Abstract
The giant cell granuloma is an identical reactive lesion which is mostly progressive in nature. The clinical behavior of these lesions varies from indolent to aggressive variant. The central form of giant cell granuloma involves the craniofacial bone, followed by long bones of hands and feet. These lesions are usually asymptomatic lesions and are discovered incidentally during routine radiographic examination. Radiograph features reveal multilocular jaw lesions, generally anterior to the first molar regions. Histologically, the lesion shows proliferating spindle-shaped stromal cells in a fibrovascular connective tissue stroma, which characteristically contains multiple multinucleated giant cells. Hemorrhage and hemosiderin pigmentations are often seen in tumor. Central giant cell granuloma is often confused with giant cell tumor of bone histologically. Here, we report a young male who was found to have large central giant cell granuloma in the anterior part of the mandible. The surgical treatment approach of central giant cell granuloma is discussed in this article.
KEYWORDS: Giant cells and peripheral ostectomy, osteolytic lesion, progressive
INTRODUCTION
Central giant cell granuloma is an intraosseous destructive giant cell lesion, which often affects the anterior part of the lower jawbone. The exact etiopathogenesis of central giant cell granuloma is unknown, but causes have been suggested by different investigators which are developed as a reparative process in response to the intrabony hemorrhage/inflammation or a truly neoplastic condition. This lesion usually occurs among young adults below the age of 30 with female predilection. Most of the lesions develop in the tooth-bearing areas of the jaw and may even cross the midline of the mandibular bone. Clinically, all are initially asymptomatic, but a proportion becomes expansile. On rare occasions, more than one lesion of central giant cell granuloma may develop simultaneously in the jaw. Radiographically, the lesions reported various sizes from 5 mm to 10 cm in diameter. Histologically, central giant cell granuloma exhibits multiple multinucleated giant cells of varying size which are dispersed throughout the fibrous tissue stroma, where numerous small blood capillaries are also found. Several areas of hemorrhage and hemosiderin pigmentation are also evident. Giant cells are often found around the blood capillaries or near the areas of hemorrhage. The stromal cells are plump and spindle shaped, and these cells often exhibit frequent mitosis. In the differential diagnosis of central giant cell granuloma should be included brown tumor of hyperparathyroidism, giant cell tumor of bone, ameloblastoma, aneurysmal bone cyst, and cherubism.[1] Medical treatments such as calcitonin, denosumab, and intralesional steroid injection are used for large lesions which are reported to be effective.[2,3] Lesions approached with wide access thorough curettage rarely recur.[4]
CASE REPORT
A 19 years old male patient reported a history of painless progressive enlargement over 8 months in the anterior tooth region of the mandible. Extra oral examination revealed facial asymmetry, not associated with pain and occlusion disturbance. The patient had no history of trauma. Intraoral examination shows a large lingual swelling in the region of lower right first premolar to left second premolar region of the mandible. The swelling was in labio-buccal aspect extending from 31 to 35area obliterating the vestibule [Figure 1a and b]. 32 and 33 number teeth had a Grade II mobility. Orthopantomogram showed a multilocular radiolucency extending from 44 to mesial aspect of 34 [Figure 1c]. Two- and three-dimensional computerized tomography revealed osteolytic and erosive lesions on the left side of the mandible with adjacent soft-tissue component [Figure 1d and e]. Laboratory investigations of serum calcium, phosphorus, parathyroid hormone, and alkaline phosphatase were within normal limits, ruling out cherubism and brown tumors of hyperparathyroidism. Surgery was performed under general anesthesia. Intraoral crevicular incision was done. Bilateral releasing incision was done. Mucoperiosteal flap was reflected that a reciprocating saw is used to cut the cortical bone around the lesion approximately 0.5 cm from its margin. The lesion is reflected in toto with the associated tissues removed. The cavity is saucerized by reducing the height of its osseous wall [Figure 1f and 1g]. Subsequently, peripheral ostectomy is performed and layered closure was done. Histopathological and immunostain of CD68 findings are in favor of central giant cell granuloma [Figure 1h]. The patient has been on regular follow-up [Figure 2] and no sign of recurrence.
Figure 1.
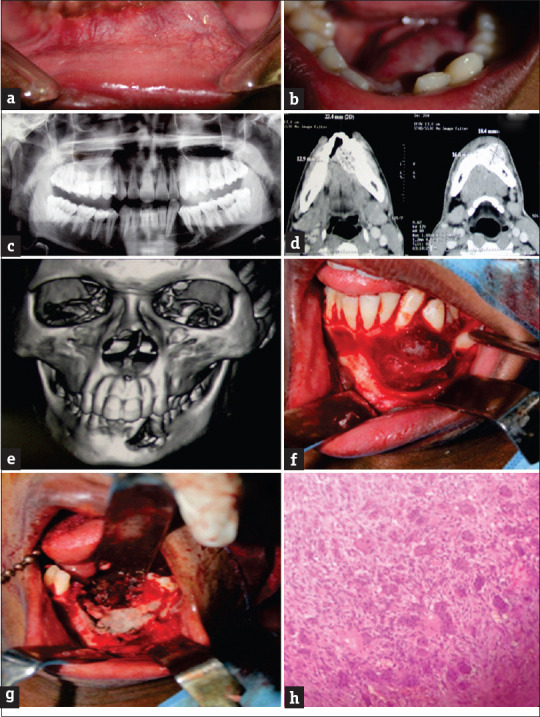
(a and b) Intraoral pictures show swelling with vestibular obliteration. Orthopantomography(c) and Three-dimensional computed tomography scan (d &e) revealed an osteolytic lesion in the anterior mandible. Intraoperative aspect of the surgical site, showing the boundaries of the resection of the lesion (f &g.) H&E staining ×40 shows the presence of Multinucleated giant cell. (h)
Figure 2.

Postoperative follow-up
DISCUSSION
According to the WHO, central giant cell granuloma is defined as a localized benign but sometimes aggressive osteolytic proliferation consisting of fibrous tissue with hemorrhage and hemosiderin deposits, presence of osteoclast-like giant cells, and reactive bone formation. The central giant cell granuloma is more common in a female patient in the 2nd decades of life and more frequently occurs in the anterior to the first permanent molar of the mandible.[1] Clinically, the lesion produces a fast enlarging, large, painful swelling in the jaw, with anesthesia or paresthesia in the region and displacement or mobility of the regional teeth due to expansion and distortion/perforation of both buccal and lingual cortical plates. Larger lesions cause loosening or displacement of teeth, divergence of roots, and root resorption, but the teeth in the affected region are always vital.[5,6] Radiographic appearances of large lesions appear multilocular but are unilocular with a lobular margin.[7] It is often difficult to differentiate between central giant cell granuloma and brown tumor of hyperparathyroidism on the basis of clinical, radiological, and histopathological features. For this reason, biochemical analysis of blood is always necessary. Normally, the raised serum calcium and serum alkaline phosphatase levels along with depressed serum phosphate levels confirm the diagnosis of hyperparathyroidism. However, in cases of central giant cell granuloma, the abovementioned biochemical changes in the blood are not observed.[8] The treatment of choice is surgical excision and thorough curettage with cryosurgery or peripheral ostectomy.[9] Bataineb et al. reported that clinical and histomorphometric features may be reliable indicators for the differentiation between aggressive and nonaggressive lesions. This should be accounted for to improve the individual planning of the treatment and follow-up.[10]
CONCLUSION
Our case report of central giant cell granuloma clinical, radiographic, and histopathological features is consistent with the literatures. This case report reemphasizes the surgical resection and peripheral ostectomy procedure, used in the success of large lesions of central giant cell granuloma in the mandible.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Barnes L, Eyeson J, Reichart P, Sjdransky D. Pathology and Genetics of Head and Neck Tumours. Lyon: IARC Press; 2005. [Google Scholar]
- 2.Bredell M, Rordorf T, Kroiss S, Rücker M, Zweifel DF, Rostetter C. Denosumab as a treatment alternative for central giant cell granuloma: A long-term retrospective cohort study. J Oral Maxillofac Surg. 2018;76:775–784. doi: 10.1016/j.joms.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 3.Carlos R, Sedano HO. Intralesional corticosteroids as an alternative treatment for central giant cell granuloma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:161–6. doi: 10.1067/moe.2002.119971. [DOI] [PubMed] [Google Scholar]
- 4.Daroit NB, De Marco RG, Sant’Anna Filho M, Fritscher GG. The challenge in the treatment of central giant cell granuloma – What is the best approach? J Oral Maxillofac Surg Med Pathol. 2017;29:122–8. [Google Scholar]
- 5.Buduru K, Podduturi SR, Vankudoth DS, Prakash J. Central giant cell granuloma: A case report and review. J Indian Acad Oral Med Radiol. 2017;29:145–8. [Google Scholar]
- 6.Kudva A, Cariappa K, Dhara V, Solomon M. Central giant cell granuloma: An uncommon presentation. Oral Maxillofac Surg Case. 2018;4:135–40. [Google Scholar]
- 7.Khanna JN, Ramaswami R, Shah M. Giant cell reparative granuloma of mandibular condyle – A case report. J Oral Maxillofac Surg Med Pathol. 2018;30:515–8. [Google Scholar]
- 8.Yadav S, Singh A, Kumar P, Tyagi S. Recurrent case of central giant cell granuloma with multiple soft tissue involvement. Natl J Maxillofac Surg. 2014;5:60–6. doi: 10.4103/0975-5950.140181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kruse-Lösler B, Diallo R, Gaertner C, Mischke KL, Joos U, Kleinheinz J. Central giant cell granuloma of the jaws: A clinical, radiologic, and histopathologic study of 26 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:346–54. doi: 10.1016/j.tripleo.2005.02.060. [DOI] [PubMed] [Google Scholar]
- 10.Bataineb AB, Khateeb TA, Rawashdeh MA. The surgical treatment of central giant cell granuloma of the mandible. J Oral Maxillofac Surg. 2002;60:756–61. doi: 10.1053/joms.2002.33241. [DOI] [PubMed] [Google Scholar]


