Abstract
Purpose
To characterize chest radiograph and CT imaging appearance in patients with breakthrough COVID-19 (defined as an illness occurring in patients that previously received a COVID-19 vaccination) in a hospital setting.
Materials and Methods
In this retrospective study, all patients admitted to the hospital between August 26 and September 8, 2021 with a positive SARS-CoV-2 reverse transcription polymerase chain reaction-confirmed infection who were fully vaccinated against COVID-19 were evaluated. Clinical, laboratory data, and outcomes were collected and assessed. All patients had chest imaging performed (either radiography, CT, or a combination of both). Chest radiographs and CTs were assessed and scored on admission and on follow up to determine the extent and type of pulmonary involvement. Descriptive statistics were used.
Results
Charts of 60 hospitalized patients that tested positive for SARS-CoV-2 were reviewed for a prior history of COVID-19 vaccination. Eight (13.3%) such patients were identified and included for analysis (mean age, 54 years; range 34–81 years; four women). Patients received either two doses of Pfizer-BioNTech (n = 6), two doses of Moderna (n = 1), or one dose of Johnson and Johnson (n = 1). Five (63%) patients were immunosuppressed at the time of presentation, and six (75%) reported respiratory symptoms. Most of the patients had normal radiographs (4 of 7; 57%). The most common chest CT findings were ground glass opacities (three of five), with mild to moderate severity scores (average, 51; range 8–88). Two patients required intensive care unit admission. However, no patients died and all were either discharged or were on room air without residual respiratory symptoms by the end of the study period.
Conclusion
In hospitalized patients with COVID-19 breakthrough illness, normal to mild or moderately positive imaging findings were observed.
©RSNA, 2021
Summary
The majority of patients with breakthrough COVID-19 illness in this study had absent or mild imaging findings and a benign clinical course.
Key Points
In this retrospective study of eight hospitalized patients with breakthrough COVID-19 infection, five of eight (63%) patients were immunosuppressed and four of five (80%) of these patients had imaging abnormalities.
Six of the of eight (75%) patients had been discharged as of the cut-off date of the study, including one who required intensive care unit admission.
Introduction
Since the onset of the pandemic, the severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) virus, the cause of COVID-19, is responsible for 651,753 deaths in the United States and 4,592,304 worldwide as of September 8, 2021 (1). In response, more than 173 million Americans have been fully vaccinated as of August 31, 2021, according to the CDC (2). Despite the demonstrated effectiveness of the COVID-19 directed vaccines, notably messenger RNA vaccines, a proportion of fully vaccinated individuals still develop COVID-19 illness. These infections are being reported as “breakthrough” cases. It is well recognized that no vaccine is 100% effective and thus breakthrough illness in some individuals is expected. Patients who develop such COVID-19 breakthrough illness may be asymptomatic or symptomatic requiring outpatient or inpatient treatment, rarely leading to death. As the protective effects of the vaccine wane and new variants arise, the number of breakthrough cases will likely increase. While the clinical aspects of COVID-19 breakthrough have been described, there has been minimal attention devoted to its imaging manifestations. In this study, we report the chest imaging findings in a series of individuals with breakthrough COVID-19 who required hospitalization.
Materials and Methods
Patient Inclusion
This retrospective study was performed at a single urban academic center. The study received an exemption from the institutional review board. The requirement for informed consent was waived. All patients who were admitted to the hospital with a positive COVID-19 polymerase chain reaction (PCR) test between August 26-September 8, 2021, were included. Patients with a prior history of known COVID-19 infection and those with no history of COVID-19 vaccination were excluded. A review of the electronic medical charts was performed periodically after initial review. Relevant clinical information including demographics and prior medical history, biochemical laboratories, and imaging was recorded in a secure Health Insurance Portability and Accountability Act compliant database. A patient was considered to be fully vaccinated if the date of presentation was two weeks or more following the second dose of vaccine (Pfizer-BioNTech and Moderna), or the first dose of vaccine for the Johnson and Johnson vaccine.
Image Acquisition
All chest CT data were acquired using a Philips Brilliance iCT (256-slice) or Brilliance 64 (Philips Healthcare, Cambridge, MA), or Siemens Force (Siemens Medical Solutions USA, Malvern, PA). Image resolution ranged from 1 to 4 mm in the axial reconstructed view and from 0.45 to 0.75 mm slice thickness. CT scans were not gated for ECG.
Image Review
Two board-certified, thoracic radiologists (five (RH) and 30 (CW) years of experience) reviewed each study. All studies were reviewed using a consensus read technique.
Chest Radiographic Evaluation
The readers rated pulmonary parenchymal involvement using a semiquantitative severity score described by Monaco et al (3). Each lung was subdivided into three zones: upper zone (from the lung apex to the aortic arch profile), middle zone (from the aortic arch profile to the lower margin of the left pulmonary hilum), and lower zone (from the lower margin of the left pulmonary hilum to the diaphragm). For each zone, a score on a scale from 0 to 3 in 1-point increments based on increased severity was assigned: 0, normal lung parenchyma; 1, interstitial involvement only; 2, presence of radiopacity for less than 50% of the visible lung parenchyma; 3, presence of radiopacity for 50% or more than 50% of the visible lung parenchyma. The chest radiograph performed at the time of admission was scored, and if a subsequent image was obtained it was graded as stable, decreased, or increased in comparison to the initial study.
Chest CT Evaluation
Reviewers assessed the presence of nodules, ground glass opacities, consolidation, septal thickening, pleural effusion, reverse halo, traction bronchiectasis, and reticulations. Imaging findings were graded based on the study by Francone et al (4). This CT severity score index was used to assess the lung changes and involvement by COVID-19 based on an approximate estimation of pulmonary parenchymal involvement. Each of the five lung lobes was visually scored as follows from 1 to 5: 1, representing less than 5% lobar involvement; 2, 5–25% lobar involvement, 3, 26–50% lobar involvement; 4, 51–75% lobar involvement; and 5, greater than 75% lobar involvement.
The final score was calculated as the sum of individual lobar scores, out of a possible 25 (total score); the total lung involvement was then calculated by multiplying the total score by 4. If a patient had a follow-up CT, comparison was made to initial CT and graded as stable, increased, or decreased involvement. Imaging features of chronic or interstitial lung disease (such as traction bronchiectasis, volume loss, subpleural reticulation, honeycombing) were also noted.
Patient Demographics and Clinical Characteristics
The sex, age, date of vaccine, vaccination type, COVID-19 symptoms, comorbidities, immune status, and laboratory tests from each patient were reviewed. Clinical outcomes, such as intensive care unit (ICU) admission and discharge or death, were retrospectively retrieved.
Statistical Analysis
Descriptive statistics were used for this study.
Results
Patient Overview and Characteristics
Over the enrollment period, 60 patients were admitted to the hospital with a positive COVID-19 PCR test. Eight (13.3%) met the inclusion criteria of having a positive COVID-19 PCR test while being fully vaccinated. Specifically, all patients had a positive nasal COVID-19 PCR test. Patient #1 had two negative PCR tests around the time of admission, prior to the first positive test. Patient demographics, clinical information (including comorbidities), and radiograph findings are summarized in Table 1.
Table 1.
Patient Demographics, Clinical Information, and Chest Radiograph Findings
Of the eight patients, the average age was 54 years (range 34–81); four were women. The average body mass index was 24.4 kg/m2 (range 16.9–30.5). Patients were fully vaccinated with two doses of either the Pfizer-BioNTech vaccine (75%; n = 6), Moderna (12.5%; n = 1), or a single dose of Johnson and Johnson (12.5%; n = 1). One patient had a known COVID-19 contact. Respiratory COVID-19-related symptoms were reported in six (75%) of the patients. One patient was transferred from an outside hospital with a positive COVID-19 test. Five (63%) patients were immunosuppressed at the time of presentation.
Chest Radiograph Imaging Findings
Seven of the patients had a chest radiograph acquired around the time of the COVID-19 test (mean 2 days). The single patient who did not have a chest radiograph performed at the time of admission (patient #8) had a chest CT performed on the same day.
Four (57.1%) of the seven patients had a normal chest radiographs. Three (42.9%) of the seven-chest radiographs showed a combination of consolidation and hazy opacities with an average severity score of 9 out of 18. Four of these patients had a follow-up chest radiography performed, three (75%) demonstrating stable to decreased opacities, and one (25%) patient demonstrating increased opacities.
Chest CT Imaging Findings
Chest CT imaging findings are summarized in Table 2. Five (63%) of the eight patients had a chest CT performed around the time of PCR diagnosis of COVID-19 (average, 1.6 days). Three of the five (60%) patients had dominant findings that were ground glass opacities, two with predominant consolidative opacities. Mid to lower lung zone involvement across craniocaudal distribution was observed in three out of five patients (60%) and lower lobe predominant finding was observed in two. Peripheral findings were observed in three out of five patients (60%), and diffuse opacities were observed in two patients. No patients had septal thickening. Two out of five patients had pleural effusions. Nodules were observed in only one patient, with centrilobular in distribution. Reverse halo sign was observed in one patient. Reticulation and traction bronchiectasis was not present on initial imaging in any patient. The average severity score was 51.2 out of 100. The highest severity score of 88 was in patient # 3, who also required ICU admission, but has been discharged on room air. Two of the five patients had repeat CT imaging, both demonstrating interval decrease of opacities. One patient had near complete resolution (Fig 1), and patient #3 demonstrated chronic lung disease findings including traction bronchiectasis, volume loss and reticulations (Fig 2).
Table 2.
Chest CT Findings
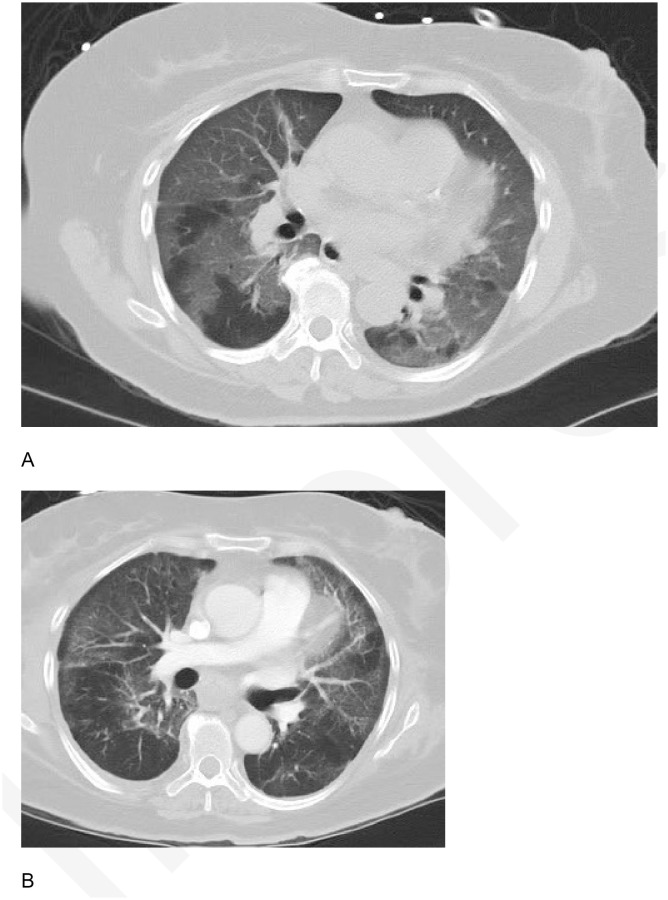
Figure 1:
(A) Axial chest CT on lung windows of patient #4 at presentation demonstrates bilateral right greater than left lower lobe consolidations with surrounding ground glass opacities. (B) Follow-up image 2 weeks later demonstrates substantial improvement in bilateral lower lobe consolidations with minimal residual opacities and tiny effusions.
Figure 2:
(A) Axial chest CT on lung windows of patient #3 at initial presentation demonstrates widespread diffuse ground glass opacities affecting all five lobes. (B) Follow-up image 27 days later demonstrates decreasing ground glass opacities, with areas of subpleural clearance.
Hospital Course, Short Term Follow-Up, and Clinical Outcome
Six out of eight (75%) patients were discharged as of the cut-off date of the study with an average length of stay for 13.5 days (range 4–31). The remaining two patients were still hospitalized. Of the five patients who were immunosuppressed, all but one had abnormalities either on chest radiography or CT. Two patients were considered to be potentially coinfected with respiratory viral or bacterial infection (patient #1 and 4). Five (63%) patients received COVID-19 specific treatment (such as remdesivir, antibody cocktail, dexamethasone, and antibiotics). Two patients (25%) required ICU admission. The two patients requiring ICU admission (#3 and 4) also had the highest severity score of CT findings (88 and 60, respectively). Since admission, patient #3 has been discharged on room air and patient #4 is transferred to the regular medical floor without respiratory symptoms on room air. No patients died during hospitalization during the study period.
Discussion
In the current study, we provide an initial description of the chest radiographic and CT findings of patients with COVID-19 breakthrough illness in the hospital setting. Most patients (57%) had a normal chest radiograph. The most common findings on abnormal chest radiographs were a combination of hazy opacities and consolidation. In those patients who had follow up radiographs, 75% (three of four) demonstrated stable to decreased opacities. The most common imaging findings on a chest CT were ground glass opacities which were observed in 60% (three of five) of the patients. In those patients who had follow-up chest CT, all demonstrated improvement in parenchymal findings, with one patient demonstrating signs of post infectious lung disease and/or chronic lung disease. A majority (75%; six of eight) of the hospitalized patients with breakthrough COVID-19 received the Pfizer-BioNTech vaccine.
The majority of our patients (75%; six of eight) reported mild respiratory symptoms prior to presentation, and one patient presented with gastrointestinal and genitourinary symptoms at the time of admission. As of the end of the study, six of eight patients were discharged without residual respiratory symptoms. Although two patients required ICU admission, one was discharged with no residual respiratory symptoms on room air, and the second patient was transferred to a medical floor on room air and without residual respiratory symptoms.
Breakthrough COVID-19 cases are very uncommon to date. According to a large study performed in Israel among 11,500 fully vaccinated individuals, only 39 (0.34%) individuals were identified as having breakthrough COVID-19 (5). All affected patients had mild to no symptoms. Individuals fully vaccinated against COVID-19 are less likely to become infected with SARSCoV-2 particularly if they have high levels of antibodies. As the vaccinated population continues to rise, there will likely be an increase in the number of breakthrough cases. The Center for Disease Control (CDC) is pursuing multiple effectiveness studies and is monitoring breakthrough cases, but despite such cases, the CDC strongly encourages individuals to receive the COVID-19 vaccine as it is effective and crucial for combating the pandemic.
Our results are in line with the clinical findings of COVID-19 breakthrough as reported in the literature, demonstrating that imaging findings in such patients are commonly mild (5). Outcomes in our patients were generally favorable. While larger studies are needed to establish imaging differences between breakthrough and unvaccinated populations, awareness of the variability of COVID-19 breakthrough imaging findings is critical.
The pathophysiology of breakthrough illness is hypothesized to be related to low titers of neutralizing antibody and S-specific IgG antibody and this may serve as a marker of breakthrough infection (5). Several studies support the concept that vaccinated individuals are less contagious than unvaccinated persons (6–9).
There are a few limitations of this study, including the small patient population size and the use of a retrospective analysis technique. In addition, there may be some selection bias as only hospitalized COVID-19 breakthrough patients were analyzed.
In conclusion, we present eight patients who were fully vaccinated and hospitalized with COVID-19 infection. The majority of the patients with COVID-19 breakthrough illness had absent or mild imaging findings and a benign clinical course. As the number of COVID-19 breakthrough cases is likely to increase, it will be important to continually document imaging findings to determine if the imaging patterns remain consistent with those observed in this study or whether they evolve.
Footnotes
Authors declared no funding for this work.
Disclosures of conflicts of interest: R.H. No relevant relationships. J.J. No relevant relationships. C.S.W. Associate editor of Radiology: Cardiothoracic Imaging.
References
- 1.Covid-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University https://coronavirus.jhu.edu/map.html. In, 2020
- 2. https://www.cdc.gov/vaccines/covid-19/health-departments/breakthrough-cases.html .
- 3. Monaco CG , Zaottini F , Schiaffino S , et al . Chest x-ray severity score in COVID-19 patients on emergency department admission: a two-centre study [Erratum in: Eur Radiol Exp. 2021 Apr 14;5] [1] [:17. PMID: 33319321; PMCID: PMC7735892] . Eur Radiol Exp 2020. ; 4 ( 1 ): 68 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Francone M , Iafrate F , Masci GM , et al . Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis . Eur Radiol 2020. ; 30 ( 12 ): 6808 – 6817 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bergwerk M, Gonen T, Lustig Y, et al. Covid-19 Breakthrough Infections in Vaccinated Health Care Workers. N Engl J Med 2021;385(16):1474–1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Regev-Yochay G , Amit S , Bergwerk M , et al . Decreased infectivity following BNT162b2 vaccination: A prospective cohort study in Israel . Lancet Reg Health Eur 2021. ; 7 : 100150 – 100150 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Petter E , Mor O , Zuckerman N , . Initial real world evidence for lower viral load of individuals who have been vaccinated by BNT162b2 . . [Google Scholar]
- 8.Pratò S, Paladino ME, Riva MA, Deni M, Belingheri M.. SARS-CoV-2 transmission risk to household and family contacts by vaccinated healthcare workers. J Occup Environ Med 2021;63(7):e474–e476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shah ASV , Gribben C , Bishop J , et al . Effect of vaccination on transmission of COVID-19: an observational study in healthcare workers and their households . . [Google Scholar]