Abstract
Sturge–Weber syndrome (SWS) is a neurocutaneous syndrome characterized by capillary venous malformations in the skin, eye, and brain with the occurrence of angiomas of the face, choroid, and leptomeninges. The characteristics signs include facial port-wine birth mark, glaucoma, choroidal hemangioma with brain malformations, and cognitive abnormalities. In this article, we have documented the case report of a 24-year-old male with SWS presenting with glaucoma.
KEYWORDS: Glaucoma, neurocutaneous syndrome, Sturge–Weber syndrome
INTRODUCTION
Sturge–Weber syndrome (SWS) is a neurocutaneous syndrome characterized by capillary venous malformations in the skin, eye, and brain with the occurrence of angiomas of the face, choroid, and leptomeninges. The characteristics signs include facial port-wine birth mark, glaucoma, choroidal hemangioma with brain malformations, and cognitive abnormalities. It is the third most common neurocutaneous syndrome, predominantly occurring in the regions supplied by the trigeminal nerve, especially its ophthalmic and maxillary divisions, and to some extent the mandibular division. The SWS is also known as the also known as “port-wine stain” or “nevus flammeus” or encephalotrigeminal angiomatosis. In many cases, the clinical outcome can be as severe as frequent strokes, tonic or myoclonic seizures and glaucoma. In this article, we have documented the case report of a 24-year-old male with SWS presenting with glaucoma.
CASE REPORT
A 24-year-old male presented to the hospital with complaints of right eye defective vision for the past 3 months. He gives a history of gradual progressive painless loss of vision. History of redness of both eyes was present since childhood. There is no history of ocular trauma, ocular medication, and surgery. There was no history of any systemic illness, no history of drug intake, and no significant family history.
On examination, pink well-defined patches seen on the forehead and temporozygomatic part of the face on both sides were seen. There was no facial asymmetry or significant head posture, corneal reflex was central, and the cover test was orthophoric. Best-corrected visual acuity was RE 6/24, LE 6/6.
Scleral AV malformation was evident and on performing gonioscopy, both eyes showed open angles with increased pigmentation were observed.
Glaucomatous atrophy of the disc, normal vessels, and foveal reflex in the macula observed during fundus examination of the right eye. The visual field analysis was done Figures 3 and 4. Disc with 0.9 cupping and bipolar notch, normal vessels, and macula with foveal reflex were observed on the fundus examination of the left eye.
Figure 3.
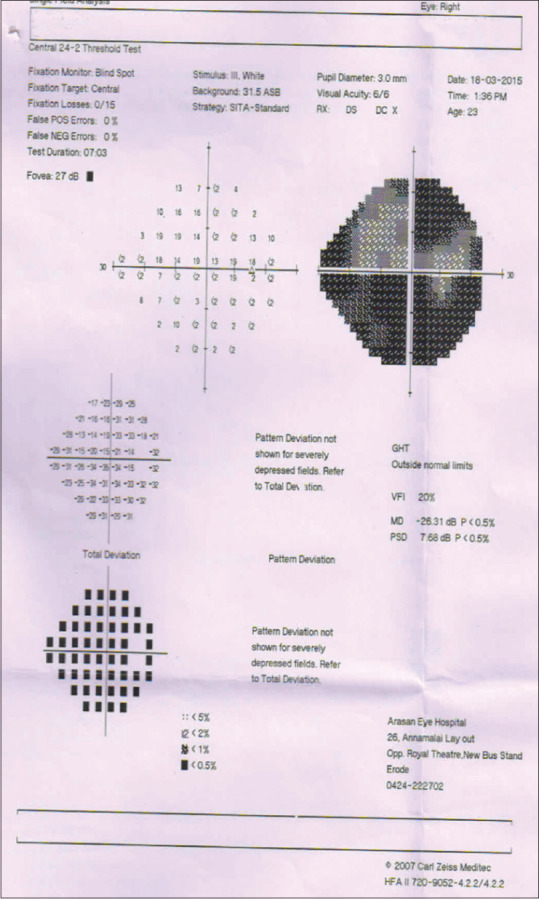
RE: Advanced glaucomatous visual field changes seen in 24-2
Figure 4.
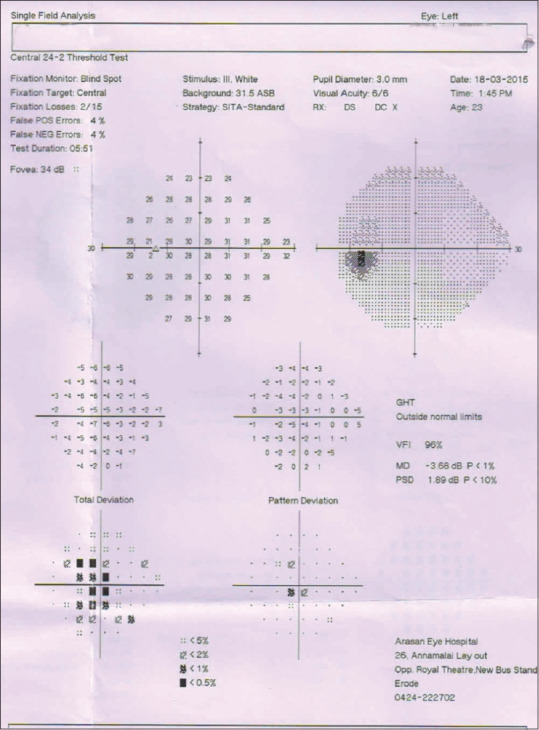
LE small central scotoma seen
With the above clinical findings, we arrived at a diagnosis of glaucoma associated with SWS involving v1 and v2 dermatome. MRI of the brain was taken to rule out intracranial hemangiomas. The patient was started on antiglaucoma medication and advised follow-up.
DISCUSSION
SWS (encepahalotrigeminalangiomatosis) belong to group of disorders known as phakomatoses. Developmental defect in the 1st month of gestation – persistence of vascular plexus around the cephalic portion of neural tube, which is caused by the defect in GNAQ gene located on chromosome 9 is the genetic cause of the disease. The skin manifestations show 20% facial involvement, especially of the forehead and upper lid (v1). Concomitant involvement of maxillary (v2) and mandibular branch (v3) involvement occurs in 2%–23% of patients.
In addition, orally, it gets manifested as, oral mucosal hemangioma, bone overgrowth, tooth maleruption, macroglossia, and hypertrophy of maxillary bone. The neurological manifestations include the seizures, transient stroke, behavioral problems, hemiplegia, and heminopsia.
Ocular manifestations include glaucoma, choroidal hemangioma, episcleral vessel dilatation, iris heterochromia, optic disc coloboma, and cataract [Figure 1]. Developmental anomalies of anterior chamber angle with elevated episcleral venous pressure and with gonoscopy showing increased pigmentation of trabecular meshwork [Table 1].
Figure 1.
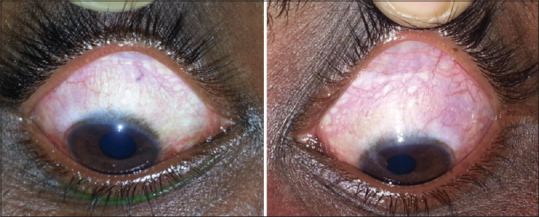
Episceleral vessels dilated
Table 1.
Ocular examination
| Slit lamp examination | Right eye | Left eye |
|---|---|---|
| Lids | Pink patches (v1 dermatome) | Pink patches (v1 dermatome) |
| Conjunctiva | Episcleral vessel dilatation | Episcleral vessel dilatation |
| Cornea | clear | Clear |
| Anterior chamber | Normal depth and quiet | Normal depth and quiet |
| Iris | Normal in colour and pattern | Normal in colour and pattern |
| Pupil | RAPD | Reacting to light (direct) |
| Lens | Clear | Clear |
| Gonioscopy | Open | Open |
| Intraocular pressure | 40 mmHg | 28 mmHg |
RAPD: Relative afferent pupil defect
Roach scale classification classifies SWS as:
Type 1: (involving v1 dermatome) – Facial and leptomeningeal angiomas and glaucoma
Type 2: (involving v2 dermatome) – Facial angioma, glaucoma Tab. Zerodol
Type 3: (involving v3 dermatome) – Isolated leptomeningeal angioma and absence of glaucoma.
Investigation includes magnetic resonance imaging without contrast showing cerebral atrophy both in T1- and T2-weighted sequences, diploic prominence and enlarged choroid plexus. Calcifications can be seen in T2-weighted, especially, in gradient-echo images, as areas of low signal [Figure 2]. Accelerated myelination may produce the areas of hypointensity in T2-weighted. Hyperintensity on T2-weighted representing areas of gliosis may also be seen.
Figure 2.
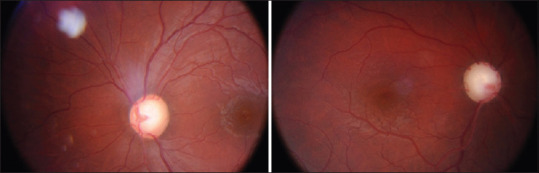
Fundus
Management
Medical therapy involves the administration of antiglaucoma drugs to control intraocular pressure (IOP). Surgical treatment involves procedures such as trabeculectomy and application of glaucoma drainage devices. The chances of failure of trabeculectomy are more, so glaucoma drainage devices are better in the management of glaucoma associated with SWS. The complications of surgical management include the expulsive hemorrhage and intraoperative choroidal effusion.
Hamush et al.[1] in their study of 11 eyes implanted with Ahmed valve in childhood glaucoma associated with SWS reported success rate of 79% at 2 years and came down to 30% after 5 years follow-up. Kaushik et al.[2] reported that the primary Ahmed valve implantation provided a safe and effective option in the management of childhood glaucoma with SWS.
According to Day et al.,[3] the children with worst prognostic factors with SWS brain and skin involvement should be managed to prevent seizures and stroke. According to Comi,[4] continued safe screening methods should be utilized to detect presymptomatic brain and eye involvement. In the study by Zhao,[5] the optical coherence tomography angiography (OCTA) images demonstrated severe dilated dense vessels in limbal epi-sclera in SWS patients.
Early prophylactic interventions such as posterior sclerotomy, radiotherapy or laser photocoagulation of choroidal hemangioma, and electro cautery of anterior episcleral vascular malformation can avoid complications during intraocular surgery.
According to Porsia and Nicoletti[6] a case of 4-month-old healthy infant treated with 360° ab internotrabeculotomy for congenital glaucoma produced low IOP without the need for medications.
CONCLUSION
Thus, the OCTA evaluation of epi-scleral vasculature can be used for the investigation of vascular glaucoma and provides quantitative measurement of vascular anomalies. This OCTA technique is noninvasive, more precise, and reliable to conventional slit-lamp examination.
Omni surgical system (combined vasodilation of Schlemm's canal and collector channels and 360° AB internotrabeculotomy) is more efficient in treating congenital glaucoma (sws) than anti-glaucoma medications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardian has given his consent for images and other clinical information to be reported in the journal. The guardian understands that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hamush NG, Coleman AL, Wilson MR. Ahmed glaucoma valve implant for management of glaucoma in Sturge-Weber syndrome. Am J Ophthalmol. 1999;128:758–60. doi: 10.1016/s0002-9394(99)00259-7. [DOI] [PubMed] [Google Scholar]
- 2.Kaushik J, Parihar JKS, Jain VK, Mathur V. Ahmed valve implantation in childhood glaucoma associated with Sturge-Weber syndrome: Our experience. Eye (Lond) 2019;33:464–8. doi: 10.1038/s41433-018-0233-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Day AM, McCulloch CE, Hammill AM, Juhász C, Lo WD, Pinto AL, et al. Physical and family history variables associated with neurological and cognitive development in Sturge-Weber Syndrome. Pediatr Neurol. 2019;96:30–6. doi: 10.1016/j.pediatrneurol.2018.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Comi A. Current therapeutic options in Sturge-Weber Syndrome. Semin Pediatr Neurol. 2015;22:295–301. doi: 10.1016/j.spen.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhao Z, Xu L, Ding X, Wu Y, Zhu X, Fu Y, et al. Optical coherence tomography angiography of perilimbal vasculature in port-wine stain and Sturge-Weber syndrome patients. Invest Ophthalmol Vis Sci. 2020;61:43. doi: 10.1167/iovs.61.4.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Porsia L, Nicoletti M. Combined viscodilation of Schlemm's canal and collector channels and 360° ab-interno trabeculotomy for congenital glaucoma associated with Sturge-Weber syndrome. Int Med Case Rep J. 2020;13:217–20. doi: 10.2147/IMCRJ.S252725. [DOI] [PMC free article] [PubMed] [Google Scholar]


