Abstract
Aims
To explore the practice effect of establishing an integrated treatment process by stroke emergency nurses in general hospitals for acute ischaemic stroke (AIS).
Design
Compared the time spent in each link before and after the establishment of AIS integrated treatment.
Methods
Since March 2016, we set up a team of emergency stroke nurses (ESN), trained and assessed the knowledge of emergency stroke, and set up a post of ESN.
Results
The median time of admission‐judgement, admission‐establishment of venous access, admission‐cranial CT examination and admission‐intravenous thrombolytic therapy was statistically significantly shortened after the implementation of the integrated treatment process of AIS coordinated by stroke emergency nurses (p < .01). The new treatment process of AIS further shortens the time of each treatment link and promotes the timeliness.
Keywords: acute ischaemic stroke, integrated process, nurses
What does this paper contribute to the wider global clinical community?
The implementation of the integrated treatment process included a team of emergency stroke nurses, trained and assessed the knowledge and skills of emergency stroke, and a post of emergency stroke nurses to coordinate the whole process of acute ischaemic stroke treatment. The implementation of the integrated treatment process of acute ischaemic stroke further shortens the time of each treatment link in hospital and promotes the timeliness and effectiveness of the treatment of acute ischaemic stroke patients.
1. INTRODUCTION
Stroke is one of the major diseases leading to disability and death in humans. Acute ischaemic stroke (AIS) accounts for about 80% of all strokes. The timeliness and effectiveness of its treatment are essential to reduce the morbidity and mortality of patients and can greatly improve the quality of life of patients and improve the prognosis (Emberson et al., 2014; Wang et al., 2019). However, the treatment of AIS involves many departments, including neurology, cerebrovascular surgery, emergency department, imaging department, interventional operating room and so on. It is urgent to strengthen the unification and management of AIS first aid and improve the treatment efficiency. The shorter the door to needle time (DNT), the earlier the vascular recanalization, the better the prognosis (Emberson et al., 2014). Continuously optimizing the process, shortening the treatment time of each link and shortening DNT are the goals that our centre has been pursuing. In August 2016, the centre began to explore the integrated treatment process of in‐hospital AIS coordinated by stroke emergency nurses and achieved good results. The introduction is as follows.
2. BACKGROUND
Stroke is one of the main diseases that cause human disability and death. Acute ischaemic stroke (AIS) is the cause of most stroke attacks, and due to the short treatment window of thrombolytic therapy, many patients cannot obtain satisfactory treatment results, resulting in high disability and death worldwide rate. Therefore, how to shorten the processing time of each link and shorten the DNT to enable fast and effective AIS emergency management, when the patient is admitted to the hospital is the crucial issue to reduce the disability rate and mortality rate. Lou et al. pointed out that there was a positive correlation between the level of professional knowledge of nurses and the quality of care of patients (Lou, 2011). Studies have shown that equipping the thrombolysis team with trained nurses and coordinating green channels can effectively improve the rate of intravenous thrombolysis and reduce intravenous thrombolysis DNT (Middleton et al., 2015). Our hospital was enrolled in the National Base for Stroke Screening and Prevention in 2013 and became the first national high‐level stroke centre in 2015. The in‐hospital treatment process of AIS was continuously optimized, which shortened the DNT to 45 min (X. Wang et al., 2015).
3. METHODS
3.1. Research design and research objects
This study is a single‐centre retrospective study. The data of the treatment time of AIS patients in hospital from August 2015–July 2018 were collected from the central database for statistical analysis. August 2015–July 2016 was the first aid nurse stage without stroke, as the pre‐operation group. August 2016–July 2017 was the trial run stage of the first aid nurse with daytime stroke, as the trial operation group. August 2017–July 2018 is the overall coordination stage for stroke emergency nurses, as the full‐day operation group. Inclusion criteria: Patients hospitalized in our department from 2015–2018 and met the following inclusion criteria were selected as study participants: 1. Patients who met the diagnostic criteria of ischaemic stroke in the Guidelines for the Diagnosis and Treatment of Acute Ischemic Stroke in China (2014). 2. No serious diseases of other organs. 3. Accompanied by family members. The study was reviewed by the hospital ethics committee and informed consent was signed with all patients.
3.2. Effect evaluation
The primary endpoint is the treatment time of each link. The treatment time of each link was collected through the information system. Radio frequency identification device (RFID) was installed in the hospital's emergency pre‐examination desk, emergency CT room and rescue room. After the patient was admitted to the hospital and judged to be suspected of stroke, he was positioned by wearing an RFID bracelet at the emergency pre‐examination desk. When the patient arrives at the emergency pre‐examination desk, emergency CT room and emergency room, the RFID hand ring automatically grabs the arrival time point and sends it to the cloud server through wireless network. The background can directly collect data analysis. Two‐dimensional codes were designed on emergency pre‐examination desk and thrombolytic medicine box, and personal digital assistant (PDA) scanning was used to record the time nodes of AIS patients' treatment.
Statistical data included time of admission‐judgement (AJT, refers to the time from admission to the stroke doctor), time of admission‐establishment of venous access (AVT, time from admission to first establishment of venous access), time of admission‐cranial CT examination (ACT, time from admission to completion of the first cranial CT examination) and median of door to needle time (DNT, time from admission to intravenous thrombolysis).
3.3. Analysis of AIS integrated treatment process
This manuscript was adherence to the SQUIRE guideline. The flow chart of AIS integrated treatment before improvement in our hospital is shown in Figure 1.
FIGURE 1.
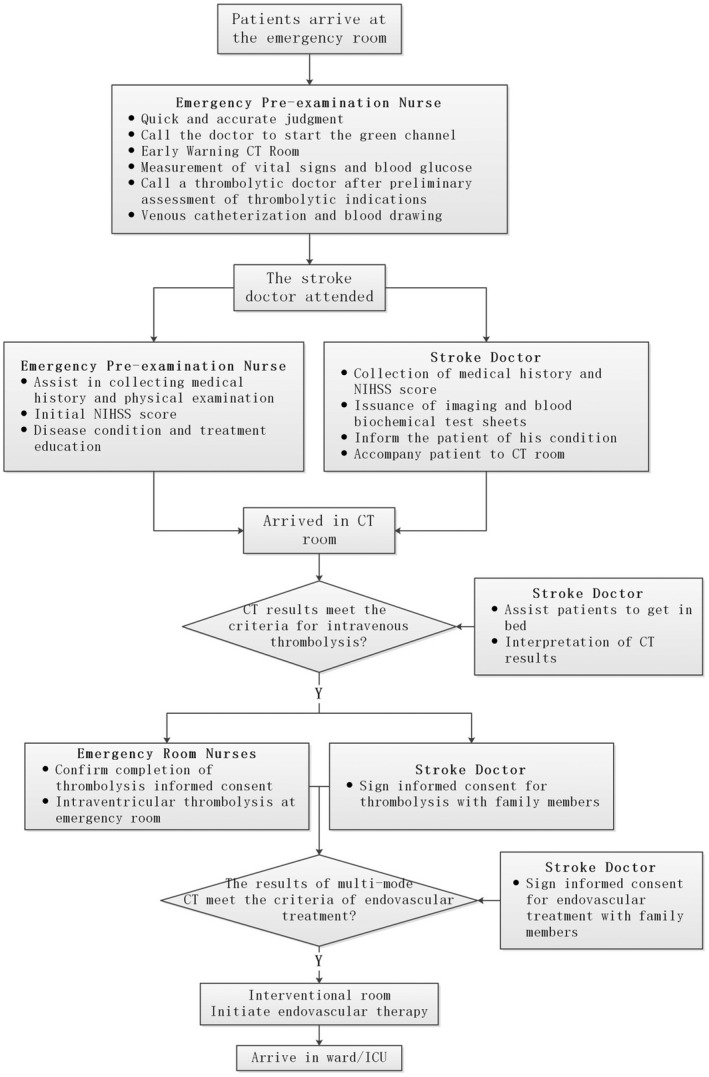
Flow chart of integrated treatment for AIS before improvement
By tracking the time nodes of each link of the treatment process through the information system, combining the current status of the treatment process and combining with the case review and analysis of the operation efficiency of the process, the following points are summarized: 1. After patients arrive at the emergency department, the professional level of nurses varies, the standardization of triage is insufficient, and it takes 7 min to judge the time of stroke. 2. The procedure does not specify the details of indwelling venous access; the technical level of the pre‐examination nurses is uneven. There is no special person to care for the indwelling needle during the whole transfer process, which leads to the occurrence of venous access obstruction and requiring re‐catheterization. It takes 29 min from admission to establish venous access. 3. There is no full‐time nurse in the CT room. Patients must be transported from the CT room to the rescue room to start thrombolysis. The time from admission to intravenous thrombolysis is 43 min. 4. There was no full‐time nurse responsible for the coordination and management of the treatment of AIS patients, resulting in poor link‐up. When multiple stroke patients visited the hospital at the same time, there was a lack of backup nurses for stroke treatment.
3.4. Construction of integrated treatment process for acute ischaemic stroke coordinated by emergency nurses
3.4.1. Establishment of emergency stroke nurse team
From March–June 2016, with the leadership of the vice president of the hospital (director of the stroke centre), the management team of the stroke centre selected 33 nurses from the emergency department, interventional operating room, neurology and cerebrovascular surgery department of the hospital to form a group of emergency stroke nurses. According to the study of the expert meeting of the central management team, the admission conditions for emergency stroke nurses are as follows: college education or above, working in the above departments for more than 5 years, and obtaining the title of Nurse Practitioner or above; excellent standardized training and assessment, strong sense of responsibility, good at learning; good communication skills; active work and willing to serve the cause of stroke nursing.
3.4.2. Organize the theory and skill training assessment of emergency stroke nurses
The contents of theoretical training for emergency stroke nurses refer to the Guidelines for Diagnosis and Treatment of Acute Ischemic Stroke in China 2014 (Liu & Pu, 2015), Guidelines for Intravenous Thrombolysis in Acute Ischemic Stroke in China (Liu et al., 2016), and the knowledge points of the Accreditation Examination for Stroke Specialized Nurses of the American Academy of Neurological Nurses (https://abnncertification.org/scrn/about), including the theoretical knowledge of anatomy and physiology related to the emergency treatment chain of stroke, the judgement of stroke, special examination related to stroke, indications and contraindications of thrombolytic drug use, monitoring of complications and interpretation of the latest guidelines. The theoretical training period is 2 months, and 4 hr of theoretical teaching are arranged every week. The teachers are university part‐time teachers, professors and head nurses with intermediate titles or above who are engaged in stroke‐related specialties. Before and after the theoretical training, the assessment is carried out separately. Those who pass the theoretical examination begin skill training. The expert meeting of the management team of the stroke centre before skill training determines the operation process and scoring criteria of each skill, with emphasis on the judgement of stroke, the use of thrombolytic drugs and the cooperation of mechanical thrombectomy. Skills training lasts for 3 weeks. Each nurse must complete the whole process of tracking and rescuing more than 20 cases of AIS green channel in the emergency room, interventional operating room and ward for one week. Before and after the training, head nurses and teaching faculty in the ward, emergency room and interventional operating room were assessed according to the scoring criteria. All nurses cannot work until they have passed the theory and skills training.
3.4.3. Constructing the integrated treatment process of AIS for stroke emergency nurses
The flow chart of integrated treatment of acute ischaemic stroke coordinated by emergency stroke nurses is shown in Figure 2.
FIGURE 2.
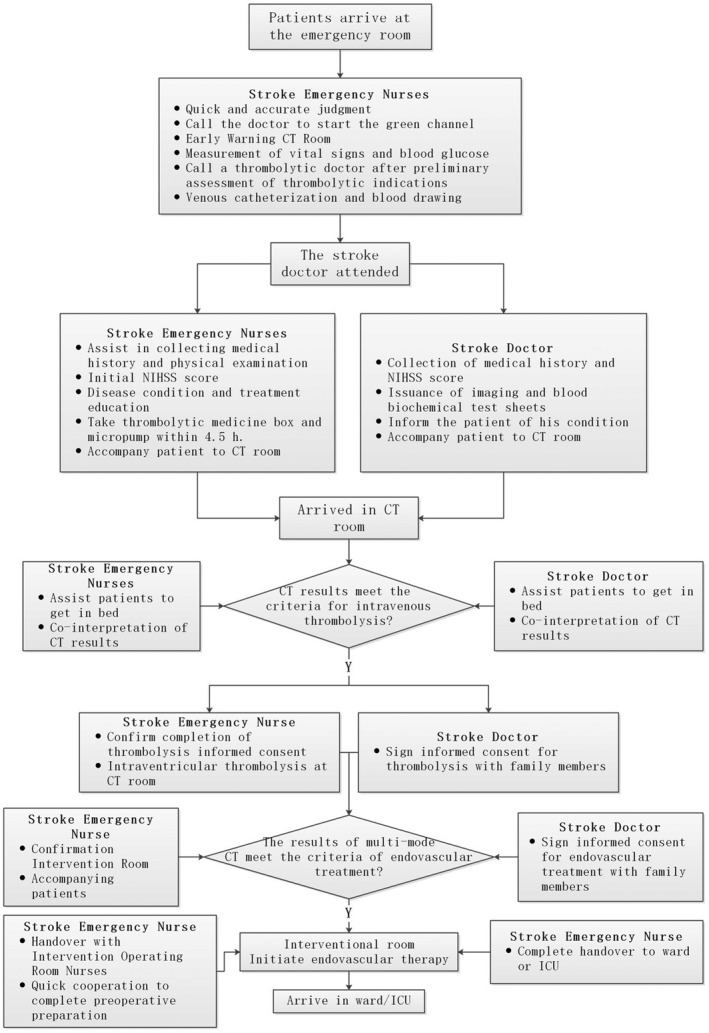
Flow chart of integrated treatment of acute ischaemic stroke coordinated by emergency stroke nurses
Define the workflow of emergency stroke nurses
The post of emergency stroke nurses is at the emergency pre‐examination triage. (1) When the patient arrives at the emergency department, the emergency stroke nurses call the stroke doctor to start the green channel after quick judgement, warn the CT room, measure vital signs and blood glucose, establish the venous channel and draw blood. (2) Assist stroke doctors to collect medical history and physical examination, carry thrombolytic box and micropump and accompany patients to CT room. (3) CT results confirmed the diagnosis of AIS and met the criteria for intravenous thrombolysis treatment. After confirming that the consent for intravenous thrombolysis was signed, intravenous thrombolysis was performed in the CT room. (4) The results of multimodal CT meet the criteria for endovascular treatment, confirm the operating room with the interventional operating room, accompany the patient to the interventional operating room; (5) cooperate with the nurses in the interventional operating room to quickly complete the preoperative preparation. (6) After completion of endovascular treatment, accompany the transfer and complete the transfer with the ward or ICU.
Reduce the nurse transfer link
From the previous rotation from emergency pre‐examination nurses to CT room nurses to emergency room nurses, to the full follow‐up of stroke emergency nurses throughout the treatment process.
Manage venous access throughout
Throughout the treatment process, stroke emergency nurses are responsible for a series of observation and treatment from indwelling venous channels, blood collection, thrombolysis to thrombolysis and infusion.
Location of use of thrombolytic drugs moved forward
Before the implementation of the procedure, patients were transferred to the emergency room and thrombolysis was started by the nurses in the emergency room. After implementation, it was improved to carry intravenous thrombolysis box and micropump for emergency stroke nurses, accompany the patients to the CT room with stroke doctors, move forward to the CT room for intravenous thrombolysis dispensing and bolus injection, continuously input thrombolysis drugs by micropump and transfer them to the rescue room to continue thrombolysis, which greatly shortened the DNT time.
Give backup rescue nurses
All emergency pre‐examination nurses participated in the stroke emergency nurses training and passed the examination. As a green channel for emergency treatment of stroke, the reserve nurses ensure the homogeneity of multiple patients' visits at the same time.
Quality supervision and management of integrated process
With the leadership of the vice president of the hospital stroke emergency nurses supervise and manage the quality of the integrated process. In the process of controllable and improved treatment of stroke patients in the whole DNT, it involves the cooperation of multiple disciplines and departments. Through the practice of the whole process of stroke emergency nurses, process details are found and submitted to the team to discuss its feasibility. Then the PDCA cycle can be implemented, so that the treatment process can be institutionalized and standardized, and the quality of operation can be improved.
3.5. Statistical analysis
SPSS18.0 was selected to complete the data information sorting and statistics. Because the measurement data did not conform to the characteristics of normal distribution, the median (P10, P90) was used to express, and the non‐reference test was chosen. The chi‐squared test was chosen in this study, and the difference was statistically significant when p < .01.
4. RESULTS
After the trial operation of the overall coordination system for emergency nurses during the day, the time spent in each link has been greatly reduced. In the full‐day operation group, the time spent was further shortened, especially the median time from admission to diagnosis was shortened from 6.67 min–0.15 min (p < .0001), that is, rapid diagnosis was achieved and time was saved for patient rescue. For the most important DNT, it is shortened from 43 min–20 min (p < .0001), which is more than double (Figure 3). According to the current medical research results, the gold treatment time of acute ischaemic stroke is 4.5 hr, which is commonly known as the "time window" of thrombolytic therapy. The pathological changes of brain tissue in this period after cerebral infarction are slight, without obvious ischaemic changes and necrosis. The ischaemic penumbra still exists and occupies the majority of the lesions. It is in the ischaemia‐reperfusion time window, which is the key period of treatment. Early reperfusion of cerebral blood flow can reduce the degree of ischaemia and limit the damage of nerve cells and their functions. The reduction of DNT time greatly improves the treatment effect and prognosis of patients.
FIGURE 3.
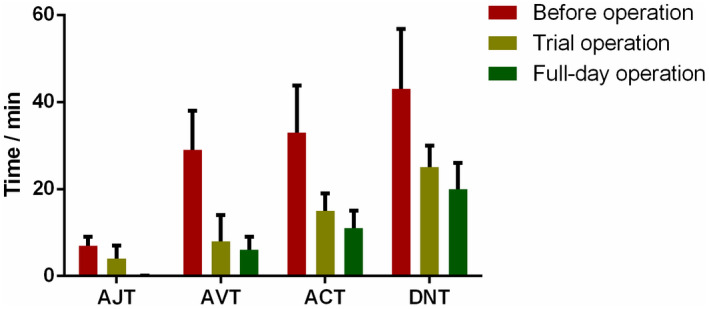
Treatment time of each link of AIS patients at different stages
5. DISCUSSION
AIS has the characteristics of high incidence, high disability rate, high mortality rate and high recurrence rate. Intravenous thrombolysis and mechanical thrombectomy after the onset of AIS are effective treatment methods, but the treatment effect has a clear correlation with time (Liu & Pu, 2015; X. Wang et al., 2015). The centre set up a team of emergency stroke nurses, whose members worked after unified training. Stroke nurses coordinate the green channel and reduce the rotation of nurses in multiple positions in emergency pre‐examination to CT room to emergency room. The venous thrombolysis site was moved forward to the CT room, which reduced the invalid transit time from the CT room to the rescue room. Stroke nurses also conduct quality supervision and management of the integrated process. The results showed that after the implementation of the integrated treatment process of AIS coordinated by stroke emergency nurses, the treatment time of each link in the hospital was shortened, DNT was statistically significantly shortened, and the treatment efficiency of stroke was statistically significantly improved.
In range from <35, 000–>27 million neurons will die every minute after AIS, and irreversible damage to the brain may occur if blood flow does not recover in time (Desai et al., 2019). Poisson (Poisson & Josephson, 2011) and other studies suggested that patients receiving intravenous rt‐PA in 90 min had better prognosis than patients receiving rt‐PA in 90–180 min. Therefore, shortening the treatment time as much as possible is the key to improve the treatment effect of AIS and improve the prognosis of patients (X. Wang et al., 2015). However, stroke treatment involves multi‐disciplinary cooperation of neurology, surgery, radiology and emergency. These departments have clear boundaries and interdisciplinary cooperation is extremely challenging. At the beginning of the establishment of the Cerebrovascular Disease Diagnosis and Treatment Center of our hospital, doctors of Neurology and surgery were organized together in the hospital, but each person's administrative relationship belongs to their own departments, so it is difficult to change the treatment habits starting from their own specialty. Since September 2013, the construction of stroke centre in our hospital has been regarded as a top leadership project. The deputy president of the hospital serves as the director of the stroke centre, integrates stroke‐related departments, and establishes a new in‐hospital stroke treatment model, which statistically significantly improves the early treatment efficiency of AIS patients (Chen et al., 2018). Under the leadership of the vice president, the central management team regularly supervises and organizes expert meetings to summarize and analyse the in‐hospital treatment process and continuously improve it. We innovatively allocated stroke emergency nurses to coordinate the integrated treatment process, and maintained the median DNT for 20 min, reaching the first domestic and international leading level.
6. CONCLUSION
The number of stroke patients in China is huge and increasing year by year. At the 2018 China Stroke Congress, the integrated treatment process of AIS coordinated by stroke emergency nurses was promoted to the whole country as one of the highlights of the "Changhai Model." As the stroke training base of the National Brain Defense Commission of China, more than 300 emergency stroke nurses have been trained. After the implementation of AIS integrated treatment process, the time of each link of AIS first aid has been statistically significantly shortened, which has won valuable time for rescuing patients. However, the current emergency stroke nurses are far from meeting the needs of stroke patients, so it is urgent to strengthen training efforts and make a good staff reserve.
6.1. Limitation
Due to the characteristic of the research design, it was not possible to establish control procedures for potential confounding variables to avoid potential bias in results. However, the study does make it possible to establish the possible relationship between the variables involved to conduct analytical studies.
6.2. Relevance to clinical practice
Since the pneumonia outbreak of new coronavirus infection occurred in Wuhan and other regions at the end of December, 2019, the epidemic wave and regions have been expanding, and the situation of prevention and control is very serious. The posts of emergency stroke nurses are under the double pressure of disease treatment and infection prevention at the emergency pre‐examination desk. In the follow‐up training, it is necessary to increase the emergency treatment ability and prevention and control skills of infectious diseases, so as to achieve good protection while completing the treatment of stroke patients.
CONFLICT OF INTEREST
The authors declared that they have no conflict of interest.
AUTHOR CONTRIBUTIONS
Dongmei Li performed the research; Hongjian Zhang analysed the data; Xiaoying Lu and Lingjuan Zhang designed the study; Jianmin Liu conceived of the study; all authors discussed the results and revised the manuscript.
ACKNOWLEDGEMENTS
None.
Li, D. , Zhang, H. , Lu, X. , Zhang, L. , & Liu, J. (2021). Practice of integrated treatment process for acute ischaemic stroke in hospital coordinated by emergency stroke nurses. Nursing Open, 9, 586–592. 10.1002/nop2.1101
Funding information
This study was supported by the Third Changhai Hospital Nursing Research Project of National Key Clinical Specialty Construction Program (2018HLZD06)
Dongmei Li and Hongjian Zhang have contributed equally to the manuscript.
[Correction added on 18 December 2021 after first online publication: details for co‐corresponding author Jianmin Liu and the contribution statement have been added in this version]
Contributor Information
Lingjuan Zhang, Email: lindazhang_cn@hotmail.com.
Jianmin Liu, Email: liu118@vip.163.com.
DATA AVAILABILITY STATEMENT
All data included in this study are available upon request by contact with the corresponding author.
REFERENCES
- Chen, M. , Liu, J. , Weng, Y. Y. , Yu, L. J. , Li, D. M. , & Zhang, L. J. (2018). Effect of intravenous thrombolysis process reengineering in acute ischemic stroke involving stroke emergency nurses. Nursing Journal of Chinese People's Liberation Army, 3, 57–61. [Google Scholar]
- Desai, S. M. , Rocha, M. , Jovin, T. G. , & Jadhav, A. P. (2019). High variability in neuronal loss. Stroke, 50(1), 34–37. 10.1161/STROKEAHA.118.023499 [DOI] [PubMed] [Google Scholar]
- Emberson, J. , Lees, K. R. , Lyden, P. , Blackwell, L. , Albers, G. , Bluhmki, E. , Brott, T. , Cohen, G. , Davis, S. , Donnan, G. , Grotta, J. , Howard, G. , Kaste, M. , Koga, M. , von Kummer, R. , Lansberg, M. , Lindley, R. I. , Murray, G. , Olivot, J. M. , … Hacke, W. (2014). Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: A meta‐analysis of individual patient data from randomised trials. The Lancet, 384(9958), 1929–1935. 10.1016/S0140-6736(14)60584-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, M. , Cui, L. Y. , He, M. L. , Xu, Y. , Zeng, J. S. , Liu, J. F. , & Chang, X. L. (2016). Guidelines for intravenous thrombolysis in acute ischemic stroke. [Google Scholar]
- Liu, M. , & Pu, C. Q. (2015). Chinese guidelines for the diagnosis and treatment of acute ischemic stroke 2014. Chinese Journal of Neurology, 48(4), 246–257. 10.3760/cma.j.issn.1006-7876.2015.04.002 [DOI] [Google Scholar]
- Lou, F. L. (2011). Thoughts on promoting the ability development of nursing managers. Chinese Nursing Management, 6, 76–78. [Google Scholar]
- Middleton, S. , Grimley, R. , & Alexandrov, A. W. (2015). Triage, treatment, and transfer: Evidence‐based clinical practice recommendations and models of nursing care for the first 72 hours of admission to hospital for acute stroke. Stroke, 46(2), e18–25. 10.1161/strokeaha.114.006139 [DOI] [PubMed] [Google Scholar]
- Poisson, S. N. , & Josephson, S. A. (2011). Quality measures in stroke. Neurohospitalist, 1(2), 71–77. 10.1177/1941875210392052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, L. D. , Liu, J. M. , Yang, Y. , Peng, B. , & Wang, Y. L. (2019). The Prevention and treatment of stroke still face huge challenges ——brief report on stroke prevention and treatment in China, 2018. Chinese Circulation Journal, 34(2), 105–119. 10.3969/j.issn.1000-3614.2019.02.001 [DOI] [Google Scholar]
- Wang, X. , Gao, S. Q. , Yu, L. J. , & Mao, Y. J. (2015). Effect of one‐stop care mode in improving the nursing quality of ischemic stroke. Nursing Journal of Chinese People's Liberation Army, 20, 57–59,63. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data included in this study are available upon request by contact with the corresponding author.


