Abstract
Introduction
The 1-year mortality rate after femoral intertrochanteric fracture is higher than that of femoral neck fracture, which also belongs to hip fracture (Cui et al. in Arch Osteoporos 14(1):55, 2019). With the application of the concept of co-management model of orthopedics and geriatrics, the short-term and long-term mortality of all types of hip fractures has decreased (Van Heghe et al. in Calcif Tissue Int, 2021, https://doi.org/10.1007/s00223-021-00913-5). However, the mortality of Chinese femoral intertrochanteric fracture patients under this model has not been reported in the literatures.
Aim
This paper aims to study the risk factors of postoperative all-cause mortality in aged patients with femoral intertrochanteric fracture under the co-management model of orthopedics and geriatrics.
Materials and methods
This is a single-center prospective cohort study based on the real world, under the co-management of orthopedics and geriatrics, 363 patients aged ≥ 65 years with femoral intertrochanteric fracture were enrolled and followed up for 2–3 years; 52 patients were lost to follow up. Age, gender, body mass index (BMI), history of comorbidities, hip Bone Mineral Density (BMD), fracture history, 25(OH)D level, hemoglobin level, anti-osteoporosis treatment were risk factors to be tested. Kaplan–Meier survival curves and multivariate Cox proportional hazards models were constructed to analyze the impact of factors on all-cause mortality.
Results
(1) Most of the dead patients were older (the mean age was 83.4 years, compared with 79.8 years for surviving patients), with more complications and without anti-osteoporosis medication; gender, pre-fracture history, BMI, total hip BMD, hemoglobin, 25(OH)D had no difference between the dead and the living patients. (2) Elderly patients with Intertrochanteric fracture can benefit from the early treatment of Zoledronic Acid (within 3 days after the operation).
Conclusion
Under the co-management of orthopedics and geriatrics, to Chinese patients with Femoral Intertrochanteric fracture, Doctors should pay more attention to their age and chronic disease, and give anti-osteoporosis treatment if allowed.
Keywords: Osteoporosis, Femoral intertrochanteric fracture, Zoledronic acid, Mortality
Background
Due to the increased proportion of the elderly population, increasing life expectancy, and light labor lifestyle, the number of patients with osteoporosis and osteoporotic fractures had increased, and brought a high economic burden and nursing management challenges to patients, medical staff, and society [3, 4]. The number of osteoporosis-related fractures would grow to about 6 million and cost $25.4 billion annually by the year 2050 [3]. And Hip fracture is one of the main consequences of osteoporosis, with devastating results for the affected patients, including markedly increased subsequent fracture risk [5] and significant increased all-cause mortality [6]. Approximately 33% of men and 22% of women suffering a hip fracture will die within 1 year [7, 8]. To patients older than 75, Intertrochanteric fracture contributed more to the crude growth rate than femoral neck fracture [9]. And according to a systematic analysis, the pooled estimate of the 1-year mortality rate was 17.47% after femoral intertrochanteric fracture and 9.83% after femoral neck fracture between 2000 and 2018 [1]. Although hip fracture is discussed as a unified discussion, there is a significant difference in the incidence rate and mortality after operation for femoral intertrochanteric fracture and femoral neck fracture.
Now, clinicians believe that re-fracture [10] and all-cause mortality [11] can be reduced by early surgery [12], reduced bed rest, and anti-osteoporosis treatment [10, 13]. Especially in recent years, with the participation of orthogeriatrics, the proposal of the concept of rapid rehabilitation, the increase in the use of anti-osteoporosis drugs, and the improvement of medical care and patients' understanding of the disease, the in-hospital mortality and all-cause mortality of elderly hip fracture patients have been further reduced. It can also be seen from the repeated correction of the Nottingham Hip Fracture Score (NHFS) [14–16].
In this context, this paper aims to explore the risk factors of all-cause mortality in patients with femoral intertrochanteric fracture under the co-management of orthopedics and geriatrics.
Patients and methods
Study population
After the patient is admitted to the emergency department a pelvic X-ray is made as soon as possible; after diagnosing a hip fracture, a geriatrician is consulted before surgery for each patient with a hip fracture. All the patients over 65 years will be admitted to the geriatric trauma unit within the orthopedic trauma department, and geriatrics and orthopedics were managed together throughout the hospitalization. No surgery during weekends. Almost all patients used proximal femoral nail fixation, seldom of patients used dynamic hipscrew, and no patients used hip arthroplasty. Early mobilization after surgery with a physiotherapist was arranged on the first day from postoperative.
All patients were given osteoporosis health education and had basic calcium and vitamin D3. No patients had nonunion at the end of the follow-up.
Inclusion and exclusion criteria
The inclusion criteria in our study were: (1) patients admitted with new femoral intertrochanteric fracture (≤ 3 weeks) and patients aged ≥ 65 years; (2) patients who received no anti-osteoporosis medication before, except calcium + vitamin D supplementations; (3) only unilateral fracture; (4) creatinine clearance rate was higher than 35 ml/min(Cockcroft-Gault formula).
Exclusion criteria were as follows: (1) pathological fractures caused by malignant tumors; (2) patients with secondary osteoporosis; (3) high-energy fractures and/or age below 65 years; (4) patients who have received other anti-osteoporosis medications except for ZOL and basement therapy, such as teriparatide acetate, Denosumab, after surgery;(5) patients with life expectancy less than 2 years, patients with tumor metastasis.
Follow-up method
The physicians followed up the patients or the family members who lived with the patients by outpatient service and telephone in this study. Time was expressed in months; time to death was calculated from the date of surgery. The date of death or the last interview with the patients or the family members was used to determine the end of follow-up.
Risk factors
Age, gender, body mass index, history of comorbidities (using CCI), hip BMD (DXA), fracture history, 25(OH)D level, and hemoglobin level were determined at the admission date. The date of ZOL use voluntarily was recorded; as the number of patients treated with anti-osteoporosis drugs other than ZOL is very small, only single digits, so this study does not include these patients. The secondary fractures were recorded during follow-up. Confounders were included in the final model if they changed the beta coefficient of the association > 5%.
Statistical analysis
An estimated 294 cases would be needed to provide 90% power for a COX regression module of PASS15.0 software, assuming all-cause mortality after fracture was 10%, incident rate was 45%, and the hazard ratio of risk factors was 0.3, with a two-sidedαof 0.05 and 20% loss of follow-up rate.
A summary of the data was presented as mean ± SD, and/or percentage. Cases with missing values are deleted. For comparisons of patients’ age, BMI, and CCI between two groups, t tests were used. For comparisons of gender, patients with CCI ≥ 3, and pre-fracture and post-fracture numbers between two groups, χ2-tests were used.
Kaplan–Meier survival curves were constructed and stratified by gender, age, CCI, and dosing ZOL or not. The impact factors on all-cause mortality were analyzed in multivariate Cox proportional hazards models. Forward and backward stepwise models and the Akaike information criterion were used to determine the most parsimonious models and address potential biases. All statistical analyses were performed using SPSS IBM version 19.0 software. P < 0.05 was considered statistically significant.
The study was approved by the Beijing Jishuitan hospital Review Board, approbation number 201907-09-02 in 2019.
Results
General information
A total of 363 patients aged ≥ 65 years with femoral intertrochanteric fracture were enrolled in this prospective cohort study, the patients were consecutively admitted from May 2015 to December 2017; 52 patients were lost to follow-up, 311 patients were followed up for 2–3 years. The patients were aged from 65 to 99 years, with an average of 80.2 ± 6.5 years. There were 80 men and 231 women. There were 223 (72.9%) patients with internal diseases and 69 (22.5%) with three or more types of internal disease. The Charlson comorbidity index (CCI) was 0–6. The mean time from admission to surgery was 66.5 h, and 49.8% of patients had surgery within 48 h on admission. The average time from fracture to surgery was 4.3 days, 22.7% of patients had surgery within 48 h after fracture. One hundred and thirty-nine patients accepted Zoledronic Acid 5 mg (Aclasta) on their own free will less than 3 days after surgery.
The general data of living and dead patients were compared. The results showed that most of the dead patients were older, lighter weight, with more complications. However, the previous history of fragile fracture, total hip BMD, HGB, 25OHD had no difference between the dead and the living patients. The data are shown in Table 1. The average age of men was 80.7 ± 6.6 years old and that of women was 80.1 ± 6.4 years old. There was no significant difference in age between genders (P = 0.470). There were 4 males (5.0%) and 14 females (6.1%) over 90 years old.
Table 1.
General condition of the femoral intertrochanteric fracture patients
| Case M/F |
Age | Pre-fracture M/F |
Re-fracture M/F |
BMI g/cm2 |
Hip-BMD g/cm2 |
HGB g/l |
25OHD ng/ml |
CCI ≥ 3 n (%) |
Zoledronic acid n (%) |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Alive | 274 (67/207) | 79.8 ± 6.4 | 13/55 | 5/19 | 23.5 ± 3.6 | 0.666 ± 0.125 | 113.7 ± 17.0 | 12.5 ± 8.2 | 58 (21.2) | 128 (46.7) |
| Death | 37 (13/24) | 83.4 ± 6.0 | 3/2 | 0/1 | 22.2 ± 4.0 | 0.647 ± 0.162 | 108.2 ± 20.5 | 11.0 ± 7.3 | 12 (32.4) | 11 (29.7) |
| Total | 311 (80/231) | 80.2 ± 6.5 | 16/57 | 5/20 | 23.4 ± 3.6 | 0.664 ± 0.130 | 113.0 ± 17.4 | 12.3 ± 8.1 | 70 (22.5) | 139 (44.7) |
| P valuea | 0.253 | 0.001 | 0.126 | 0.759 | 0.042 | 0.448 | 0.087 | 0.333 | 0.035 | 0.140 |
M, Male; F, female; BMI, body mass index; BMD, bone mineral density; HGB, hemoglobin; CCI, Charlson comorbidity index
aThe compare between alive and death;
All-cause mortality of cumulative survival rate
A total of 311 patients with fractures followed with an average time of 23.5 ± 5.0 months; 37 patients died during the follow-up period, the cumulative mortality after fracture was 10.8%, annual mortality for fracture was 5.4%. There were 13 men and 24 women among these 37 deaths, and the annual mortality was 6.1% in the male patients and 4.1% in the female patients. Of 37 deaths, 4 occurred within the hospital, 6 occurred within 3 months, 4 within 6 months, and 14 within 1 year after the fracture. The most common causes of mortality were cardiovascular events and pneumonia.
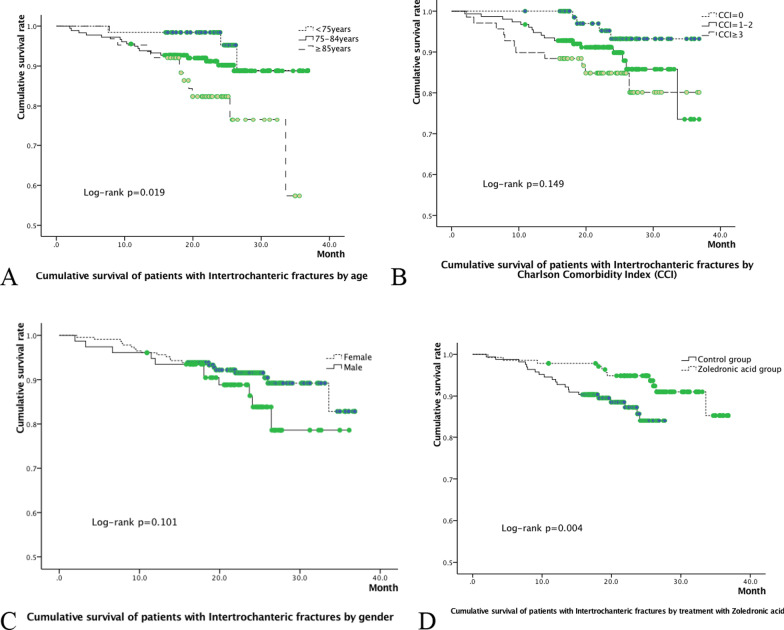
Kaplan–Meier survival curves analysis showed that all-cause mortality increased in more elderly patients (P = 0.019, Fig. 1A); but only had a growing trend with CCI 3 or bigger (P = 0.149, Fig. 1B), and showed no gender difference (P = 0.101, Fig. 1C), and there was a correlation between using ZOL and the cumulative survival rate (P = 0.004, Fig. 1D).
Fig. 1.
Cumulative survival of Intertrochanteric fracture patients by gender (A), age (B), Charlson comorbidity index (C) and dosing zoledronic acid or not (D)
Multivariate cox regression analysis
The multivariate Cox proportional hazards model was applied to estimate the effects of factors on cumulative survival rate. The factors evaluated in this model included age, gender, BMI, fracture history, hip BMD, hemoglobin, 25OHD, CCI, and dosing ZOL. In this study, BMI, fracture history, hip BMD, hemoglobin, and 25OHD were not associated with all-cause mortality.
In Intertrochanteric fracture patients, during a mean observation period of 23.5 months, age (P = 0.022), CCI (P = 0.046), and early use of ZOL (P = 0.005) were associated with all-cause mortality; gender (P = 0.126) was not relevant (Table 2). In Intertrochanteric fracture patients, the elderly over 85 years had a 1.87-fold higher risk than the younger elderly, and those with a CCI index over 3 had a 1.63-fold higher risk of all-cause mortality than those with less than 3. In Intertrochanteric fracture patients, the early postoperative use of ZOL reduced the risk of all-cause mortality by 67%.
Table 2.
Multivariate cox proportional analysis of risk factors for mortality in hip fracture patients
| Type | Variable | HR (95% CI) | P value |
|---|---|---|---|
| Intertrochanteric fracture | Gender, male/female | – | 0.126 |
| Age, ≥ 85/75 to 85/< 75 years | 1.87 (1.10–3.19) | 0.022 | |
| CCI, ≥ 3/1 to 2/0 | 1.63 (1.01–2.63) | 0.046 | |
| ZOL, use/none | 0.33 (0.16–0.71) | 0.005 |
Blank cells indicate variables were not significant in the multivariate Cox proportional hazards models
CI, Confidence interval; HR, hazard ration; CCI, Charlson comorbidity index; ZOL, zoledronic acid
Discussion
Most studies have treated hip fracture as a single, homogeneous condition, while hip fracture includes two major anatomic types: fractures of the intertrochanteric region and fractures of the femoral neck; the former is an extracapsular fracture, and the latter belongs to intracapsular fracture. And the trochanteric region has a greater proportion of trabecular bone than the femoral neck (50% vs 25%) [17]. The composition of bone in the two regions differs, so the etiology of each fracture type may also differ. A prospective study showed femoral neck and intertrochanteric fractures have different risk factors [18], BMD and poor functional ability largely predicted femoral neck fracture, while aging and poor health status predisposes to intertrochanteric fracture. Another prospective study showed that differences in patient characteristics and sequelae do exist between the femoral neck and intertrochanteric hip fracture patients that impact upon recovery. And it appears that intertrochanteric fracture patients have intrinsic factors (older age, poor health) impacting upon their risk of fracture and ability to recover [19]. A retrospective study showed mortality rate at 90 days was 12.1% for intertrochanteric fractures and 9.6% for femoral neck fractures [20]. Another prospective study even suggested that fracture type is an independent predictor of mortality in hip fracture patients, both at 1 month and at 1 year after injury [21]. So we should treat the intertrochanteric fracture and femoral neck fracture differently, and analysis their mortality rate separately at least. We discuss all-cause mortality risk in the aged femoral intertrochanteric fracture in this article.
In recent years, many guidelines and expert consensus recommend that the multi-department cooperative treatment group should be established in the treatment of hip fracture in elderly patients to improve perioperative safety, and operate as soon as possible (within 48 h), and then accelerate rehabilitation under the guidance of rehabilitation doctors [22–24]. In the process of multi-department collaborative treatment, the cooperation between orthopedics and geriatrics is important. Grigoryan et al. [25] summarized 18 studies through meta-analysis and found that the cooperative treatment of elderly hip fractures by orthopedics doctors and geriatricians can shorten the length of hospital stay and reduce in-hospital mortality and long-term mortality. So it is a more efficient way to establish a special ward and adopt the co-management model between orthopedics and geriatrics (or internal medicine) [26, 27]. With the co-management of orthopedics and geriatrics, an all-cause mortality rate of patients included in this article decreased significantly, the 1-year mortality rate was 4.5% compared with 17.47%, which was from a systematic analysis data after femoral intertrochanteric fracture between the years 2000 and 2018 in Mainland China [1]. Therefore, this article explored the risk factors of all-cause mortality under this model.
Under the co-management model of orthopedics and geriatrics, from our data, risk factors of all-cause mortality were older age, CCI, and early use of ZOL; they were consistent with previous studies [28–31]. While male gender was not a risk factor. It is speculated that different data have different gender and age distribution; it is also possible that the number of data in this paper is still insufficient and cannot show the difference. Old age is an important predictor of all-cause mortality, even accounting for 3–4 points in NHFS score [16]. Charlson proposed CCI in 1987, 19 concomitant diseases that significantly affect the survival time are weighted according to the severity, which can well reflect the comorbid state of patients.
To the dosing of ZOL, we summarized different studies about all-cause mortality after bisphosphonates treatment in patients with hip fracture (Table 3), from the hazard ratios, it seems China's hip fracture population had better effects. The influence of ethnicity is huge. Such as, Chinese people are prone to atypical fracture after continuous BPs [32–34]. It may also be related to the better effect in patients with femoral intertrochanteric fracture.
Table 3.
Simple summary of different studies on improving all-cause mortality after bisphosphonates treatment in patients with hip fractures
| References | Anti-OP drug | Use time | Frequency | Fracture type | Race or region | Research type | Treated cases N | Age | Mean follow-up time (M) | HR (95% CI) | P value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lyles et al. [45] | ZOL | ≤ 90 days after surgical | Yearly | Hip fracture | No Asia | Randomized, double-blind, placebo-controlled trial | 1065 | ≥ 50 | 22.8 | 0.72 (0.56, 0.93) | 0.01 |
| Eriksen et al. [46] | ZOL | ≤ 2 week after surgical | Yearly | Hip fracture | No Asia | Randomized, double-blind, placebo-controlled trial | 56 | ≥ 50 | 22.8 | – | > 0.05 |
| Bergman et al. [47] | ZOL | – | – | Hip fracture | Sweden | Retrospective cohort study | 161 | ≥ 50 | 33.6 | 1.51 (1.00, 2.28) | 0.048 |
| Wang et al. [48] | ZOL | ≤ 2 weeks after admission | – | Hip fracture | China | Retrospective study | 80 | ≥ 50 | 28.5 | 0.36 (0.19, 0.65) | < 0.01 |
| Brozek et al. [49] | All BP and Denosumab | ≤ 1 year | – | Hip fracture | Austria | Retrospective nationwide cohort study | 2166 | ≥ 50 | 36 | 0.48 (0.42, 0.55) | < 0.0001 |
| Bergman et al. [47] | Alendronate | – | – | Hip fracture | Sweden | Retrospective cohort study | 4689 | ≥ 50 | 33.6 | 0.82 (0.76, 0.89) | < 0.001 |
| Bondo et al. [50] | Oral BP | 5 month after fracture | > 2 packs | Hip fracture | Danish | Nationwide register-based open cohort study | 1096 | ≥ 55 | 45.6 | 0.73 (0.61, 0.88) | 0.001 |
| Axelsson et al. [51] | Alendronate | – | ≥ 3 months | Hip fracture | Sweden | Prospective observational register-based study | 1961 | ≥ 80 | 19.2 | 0.88 (0.82, 0.95) | < 0.01 |
| Beaupre et al. [52] | Oral BP | 1 and 2 years | 64% yearly | Hip fracture | Canada | Randomized controlled trial | 101 | > 50 | 36 | 0.92 (0.88, 0.97) | 0.001 |
| Van Geel et al. [53] | Oral BP | 2 weeks later | Continued 5 years | Clinical fracture (21.7% for hip fracture) | Scotland | Prospective cohort study | 2534 | ≥ 50 | 44.9 | 0.79 (0.64, 0.97) | 0.021 |
| This study | ZOL | ≤ 3 days after surgical | Once | Intertrochanteric fracture | China | Prospective cohort study | 139 | ≥ 65 | 23.5 | 0.33 (0.16–0.71) | 0.005 |
– Indicate variables were not significant in the multivariate Cox proportional hazards models
OP, Osteoporosis; HR, hazard ration; CI, confidence interval; ZOL, Zoledronic acid; BP, Bisphosphonates
As we know, bisphosphonates (BPs) bind to hydroxyapatite crystals in bone, especially at sites with high bone turnover [35], which means BPs bind strongly at sites of new mineral deposition, also binds well to resorption sites. And more BPs is taken up by trabecular bone than cortical bone, for a higher rate of turnover and greater surface area available in trabecular bone [36]. BPs released from bone may undergo re-uptake onto bone surfaces, so they can be detected in urine for years after treatment discontinuation [37, 38]. Patents healing after fracture is in the period of rich callus formation, and their bone metabolism is more active; therefore, after using ZOL during fracture healing, patients will retain more ZOL in the bone, which can play a more effective and longer anti-osteoporosis effect. As there is more bone trabecular in the intertrochanteric region, and bone turnover markers are higher after operation of intertrochanteric fracture [39], we have reasons to believe that ZOL deposit more in intertrochanteric fracture, so it may also affect the long-term prognosis.
However, we cannot consider that ZOL reduces the all-cause mortality of patients with femoral intertrochanteric fracture by reducing secondary fractures. A meta-analysis collected all randomized controlled trial study of osteoporosis agents with proven anti-fracture indicated that mortality risk reduction was not associated with the reduction in the incidence of a new hip, vertebral or non-hip non-vertebral fracture [40]. And, there are clinical, animal, and molecular studies that proved immune-modulatory effects; bone loss and bone turnover decreasing; fibrosis and apoptosis effects are all had effects on decreasing all-cause mortality [41].
The feature of this study was that ZOL was used within 3 days after surgery, which is early; most of the published studies on the use of BPs after hip fracture have been used for 2–4 weeks or later. On the other hand, it verified that the early use of ZOL did not bring more adverse. Another feature of the study was that ZOL was used only once during the observation period of 2–3 years, due to the less attention paid to osteoporosis treatment by patients and their families and the inconvenient activities of patients. For ZOL effects on BMD and fracture risk persisted for at least 2 years [42–44], which makes ZOL a more attractive proposition. This design also avoids immortal time bias, multiple medication bias, the arbitrary time point of administration, and adherence bias.
Conclusion
Determination of risk factors supports doctors to identify patients who were at high risk for mortality and enables accurate preoperative risk assessment. We should pay attention to the patients with femoral intertrochanteric fracture over 85 years old and CCI greater than or equal to 3, and give ZOL and basic anti-osteoporosis treatment in time.
Limitations
This study has two major limitations. First, this is a single-center study, the sample size was relatively small, while data are homogeneous thus eliminating the potential confounding factors; however, a multi-centric study with more patients evaluated could better address the risk factor in elderly patients who have undergone a hip fracture. Second, some data are incompletely reported, and this could influence the evaluation of data.
Acknowledgements
Thank all colleagues in the elderly hip fracture ward for their hard work.
Authors’ contributions
XL designed the study, performed the analysis and prepared the first draft of the paper. MY and PZ contributed to acquisition and interpretation of data. SZ, XW, and XJ contributed to the design of the work and the interpretation of data. All authors revised the paper critically for intellectual content and approved the final version. All authors agree to be accountable for the work and to ensure that any questions relating to the accuracy and integrity of the paper are investigated and properly resolved.
Funding
Beijing Municipal Administration of Hospitals Incubating Program, Code: PX 2019015; Beijing Municipal Health Committee Scientific Research Project, Code: Beijing 19-17; Capital’s Funds for Health Improvement and Research, Code: 2018-1-2071.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
The Ethics Board of Beijing Jishuitan Hospital approved the study with the approval number of 201907-09.
Consent for publication
All authors consent for publication.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cui Z, Feng H, Meng X, Zhuang S, Liu Z, Ye K, et al. Age-specific 1-year mortality rates after hip fracture based on the populations in mainland China between the years 2000 and 2018: a systematic analysis. Arch Osteoporos. 2019;14(1):55. doi: 10.1007/s11657-019-0604-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van Heghe A, Mordant G, Dupont J, Dejaeger M, Laurent MR, Gielen E. Effects of orthogeriatric care models on outcomes of hip fracture patients: a systematic review and meta-analysis. Calcif Tissue Int. 2021 doi: 10.1007/s00223-021-00913-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Si L, Winzenberg TM, Jiang Q, Chen M, Palmer AJ. Projection of osteoporosis-related fractures and costs in China: 2010–2050. Osteoporos Int. 2015;26(7):1929–1937. doi: 10.1007/s00198-015-3093-2. [DOI] [PubMed] [Google Scholar]
- 4.Biz C, Fantoni I, Crepaldi N, Zonta F, Buffon L, Corradin M, et al. Clinical practice and nursing management of pre-operative skin or skeletal traction for hip fractures in elderly patients: a cross-sectional three-institution study. Int J Orthop Trauma Nurs. 2019;32:32–40. doi: 10.1016/j.ijotn.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Gibson-Smith D, Klop C, Elders P, Welsing P, Schoor N, Leufkens H, et al. The risk of major and any (nonhip) fragility fracture after hip fracture in the United Kingdom: 2000–2010. Osteoporos Int. 2014;25:2555–2563. doi: 10.1007/s00198-014-2799-x. [DOI] [PubMed] [Google Scholar]
- 6.Nazrun AS, Tzar MN, Mokhtar SA, Mohamed IN. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Manag. 2014;10:937–948. doi: 10.2147/TCRM.S72456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573–1579. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klop C, Welsing PM, Cooper C, Harvey N, Elders P, Bijlsma J, et al. Mortality in British hip fracture patients, 2000–2010: a population-based retrospective cohort study. Bone. 2014;66:171–177. doi: 10.1016/j.bone.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 9.Gong XF, Li XP, Zhang LX, Center JR, Bliuc D, Shi Y, et al. Current status and distribution of hip fractures among older adults in China. Osteoporos Int. 2021;32(9):1785–1793. doi: 10.1007/s00198-021-05849-y. [DOI] [PubMed] [Google Scholar]
- 10.Lee SY, Jung SH, Lee SU, Ha YC, Lim JY. Can bisphosphonates prevent recurrent fragility fractures? A systematic review and meta-analysis of randomized controlled trials. J Am Med Dir Assoc. 2018;19(5):384–390. doi: 10.1016/j.jamda.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Abtahi S, Burden AM, Geusens P, van den Bergh JP, van Staa T, de Vries F. The association of oral bisphosphonate use with mortality risk following a major osteoporotic fracture in the United Kingdom: population-based cohort study. J Am Med Dir Assoc. 2020;21(6):811–816. doi: 10.1016/j.jamda.2019.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Li W, Yang M. Fragility fracture network (FFN)-China successfully held forum to support FFN global call to action to improve the care of people with fragility fractures. Aging Med. 2018;1:280–281. doi: 10.1002/agm2.12048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, et al. IOF Fracture Working Group. Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int. 2013;24(8):2135–52. [DOI] [PMC free article] [PubMed]
- 14.Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth. 2008;101:511–517. doi: 10.1093/bja/aen236. [DOI] [PubMed] [Google Scholar]
- 15.Marufu TC, White SM, Griffiths R, Moonesinghe SR, Moppett IK. Prediction of 30-day mortality after hip fracture surgery by the Nottingham hip fracture score and the surgical outcome risk tool. Anaesthesia. 2016;71(5):515–521. doi: 10.1111/anae.13418. [DOI] [PubMed] [Google Scholar]
- 16.Moppett IK, Parker M, Griffiths R, Bowers T, White SM, Moran CG. Nottingham hip fracture score: longitudinal and multi-centre assessment. Br J Anaesth. 2012;109(4):546–550. doi: 10.1093/bja/aes187. [DOI] [PubMed] [Google Scholar]
- 17.Riggs BL, Wahner HW, Seeman E, Offord KP, Dunn WL, Mazess RB, et al. Changes in bone mineral density of the proximal femur and spine with aging: differences between the postmenopausal and senile osteoporosis syndromes. J Clin Invest. 1982;70:716–723. doi: 10.1172/JCI110667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fox KM, Cummings SR, Williams E, Stone K; Study of Osteoporotic Fractures. Femoral neck and intertrochanteric fractures have different risk factors: a prospective study. Osteoporos Int. 2000;11(12):1018–23. [DOI] [PubMed]
- 19.Fox KM, Magaziner J, Hebel JR, Kenzora JE, Kashner TM. Intertrochanteric versus femoral neck hip fractures: differential characteristics, treatment, and sequelae. J Gerontol A Biol Sci Med Sci. 1999;54(12):M635–M640. doi: 10.1093/gerona/54.12.m635. [DOI] [PubMed] [Google Scholar]
- 20.Frisch NB, Wessell N, Charters M, Greenstein A, Shaw J, Peterson E, Trent GS. Hip fracture mortality: differences between intertrochanteric and femoral neck fractures. J Surg Orthop Adv. 2018;27(1):64–71. [PubMed] [Google Scholar]
- 21.Haentjens P, Autier P, Barette M, Venken K, Vanderschueren D, Boonen S; Hip Fracture Study Group. Survival and functional outcome according to hip fracture type: a one-year prospective cohort study in elderly women with an intertrochanteric or femoral neck fracture. Bone. 2007;41(6):958–64. [DOI] [PubMed]
- 22.De Vincentis A, Behr AU, Bellelli G, Bravi M, Castaldo A, Galluzzo L, et al. Orthogeriatric co-management for the care of older subjects with hip fracture: recommendations from an Italian intersociety consensus. Aging Clin Exp Res. 2021;33(9):2405–2443. doi: 10.1007/s40520-021-01898-9. [DOI] [PubMed] [Google Scholar]
- 23.Mukherjee K, Brooks SE, Barraco RD, Como JJ, Hwang F, Robinson BRH, Crandall ML. Elderly adults with isolated hip fractures orthogeriatric care versus standard care: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2020;88(2):266–278. doi: 10.1097/TA.0000000000002482. [DOI] [PubMed] [Google Scholar]
- 24.Chinese Geriatrics Society Bone and Joint Association Orthopaedic Trauma Committee. Experts' concensus on diagnosis and management of geriatric hip fractures (2017). Chin J Orthop Trauma. 2017;19(11):921–27.
- 25.Grigoryan KV, Javedan H, Rudolph JL. Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma. 2014;28(3):49–55. doi: 10.1097/BOT.0b013e3182a5a045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Biber R, Singler K, Curschmann-Horter M, Wicklein S, Sieber C, Bail HJ. Implementation of a co-managed geriatric fracture center reduces hospital stay and time-to-operation in elderly femoral neck fracture patients. Arch Orthop Trauma Surg. 2013;133(11):1527–1531. doi: 10.1007/s00402-013-1845-z. [DOI] [PubMed] [Google Scholar]
- 27.Prestmo A, Hagen G, Sletvold O, Helbostad JL, Thingstad P, Taraldsen K, et al. Comprehensive geriatric care for patients with hip fractures: a prospective, randomised, controlled trial. Lancet. 2015;385(9978):1623–1633. doi: 10.1016/S0140-6736(14)62409-0. [DOI] [PubMed] [Google Scholar]
- 28.Wang CB, Lin CF, Liang WM, Cheng CF, Chang YJ, Wu HC, et al. Excess mortality after hip fracture among the elderly in Taiwan: a nationwide population-based cohort study. Bone. 2013;56(1):147–153. doi: 10.1016/j.bone.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 29.Ho-Le TP, Tran TS, Bliuc D, Pham HM, Frost SA, Center JR, Eisman JA, Nguyen TV. Epidemiological transition to mortality and refracture following an initial fracture. Elife. 2021;10:e61142. [DOI] [PMC free article] [PubMed]
- 30.Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5):513–521. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- 31.Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B. Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing. 2010;39(2):203–9. [DOI] [PubMed]
- 32.Koh JH, Myong JP, Yoo J, Lim YW, Lee J, Kwok SK, Park SH, Ju JH. Predisposing factors associated with atypical femur fracture among postmenopausal Korean women receiving bisphosphonate therapy: 8 years' experience in a single center. Osteoporos Int. 2017;28(11):3251–3259. doi: 10.1007/s00198-017-4169-y. [DOI] [PubMed] [Google Scholar]
- 33.Gedmintas L, Solomon DH, Kim SC. Bisphosphonates and risk of subtrochanteric, femoral shaft, and atypical femur fracture: a systematic review and meta analysis. J Bone Miner Res. 2013;28(8):1729–1737. doi: 10.1002/jbmr.1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lo JC, Hui RL, Grimsrud CD, Chandra M, Neugebauer RS, Gonzalez JR, et al. The association of race/ethnicity and risk of atypical femur fracture among older women receiving oral bisphosphonate therapy. Bone. 2016;85:142–147. doi: 10.1016/j.bone.2016.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fleisch H, Russell RG, Francis MD. Diphosphonates inhibit hydroxyapatite dissolution in vitro and bone resorption in tissue culture and in vivo. Science. 1969;165(3899):1262–1264. doi: 10.1126/science.165.3899.1262. [DOI] [PubMed] [Google Scholar]
- 36.Weiss HM, Pfaar U, Schweitzer A, Wiegand H, Skerjanec A, Schran H. Biodistribution and plasma protein binding of zoledronic acid. Drug Metabol Dispos. 2008;36(10):2043–2049. doi: 10.1124/dmd.108.021071. [DOI] [PubMed] [Google Scholar]
- 37.Khan SA, Kanis JA, Vasikaran S, Kline WF, Matuszewski BK, McCloskey EV, et al. Elimination and biochemical responses to intravenous alendronate in postmenopausal osteoporosis. J Bone Miner Res. 1997;12(10):1700–1707. doi: 10.1359/jbmr.1997.12.10.1700. [DOI] [PubMed] [Google Scholar]
- 38.Papapoulos SE, Cremers SC. Prolonged bisphosphonate release after treatment in children. N Engl J Med. 2007;356(10):1075–1076. doi: 10.1056/NEJMc062792. [DOI] [PubMed] [Google Scholar]
- 39.Li XP, Li XY, Yang MH, Zhu SW, Wu XB, Zhang P. Changes of bone turnover markers after elderly hip fracture surgery. J Bone Miner Metab. 2021;39(2):237–244. doi: 10.1007/s00774-020-01140-y. [DOI] [PubMed] [Google Scholar]
- 40.Bolland MJ, Grey AB, Gamble GD, Reid IR. Effect of osteoporosis treatment on mortality: a meta-analysis. J Clin Endocrinol Metab. 2010;95(3):1174–1181. doi: 10.1210/jc.2009-0852. [DOI] [PubMed] [Google Scholar]
- 41.Center JR, Lyles KW, Bliuc D. Bisphosphonates and lifespan. Bone. 2020;141:115566. doi: 10.1016/j.bone.2020.115566. [DOI] [PubMed] [Google Scholar]
- 42.Grey A, Bolland MJ, Wattie D, Horne A, Gamble G, Reid IR. The antiresorptive effects of a single dose of zoledronate persist for two years: a randomized, placebo-controlled trial in osteopenic postmenopausal women. J Clin Endocrinol Metab. 2009;94(2):538–544. doi: 10.1210/jc.2008-2241. [DOI] [PubMed] [Google Scholar]
- 43.Reid IR, Horne AM, Mihov B, Stewart A, Garratt E, Wong S, et al. Fracture prevention with zoledronate in older women with osteopenia. N Engl J Med. 2018;379(25):2407–2416. doi: 10.1056/NEJMoa1808082. [DOI] [PubMed] [Google Scholar]
- 44.Reid IR, Black DM, Eastell R, Bucci-Rechtweg C, Su G, Hue TF, et al. HORIZON Pivotal Fracture Trial and HORIZON Recurrent Fracture Trial Steering Committees. Reduction in the risk of clinical fractures after a single dose of zoledronic Acid 5 milligrams. J Clin Endocrinol Metab. 2013;98(2):557–63. [DOI] [PubMed]
- 45.Lyles KW, Colón-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, et al. HORIZON Recurrent Fracture Trial. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357(18):1799–809. [DOI] [PMC free article] [PubMed]
- 46.Eriksen EF, Lyles KW, Colón-Emeric CS, Pieper CF, Magaziner JS, Adachi JD, et al. Antifracture efficacy and reduction of mortality in relation to timing of the first dose of zoledronic acid after hip fracture. J Bone Miner Res. 2009;24(7):1308–1313. doi: 10.1359/jbmr.090209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bergman J, Nordström A, Hommel A, Kivipelto M, Nordström P. Bisphosphonates and mortality: confounding in observational studies? Osteoporos Int. 2019;30(10):1973–1982. doi: 10.1007/s00198-019-05097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang PW, Li YZ, Zhuang HF, Yu HM, Cai SQ, Xu H, et al. Anti-osteoporosis medications associated with decreased mortality after hip fracture. Orthop Surg. 2019;11(5):777–783. doi: 10.1111/os.12517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brozek W, Reichardt B, Zwerina J, Dimai HP, Klaushofer K, Zwettler E. Antiresorptive therapy and risk of mortality and refracture in osteoporosis-related hip fracture: a nationwide study. Osteoporos Int. 2016;27(1):387–396. doi: 10.1007/s00198-015-3415-4. [DOI] [PubMed] [Google Scholar]
- 50.Bondo L, Eiken P, Abrahamsen B. Analysis of the association between bisphosphonate treatment survival in Danish hip fracture patients a nationwide register based open cohort study. Osteoporos Int. 2013;24(1):245–252. doi: 10.1007/s00198-012-2024-8. [DOI] [PubMed] [Google Scholar]
- 51.Axelsson KF, Wallander M, Johansson H, Lundh D, Lorentzon M. Hip fracture risk and safety with alendronate treatment in the oldest-old. J Intern Med. 2017;282(6):546–559. doi: 10.1111/joim.12678. [DOI] [PubMed] [Google Scholar]
- 52.Beaupre LA, Morrish DW, Hanley DA, Maksymowych WP, Bell NR, Juby AG, Majumdar SR. Oral bisphosphonates are associated with reduced mortality after hip fracture. Osteoporos Int. 2011;22(3):983–991. doi: 10.1007/s00198-010-1411-2. [DOI] [PubMed] [Google Scholar]
- 53.Van Geel TACM, Bliuc D, Geusens PPM, Center JR, Dinant GJ, Tran T, et al. Reduced mortality and subsequent fracture risk associated with oral bisphosphonate recommendation in a fracture liaison service setting: a prospective cohort study. PLoS ONE. 2018;13(6):e0198006. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.