Abstract
Objective
To characterise the extent to which health professionals perform SBAR (situation, background, assessment, recommendation) as intended (ie, with high fidelity) and the extent to which its use improves communication clarity or other quality measures.
Data sources
Medline, Healthstar, PsycINFO, Embase and CINAHL to October 2020 and handsearching selected journals.
Study selection and outcome measures
Eligible studies consisted of controlled trials and time series, including simple before-after design, assessing SBAR implementation fidelity or the effects of SBAR on communication clarity or other quality measures (eg, safety climate, patient outcomes).
Data extraction and synthesis
Two reviewers independently abstracted data according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses on study features, intervention details and study outcomes. We characterised the magnitude of improvement in outcomes as small (<20% relative increase), moderate (20%–40%) or large (>40%).
Results
Twenty-eight studies (3 randomised controlled trials, 6 controlled before-after studies, and 19 uncontrolled before-after studies) met inclusion criteria. Of the nine studies assessing fidelity of SBAR use, four occurred in classroom settings and three of these studies reported large improvements. The five studies assessing fidelity in clinical settings reported small to moderate effects. Among eight studies measuring communication clarity, only three reported large improvements and two of these occurred in classroom settings. Among the 17 studies reporting impacts on quality measures beyond communication, over half reported moderate to large improvements. These improvements tended to involve measures of teamwork and culture. Improvements in patient outcomes occurred only with intensive multifaceted interventions (eg, early warning scores and rapid response systems).
Conclusions
High fidelity uptake of SBAR and improvements in communication clarity occurred predominantly in classroom studies. Studies in clinical settings achieving impacts beyond communication typically involved broader, multifaceted interventions. Future efforts to improve communication using SBAR should first confirm high fidelity uptake in clinical settings rather than assuming this has occurred.
PROSPERO registration number
CRD42018111377.
Keywords: quality in health care, medical education & training, protocols & guidelines
Strengths and limitations of this study.
We undertook this systematic review in accordance with the Cochrane Collaboration standards using a validated tool to assess the quality of identified studies.
We considered SBAR (situation, background, assessment, recommendation) implementation strategies and its potential impact on fidelity to SBAR, clarity of communication and other quality-related measures.
The included studies were too heterogeneous to test for publication bias or to perform a meta-analysis.
Introduction
Analyses of adverse events and other critical incidents commonly identify communication failures between healthcare providers as major contributing factors.1–4 Standardised, structured communication techniques have emerged as a potential solution to these recurring problems.5 6 The mnemonic SBAR (situation, background, assessment, recommendation) constitutes the most well-known such technique.7 Borrowed from the US Navy where it was applied as a hierarchy-flattening approach to communicating situation reports, SBAR was initially adopted in healthcare to guide conversations between nurses and physicians about issues that required immediate attention.5 8 SBAR has since been widely promoted, by organisations such as the Institute for Healthcare Improvement9 and the National Health Service,10 to enhance communication.
A recent systematic review drew attention to the mixed impacts of SBAR on patient outcomes and patient safety and the lack of high-quality studies.11 This review usefully highlighted the discordance between the limited evidence supporting SBAR and the widespread recommendations to use it. Yet, the review only included studies reporting impacts on patient outcomes. While patient outcomes represent the bottom line for any improvement intervention, we do not want to dismiss potentially effective interventions just because they have not yet improved patient outcomes. We do not know, for instance, if the mixed results of SBAR on patient outcomes reflect problems with implementation (eg, SBAR as implemented may not reflect the intended approach to communication). Alternatively, even when implemented as intended, SBAR may not improve communication to an extent sufficient to improve patient outcomes.
In undertaking this systematic review, we sought to characterise gaps in the existing literature for SBAR as a strategy for improving communication and patient safety more generally. We sought to determine the extent to which users perform SBAR as intended (ie, with high fidelity) and the extent to which SBAR improves clarity of communication. We also looked for examples of interventions using SBAR showing impacts on other quality-related measures.
Methods
We registered the study protocol (CRD42018111377 Available from: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018111377) in November 2018 following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendation.12
Search strategy and study selection
Using the search strategy outlined in appendix A, we searched Medline, Healthstar, PsycINFO, Embase and CINAHL databases for studies evaluating SBAR (or variants of the standard mnemonic). The last search date was 23 October 2020.
We applied the following inclusion and exclusion criteria to all original research articles on SBAR.
Inclusion criteria were:
SBAR was taught or implemented as the framework to structure verbal communication between healthcare providers or trainees delivering care to any patient population. We allowed studies of SBAR as a standalone intervention as well as those which explicitly identified SBAR as a component of a multifaceted intervention.
Study design of a controlled trial (randomised or not) or time series, including simple before–after studies.
Study assessed one of the following eligible outcomes: fidelity to SBAR (eg, measures of adherence to the mnemonic during communication), clarity of communication, clinical outcomes, or measures of quality, such as teamwork and patient safety climate assessed by validated instruments.
For measures of fidelity and clarity of communication, we required assessment by two independent observers. We accepted outcomes ascertained by a single reviewer if the authors confirmed inter-rater agreement of at least moderate reliability (eg, kappa >0.4) on a subset of at least 10% of total observations. We applied this requirement given the subjective judgments underpinning these measures.
Exclusion criteria were:
Studies with no control group (eg, studies reporting only postintervention results for a single group and head-to-head trials of different versions of SBAR).
Outcomes obtained solely from incident reporting, given that incident reporting reflects reporting behaviour and safety culture far more than the actual frequency of any given adverse event.13
Studies from the grey literature or published solely as conference abstracts, as they offered too few details about SBAR training and implementation and also omitted key methodological details such as how communication clarity was judged.
Two reviewers (LL, LR) applied the above criteria in two stages: first independently screening abstracts of retrieved articles and then independently reviewing the full text of each potentially eligible article. Independent screenings of title and abstracts for inclusion achieved excellent inter-rater agreement (kappa = 0.81, 95% CI 0.77 to 0.86).14 Agreement about inclusion at the stage of full-text review also achieved substantial inter-rater agreement (kappa=0.76, 95% CI 0.67 to 0.86).
Quality assessment
Two investigators (LL, LR) independently assessed randomised controlled trials (RCTs) using the six domains from the revised Cochrane risk-of-bias tool for randomised trials15 and non-RCTs using the seven domains from the Cochrane Risk Of Bias In Non-Randomized Studies of Interventions tool.16 We resolved disagreements through consensus, involving a third investigator (KS) as needed, and excluded studies judged to have ‘critical risk’ of bias, as recommended by the Cochrane Collaboration.16 Online supplemental appendix B table 1 lists all studies excluded for critical risk of bias as well as a representative list of other excluded articles along with reasons for their exclusions.
bmjopen-2021-055247supp001.pdf (943.6KB, pdf)
Data extraction and synthesis
Two reviewers (LL, LR) independently abstracted data from included studies onto a piloted data collection form and resolved disagreements through arbitration by a third reviewer (KS). We extracted the first author, year of publication, country, participant profession, clinical setting, study design, type of communication for which SBAR was used, details around SBAR implementation and training, study outcomes and study limitations. For studies reporting impact beyond clarity of communication, we also documented the stated study purpose and any proposed mechanism by which SBAR would influence the selected quality measures. For missing or unclear data elements, we emailed corresponding authors for clarification, receiving 5 responses from 10 such queries.
As outlined in the registered protocol for the review, we planned to undertake quantitative synthesis of included studies if they did not exhibit substantial heterogeneity. Once we saw the wide variation in clinical settings, target populations, study designs, complexity of SBAR interventions and measures of impact in the included studies, we realised that the substantial heterogeneity would preclude quantitative synthesis using meta-analysis. We thus undertook a more qualitative approach to data synthesis. Yet, we still sought to characterise the impact of SBAR interventions more concretely, so defined categories conveying the magnitude of effect reported for each included outcome. We defined relative improvements <20% as ‘small’, relative improvements in the range of 20%–40% as ‘moderate’ in size, and improvements >40% as ‘large’. For implementation fidelity, we also noted whether the improvement achieved an absolute fidelity threshold of at least 80%. While no well-established threshold for fidelity exists, the potential effect size from any intervention decreases with lower levels of fidelity.17
Results
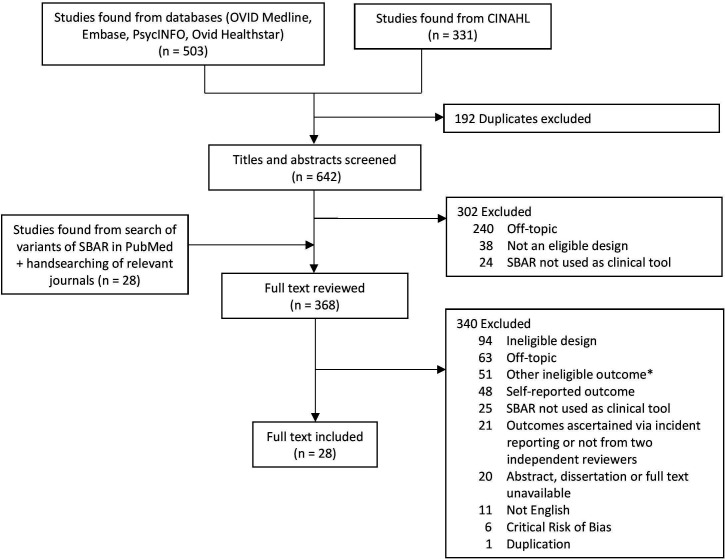
The database search retrieved 642 unique citations. After screening titles and abstracts, we reviewed 340 full-text articles, 34 of which met inclusion criteria. We excluded 6 articles judged to have critical risk of bias18–23 (see online supplemental appendix B table 1), leaving a total of 28 articles reporting 27 studies (figure 1). These included 3 RCTs,24–26 6 controlled before–after studies,27–32 and 19 uncontrolled before-and-after comparisons33–51 (table 1). Online supplemental appendix B table 2 presents an overview of the 28 articles, including details of the study purpose and intervention, and outcomes included in the review. For these 28 studies, 5 (18%) had low risk of bias; 1 scored as ‘some concerns’; 17 (60%) exhibited moderate risk; and, 5 (18%) had serious risk of bias (online supplemental appendix B figure 1A, B).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of included studies depicting steps of identification, screening, eligibility and inclusion. *Outcomes not of interest, in unreportable format, cannot be disetangle, or no reported outcomes at all. SBAR, situation, background, assessment, recommendation.
Table 1.
Characteristics of 28 included articles
| Characteristics | N (%) |
| Country | |
| USA | 9 (32) |
| Europe | 6 (21) |
| Australia | 5 (18) |
| Canada | 4 (14) |
| Other | 4 (14) |
| Study design | |
| Randomised controlled trial | 3 (11) |
| Controlled before-and-after | 6 (21) |
| Uncontrolled before-and-after | 19 (68) |
| Type of communication SBAR was applied to improve | |
| Handover between wards, handover at shift change and patient transfers | 16 (57) |
| Changes in patient status or obtaining immediate help with patients | 13 (46) |
| Other (general communication, multidisciplinary rounds) | 3 (11) |
| Disciplines involved in the communication | |
| Interdisciplinary | 15 (54) |
| Nurse to physician | 12 (80) |
| Other | 3 (20) |
| Intradisciplinary | 15 (54) |
| Nurse to nurse | 9 (60) |
| Physician to physician | 6 (40) |
| Type of outcomes reported | |
| Fidelity of SBAR use | 9 (32) |
| In classroom setting | 4 (44) |
| Clarity of communication | 8 (28) |
| In class room setting | 3 (38) |
| Impact beyond communication | 17 (61) |
bmjopen-2021-055247supp002.pdf (88.5KB, pdf)
bmjopen-2021-055247supp003.pdf (245.3KB, pdf)
Twenty-four studies evaluated the impact of SBAR and/or the fidelity of its implementation in the clinical setting24 28–43 45–51 and four in classroom settings.25–27 44 Most studies in the clinical setting (20/24; 83%) took place in hospitals, including medical and surgical wards27 35 40–42 49 52 and post-anaesthesia care units.28 29 33 As shown in table 1, 13 studies used SBAR to improve communications related to changes in patient status or obtaining immediate help with patients.24–27 32 38–40 42 44 46 50 51 Other applications included communication during multidisciplinary rounds, handovers between wards, shift change and patient transfers.28–30 33–37 41–43 45 47–49 Four targeted more than one type of communication.32 41 42 46
Most studies in clinical settings (17/24; 71%) focused on communication involving nurses, including nurse-to-physician,24 38–40 42 47 50 51 nurse-to-nurse27 33 34 41 42 46 48 49 and nurse-to-allied health communications.41 Two studies targeted physician-to-physician communication,35 45 though four studies in classroom settings aimed to improve communication between trainees and more senior physicians.25 26 30 44
Fidelity to SBAR technique
Nine studies25–27 35–37 44 45 47 assessed the degree to which participants used SBAR as intended, including four studies in classrooms and five in clinical settings (table 2). Investigators typically operationalised fidelity as a composite score based on adherence to predetermined elements of the SBAR mnemonic as assessed by two observers. Studies assessing fidelity varied in the time allotted for SBAR training, from as little as 10 min25 to a full-day session,37 but typically reported training sessions of 30–60 min. Most studies25 26 35–37 45 employed reminder aids, such as pocket cards or posters, to facilitate SBAR uptake. All studies in classroom settings25–27 44 and three of five in clinical settings35 45 47 assessed fidelity to SBAR immediately after training. For the remaining two in clinical settings, one36 assessed fidelity 2 months and another37 2 years after training. In the clinical setting, the data collection period ranged from 4 weeks to a year.
Table 2.
Studies evaluating fidelity of SBAR uptake
| Author, year | Main intervention | Fidelity measure | Time of fidelity assessment post training | Reported results | Magnitude of improvement (qualitative size) | Fidelity reached 80%? |
| Classroom-based studies | ||||||
| Cunningham et al 201225 | 10-min 1-on-1 didactic SBAR training for 69 junior physicians on medical/surgical wards and emergency departments for physician-physician telephone referral | Total item score of SBAR elements from 66 audio recordings | Immediately after training | SBAR exposure: 8.5 versus control: 8.0 on 12-point scale, p=0.051 | 6% (Small) | No (71%) |
| Marshall et al 200926 | 40-min ISBAR training (including role playing) for 17 teams of medical students for physician–physician telephone referral | Total item score of ISBAR elements from 17 video and audio recordings | Immediately after training | SBAR exposure: 17.4 versus control: 10.2 on 20-point scale, p=0.001 | 71% (Large) | Yes (87%) |
| McCrory et al 201244 | 45-min didactic ABC-SBAR training for 26 paediatric interns for physician–physician communication for immediate help for patient | Total item score of ABC-SBAR elements and format from 52 video recordings | Immediately after training | 3.1 to 7.8 on 10-point scale, p<0.001 | 152% (Large) | No (78%) |
| Uhm et al 201927 | 4-hour SBAR training (including role-playing) embedded in 1-week practicum for 81 nursing students for nurse–physician communication for help for patient | Total item score of SBAR elements from 81 audio recordings | Immediately after training | SBAR exposure: 17.6 versus control: 9.0 on 24-point scale, p<0.001 | 96% (Large) | No (74%) |
| Studies in clinical setting | ||||||
| Shahid et al 202047 | Implementation of a modified SBAR tool and didactic training with videos for 10 nurses over 1 month for nurse–physician communication during interfacility neonatal transports | Total item score of SBAR elements from 165 audio recordings | Assessment began immediately after training but was ongoing over 1 year period | 21.7 to 30.2 on 38-point scale, p≤0.001 | 39% (Moderate) | Yes (80%) |
| Smith et al 201835 | SBAR-DR implementation, electronic handover template, and 30 min didactic training with videos and demonstrations for 68 physicians in emergency department for physician–physician telephone communication at admission handover | Total item score of SBAR-DR elements and format from 220 audio recordings | Assessment began immediately after training but was ongoing over 60-day period | 7.6 to 8.4 on 16-point scale, p=0.009 | 12% (Small) | No (53%) |
| Thompson et al 201145 | ISBAR implementation and 1-hour training held at 4 separate times for 44 junior med officers over 4 weeks for physician–physician at after-hour handover on in-patient ward | Total item score of ISBAR elements from 63 audio recordings | Assessment began immediately after training but was ongoing over 4 week period | 9.2 to 10.4 on a 19-point scale, p=0.004 | 13% (Small) | No (55%) |
| Uhm et al 201836 | SBAR implementation and didactic training (duration not reported) for 102 nurses for nurse–nurse handover from paediatric cardiac ICU to cardiac ward | Total item score of SBAR elements from 59 audio recordings | Assessment began 2 months after training but was ongoing over 40-day period | 2.3 to 2.9 on 4-point scale, p<0.001 | 25% (Moderate) | No (73%) |
| Wilson et al 201737 | SBAR implementation and full day training (including role playing) over 1 month for nurses-physician-respiratory therapist communication during interfacility neonatal and paediatric transports | Total item score of SBAR elements from 187 audio recordings | Assessment began 2 years after training but was ongoing over 7 month period | 7.0 to 8.3 on 10-point scale, p<0.001 | 19% (Small) | Yes (83%) |
ABC-SBAR, airway, breathing, circulation followed by SBAR; ICU, Intensive Care Unit; ISBAR, Identification of self followed by standard SBAR; SBAR, situation, background, assessment, recommendation; SBAR-DR, Situation, Background, Assessment, Responsibilities & Risk, Discussion & Disposition, Read-back & Record.
Three of the four studies of SBAR implementation in classroom settings demonstrated large improvements in fidelity to SBAR,26 27 44 whereas all five studies in clinical settings reported small to moderate improvements in fidelity (table 2). Only three studies26 37 47 achieved fidelity of at least 80%. One of these studies reported a baseline of 78% fidelity37 so the post-intervention fidelity of 83% constituted a marginal improvement. Only two studies reported large relative improvements in fidelity and also achieved an absolute fidelity of at least 80%.26 37 These studies both used role-playing in addition to didactic methods for their SBAR training. Two other studies using role-playing fell short of 80% fidelity but both did report large effect sizes.27 44
Clarity of communication
Eight studies25–27 29 35 37 47 51 evaluated the clarity of communication using SBAR (table 3). Half of these studies used implicit assessments25 35 37 47 or global ratings of communication. The others judged clarity of communication using explicit criteria, such as conveying specific elements of information26 27 37 or recall of information by receivers of communication.29 51
Table 3.
Effect of SBAR on clarity of communication
| Author, year | Study design | SBAR training | Objective of communication | Measure of quality of communication | Reported results | Relative improvement (qualitative size) |
| Classroom-based studies | ||||||
| Cunningham et al 201225 | RCT | 10-min didactic session explaining the SBAR method of clinical handover and its application in telephone referrals immediately prior to test scenario | Contacting senior member of staff via telephone (medical or surgical registrar) to refer a medical patient with chest pain or surgical patient with abdominal pain | Implicit assessment: ability ‘to get the message across’ as measured by 4-point scale for poor, fair, good or excellent as judged by a senior clinician reviewing 66 audio recordings, with a second clinician independently reviewing 30% | SBAR exposure: 3.0 versus control: 2.0 on 4-point scale, p=0.003 | 50% (Large) |
| Marshall et al 200926 | RCT | 40-min ISBAR training (including role-playing) for 17 teams of medical students learning how to communicate in telephone referrals to more senior physicians | Contacting senior colleague via telephone for assistance with management of an unstable trauma patient in high fidelity simulation centre | Explicit assessment: clarity and delivery of communication as measured by rating referral according to the presence of elements of quality (eg, coherence, conciseness, etc) as judged by senior clinician reviewing 17 video and audio recordings (a second clinician reviewed first half to ensure adequate agreement) | SBAR exposure group had higher score on 5-point scale for clarity as measured by Spearmen rank correlation (r=0.903), p=0.001 | N/A (large based on r statistic >0.5) |
| Uhm et al 201927 | Controlled before–after | 4-hour SBAR training (including role-playing) embedded in 1-week practicum for nursing students for various nurse-physician communications | Notifying physician about patient’s status of bronchiolitis with desaturation or acute gastroenteritis with severe dehydration | Explicit assessment: clarity of communication according to presence of elements of quality (eg, coherence, conciseness, etc) as judged by two investigators independently reviewing 81 audio recordings | SBAR exposure: 29.9 versus control: 22.4 on 40-point scale, p<0.001 | 33% (Moderate) |
| Studies in clinical setting | ||||||
| Randmaa et al 201629 | Controlled before–after | SBAR Implementation and 2.5-hour training (including role-playing) for nurses and physicians for nurse–nurse communication at rounds or shift change and nurse–physician communication at rounds or handover | Nurse–nurse communication at rounds or shift change and nurse–physician communication at rounds or handover | Explicit assessment: percentage of recalled information sequences by receivers as measured by counting identified sequences from 164 audio recordings and observations | SBAR exposure: 43.4% to 52.6% - (↑ 9.2%) Control: 51.3% to 52.6% - (↑ 1.3%) Not significant (p value not reported) |
18% (Small) |
| Shahid et al 202047 | Uncontrolled before–after | Implementation of a modified SBAR tool and didactic training with videos for 10 nurses for nurse–physician communication during interfacility neonatal transports | Neonatal transport cases | Implicit assessment: global rating score as measured by rating the quality of the handover using 165 audio recordings | 3.0 to 3.9 on 5-point scale, p<0.001 | 30% (Moderate) |
| Smith et al 201835 | Uncontrolled before–after | SBAR-DR implementation and 30-min didactic training with videos and demonstrations for 68 physicians in emergency department for physician–physician telephone communication at admission handover | Physician–physician telephone communication at admission handover | Implicit assessment: global rating score as measured by rating on an anchored scale using 220 audio recordings | 2.9 to 3.1 on 5-point scale, p=0.236 | 5% (Small) |
| Vlitos and Kamara 201651 | Uncontrolled before–after | Implementation of a modified SBAR tool and training (including role-play) for nurses for nurse–physician communication between ward staff and physicians on duty | Contacting physician on duty via telephone for triaging cases | Explicit assessment: percentage of physicians given adequate information to safely triage cases measured using 103 audited calls | 58% to 84%, p value not reported | 45% (Large) |
| Wilson et al 201737 | Uncontrolled before–after | SBAR implementation with reminder tools and full-day training (including role-playing) for nurses-physician-respiratory therapist communication during interfacility neonatal and paediatric transports | Paediatric transport cases | Explicit assessment: integration of content as measured by scoring on tool for related items using 187 audio recordings | 7.3 to 8.4 on 10-point scale, p<0.001 | 16% (Small) |
| Implicit assessment: global rating score as measured by rating the handover using 187 audio recordings | 3.4 to 3.9 on 5-point scale, p<0.001 | 15% (Small) | ||||
ISBAR, identification of self followed by SBAR; RCT, randomised controlled trial; SBAR, situation, background, assessment, recommendation; SBAR-DR, Situation, Background, Assessment, Responsibilities & Risk, Discussion & Disposition, Read-back & Record.
Studies assessing clarity of communication varied in the time allotted for SBAR training, from as little as 10 min25 to a full-day session,37 with most reporting role-playing as part of the training.26 27 29 37 51 Most studies employed reminder aids, such as pocket cards or posters, to facilitate SBAR uptake25 26 29 35 37 47 51 -one also had the SBAR template clinically embedded in the workflow.35
Six studies assessed both clarity of communication and fidelity to SBAR.25–27 35 37 47 The studies in the classroom setting25–27 demonstrated moderate to large improvements in clarity of communication, with the level of fidelity reached ranging from 71% to 87%. In contrast, studies in clinical settings35 37 47 demonstrated no improvement to moderate improvements in clarity, with fidelity ranging from 53% to 83%.
Impacts beyond communication
Seventeen studies24 28 30–34 38–43 46 48–50 reported the impact of SBAR on quality measures beyond clarity of communication (see online supplemental appendix B table 3). Unfortunately, none of these studies also assessed communication clarity or fidelity.
Ten studies reported on patient outcomes,24 30 38–43 48 50 including mortality,39 40 42 unplanned ICU admissions,40 42 cardiac arrests,40 43 adverse events,24 30 hospital readmission,41 urinary catheter removal41 and patient satisfaction,41 48 among others. Of these 10 studies, 7 reported moderate or large improvements for at least one outcome.39–43 48 50 In five of these studies, SBAR constituted just one facet of broader, intensive initiatives that included a structured process to assess patient status, such as an early warning system protocol39 40 42 43 or readmission risk assessment and daily interdisciplinary rounds41 that may in itself have greater power to influence such patient outcomes.
Two studies reported on changes in provider behaviours, including small relative improvements in duplicated, cancelled and wrong patient order entries,30 and a large relative improvement (8.3% to 16.7%, p<0.001) in the recognition of adverse events by nurses in postanaesthesia care units.33 Two studies measured organisational efficiency, reporting large relative improvements (though without testing for significance) in some measures of bed assignment and patient turnover.34 49
Five studies reported on teamwork,38 46 safety climate28 38 46 and patient safety culture.31 32 Two studies28 38 reported a small significant improvement in safety climate and moderate significant improvement in teamwork. Two studies found small to moderate significant improvements in patient safety culture dimensions of organisational learning, feedback and communication about error, and teamwork across hospital units.31 32
Discussion
Overall, we found that teaching SBAR technique to healthcare providers can promote high fidelity uptake. Importantly, however, studies of SBAR implementation reporting large improvements in fidelity26 27 44 all occurred in classroom settings. Conversely, the five studies assessing SBAR fidelity in clinical settings reported small to moderate improvements. Only two studies,26 37 both in the classroom setting, reported large relative improvements in fidelity and also achieved an absolute fidelity of at least 80%, a minimum fidelity suggested for intervention impact.53
Additionally, we found that teaching the SBAR technique to healthcare providers can improve clarity of communication, in both classroom and clinical settings. Most of the studies in the classroom setting demonstrated large improvements in clarity, whereas four of the five studies in the clinical setting reported only small to moderate improvements.29 35 37 47 These findings suggest greater challenges of improving clarity of communication in the clinical setting compared with the classroom, potentially related to increased distractions and competing priorities inherent in clinical practice. The better results from classroom-based studies may also indicate a recency effect. Classroom studies assessed outcomes immediately after training. Studies in clinical settings necessarily measured outcomes, including fidelity of uptake and clarity of communication, over weeks to months. It is also possible that a greater Hawthorne effect occurred in classroom-based evaluations compared with studies in clinical settings.
Six of the included studies measured both fidelity to SBAR and clarity of communication, and their results again highlighted the difference between studies in classrooms versus clinical settings. Classroom-based studies achieved levels of fidelity ranging from 71% to 87% and reported moderate to large improvements in clarity of communication. Again, this difference may reflect the immediacy of the fidelity assessments following training in the classroom-based studies and/or a greater Hawthorne effect. The studies in clinical settings35 37 47 demonstrated no improvement to moderate improvements in clarity, with fidelity ranging from 53% to 83%.
The lesser improvements in communication clarity seen in studies from clinical settings suggest the need for establishing higher levels of fidelity to SBAR as intended. Proceeding directly to implementation without confirming fidelity, or exposing clinicians to SBAR solely in classroom settings, seems unlikely to produce the intended improvements in communication. None of the SBAR interventions included in this review incorporated audits or other monitoring of SBAR use, potentially limiting impact of SBAR on both communication and quality of care.54
The challenges of achieving clinically impactful improvements in clarity of communication may, in part, explain our findings and others’11 that there are mixed impacts of SBAR on outcomes beyond communication. SBAR education and implementation positively enhanced safety culture and teamwork,28 31 32 38 while the relationship with other clinical outcomes was less straightforward. Studies that embedded SBAR as a component of a larger initiative, such as an early warning system protocol39 40 42 43 or readmission risk assessment and daily interdisciplinary rounds,41 demonstrated larger impacts on patient outcomes, compared with those that implemented SBAR on its own. Unfortunately, none of the studies aimed at outcomes beyond communication24 28 30–34 38–43 46 48 49 assessed SBAR fidelity or clarity of communication. Thus, we cannot know if the multifaceted interventions achieved their impacts because they implemented SBAR successfully or because of the other components of these interventions, such as early warning scores and rapid response systems.
Limitations
A limitation of this study is the variable quality of research in this domain. One frequently cited study18 lacked basic information about the basis for choosing the outcomes reported and how relevant data were obtained. Even after excluding that study and five others with critical risk of bias, 60% of included studies exhibited moderate risk of bias and 18% had high risk. Another limitation of the study is the heterogeneity in the types of communication activities targeted, compounded by variation in in the interventions—from SBAR on its own to SBAR as just one part of an intensive multifaceted initiative. A final limitation is the likelihood of publication bias, such that additional studies reporting poor fidelity or no improvements in communication clarity may have gone unpublished.
Conclusion
Our study adds to the growing consensus that the impact of SBAR is variable. We provide a more nuanced analysis of reasons for these findings by showing that uptake of SBAR with high fidelity cannot be taken for granted. Fidelity appears reasonably easy to achieve in classroom settings. But, studies in clinical contexts either did not achieve sufficient improvements in fidelity or they simply skipped assessing it. Organisations have promoted the use of SBAR for a range of communication and nurses are often told to use it in all clinical communications. If organisations want to achieve the intended impact of SBAR, they need to attend to its implementation and ongoing monitoring. As with any improvement intervention, one cannot assume that uptake will occur smoothly or as intended.
Footnotes
Contributors: LL: provided the conception and design of the study, supplied the acquisition of data, provided analysis and interpretation of data, drafted the article, revised it critically for important intellectual content, and gave final approval of the version to be submitted; LR: provided analysis and interpretation of data, drafted the article, revised it critically for important intellectual content, and gave final approval of the version to be submitted; KS: provided analysis and interpretation of data, revised it critically for important intellectual content, and gave final approval of the version to be submitted. LL is the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants.
References
- 1.Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med 2004;79:186–94. 10.1097/00001888-200402000-00019 [DOI] [PubMed] [Google Scholar]
- 2.Neale G, Woloshynowych M, Vincent C. Exploring the causes of adverse events in NHS hospital practice. J R Soc Med 2001;94:322–30. 10.1177/014107680109400702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilson RM, Harrison BT, Gibberd RW, et al. An analysis of the causes of adverse events from the quality in Australian health care study. Med J Aust 1999;170:411–5. 10.5694/j.1326-5377.1999.tb127814.x [DOI] [PubMed] [Google Scholar]
- 4.Clapper TC, Ching K. Debunking the myth that the majority of medical errors are attributed to communication. Med Educ 2020;54:74–81. 10.1111/medu.13821 [DOI] [PubMed] [Google Scholar]
- 5.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care 2004;13:i85–90. 10.1136/qhc.13.suppl_1.i85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dayton E, Henriksen K. Communication failure: basic components, contributing factors, and the call for structure. Jt Comm J Qual Patient Saf 2007;33:34–47. 10.1016/s1553-7250(07)33005-5 [DOI] [PubMed] [Google Scholar]
- 7.Riesenberg LA, Leitzsch J, Little BW. Systematic review of handoff mnemonics literature. Am J Med Qual 2009;24:196–204. 10.1177/1062860609332512 [DOI] [PubMed] [Google Scholar]
- 8.Thomas CM, Bertram E, Johnson D. The SBAR communication technique: teaching nursing students professional communication skills. Nurse Educ 2009;34:176–80. 10.1097/NNE.0b013e3181aaba54 [DOI] [PubMed] [Google Scholar]
- 9.Institute for Healthcare Improvement . SBAR tool: situation-background-assessment-recommendation. Available: http://www.ihi.org/resources/Pages/Tools/SBARToolkit.aspx [Accessed 13 May 2020].
- 10.National Health Service . SBAR communication tool- situation, background, assessment, recommendation. Available: https://webarchive.nationalarchives.gov.uk/20180501161349/https://improvement.nhs.uk/resources/sbar-communication-tool/ [Accessed 13 May 2020].
- 11.Müller M, Jürgens J, Redaèlli M, et al. Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open 2018;8:e022202. 10.1136/bmjopen-2018-022202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shojania KG. Incident reporting systems: what will it take to make them less frustrating and achieve anything useful? Jt Comm J Qual Patient Saf 2021;47:755–8. 10.1016/j.jcjq.2021.10.001 [DOI] [PubMed] [Google Scholar]
- 14.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74. 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- 15.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 16.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Etchells E, Woodcock T. Value of small sample sizes in rapid-cycle quality improvement projects 2: assessing fidelity of implementation for improvement interventions. BMJ Qual Saf 2018;27:61–5. 10.1136/bmjqs-2017-006963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haig KM, Sutton S, Whittington J. SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Patient Saf 2006;32:167–75. 10.1016/s1553-7250(06)32022-3 [DOI] [PubMed] [Google Scholar]
- 19.Christie P, Robinson H. Using a communication framework at handover to boost patient outcomes. Nurs Times 2009;105:13–15. [PubMed] [Google Scholar]
- 20.Hamilton P, Gemeinhardt G, Mancuso P. SBAR and nurse-physician communication: pilot testing an educational intervention. Nurs Adm Q 2006;30:295–9. [Google Scholar]
- 21.Freitag M, Carroll VS. Handoff communication: using failure modes and effects analysis to improve the transition in care process. Qual Manag Health Care 2011;20:103–9. 10.1097/QMH.0b013e3182136f58 [DOI] [PubMed] [Google Scholar]
- 22.Martin HA, Ciurzynski SM. Situation, background, assessment, and Recommendation-Guided Huddles improve communication and teamwork in the emergency department. J Emerg Nurs 2015;41:484–8. 10.1016/j.jen.2015.05.017 [DOI] [PubMed] [Google Scholar]
- 23.Campbell D, Dontje K. Implementing bedside handoff in the emergency department: a practice improvement project. J Emerg Nurs 2019;45:149–54. 10.1016/j.jen.2018.09.007 [DOI] [PubMed] [Google Scholar]
- 24.Field TS, Tjia J, Mazor KM, et al. Randomized trial of a warfarin communication protocol for nursing homes: an SBAR-based approach. Am J Med 2011;124:179.e1–179.e7. 10.1016/j.amjmed.2010.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cunningham NJ, Weiland TJ, van Dijk J, et al. Telephone referrals by junior doctors: a randomised controlled trial assessing the impact of SBAR in a simulated setting. Postgrad Med J 2012;88:619–26. 10.1136/postgradmedj-2011-130719 [DOI] [PubMed] [Google Scholar]
- 26.Marshall S, Harrison J, Flanagan B. The teaching of a structured tool improves the clarity and content of interprofessional clinical communication. Qual Saf Health Care 2009;18:137–40. 10.1136/qshc.2007.025247 [DOI] [PubMed] [Google Scholar]
- 27.Uhm J-Y, Ko Y, Kim S. Implementation of an SBAR communication program based on experiential learning theory in a pediatric nursing practicum: a quasi-experimental study. Nurse Educ Today 2019;80:78–84. 10.1016/j.nedt.2019.05.034 [DOI] [PubMed] [Google Scholar]
- 28.Randmaa M, Mårtensson G, Leo Swenne C, et al. SBAR improves communication and safety climate and decreases incident reports due to communication errors in an anaesthetic clinic: a prospective intervention study. BMJ Open 2014;4:e004268. 10.1136/bmjopen-2013-004268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Randmaa M, Swenne CL, Mårtensson G, et al. Implementing situation-background-assessment-recommendation in an anaesthetic clinic and subsequent information retention among receivers: a prospective interventional study of postoperative handovers. Eur J Anaesthesiol 2016;33:172–8. 10.1097/EJA.0000000000000335 [DOI] [PubMed] [Google Scholar]
- 30.Telem DA, Buch KE, Ellis S, et al. Integration of a formalized handoff system into the surgical curriculum: resident perspectives and early results. Arch Surg 2011;146:89–93. 10.1001/archsurg.2010.294 [DOI] [PubMed] [Google Scholar]
- 31.Andreoli A, Fancott C, Velji K, et al. Using SBAR to communicate falls risk and management in inter-professional rehabilitation teams. Healthc Q 2010;13:94–101. [PubMed] [Google Scholar]
- 32.Velji K, Baker GR, Fancott C, et al. Effectiveness of an adapted SBAR communication tool for a rehabilitation setting. Healthc Q 2008;11:72–9. 10.12927/hcq.2008.19653 [DOI] [PubMed] [Google Scholar]
- 33.Street M, Phillips NM, Haesler E, et al. Refining nursing assessment and management with a new postanaesthetic care discharge tool to minimize surgical patient risk. J Adv Nurs 2018;74:2566–76. 10.1111/jan.13779 [DOI] [PubMed] [Google Scholar]
- 34.Potts L, Ryan C, Diegel-Vacek L, et al. Improving patient flow from the emergency department utilizing a standardized electronic nursing handoff process. J Nurs Adm 2018;48:432–6. 10.1097/NNA.0000000000000645 [DOI] [PubMed] [Google Scholar]
- 35.Smith CJ, Buzalko RJ, Anderson N, et al. Evaluation of a novel handoff communication strategy for patients admitted from the emergency department. West J Emerg Med 2018;19:372. 10.5811/westjem.2017.9.35121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Uhm J-Y, Lim EY, Hyeong J. The impact of a standardized inter-department handover on nurses' perceptions and performance in Republic of Korea. J Nurs Manag 2018;26:933–44. 10.1111/jonm.12608 [DOI] [PubMed] [Google Scholar]
- 37.Wilson D, Kochar A, Whyte-Lewis A, et al. Evaluation of situation, background, assessment, recommendation tool during neonatal and pediatric interfacility transport. Air Med J 2017;36:182–7. 10.1016/j.amj.2017.02.013 [DOI] [PubMed] [Google Scholar]
- 38.Ting W-H, Peng F-S, Lin H-H, et al. The impact of situation-background-assessment-recommendation (SBAR) on safety attitudes in the obstetrics department. Taiwan J Obstet Gynecol 2017;56:171–4. 10.1016/j.tjog.2016.06.021 [DOI] [PubMed] [Google Scholar]
- 39.Mullany DV, Ziegenfuss M, Goleby MA, et al. Improved hospital mortality with a low MET dose: the importance of a modified early warning score and communication tool. Anaesth Intensive Care 2016;44:734–41. 10.1177/0310057X1604400616 [DOI] [PubMed] [Google Scholar]
- 40.Ludikhuize J, Brunsveld-Reinders AH, Dijkgraaf MGW, et al. Outcomes associated with the nationwide introduction of rapid response systems in the Netherlands. Crit Care Med 2015;43:2544–51. 10.1097/CCM.0000000000001272 [DOI] [PubMed] [Google Scholar]
- 41.Townsend-Gervis M, Cornell P, Vardaman JM. Interdisciplinary rounds and structured communication reduce re-admissions and improve some patient outcomes. West J Nurs Res 2014;36:917–28. 10.1177/0193945914527521 [DOI] [PubMed] [Google Scholar]
- 42.De Meester K, Verspuy M, Monsieurs KG, et al. SBAR improves nurse-physician communication and reduces unexpected death: a pre and post intervention study. Resuscitation 2013;84:1192–6. 10.1016/j.resuscitation.2013.03.016 [DOI] [PubMed] [Google Scholar]
- 43.Beckett DJ, Inglis M, Oswald S, et al. Reducing cardiac arrests in the acute admissions unit: a quality improvement journey. BMJ Qual Saf 2013;22:1025–31. 10.1136/bmjqs-2012-001404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McCrory MC, Aboumatar H, Custer JW, et al. “ABC-SBAR” training improves simulated critical patient hand-off by pediatric interns. Pediatr Emerg Care 2012;28:538–43. 10.1097/PEC.0b013e3182587f6e [DOI] [PubMed] [Google Scholar]
- 45.Thompson JE, Collett LW, Langbart MJ, et al. Using the ISBAR handover tool in junior medical officer handover: a study in an Australian tertiary hospital. Postgrad Med J 2011;87:340–4. 10.1136/pgmj.2010.105569 [DOI] [PubMed] [Google Scholar]
- 46.Beckett CD, Kipnis G. Collaborative communication: integrating SBAR to improve quality/patient safety outcomes. J Healthc Qual 2009;31:19–28. 10.1111/j.1945-1474.2009.00043.x [DOI] [PubMed] [Google Scholar]
- 47.Shahid S, Thabane L, Marrin M, et al. Evaluation of a modified SBAR report to physician tool to standardize communication on neonatal transport. Am J Perinatol 2020:1. 10.1055/s-0040-1715524 [DOI] [PubMed] [Google Scholar]
- 48.Abbaszade A, Assarroudi A, Armat MR. Evaluation of the impact of handoff based on the SBAR technique on quality of nursing care. J Nursing Care Qual 2020. [DOI] [PubMed] [Google Scholar]
- 49.Sermersheim ER, Moon MC, Streelman M, et al. Improving patient throughput with an electronic nursing handoff process in an academic medical center: a rapid improvement event approach. J Nurs Adm 2020;50:174–81. 10.1097/NNA.0000000000000862 [DOI] [PubMed] [Google Scholar]
- 50.Leonard C, Zomorodi M. Bringing the R back to SBAR: a focused heart failure SBAR tool. Home Health Care Manag Pract 2019;31:179–85. 10.1177/1084822319841572 [DOI] [Google Scholar]
- 51.Vlitos K, Kamara S. Improving communication of important information using the SBARD tool. Ment Health Pract 2016;20:34–8. 10.7748/mhp.2016.e1062 [DOI] [Google Scholar]
- 52.Poots AJ, Reed JE, Woodcock T, et al. How to attribute causality in quality improvement: lessons from epidemiology. BMJ Qual Saf 2017;26:933–7. 10.1136/bmjqs-2017-006756 [DOI] [PubMed] [Google Scholar]
- 53.Lorencatto F, Gould NJ, McIntyre SA, et al. A multidimensional approach to assessing intervention fidelity in a process evaluation of audit and feedback interventions to reduce unnecessary blood transfusions: a study protocol. Implement Sci 2016;11:163. 10.1186/s13012-016-0528-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Polaha J, Smith JD, Sunderji N. A recipe for assessing fidelity in family and health systems. Fam Syst Health 2019;37:101–6. 10.1037/fsh0000421 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-055247supp001.pdf (943.6KB, pdf)
bmjopen-2021-055247supp002.pdf (88.5KB, pdf)
bmjopen-2021-055247supp003.pdf (245.3KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.