this study is the voice it gives to the children in describing what they regard as beneficial support during treatment for ALL. Although the children were quite young, they were willing and able to share their preferences. The idea of using a drawing as a starting point for the discussion was useful in some interviews, but others were not interested in this activity. Another strength of the study is its longitudinal design, which enabled rich data because the children got to know the researcher during the repeated interviews, and the second and third interview sessions became more predictable and comfortable for them. The longitudinal design also allowed us to determine which supports were considered most important at different times and across all interviews. We could not, however, determine whether changes in preferences for support varied because of the children's growing experience of being ill and under treatment, changes in treatment as determined by the treatment protocol or the child's development over the study time. It is likely that numerous factors are involved in this change. The main challenge in the interviews was encouraging the children to think about and elaborate on various types of support, for example closeness and kindness, which they regarded simply as the natural behaviour of parents and healthcare professionals. The limited number of participants could be regarded as another limitation, but the children were recruited from various cancer centres around the country and participated in repeated interviews, a total of 35, which resulted in rich data.
7. CONCLUSION AND RELEVANCE FOR CLINICAL PRACTICE
Both parents and healthcare professionals are important to children undergoing treatment for ALL, and they have important, but different, roles in supporting those children during their illness trajectory. Although support from parents and professionals shared some aspects, some support identified as important also differed between parents and professionals. All participating children found it supportive to have their parents close to them, emotionally and physically. They also found it supportive when the parents and healthcare professionals encouraged the children to participate in their own care. This latter is in line with the United Nations Convention of the Rights of the Child. On the group level, what children experienced as supportive varied over time. Thus, healthcare professionals should acquaint themselves with each individual child´s fears and preferred type of support in order to meet their changing needs over time. They also need to know about the child's preferences about parental support in order to support the parents to help their children.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ACKNOWLEDGEMENTS
We wish to thank all the children that participated in this research, and their parents who generously shared their time and effort by arranging for us to conduct the interviews. We also wish to thank the contact nurses at the Regional Child Oncology Centres who helped with the recruitment and finally, the experienced secretaries that transcribed all the interviews and Jonas Birkelöf for assisting with the illustrations.
Leibring, I. , & Anderzén‐Carlsson, A. (2022). Young children’s experiences of support when fearful during treatment for acute lymphoblastic leukaemia—A longitudinal interview study. Nursing Open, 9, 527–540. 10.1002/nop2.1092
Funding information
The research was funded by The Swedish Childhood Cancer Foundation (Grant number PR2009‐0016)
DATA AVAILABILITY STATEMENT
Research data are not shared, due to no ethical approval to do so.
REFERENCES
- Anderzén‐Carlsson, A. , Kihlgren, M. , Skeppner, G. , & Sørlie, V. (2007). How physicians and nurses handle fear in children with cancer. Journal of Pediatric Nursing, 22(1), 71–80. 10.1016/j.pedn.2006.05.010 [DOI] [PubMed] [Google Scholar]
- Anderzén‐Carlsson, A. , Kihlgren, M. , Svantesson, M. , & Sorlie, V. (2010). Parental handling of fear in children with cancer; caring in the best interests of the child. Journal of Pediatric Nursing, 25(5), 317–326. 10.1016/j.pedn.2008.10.004 [DOI] [PubMed] [Google Scholar]
- Björk, M. , Nordström, B. , & Hallström, I. (2006). Needs of young children with cancer during their initial hospitalization: An observational study. Journal of Pediatric Oncology Nursing, 23(4), 210–219. 10.1177/1043454206289737 [DOI] [PubMed] [Google Scholar]
- Bray, L. , Carter, B. , Ford, K. , Dickinson, A. , Water, T. , & Blake, L. (2018). Holding children for procedures: An international survey of health professionals. Journal of Child Health Care, 22(2), 205–215. 10.1136/archdischild-2017-313087.41 [DOI] [PubMed] [Google Scholar]
- Bray, L. , Ford, K. , Dickinson, A. , Water, T. , Snodin, J. , & Carter, B. (2019). A qualitative study of health professionals’ views on the holding of children for clinical procedures: Constructing a balanced approach. Journal of Child Health Care, 23(1), 160–171. 10.1177/1367493518785777 [DOI] [PubMed] [Google Scholar]
- Coyne, I. (2006). Children's experiences of hospitalization. Journal of Child Health Care, 10(4), 326–336. 10.1177/1367493506067884 [DOI] [PubMed] [Google Scholar]
- Coyne, I. , Hallström, I. , & Söderbäck, M. (2016). Reframing the focus from a family‐centred to a child‐centred care approach for children’s healthcare. Journal of Child Health Care, 20(4), 494–502. 10.1177/1367493516642744 [DOI] [PubMed] [Google Scholar]
- Coyne, I. , & Kirwan, L. (2012). Ascertaining children’s wishes and feelings about hospital life. Journal of Child Health Care, 16(3), 293–304. 10.1177/1367493512443905 [DOI] [PubMed] [Google Scholar]
- Darcy, L. , Björk, M. , Enskär, K. , & Knutsson, S. (2014). The process of striving for an ordinary, everyday life, in young children living with cancer, at six months and one year post diagnosis. European Journal of Oncology Nursing, 18(6), 605–612. 10.1016/j.ejon.2014.06.006 [DOI] [PubMed] [Google Scholar]
- Darcy, L. , Björk, M. , Knutsson, S. , Granlund, M. , & Enskär, K. (2016). Following young children's health and functioning in everyday life through their cancer trajectory. Journal of Pedatric Oncology Nursing, 33(3), 173–189. 10.1177/1043454215610489 [DOI] [PubMed] [Google Scholar]
- Delvecchio, E. , Salcuni, S. , Lis, A. , Germani, A. , & Di Riso, D. (2019). Hospitalized children: Anxiety, coping strategies, and pretend play. Frontiers in Public Health, 7, 250. 10.3389/fpubh.2019.00250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depianti, J. R. B. , Melo, L. D. L. , & Ribeiro, C. A. (2018). Playing to continue being a child and freeing itself from the confinement of the hospitalization under precaution. Escola Anna Nery, 22(2), 10.1590/2177-9465-ean-2017-0313 [DOI] [Google Scholar]
- Dupuis, L. L. , Lu, X. , Mitchell, H. R. , Sung, L. , Devidas, M. , Mattano, L. A. Jr , Carroll, W. L. , Winick, N. , Hunger, S. P. , Maloney, K. W. , & Kadan‐Lottick, N. S. (2016). Anxiety, pain, and nausea during the treatment of standard‐risk childhood acute lymphoblastic leukemia: A prospective, longitudinal study from the Children's Oncology Group. Cancer, 122(7), 1116–1125. 10.1002/cncr.29876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enskär, K. , Carlsson, M. , Golsäter, M. , & Hamrin, E. (1997). Symptom distress and life situation in adolescents with cancer. Cancer Nursing, 20(1), 23–33. 10.1097/00002820-199702000-00004 [DOI] [PubMed] [Google Scholar]
- Enskär, K. , Knutsson, S. , Huus, K. , Granlund, M. , Darcy, L. , & Björk, M. (2014). A literature review of the results from nursing and psychosocial research within Swedish pediatric oncology. Journal of Nursing & Care, 3(6), 1–8. 10.4172/2167-1168.1000217 [DOI] [Google Scholar]
- EACH, the European Association for Children in Hospital . Available at: https://each‐for‐sick‐children.org. Retrieved 11 Oct 2021.
- Gariépy, N. , & Howe, N. (2003). The therapeutic power of play: Examining the play of young children with leukaemia. Child: Care, Health and Development, 29(6), 523–537. 10.1046/j.1365-2214.2003.00372.x [DOI] [PubMed] [Google Scholar]
- Hallström, I. , & Elander, G. (2004). Decision‐making during hospitalization: Parents’ and children's involvement. Journal of Clinical Nursing, 13(3), 367–375. 10.1046/j.1365-2702.2003.00877.x [DOI] [PubMed] [Google Scholar]
- Han, J. , Liu, J. E. , & Xiao, Q. (2017). Coping strategies of children treated for leukemia in China. European Journal of Oncology Nursing, 30, 43–47. 10.1016/j.ejon.2017.08.002 [DOI] [PubMed] [Google Scholar]
- Han, J. , Liu, J. E. , Xiao, Q. , Zheng, X. L. , Ma, Y. H. , & Ding, Y. M. (2011). The experiences and feelings of Chinese children living with leukemia: A qualitative study. Cancer Nursing, 34(2), 134–141. 10.1097/NCC.0b013e3181efea47 [DOI] [PubMed] [Google Scholar]
- Han, J. , Liu, J.‐E. , Zheng, X.‐L. , Ma, Y.‐H. , Xiao, Q. , & Ding, Y.‐M. (2014). Caring in nursing: Investigating the meaning of caring from the perspective of Chinese children living with leukemia. International Journal of Nursing Sciences, 1(1), 34–41. 10.1016/j.ijnss.2014.02.003 [DOI] [Google Scholar]
- Harder, M. , Christensson, K. , Coyne, I. , & Söderbäck, M. (2011). Five‐year‐old children’s tuning‐in and negotiation strategies in an immunization situation. Qualitative Health Research, 21(6), 818–829. 10.1177/1049732311400629 [DOI] [PubMed] [Google Scholar]
- Jones, M. (2018). The necessity of play for children in health care. Children's Health Care, 16(3), 142–149. 10.1207/s15326888chc1603_3 [DOI] [Google Scholar]
- Karlsson, K. , Galvin, K. , & Darcy, L. (2019). Medical procedures in children using a conceptual framework that keeps a focus on human dimensions of care–a discussion paper. International Journal of Qualitative Studies on Health and well‐being, 14(1), 1675354. 10.1080/17482631.2019.1675354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kars, M. C. , Duijnstee, M. S. H. , Pool, A. , van Delden, J. J. M. , & Grypdonck, M. H. F. (2008). Being there: Parenting the child with acute lymphoblastic leukaemia. Journal of Clinical Nursing, 17(12), 1553–1562. 10.1111/j.1365-2702.2007.02235.x [DOI] [PubMed] [Google Scholar]
- Kassa, A. M. , Engvall, G. , & Engstrand Lilja, H. (2017). Young children with severe congenital malformations (VACTERL) expressed mixed feelings about their condition and worries about needles and anaesthesia. Acta Paediatrica, 106(10), 1694–1701. 10.1111/apa.13973 [DOI] [PubMed] [Google Scholar]
- Kleye, I. , Heden, L. , Karlsson, K. , Sundler, A. J. , & Darcy, L. (2021). Children’s individual voices are required for adequate management of fear and pain during hospital care and treatment. Scandinavian Journal of Caring Sciences, 35(2), 530–537. 10.1111/scs.12865 [DOI] [PubMed] [Google Scholar]
- Kortesluoma, R. L. , Hentinen, M. , & Nikkonen, M. (2003). Conducting a qualitative child interview: Methodological considerations. Journal of Advanced Nursing, 42(5), 434–441. 10.1046/j.1365-2648.2003.02643.x [DOI] [PubMed] [Google Scholar]
- Koukourikos, K. , Tzeha, L. , Pantelidou, P. , & Tsaloglidou, A. (2015). The importance of play during hospitalization of children. Materia Socio‐Medica, 27(6), 438. 10.5455/msm.2015.27.438-441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert, V. , Coad, J. , Hicks, P. , & Glacken, M. (2014). Young children’s perspectives of ideal physical design features for hospital‐built environments. Journal of Child Health Care, 18(1), 57–71. 10.1177/1367493512473852 [DOI] [PubMed] [Google Scholar]
- Leibring, I. , & Anderzén‐Carlsson, A. (2019). Fear and coping in children 5–9 years old treated for acute lymphoblastic leukemia‐A longitudinal interview study. Journal of Pediatric Nursing, 46, e29–e36. 10.1016/j.pedn.2019.02.007 [DOI] [PubMed] [Google Scholar]
- Lindeke, L. , Nakai, M. , & Johnson, L. (2006). Capturing children's voices for quality improvement. MCN: the American Journal of Maternal/Child Nursing, 31(5), 290–295. 10.1097/00005721-200609000-00005 [DOI] [PubMed] [Google Scholar]
- Lööf, G. , Andersson‐Papadogiannakis, N. , & Silén, C. (2019). Children's own perspectives demonstrate the need to improve paediatric perioperative care. Nursing Open, 6(4), 1363–1371. 10.1002/nop2.332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslak, K. , Favara‐Scacco, C. , Barchitta, M. , Agodi, A. , Astuto, M. , Scalisi, R. , Italia, S. , Bellia, F. , Bertuna, G. , D'Amico, S. , Spina, M. , Licciardello, M. , Lo Nigro, L. , Samperi, P. , Miraglia, V. , Cannata, E. , Meli, M. , Puglisi, F. , Parisi, G. F. , … Di Cataldo, A. (2019). General anesthesia, conscious sedation, or nothing: Decision‐making by children during painful procedures. Pediatric Blood & Cancer, 66(5), e27600. 10.1002/pbc.27600 [DOI] [PubMed] [Google Scholar]
- McGrath, P. (2002). Beginning treatment for childhood acute lymphoblastic leukemia: Insights from the parents' perspective. Oncology Nursing Forum, 29(26), 988–996. 10.1188/02.ONF.988-996 [DOI] [PubMed] [Google Scholar]
- Miles, M. B. , Huberman, A. M. , & Saldaña, J. (2014). Qualitative data analysis: A methods sourcebook. Sage. [Google Scholar]
- Miller, A. R. , Condin, C. J. , McKellin, W. H. , Shaw, N. , Klassen, A. F. , & Sheps, S. (2009). Continuity of care for children with complex chronic health conditions: Parents' perspectives. BMC Health Services Research, 9(1), 242. 10.1186/1472-6963-9-242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore, L. , & Kirk, S. (2010). A literature review of children’s and young people’s participation in decisions relating to health care. Journal of Clinical Nursing, 19(15–16), 2215–2225. 10.1111/j.1365-2702.2009.03161.x [DOI] [PubMed] [Google Scholar]
- Muskat, B. , Jones, H. , Lucchetta, S. , Shama, W. , Zupanec, S. , & Greenblatt, A. (2017). The experiences of parents of pediatric patients with acute lymphoblastic leukemia, 2 months after completion of treatment. Journal of Pediatric Oncology Nursing, 34(5), 358–366. 10.1177/1043454217703594 [DOI] [PubMed] [Google Scholar]
- Myers, R. M. , Balsamo, L. , Lu, X. , Devidas, M. , Hunger, S. P. , Carroll, W. L. , Winick, N. J. , Maloney, K. W. , & Kadan‐Lottick, N. S. (2014). A prospective study of anxiety, depression, and behavioral changes in the first year after a diagnosis of childhood acute lymphoblastic leukemia: A report from the Children's Oncology Group. Cancer, 120(9), 1417–1425. 10.1002/cncr.28578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pålsson, A. , Malmström, M. , & Follin, C. (2017). Childhood leukaemia survivors' experiences of long‐term follow‐ups in an endocrine clinic – A focus‐group study. European Journal of Oncology Nursing, 26, 19–26. 10.1016/j.ejon.2016.10.006 [DOI] [PubMed] [Google Scholar]
- Pelander, T. , & Leino‐Kilpi, H. (2010). Children’s best and worst experiences during hospitalisation. Scandinavian Journal of Caring Sciences, 24(4), 726–733. 10.1111/j.1471-6712.2010.00770.x [DOI] [PubMed] [Google Scholar]
- Rejane Rolim Gomes, N. , Costa Maia, E. , & Van Deursen Varga, I. (2018). The benefits of playing for children's health: A systematic review. Artigo de revisao, 25(2), 47–51. 10.17696/2318-3691.25.2.8.867201 [DOI] [Google Scholar]
- Rindstedt, C. (2014). Children's strategies to handle cancer: A video ethnography of imaginal coping. Child: Care, Health and Development, 40(4), 580–586. 10.1111/cch.12064 [DOI] [PubMed] [Google Scholar]
- Sahlberg, S. , Karlsson, K. , & Darcy, L. (2020). Children's rights as law in Sweden–every health‐care encounter needs to meet the child's needs. Health Expectations, 23(4), 860–869. 10.1111/hex.13060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmela, M. , Salantera, S. , & Aronen, E. (2009). Child‐reported hospital fears in 4 to 6‐year‐old children. Pediatric Nursing, 35(5), 269–276, 303. 10.1111/j.1365-2214.2010.01171.x [DOI] [PubMed] [Google Scholar]
- Salmela, M. , Salantera, S. , Ruotsalainen, T. , & Aronen, E. T. (2010). Coping strategies for hospital‐related fears in pre‐school‐aged children. Journal of Paediatrics and Child Health, 46(3), 108–114. 10.1111/j.1440-1754.2009.01647.x [DOI] [PubMed] [Google Scholar]
- Schalkers, I. , Dedding, C. W. M. , & Bunders, J. F. G. (2015). ‘[I would like] a place to be alone, other than the toilet’–Children's perspectives on paediatric hospital care in the Netherlands. Health Expectations, 18(6), 2066–2078. 10.1111/hex.12174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sitaresmi, M. N. , Mostert, S. , Gundy, C. M. , Sutaryo, S. , & Veerman, A. J. P. (2008). Health‐related quality of life assessment in Indonesian childhood acute lymphoblastic leukemia. Health and Quality of Life Outcomes, 6(1), 96. 10.1186/1477-7525-6-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stålberg, A. , Sandberg, A. , Larsson, T. , Coyne, I. , & Söderbäck, M. (2018). Curious, thoughtful and affirmative—Young children's meanings of participation in healthcare situations when using an interactive communication tool. Journal of Clinical Nursing, 27(1–2), 235–246. 10.1111/jocn.13878 [DOI] [PubMed] [Google Scholar]
- Taddio, A. , & McMurtry, C. M. (2015). Psychological interventions for needle‐related procedural pain and distress in children and adolescents. Paediatrics & Child Health, 20(4), 195–196. 10.1093/pch/20.4.195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toft, N. , Birgens, H. , Abrahamsson, J. , Griskevicius, L. , Hallbook, H. , Heyman, M. , Klausen, T. W. , Jonsson, O. G. , Palk, K. , Pruunsild, K. , Quist‐Paulsen, P. , Vaitkeviciene, G. , Vettenranta, K. , Asberg, A. , Frandsen, T. L. , Marquart, H. V. , Madsen, H. O. , Noren‐Nystrom, U. , & Schmiegelow, K. (2018). Results of NOPHO ALL2008 treatment for patients aged 1–45 years with acute lymphoblastic leukemia. Leukemia, 32(3), 606–615. 10.1038/leu.2017.265 [DOI] [PubMed] [Google Scholar]
- UNICEF . (1989). Convention on the Rights of the Child: Adopted and opened for signature, ratification and accession by General Assembly resolution 44/25 of 20 November 1989 entry into force 2 September 1990, in accordance with article 49. http://www.ohchr.org/EN/ProfessionalInterest/Pages/CRC.aspx [Google Scholar]
- Wang, J. , Yao, N. , Shen, M. , Zhang, X. , Wang, Y. , Liu, Y. , Geng, Z. , & Yuan, C. (2016). Supporting caregivers of children with acute lymphoblastic leukemia via a smartphone app: A pilot study of usability and effectiveness. CIN: Computers, Informatics, Nursing, 34(11), 520–527. 10.1097/cin.0000000000000265 [DOI] [PubMed] [Google Scholar]
- Willingham Piersol, L. , Johnson, A. , Wetsel, A. , Holtzer, K. , & Walker, C. (2008). Decreasing psychological distress during the diagnosis and treatment of pediatric leukemia. Journal of Pediatric Oncology Nursing, 25(6), 323–330. 10.1177/1043454208323293 [DOI] [PubMed] [Google Scholar]
- Zimmer‐Gembeck, M. J. , & Skinner, E. A. (2011). The development of coping across childhood and adolescence: An integrative review and critique of research. International Journal of Behavioral Development, 35(1), 1–17. 10.1177/0165025410384923 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared, due to no ethical approval to do so.


