Abstract
Objective
This systematic review and meta-analysis were conducted to study the prevalence and pattern of sleep disturbances in children and adolescents during the COVID-19 pandemic.
Methods
MEDLINE, EMBASE, and Web of Science were searched for original studies describing sleep abnormalities in children and adolescents with or without pre-existing neurobehavioral disorders during the COVID-19 pandemic. The pooled estimates for various sleep abnormalities were calculated using a random-effect model.
Results
Of 371 articles screened, 16 studies were included. Among these, five studies were in preschool children, two were in children with pre-existing neurobehavioral disorders and the remaining were in school going children and adolescents. The outcome measures used for sleep were markedly heterogeneous across the studies.
The pooled prevalence of any sleep disturbance in children during the pandemic was 54%(95%CI:50–57%). Interestingly, the prevalence in pre-school children was lower than pre-pandemic times (RR = 0.87; 95% CI:0.58–1.30) but this was not statistically significant. The pooled prevalence of children not meeting sleep recommendation was 49% (95%CI: 39–58%).
Conclusion
The prevalence of sleep problems in children and adolescents during the COVID-19 pandemic is alarming. Pre-school children had a trend towards relatively fewer sleep disturbances due to home confinement measures in comparison with pre-pandemic times. Sleep duration recommendations were not met in nearly half of healthy children. However, these conclusions need to be seen in light of limited literature on the topic, few included studies done in heterogenous populations, and dubious quality of inferences drawn from these studies which were predominantly online surveys.
Prospero registration id
CRD42020213788.
Keywords: Sleep, Children, Adolescents, COVID-19, Pandemic
1. Introduction
It has been more than a year since the first report of coronavirus disease-19 (COVID-19) caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) from Wuhan, China. On March 11th 2020, it was declared as a pandemic by the World Health Organization (WHO). The pandemic subsequently engulfed more than 200 countries with more than 165 million people being affected and around three million deaths [1]. COVID-19 pandemic along with the inevitable lockdowns have had a significant impact on lifestyle behaviors and patient-care worldwide [2]. With new waves of COVID-19 and the re-imposition of lockdowns in different parts of the world, it becomes imperative to study the true impact of initial lockdown in the early phase of the COVID-19 pandemic.
Although SARS-CoV-2 infection is associated with asymptomatic or mild disease course in children, the indirect accompaniments of the pandemic such as lockdowns, travel restrictions, and closure of schools and recreational activities have also influenced the lifestyle and movement behaviors in children [3,4]. The effect on sleep in healthy children during the pandemic has been studied in various online survey studies with varied conclusions. Sleep disturbances being an important co-morbidity in neurobehavioral disorders, it is essential to study the impact of the pandemic on children with these disorders considering the huge unmet needs [5]. Hence, there is a need to comprehensively study the repercussions of the pandemic and precautionary measures on sleep in healthy children and adolescents and in those with neurobehavioral disorders. This can help in devising guidelines focusing on lifestyle behaviors in children and adolescents during such times of crisis. This systematic review and meta-analysis were conducted to study the prevalence and pattern of sleep disturbances in children and adolescents brought about during the COVID-19 pandemic.
2. Methods
2.1. Study objectives
This systematic review aimed to study the impact of the COVID-19 pandemic and quarantine measures on the sleep pattern of children and adolescents with the primary objective being the estimation of prevalence and spectrum of sleep disturbances in children and adolescents during the COVID-19 pandemic. Additional outcomes included the effect of the pandemic on sleep quality, duration, insomnia severity in healthy children and adolescents and in those with neurobehavioral disorders such as autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD). Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines were followed during this study.
2.2. Search strategy
The literature search was performed by two authors independently using search engines MEDLINE, EMBASE, and Web of Science. Articles were searched from inception to October 13th, 2020. The Search terminologies were divided into three categories: Study population (infants/toddlers/children/pediatrics/ adolescents)COVID-19(COVID-19/SARS-CoV-2/coronavirus/2019 nCoV) and sleep (Sleep/Sleep patterns/insomnia/movement behaviors). After the electronic search, a manual search of the references of the selected articles was done to identify additional articles. The detailed search strategy is described in supplementary table 1.
2.3. Eligibility of studies
Original articles assessing the prevalence and spectrum of sleep disturbances during the pandemic with the population of study being children and adolescents were included in the research. Studies including children as a part of a larger study population were also included if separate details were available for children and adolescents. Articles in languages other than English were excluded. Case reports, case series, commentaries, reviews (narrative/systematic), perspectives, editorial communications, theses, abstract-only articles, conference papers, animal studies, and studies describing other serotypes of coronaviruses were also excluded. In addition, research aiming to study sleep pattern in patients with medical illnesses other than neurobehavioral disorders were excluded.
2.4. Outcome measures
The primary outcome measure was the prevalence and pattern of sleep disturbances in healthy children and adolescents during the COVID-19 pandemic. Measures of effect were pooled estimates/prevalence. Additional outcome studied were the effect of the pandemic on sleep quality, sleep duration, and insomnia severity in healthy children and children with pre-existing behavioural or neurodevelopmental disorders like ASD, ADHD.
2.5. Study selection, data extraction, and assessment of the methodological quality
After the removal of duplicates, two authors (SA and MS) independently screened the titles and abstracts of retrieved studies as per predefined inclusion criteria. Subsequently, full texts of the potentially relevant studies were retrieved and assessed by two authors independently. Discrepancies were resolved through discussion with a third review author (PM). The following data were extracted from the included articles: author, country, age group of the children and adolescents, the total number of children included in the specific study, measures used to assess sleep pattern, scales used (if any), rating of questionnaires (self or caregiver), the prevalence of sleep abnormality, and the effect of the pandemic on sleep duration and sleep quality. Efforts were made to prevent duplication of data.
Two authors independently assessed the quality of the included studies using a standardized Joanna Briggs Institute (JBI) critical appraisal instrument, the JBI Critical Appraisal Checklist for Analytical Cross-sectional Studies [6,7]. Any disagreement between two authors in assessment was resolved by discussion with third author.
2.6. Data synthesis and statistical analysis
Data were extracted using Microsoft Excel and analyzed through R studio with Metaprop and Metafor packages. The study characteristics were presented in tables using descriptive statistics and described narratively. The pooled prevalence was presented as proportions and 95% confidence interval (CI), whereas the pooled estimates for other outcomes were presented as risk ratio (RR) along with CI. We used a random-effect model, assuming that the variations in the frequency of the outcomes across the different studies. The statistical heterogeneity was calculated using I2 method with p-value. Also, an attempt was made to assess the presence of publication bias.
3. Results
3.1. Study selection
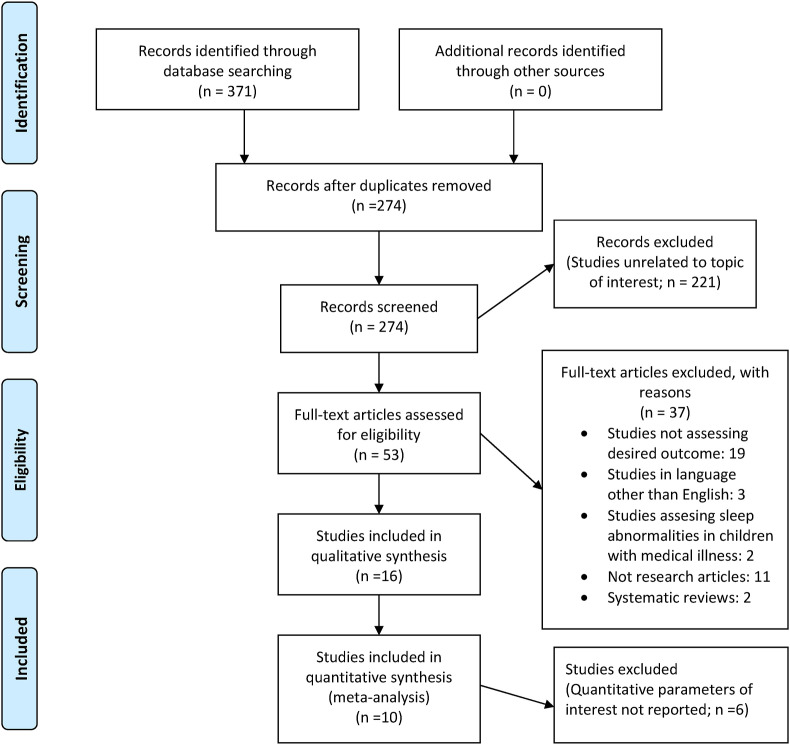
The initial electronic search identified a total of 371 articles. After removing 97 duplicates, the remaining 274 citations were screened for eligibility (Fig. 1 ). Of these, 221 were unrelated to the topic of interest and were excluded. The full texts of 53 potentially relevant articles were evaluated of which 16 articles [[8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23]] fulfilled the study selection criteria and were included for the review. Ten studies reporting the parameters of interest quantitatively were included in the meta-analysis (quantitative synthesis for different variables). Six studies could not be included in quantitative synthesis since they did not report parameters of interest quantitatively.
Fig. 1.
PRISMA flow diagram.
3.2. Methodological quality of included studies and publication bias
Of the 16 studies, all studies failed to provide adequate answers to one of the questions of the JBI critical appraisal tool (supplementary table 2). All studies failed to reliably evaluate the exposure (ie confinement) since most of them were online surveys. None of the studies assessed the strictness of confinement (exposure) measures (whether children/family could go out to a neighbour's place or were confined to home) which were being followed during the study period. Since very few studies were eligible for meta-analysis for each variable [three studies for pooled prevalence of any sleep disturbance (including two studies for pre and post pandemic comparison) [8,9,18], four studies for change in sleep quality/duration [10,11,15,17], four studies for prevalence of children not meeting sleep recommendation[13,16,18,19], sensitivity analysis and publication bias assessment could not be done.
3.3. Study designs and scales used
Fourteen studies [[8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21]] evaluated healthy children while two were conducted in children with behavioral disorders [22,23]. Among the studies included in the review, 12 were cross-sectional while four were longitudinal studies. There was a comparator arm in four studies. Almost all the studies were online surveys. Specific questionnaire for the respective studies was designed in five studies whereas various pre-existing scales such as Sleep Disturbances Scale for Children (SDSC), Pittsburgh Sleep Quality Index (PSQI), Canadian Health Measures Survey, Brief Infant/Child Sleep Questionnaire, and Children's Sleep Habit Questionnaire (CSHQ) were used in 11 studies. Sleep was the primary parameter of assessment in nine studies [[8], [9], [10],12,17,18,20,22,23], whereas, in seven studies, sleep was assessed as part of health-related or movement or lifestyle behavior or depression correlates [11,[13], [14], [15], [16],19,21].
3.4. Summary of the included studies
3.4.1. Healthy pre-schoolers
A Chinese study by Liu et al. assessed the sleep pattern in pre-schoolers (aged 4–6 years) as rated by 1619 caregivers on the Children's Sleep Habit Questionnaire (CSHQ) and compared it with a similar cohort from the year 2018 [8]. During the pandemic, children had significantly delayed bedtime and waketime, both during weekdays and weekends and the total duration of sleep decreased by 7 min during weekends and increased by 10 min during weekdays. Surprisingly, the prevalence of overall sleep disturbances reduced during the outbreak (Table 1 ). Bedtime resistance, delays in sleep onset, sleep anxiety, parasomnias, night-time awakenings, sleep-disordered breathing, and daytime sleepiness improved during the outbreak. This study also concluded that a harmonious family environment, good dietary practices, communication between parent–children, and less electronic media use were associated with better sleep outcomes.
Table 1.
Summary of the included studies on sleep in healthy children.
| S no. | Author, country | Time of the study | Participants | Scales for sleep | Study design | Comparator | Prevalance of sleep disturbance | Sleep quality | Sleep duration | Other results |
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-schoolers | ||||||||||
| 1. | Liu et al. [8], China | February 17–19, 2020 (Home confinement measures in place) |
1619 caregivers of presechooler, aged 4–6 years) | Children's Sleep Habit Questionnaire (CSHQ) | Cross sectional, online survey (WeChat) | Sociodemographically similar sample of preschoolers in 2018 | CSHQ score>41: 900/1619 (55.6%)in COVID-19 sample and 339/436 (77.7%) in 2018 sample | CSHQ total and subscale scores were all significantly lower in the COVID-19 sample | During COVID-19 outbreak, there was
|
|
| 2. | Giorgio et al. [9], Italy |
April 1st- 9th, 2020; national lockdown in Italy | 245 mothers of preschool children aged 2–5 years |
Sleep Disturbance Scale for Children (SDSC, Italian version provided by Bruni) |
Cross sectional, Online survey | Retrospective account before the lockdown (in February, 2020) | SDSC score > 39 in 110/245 (44.7%) during the lockdown and 102/245 (41.5%) before lockdown | Total SDSC score did not signifcantly change during lockdown | During COVID-19 outbreak
|
|
| 3. | Zreik G et al. [10], Israel | April 20–30, 2020; after 4 weeks of lockdown in Israel | Mothers of 264 children aged 6–72 months | Brief Infant/Child Sleep Questionnaire Based on child's sleep during the last 2 weeks of home confinement |
Cross-sectional, web based survey | none | Not mentioned | Negative change in 76/264 (29%), improved 32/264 (12%), no change in 59% | Decreased in 92/264 (35%), increase in 66/264 (25%), no change in 40% |
|
| 4. | Carroll N et al. [11], Canada | 20 April 2020 to 15 May 2020 | Parents of 310 children aged 18 months to 5 years | Sleep duration parameter Pittsburgh Sleep Quality Index Qualitative sleep assessment: self-made questionnaire |
Longitudinal family-based cohort, online survey | – | Remained same in (211/310) 68%; Increased in 53/310 (17%) |
|||
| 5. | Dellagiulia A et al. [12]; Italy | Feb 25- March 25; Lockdown in place |
37 mothers of preschool children aged 3–6 years | Questionnaire investigating trajectory of sleep duration, sleep quality and bed-time routine administered twice a day for 30 days | Longitudinal study | – | Piecewise growth curve with a linear and decreasing pattern from first day of study till March 11with subsequent stablization | Quadratic pattern with decrease and then stabilization of this pattern of decrease | ||
| Children and adolescents | ||||||||||
| 1. | Guerrero et al. [13], Canada | April 2020, containment measures in place | A national sample of 1472 Canadian parents of children (5–11 y; N = 693) and youth (12–17 years; N = 779) | A 1-item measure taken from the Canadian Health Measures Survey. Duration of sleep/24 h in last 1 week was enquired. | Cross sectional, online survey | – | Not mentioned | Not mentioned | 426/1472 (28.9%) did not meet sleep duration recommendation | The adherence group included those with household annual income ≥100,000 CAD and whose parents reported a slight increase in their child's sleep duration since COVID-19 |
| 2. | Moore et al. [14], Canada | April 2020, containment measures in place | Same as study by Guerrero et al. | Same as study by Guerrero et al. | Cross sectional, online survey | 208/690(30.1%) children aged 5-13y and 216/774 (27.9%) youth (14-17y) did not meet sleep duration recommendations had longer sleeping hours than boys | Improvement in sleep time and quality was associated with
|
|||
| 3. | Mitra R et al. [15], Canada | April 2020, containment measures in place | Same as study by Guerrero et al. | Same as study by Guerrero et al. | Cross sectional, online survey | Decrease in 209/1472(14%); Increase in 251/1472(17%). However the quantum of change or in abnormal range not specified | Increased in 609/1472 (41.4%); Decreased in 101/1472 (6.9%) | Children with decreased outdoor activities had increased sleeping time and decrease in sleep quality. | ||
| 4. | Medrano M et al. [16]; Spain | At end of March 2020, COVID-19 confinement measures in place | Children aged 8–16 years (55 girls) enrolled in MUGI project who agreed to participate (N = 113) | Sleep time was calculated on the basis of wake-up time and bedtime from the daily log of each child | Longitudnal online survey with two time points | Timepoint before confinement September–December 2019 (N = 291) |
Not meeting sleep recommendation (<8 or >9 h/d):96/108 (88.9%) during weekdays and 102/108 (94.4%) during weekends; sleep duration increased on both during weekdays and weekend | |||
| 5. | Baptista AS et al. [17], Brazil and Portugal | April 24–26, 2020; social distancing measures in place | Parents/caregivers of 3- to 15-year-old children (N = 253); 50.2% from Brazil | Sleep Disturbances Scale for Children | Cross-sectional online questionnaire | – | Change in sleep quality was assessed. Poorer sleep quality in 108/253 (42.7%) | Sleep breathing disorders, sleep-wake transition disorders, and disorders of excessive somnolence were associated with poor oral hygiene | ||
| 6. | Zhou SJ et al. [18], China | March 8th – 15th, 2020; Lockdown in place |
11,835 adolescents and young adults aged 12–29 years from 21 provinces; Self- rated, School going adolescents: 7736 |
Pittsburgh Sleep Quality Index (PSQI) for sleep quality during the previous month based on 7 components. |
Cross-sectional, Online survey, Wenjuanxing platform | – | Sleep disturbance: 4283/7736 (55.4%), insomnia:1693 (21.9%), those using sleep medication: 84/7736 (1.1%); | Bad or poor sleep quality: 818/7736 (10.6%) Sleep efficiency< 85%: 1528/7736 (19.8%); sleep latency > 30 min: 711/7736 (9.19%); daytime dysfunction:4065/7736 (52.6%) |
No more than 7 h: 2896/7736 (37.4%); More than 9 h: 765/7736 (9.9%) |
|
| 7. | Zhou J et al. [19], China | Feb 20–27, 2020 (Home confinement measures in place) | 4805 female adolescents; 11–18) years; self | Sleep duration per day | Cross sectional online survey (WeChat) | <6 h: 218 (4.5%) 6–8 h: 2854 (59.45%) >8 h/day: 1733 (36.1%) |
Sleep was assessed as a part of depression correlates. Adolescents with sleep duration<6 h had significantly higher odds of suffering from depression on univariate and multivariate logistical regression analyses | |||
| 8. | AMHSI Research team [20]; USA and Israel | March 1 to June 15, 2020; stay at home period of ≥1 month | 1142 adolescents aged 15–18 y. | Daily logs, the sleep-wake patterns questionnaire, phone/Zoom interviews | Longtudinal online survey | Evening bedtime unchanged: 18.6%; was later (“owls”) in 66.1%. Morning getup time unchanged in12.6% and became late (“owls”) in 83.3% |
|
|||
| 9. | Lopez- Bueno et al. [21]; Spain | March 22-May 10, 2020; national confinement in place | 516 parents of 860 children and adolescents aged 3–16 years | Sleep time/day | Cross sectional; online web-form | Before the confinement (retrospective questioning) | Sleep time tended to slightly increase during the confinement. The subgroup of younger children had more sleep hours compared with older ones. | |||
Similarly, Giorgio et al. reported delayed bedtime and waketime during the COVID -19 pandemic as rated by 245 mothers of pre-school children (age 2–5 years) [9]. However, the proportion of children with sleep difficulties remained almost the same before and during the lockdown. It was also seen that the sleep quality of mothers affected the sleep quality of children.
Another study by Zreik et al. reported that mothers of children (aged 6–72 months) found that the sleep quality worsened in 29% of children and improved in 12% while 59% of children had no change [10]. Also, sleep duration decreased in 35% of children during home confinement. It was also observed that maternal COVID-19 anxiety correlated positively with the child's sleep latency while negatively with the child's sleep duration.
Carroll N et al. assessed health behaviors during the pandemic in families with young children and found that sleep duration did not change in two-third of children while it increased in 17% and decreased in 15% [11]. The average sleep duration for children was found out to be 11 h per night.
Dellagiulia A et al. assessed the sleep trajectory of pre-schoolers over 30 days from the start of lockdown by questioning 31 Italian mothers [12]. A quadratic pattern with decrease and then stabilization of this pattern of decrease in sleep duration was observed.
3.4.2. Healthy children and adolescents
Three studies on the same study sample of 1472 Canadian parents of children aged 5–17 years assessed the impact of the COVID-19 pandemic and containment measures on movement behaviors in children (based on adherence to the 24-h movement guidelines). They also evaluated the determinants of this impact. The 24-h movement guidelines provide sleep recommendations for two age groups- 5–13 years (9–11 h per day) and 14–17 years (8–10 h per day of uninterrupted sleep). Guerrero et al. reported that 71.1% of children met these sleep guidelines during the pandemic [13]. Besides, parents' ability to control the screen time, increase in physical activity or outdoor time, being a boy, and parents’ age younger than 43 years were the factors promoting the adherence to 24-h movement guidelines. Moore et al. described that girls had longer sleeping hours than boys in both age groups [14]. Mitra et al. studied the role of neighborhood environment on the movement behaviors [15]. It was seen that the cluster of children with decreased outdoor activities had a large decline in total physical activity and increased screen time. Although they slept more than those with increased outdoor activities, their sleep quality declined by a small amount. Sleep duration increased in 41.4% of the study population; 27.1% in children and 54.0% in youth. Sleep quality decreased in 14.2% of the study population.
A longitudinal study by Medrano M et al. assessed sleep time along with physical activity (PA), screen time, and adherence to the Mediterranean diet during the pandemic [16]. They found an increase in sleeping hours in children (aged 8–16 years) both during weekdays and weekends. During the confinement, around 88.9% and 94.4% didn't meet sleep recommendations on weekdays and weekends respectively.
In a cross-sectional study on 3- to 15-year-old children, Baptista AS et al. found that 72.2% of parents reported changes in child's routine during the pandemic and 42.7% of parents reported worsening of sleep quality while 3.2% reported improvement [17]. Interestingly, this study further added that several sleep disorders like sleep-wake transition disorders, sleep breathing disorders, etc. during the pandemic were associated with poor oral hygiene.
Zhou SJ assessed sleep problems and their correlates in Chinese adolescents and young adults (aged 12–29 years) during the pandemic and containment [18]. Although the study groups were not based on specified age cut-offs, high school students constituted of 7736 students (presumed to be adolescents). The prevalence of insomnia was 21.9% in school-going adolescents. Junior high school students slept better. The risk factors for insomnia symptoms in adolescents and young adults included female gender, depression, and anxiety. Those with good knowledge about the pandemic, more optimistic projections about COVID-19, better social support systems, and those experiencing a lesser impact of the pandemic on study and life, had lower rates of sleep abnormalities.
A large cross-sectional study by Jiaojiao Zhou et al. evaluated depression correlates (including sleep abnormalities) during the pandemic in 4805 female adolescents (11–18 years old) [19]. Nearly 40% of the study population was shown to have syndromal depression. Abnormal sleep duration ie < 6 h/day or >8 h/day was seen in 4.5% and 36.1% of the study population respectively. Furthermore, sleep duration of <6 h/day, and physical exercise <30 min/day were found to be independent risk factors for depression.
A longitudinal study by AMHSI Research Team studied the differences in sleep (in 1142 adolescents) during the normal conditions and home confinement [20]. Two months into the lockdown, the evening bedtime and morning getup time remain unchanged in 18.6% and 12.6% adolescents respectively. The morning getup time and evening bed time (owls) became late in 83.3% and 66.1% of the study population respectively. The most significant changes in sleep timing occurred during the first week of stay-at-home.
A Spanish study on health-related behavior in children (as reported by parents) concluded that sleep time tended to slightly increase during confinement. The subgroup of younger children had more sleep hours compared with older ones [21].
3.4.3. Children with pre-existing behavioral abnormalities
Çetin FH et al. evaluated the relationship between sleep problems/chronotype (individual's preferred sleep-wake schedule) and symptom severity in 76 children with ADHD during the COVID-19 pandemic [23]. CSHQ scores of the eveningness type group differed significantly from the non-eveningness type group. The eveningness type group reported higher trauma scores, greater sleep problems, and worse ADHD symptoms during the pandemic. Also, sleep problems were found to have a full mediation effect on the relationship of trauma reactions and chronotype with ADHD symptom severity.
Similarly, the study by Türkoğlu et al. assessed the relationship between chronotype, sleep, and autism symptom severity during the COVID-19 pandemic and home confinement period in 46 children with autism (aged 4–17 years) [22]. Parents rated that their children had more bedtime resistance, more sleep anxiety, parasomnias, night awakenings, delay in falling asleep, and feeling more sleepy during the daytime despite the increase in total duration of sleep in the post-confinement period. When compared with two months before confinement, the differences were statistically significant. Also, during the quarantine period, it was seen that chronotype scores had a significant effect on sleep problems and autism symptom severity. Sleep problems also directly affected autism severity scores. This study concluded that during the home confinement period, children with ASD had higher sleep problems and chronotype scores which had a direct influence on the severity of autism symptoms.
3.4.4. Quantitative sleep outcomes
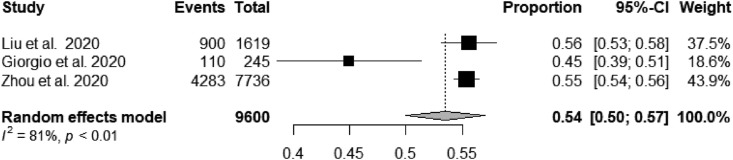
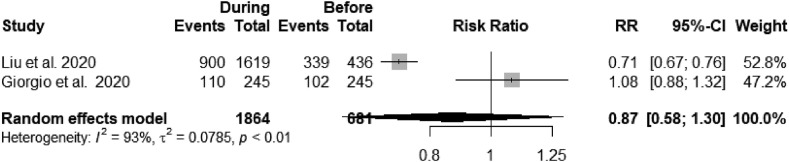
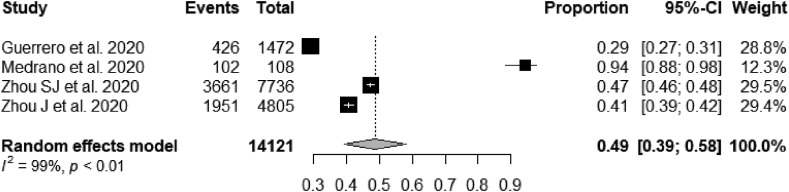
Since different reporting measures had been used for sleep in different studies, the results of all studies couldn't be pooled. The pooled prevalence of any sleep disturbance in children during the COVID-19 pandemic was 54% (95%CI: 50–57%) (Fig. 2 ) [8,9,18]. When comparing the prevalence of sleep disturbances in preschool children during and before the pandemic, the prevalence was lower during the pandemic (RR = 0.87; 95% CI: 0.58–1.30) but this was not statistically significant (Fig. 3 ) [8,9]. The pooled prevalence of children with worsening of sleep quality was 27% (95% CI: 12–49%) and with improvement in sleep quality during the pandemic was 10% (95%CI: 5–19%) [10,15,17]. The pooled prevalence for children with reduced sleep duration during the pandemic was 16% (95%CI: 5–40%) [10,11,15]. The pooled prevalence of children not meeting sleep duration recommendation was 49% (95%CI: 39–58%) (Fig. 4 ) [13,16,18,19].
Fig. 2.
Forest plot for the frequency of any sleep disturbance in children during the COVID-19 pandemic and home confinement.
Fig. 3.
Forest plot for any sleep disturbance in children (preschool) during and before the COVID-19 pandemic and home confinement.
Fig. 4.
Forest plot for the proportion of children not meeting sleep duration recommendations during the COVID-19 pandemic and home confinement.
4. Discussion
Sleep was probably the only lifestyle behavior that was under individual control even during the home confinement due to the pandemic. However, the rampant psychological concerns and fear probably escalated the sleep problems in adults [24]. New-onset psychological concerns have also been identified in children and adolescents during the pandemic which may be associated with sleep abnormalities [25]. This systematic review and meta-analysis brings forth the burden and spectrum of sleep abnormalities in children during the COVID-19 pandemic.
Before the pandemic, different studies have reported different prevalence of sleep problems in typically developing children across different age groups with a range of 25–50% in pre-schoolers to 6–37% school children and 40% in adolescents [[26], [27], [28], [29]]. With sleep problems reported in nearly 25% of typically developing children otherwise, the pooled prevalence observed (more than two times) during the pandemic is alarming [30]. However, the pooled prevalence was lower in pre-schoolers as compared with pre-pandemic prevalence (although not statistically significant) [8,9]. The sleep duration recommendations were not met in nearly half of the children enrolled in the included studies which is also worrisome. Also, an increase in sleep problems was reported in children with neurobehavioral disorders like ASD and ADHD (eveningness type) which have been reported to have a higher burden of sleep problems even in the pre-pandemic era [31,32].
Preschool children behaved differently in context to sleep during the pandemic when compared to older children and adolescents [8]. There are many underlying factors which may be responsible for the contrasting outcome in pre-schoolers. Preschool children spend the majority of their time at home and usually don't have large social friend groups as in school. Besides, they are too puerile to understand or get affected by any viral disease or calamity. Their comfort zone with family at home is their sole need which is what happened during the first 6 months of the COVID-19 pandemic. With work from home and home confinement regulations in place, the family time increased.
However, the school-going children and adolescents could understand the prevailing conditions in the world. They were impacted by the closure of schools and recreational activities and distancing from peers. All these factors directly or indirectly affected their sleep. Besides, the relaxation due to the closure of schools resulted in delayed bedtime and wake-up time during the initial phase of pandemic and home confinement. The delayed wakeup time might have been useful for parents and caregivers who could cluster most of the household chores while the child was asleep. Also, the fear of illness, psychological stress, and sleep issues in caregivers might have contributed to poor sleep quality in children and adolescents.
A recent meta-analysis by Jahrami H et al. on sleep problems among the general population concluded that sleep problems affected 40% of the adult population during the COVID-19 pandemic [24]. However, this study primarily described the adult and elderly populations while children and adolescents were not taken into account in their meta-analysis. The authors reported that maximum sleep problems were encountered during the active COVID phase when someone got infected. This was presumed to be due to the nature of the disease as the core symptoms of the disease involve coughing, fever, and difficulty in breathing, all of which have been associated with sleep problems. But this salient observation was not seen in our study which did not take into account the studies on the sleep of SARS-CoV-2 infected children.
The COVID-19 pandemic has forced the world into unwanted territories with various restrictions. This has left the economies devastated, and people scared for themselves and their dear ones. With such an unprecedented situation staring at us, it is unjustifiable to not give due importance to sleep as healthy sleep is the best rejuvenation associated with numerous benefits like physical wellbeing and robust functioning of the immune circuitry. Besides, it is the primary determinant of mental and emotional health allaying anxiety, stress, and depression. Also, it is associated with diverse developmental consequences [33]. Even the WHO recommendations for children to cope with COVID-19 suggest maintenance of regular sleep hygiene and day-to-day routine [34]. The spread of information about positive sleep habits and the ill-effects of poor sleep quality is of utmost importance.
The index study is the first systematic review capturing sleep in children during the COVID-19 pandemic. However, very few studies were eligible for inclusion and most of the included studies were not high quality and assessed sleep based on parental reporting who were themselves under psychological stress due to the pandemic. Besides, the included studies were conducted in different sample populations and had significant heterogeneity making the generalizability of this review debatable. Also, this review did not assess the published literature on the sleep of children with COVID-19 or other medical illnesses during the pandemic. These children are expected to have a higher burden of sleep problems.
5. Conclusion
The prevalence of sleep problems in children and adolescents during the COVID-19 pandemic is alarming. Pre-school children had a trend towards relatively fewer sleep disturbances in comparison with pre-pandemic times. Besides, the proportion of children with worsening sleep quality during the pandemic was nearly three times the proportion of those with improvement. Sleep duration recommendations were not met in nearly half of healthy children during the pandemic. However, these findings need to be seen in light of limited literature on the topic, few included studies done in heterogenous populations, and dubious quality of inferences drawn from these studies which were predominantly online surveys. Although the future neurobehavioral consequences of sleep problems observed during the pandemic are yet to be determined, these figures might serve as an impetus for formulating recommendations for prophylactically managing sleep during such exceptional times of crisis.
Author credit statement
MS and SA contributed by conception, literature search, writing initial draft, and statistical analysis.
PM contributed by literature search, writing initial draft, and critical review of manuscript.
LS contributed by writing initial draft and critical review of manuscript MB contributed by critical review of manuscript for intellectual content.
All authors approved the final version of manuscript to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
None.
Acknowledgement
None.
Footnotes
The authors have no conflict of interest to disclose with regard to this article.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2021.06.002.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sleep.2021.06.002.
Conflict of interest
The following is the supplementary data related to this article:
Multimedia component 3
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Coronavirus disease (COVID-19) World health organization. [Internet]Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 2.Gupta J., Madaan P., Chowdhury S.R., et al. COVID-19 and pediatric neurology practice in a developing country. Pediatr Neurol. 2020 Dec 1;113:1. doi: 10.1016/j.pediatrneurol.2020.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castagnoli R., Votto M., Licari A., et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatrics. 2020 Sep 1;174(9):882–889. doi: 10.1001/jamapediatrics.2020.1467. [DOI] [PubMed] [Google Scholar]
- 4.Mustafa N.M., A Selim L. Characterisation of COVID-19 pandemic in paediatric age group: a systematic review and meta-analysis. J Clin Virol: Off Pub Pan Am Soc Clin Virol. 2020;128:104395. doi: 10.1016/j.jcv.2020.104395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gulati S., Gupta J., Madaan P. COVID-19 and child neurology care. Neurol India. 2020;68(4):952. doi: 10.4103/0028-3886.293484. [DOI] [PubMed] [Google Scholar]
- 6.Moola S., Munn Z., Tufanaru C., et al. In: JBI manual for evidence synthesis. Aromataris E., Munn Z., editors. JBI; 2020. Chapter 7: systematic reviews of etiology and risk.https://wiki.jbi.global/display/MANUAL/Chapter+7%3A+Systematic+reviews+of+etiology+and+risk [Internet] Available from: [Google Scholar]
- 7.Ma L.-L., Wang Y.-Y., Yang Z.-H., et al. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Military Med Res. 2020 Feb 29;7(1):7. doi: 10.1186/s40779-020-00238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Z., Tang H., Jin Q., et al. Sleep of preschoolers during the coronavirus disease 2019 (COVID-19) outbreak. J Sleep Res. 2020 Jul 27:e13142. doi: 10.1111/jsr.13142. [DOI] [PubMed] [Google Scholar]
- 9.Di Giorgio E., Di Riso D., Mioni G., et al. The interplay between mothers' and children behavioral and psychological factors during COVID-19: an Italian study. Eur Child Adolesc Psychiatr. 2020 Aug 31:1–12. doi: 10.1007/s00787-020-01631-3. ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zreik G, Asraf K, Haimov I, Tikotzky L. Maternal perceptions of sleep problems among children and mothers during the coronavirus disease 2019 (COVID-19) pandemic in Israel. J Sleep Res. n/a(n/a):e13201. [DOI] [PMC free article] [PubMed]
- 11.Carroll N., Sadowski A., Laila A., et al. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients. 2020 Aug;12(8):2352. doi: 10.3390/nu12082352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dellagiulia Antonio, Lionetti Francesca, Fasolo Mirco, et al. Early impact of COVID-19 lockdown on children's sleep: a 4-week longitudinal study. J Clin Sleep Med. 16(9):1639–1640. [DOI] [PMC free article] [PubMed]
- 13.Guerrero M.D., Vanderloo L.M., Rhodes R.E., et al. Canadian children's and youth's adherence to the 24-h movement guidelines during the COVID-19 pandemic: a decision tree analysis. J Sport Health Sci. 2020 Jul 1;9(4):313–321. doi: 10.1016/j.jshs.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moore S.A., Faulkner G., Rhodes R.E., et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Activ. 2020 06;17(1):85. doi: 10.1186/s12966-020-00987-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mitra R., Moore S.A., Gillespie M., et al. Healthy movement behaviours in children and youth during the COVID-19 pandemic: exploring the role of the neighbourhood environment. Health Place. 2020 Aug 29;65:102418. doi: 10.1016/j.healthplace.2020.102418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Medrano M, Cadenas-Sanchez C, Oses M, Arenaza L, Amasene M, Labayen I. Changes in lifestyle behaviours during the COVID-19 confinement in Spanish children: a longitudinal analysis from the MUGI project. Pediatric Obesity. n/a(n/a):e12731. [DOI] [PubMed]
- 17.Baptista A.S., Prado I.M., Perazzo M.F., et al. Can children's oral hygiene and sleep routines be compromised during the COVID-19 pandemic? Int J Paediatr Dent. 2021;31(1):12–19. doi: 10.1111/ipd.12732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou S.-J., Wang L.-L., Yang R., et al. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020;74:39–47. doi: 10.1016/j.sleep.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou J., Yuan X., Qi H., et al. Prevalence of depression and its correlative factors among female adolescents in China during the coronavirus disease 2019 outbreak. Glob Health. 2020 28;16(1):69. doi: 10.1186/s12992-020-00601-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rome O., Sinai L., Sevitt R., et al. Owls and larks do not exist: COVID-19 quarantine sleep habits. Sleep Med. 2021;77:177–183. doi: 10.1016/j.sleep.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.López-Bueno R., López-Sánchez G.F., Casajús J.A., et al. Health-related behaviors among school-aged children and adolescents during the Spanish covid-19 confinement. Front Pediatr. 2020 Sep 11;8 doi: 10.3389/fped.2020.00573. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7516648/ [Internet]Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Türkoğlu S., Uçar H.N., Çetin F.H., et al. The relationship between chronotype, sleep, and autism symptom severity in children with ASD in COVID-19 home confinement period. Chronobiol Int. 2020 Aug 4:1–7. doi: 10.1080/07420528.2020.1792485. 0(0) [DOI] [PubMed] [Google Scholar]
- 23.Çetin F.H., Uçar H.N., Türkoğlu S., et al. Chronotypes and trauma reactions in children with ADHD in home confinement of COVID-19: full mediation effect of sleep problems. Chronobiol Int. 2020 Aug 28:1–8. doi: 10.1080/07420528.2020.1785487. [DOI] [PubMed] [Google Scholar]
- 24.Jahrami H., BaHammam A.S., Bragazzi N.L., et al. Sleep problems during COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17(2):299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Panda P.K., Gupta J., Chowdhury S.R., et al. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: a systematic review and meta-analysis. J Trop Pediatr. 2021;67(1) doi: 10.1093/tropej/fmaa122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blader J.C., Koplewicz H.S., Abikoff H., et al. Sleep problems of elementary school children. A community survey. Arch Pediatr Adolesc Med. 1997 May;151(5):473–480. doi: 10.1001/archpedi.1997.02170420043007. [DOI] [PubMed] [Google Scholar]
- 27.Owens J.A., Spirito A., McGuinn M., et al. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr. 2000 Feb;21(1):27–36. doi: 10.1097/00004703-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Vignau J., Bailly D., Duhamel A., et al. Epidemiologic study of sleep quality and troubles in French secondary school adolescents. J Adolesc Health. 1997 Nov;21(5):343–350. doi: 10.1016/S1054-139X(97)00109-2. [DOI] [PubMed] [Google Scholar]
- 29.Pagel J.F., Forister N., Kwiatkowki C. Adolescent sleep disturbance and school performance: the confounding variable of socioeconomics. J Clin Sleep Med. 2007 Feb 15;3(1):19–23. [PubMed] [Google Scholar]
- 30.Owens J. Classification and epidemiology of childhood sleep disorders. Prim Care. 2008 Sep;35(3):533–546. doi: 10.1016/j.pop.2008.06.003. vii. [DOI] [PubMed] [Google Scholar]
- 31.Mazzone L., Postorino V., Siracusano M., et al. The relationship between sleep problems, neurobiological alterations, core symptoms of autism spectrum disorder, and psychiatric comorbidities. J Clin Med. 2018 May 3;7(5) doi: 10.3390/jcm7050102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tsai M.-H., Hsu J.-F., Huang Y.-S. Sleep problems in children with attention deficit/hyperactivity disorder: current status of knowledge and appropriate management. Curr Psychiatr Rep. 2016 Aug;18(8):76. doi: 10.1007/s11920-016-0711-4. [DOI] [PubMed] [Google Scholar]
- 33.Spruyt K. A review of developmental consequences of poor sleep in childhood. Sleep Med. 2019 Aug;60:3–12. doi: 10.1016/j.sleep.2018.11.021. [DOI] [PubMed] [Google Scholar]
- 34.Sleep guidelines and help during the COVID-19 pandemic. Sleep Foundation. 2021. https://www.sleepfoundation.org/sleep-guidelines-covid-19-isolation [Internet]Available from: [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 3