Abstract
Background:
Anaphylaxis is a potentially fatal acute allergic reaction. Its overall prevalence appears to be rising, but little is known about US hospitalization trends among infants and toddlers.
Objective:
To identify the trends and predictors of hospitalization for anaphylaxis among infants and toddlers.
Methods:
We used the nationally representative National Inpatient Sample (NIS), from 2006 to 2015, to perform an analysis of trends in US hospitalizations for anaphylaxis among infants and toddlers (age, <3 years) and other children (age, 3–18 years). For internal consistency, we identified patients with anaphylaxis by the International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis code and excluded those with the International Classification of Diseases, Tenth Revision, Clinical Modification (late 2015). We calculated trends in anaphylaxis hospitalizations over time by age group and then used multivariable logistic regression to describe anaphylaxis hospitalizations among infants and toddlers.
Results:
Among infants and toddlers, there was no significant change in anaphylaxis hospitalizations during the 10-year study period (Ptrend = .14). Anaphylaxis hospitalization among infants and toddlers was more likely in males, with private insurance, in the highest income quartile, with chronic pulmonary disease, who presented on a weekend day, to an urban teaching hospital, located in the Northeast. In contrast, anaphylaxis hospitalizations among older children (age, 3-<18 years) rose significantly during the study (Ptrend < .001).
Conclusion:
Anaphylaxis hospitalizations among infants and toddlers in the United States were stable from 2006 to 2015, whereas hospitalizations among older children were rising. Future research should focus on the trends in disease prevalence and health care utilization in the understudied population of infants and toddlers.
Introduction
Anaphylaxis is a severe and potentially life-threatening acute allergic reaction (AAR) that can occur at any age.1 The lifetime prevalence of anaphylaxis is likely rising,2 although little is known about the trends in health care utilization among children with anaphylaxis. Even less is known about the trends for the youngest children—infants and toddlers. Infants and toddlers are an understudied patient population with variable clinical presentation and high rates of food-induced anaphylaxis (FIA).3,4
The rising prevalence of food allergy and anaphylaxis has a substantial impact on patients, families, and our health care system.5,6 Children with food allergies, and their parents, have decreased health-related quality of life.7 In 2007, the direct medical costs of food-induced AARs (FAARs), including FIA, were estimated at $225 million, with a large portion attributable to hospitalization.8 To more fully understand the trends in health care utilization for anaphylaxis among infants and toddlers, we used a nationally representative database of US hospital inpatient stays to investigate the trends and predictors of hospitalization from 2006 to 2015.
Methods
We conducted a study of the trends in anaphylaxis hospitalizations among infants and toddlers (age, <3 years) in the United States from 2006 to 2015. To maintain internal validity, we excluded data from the final quarter of 2015 after the transition to the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) coding.
Data Sources
We utilized data from the Healthcare Cost and Utilization Project National (Nationwide) Inpatient Sample (NIS),9 a nationally representative US database of hospital inpatient stays, maintained by the Agency for Healthcare Research and Quality (AHRQ). The NIS is a large, publicly available, all-payer inpatient health care database. It provides US regional and national estimates of inpatient utilization, access, quality, and outcomes. With weighting, it estimates more than 35 million hospitalizations annually, comprising more than 95% of all discharges in the United States. This study was approved by the local institutional review board.
Study Population
We identified hospitalization diagnoses among infants and toddlers (age, <3 years) and older children (age, 3-<18 years) by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes as follows:
Anaphylaxis
Anaphylactic shock owing to unspecified food (995.60), anaphylactic shock owing to specified food (995.61–995.69), and other anaphylactic shock (995.00) comprise this category. The anaphylaxis definition corresponds to method 1 of the previously validated algorithm by Harduar-Morano et al.10 This anaphylaxis definition includes FIA, in addition to other nonfood triggers of anaphylaxis.
AAR
Allergy unspecified (995.3), dermatitis owing to ingested food (693.1), anaphylactic shock owing to unspecified food (995.60), anaphylactic shock owing to specified food (995.61–995.69), and other anaphylactic shock (995.00) comprise this category. This is the broadest category of allergic reaction. Overall AAR contains the codes for anaphylaxis, FAAR, FIA, and additional codes related to allergic reactions.
FIA
Anaphylactic shock owing to unspecified food (995.60) and anaphylactic shock owing to specified food (995.61–995.69) comprise this category. The FIA includes only the anaphylaxis codes directly related to FIA.
FAAR
Dermatitis owing to ingested food (693.1), anaphylactic shock owing to unspecified food (995.60), and anaphylactic shock owing to specified food (995.61–995.69) comprise this category. Overall FAAR includes the codes for FIA and those within AAR that are associated with food-induced allergy.
These 4 categories of allergic reactions (anaphylaxis, AAR, FIA, FAAR) are not mutually exclusive but rather represent 4 groupings of ICD-9-CM codes based on potential reaction severity and trigger.
Outcomes
The primary outcome of the study was to characterize the temporal trend in US hospitalizations for anaphylaxis among infants and toddlers. The secondary outcomes were to characterize the trends in hospitalizations for overall AAR, FIA, and overall FAAR.
Covariates
We evaluated multiple covariates, including patient demographics and hospital characteristics. Patient demographics include age, sex, race and ethnicity, primary payer, and median household income quartile.
Hospital characteristics include discharge quarter, hospitalization day (weekday vs weekend), hospital region, hospital size, hospital status (rural or urban, teaching or nonteaching), endotracheal intubation or mechanical ventilation, number of procedures, length of stay (days), and hospital disposition (home, other medical facility, deceased, other). Use of endotracheal intubation and mechanical ventilation was identified by ICD-9-CM procedure codes 96.7 and 96.04, respectively. Chronic pulmonary disease was identified by the Chronic Condition Indicator (maintained by the NIS), which allows for identification of a condition that was chronic and likely presented before admission. Chronic conditions are then mapped to 18 different body systems, including respiratory diseases. The Chronic Condition Indicator for pulmonary disease includes asthma and other chronic respiratory diseases. Admission to the intensive care unit was not available in this data set.
Statistical Analyses
All analyses were performed using SAS version 9.4 (SAS Institute, Cary, North Carolina). Data are presented as proportions with 95% confidence intervals, or medians with interquartile ranges (IQRs), as appropriate. We calculated the trends in the number of total hospitalizations per 100,000 visits by age group during the study period using appropriate survey weighting. All 2015 proportions were weighted to account for censoring of ICD-10-CM codes in the final quarter of 2015. To examine anaphylaxis hospitalizations, we performed multivariable logistic regression modeling comparing anaphylaxis hospitalizations to hospitalizations for other causes. We included multiple covariates in the model, including year, age, sex, race and ethnicity, primary payer, median household income quartile, discharge quarter, hospitalization day (weekday vs weekend), hospital region, hospital size, hospital status (rural or urban, teaching or nonteaching), endotracheal intubation or mechanical ventilation, history of chronic pulmonary disease, number of procedures, and length of stay (days). All P values were 2-tailed, with P < .05 considered statistically significant.
Results
Trends in Hospitalization
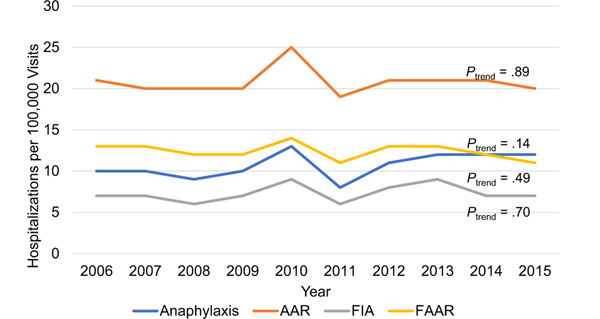
Anaphylaxis hospitalizations among infants and toddlers remained stable at 10 per 100,000 visits in 2006 and 12 per 100,000 visits in 2015 (Ptrend = .14) (Fig 1). Infants and toddlers hospitalized for FIA also remained stable at 7 per 100,000 visits in 2006 and 2015 (Ptrend = .70). A similar, stable trend was found among infants and toddlers hospitalized for AAR (Ptrend = .89) and FAAR (Ptrend = .49) (Table 1 and eTable 2).
Figure 1.
Hospitalizations among infants and toddlers (age, <3 years) by type of allergic reaction in the United States from 2006 to 2015. Overall AAR includes codes for anaphylaxis, FIA, and FAAR. Anaphylaxis includes FIA and non–food-related anaphylaxis. Overall FAAR includes FIA and other food-related codes. AAR, acute allergic reaction; FAAR, food-induced acute allergic reaction; FIA, food-induced anaphylaxis.
Table 1.
Hospitalizations for Allergic Reactions Among Infants and Toddlers (Age, <3 Years) in the United States From 2006 to 2015
| Diagnosis groupa | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | Absolute change | P trend |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|||
| Weighted admissions (95% CI) per 100,000 visits | ||||||||||||
| Anaphylaxis | 10 (6–13) | 10 (7–12) | 9 (6–12) | 10 (7–13) | 13 (8–18) | 8 (6–10) | 11 (8–14) | 12 (9–15) | 12 (9–14) | 12 (8–15) | 2 | .14 |
| Overall AAR | 21 (16–26) | 20 (16–24) | 20 (16–25) | 20 (15–24) | 25 (18–32) | 19 (15–22) | 21 (17–25) | 21 (17–25) | 21 (17–25) | 20 (15–24) | −1 | .89 |
| FIA | 7 (4–11) | 7 (5–9) | 6 (4–9) | 7 (5–10) | 9 (5–14) | 6 (4–7) | 8 (6–10) | 9 (7–11) | 7 (5–9) | 7 (5–9) | 0 | .70 |
| Overall FAAR | 13 (9–17) | 13 (10–16) | 12 (8–15) | 12 (9–15) | 14 (9–20) | 11 (8–13) | 13 (10–16) | 13 (10–16) | 12 (9–14) | 11 (8–14) | −2 | .49 |
Abbreviations: ARR, acute allergic reaction; CI, confidence interval; FAAR, food-induced acute allergic reaction; FIA, food-induced anaphylaxis.
Overall AAR includes codes for anaphylaxis, FIA, and FAAR. Anaphylaxis includes FIA and none-food-related anaphylaxis. Overall FAAR includes FIA and other food-related codes.
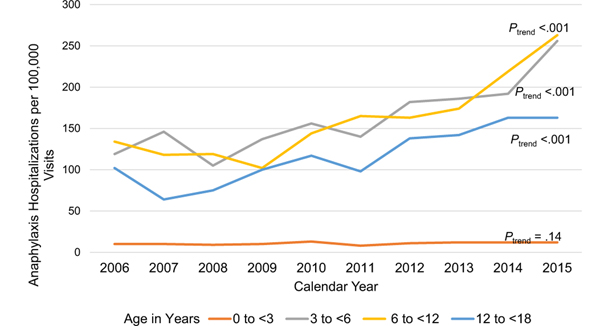
Conversely, among older children aged 3 to <6 years, 6 to <12 years, and 12 to <18 years, hospitalizations for anaphylaxis and AAR increased significantly over time (all groups Ptrend < .001) (Fig 2 and eTable 1). The highest absolute increase in anaphylaxis hospitalizations of 137 per 100,000 visits occurred in those aged 3 years to <6 years (Ptrend < .001). FIA hospitalizations among children aged 6 to <12 years (Ptrend = .001) and 12 to <18 years (Ptrend < .001) also increased, whereas FIA hospitalizations in children aged 3 to <6 years remained stable (Ptrend = .06).
Figure 2.
Anaphylaxis hospitalizations by age group among children (age, <18 years) in the United States from 2006 to 2015.
Patient and Hospital Characteristics
The characteristics of infants and toddlers hospitalized for anaphylaxis changed over time. Anaphylaxis hospitalizations among non-Hispanic Black, Hispanic, publicly insured, and in the lowest income quartile increased during the 10-year study period (Table 2). Similarly, anaphylaxis hospitalization increased in those admitted on a weekend day, in the South region of the United States, admitted to a large hospital, and with a history of chronic pulmonary disease.
Table 2.
Patient and Hospital Characteristics of Infants and Toddlers (Age, <3 Years) Hospitalized for Anaphylaxis in the United States From 2006 to 2015
| Characteristic | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | Absolute change | P trend c |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|||
| Weighted admissions per 100,000 population | ||||||||||||
| Age (<3 y) | 10 | 9 | 9 | 9 | 13 | 8 | 11 | 12 | 11 | 11 | 1 | .12 |
| Sex | ||||||||||||
| Male | 11 | 12 | 11 | 11 | 14 | 10 | 14 | 14 | 15 | 16 | 5 | .06 |
| Female | 8 | 6 | 7 | 7 | 12 | 5 | 8 | 10 | 8 | 6 | −2 | .72 |
| Race and ethnicity | ||||||||||||
| Non-Hispanic White | 12 | 11 | 10 | 8 | 13 | 7 | 10 | 10 | 10 | 8 | −4 | .33 |
| Non-Hispanic Black | 8 | 8 | 11 | 12 | 5 | 6 | 14 | 17 | 19 | 18 | 10 | .002 |
| Hispanic | 3 | 4 | 7 | 10 | 16 | 7 | 8 | 10 | 11 | 15 | 12 | <.001 |
| Other | 11 | 9 | 8 | 10 | 15 | 11 | 16 | 14 | 10 | 9 | −2 | .33 |
| Primary health insurance | ||||||||||||
| Public | 6 | 7 | 7 | 7 | 11 | 6 | 12 | 10 | 13 | 9 | 3 | .003 |
| Private | 14 | 10 | 12 | 11 | 16 | 11 | 12 | 15 | 11 | 15 | 1 | .72 |
| Self-pay | 4 | 6 | 2 | 15 | 10 | 3 | 3 | 6 | 5 | 4 | 0 | .82 |
| Other | 3 | 8 | 16 | 4 | 14 | 3 | 0 | 15 | 4 | 5 | 2 | .68 |
| Median household income quartilea | ||||||||||||
| 1 (lowest) | 6 | 6 | 8 | 8 | 9 | 6 | 9 | 12 | 12 | 8 | 2 | .01 |
| 2 | 9 | 9 | 7 | 6 | 9 | 7 | 7 | 10 | 11 | 11 | 2 | .40 |
| 3 | 9 | 8 | 9 | 11 | 16 | 9 | 11 | 9 | 10 | 10 | 1 | .76 |
| 4 (highest) | 17 | 12 | 14 | 12 | 20 | 10 | 19 | 18 | 14 | 17 | 0 | .53 |
| Discharge quarter | ||||||||||||
| First quarter (Jan-Mar) | 9 | 7 | 5 | 6 | 13 | 6 | 12 | 9 | 11 | 12 | 3 | .10 |
| Second quarter (Apr-Jun) | 15 | 12 | 11 | 11 | 12 | 8 | 10 | 13 | 14 | 14 | −1 | .78 |
| Third quarter (Jul-Sep) | 7 | 8 | 10 | 10 | 14 | 8 | 12 | 12 | 11 | 8 | 1 | .24 |
| Fourth quarter (Oct-Dec) | 8 | 9 | 11 | 9 | 14 | 9 | 11 | 14 | 10 | — | — | — |
| Admission on weekend | ||||||||||||
| No | 9 | 8 | 8 | 8 | 12 | 6 | 9 | 10 | 10 | 10 | 1 | .42 |
| Yes | 14 | 11 | 13 | 15 | 18 | 15 | 21 | 20 | 18 | 16 | 2 | .03 |
| Hospital region | ||||||||||||
| Northeast | 29 | 10 | 25 | 18 | 19 | 16 | 21 | 24 | 16 | 25 | −4 | .96 |
| Midwest | 7 | 11 | 4 | 5 | 5 | 7 | 9 | 14 | 9 | 4 | −3 | .70 |
| South | 6 | 9 | 4 | 7 | 9 | 7 | 8 | 8 | 13 | 10 | 4 | .02 |
| West | 5 | 5 | 10 | 11 | 22 | 4 | 12 | 9 | 9 | 11 | 6 | .25 |
| Hospital sizeb | ||||||||||||
| Small | 14 | 14 | 7 | 7 | 27 | 4 | 14 | 9 | 9 | 12 | −2 | .57 |
| Medium | 11 | 8 | 10 | 11 | 11 | 7 | 10 | 12 | 7 | 11 | 0 | .97 |
| Large | 8 | 8 | 9 | 9 | 12 | 9 | 11 | 13 | 15 | 11 | 3 | .01 |
| Hospital status | ||||||||||||
| Rural | 6 | 4 | 4 | 3 | 6 | 3 | 2 | 2 | 5 | 3 | −3 | .42 |
| Urban nonteaching | 4 | 5 | 5 | 6 | 5 | 5 | 5 | 4 | 2 | 3 | −1 | .16 |
| Urban teaching | 15 | 13 | 13 | 13 | 21 | 11 | 17 | 19 | 15 | 15 | 0 | .35 |
| Endotracheal intubation or mechanical ventilation | ||||||||||||
| No | 10 | 9 | 9 | 9 | 13 | 8 | 11 | 11 | 11 | 11 | 1 | .18 |
| Yes | 11 | 14 | 4 | 7 | 24 | 12 | 20 | 28 | 12 | 21 | 10 | .09 |
| Chronic pulmonary disease | ||||||||||||
| No | 9 | 8 | 8 | 8 | 11 | 7 | 10 | 10 | 11 | 10 | 1 | .16 |
| Yes | 78 | 123 | 166 | 138 | 210 | 68 | 191 | 244 | 160 | 239 | 161 | .02 |
| Hospitalization disposition | ||||||||||||
| Home | 10 | 9 | 9 | 10 | 14 | 8 | 11 | 12 | 12 | 11 | 1 | .10 |
| Other medical facility | 4 | 4 | 9 | 0 | 4 | 0 | 6 | 0 | 6 | 8 | 4 | NC |
| Deceased | 25 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | NC |
| Other | 13 | 16 | 10 | 3 | 0 | 0 | 17 | 9 | 15 | 0 | 0 | NC |
| Number of procedures on discharge, median (IQR) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | .44 |
| Hospitalization length of stay (d), median (IQR) | 0.6 (0.2, 0.9) | 0.7 (0.3, 1.4) | 0.6 (0.3, 0.9) | 0.7 (0.3, 1.3) | 0.7 (0.3, 1.3) | 0.7 (0.3, 1.5) | 0.6 (0.1, 1.0) | 0.7 (0.3, 1.2) | 0.7 (0.3, 1.6) | 0.7 (0.2, 1.3) | 0.08 | <.001 |
Abbreviations: Apr, April; CI, confidence interval; Dec, December; IQR, interquartile range; Jan, January; Jul, July; Jun, June; Mar, March; NC, noncalculable; Oct, October; Sep, September.
NOTE: For 95% CIs, please see eTable 2.
Median household income quartile: (1) 0 to 25th percentile, (2) 26th to 50th percentile, (3) 51st to 75th percentile, and (4) 76th to 100th percentile.
Hospital size was determined by the bed size and classified by the hospital region and teaching status.
P value < .05 is considered significant.
Mechanical Ventilation, Procedures, Length of Stay, and Disposition
There was no significant change in the trend of infants and toddlers requiring mechanical ventilation or endotracheal intubation during the study period (Ptrend = .09). The median number of procedures remained stable at 0 throughout the study period (P = .44). The median length of stay remained less than 1 day during the study period but was rising over time from 0.6 days (IQR, 0.2–0.9) in 2006 to 0.7 (IQR, 0.2–1.3) in 2015 (P < .001) (Table 2). Most of the patients were discharged home after hospitalization. There were a total of 5 deaths during the entire study period; owing to low absolute numbers, we were unable to calculate trends over time.
Anaphylaxis Hospitalizations
Among infants and toddlers, anaphylaxis hospitalization was more likely among males, those with private insurance, in the highest income quartile, admitted on a weekend day, in the Northeast, admitted at urban teaching hospitals, requiring mechanical ventilation or endotracheal intubation, and with history of chronic pulmonary disease (Table 3). The number of procedures, but not the length of stay, was associated with anaphylaxis hospitalization.
Table 3.
Anaphylaxis Hospitalization Among Infants and Toddlers (Age, <3 Years) in the United States From 2006 to 2015
| Variable | aOR | 95% CI | P c |
|---|---|---|---|
| Year | 1.04 | (1.01–1.07) | .02 |
| Age | 5.64 | (5.18–6.14) | <.001 |
| Sex | |||
| Male | 1.00 | (Reference) | |
| Female | 0.61 | (0.53–0.71) | <.001 |
| Race and ethnicity | |||
| Non-Hispanic White | 1.00 | (Reference) | |
| Non-Hispanic Black | 1.12 | (0.90–1.39) | .29 |
| Hispanic | 0.83 | (0.67–1.03) | .09 |
| Other | 1.22 | (1.02–1.46) | .03 |
| Primary payer | |||
| Public | 1.00 | (Reference) | |
| Private | 1.48 | (1.27–1.73) | <.001 |
| Self-pay | 0.86 | (0.55–1.34) | .50 |
| Other | 0.80 | (0.50–1.28) | .35 |
| Median household income quartilea | |||
| 1 (lowest) | 1.00 | (Reference) | |
| 2 | 1.12 | (0.91–1.38) | .28 |
| 3 | 1.23 | (1.00–1.51) | .05 |
| 4 (highest) | 1.64 | (1.33–2.01) | <.001 |
| Discharge quarter | |||
| First quarter (Jan-Mar) | 1.00 | (Reference) | |
| Second quarter (Apr-Jun) | 1.56 | (1.33–1.85) | <.001 |
| Third quarter (Jul-Sep) | 1.48 | (1.24–1.77) | <.001 |
| Fourth quarter (Oct-Dec) | 1.33 | (1.11–1.60) | .002 |
| Admission on weekend | |||
| No | 1.00 | (Reference) | |
| Yes | 1.57 | (1.37–1.81) | <.001 |
| Hospital region | |||
| Northeast | 1.00 | (Reference) | |
| Midwest | 0.41 | (0.31–0.55) | <.001 |
| South | 0.40 | (0.32–0.50) | <.001 |
| West | 0.62 | (0.46–0.84) | .002 |
| Hospital sizeb | |||
| Small | 1.00 | (Reference) | |
| Medium | 0.94 | (0.64–1.38) | .75 |
| Large | 1.03 | (0.72–1.47) | .88 |
| Hospital status | |||
| Rural | 1.00 | (Reference) | |
| Urban nonteaching | 1.13 | (0.76–1.67) | .54 |
| Urban teaching | 2.58 | (1.80–3.69) | <.001 |
| Endotracheal intubation or mechanical ventilation | |||
| No | 1.00 | (Reference) | |
| Yes | 4.49 | (2.85–7.05) | <.001 |
| Chronic pulmonary disease | |||
| No | 1.00 | (Reference) | |
| Yes | 2.21 | (1.78–2.73) | <.001 |
| Number of procedures on discharge | 0.63 | (0.54–0.75) | <.001 |
| Hospitalization length of stay (d) | 1.00 | (0.96–1.04) | .93 |
Abbreviations: aOR, adjusted odds ratio; Apr, April; CI, confidence interval; Dec, December; Jan, January; Jul, July; Jun, June; Mar, March; Oct, October; Sep, September.
Median household income quartile: (1) 0 to 25th percentile, (2) 26th to 50th percentile, (3) 51st to 75th percentile, and (4) 76th to 100th percentile.
Hospital size was determined by the bed size and classified by the hospital region and teaching status.
P < .05 is considered significant.
Discussion
Using a nationally representative database from 2006 to 2015, we found no change in anaphylaxis hospitalizations among infants and toddlers (age, <3 years). We also found that there was no significant change in the trend of hospitalizations among infants and toddlers for overall AAR, FIA, and overall FAAR. In contrast, anaphylaxis hospitalization significantly increased among older children (age, 3-<18 years).
Trends in Hospitalizations
Few studies have specifically focused on the trends in anaphylaxis hospitalization among infants and toddlers. Infants and toddlers with anaphylaxis are a unique and vulnerable population owing to limited verbal skills and a variable, often nonspecific clinical presentation, all of which pose a considerable diagnostic challenge. Moreover, treatment of these small children can be complicated owing to limited access to appropriate weight-based epinephrine autoinjectors.3,11
Previous studies investigating trends in anaphylaxis hospitalization (including FIA) among children have reported conflicting results, and data with a specific focus on infants and toddlers are sparse. Several studies find similar trends of stable or declining anaphylaxis hospitalizations, with most studies focusing specifically on FIA, as this is the most common trigger of anaphylaxis among children.3,12,13 Our group previously reported a stable hospitalization rate among the youngest children (age, <2 years) for FIA using the nationally representative Healthcare Cost and Utilization Project Kids database from 2000 to 2009, despite a rising rate of hospitalization for FIA among older children.14 Similarly, using data from the NIS, one study reported a stable rate of anaphylaxis hospitalizations among children and adults from 2001 to 2014 with a rise found only in children aged 5 to 14 years with food-related reactions.15 Using a large administrative database of privately insured children from 2005 to 2014, there was a significant decline in hospitalization for children presenting with FIA despite a rise in emergency department (ED) visits.16 However, there was no specific analysis of younger children, infants or toddlers. In contrast, one study reported rising rates of FIA hospitalizations and ED visits among all children using a database of hospitals in Illinois from 2008 to 2012.17 The highest rates occurred in children aged 0 to 4 years.
Although the underlying reasons for the stable trends in anaphylaxis hospitalizations among infants and toddlers are not known, we propose a few possible explanations. We do not believe that our findings are due to a decline in overall prevalence of anaphylaxis or overall AAR. Although studies focusing specifically on infants and toddlers are limited, recent studies on the trends in prevalence of anaphylaxis and food allergy support a rising prevalence.5,16–19 A stable trend in hospitalization among only infants and toddlers, in the setting of rising hospitalizations among older children, is likely to be the result of factors unique to infants and toddlers, including changes in disease recognition, severity, management, and health care utilization.
This diagnostic challenge of anaphylaxis may lead to underdiagnosis of anaphylaxis among infants and toddlers and, thus, could potentially result in a falsely low report of hospitalizations.3 Anaphylaxis, even among older children, is often missed.4 The common symptomology of infant and toddler anaphylaxis, though not well defined, often includes nonspecific symptoms.3 Many of the more severe features of anaphylaxis (eg, cardiovascular collapse) appear to be rare, whereas more mild cutaneous and gastrointestinal symptoms appear to be common.11 This may suggest that the presentation of anaphylaxis among infants and toddlers is less severe and potentially even more susceptible to underdiagnosis. Our findings of few procedures and a low rate of mechanical ventilation during hospitalization generally support a mild severity of anaphylaxis among infants and toddlers. Thus, it is plausible that among infants and toddlers with anaphylaxis, the mild severity of reactions may make hospitalization unnecessary in many cases. These issues merit further investigation.
Although there are currently no specific guidelines on infant anaphylaxis, intramuscular epinephrine is widely accepted as first-line treatment.1,3 Delay in administration of epinephrine is associated with poor outcomes.20,21 In fact, early and appropriate treatment with epinephrine has been found to decrease risk of hospitalization.22 Over time, rates of epinephrine administration for anaphylaxis in general are increasing.23,24 Little is known about the trends of epinephrine administration among infants and toddlers. It is possible that owing to a less severe presentation of anaphylaxis, improved rates of epinephrine treatment among infants and toddlers would have a greater effect. Other changes in patterns of health care utilization, including use of ED observation units and urgent care centers, may have evolved during the study period, but we are unable to fully assess these trends in this study.
Importantly, our study was conducted before the publication and dissemination of both the paradigm-shifting Learning Early About Peanut study (2015)25 and the addendum National Institutes of Health food allergy guidelines (2017)26 for primary prevention of peanut allergy through early introduction of peanut. During our study period, many high-risk children probably were not exposed to allergenic foods as infants and toddlers, which could lead to fewer high-risk children having severe reactions at young ages. To more fully understand recent trends of anaphylaxis among infants and toddlers, it is imperative that we continue to study the trends in anaphylaxis in the era of early allergen introduction. This will be complicated by the ICD-10-CM transition in late 2015, but, with additional years of data, it may be possible to ascertain temporal changes despite this methodological challenge.
Patterns of Patient and Hospital Characteristics
During the study period, the proportion of infants and toddlers hospitalized for anaphylaxis were rising among non-Hispanic Black, Hispanics, publicly insured, and from the lowest income quartile. Despite these trends, White males with private insurance from the highest income quartile were the more likely to have an anaphylaxis hospitalization. This observed shift may represent a change in demographics of food allergy or differences in access to care.27 Racial/ethnic disparities have been associated with poor outcomes in anaphylaxis and differences in health care utilization in food allergy.28,29
Chronic pulmonary disease, which includes childhood asthma, was increasingly more common among infants and toddlers during the study period with anaphylaxis hospitalizations. This is consistent with previous studies that have revealed asthma is associated with severe anaphylaxis.20,30 Consistent with previous studies, we found the highest number of anaphylaxis hospitalizations in the Northeast.14,31 However, hospitalizations were rising significantly over time in the South.
Mechanical Ventilation, Length of Stay, Procedures, and Mortality
In this study, the use of mechanical ventilation or endotracheal intubation was rare and stable over time among infants and toddlers. The median number of procedures throughout the study period was 0 (Ptrend = .44). This is consistent with a previous study which found that children hospitalized with FAAR received few interventions during hospitalization.32 Despite a rising trend in length of stay (days), the median length of stay remained less than 1 day throughout the study period (P < .001). This is consistent with previous studies showing a short length of stay for children admitted with AAR or FIA.14,17,32 These findings support a low severity of anaphylaxis among hospitalized infants and toddlers or possibly a quick recovery. Cohort studies are needed to explore this important issue.
Potential Limitations
This study has several potential limitations. First, owing to the use of administrative data, coding errors resulting diagnostic misclassification is possible. On the basis of previous studies, anaphylaxis is often underdiagnosed by ICD-9-CM codes, and thus, we expect that we may be reporting an underestimate of the trend in hospitalization for anaphylaxis.4 As previously discussed, the diagnostic challenges of infants and toddlers may compound this underdiagnosis. However, we found similar results using ICD-9-CM codes for less severe allergic reactions, including overall AAR and overall FAAR. Owing to the transition from ICD-9-CM to ICD-10-CM in late 2015, we have data only from the first 3 quarters of 2015; however, the overall trends in hospitalization among infants and toddlers are present before 2015 and weighted estimates were used. Importantly, based on the nature of data in our study (hospitalization), we are unable to determine if the observed trends are due to change in prevalence or severity of anaphylaxis or changes in health care utilization. In addition, owing to limitations of the database, we are unable to accurately account for intensive care unit admission as a marker of severity. In the future, use of other data sets (eg, State Inpatient Database) and cohort studies will allow for more detailed study of these important topics.
In summary, using nationally representative data, we found that anaphylaxis hospitalizations among infants and toddlers were stable from 2006 to 2015, in contrast to rising trends in older children. Anaphylaxis hospitalization among infants and toddlers, as compared with other causes of hospitalization, was more likely in males, with private insurance, in the highest income quartile, with chronic pulmonary disease, admitted on a weekend day, to an urban teaching hospital, and located in the Northeast. Future research should focus on underlying trends in prevalence, severity, and health care utilization patterns of infants and toddlers with anaphylaxis. As additional years of data become available, we encourage future research on the trends in anaphylaxis among infants and toddlers in the era of early allergen introduction (ie, after landmark publications during 2015–2017).25,26 We anticipate that sufficient data through 2019 will be available in late 2021. Our study will be the benchmark by which we can compare future trends in the era of early allergen introduction.
Supplementary Material
Acknowledgments
Funding: Dr Robinson was supported by the National Institutes of Health award T32HL116275. Partial funding for this data analysis project was provided to Dr Camargo by kaleo, Inc (Richmond, Virginia).
Footnotes
Disclosures: The authors have no conflicts of interest to report.
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Supplementary Data
Supplementary data related to this article can be found at https://doi.org/10.1016/j.anai.2020.09.003.
References
- 1.Sampson HA, Muñoz-Furlong A, Campbell RL, et al. Second symposium on the definition and management of anaphylaxis: summary report—second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006;117(2):391–397. [DOI] [PubMed] [Google Scholar]
- 2.Wood RA, Camargo CA Jr, Lieberman P, et al. Anaphylaxis in America: the prevalence and characteristics of anaphylaxis in the United States. J Allergy Clin Immunol. 2014;133(2):461–467. [DOI] [PubMed] [Google Scholar]
- 3.Greenhawt M, Gupta RS, Meadows JA, et al. Guiding principles for the recognition, diagnosis, and management of infants with anaphylaxis: an expert panel consensus. J Allergy Clin Immunol Pract. 2019;7(4):1148–1156.e5. [DOI] [PubMed] [Google Scholar]
- 4.Rudders SA, Banerji A, Clark S, Camargo CA Jr. Age-related differences in the clinical presentation of food-induced anaphylaxis. J Pediatr. 2011;158(2):326–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta RS, Springston EE, Warrier MR, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011; 128(1):e9–e17. [DOI] [PubMed] [Google Scholar]
- 6.Sicherer SH, Sampson HA. Food allergy: a review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. J Allergy Clin Immunol. 2018;141(1):41–58. [DOI] [PubMed] [Google Scholar]
- 7.Flokstra-de Blok BMJ, Dubois AEJ. Quality of life measures for food allergy. Clin Exp Allergy. 2012;42(7):1014–1020. [DOI] [PubMed] [Google Scholar]
- 8.Patel DA, Holdford DA, Edwards E, Carroll NV. Estimating the economic burden of food-induced allergic reactions and anaphylaxis in the United States. J Allergy Clin Immunol. 2011;128(1):110–115.e5. [DOI] [PubMed] [Google Scholar]
- 9.Agency for Healthcare Research and Quality. HCUP databases. Available at: www.hcup-us.ahrq.gov/databases.jsp. Accessed June 1, 2020.
- 10.Harduar-Morano L, Simon MR, Watkins S, Blackmore C. Algorithm for the diagnosis of anaphylaxis and its validation using population-based data on emergency department visits for anaphylaxis in Florida. J Allergy Clin Immunol. 2010;126(1):98–104.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simons FE, Sampson HA. Anaphylaxis: unique aspects of clinical diagnosis and management in infants (birth to age 2 years). J Allergy Clin Immunol. 2015; 135(5):1125–1131. [DOI] [PubMed] [Google Scholar]
- 12.Grabenhenrich LB, Dolle S, Moneret-Vautrin A, et al. Anaphylaxis in children and adolescents: the European Anaphylaxis Registry. J Allergy Clin Immunol. 2016;137(4):1128–1137.e1. [DOI] [PubMed] [Google Scholar]
- 13.Lee S, Hess EP, Lohse C, Gilani W, Chamberlain AM, Campbell RL. Trends, characteristics, and incidence of anaphylaxis in 2001–2010: a population-based study. J Allergy Clin Immunol. 2017;139(1):182–188.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rudders SA, Arias SA, Camargo CA Jr. Trends in hospitalizations for food-induced anaphylaxis in US children, 2000–2009. J Allergy Clin Immunol. 2014; 134(4):960–962.e3. [DOI] [PubMed] [Google Scholar]
- 15.Shrestha P, Dhital R, Poudel D, Donato A, Karmacharya P, Craig T. Trends in hospitalizations related to anaphylaxis, angioedema, and urticaria in the United States. Ann Allergy Asthma Immunol. 2019;122(4):401–406.e2. [DOI] [PubMed] [Google Scholar]
- 16.Motosue MS, Bellolio MF, Van Houten HK, Shah ND, Campbell RL. National trends in emergency department visits and hospitalizations for food-induced anaphylaxis in US children. Pediatr Allergy Immunol. 2018;29(5): 538–544. [DOI] [PubMed] [Google Scholar]
- 17.Dyer AA, Lau CH, Smith TL, Smith BM, Gupta RS. Pediatric emergency department visits and hospitalizations due to food-induced anaphylaxis in Illinois. Ann Allergy Asthma Immunol. 2015;115(1):56–62. [DOI] [PubMed] [Google Scholar]
- 18.Motosue MS, Bellolio MF, Van Houten HK, Shah ND, Campbell RL. Increasing emergency department visits for anaphylaxis, 2005–2014. J Allergy Clin Immunol Pract. 2017;5(1):171–175.e3. [DOI] [PubMed] [Google Scholar]
- 19.Rudders SA, Banerji A, Vassallo MF, Clark S, Camargo CA Jr. Trends in pediatric emergency department visits for food-induced anaphylaxis. J Allergy Clin Immunol. 2010;126(2):385–388. [DOI] [PubMed] [Google Scholar]
- 20.Pouessel G, Turner PJ, Worm M, et al. Food-induced fatal anaphylaxis: from epidemiological data to general prevention strategies. Clin Exp Allergy. 2018; 48(12):1584–1593. [DOI] [PubMed] [Google Scholar]
- 21.Turner PJ, Jerschow E, Umasunthar T, Lin R, Campbell DE, Boyle RJ. Fatal anaphylaxis: mortality rate and risk factors. J Allergy Clin Immunol Pract. 2017; 5(5):1169–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fleming JT, Clark S, Camargo CA Jr, Rudders SA. Early treatment of food-induced anaphylaxis with epinephrine is associated with a lower risk of hospitalization. J Allergy Clin Immunol Pract. 2015;3(1):57–62. [DOI] [PubMed] [Google Scholar]
- 23.Clark S, Boggs KM, Balekian DS, et al. Changes in emergency department concordance with guidelines for the management of food-induced anaphylaxis: 1999–2001 versus 2013–2015. J Allergy Clin Immunol Pract. 2019;7(7): 2262–2269. [DOI] [PubMed] [Google Scholar]
- 24.Clark S, Boggs KM, Balekian DS, et al. Changes in emergency department concordance with guidelines for the management of stinging insect-induced anaphylaxis: 1999–2001 vs 2013–2015. Ann Allergy Asthma Immunol. 2018; 120(4):419–423. [DOI] [PubMed] [Google Scholar]
- 25.Du Toit G, Roberts G, Sayre PH, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372(9):803–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Togias A, Cooper SF, Acebal ML, et al. Addendum guidelines for the prevention of peanut allergy in the United States: report of the National Institute of Allergy and Infectious Diseases-sponsored expert panel. J Allergy Clin Immunol. 2017;139(1):29–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McGowan EC, Keet CA. Prevalence of self-reported food allergy in the National Health and Nutrition Examination Survey (NHANES) 2007–2010. J Allergy Clin Immunol. 2013;132(5):1216–1219.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jerschow E, Lin RY, Scaperotti MM, McGinn AP. Fatal anaphylaxis in the United States, 1999–2010: temporal patterns and demographic associations. J Allergy Clin Immunol. 2014;134(6):1318–1328.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mahdavinia M, Fox SR, Smith BM, et al. Racial differences in food allergy phenotype and health care utilization among US children. J Allergy Clin Immunol Pract. 2017;5(2):352–357.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith PK, Hourihane JOB, Lieberman P. Risk multipliers for severe food anaphylaxis. World Allergy Organ J. 2015;8(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Camargo CA Jr, Clark S, Kaplan MS, Lieberman P, Wood RA. Regional differences in EpiPen prescriptions in the United States: the potential role of vitamin D. J Allergy Clin Immunol. 2007;120(1):131–136. [DOI] [PubMed] [Google Scholar]
- 32.Rudders SA, Clark S, Camargo CA Jr. Inpatient interventions are infrequent during pediatric hospitalizations for food-induced anaphylaxis. J Allergy Clin Immunol Pract. 2017;5(5):1421–1424.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.