Abstract
Background: Studies have shown a decline in hospitalizations due to acute exacerbation of chronic obstructive pulmonary disease (AECOPD) during the coronavirus disease 2019 (COVID-19) pandemic. However, the impact of the pandemic on AECOPDs of all severities in longitudinal cohorts of patients is lacking.
Methods: We conducted analysis of 123 individuals with COPD who have been followed since 2017. AECOPDs of mild (treatment at home), moderate (emergency department or urgent visit evaluation), and severe (hospitalization) type were assessed by chart review and patient interview. Compliance with preventive measures to avoid COVID-19 infection was assessed in 2020. Differences between the rate of AECOPD by year was analyzed as well as differences in preventive measures by COPD disease severity.
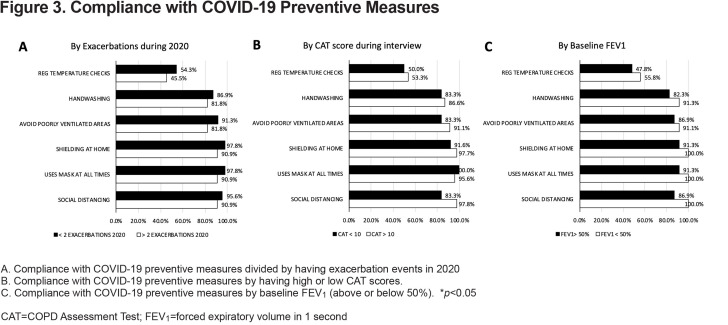
Results: During the COVID-19 pandemic in 2020, there was a significant reduction in AECOPDs in our cohort with 26 participants (21%) having an exacerbation compared to 46 (37%) in 2019, 52 (42%) in 2018, and 44 (36%) in 2017. Mean exacerbation rates decreased 54% overall and 74% in frequent exacerbators compared with the prior 3-year average. The decrease was noted in AECOPDs of all severities. Overall, there was a high rate of reported compliance with social distancing and face mask use that was significantly higher in the group with more severe COPD based on symptoms and forced expiratory volume in 1 second.
Conclusions: Individuals with COPD, including frequent exacerbators, showed a marked decrease in AECOPD during the COVID-19 pandemic and high adherence to recommended preventive measures. Evaluation of the impact of preventive strategies on AECOPD in a non-pandemic setting may be of value and requires further study.
Keywords: copd, exacerbations, COVID-19
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has brought devastating health consequences related to the severe respiratory complications directly caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection. In addition, it has indirectly affected the natural course of many other conditions by delaying timely health care driven by institutional restriction policies or by patients’ fear of infection. Surprisingly, reports have emerged describing a significant reduction in the incidence of several acute conditions. For example, using a neuroimaging database, it was observed that the number of patients being evaluated for acute ischemic cerebrovascular accidents decreased 39% in the early pandemic compared with the pre-pandemic epoch1 and using hospital admission data, the incidence of acute coronary syndromes decreased 27% during the early pandemic.2 Although some possible reasons for this can be inferred, the dynamics of why these acute conditions presented less to health systems and their real incidence is unclear.
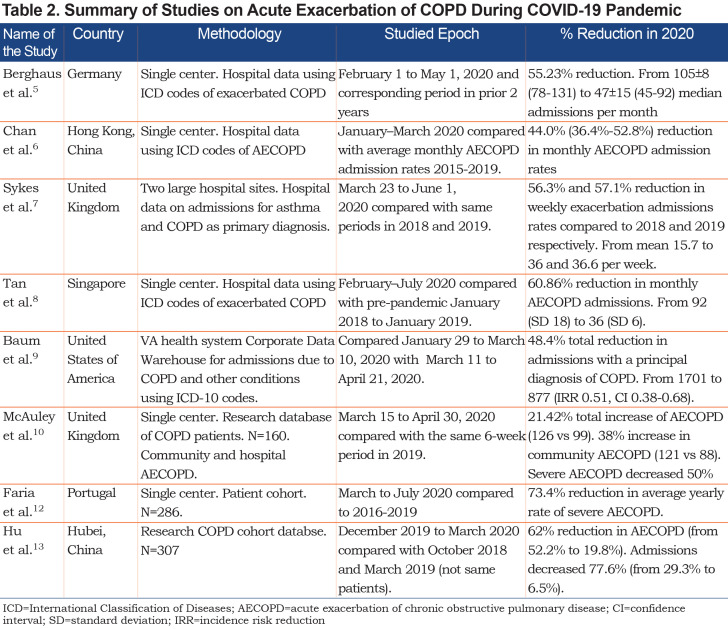
A similar phenomenon has been reported in individuals with COPD, a population more vulnerable to developing respiratory complications and health care utilization from SARS-CoV-2 infection.3,4 Using hospital admission data, a reduction in emergency department visits and admissions due to respiratory illnesses in individuals with COPD has been reported from institutions in Germany,5 Hong Kong,6 the United Kingdom,7 and Singapore.8 In the United States, Baum and Schwartz analyzed admissions for several conditions using a large Veterans Administration (VA) database and reported a 48% reduction in admissions related to COPD exacerbations.9 These reports, based on hospital data, include only severe exacerbations, ignoring events of lesser severity or exacerbations treated at home. By contrast, using a research COPD cohort in the United Kingdom, McAuley et al noted that despite a decrease in severe acute exacerbation of COPD (AECOPD), the total number of AECOPDs increased 21.4% due to a 38% increase in AECOPDs treated at home.10
Because of this latter report, we opted to study the incidence of AECOPD in a cohort of individuals with prior data where frequent exacerbators were well characterized before the pandemic. We also inquired about the measures these COPD individuals applied to protect themselves against COVID-19 infection and how these measures may have influenced the frequency of AECOPD.
Methods
The study was conducted on a single-center cohort of COPD patients at the Miami VA Medical Center being followed since 2017. For this analysis, we included 123 individuals with well characterized COPD who had a complete set of exacerbation data since 2017 and who were alive by January 1, 2020. COPD was defined as symptomatic individuals with a > 10 pack-year smoking history with airflow obstruction in spirometry. AECOPD events that occurred from January 1, 2017, to December 31, 2020, were recorded prospectively every 3 months at each research visit, by patient recall and review of each individual’s medical record including pharmacy records. AECOPD events were determined by the investigator’s assessment of symptoms (directly asking the patient details about the event) in conjunction with documentation of escalation of therapy recorded in the medical record. AECOPDs were defined as events of acute worsening of COPD symptoms requiring escalation of treatment with either antibiotics or steroids at home (mild), urgent physician visit including the emergency department (moderate), or hospitalization (severe).11 During 2020, follow-ups were done over the phone. An additional phone call survey was performed to inquire about the measures taken to avoid COVID-19 infection, assess their symptoms, and confirm the recorded AECOPD events. The study was approved by the Miami VA Medical Center’s Institutional Review Board.
Additional data was obtained from chart review including demographics, smoking history, complete lung function (forced expiratory volume in 1 second [FEV1], forced vital capacity [FVC], FEV1/FVC ratio, total lung capacity [TLC], residual volume [RV], diffusing capacity for carbon monoxide [DLCO]), COPD Assessment Test (CAT) score, modified Medical Research Council (mMRC) dyspnea scale, comorbidities (including heart disease, previous cardiothoracic surgery), medication use (inhaled and systemic steroid use in particular) and available laboratory data, and hospital admissions.
Data analysis was performed using SPSS version 27. Comparison between groups was performed using the paired t-test or signed-rank test for parametric data or nonparametric data, respectively for continuous variables, and the Chi-square test for categorical variables. Differences between rate of exacerbations by year was analyzed using a generalized linear model for repeated variables using multivariate analysis of variance.
Results
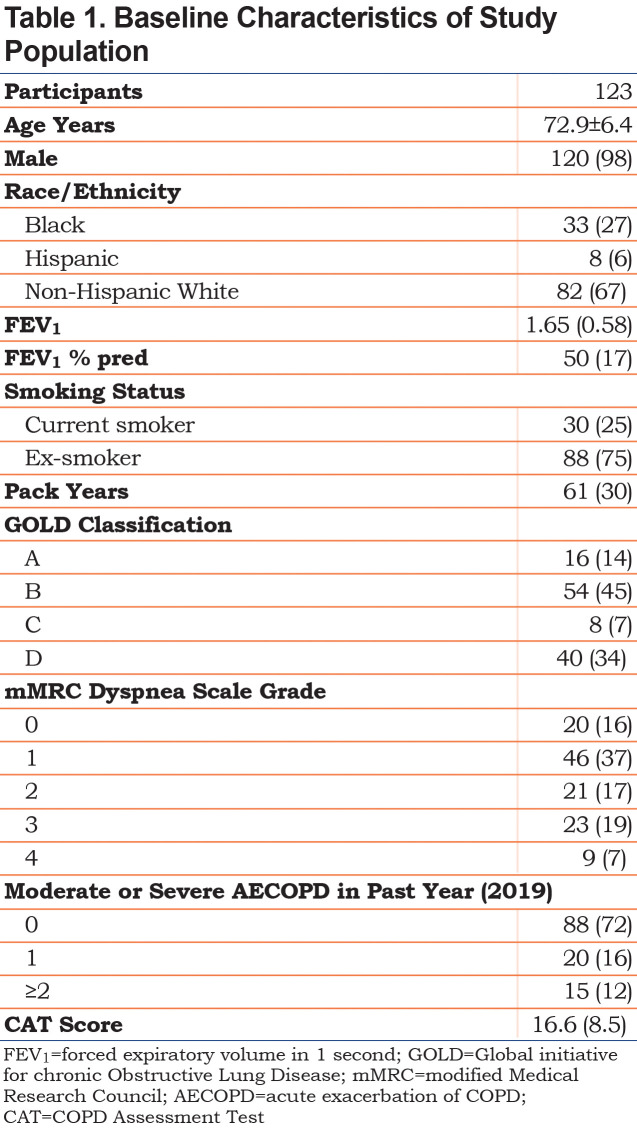
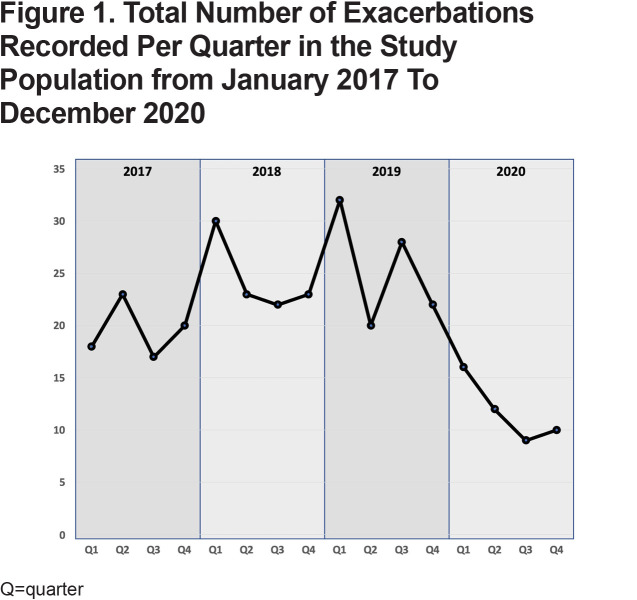
The clinical and demographic characteristics of the 123 individuals included is shown in Table 1. Most individuals had moderate disease with an average FEV1 50% predicted and Global initiative for chronic Obstructive Lung Disease (GOLD) group B. Sixteen individuals were frequent exacerbators (2 or more exacerbations in each of the prior 3 years). In comparison to each the previous 3 years, the cohort experienced significantly fewer AECOPDs in 2020. Figure 1 shows the total number of exacerbations recorded per quarter from 2017–2020. Overall, in 2020, 26 participants (21%) had any exacerbation compared to 46 (37%) in 2019, 52 (42%) in 2018, and 44 (36%) in 2017. This represents a reduction of 45% in the number of individuals who experienced an exacerbation compared with the prior 3-year average.
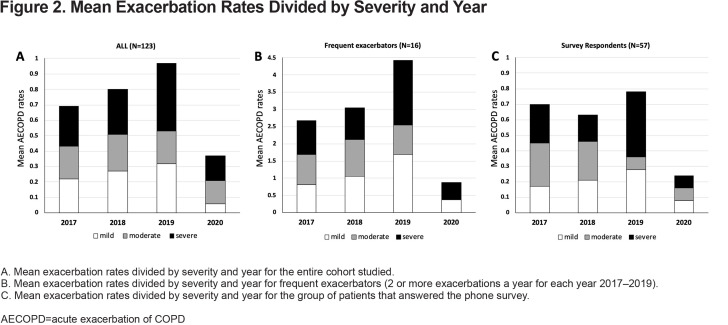
The mean number of AECOPDs per person was significantly lower in 2020 (mean 0.38; standard deviation [SD]=0.937) compared to 2019 (mean 0.98; SD=2.333), 2018 (mean 0.81; SD=1.295), and 2017 (mean 0.70; SD=1.248) (Wilks’ lambda=0.87, F=5.94, p<0.001). This represents a 54% reduction in mean exacerbation rate compared with the prior 3-year average. Figure 2A shows the rate of exacerbations in each study year categorized by severity. The mean number of mild exacerbations was significantly lower in 2020 (Wilks’ lambda=0.86, F=6.54, p<0.001), as were the mean number of severe exacerbations (Wilks’ lambda=0.90, F=4.47, p=0.005), while moderate exacerbations were not significantly different. The magnitude in AECOPD reduction (54% reduction in mean exacerbation rates and 45% reduction in the number of individuals who experienced an exacerbation) is comparable in magnitude to the reductions of 40%-60% observed in other locations worldwide using hospital data as summarized in Table 2.12,13
Individuals with frequent exacerbations prior to 2020 (≥2/year), also experienced a significant reduction in AECOPDs in 2020 (mean 0.88; SD=1.5) compared to 2019 (mean 4.44; SD=4.86), 2018 (mean 3.06; SD=1.95), and 2017 (mean 2.69; SD=1.96) (Wilks’ lambda=0.18, F=19.3, p<0.001). This represents a 74% reduction in mean exacerbation rate compared with the prior 3-year average. Figure 2B shows the rate of AECOPDs in each year categorized by severity in the frequent exacerbator group.
A subset of participants (N=57) was able to be contacted for this study to inquire about their attitudes towards the pandemic. This group did not differ from the entire cohort in age, lung function, or average exacerbation rates. They also experienced a significant reduction in AECOPD of 64% during year 2020 as shown in Figure 2C. The group reported a high rate of adherence to guidelines on preventing COVID-19 infection as shown in Figure 3. There were no significant differences in adherence to guidelines in patients who experienced an exacerbation in 2020 compared to those who did not. However, there was a higher rate of social distancing compliance in the group with a CAT score >10 in 2020 (97.8% versus 83.3%; χ2=3.96; p=0.046) and in those with an FEV1 below 50% predicted (100% versus 86.9%; χ2=4.68; p=0.030). Interest in getting vaccinated against COVID-19 was generally high (91.2%) but was significantly higher in the group with FEV1<50% (100% versus 78.3%; χ2=8.10; p=0.004) and in those who experienced an exacerbation in 2019 (100% versus 84.8%; χ2=3.99; p=0.046).
Discussion
We report here a marked decrease in AECOPDs and admissions during the COVID-19 pandemic in a cohort of patients that had been closely monitored for the preceding 3 years. As noted in Table 2, most reports focused on hospital data that mostly reflect severe events. In contrast, our study also included mild and moderate events. It differs from the results of a research cohort of COPD individuals in the United Kingdom in which the investigators noted an increase in total AECOPDs due to increased events treated in the community during the first 6 weeks of the pandemic.10 Our study is unique in that our follow-up included the entire year of 2020 covering 2 pandemic waves. It is important to highlight that the impact of the pandemic on AECOPD reduction was greater in the frequent exacerbator group.
The factor that most likely explains the decrease in AECOPDs is compliance with preventative measures to reduce viral transmission. Individuals with COPD may be intuitively aware of their increased vulnerability to develop severe COVID-19 disease and achieve high rates of compliance with social containment measures as noted in our cohort. Viruses, in particular rhinovirus, accounts for nearly 50% of all AECOPDs.14 Tan et al8 reported that despite increased viral testing during the pandemic, the proportion of individuals with exacerbations testing positive for respiratory viruses decreased from 49% to 11%. Also, influenza surveillance in the United States15 has shown that community mitigation measures to reduce SARS-CoV-2 caused a decrease in influenza positivity rates in respiratory specimens from >20% to 2.3%.
Using a log-linear model, Chan et al estimated that a 1% increase in masking usage was associated with 1% decrease in admissions for AECOPD.6 Social distancing was the measure most complied with in our cohort (95%), higher than a report of 79.9% compliance with shielding and less visitation during the pandemic in a United Kingdom cohort.10 Interestingly, we observed a trend that “healthier” individuals, those with COPD assessment test scores <10 and those with an FEV1 > 50%, tend to be less complaint with social distancing practices and other recommended protective measures. This is an alarming trend that should be addressed as these individuals remain at higher risk. Nevertheless, it is probable that community level compliance with lockdown policies is an important contributor to AECOPD reduction for individuals with lower personal compliance with COVID-19 preventive measures. In that line, it is possible that the slight increase in AECOPDs observed during the last quarter of 2020 (Figure 1) is related to the re-opening of businesses in Florida.
Another factor that may explain the marked decrease in AECOPD rates during the COVID-19 pandemic, although probably not the main factor in the geographical area of our study, is a significant decrease in airway pollution. New data has emerged that during the COVID-19 pandemic, particulate matter (PM2.5) and nitrogen dioxide (NO2) levels decreased as much as 25% in areas where non-essential business closure restrictions were instituted.16 The reduction in both NO2 and PM2.5 during the pandemic has been attributed to reducing more than 10,000 deaths in China, of which 65% are attributed to cardiovascular and pulmonary reasons including COPD.17
Because of the facts mentioned above, COPD is a condition largely underrepresented in cohorts of individuals infected by COVID-19, representing only 2% (95% CI, 1%-3%) among 2473 patients with COVID-19 infection in a meta-analysis of 15 studies.18 Strict social containment measures, such as washing hands frequently, wearing a face mask, avoiding crowds, and social distancing may have impacted the frequency of AECOPDs significantly but this, along with the fear of getting infected, can also affect individuals with COPD in a negative way. Studies are emerging on the impact on mental health, with increased levels of anxiety and depression7,10 and delays in proven effective interventions such as pulmonary rehabilitation.19 Hopefully, with the progress made in vaccination practices, rapid restoration to pre-pandemic routines will follow.
We believe that although our current study is restricted to a single center, our COPD population is comparable with those of other VA centers and COPD populations in general. In fact, the reduction in AECOPDs observed by us is similar in magnitude to an analysis of total VA AECOPD admission data.9 Other limitations of our study include not knowing the etiology of those exacerbations that occurred during the pandemic and the limited number of individuals studied including the small number of individuals interviewed. Since the study focuses on AECOPD rate changes with the COVID-19 pandemic, the study included only individuals with well-documented exacerbation rates over several years. Therefore, only cohort participants who were alive by January 2020 were included. It is possible that survival bias may have influenced exacerbation rates as we could have missed some AECOPD events that led to deaths in 2020. Nevertheless, we believe our findings are solid as these include strengths such as individual pre- and post-pandemic data with a diligent account for all exacerbations including those treated in a non-hospital setting.
Despite its disastrous effects, the pandemic has taught humanity several important lessons. It is well recognized that AECOPDs have a profound impact on lung function decline, mortality, and health-related quality of life in affected individuals. The marked decrease in AECOPDs observed during the COVID-19 pandemic is impressive and of a much greater magnitude than our current preventive measures. Although it is impossible to tease out how much of the reduction was from reduced transmissibility of viral infections over the effects of decreased pollution, simple interventions such as increased hygiene appear to be cost-efficient to institute. Other measures such as universal masking, proven to be safe in COPD individuals,20 and enforcement of voluntary social distancing for those with acute viral illnesses in a post pandemic era need to be studied in terms of balancing their potential negative effects on mental health and mobility.
Abbreviations
Abbreviations: acute exacerbations of COPD, AECOPD; coronavirus disease 2019, COVID-19; severe acute respiratory syndrome coronavirus-2, SARS-CoV-2; Veterans Administration, VA; forced expiratory volume in 1 second, FEV1; forced vital capacity, FVC; total lung capacity, TLC; residual volume, RV; diffusing capacity for carbon monoxide, DLCO; COPD Assessment Test, CAT; modified Medical Research Council, mMRC; Global initiative for chronic Obstructive Lung Disease, GOLD; standard deviation, SD; International Classification of Diseases, ICD; incidence risk reduction, IRR
Funding Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Kansagra AP,Goyal MS,Hamilton S,Albers GW.Collateral effect of COVID-19 on stroke evaluation in the United States. N Engl J Med. 2020;383(4):400-401. doi: https://doi.org/10.1056/NEJMc2014816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Filippo O,D'Ascenzo F,Angelini F,et al. Reduced rate of hospital admissions for ACS during COVID-19 outbreak in northern Italy. N Engl J Med. 2020;383(1):88-89. doi: https://doi.org/10.1056/NEJMc2009166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gerayeli FV,Milne S,Cheung C,et al. COPD and the risk of poor outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2021;33:100789.doi: https://doi.org/10.1016/j.eclinm.2021.100789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rabbani G,Shariful Islam SM,Rahman MA,et al. Pre-existing COPD is associated with an increased risk of mortality and severity in COVID-19: a rapid systematic review and meta-analysis. Expert Rev Respir Med. 2021;15(5):1-12. doi: https://doi.org/10.1080/17476348.2021.1866547 [DOI] [PubMed] [Google Scholar]
- 5.Berghaus TM,Karschnia P,Haberl S,Schwaiblmair M.Disproportionate decline in admissions for exacerbated COPD during the COVID-19 pandemic. Respir Med. 2020 Aug 14;In Press. doi: https://doi.org/10.1016/j.rmed.2020.106120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan KPF ,Ma TF,Kwok WC,et al. Significant reduction in hospital admissions for acute exacerbation of chronic obstructive pulmonary disease in Hong Kong during coronavirus disease 2019 pandemic. Respir Med. 2020;171:106085. doi: https://doi.org/10.1016/j.rmed.2020.106085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sykes DL,Faruqi S,Holdsworth L,Crooks MG. Impact of COVID-19 on COPD and asthma admissions, and the pandemic from a patient's perspective. ERJ Open Res. 2021;7(1). doi: https://doi.org/10.1183/23120541.00822-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tan JY,Conceicao EP,Wee LE,Sim XYJ ,Venkatachalam I.COVID-19 public health measures: a reduction in hospital admissions for COPD exacerbations. Thorax. 2020;76(5):512-513.doi: https://doi.org/10.1136/thoraxjnl-2020-216083 [DOI] [PubMed] [Google Scholar]
- 9.Baum A,Schwartz MD. Admissions to Veterans Affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020;324(1):96-99. doi: https://doi.org/10.1001/jama.2020.9972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McAuley H,Hadley K,Elneima O,et al. COPD in the time of COVID-19: an analysis of acute exacerbations and reported behavioural changes in patients with COPD. ERJ Open Res. 2021;7(1). doi: https://doi.org/10.1183/23120541.00718-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rodriguez-Roisin R.Toward a consensus definition for COPD exacerbations*. Chest. 2000;117(5 Suppl 2):398S-401S. doi: https://doi.org/10.1378/chest.117.5_suppl_2.398S [DOI] [PubMed] [Google Scholar]
- 12. Faria N,Costa MI,Gomes J,Sucena M.Reduction of severe exacerbations of COPD during COVID-19 pandemic in Portugal: a protective role of face masks? COPD. 2021;18(2):1-9.doi: https://doi.org/10.1080/15412555.2021.1904387 [DOI] [PubMed] [Google Scholar]
- 13. Hu W,Dong M,Xiong M,et al. Clinical courses and outcomes of patients with chronic obstructive pulmonary disease during the COVID-19 epidemic in Hubei, China. Int J Chron Obstruct Pulmon Dis. 2020;15:2237-2248.doi: https://doi.org/10.2147/COPD.S265004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dimopoulos G,Tsiodras S,Lerikou M,et al. Viral Profile of COPD exacerbations according to patients. Open Respir Med J. 2015;9:1-8. doi: https://doi.org/10.2174/1874306401509010001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Olsen SJ,Azziz-Baumgartner E,Budd AP,et al. Decreased influenza activity during the COVID-19 pandemic-United States, Australia, Chile, and South Africa, 2020. Am J Transplant. 2020;20(12):3681-3685. doi: https://doi.org/10.1111/ajt.16381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Berman JD,Ebisu K.Changes in U.S. air pollution during the COVID-19 pandemic. Sci Total Environ. 2020;739:139864. doi: https://doi.org/10.1016/j.scitotenv.2020.139864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chen K,Wang M,Huang C,Kinney PL,Anastas PT. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health. 2020;4(6):e210-e212. doi: https://doi.org/10.1016/S2542-5196(20)30107-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Alqahtani JS,Oyelade T,Aldhahir AM,et al. Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: a rapid systematic review and meta-analysis. PloS One. 2020;15(5):e0233147.doi: https://doi.org/10.1371/journal.pone.0233147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tsutsui M,Gerayeli F,Sin DD. Pulmonary rehabilitation in a post-COVID-19 world: telerehabilitation as a new standard in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2021;16:379-391.doi: https://doi.org/10.2147/COPD.S263031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Samannan R,Holt G,Calderon-Candelario R,Mirsaeidi M,Campos M. Effect of face masks on gas exchange in healthy persons and patients with chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2021;18(3):541-544.doi: https://doi.org/10.1513/AnnalsATS.202007-812RL [DOI] [PMC free article] [PubMed] [Google Scholar]