Abstract
Aortic injury represents a rare but potentially fatal complication of invasive coronary angiography. The authors present a series of four patients with aortic injury after invasive coronary angiography and intervention (mean age, 71 years; three women). In three patients, CT showed subintimal staining from undiluted contrast media (CM) in the aortic root with no communication to the aortic lumen. Short-term follow-up CT showed resolution of CM staining in all patients. Classic aortic dissection occurred in one patient, with undiluted CM from invasive angiography in the false lumen in the aortic root. Preliminary evidence suggests that iatrogenic injury from invasive coronary angiography resulting in subintimal CM staining of the aortic wall at CT, without evidence of communication with the lumen of the aortic root, shows favorable short-term outcome.
Keywords: CT Angiography, Percutaneous, Fluoroscopy
Supplemental material is available for this article.
© RSNA, 2021
Keywords: CT Angiography, Percutaneous, Fluoroscopy
Summary
Early CT shows in the majority of patients with iatrogenic injury isolated subintimal contrast media staining in the aortic wall without imaging evidence of communication with the lumen of the aortic root. This finding is associated with excellent short-term prognosis.
Key Points
■ Accumulation of undiluted contrast media (CM) in the wall of the aortic root can be found at CT performed early after complicated invasive coronary angiography and intervention.
■ Preliminary experience in our small patient series suggests that subintimal CM staining of the aortic wall, without imaging evidence of communication with the lumen of the aortic root, shows favorable short-term outcome.
Introduction
The number of invasive coronary angiography (ICA) procedures and percutaneous coronary interventions (PCIs) is constantly increasing, with an estimated 1.02 million catheterizations performed annually in the United States (1). Parallel to the increase in the number of interventions, there is escalating case complexity (2). While ICA and PCI are considered safe, there is a small risk of major complications occurring in around 0.082% of procedures (1). Of those, iatrogenic aortic dissection can be seen in 0.02%–0.07% (3) and coronary perforations in 0.19%–1.46% of procedures (4). Coronary injury occurs more often (4.8%) during interventions of chronic total occlusion (CTO) (5) and during PCI of the right coronary artery (RCA) (3,6–8) and often extends to the aortic root (9).
The suspicion of iatrogenic coronary and/or aortic injury first occurs during ICA, which shows extravasation of contrast media (CM). However, the true extent of injury is often underestimated (10), necessitating second-line imaging including CT, which combines speed, noninvasiveness, and high accuracy for disease classification (11,12), hereby guiding further management. Dunning et al (3) classified iatrogenic aortic injury from ICA into three groups: local involvement of the ipsilateral aortic cusp, representing type I; less than 40-mm extension along the ascending aorta, representing type II; and greater than 40-mm extension along the ascending aorta, representing type III. Patients with injury types I and II were proposed to be managed conservatively, while the more extensive type III should undergo surgery (3).
In this case series, we report on early and follow-up CT imaging findings in four patients with iatrogenic aortic root injury from ICA and PCI.
Case Presentations
Case 1
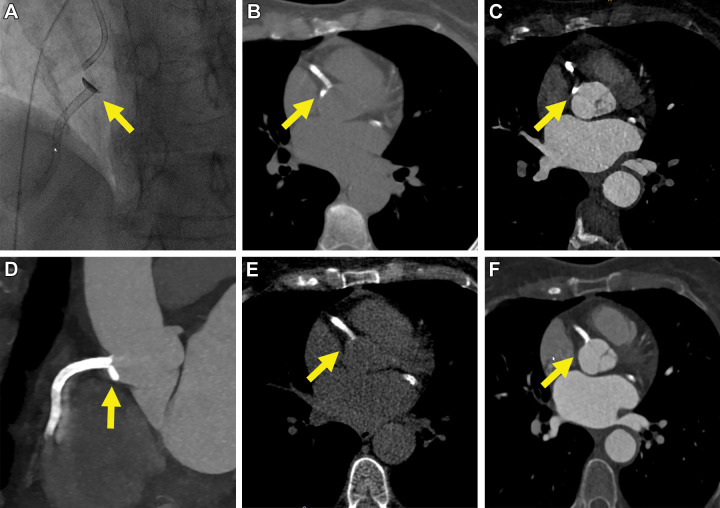
A 68-year-old female patient with known three-vessel coronary artery disease had atypical chest pain and elevated high-sensitivity cardiac troponin levels after pelvic surgery. The patient underwent ICA with the aim of circumflex artery recanalization (Table E1 [supplement]). After the first CM injection in the aortic root, extravasation was noticed. No emergency intervention was performed. Emergency transthoracic echocardiography (TTE) showed no pericardial hematoma. CT performed 30 minutes after ICA demonstrated a crescent-shaped hyperattenuation reflecting undiluted CM from ICA in the aortic wall extending 40 mm above the aortic annulus, representing Dunning type III (Fig 1). There was no perfusion or contrast enhancement of the aortic wall from intravenously administered CM. Follow-up CT after 21 hours showed complete resolution of the CM accumulation. The patient was managed conservatively and recovered completely.
Figure 1:
![Serial chest CT images in a 68-year-old female patient (patient 1). (A) Axial chest CT image at the level of the aortic root. The nongated chest CT examination was performed to rule out pulmonary embolism before the actual hospitalization. The arrow indicates a normal aortic wall. Two weeks later, the patient underwent invasive coronary angiography for recanalization of the circumflex artery. After the first contrast media injection in the aortic root, extravasation of contrast media into the aortic wall was noticed (image not shown). CT performed 30 minutes after invasive coronary angiography demonstrated a crescent-shaped hyperattenuation, reflecting undiluted contrast media in the aortic wall (Dunning type III; arrow on B, an electrocardiographically [ECG]–gated nonenhanced chest CT image and C, an ECG-gated contrast-enhanced chest CT image). Follow-up CT the following day showed complete resolution of the contrast media accumulation (arrow in D).](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/2692/8686001/0155a744b515/ryct.2021210241.fig1.jpg)
Serial chest CT images in a 68-year-old female patient (patient 1). (A) Axial chest CT image at the level of the aortic root. The nongated chest CT examination was performed to rule out pulmonary embolism before the actual hospitalization. The arrow indicates a normal aortic wall. Two weeks later, the patient underwent invasive coronary angiography for recanalization of the circumflex artery. After the first contrast media injection in the aortic root, extravasation of contrast media into the aortic wall was noticed (image not shown). CT performed 30 minutes after invasive coronary angiography demonstrated a crescent-shaped hyperattenuation, reflecting undiluted contrast media in the aortic wall (Dunning type III; arrow on B, an electrocardiographically [ECG]–gated nonenhanced chest CT image and C, an ECG-gated contrast-enhanced chest CT image). Follow-up CT the following day showed complete resolution of the contrast media accumulation (arrow in D).
Case 2
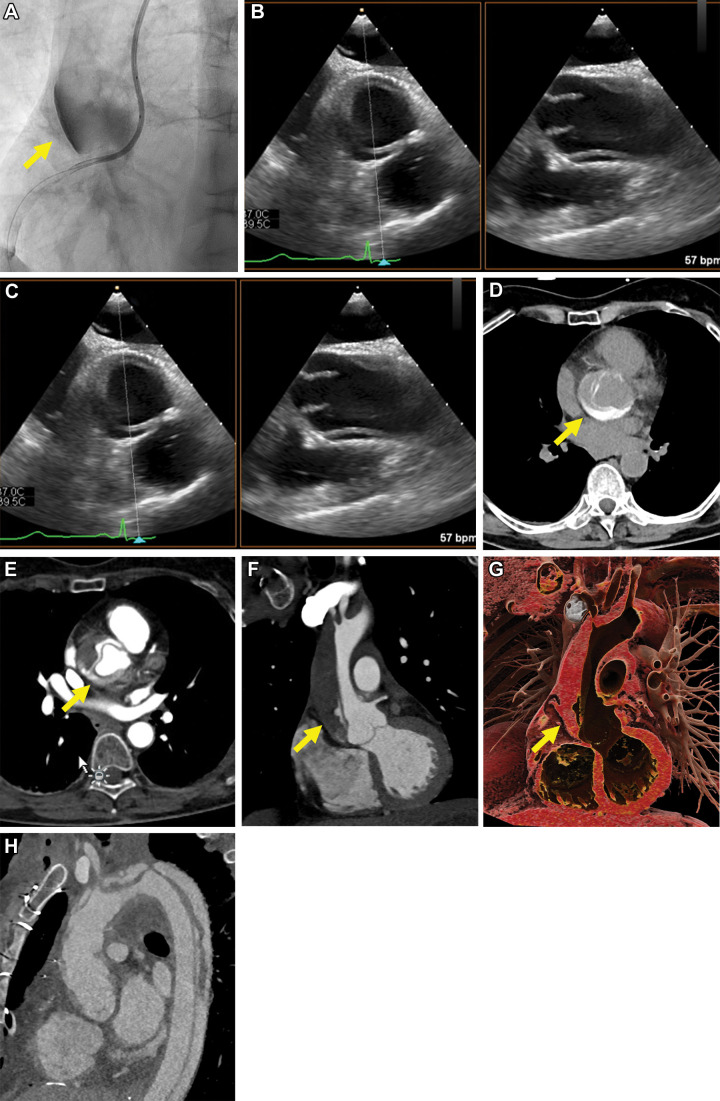
A 72-year-old male patient with typical angina, known three-vessel coronary artery disease, and previous coronary artery bypass graft surgery to the left anterior descending and circumflex arteries underwent PCI for recanalization of a CTO of the RCA (Table E1 [supplement]). After placement of an ostial stent, extravasation of CM near the ostium of the proximal RCA occurred. A covered stent was immediately implanted. Emergency TTE showed no pericardial hematoma. CT performed 1.5 hours after PCI showed a hematoma including undiluted CM from the intervention adjacent to the proximal RCA extending to the ascending aorta, the latter showing lower attenuation, to around 40 mm above the level of the aortic annulus (Dunning III). There was extension of the hematoma in the wall of the pulmonary trunk and pulmonary arteries, eventually reaching the lobar pulmonary arteries of both lungs. There was no perfusion or contrast enhancement of the aortic wall from intravenous CM. Perihilar, perivascular ground-glass opacities compatible with alveolar hemorrhage in this patient, who presented with hemoptysis, was found in all pulmonary lobes, corresponding to extension of the hematoma to the alveoli (Fig 2). Follow-up CT after 2 days showed marked reduction of intramural hematoma of the aortic root, complete resolution of intramural hematoma of the pulmonary trunk and pulmonary and lobar pulmonary arteries, and reduction of mediastinal hematoma and alveolar hemorrhage. The patient was managed conservatively and recovered completely.
Figure 2:
Images in a 72-year-old male patient (patient 2) undergoing coronary intervention for recanalization of a chronic total occlusion of the right coronary artery. (A) Coronary angiogram shows extravasation of contrast media recognized during the procedure (yellow arrow). The perforation was treated with immediate implantation of a covered stent. CT performed 1.5 hours after percutaneous coronary intervention showed a focal hyperattenuated layering of contrast media adjacent to the proximal right coronary artery, with additional intramural hematoma extending to the ascending aorta (Dunning III; yellow arrows on B, C, axial non–contrast-enhanced and D, contrast-enhanced CT images) and to the pulmonary arteries to the level of the lobar arteries of both lungs (yellow arrows on C, non–contrast-enhanced and D, contrast-enhanced CT images). Perivascular ground-glass opacities compatible with alveolar hemorrhage in this patient with hemoptysis were found in all pulmonary lobes, corresponding to extension of the hematoma to the alveoli (category III, according to Sueyoshi et al [13]; yellow arrows in E). Follow-up CT after 2 days revealed marked reduction of intramural hematoma of the aortic root and complete resolution of the intramural hematoma in the pulmonary trunk (yellow arrows) and lobar pulmonary arteries, along with F, a reduction of mediastinal hematoma and alveolar hemorrhage.
Case 3
A 72-year-old woman with known two-vessel coronary artery disease and previous non–ST-elevation myocardial infarction treated with PCI of the RCA and circumflex artery had intermittent atypical angina. Stress perfusion MRI revealed inducible ischemia in the RCA territory (Table E1 [supplement]). ICA revealed subtotal in-stent restenosis of the RCA. During intervention, extravasation of CM at the RCA ostium occurred, which was immediately treated with placement of a stent overlapping the proximal stent and extending it to the coronary ostium. Emergency TTE showed no abnormality. Thirty minutes after PCI, CT demonstrated a small, crescent-shaped hyperattenuation of the aortic wall adjacent to the RCA ostium (Dunning I) (Fig 3). There was no perfusion or contrast enhancement of the aortic wall from intravenous CM. Follow-up CT after 24 hours showed complete resolution of the findings.
Figure 3:
Images in a 72-year-old female patient (patient 3) undergoing intervention for recanalization of a subtotal (99%) in-stent restenosis of the right coronary artery (RCA). There was focal extravasation of contrast media at the RCA ostium (yellow arrow in A). The extravasation was immediately treated with stent extension to the RCA ostium. Thirty minutes after the intervention, CT demonstrated a small, focal, crescent-shaped hyperattenuation of the aortic wall adjacent to the RCA ostium, compatible with subintimal contrast media staining (Dunning I; yellow arrow on B, axial and C, contrast-enhanced CT images and D, multiplanar reformation of contrast-enhanced CT images). Follow-up CT after 24 hours showed complete resolution of the undiluted contrast media accumulation (yellow arrow on E, axial non–contrast-enhanced and F, contrast-enhanced CT images).
Case 4
A 70-year-old female patient with chest pain and non–ST-elevation myocardial infarction underwent PCI for recanalization of an acute-on-chronic occlusion of the RCA (Table E1 [supplement]). Following balloon predilation of the proximal to mid RCA, extravasation of CM into the wall of the aortic root occurred. No further intervention was performed. Emergency TEE showed acute dissection of the ascending aorta. CT performed 30 minutes after PCI helped confirm Stanford type A acute aortic dissection extending to the origin of an arteria lusoria, including hyperattenuated CM from invasive angiography in the aortic root (Dunning III), along with mild mediastinal hematoma (Fig 4). The patient underwent emergency replacement of the ascending aorta and aortic arch. Follow-up CT 12 hours after PCI showed progression of the dissection to the level of the left common iliac artery. Eight days after PCI, CT showed unchanged findings. The patient is currently stable and undergoes regular outpatient clinical and imaging follow-up.
Figure 4:
Images in a 70-year-old female patient (patient 4) undergoing recanalization of an acute-on-chronic occlusion of the right coronary artery (RCA). Following balloon predilation of the proximal to mid RCA, extravasation of contrast media in the wall of the ascending aorta occurred (yellow arrow in A). (B, C) Emergency transthoracic echocardiography showed dissection of the ascending aorta. CT performed 30 minutes after percutaneous coronary intervention helped confirm a Stanford type A acute aortic dissection, extending to the origin of an arteria lusoria (Dunning III), with partial layering of hyperattenuated contrast media from the intervention in the aortic root (yellow arrow in D–G). (H) Follow-up CT performed 12 hours after the intervention and after emergency replacement of the ascending aorta and aortic arch showed progression of the dissection to the descending aorta.
Discussion
This case series illustrates early and follow-up CT imaging findings in four patients with iatrogenic aortic root injury from ICA and PCI. In three patients, findings from early CT performed less than 2 hours after the intervention showed a crescent-shaped CM staining from ICA in the wall of the aortic root. Follow-up CT in these three patients showed complete resolution of the subintimal CM staining, with residual intramural hematoma remaining in one. Classic aortic dissection occurred in one patient, including undiluted CM from ICA in the false lumen in the aortic root. This patient underwent subsequent repair of the ascending aorta.
Iatrogenic injury to the aortic root from ICA is rare (1). Most aortic root injuries in our series occurred during intervention of the RCA, which is compatible with the literature (14). While one patient developed a classic Stanford type A aortic dissection, in the majority, early CT, performed less than 2 hours after the intervention, showed a crescent-shaped staining from undiluted CM in the wall of the aortic root. This CT imaging finding has been previously reported only rarely (12, 14–16). García Iglesias et al (15) showed a case with subintimal staining with undiluted CM in the right coronary sinus after PCI (the time interval between intervention and CT was not provided), showing a complete resolution after 4 days. Song (16) showed a case with crescentic aortic wall thickening with undiluted CM after ICA (time interval not provided), which showed complete resolution at CT performed after more than 2 months. Tanasie et al (14) showed two cases with CT performed less than 1 hour after ICA and PCI, both showing highly attenuated, undiluted CM in the aortic wall. In one patient, regression was demonstrated in findings at CT performed 48 hours later, while one patient died within hours after failed RCA stenting due to massive right ventricular infarction, without available follow-up imaging (14). In their review, Goerne et al (12) showed images in two patients with highly attenuating CM from ICA in the ascending aorta, with the hyperattenuated CM accumulation extending to the descending aorta in one patient.
In our series, two of the three patients with subintimal CM staining (one with Dunning type III and one with Dunning type I) showed complete resolution of abnormalities at short-term follow-up CT, while one patient (with Dunning type III) showed resolution of CM staining with residual intramural hematoma in the aortic root. On the basis of our preliminary experience in a limited number of patients, it appears that subintimal CM staining alone—without imaging evidence of direct communication between the aortic lumen and wall—seems to resolve, even in the case of intramural hematoma of the pulmonary arteries, and even if extending beyond 4 cm above the level of the aortic annulus. This is in line with the literature reporting good outcome for patients sustaining iatrogenic aortic injury from invasive coronary interventions, with adequacy of medical management in most cases (7,11,14,17–19).
We hypothesize that in patients with subintimal CM staining, at some point there had to be a communication, even if very small, through which the CM entered the aortic wall. If small enough and in a normal aorta, this does not lead to a large tear or dissection and seals off once the catheter or wire is retracted. In the patient with dissection, underlying media degeneration must have been present, and in this situation, the tear triggered a classic dissection.
In line with the literature, we consider CT the imaging modality of choice when aortic root injury is suspected. The protocol should be performed with electrocardiographic gating including a nonenhanced and a contrast-enhanced arterial phase.
In conclusion, in most patients with iatrogenic injury, early CT shows isolated subintimal CM staining in the aortic wall without imaging evidence of communication with the lumen of the aortic root. This finding is associated with excellent short-term prognosis.
Footnotes
Authors declared no funding for this work.
Disclosures of conflicts of interest: L.A.C. No relevant relationships. M.E. No relevant relationships. C.T. No relevant relationships. P.R.V. No relevant relationships. R.M. No relevant relationships. H.A. No relevant relationships.
References
- 1. Virani SS , Alonso A , Benjamin EJ , et al . Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association . Circulation 2020. ; 141 ( 9 ): e139 – e596 . [DOI] [PubMed] [Google Scholar]
- 2. Doll JA , Hira RS , Kearney KE , et al . Management of Percutaneous Coronary Intervention Complications: Algorithms From the 2018 and 2019 Seattle Percutaneous Coronary Intervention Complications Conference . Circ Cardiovasc Interv 2020. ; 13 ( 6 ): e008962 . [DOI] [PubMed] [Google Scholar]
- 3. Dunning DW , Kahn JK , Hawkins ET , O’Neill WW . Iatrogenic coronary artery dissections extending into and involving the aortic root . Catheter Cardiovasc Interv 2000. ; 51 ( 4 ): 387 – 393 . [DOI] [PubMed] [Google Scholar]
- 4. Shaukat A , Tajti P , Sandoval Y , et al . Incidence, predictors, management and outcomes of coronary perforations . Catheter Cardiovasc Interv 2019. ; 93 ( 1 ): 48 – 56 . [DOI] [PubMed] [Google Scholar]
- 5. Sapontis J , Salisbury AC , Yeh RW , et al . Early Procedural and Health Status Outcomes After Chronic Total Occlusion Angioplasty: A Report From the OPEN-CTO Registry (Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion Hybrid Procedures) . JACC Cardiovasc Interv 2017. ; 10 ( 15 ): 1523 – 1534 . [DOI] [PubMed] [Google Scholar]
- 6. López-Mínguez JR , Climent V , Yen-Ho S , González-Fernández R , Nogales-Asensio JM , Sánchez-Quintana D . Structural features of the sinus of valsalva and the proximal portion of the coronary arteries: their relevance to retrograde aortocoronary dissection [in Spanish] . Rev Esp Cardiol 2006. ; 59 ( 7 ): 696 – 702 . [PubMed] [Google Scholar]
- 7. Núñez-Gil IJ , Bautista D , Cerrato E , et al . Incidence, Management, and Immediate- and Long-Term Outcomes After Iatrogenic Aortic Dissection During Diagnostic or Interventional Coronary Procedures . Circulation 2015. ; 131 ( 24 ): 2114 – 2119 . [DOI] [PubMed] [Google Scholar]
- 8. Gómez-Moreno S , Sabaté M , Jiménez-Quevedo P , et al . Iatrogenic dissection of the ascending aorta following heart catheterisation: incidence, management and outcome . EuroIntervention 2006. ; 2 ( 2 ): 197 – 202 . [PubMed] [Google Scholar]
- 9. Maehara A , Mintz GS , Bui AB , et al . Incidence, morphology, angiographic findings, and outcomes of intramural hematomas after percutaneous coronary interventions: an intravascular ultrasound study . Circulation 2002. ; 105 ( 17 ): 2037 – 2042 . [DOI] [PubMed] [Google Scholar]
- 10. Cereda AF , Toselli M , Khokhar A , et al . Iatrogenic aorta-coronary dissection: Case report and systematic review . Catheter Cardiovasc Interv 2021. ; 97 ( 7 ): E900 – E910 . [DOI] [PubMed] [Google Scholar]
- 11. Garg P , Buckley O , Rybicki FJ , Resnic FS . Resolution of iatrogenic aortic dissection illustrated by computed tomography . Circ Cardiovasc Interv 2009. ; 2 ( 3 ): 261 – 263 . [DOI] [PubMed] [Google Scholar]
- 12. Goerne H , de la Fuente D , Cabrera M , et al . Imaging Features of Complications after Coronary Interventions and Surgical Procedures . RadioGraphics 2021. ; 41 ( 3 ): 699 – 719 . [DOI] [PubMed] [Google Scholar]
- 13. Sueyoshi E , Matsuoka Y , Sakamoto I , Uetani M . CT and clinical features of hemorrhage extending along the pulmonary artery due to ruptured aortic dissection . Eur Radiol 2009. ; 19 ( 5 ): 1166 – 1174 . [DOI] [PubMed] [Google Scholar]
- 14. Tanasie C , Chandonnet M , Chin A , et al . Catheter-induced aortic dissection after invasive coronary angiography: evaluation with MDCT . AJR Am J Roentgenol 2011. ; 197 ( 6 ): 1335 – 1340 . [DOI] [PubMed] [Google Scholar]
- 15. García Iglesias D , Martín Fernández M , López Iglesias F , Calvo Blanco J , Morís de la Tassa C . Iatrogenic Aortic Dissection: One or More Entities? Ann Thorac Surg 2016. ; 101 ( 1 ): 414 – 415 . [DOI] [PubMed] [Google Scholar]
- 16. Song JK . Update in acute aortic syndrome: intramural hematoma and incomplete dissection as new disease entities . J Cardiol 2014. ; 64 ( 3 ): 153 – 161 . [DOI] [PubMed] [Google Scholar]
- 17. Baumann S , Behnes M , Sartorius B , et al . Follow-up of iatrogenic aorto-coronary “Dunning” dissections by cardiac computed tomography imaging . BMC Med Imaging 2017. ; 17 ( 1 ): 64 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Boukhris M , Tomasello SD , Marzà F , Azzarelli S , Galassi AR . Iatrogenic aortic dissection complicating percutaneous coronary intervention for chronic total occlusion . Can J Cardiol 2015. ; 31 ( 3 ): 320 – 327 . [DOI] [PubMed] [Google Scholar]
- 19. Muhyieddeen K , Samim A , Roberts M , Srikanth S . A Case of Iatrogenic Aortic Intramural Hematoma . Methodist DeBakey Cardiovasc J 2017. ; 13 ( 1 ): 37 – 38 . [DOI] [PMC free article] [PubMed] [Google Scholar]



![Images in a 72-year-old male patient (patient 2) undergoing coronary intervention for recanalization of a chronic total occlusion of the right coronary artery. (A) Coronary angiogram shows extravasation of contrast media recognized during the procedure (yellow arrow). The perforation was treated with immediate implantation of a covered stent. CT performed 1.5 hours after percutaneous coronary intervention showed a focal hyperattenuated layering of contrast media adjacent to the proximal right coronary artery, with additional intramural hematoma extending to the ascending aorta (Dunning III; yellow arrows on B, C, axial non–contrast-enhanced and D, contrast-enhanced CT images) and to the pulmonary arteries to the level of the lobar arteries of both lungs (yellow arrows on C, non–contrast-enhanced and D, contrast-enhanced CT images). Perivascular ground-glass opacities compatible with alveolar hemorrhage in this patient with hemoptysis were found in all pulmonary lobes, corresponding to extension of the hematoma to the alveoli (category III, according to Sueyoshi et al [13]; yellow arrows in E). Follow-up CT after 2 days revealed marked reduction of intramural hematoma of the aortic root and complete resolution of the intramural hematoma in the pulmonary trunk (yellow arrows) and lobar pulmonary arteries, along with F, a reduction of mediastinal hematoma and alveolar hemorrhage.](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/2692/8686001/75b12417258a/ryct.2021210241.fig2.jpg)