Background:
In 2010, this Journal published my comprehensive review of the literature on hypertrophic scars and keloids. In that article, I presented evidence-based algorithms for the prevention and treatment of these refractory pathologic scars. In the ensuing decade, substantial progress has been made in the field, including many new randomized controlled trials. To reflect this, I have updated my review.
Methods:
All studies were evaluated for methodologic quality. Baseline characteristics of patients were extracted along with the interventions and their outcomes. Systematic reviews, meta-analyses, and comprehensive reviews were included if available.
Results:
Risk factors that promote hypertrophic scar and keloid growth include local factors (tension on the wound/scar), systemic factors (e.g., hypertension), genetic factors (e.g., single-nucleotide polymorphisms), and lifestyle factors. Treatment of hypertrophic scars depends on scar contracture severity: if severe, surgery is the first choice. If not, conservative therapies are indicated. Keloid treatment depends on whether they are small and single or large and multiple. Small and single keloids can be treated radically by surgery with adjuvant therapy (e.g., radiotherapy) or multimodal conservative therapy. For large and multiple keloids, volume- and number-reducing surgery is a choice. Regardless of the treatment(s), patients should be followed up over the long term. Conservative therapies, including gel sheets, tape fixation, topical and injected external agents, oral agents, and makeup therapy, should be administered on a case-by-case basis.
Conclusions:
Randomized controlled trials on pathologic scar management have increased markedly over the past decade. Although these studies suffer from various limitations, they have greatly improved hypertrophic scar and keloid management. Future high-quality trials are likely to improve the current hypertrophic scar and keloid treatment algorithms further.
In 2010, this Journal published my review on hypertrophic scars and keloids and the treatment and prevention algorithms for these refractory scars.1 Since then, many randomized controlled trials on pathologic scar management and guidelines2–5 have been published. To reflect these considerable advancements, I have reprised my review and the algorithms (Figs. 1 and 2).
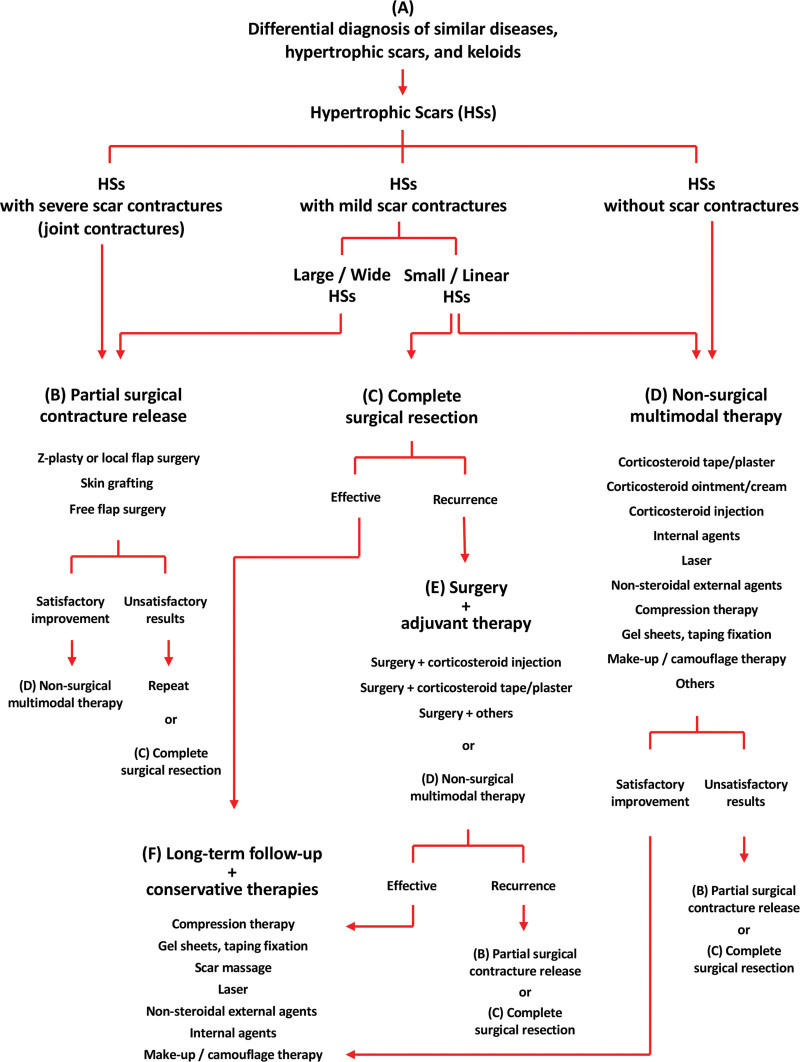
Fig. 1.
Treatment algorithm for hypertrophic scars (HSs). The scar should first be assessed for the degree of scar contracture. If the contracture is severe, surgery that releases the contracture is the first choice. If the contracture is mild, the scar can be resected completely; however, nonsurgical multimodal therapy is also a choice.
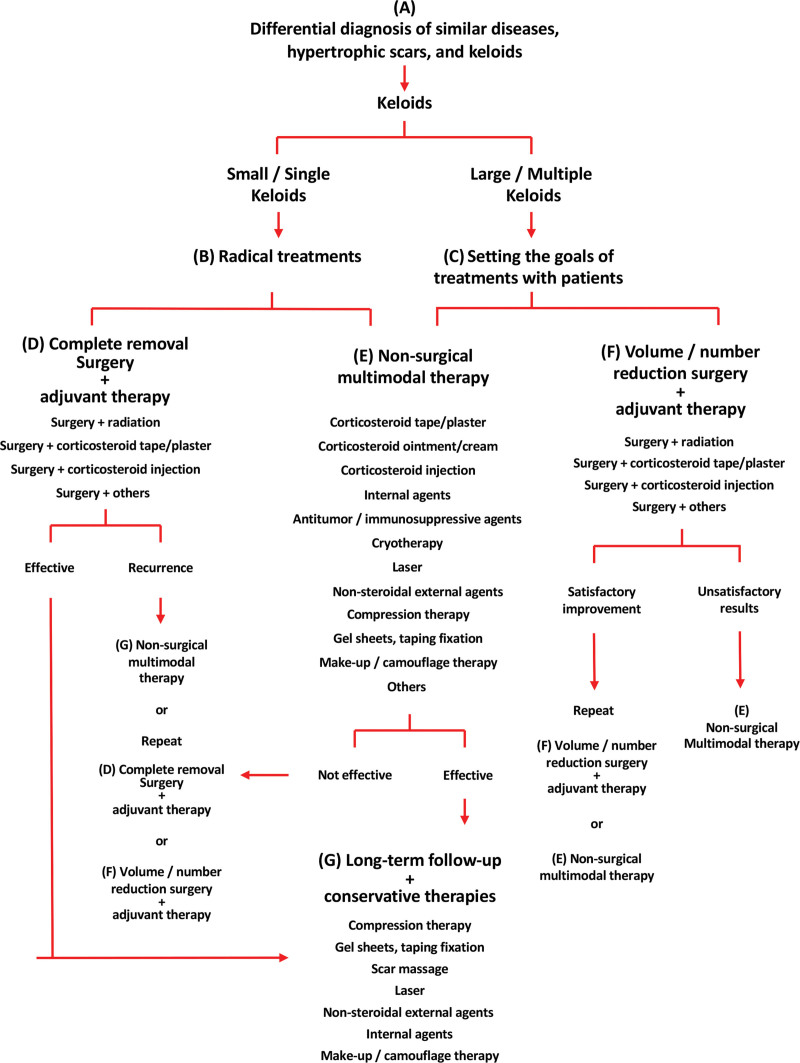
Fig. 2.
Treatment algorithm for keloids. The selected treatment method for keloids depends on whether the keloids are small and single or large and multiple. Small and single keloids can be treated radically by surgery with adjuvant therapy (including radiation therapy); alternatively, they could be treated with nonsurgical multimodal therapy. For large and multiple keloids, volume- and number-reduction surgery is a choice.
NEW DEVELOPMENTS IN THE PAST DECADE
The past decade has seen a remarkable growth in our understanding of how hypertrophic scars and keloids develop and progress. Consequently, hypertrophic scars and keloids are now known to be caused by chronic inflammation in the reticular dermis. Risk factors associated with hypertrophic scar and keloid development and aggravation have been identified, thereby aiding treatment optimization and effectiveness. Several major advancements in preventing and treating hypertrophic scars and keloids have been made, as follows. First, deprodone propionate (a stronger steroid) plaster was found to both prevent and treat hypertrophic scars and keloids very effectively. Second, surgical methods have been optimized for each body region, thereby improving cosmetic and functional outcome, safety, and recurrence rates. Third, the postoperative radiotherapy protocol has been fine-tuned, making it safer while remaining equally effective. The previous algorithm has been greatly improved by the inclusion of these modalities. I anticipate that further high-quality evidence for these modalities, and additional new modalities, will emerge in the next decade.
hypertrophic scar and keloid diagnosis
Differential Diagnosis
Hypertrophic scars and keloids are fibroproliferative disorders in the reticular dermis layer: this layer exhibits continuous inflammation,6 excessive angiogenesis, and abundant collagen accumulation. Compared to classic hypertrophic scars, classic keloids spread aggressively, rarely resolve spontaneously, and, at the histologic level, contain keloidal collagen, whereas hypertrophic scars only have nodules. However, many scars bear the clinical and pathologic features of both classic keloids and hypertrophic scars. This suggests that classic hypertrophic scars and keloids are polar manifestations of the same skin disorder, between which lies a spectrum of intermediate scars.
The clinical and histologic differences between classic hypertrophic scars and keloids probably reflect differences in the intensity and duration of reticular dermis inflammation. These differences in turn may reflect the presence and severity of local, systemic, genetic, and lifestyle risk factors.6,7
International Differences in Hypertrophic Scar and Keloid Diagnosis
Classic keloids are strongly driven by genetics.8–13 This partly explains ethnic differences in keloid susceptibility: keloids are common in Africans (5 to 10 percent are affected), less common in Asians (0.1 to 1 percent), and rare in Europeans/North Americans (<0.1 percent).14
These ethnic differences mean that physicians in certain regions have more experience with keloids than others. It is my impression, gained through attending many international scar conferences, that this can influence physician diagnoses. Thus, in Western countries, most abnormal scars are classic hypertrophic scars: consequently, Western physicians often diagnose scars as keloids if they exhibit minor spreading. However, African physicians see many patients with classic keloids: consequently, they often diagnose all scars as hypertrophic scars unless they grow rapidly. This should be taken into account when reviewing international literature.
Differential Diagnosis of Hypertrophic Scars and Keloids from Similarly Appearing Diseases
Hypertrophic scar and keloid diagnosis is often based on clinical features alone. However, malignant tumors such as dermatofibrosarcoma protuberans15–18 and giant-cell fibroblastoma19 can be misdiagnosed clinically as keloids.20 Moreover, analysis of 378 hypertrophic scars and keloids showed that 1.06 percent were other diseases.20 Thus, biopsy is warranted if malignancy is suspected.20–22
Prevention of postsurgical Hypertrophic scars and keloids
Patients with a hypertrophic scar and keloid history are at high risk, as are patients with one or more of the following risk factors (special care must be taken during and after surgery).
Risk Factors
Local
Hypertrophic scars and keloids occur frequently on sites that are frequently stretched by daily body movements, including the major joints, anterior chest, scapula, and lower abdomen.23 By contrast, hypertrophic scars and keloids occur rarely on the scalp and anterior lower leg, where stretching tension is low.23 This is because stretching a wound prolongs and worsens its inflammation, thereby provoking hypertrophic scar and keloid formation.24–26
To prevent hypertrophic scar and keloid formation after surgery on susceptible body regions, surgical techniques that limit dermal tension should be used, namely, flaps, Z-plasties, and subcutaneous and deep fascial tensile-reduction sutures. Moreover, postsurgical wound stretching should be limited by fixation materials such as paper tape, gel sheets, gels, or compression bandages and garments. All are supported by meta-analyses/randomized controlled trials. Regarding paper tape, a randomized controlled trial26 demonstrated that paper tape fixation reduced the hypertrophic scar risk after cesarean section by 13.6-fold. Regarding gel sheets, a meta-analysis on 20 trials27 concluded that silicone gel sheets may prevent hypertrophic scar and keloid formation in scar-prone people with newly healed wounds; however, they commented that trial quality was poor.27 A recent review on 10 trials had similar conclusions.28 Regarding gels, a randomized controlled trial29 showed that silicone gel reduces sternotomy scar pigmentation, erythema, hardness, height, and pain and itchiness. This was confirmed by a review.28 Regarding compression therapy, a meta-analysis of 12 trials confirmed that 15- to 25-mmHg compression therapy reduces burn scar thickness, erythema, and hardness.30
All patients undergoing surgery on susceptible body areas should be monitored closely for hypertrophic scars and keloids for 3 to 12 months. If induration is observed, steroid tape and plaster should be started and replaced with steroid injection if the induration prevails.
Systemic
Systemic factors include the female hormone estrogen31: a large cross-sectional study showed that keloids may predominate in women.32 Moreover, estrogen-induced vasodilation could worsen wound and scar inflammation: indeed, hypertrophic scars and keloids worsen during pregnancy33,34 and improve after delivery. Another systemic factor is hypertension, which may aggravate hypertrophic scars and keloids.35 Moreover, hypercytokinemic diseases (e.g., Castleman disease) can greatly worsen hypertrophic scars and keloids.36,37 Thus, surgery on pregnant, hypertensive, and hypercytokinemic patients should be conducted with the surgical and wound fixation techniques described above, followed by close monitoring.
Genetic
As mentioned, keloids are often strongly underpinned by genetic factors, including ethnic14 and familial genes: multiple cases of keloid-susceptible families have been reported.38,39 Moreover, several single-nucleotide polymorphisms associate with keloids40–42: four promote keloidogenesis40 and one associates with severe keloids.41
Several genetic diseases associate with keloidogenesis, including Rubinstein-Taybi syndrome43,44: a cross-sectional study44 reported that 24 percent of such patients had spontaneously growing keloids. Multiple hereditary exostoses also associate with keloidogenesis.45
These risk factors cannot be obviated. Thus, patients with familial history and genetic diseases should be treated carefully during and after surgery. The relatively low frequency of keloid-associated single-nucleotide polymorphisms means that testing for them is impractical.
Lifestyle
Several lifestyle factors could exacerbate surgery-induced wound and scar inflammation, including strenuous wound-stretching physical activity. Athletes and manual laborers should rest their wounds. Certain diets and hot baths could aggravate surgery-induced inflammation46: my experience with thousands of patients suggests they often experience itch and pain after consuming hot and spicy foods or taking hot baths.
Early detection and FIRST-LINE hypertrophic scar and keloid treatment
Hypertrophic scars and keloids should be detected early because they may respond well to conservative therapy. As discussed later, the first-line conservative therapy for hypertrophic scars and keloids in the 2019 Japanese guideline5 is long-term/continuous steroid tape or plaster application. Strong steroid (deprodone propionate) plaster effectively extinguishes early hypertrophic scars and keloids5,31,47,48 but is only available in Japan.47 Nevertheless, if applied very early and continuously, even weaker fludroxycortide tape can extinguish early hypertrophic scars and keloids.5
hypertrophic scar Treatment
Hypertrophic scars are detected several weeks after injury (Fig. 1). They grow for 3 to 6 months; if risk factors are minor, they then plateau and regress spontaneously. This process can be accelerated by the following conservative therapies, which reduce hypertrophic scar volume and suppress pain and itch. Hypertrophic scars rarely require surgery unless they contract and cause joint dysfunction49,50; in this case, reconstructive surgery is indicated.
Compression Therapy
A recent meta-analysis (12 randomized controlled trials) showed that 15- to 25-mmHg compression therapy improves burn and hypertrophic scar thickness, erythema, and hardness.30 Compression therapy may promote wound healing by means of local vasoconstriction that limits burn-induced inflammation.
Gel Sheets
Gel sheets are soft and self-adhesive. A meta-analysis (20 trials)27 reported that continuous gel sheeting improves hypertrophic scar maturation. A new meta-analysis51 on this question is currently underway: it will be of interest to learn their findings.
The type of material may not matter: a randomized controlled trial52 showed that silicone and hydrocolloid matrix gel sheets reduce hypertrophic scar dimensions equally well. More important may be patient education: a randomized controlled trial53 on burn and hypertrophic scar patients suggests that instructional handouts and videotapes increase gel sheet effectiveness. Computer analysis suggests that gel sheets may prevent hypertrophic scar formation and promote hypertrophic scar maturation by limiting wound and scar tension.54
Scar Massage
Randomized controlled trials on burn rehabilitation massage have conflicting results, and a meta-analysis of 10 randomized controlled trials concluded that the supporting evidence is weak.55 I advise caution regarding massage therapy. Wound healing associates with initial inflammation that normally slowly wanes. At this point, massage may promote mature scarring. However, in patients with risk factors, inflammation rises rather than subsides. Because massage stretches the scar, it could induce and worsen hypertrophic scars and keloids. Thus, scar massage in high-risk patients should be avoided.
Corticosteroid Injection
Recent meta-analyses of four to 14 trials,28,56,57 a network meta-analysis of 23 trials,58 a systematic review of 11 studies,59 comprehensive reviews,60,61 and several new randomized controlled trials62,63 show that intralesional corticosteroid can induce 50 to 100 percent regression of both hypertrophic scars and keloids. An international expert panel recommends triamcinolone acetonide at doses of 2.5 to 40 mg/site.64 The injections probably act by decreasing inflammatory cytokine production.65 However, disadvantages include injection-induced pain, systemic side effects (e.g., menstrual dysfunction, adrenocortical suppression,66 and cataracts and glaucoma), and local side effects (e.g., skin thinning and atrophy, steroid acne, capillary dilatation, and hypopigmentation).
Corticosteroid Tape and Plaster
Corticosteroid tape and plaster is a painless alternative to corticosteroid injections. When 60 hypertrophic scar and keloid patients were treated with fludroxycortide (weak steroid) tape, 20 percent of the 30 adults and 80 percent of the 30 children exhibited improved scar elevation and erythema and pruritus after 12 months. The strong pediatric response may reflect thinner skin. When the 24 nonresponsive adults were switched to deprodone propionate (stronger steroid) plaster, 70.8 percent demonstrated improved scar features after 6 months.47,67 Other observational studies and good clinical experiences with steroid tape and plaster have caused it to become a mainstay of scar-management protocols.31 Consequently, a Japanese guideline5 recently recommended that corticosteroid tape and plaster should be the first-line hypertrophic scar and keloid therapy. Figure 3 depicts a deprodone propionate plaster–treated hypertrophic scar. Tape and plaster should be used continuously as early as possible5 for at least 3 months. If unsuccessful, it should be replaced with stronger treatments.
Fig. 3.
Treatment of hypertrophic scars with deprodone propionate plaster. (Left) Pretreatment view. (Right) Three years after starting deprodone propionate plaster. A 50-year-old woman had several hypertrophic scars as a result of cesarean delivery. She was provided with deprodone propionate plaster and told to apply it 24 hours per day until further notice. She was instructed to peel it off while taking a bath and then reapply it. When the plaster lost its adhesiveness, it was replaced by a new plaster. After 6 months, the scar became soft. After 3 years, the scar became completely flat and its tone was close to that of the surrounding skin.
Corticosteroid Ointment and Cream
Randomized controlled trials on corticosteroid ointment and cream are lacking, but a case series study68 showed that triamcinolone acetonide injections of hypertrophic scar and keloid-excision sites combined with twice-daily 6-month corticosteroid ointment application yielded keloid and hypertrophic scar recurrence rates of 14.3 percent and 16.7 percent, respectively. These outcomes and good clinical experiences recently led several Japanese burn and scar societies5,69 to recommend corticosteroid ointment and cream materials for superficial dermal burns70 and hypertrophic scar prevention and treatment.5 However, since corticosteroid ointment and cream should be applied four times daily to generate steroid tape and plaster effects,67 patient education is necessary.
Laser
Two reviews70,71 and a meta-analysis72 showed that pulsed-dye laser significantly reduces hypertrophic scar erythema and pruritus73–77 because its wavelength (585 to 595 nm) reaches the hypertrophic scar angiogenic region: its heat reduces hypertrophic scar blood flow and therefore inflammation. Neodymium:yttrium-aluminum-garnet laser (532/1064 nm) has similar effects, as shown by a review,71 a meta-analysis,72 case-series studies,48,78 and a randomized controlled trial.79 Randomized controlled trials showed that nonablative/ablative carbon dioxide fractional lasers have no beneficial effects.80,81 Fully ablative laser therapy is not recommended for pathologic scars because of high recurrence.82,83
Surgery
When hypertrophic scars occur near or on a joint, their contraction can induce joint dysfunction. Such scar contractures should be released surgically. This also accelerates maturation of surrounding hypertrophic scars. Small and linear hypertrophic scars can be treated by complete resection. All hypertrophic scar operations should involve tension-releasing techniques,5 including Z-plasty,84 W-plasty,85 and local flaps.86–89 Figure 4 shows a Z-plasty–treated hypertrophic scar contracture.
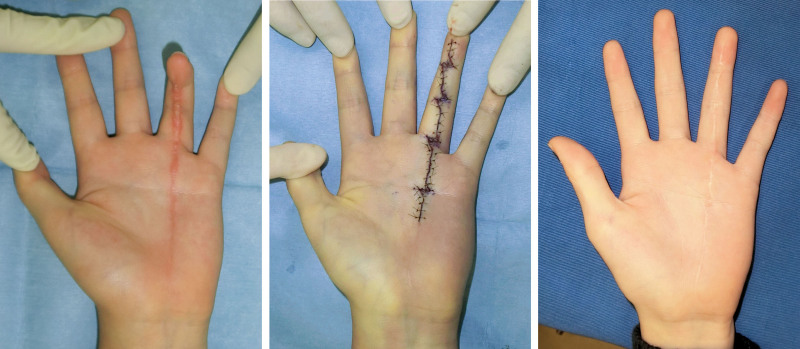
Fig. 4.
Treatment of a traumatic scar contracture between the finger and palm by using Z-plasty. (Left) Preoperative view. (Center) Immediately after surgery. (Right) Eighteen months after surgery. A 10-year-old boy sustained trauma to his left ring finger and palm. A hypertrophic scar with mild scar contracture developed. Because the width of the scar was narrow, the scar could be removed completely. Thereafter, Z-plasties were placed over the joints and the main crease in the palm. After surgery, the inflammation decreased uneventfully. The scar became mature over the next year.
One randomized controlled trial suggests that absorbable/nonabsorbable sutures do not differ in hypertrophic scar risk,90 but another91 showed that nonabsorbable sutures reduce hypertrophic scar frequency. The suturing method is probably more important than the material: clinical experience92 suggests that tensile-reduction sutures reduce hypertrophic scar and keloid scarring and recurrence because they decrease dermal tension.6,92,93
Other Hypertrophic Scar Therapies
Other therapies have been proposed for hypertrophic scars. Some may also be suitable for keloids. The evidence level is generally low. One is adipose tissue transplantation by using lipotransfer and lipoinjection techniques. A recent review94 noted that adipose-derived stem cells can secrete trophic factors that alter fibrotic and remodeling mediator expression. The evidence is too limited to justify changes in clinical practice. A recent review95 of case series studies showed that cryotherapy is safe and achieves good scar reduction, albeit with some adverse effects (depigmentation, recurrence, pain).
Recent meta-analyses and reviews28 show that 5-fluorouracil injections are effective as a monotherapy but reduce hypertrophic scar and keloid elevation and erythema better when combined with triamcinolone acetonide injections. Intralesional botulinum toxin type A (Botox; Allergan, Inc., Dublin, Ireland) injections may improve and prevent hypertrophic scars and keloids by suppressing scar tension and fibroblast activities.96 Recent randomized controlled trials97,98 show that postsurgical Botox injections prevent hypertrophic scar development. A meta-analysis of 14 studies57 showed that, compared to placebo, Botox injections significantly improved hypertrophic scar and keloid appearance and width.
A meta-analysis99 of five trials showed that bleomycin injections improved hypertrophic scars and keloids more effectively than triamcinolone acetonide and/or 5-fluorouracil injections. A 14-study review on topical onion extract gel (a nonsteroidal antiinflammatory drug) reported that 11 detected beneficial effects on hypertrophic scars and keloids.100
Oral tranilast (an antiallergic drug) improves inflammatory diseases with few adverse effects. It has long been used in Japan to treat hypertrophic scars and keloids.5,101–103 Randomized controlled trials showed that tranilast improved hypertrophic scars and keloids and reduced the redness of new postsurgical hypertrophic scars.104
keloid Treatment
Keloid treatment starts with determining the keloid number and size (Fig. 2): this indicates the strength of the patient’s keloid risk factors.1 If there is one keloid or the keloids are small, skin tension is probably the cause. However, if there are multiple or large keloids, genetic and systemic factors should be considered, especially when keloids are on different body regions. Single or small keloids can be treated with conservative therapy. Thick, large, multiple keloids should be assessed for surgery plus adjuvant therapy because they respond poorly to topical drugs. Physicians must carefully discuss therapeutic options with the patient and establish treatment goals.
Keloid inflammation generally worsens over time. Because scar massage, ablative lasers, and surgical monotherapy provoke inflammation and worsen keloids, they should be avoided.
Gel Sheets
The meta-analysis of O’Brien and Jones27 showed that silicone gel sheets alone can reduce keloid thickness and erythema.
Corticosteroid Injection
Many studies show that intralesional corticosteroid injections induce keloid regression.58–63 However, combining corticosteroid injections with 5-fluorouracil, pulsed-dye laster, or cryotherapy has better outcomes than corticosteroid injections alone.70
Corticosteroid Tape and Plaster
As with hypertrophic scars, corticosteroid tape and plaster is the first-line keloid therapy in the 2019 Japanese guideline.5 Its long-term, continuous application softens and then flattens the mass. It also reduces pruritus and erythema.47,67 Figure 5 shows a steroid plaster–treated keloid. However, in my experience, rapidly growing keloids cannot be stopped by steroid tape and plaster alone, and this therapy must be combined with triamcinolone acetonide injections or other methods. The greatest advantages of steroid tape and plaster are its painlessness and few side effects. Strong steroid (deprodone propionate) plaster, which is available only in Japan, is more effective than fludroxycortide tape. It should become available worldwide for treating pathologic scars.
Fig. 5.
Treatment of keloids using deprodone propionate plaster. (Left) Pretreatment view. (Right) Three years after starting deprodone propionate plaster. A 40-year-old woman developed a keloid on her left shoulder as a result of folliculitis. She was treated with deprodone propionate plaster for 24 hours/day. The patient changed the tape every day and continued to use it for 3 years. Six months after starting this therapy, the scar became soft. In the ensuing 3 years, the scar became almost flat.
Corticosteroid Ointment and Cream
Case series studies showed that multiple daily corticosteroid cream applications had excellent to good effects on existing keloids105 and reduced recurrence to 14.3 percent when applied postoperatively.68 However, a limitation is that the cream is easily rubbed off.
Cryotherapy
Recent reviews56,106 showed that cryotherapy (monotherapy or with triamcinolone acetonide injection) effectively reduces keloid size. Cryotherapy methods include direct contact,107 sprays,107–109 and intralesional needles. 109,110 However, supporting evidence is limited to case series studies.106
Antitumor and Immunosuppressive Agents
Recent meta-analyses, reviews, and new randomized controlled trials58–60 show that intralesional 5-fluorouracil injection is an effective keloid monotherapy and reduces postoperative recurrence.58–60 They also show that 5-fluorouracil effectively reduces keloid elevation and erythema when combined with triamcinolone acetonide injections.58–60 A meta-analysis99 reported that bleomycin injections improve keloids more effectively than triamcinolone acetonide and/or 5-fluorouracil injections.
Surgery
Small keloids can be radically resected. Large and multiple keloids may be suitable for partial and core excision that reduces the thick, hard areas or the number of keloids. Radical resection should always be combined with adjuvant therapies (e.g., radiation therapy) because surgery alone results in 45 to 100 percent recurrence rates.64 Surgery should involve tension-reducing techniques, namely, subcutaneous and deep fascial tensile-reduction sutures,31,92,93 Z-plasties,111–113 and local-flap transfer.114
Tensile-reduction sutures elevate the wound edges smoothly and relieve dermal tension.31,92,93 Our clinical experience112 suggests that they help reduce recurrence rates.
Regarding Z-plasty, case series studies of anterior chest wall keloids111 and upper-arm keloids113 showed that excision, tension-reduction suturing, Z-plasty, and radiotherapy led to respective recurrence rates of 10.6 and 5.3 percent, at 24 months. All recurrences were readily extinguished by steroid plaster and injections. Figure 6 depicts a Z-plasty–treated chest wall acne keloid.
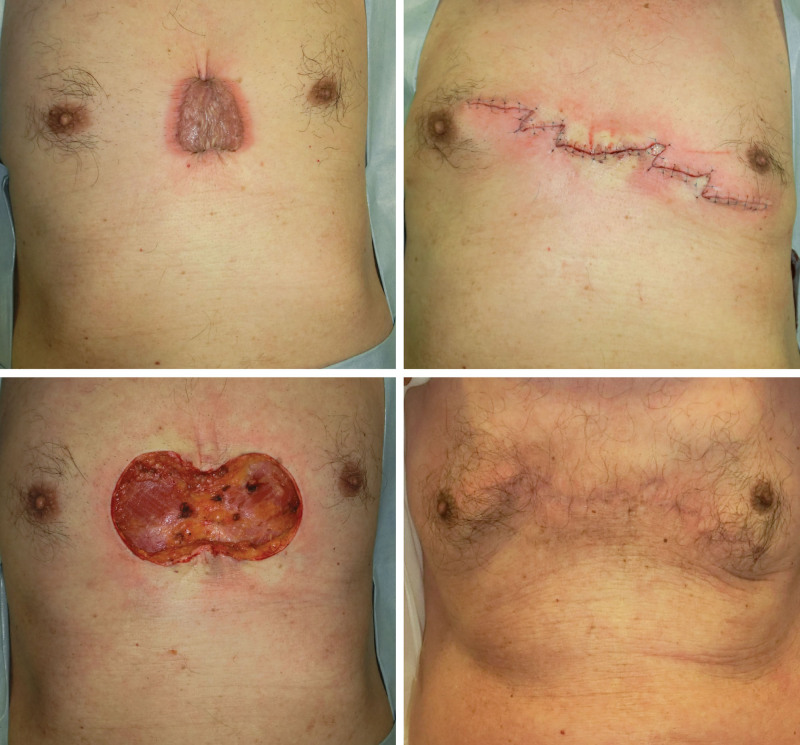
Fig. 6.
Treatment of a chest wall acne keloid by using Z-plasty and postoperative radiotherapy. (Above, left) Preoperative view. (Above, right) Immediately after total keloid excision. (Below, left) Immediately after surgery. (Below, right) Two years after surgery. A 60-year-old man developed a chest-wall keloid as a result of acne. It was excised completely and the wound was closed with Z-plasties to release the tension on the scar. The surgery was followed with electron beam radiotherapy (18 Gy, in three fractions, over 3 days). The inflammation dropped uneventfully and the scar became mature over 18 months.
Flap choice depends on the affected region. A case series study showed that none of 10 huge anterior chest wall keloids recurred after partial or total resection and flap reconstruction.114 Flaps are superior to skin grafts: the latter do not expand postoperatively and can yield pathologic scars encircling the skin graft. When using flaps, the donor-site must undergo multimodal therapy to prevent new keloids.114 Figure 7 shows a hatchet flap–treated scapular keloid.
Fig. 7.
Treatment of a scapular folliculitis keloid by using a hatchet flap and postoperative radiotherapy. (Above, left) Preoperative view. (Above, right) Immediately after total keloid excision and flap design. (Below, left) Immediately after surgery. (Below, right) Two years after surgery. A 70-year-old man developed scapular keloids. They were excised completely and reconstructed by using a hatchet flap. After surgery, the scar was irradiated (18 Gy, in three fractions, over 3 days). The inflammation fell uneventfully and the scar became mature over 18 months.
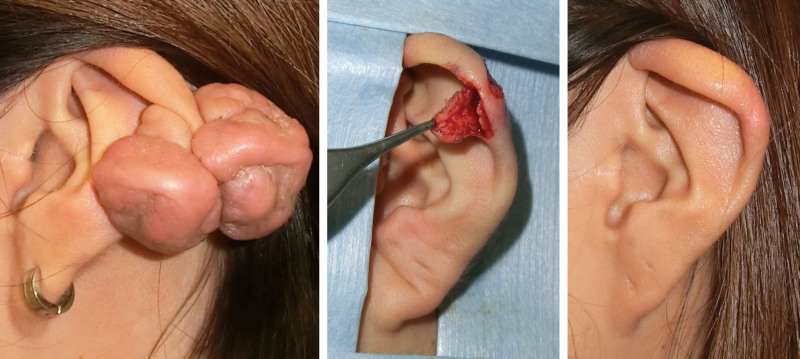
A special region is the ear. Wedge excision is recommended for earlobe keloids.5 A case series study112,115 of earlobe keloids showed that wedge excision and radiotherapy yielded 4.7 percent recurrence at 18 months. Core excision is recommended for auricular cartilage keloids.5 A case series study116 showed that core excision of earlobe and auricular keloids plus steroid injections yielded 9.5 percent recurrence rate at 22 months. Similarly, another case series study117 showed that total and core excision led to 8.1 and 0 percent recurrence, respectively. Figure 8 depicts a core excision–treated auricular keloid.
Fig. 8.
Treatment of an auricular keloid by using the core excision method and postoperative radiotherapy. (Left) Preoperative view. (Center) The flap made on the keloid after the core was removed. (Right) Two years after surgery. A 20-year-old woman developed auricular keloids. A flap was designed on the anterior side of the keloid and the core was removed. The flap was sutured using 6-0 polypropylene sutures. After surgery, the site was irradiated (15 Gy, in two fractions, over 2 days). The inflammation dropped uneventfully and the scar became mature over 18 months.
Radiation Therapy
Radiotherapy effectively treats or prevents keloids by suppressing angiogenesis and therefore inflammation.118 Radiation monotherapy should be reserved for older patients or those with huge keloids because large radiation doses are needed. It immediately reduces pain and itch and slowly ameliorates scar color and thickness in the next year.31
Radiotherapy is particularly effective as a surgery adjunct. Recent meta-analysis of 72 studies119 showed that surgery plus radiotherapy is associated with fewer recurrences (22 percent) than radiation monotherapy (37 percent). Notably, this surgery plus radiotherapy rate is higher than the rate in our center (<10 percent).112 This may reflect the fact that the meta-analysis examined studies published from 1957 to 2014.112 Refinements in surgery, radiotherapy, and postoperative care techniques probably all contribute to our low recurrence rate.
Superficial or orthovoltage x-rays (photons) were once used,120,121 but many institutions now prefer electron beam (β-ray) instruments because of fewer internal organ side effects.122–124 High-dose-rate brachytherapy (mainly γ-rays) is increasingly used,125,126 but its safety for internal organs should be studied further.
The maximal biologically effective dose for keloids is 30 Gy.127–129 Doses exceeding this have no gains in efficacy and only increase the secondary carcinogenesis risk. Given that body sites vary in recurrence susceptibility, a 30-Gy biologically effective dose is not always necessary. Our facility exploits this to further decrease the secondary carcinogenesis risk: we apply body site–specific postoperative irradiation for keloids, namely, 18 Gy in three fractions over 3 days (biologically effective dose, approximately 30 Gy) to high-recurrence sites, 8 Gy in one fraction over 1 day to earlobes, and 15 Gy in two fractions over 2 days to other body sites.112
Over 70 years, there has been a small handful of case reports of malignant carcinogenesis after keloid radiotherapy.129–134 Mostly, it is unclear whether these are true secondary carcinogenesis cases. Moreover, a survey135 of radiation oncologists worldwide showed that greater than 90 percent considered keloids to be an acceptable radiotherapy indication. Thus, before excluding the possibility of keloid radiotherapy, surgeons should discuss the issue with radiation oncologists.129
LONG-TERM POSTTREATMENT FOLLOW-UP OF HYPERTROPHIC SCARS AND KELOIDS
Treated hypertrophic scar and keloid patients should be educated about scar management and followed-up over the long-term. Close follow-up allows early detection and treatment of small recurrences that respond well to steroid tape, plaster, or injection. Thus, patients should be followed up for greater than 18 to 24 months. Follow-up can stop when the scar is flat and soft.
Hypertrophic scar and keloid patients often experience psychological stress that may aggravate their scars. They may benefit from makeup or camouflage therapies136–139 because they improve cosmetic appearance and promote beneficial physiologic changes.
CONCLUSIONS
In the past decade, many high-quality studies have been conducted, and the level of evidence for many treatment or prevention regimens has strengthened. As reflected in my reprised review here, these changes have led to pathologic scar management strategies that now effectively and safely prevent, eliminate, or ameliorate these pernicious scars. However, given ethnic differences in pathologic scar propensity, prevention and treatment algorithms should be optimized for each human race by means of international collaboration.
Footnotes
Disclosure: There are no financial disclosures to be made.
By reading this article, you are entitled to claim one (1) hour of Category 2 Patient Safety Credit. ASPS members can claim this credit by logging in to PlasticSurgery.org Dashboard, clicking “Submit CME,” and completing the form.
REFERENCES
- 1.Ogawa R. The most current algorithms for the treatment and prevention of hypertrophic scars and keloids. Plast Reconstr Surg. 2010;125:557–568. [DOI] [PubMed] [Google Scholar]
- 2.Gold MH, Berman B, Clementoni MT, Gauglitz GG, Nahai F, Murcia C. Updated international clinical recommendations on scar management: Part 1. Evaluating the evidence. Dermatol Surg. 2014;40:817–824. [DOI] [PubMed] [Google Scholar]
- 3.Monstrey S, Middelkoop E, Vranckx JJ, et al. Updated scar management practical guidelines: Non-invasive and invasive measures. J Plast Reconstr Aesthet Surg. 2014;67:1017–1025. [DOI] [PubMed] [Google Scholar]
- 4.Seegenschmiedt MH, Micke O, Niewald M, et al. German Cooperative Group on Radiotherapy of Benign Diseases (GCG-BD). DEGRO guidelines for the radiotherapy of non-malignant disorders: Part III. Hyperproliferative disorders. Strahlenther Onkol. 2015;191:541–548. [DOI] [PubMed] [Google Scholar]
- 5.Ogawa R, Akita S, Akaishi S, et al. Diagnosis and treatment of keloids and hypertrophic scars: Japan Scar Workshop Consensus Document 2018. Burns Trauma. 2019;7:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogawa R. Keloid and hypertrophic scars are the result of chronic inflammation in the reticular dermis. Int J Mol Sci. 2017;18:E606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang C, Akaishi S, Hyakusoku H, Ogawa R. Are keloid and hypertrophic scar different forms of the same disorder? A fibroproliferative skin disorder hypothesis based on keloid findings. Int Wound J. 2014;11:517–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marneros AG, Norris JE, Olsen BR, Reichenberger E. Clinical genetics of familial keloids. Arch Dermatol. 2001;137:1429–1434. [DOI] [PubMed] [Google Scholar]
- 9.Bayat A, Bock O, Mrowietz U, Ollier WE, Ferguson MW. Genetic susceptibility to keloid disease and transforming growth factor beta 2 polymorphisms. Br J Plast Surg. 2002;55:283–286. [DOI] [PubMed] [Google Scholar]
- 10.Nakashima M, Chung S, Takahashi A, et al. A genome-wide association study identifies four susceptibility loci for keloid in the Japanese population. Nat Genet. 2010;42:768–771. [DOI] [PubMed] [Google Scholar]
- 11.Ogawa R, Watanabe A, Than Naing B, et al. Associations between keloid severity and single-nucleotide polymorphisms: Importance of rs8032158 as a biomarker of keloid severity. J Invest Dermatol. 2014;134:2041–2043. [DOI] [PubMed] [Google Scholar]
- 12.Fujita M, Yamamoto Y, Jiang JJ, et al. NEDD4 is involved in inflammation development during keloid formation. J Invest Dermatol. 2019;139:333–341. [DOI] [PubMed] [Google Scholar]
- 13.Tan S, Khumalo N, Bayat A. Understanding keloid pathobiology from a quasi-neoplastic perspective: Less of a scar and more of a chronic inflammatory disease with cancer-like tendencies. Front Immunol. 2019;10:1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang C, Wu Z, Du Y, Ogawa R. Teot L, Mustoe TA, Middelkoop E, Gauglitz GG, eds. The epidemiology of keloids. In: Textbook on Scar Management: Guidelines, State of the Art Management and Emerging Technologies. 2020:Cham, Switzerland: Springer; 29–34. [Google Scholar]
- 15.D’Andrea F, Vozza A, Brongo S, Di Girolamo F, Vozza G. Dermatofibrosarcoma protuberans: Experience with 14 cases. J Eur Acad Dermatol Venereol. 2001;15:427–429. [DOI] [PubMed] [Google Scholar]
- 16.Kamath NV, Ormsby A, Bergfeld WF, House NS. A light microscopic and immunohistochemical evaluation of scars. J Cutan Pathol. 2002;29:27–32. [DOI] [PubMed] [Google Scholar]
- 17.Martin L, Combemale P, Dupin M, et al. The atrophic variant of dermatofibrosarcoma protuberans in childhood: A report of six cases. Br J Dermatol. 1998;139:719–725. [PubMed] [Google Scholar]
- 18.Sabater-Marco V, Pérez-Vallés A, Berzal-Cantalejo F, Rodriguez-Serna M, Martinez-Diaz F, Martorell-Cebollada M. Sclerosing dermatofibrosarcoma protuberans (DFSP): An unusual variant with focus on the histopathologic differential diagnosis. Int J Dermatol. 2006;45:59–62. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen CM, Burch JM, Fitzpatrick JE, Peterson SL, Weston WL. Giant cell fibroblastoma in a child misdiagnosed as a dermatofibroma. Pediatr Dermatol. 2002;19:28–32. [DOI] [PubMed] [Google Scholar]
- 20.Ogawa R, Akaishi S, Hyakusoku H. Differential and exclusive diagnosis of diseases that resemble keloids and hypertrophic scars. Ann Plast Surg. 2009;62:660–664. [DOI] [PubMed] [Google Scholar]
- 21.Wong TW, Lee JY. Should excised keloid scars be sent for routine histologic analysis? Ann Plast Surg. 2008;60:724. [DOI] [PubMed] [Google Scholar]
- 22.Gulamhuseinwala N, Mackey S, Meagher P, Powell B. Should excised keloid scars be sent for routine histologic analysis? Ann Plast Surg. 2008;60:186–187. [DOI] [PubMed] [Google Scholar]
- 23.Ogawa R, Okai K, Tokumura F, et al. The relationship between skin stretching/contraction and pathologic scarring: The important role of mechanical forces in keloid generation. Wound Repair Regen. 2012;20:149–157. [DOI] [PubMed] [Google Scholar]
- 24.Dohi T, Padmanabhan J, Akaishi S, et al. The interplay of mechanical stress, strain, and stiffness at the keloid periphery correlates with increased caveolin-1/ROCK signaling and scar progression. Plast Reconstr Surg. 2019;144:58e–67e. [DOI] [PubMed] [Google Scholar]
- 25.Harn HI, Ogawa R, Hsu CK, Hughes MW, Tang MJ, Chuong CM. The tension biology of wound healing. Exp Dermatol. 2019;28:464–471. [DOI] [PubMed] [Google Scholar]
- 26.Atkinson JA, McKenna KT, Barnett AG, McGrath DJ, Rudd M. A randomized, controlled trial to determine the efficacy of paper tape in preventing hypertrophic scar formation in surgical incisions that traverse Langer’s skin tension lines. Plast Reconstr Surg. 2005;116:1648–1656; discussion 1657–1658. [DOI] [PubMed] [Google Scholar]
- 27.O’Brien L, Jones DJ. Silicone gel sheeting for preventing and treating hypertrophic and keloid scars. Cochrane Database Syst Rev. 2013;9:CD003826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hsu KC, Luan CW, Tsai YW. Review of silicone gel sheeting and silicone gel for the prevention of hypertrophic scars and keloids. Wounds. 2017;29:154–158. [PubMed] [Google Scholar]
- 29.Chan KY, Lau CL, Adeeb SM, Somasundaram S, Nasir-Zahari M. A randomized, placebo-controlled, double-blind, prospective clinical trial of silicone gel in prevention of hypertrophic scar development in median sternotomy wound. Plast Reconstr Surg. 2005;116:1013–1020; discussion 1021–1022. [DOI] [PubMed] [Google Scholar]
- 30.Ai JW, Liu JT, Pei SD, et al. The effectiveness of pressure therapy (15-25 mmHg) for hypertrophic burn scars: A systematic review and meta-analysis. Sci Rep. 2017;7:40185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ogawa R, Akaishi S, Kuribayashi S, Miyashita T. Keloids and hypertrophic scars can now be cured completely: Recent progress in our understanding of the pathogenesis of keloids and hypertrophic scars and the most promising current therapeutic strategy. J Nippon Med Sch. 2016;83:46–53. [DOI] [PubMed] [Google Scholar]
- 32.Noishiki C, Hayasaka Y, Ogawa R. Sex differences in keloidogenesis: An analysis of 1659 keloid patients in Japan. Dermatol Ther (Heidelb.). 2019;9:747–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Park TH, Chang CH. Keloid recurrence in pregnancy. Aesthetic Plast Surg. 2012;36:1271–1272. [DOI] [PubMed] [Google Scholar]
- 34.Kim HD, Hwang SM, Lim KR, Jung YH, Ahn SM, Kim Song J. Recurrent auricular keloids during pregnancy. Arch Plast Surg. 2013;40:70–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arima J, Huang C, Rosner B, Akaishi S, Ogawa R. Hypertension: A systemic key to understanding local keloid severity. Wound Repair Regen. 2015;23:213–221. [DOI] [PubMed] [Google Scholar]
- 36.Quong WL, Kozai Y, Ogawa R. A case of keloids complicated by Castleman’s disease: Interleukin-6 as a keloid risk factor. Plast Reconstr Surg Glob Open. 2017;5:e1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abdu Allah AMK, Mohammed KI, Farag AGA, Hagag MM, Essam M, Tayel NR. Interleukin-6 serum level and gene polymorphism in keloid patients. Cell Mol Biol (Noisy-le-grand). 2019;65:43–48. [PubMed] [Google Scholar]
- 38.Marneros AG, Norris JE, Olsen BR, Reichenberger E. Clinical genetics of familial keloids. Arch Dermatol. 2001;137:1429–1434. [DOI] [PubMed] [Google Scholar]
- 39.Chen Y, Gao JH, Liu XJ, Yan X, Song M. Characteristics of occurrence for Han Chinese familial keloids. Burns. 2006;32:1052–1059. [DOI] [PubMed] [Google Scholar]
- 40.Nakashima M, Chung S, Takahashi A, et al. A genome-wide association study identifies four susceptibility loci for keloid in the Japanese population. Nat Genet. 2010;42:768–771. [DOI] [PubMed] [Google Scholar]
- 41.Ogawa R, Watanabe A, Than Naing B, et al. Associations between keloid severity and single-nucleotide polymorphisms: Importance of rs8032158 as a biomarker of keloid severity. J Invest Dermatol. 2014;134:2041–2043. [DOI] [PubMed] [Google Scholar]
- 42.Fujita M, Yamamoto Y, Jiang JJ, et al. NEDD4 is involved in inflammation development during keloid formation. J Invest Dermatol. 2019;139:333–341. [DOI] [PubMed] [Google Scholar]
- 43.Yagi Y, Kuwatsuka Y, Asai M, Honda M, Utani A. Coexistence of keloids and pilomatricoma in a patient with Rubinstein-Taybi syndrome. Dermatol Online J. 2018;24:13030/qt4rq2k5fr. [PubMed] [Google Scholar]
- 44.van de Kar AL, Houge G, Shaw AC, et al. Keloids in Rubinstein-Taybi syndrome: A clinical study. Br J Dermatol. 2014;171:615–621. [DOI] [PubMed] [Google Scholar]
- 45.Hosalkar H, Greenberg J, Gaugler RL, Garg S, Dormans JP. Abnormal scarring with keloid formation after osteochondroma excision in children with multiple hereditary exostoses. J Pediatr Orthop. 2007;27:333–337. [DOI] [PubMed] [Google Scholar]
- 46.Katta R, Kramer MJ. Skin and diet: An update on the role of dietary change as a treatment strategy for skin disease. Skin Therapy Lett. 2018;23:1–5. [PubMed] [Google Scholar]
- 47.Goutos I, Ogawa R. Steroid tape: A promising adjunct to scar management. Scars Burn Heal. 2017;3:2059513117690937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tsai CH, Kao HK, Akaishi S, An-Jou Lin J, Ogawa R. Combination of 1,064-nm neodymium-doped yttrium aluminum garnet laser and steroid tape decreases the total treatment time of hypertrophic scars: An analysis of 40 cases of cesarean-section scars. Dermatol Surg. 2020;46:1062–1067. [DOI] [PubMed] [Google Scholar]
- 49.Choi YH, Kim KM, Kim HO, Jang YC, Kwak IS. Clinical and histological correlation in post-burn hypertrophic scar for pain and itching sensation. Ann Dermatol. 2013;25:428–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stekelenburg CM, Marck RE, Tuinebreijer WE, de Vet HC, Ogawa R, van Zuijlen PP. A systematic review on burn scar contracture treatment: Searching for evidence. J Burn Care Res. 2015;36:e153–e161. [DOI] [PubMed] [Google Scholar]
- 51.Jiang Q, Chen J, Liu Z. Silicone gel sheeting for treating hypertrophic scars. Cochrane Database Syst Rev. 2021;9:CD013357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.de Oliveira GV, Nunes TA, Magna LA, et al. Silicone versus nonsilicone gel dressings: A controlled trial. Dermatol Surg. 2001;27:721–726. [DOI] [PubMed] [Google Scholar]
- 53.So K, Umraw N, Scott J, Campbell K, Musgrave M, Cartotto R. Effects of enhanced patient education on compliance with silicone gel sheeting and burn scar outcome: A randomized prospective study. J Burn Care Rehabil. 2003;24:411–417; discussion 410. [DOI] [PubMed] [Google Scholar]
- 54.Akaishi S, Akimoto M, Hyakusoku H, Ogawa R. The tensile reduction effects of silicone gel sheeting. Plast Reconstr Surg. 2010;126:109e–111e. [DOI] [PubMed] [Google Scholar]
- 55.Shin TM, Bordeaux JS. The role of massage in scar management: A literature review. Dermatol Surg. 2012;38:414–423. [DOI] [PubMed] [Google Scholar]
- 56.Wong TS, Li JZ, Chen S, Chan JY, Gao W. The efficacy of triamcinolone acetonide in keloid treatment: A systematic review and meta-analysis. Front Med (Lausanne). 2016;3:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bi M, Sun P, Li D, Dong Z, Chen Z. Intralesional injection of botulinum toxin type A compared with intralesional injection of corticosteroid for the treatment of hypertrophic scar and keloid: A systematic review and meta-analysis. Med Sci Monit. 2019;25:2950–2958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sun P, Lu X, Zhang H, Hu Z. The efficacy of drug injection in the treatment of pathological scar: A network meta-analysis. Aesthetic Plast Surg. 2021;45:791–805. [DOI] [PubMed] [Google Scholar]
- 59.Trisliana Perdanasari A, Torresetti M, Grassetti L, et al. Intralesional injection treatment of hypertrophic scars and keloids: A systematic review regarding outcomes. Burns Trauma. 2015;3:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Morelli Coppola M, Salzillo R, Segreto F, Persichetti P. Triamcinolone acetonide intralesional injection for the treatment of keloid scars: Patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:387–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rabello FB, Souza CD, Farina Júnior JA. Update on hypertrophic scar treatment. Clinics (Sao Paulo). 2014;69:565–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Abedini R, Sasani P, Mahmoudi HR, Nasimi M, Teymourpour A, Shadlou Z. Comparison of intralesional verapamil versus intralesional corticosteroids in treatment of keloids and hypertrophic scars: A randomized controlled trial. Burns. 2018;44:1482–1488. [DOI] [PubMed] [Google Scholar]
- 63.Saki N, Mokhtari R, Nozari F. Comparing the efficacy of intralesional triamcinolone acetonide with verapamil in treatment of keloids: A randomized controlled trial. Dermatol Pract Concept. 2019;9:4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mustoe TA, Cooter RD, Gold MH, et al. International Advisory Panel on Scar Management. International clinical recommendations on scar management. Plast Reconstr Surg. 2002;110:560–571. [DOI] [PubMed] [Google Scholar]
- 65.Roques C, Téot L. The use of corticosteroids to treat keloids: A review. Int J Low Extrem Wounds. 2008;7:137–145. [DOI] [PubMed] [Google Scholar]
- 66.Fredman R, Tenenhaus M. Cushing’s syndrome after intralesional triamcinolone acetonide: A systematic review of the literature and multinational survey. Burns. 2013;39:549–557. [DOI] [PubMed] [Google Scholar]
- 67.Ogawa R, Akashi S. Téot L, Mustoe TA, Middelkoop E, Gauglitz GG, eds. Effectiveness of corticosteroid tape/plaster for keloids and hypertrophic scars: Comparative study of fludroxycortide and deprodone tape/plasters. In: Textbook on Scar Management. 2016:Cham, Switzerland: Springer; 55–60. [Google Scholar]
- 68.Hayashi T, Furukawa H, Oyama A, et al. A new uniform protocol of combined corticosteroid injections and ointment application reduces recurrence rates after surgical keloid/hypertrophic scar excision. Dermatol Surg. 2012;38:893–897. [DOI] [PubMed] [Google Scholar]
- 69.Japanese Society for Burn Injuries. Burn Practical Guideline. 2nd ed. Available at: http://www.jsbi-burn.org/members/guideline/pdf/guideline2.pdf. Accessed May 30, 2020. [Google Scholar]
- 70.Kafka M, Collins V, Kamolz LP, Rappl T, Branski LK, Wurzer P. Evidence of invasive and noninvasive treatment modalities for hypertrophic scars: A systematic review. Wound Repair Regen. 2017;25:139–144. [DOI] [PubMed] [Google Scholar]
- 71.Bouzari N, Davis SC, Nouri K. Laser treatment of keloids and hypertrophic scars. Int J Dermatol. 2007;46:80–88. [DOI] [PubMed] [Google Scholar]
- 72.Jin R, Huang X, Li H, et al. Laser therapy for prevention and treatment of pathologic excessive scars. Plast Reconstr Surg. 2013;132:1747–1758. [DOI] [PubMed] [Google Scholar]
- 73.Kono T, Erçöçen AR, Nakazawa H, Honda T, Hayashi N, Nozaki M. The flashlamp-pumped pulsed dye laser (585 nm) treatment of hypertrophic scars in Asians. Ann Plast Surg. 2003;51:366–371. [DOI] [PubMed] [Google Scholar]
- 74.Vrijman C, van Drooge AM, Limpens J, et al. Laser and intense pulsed light therapy for the treatment of hypertrophic scars: A systematic review. Br J Dermatol. 2011;165:934–942. [DOI] [PubMed] [Google Scholar]
- 75.Hultman CS, Friedstat JS, Edkins RE, Cairns BA, Meyer AA. Laser resurfacing and remodeling of hypertrophic burn scars: The results of a large, prospective, before-after cohort study, with long-term follow-up. Ann Surg. 2014;260:519–529; discussion 529–532. [DOI] [PubMed] [Google Scholar]
- 76.Anderson RR, Donelan MB, Hivnor C, et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: Consensus report. JAMA Dermatol. 2014;150:187–193. [DOI] [PubMed] [Google Scholar]
- 77.Khansa I, Harrison B, Janis JE. Evidence-based scar management: How to improve results with technique and technology. Plast Reconstr Surg. 2016;138(Suppl):165S–178S. [DOI] [PubMed] [Google Scholar]
- 78.Koike S, Akaishi S, Nagashima Y, Dohi T, Hyakusoku H, Ogawa R. Nd:YAG laser treatment for keloids and hypertrophic scars: An analysis of 102 cases. Plast Reconstr Surg Glob Open. 2014;2:e272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Al-Mohamady Ael-S, Ibrahim SM, Muhammad MM. Pulsed dye laser versus long-pulsed Nd:YAG laser in the treatment of hypertrophic scars and keloid: A comparative randomized split-scar trial. J Cosmet Laser Ther. 2016;18:208–212. [DOI] [PubMed] [Google Scholar]
- 80.Verhaeghe E, Ongenae K, Bostoen J, Lambert J. Nonablative fractional laser resurfacing for the treatment of hypertrophic scars: A randomized controlled trial. Dermatol Surg. 2013;39:426–434. [DOI] [PubMed] [Google Scholar]
- 81.van Drooge AM, Vrijman C, van der Veen W, Wolkerstorfer A. A randomized controlled pilot study on ablative fractional CO2 laser for consecutive patients presenting with various scar types. Dermatol Surg. 2015;41:371–377. [DOI] [PubMed] [Google Scholar]
- 82.Apfelberg DB, Maser MR, White DN, Lash H. Failure of carbon dioxide laser excision of keloids. Lasers Surg Med. 1989;9:382–388. [DOI] [PubMed] [Google Scholar]
- 83.Norris JE. The effect of carbon dioxide laser surgery on the recurrence of keloids. Plast Reconstr Surg. 1991;87:44–49; discussion 50–53. [PubMed] [Google Scholar]
- 84.Mandy SH. The practical use of Z-plasty. J Dermatol Surg. 1975;1:57–60. [DOI] [PubMed] [Google Scholar]
- 85.Goutos I, Yousif AH, Ogawa R. W-plasty in scar revision: Geometrical considerations and suggestions for site-specific design modifications. Plast Reconstr Surg Glob Open. 2019;7:e2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ogawa R. Surgery for scar revision and reduction: From primary closure to flap surgery. Burns Trauma. 2019;7:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Huang C, Ogawa R. Three-dimensional reconstruction of scar contracture-bearing axilla and digital webs using the square flap method. Plast Reconstr Surg Glob Open. 2014;2:e149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hifny MA. The square flap technique for burn contractures: Clinical experience and analysis of length gain. Ann Burns Fire Disasters. 2018;31:306–312. [PMC free article] [PubMed] [Google Scholar]
- 89.Yoshino Y, Kubomura K, Ueda H, Tsuge T, Ogawa R. Extension of flaps associated with burn scar reconstruction: A key difference between island and skin-pedicled flaps. Burns. 2018;44:683–691. [DOI] [PubMed] [Google Scholar]
- 90.Luck RP, Flood R, Eyal D, Saludades J, Hayes C, Gaughan J. Cosmetic outcomes of absorbable versus nonabsorbable sutures in pediatric facial lacerations. Pediatr Emerg Care. 2008;24:137–142. [DOI] [PubMed] [Google Scholar]
- 91.Durkaya S, Kaptanoglu M, Nadir A, Yilmaz S, Cinar Z, Dogan K. Do absorbable sutures exacerbate presternal scarring? Tex Heart Inst J. 2005;32:544–548. [PMC free article] [PubMed] [Google Scholar]
- 92.Ogawa R, Akaishi S, Huang C, et al. Clinical applications of basic research that shows reducing skin tension could prevent and treat abnormal scarring: The importance of fascial/subcutaneous tensile reduction sutures and flap surgery for keloid and hypertrophic scar reconstruction. J Nippon Med Sch. 2011;78:68–76. [DOI] [PubMed] [Google Scholar]
- 93.Tsuge T, Aoki M, Akaishi S, Dohi T, Yamamoto H, Ogawa R. Geometric modeling and a retrospective cohort study on the usefulness of fascial tensile reductions in severe keloid surgery. Surgery. 2020;167:504–509. [DOI] [PubMed] [Google Scholar]
- 94.Walocko FM, Eber AE, Kirsner RS, Badiavas E, Nouri K. Systematic review of the therapeutic roles of adipose tissue in dermatology. J Am Acad Dermatol. 2018;79:935–944. [DOI] [PubMed] [Google Scholar]
- 95.O’Boyle CP, Shayan-Arani H, Hamada MW. Intralesional cryotherapy for hypertrophic scars and keloids: A review. Scars Burn Heal. 2017;3:2059513117702162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kasyanju Carrero LM, Ma WW, Liu HF, Yin XF, Zhou BR. Botulinum toxin type A for the treatment and prevention of hypertrophic scars and keloids: Updated review. J Cosmet Dermatol. 2019;18:10–15. [DOI] [PubMed] [Google Scholar]
- 97.Huang RL, Ho CK, Tremp M, Xie Y, Li Q, Zan T. Early postoperative application of botulinum toxin type A prevents hypertrophic scarring after epicanthoplasty: A split-face, double-blind, randomized trial. Plast Reconstr Surg. 2019;144:835–844. [DOI] [PubMed] [Google Scholar]
- 98.Li YH, Yang J, Liu JQ, et al. A randomized, placebo-controlled, double-blind, prospective clinical trial of botulinum toxin type A in prevention of hypertrophic scar development in median sternotomy wound. Aesthetic Plast Surg. 2018;42:1364–1369. [DOI] [PubMed] [Google Scholar]
- 99.Kim WI, Kim S, Cho SW, Cho MK. The efficacy of bleomycin for treating keloid and hypertrophic scar: A systematic review and meta-analysis. J Cosmet Dermatol. 2020;19:3357–3366. [DOI] [PubMed] [Google Scholar]
- 100.Sidgwick GP, McGeorge D, Bayat A. A comprehensive evidence-based review on the role of topicals and dressings in the management of skin scarring. Arch Dermatol Res. 2015;307:461–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Suzawa H, Ichikawa K, Kikuchi S, et al. Effect of tranilast, an anti-allergic drug, on carrageenin-induced granulation and capillary permeability in rats (in Japanese). Nihon Yakurigaku Zasshi. 1992;99:241–246. [DOI] [PubMed] [Google Scholar]
- 102.Nanba K, Oura T, Soeda S, Sioya N, Tsukada S, Hanaoka K. Clinical evaluation of tranilast for keloid and hypertrophic scarring: Optimal dose finding study in a double blind study. Nessho. 1992;18:30–45. [Google Scholar]
- 103.Darakhshan S, Pour AB. Tranilast: A review of its therapeutic applications. Pharmacol Res. 2015;91:15–28. [DOI] [PubMed] [Google Scholar]
- 104.Nakamura K, Irie H, Inoue M, Mitani H, Sunami H, Sano S. Factors affecting hypertrophic scar development in median sternotomy incisions for congenital cardiac surgery. J Am Coll Surg. 1997;185:218–223. [DOI] [PubMed] [Google Scholar]
- 105.Marsden CW. Fluocinolone acetonide 0.2 per cent cream: A co-operative clinical trial. Br J Dermatol. 1968;80:614–617. [DOI] [PubMed] [Google Scholar]
- 106.O’Boyle CP, Shayan-Arani H, Hamada MW. Intralesional cryotherapy for hypertrophic scars and keloids: A review. Scars Burn Heal. 2017;3:2059513117702162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Har-Shai Y, Amar M, Sabo E. Intralesional cryotherapy for enhancing the involution of hypertrophic scars and keloids. Plast Reconstr Surg. 2003;111:1841–1852. [DOI] [PubMed] [Google Scholar]
- 108.Rusciani L, Paradisi A, Alfano C, Chiummariello S, Rusciani A. Cryotherapy in the treatment of keloids. J Drugs Dermatol. 2006;5:591–595. [PubMed] [Google Scholar]
- 109.Gupta S, Kumar B. Intralesional cryosurgery using lumbar puncture and/or hypodermic needles for large, bulky, recalcitrant keloids. Int J Dermatol. 2001;40:349–353. [DOI] [PubMed] [Google Scholar]
- 110.Har-Shai Y, Sabo E, Rohde E, Hyams M, Assaf C, Zouboulis CC. Intralesional cryosurgery enhances the involution of recalcitrant auricular keloids: A new clinical approach supported by experimental studies [published correction appears in Wound Repair Regen. 2007;15:163]. Wound Repair Regen. 2006;14:18–27. [DOI] [PubMed] [Google Scholar]
- 111.Arima J, Dohi T, Kuribayashi S, Akaishi S, Ogawa R. Z-plasty and postoperative radiotherapy for anterior chest wall keloids: An analysis of 141 patients. Plast Reconstr Surg Glob Open. 2019;7:e2177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ogawa R, Tosa M, Dohi T, Akaishi S, Kuribayashi S. Surgical excision and postoperative radiotherapy for keloids. Scars Burn Heal. 2019;5:2059513119891113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Dohi T, Kuribayashi S, Tosa M, Aoki M, Akaishi S, Ogawa R. Z-plasty and postoperative radiotherapy for upper-arm keloids: An analysis of 38 patients. Plast Reconstr Surg Glob Open. 2019;7:e2496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ogawa R, Ono S, Akaishi S, Dohi T, Iimura T, Nakao J. Reconstruction after anterior chest wall keloid resection using internal mammary artery perforator propeller flaps. Plast Reconstr Surg Glob Open. 2016;4:e1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ogawa R, Huang C, Akaishi S, et al. Analysis of surgical treatments for earlobe keloids: Analysis of 174 lesions in 145 patients. Plast Reconstr Surg. 2013;132:818e–825e. [DOI] [PubMed] [Google Scholar]
- 116.Al Aradi IK, Alawadhi SA, Alkhawaja FA, Alaradi I. Earlobe keloids: A pilot study of the efficacy of keloidectomy with core fillet flap and adjuvant intralesional corticosteroids. Dermatol Surg. 2013;39:1514–1519. [DOI] [PubMed] [Google Scholar]
- 117.Ogawa R, Akaishi S, Dohi T, Kuribayashi S, Miyashita T, Hyakusoku H. Analysis of the surgical treatments of 63 keloids on the cartilaginous part of the auricle: Effectiveness of the core excision method. Plast Reconstr Surg. 2015;135:868–875. [DOI] [PubMed] [Google Scholar]
- 118.Ogawa R, Akaishi S. Endothelial dysfunction may play a key role in keloid and hypertrophic scar pathogenesis: Keloids and hypertrophic scars may be vascular disorders. Med Hypotheses. 2016;96:51–60. [DOI] [PubMed] [Google Scholar]
- 119.Mankowski P, Kanevsky J, Tomlinson J, Dyachenko A, Luc M. Optimizing radiotherapy for keloids: A meta-analysis systematic review comparing recurrence rates between different radiation modalities. Ann Plast Surg. 2017;78:403–411. [DOI] [PubMed] [Google Scholar]
- 120.Norris JE. Superficial x-ray therapy in keloid management: A retrospective study of 24 cases and literature review. Plast Reconstr Surg. 1995;95:1051–1055. [DOI] [PubMed] [Google Scholar]
- 121.Enhamre A, Hammar H. Treatment of keloids with excision and postoperative X-ray irradiation. Dermatologica. 1983;167:90–93. [DOI] [PubMed] [Google Scholar]
- 122.Akita S, Akino K, Yakabe A, et al. Combined surgical excision and radiation therapy for keloid treatment. J Craniofac Surg. 2007;18:1164–1169. [DOI] [PubMed] [Google Scholar]
- 123.Ogawa R, Mitsuhashi K, Hyakusoku H, Miyashita T. Postoperative electron-beam irradiation therapy for keloids and hypertrophic scars: Retrospective study of 147 cases followed for more than 18 months. Plast Reconstr Surg. 2003;111:547–553; discussion 554–555. [DOI] [PubMed] [Google Scholar]
- 124.Ogawa R, Miyashita T, Hyakusoku H, Akaishi S, Kuribayashi S, Tateno A. Postoperative radiation protocol for keloids and hypertrophic scars: Statistical analysis of 370 sites followed for over 18 months. Ann Plast Surg. 2007;59:688–691. [DOI] [PubMed] [Google Scholar]
- 125.Kuribayashi S, Miyashita T, Ozawa Y, et al. Post-keloidectomy irradiation using high-dose-rate superficial brachytherapy. J Radiat Res. 2011;52:365–368. [DOI] [PubMed] [Google Scholar]
- 126.Goutos I, Ogawa R. Brachytherapy in the adjuvant management of keloid scars: Literature review. Scars Burn Heal. 2017;3:2059513117735483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Guix B, Henríquez I, Andrés A, Finestres F, Tello JI, Martínez A. Treatment of keloids by high-dose-rate brachytherapy: A seven-year study. Int J Radiat Oncol Biol Phys. 2001;50:167–172. [DOI] [PubMed] [Google Scholar]
- 128.Jones K, Fuller CD, Luh JY, et al. Case report and summary of literature: Giant perineal keloids treated with post-excisional radiotherapy. BMC Dermatol. 2006;6:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ogawa R, Yoshitatsu S, Yoshida K, Miyashita T. Is radiation therapy for keloids acceptable? The risk of radiation-induced carcinogenesis. Plast Reconstr Surg. 2009;124:1196–1201. [DOI] [PubMed] [Google Scholar]
- 130.Horton CE, Crawford J, Oakey RS. Malignant change in keloids. Plast Reconstr Surg (1946). 1953;12:86–89. [DOI] [PubMed] [Google Scholar]
- 131.Biemans RG. A rare case of sarcomatous degeneration of a cheloid. Arch Chir Neerl. 1963;15:175–185. [PubMed] [Google Scholar]
- 132.Hoffman S. Radiotherapy for keloids. Ann Plast Surg. 1982;9:265. [DOI] [PubMed] [Google Scholar]
- 133.Botwood N, Lewanski C, Lowdell C. The risks of treating keloids with radiotherapy. Br J Radiol. 1999;72:1222–1224. [DOI] [PubMed] [Google Scholar]
- 134.Bilbey JH, Müller NL, Miller RR, Nelems B. Localized fibrous mesothelioma of pleura following external ionizing radiation therapy. Chest. 1988;94:1291–1292. [DOI] [PubMed] [Google Scholar]
- 135.Leer JW, van Houtte P, Davelaar J. Indications and treatment schedules for irradiation of benign diseases: A survey. Radiother Oncol. 1998;48:249–257. [DOI] [PubMed] [Google Scholar]
- 136.Rose EH. Aesthetic restoration of the severely disfigured face in burn victims: A comprehensive strategy. Plast Reconstr Surg. 1995;96:1573–1585; discussion 1586–1587. [PubMed] [Google Scholar]
- 137.Chang CW, Ries WR. Nonoperative techniques for scar management and revision. Facial Plast Surg. 2001;17:283–288. [DOI] [PubMed] [Google Scholar]
- 138.Sidle DM, Decker JR. Use of makeup, hairstyles, glasses, and prosthetics as adjuncts to scar camouflage. Facial Plast Surg Clin North Am. 2011;19:481–489. [DOI] [PubMed] [Google Scholar]
- 139.Mee D, Wong BJ. Medical makeup for concealing facial scars. Facial Plast Surg. 2012;28:536–540. [DOI] [PubMed] [Google Scholar]