Since March 2020, the world’s attention has been focused on the morbidity and mortality suffered due to the COVID-19 pandemic. However, in the United States (US) and globally, cardiovascular disease (CVD) continues to be the leading cause of mortality.1 Although targeted public health campaigns have reduced overall death rates from CVD, the decline in CVD mortality has slowed nationally since 2010.2, 3 Moreover, the rate of premature CVD mortality continues to increase in the US, accounting for 1 in 5 deaths among persons 25–64 years of age.1 Premature morbidity and mortality from CVD among working age adults is of particular salience to public health, and there is an increasing awareness that the lack of a viable social safety net for the growing numbers of Americans in need of preventive and diagnostic health services threatens the previous progress made in improving the burden of CVD.
In this issue of Circulation, Khan et al. present an analysis of county-level variation in social vulnerability and its association with premature CVD mortality.4 The authors linked county-level data from the Centers for Disease Control and Prevention (CDC) Social Vulnerability Index (SVI) with county-level mortality data from the CDC Wide-Ranging Online Data for Epidemiologic Research (WONDER). The SVI estimates how populations are especially vulnerable to a public health emergency by accounting for 4 factors: 1) socioeconomic status (SES), 2) household composition and disability, 3) minority status and language, and 4) housing type and transportation. Concentrated vulnerability mediated through poverty may diminish a community’s ability to withstand a natural disaster or a disease outbreak, as we have recently witnessed during the COVID-19 pandemic. Early race-ethnic disparities in the death toll from COVID-19 laid the foundation for frank conversations about which populations were most susceptible during the pandemic, with social determinants of health and socioeconomic inequality emerging as the strongest risk factors for adverse outcomes due to SARS-CoV-2. Greater social adversity has also been associated with increased risk for CVD and worse clinical outcomes.5 Individual SES predicts greater burden of traditional CV risk factors, worse access to and often worse quality of healthcare, and greater psychological distress.6 Beyond individual SES, neighborhood SES and characteristics such as access to grocery stores and healthful food sources, walkability and facilities for physical activity, and greenspace are associated with ideal cardiovascular health. While favorable neighborhood conditions are associated with increased uptake of lifestyle behaviors that reduce CVD risk, neighborhoods with greater numbers of race-ethnic minorities are less likely to have favorable conditions due to structural racism, with residents of these neighborhoods having worse access to healthful food sources, less greenspace, poor walkability, and overall fewer opportunities for health promoting behaviors.7, 8 As income inequality widens in the US, it may become apparent that future public health interventions to reduce premature CVD mortality should continue to target traditional CV risk factors, but place even greater emphasis on the impact of social vulnerability.
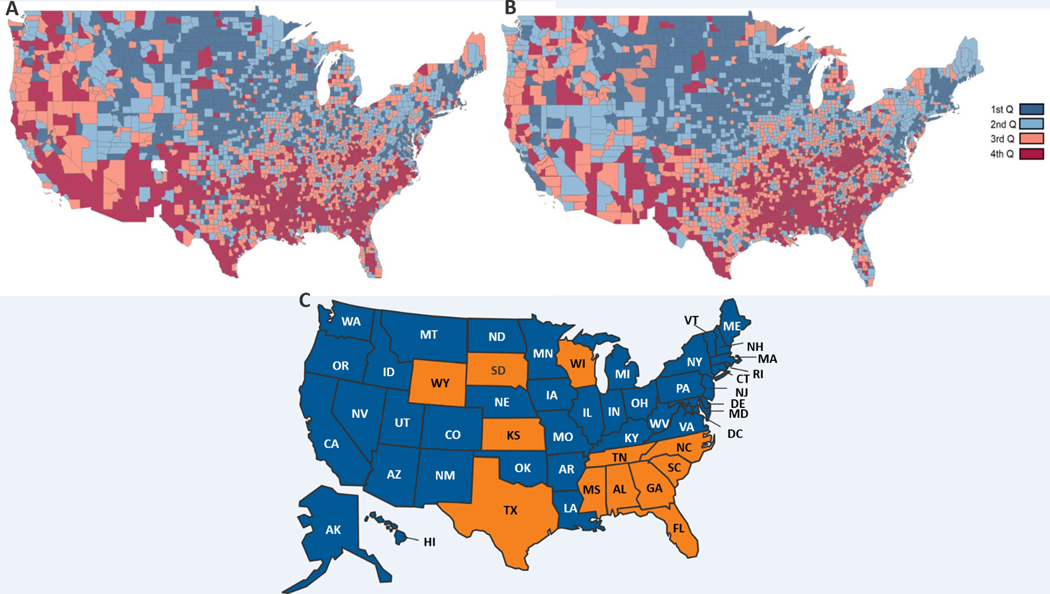
The primary finding from the analysis by Khan et al. is that US counties with more social vulnerability had higher premature mortality for CVD (onset in persons age <65 years) and CVD subtypes (ischemic heart disease, stroke, hypertension, and heart failure). However, there are several additional novel findings that are worth noting: 1) The largest concentration of counties with social vulnerability and CVD mortality were located in the Southern and Southwestern US (Figures 1A and B); 2) Social vulnerability associates with risk in a dose-dependent fashion, such that the age-adjusted mortality rates (AAMR) for CVD and its subtypes increased step-wise according to SVI quartiles (1st quartile being least vulnerable and 4th quartile being most vulnerable); and 3) the rate ratio (RR) varied by race, gender, and rural location. Non-Hispanic Black individuals had higher RRs for stroke and HF mortality when comparing the most and least vulnerable SVI quartiles. Women had a two-fold higher RR of CVD mortality, and residents of rural counties had a two- to five-fold higher RR of CVD mortality when comparing the most and least vulnerable SVI quartiles.
Figure 1.
Social vulnerability index (A) and premature cardiovascular disease mortality (B) in the United States from 2004–2018, compared to status of state Medicaid expansion decisions (C).
In panel C, states that have adopted and implemented Medicaid expansion are in blue, states that have not adopted yellow. Data is from https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/.15
The findings of this study reconfirm that the social determinants of health are a persistent and pervasive contributor to disease in vulnerable communities. Here, even with the use of an index that was developed to help public health officials respond to emergency weather events, disease outbreaks, or dangerous chemical exposures, the authors are able to demonstrate a dose-dependent association of county-level social vulnerability with rates of premature CVD mortality, with evidence of variation for specific demographic subgroups. If the SVI was developed with the intent of helping “emergency response planners and public health officials identify and map communities that will most likely need support before, during, and after a hazardous event”, then the authors have added to the literature here by helping to identify who among us is the most vulnerable. If the disease outbreak in question is premature CVD, these findings would suggest the most vulnerable among us are Black Americans, women, and Americans in rural areas, and that public health officials should devote most of their efforts to improving the health of these subgroups. Certainly, race-ethnicity and gender influence the likelihood of engaging in healthy lifestyle behaviors, even among subjects with elevated atherosclerotic CVD risk.9 However, the differential social stratification of Black Americans and women places them uniquely at risk for adverse outcomes. Both structural racism and the “gendered structural determinants of health” may have similar results for Black Americans and women – fewer opportunities for education and lower educational attainment, lower paying jobs, and higher rates of poverty, which, coupled with societal discriminatory norms, have negative influences on health outcomes for both groups.10, 11
So what are the implications of this data? Hopefully the COVID-19 pandemic has taught us that preparedness for the next disaster is key to winning the battle. And most clinicians, patients, and public health officials would agree that reducing the burden of premature CVD is a critical battle that we must meet head on. The current analysis by Khan et al. identifies regions and populations which are more vulnerable to premature CVD, and indicates the importance of addressing socioeconomic disparities in this effort. The challenge is identifying the practical interventions that can be implemented in vulnerable regions. Although years of targeting traditional CV risk factors alone has resulted in a plateau in overall CVD death rates, we have seen a recent rise in premature CVD mortality among young and middle-aged adults. The authors address this point by suggesting expansion of Medicaid to non-elderly adults facing adverse social circumstances. Indeed, ensuring equitable access to opportunities for healthy lifestyle, as well as high-quality, affordable healthcare and preventive services for all Americans should be a universal goal.12 Although recent data demonstrate that states that expanded Medicaid under the Affordable Care Act have had fewer deaths from CV causes than non-expansion states, 8 of the 12 states that have currently opted not to expand Medicaid are in regions of the US that are considered “socially vulnerable” according to the current analysis (Figure 1C).13, 14 In addition to expansion of healthcare coverage, public health interventions aimed at improving the built environment are required, including policies to increase healthy food availability, greenspace, and resources for physical activity may improve the cardiovascular health of residents in vulnerable communities. Particularly in rural communities, health officials need to continue to increase the availability of primary care and specialty health care providers, implementing cardiac rehab programs and other interventions known to improve outcomes in at-risk populations.
The current study highlights specific populations and regions that are more vulnerable to premature CVD mortality, so the real question is “who will protect the most vulnerable among us”? Enacting change on a national level will require the creation of health policies that enable positive therapeutic and healthy lifestyle behaviors in vulnerable communities, and policies that ensure our entire US population has access to adequate health services. Without addressing these social determinants of health, the prior achievements made in CVD prevention and treatment remain vulnerable to reversal.
References
- 1.Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang NY and Tsao CW. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143:e254–e743. [DOI] [PubMed] [Google Scholar]
- 2.Sidney S, Quesenberry CP Jr., Jaffe MG, Sorel M, Nguyen-Huynh MN, Kushi LH, Go AS and Rana JS. Recent Trends in Cardiovascular Mortality in the United States and Public Health Goals. JAMA cardiology. 2016;1:594–9. [DOI] [PubMed] [Google Scholar]
- 3.Ma J, Ward EM, Siegel RL and Jemal A. Temporal Trends in Mortality in the United States, 1969–2013. J Am Heart Assoc. 2015;314:1731–9. [DOI] [PubMed] [Google Scholar]
- 4.Khan SU, Javed Z, Lone AN, Dani S, Amin Z, Al-Kindi SG, Virani SS, Sharma G, Blankstein R, Blaha MJ, Cainzos-Achirica M and Nasir K. Social Vulnerability and Premature Cardiovascular Mortality Among US Counties, 2014–2018. Circulation. 2021. [DOI] [PubMed]
- 5.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M and Yancy CW. Social Determinants of Risk and Outcomes for Cardiovascular Disease. Circulation. 2015;132:873–898. [DOI] [PubMed] [Google Scholar]
- 6.Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, Quyyumi AA, Taylor HA, Gulati M, Harold JG, Mieres JH, Ferdinand KC, Mensah GA and Sperling LS. Socioeconomic Status and Cardiovascular Outcomes. Circulation. 2018;137:2166–2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unger E, Diez-Roux AV, Lloyd-Jones DM, Mujahid MS, Nettleton JA, Bertoni A, Badon SE, Ning H and Allen NB. Association of neighborhood characteristics with cardiovascular health in the multi-ethnic study of atherosclerosis. Circulation Cardiovascular quality and outcomes. 2014;7:524–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, Sanchez E, Sharrief AZ, Sims M and Williams O. Call to Action: Structural Racism as a Fundamental Driver of Health Disparities: A Presidential Advisory From the American Heart Association. Circulation. 2020;142:e454–e468. [DOI] [PubMed] [Google Scholar]
- 9.Morris AA, Ko YA, Hutcheson SH and Quyyumi A. Race/Ethnic and Sex Differences in the Association of Atherosclerotic Cardiovascular Disease Risk and Healthy Lifestyle Behaviors. J Am Heart Assoc. 2018;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nayak A, Hicks AJ and Morris AA. Understanding the Complexity of Heart Failure Risk and Treatment in Black Patients. Circulation Heart failure. 2020;13:e007264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaw LJ, Pepine CJ, Xie J, Mehta PK, Morris AA, Dickert NW, Ferdinand KC, Gulati M, Reynolds H, Hayes SN, Itchhaporia D, Mieres JH, Ofili E, Wenger NK and Bairey Merz CN. Quality and Equitable Health Care Gaps for Women: Attributions to Sex Differences in Cardiovascular Medicine. Journal of the American College of Cardiology. 2017;70:373–388. [DOI] [PubMed] [Google Scholar]
- 12.Warner JJ, Benjamin IJ, Churchwell K, Firestone G, Gardner TJ, Johnson JC, Ng-Osorio J, Rodriguez CJ, Todman L, Yaffe K, Yancy CW and Harrington RA. Advancing Healthcare Reform: The American Heart Association’s 2020 Statement of Principles for Adequate, Accessible, and Affordable Health Care: A Presidential Advisory From the American Heart Association. Circulation. 2020;141:e601–e614. [DOI] [PubMed] [Google Scholar]
- 13.Khatana SAM, Bhatla A, Nathan AS, Giri J, Shen C, Kazi DS, Yeh RW and Groeneveld PW. Association of Medicaid Expansion With Cardiovascular Mortality. JAMA cardiology. 2019;4:671–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.https://www.kff.org/medicaid/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/. Accessed February 19, 2021.
- 15.Status of State Medicaid Expansion Decisions: Interactive Map. https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/