Abstract
Purpose
To compare food safety knowledge, attitudes, and self-reported practices among medical staff in China before, during, and after the COVID-19 pandemic.
Patients and Methods
The questionnaire was anonymous. All respondents were Chinese medical personnel. A Chi-square contingency table was used to compare the knowledge and attitudes of Chinese medical staff before, during and after COVID-19. R statistical software (v4.0.0) was used for analysis.
Results
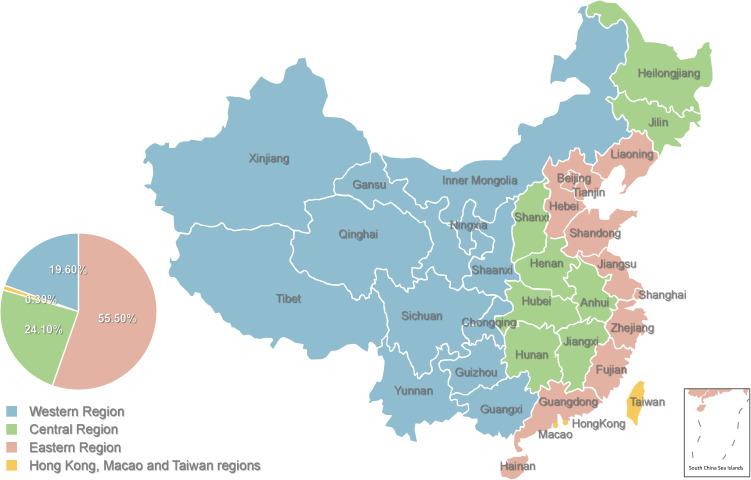
A total of 1431 valid responses (57.3% from female respondents) were included in our analysis. Medical professionals were geographically distributed as follows: eastern China, 55.5%; central China, 19.7%; western China, 24.1%; Hong Kong, Macau, or Taiwan, 0.05%. Medical professionals reported that they paid greater attention to food safety after the COVID-19 pandemic compared with before the epidemic. Self-reported knowledge of and attitudes toward food safety among medical staff were significantly different before, during, and after the COVID-19 pandemic (both P<0.001).
Conclusion
After the COVID-19 pandemic, medical professionals paid increasing attention to food safety, which is a clinically important change. Because medical professionals can influence public understanding of food safety, their increased attention to this subject may enable them to promote food safety knowledge more actively in their work. This may in turn promote a better understanding of food safety and protect the health of the general public.
Keywords: food safety, medical staff, COVID-19, questionnaire
Introduction
At the end of 2019, an outbreak of an infectious, acute respiratory disease caused by a novel SARS-CoV-2 variant (COVID-19) broke out in Wuhan, China. This outbreak severely affected the normal work and life of residents, threatened the health of the general population, and posed severe challenges to China.1,2 The first reports suggested that the emergence of COVID-19, which led to a pandemic, probably resulted from human consumption of domestic animals or wild captive animals, such as bats, snakes, marmots, or civet cats.3–5 Although it has not been proven that the spread of COVID-19 was caused by food, food safety has once again become a focus of attention in public health. In an online survey in the Philippines, which included a total of 751 people, suggested that both government and nongovernmental organizations should work together to ensure that the general public are sufficiently educated in important food safety concepts and effective methods of handling food at home, thus becoming advocates of safer food practices.6
In addition, particularly during the COVID-19 pandemic, traceability of food products, which enables their recall or withdrawal if deemed unsafe, has a vital role in ensuring food quality and safety. The Internet of Things (IoT) provides tools to monitor environmental conditions, product quality, and product availability in food production, thus augmenting traceability. A retrospective solution maximizes food safety, reducing the amounts of bacteria, fungi, and parasites in the frozen meat supply chain during the COVID-19 pandemic.7 At the same time, medical professionals on the front line of the COVID-19 pandemic8 are required to perform high-risk tasks that expose them to sources of infection.9 In the face of COVID-19 pandemic, the dissemination of food safety concepts among the general public is therefore important.10 Implementing human resource management strategies will improve mental health, job satisfaction, productivity, motivation, and workplace health and safety among medical staff during the COVID-19 pandemic11 and improve the attitudes of the general population towards food safety.
The acceptance of food safety principles also reflects general views on disease risk, as well as the general public’s attitudes and behavior patterns in the context of health, which are critical to the success of immunization programs, including for COVID-19. Good personal nutrition, which is influenced by an individual’s understanding of healthy eating concepts, may also reduce risk of infection and improve disease prognosis.12 Previous studies have shown that clinical specialists are an important source of food safety knowledge for patients, and communication between specialists and patients may therefore improve patients’ awareness of food safety. Individuals who believe they are at risk are more likely to listen to the dietary and food safety advice of medical professionals.13 However, medical staff will also have varying levels of knowledge on food safety, which in turn may limit the understanding of those in their care.14,15 At the same time, it is necessary to emphasize fact-based, people-oriented, and collaborative responses among global media outlets with regards to reporting on COVID-19, encouraging them to prioritize reporting on core public health issues, including methods of effectively attenuating or preventing the spread of COVID-19.16 This should include information on food safety. Given the importance of food safety in ensuring good public health, it is essential to know to what extent the pandemic has affected understanding of this topic among medical professionals, and which factors affect their acceptance of food safety concepts. This information is crucial for the future dissemination of food safety knowledge in China after the COVID-19 pandemic.
Previous studies have shown that public health organizations and initiatives and social media have an indispensable role in providing accurate health information during the COVID-19 pandemic,17 which may include food safety. Improving knowledge, attitudes, and behaviors among medical professionals on this subject may provide benefits to society as a whole by enhancing their food safety knowledge.
In this study, we therefore investigated food safety knowledge, attitudes, and behavior patterns among Chinese medical professionals before, during and after the COVID-19 pandemic. We analyzed the roles of these high-risk groups in providing food safety education and the extent to which COVID-19 has affected their food safety knowledge, attitudes, and behavior patterns on food safety.
Materials and Methods
Study Design
We conducted an online survey Questionnaire Star (Changsha Ranxing Information Technology Co., Ltd., Hunan, China), China’s largest online survey platform, which opened at 13:34:31 on July 28th, 2021, and closed at 19:22:05 on August 10th, 2021. Similar to Qualtrics, SurveyMonkey, or CloudResearch in Europe and the United States, Questionnaire Star provides online questionnaire design and survey functions suitable for research institutions, enterprises, and individuals. An anonymous cross-sectional online survey was conducted using a stratified random sampling method. Personal information from more than 2.6 million respondents was confirmed in the Questionnaire Star sample database. Therefore, it was possible to provide an authentic, diverse, and representative sample.
Target Population
This study targeted Chinese medical professionals living in China. A randomized sampling procedure, in which participants were stratified by age and location, was used to match the Chinese adults included in the Questionnaire Star sample base.
Questionnaire Content Design
Demographic information, including age, gender, region, and income, were collected from respondents, in addition to the main content of the questionnaire (Supplementary Material 1). The questionnaire had three sections on food safety knowledge before, during, and after the pandemic, respectively. The contents of each part of the survey (as written) are as follows:
Food safety is a serious problem for patients with weakened immune functions (such as confirmed COVID-19).
(1) Many of my patients may be at risk owing to poor food safety.
(2) It is important to ensure that patients receive food safety education.
(3) Food safety education is a part of the duties of doctors and nurses.
(4) I want to understand the risks associated with poor food safety for my patients.
(5) My patients are more interested in learning and being educated about food safety now than they were before the COVID-19 pandemic.
(6) I am willing to have a short (3 minutes) conversation with my patients to help them understand food safety concepts.
(7) Educating patients on food safety will reduce foodborne illness.
(8) My patients are better able to follow the food safety advice I provide on preventing foodborne illness now than they were before the COVID-19 pandemic.
(9) I am satisfied with the general knowledge of food safety education.
(10) I am more willing to give advice on food safety now than I was before the COVID-19 pandemic.
(11) My patients consider me a valuable resource for food safety education.
(12) In the post-COVID-19 era, a complete management system must be established for food safety.
(13) In the post-COVID-19 era, a complete emergency response plan must be established.
(14) In the post-COVID-19 era, a complete food traceability system must be established.
Respondents were stratified into those from western, central, and eastern regions of China, and further stratified according to economic level.
Statistical Analysis
We compared whether the epidemic has affected the extent of differences in attitudes and perceptions of food safety among Chinese medical professionals and what factors have influenced their acceptance of food safety knowledge. Chi-square tests were used to analyze the differences between groups. Frequencies were expressed as percentages. Differences with an associated P<0.05 were considered statistically significant. Statistical analyses were conducted using R statistical software (v3.6.1; http://www.Rproject.org).
Results
Demographic Information
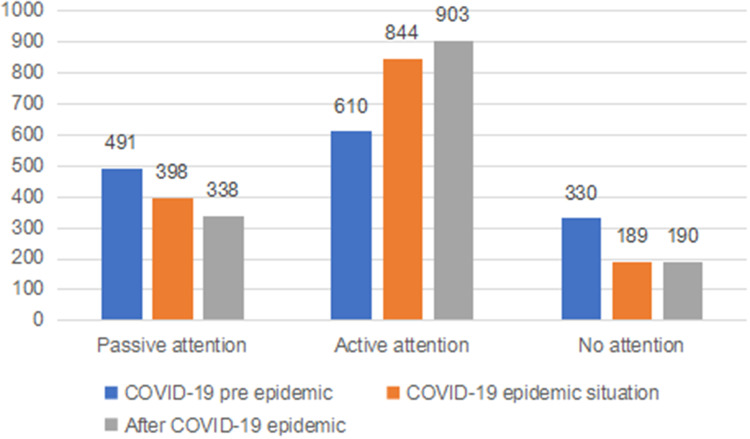
A total of 1451 individuals responded to the questionnaire. 20 invalid responses (which lacked basic information or contained incorrect data) were eliminated, leaving a total of 1431 valid responses from medical professionals that were included in the study (Table 1). Respondents of our questionnaire were from Eastern China (55.5%), Central China (19.7%), Western China (24.1%), and Hong Kong, Macau, and Taiwan (0.05%) (Figure 1). Men and women accounted for 57.3% and 42.7% of respondents, respectively. Most respondents (96.44%) were aged between 18 and 60 years. Figure 2 shows that more medical professionals actively pay attention to food safety as a result of the COVID-19 pandemic, which therefore had an impact on food safety knowledge.
Table 1.
Sociodemographic Characteristics of Medical Staff Samples
| N (1431) | |
|---|---|
| Gender | |
| Male | 610(42.62%) |
| Female | 821(57.38%) |
| Age | |
| 18–30 | 355(24.80%) |
| 31–40 | 578(40.39%) |
| 41–50 | 343(23.96%) |
| 51–60 | 86(6.00%) |
| 61–70 | 18(12.57%) |
| 71–80 | 51(3.56%) |
| Residential area | |
| Eastern China | 795(55.56%) |
| Central China | 282(19.70) |
| Western China | 346(24.17) |
| Hong Kong, Macau and Taiwan | 8(0.57%) |
| Income (RMB) | |
| 0–20,000 | 330(23.06%) |
| 20,000–50,000 | 159(11.11%) |
| 50,000–150,000 | 575(40.18%) |
| 150,000–500,000 | 352(24.59) |
| >500,000 | 15(1.06%) |
Figure 1.
The respondents of our questionnaire came from Eastern Region, Central Region, Western Region, Hong Kong, Macau and Taiwan, China.
Figure 2.
Distribution of number of people paying attention to food safety knowledge before and after the COVID-19 epidemic.
Knowledge of Food Safety Among Medical Professionals
Differences in the knowledge of food safety between the three periods (before, during and after the COVID-19 pandemic) were all significantly different (P<0.001) (Table 2). A greater number of medical professionals agreed that food safety is a serious issue for patients with weakened immune functions (such as confirmed COVID-19) after the COVID-19 pandemic, and that many patients may face risks associated with food safety, with 127 in agreement before and 189 in agreement after the COVID-19 pandemic.
Table 2.
Comparison of Differences in Perceptions of Food Safety Before and After the COVID-19 Epidemic (p-valueA: Comparison Before and During the COVID-19 Epidemic, p-value B: Comparison After the COVID-19 Epidemic and During the COVID-19 Epidemic)
| Before the COVID-19 Epidemic | During the COVID-19 Epidemic | After the COVID-19 Epidemic | p-valueA | p-valueB | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Passive attention | Active attention | Not paying attention | Passive attention | Active attention | Not paying attention | Passive attention | Active attention | Not paying attention | |||
| Food safety is a serious problem for patients with weakened immune function (such as confirmed COVID-19) | |||||||||||
| Strongly agree | 71 | 137 | 42 | 56 | 181 | 13 | 48 | 189 | 13 | <0.001 (χ2 =24.5) | <0.001 (χ2 =20.2) |
| Agree | 320 | 360 | 170 | 248 | 513 | 89 | 214 | 546 | 90 | ||
| Neutral or no answer | 75 | 73 | 105 | 75 | 98 | 80 | 60 | 116 | 77 | ||
| Disagree | 24 | 37 | 11 | 18 | 49 | 5 | 15 | 49 | 8 | ||
| Strongly disagree | 1 | 3 | 2 | 1 | 2 | 2 | 1 | 3 | 2 | ||
| Many of my patients may be at risk for food safety | |||||||||||
| Strongly agree | 67 | 109 | 31 | 47 | 145 | 15 | 40 | 155 | 12 | <0.001 (χ2 =18.7) | <0.001 (χ2 =24.1) |
| Agree | 330 | 391 | 196 | 274 | 537 | 106 | 225 | 587 | 105 | ||
| Neutral or no answer | 71 | 70 | 76 | 61 | 103 | 53 | 587 | 102 | 55 | ||
| Disagree | 23 | 39 | 25 | 58 | 59 | 13 | 58 | 16 | 58 | ||
| Strongly disagree | 0 | 1 | 2 | 1 | 1 | 2 | 1 | 32 | 2 | ||
| Ensure that patients receive food safety education | |||||||||||
| Strongly agree | 92 | 182 | 52 | 57 | 245 | 24 | 53 | 252 | 21 | <0.001 (χ2 =31.7) | <0.001 (χ2 =33.6) |
| Agree | 356 | 398 | 199 | 293 | 558 | 112 | 240 | 595 | 118 | ||
| Neutral or no answer | 38 | 27 | 68 | 49 | 37 | 47 | 37 | 51 | 45 | ||
| Disagree | 4 | 3 | 9 | 4 | 4 | 4 | 7 | 5 | 4 | ||
| Strongly disagree | 1 | 0 | 2 | 1 | 0 | 0 | 1 | 0 | 2 | ||
| Food safety education is part of the duties of doctors and nurses | |||||||||||
| Strongly agree | 73 | 123 | 44 | 46 | 170 | 24 | 34 | 181 | 25 | <0.001 (χ2 =28.7) | <0.001 (χ2 =19.8) |
| Agree | 312 | 390 | 199 | 246 | 541 | 114 | 218 | 573 | 110 | ||
| Neutral or no answer | 60 | 46 | 57 | 62 | 66 | 35 | 52 | 76 | 35 | ||
| Disagree | 41 | 46 | 23 | 40 | 59 | 11 | 30 | 65 | 15 | ||
| Strongly disagree | 5 | 5 | 7 | 4 | 8 | 5 | 4 | 8 | 5 | ||
| I want to understand the risks of food safety for my patients | |||||||||||
| Strongly agree | 70 | 123 | 40 | 42 | 166 | 25 | 38 | 174 | 21 | <0.001 (χ2 =11.2) | <0.001 (χ2 =20.1) |
| Agree | 371 | 428 | 236 | 303 | 607 | 125 | 257 | 652 | 126 | ||
| Neutral or no answer | 40 | 48 | 45 | 43 | 56 | 34 | 35 | 62 | 36 | ||
| Disagree | 9 | 10 | 7 | 8 | 4 | 4 | 7 | 14 | 5 | ||
| Strongly disagree | 1 | 1 | 2 | 2 | 1 | 1 | 1 | 1 | 2 | ||
| My patient is more interested in understanding and receiving food safety education than before the COVID-19 epidemic | |||||||||||
| Strongly agree | 43 | 100 | 34 | 37 | 125 | 15 | 33 | 130 | 14 | <0.001 (χ2 =18.7) | <0.001 (χ2 =10.4) |
| Agree | 325 | 387 | 187 | 240 | 558 | 101 | 200 | 598 | 101 | ||
| Neutral or no answer | 91 | 79 | 77 | 91 | 104 | 52 | 79 | 116 | 52 | ||
| Disagree | 31 | 42 | 30 | 30 | 54 | 19 | 26 | 56 | 21 | ||
| Strongly disagree | 1 | 2 | 2 | 0 | 3 | 2 | 0 | 3 | 2 | ||
| Educating patients on food safety will reduce foodborne illness | |||||||||||
| Strongly agree | 132 | 190 | 71 | 92 | 268 | 33 | 84 | 279 | 30 | <0.001 (χ2 =20.1) | <0.001 (χ2 =11.6) |
| Agree | 333 | 398 | 218 | 278 | 550 | 121 | 231 | 591 | 127 | ||
| Neutral or no answer | 20 | 15 | 36 | 21 | 18 | 32 | 17 | 24 | 30 | ||
| Disagree | 6 | 7 | 4 | 7 | 8 | 2 | 6 | 9 | 2 | ||
| Strongly disagree | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | ||
| My patients are better able to follow the food safety advice I provided to prevent foodborne illness than before the COVID-19 epidemic | |||||||||||
| Strongly agree | 54 | 89 | 28 | 39 | 121 | 11 | 34 | 127 | 10 | <0.001 (χ2 =14.7) | <0.001 (χ2 =17.2) |
| Agree | 340 | 410 | 212 | 266 | 585 | 111 | 221 | 623 | 118 | ||
| Neutral or no answer | 70 | 80 | 68 | 70 | 93 | 55 | 62 | 107 | 49 | ||
| Disagree | 26 | 29 | 18 | 23 | 42 | 8 | 21 | 43 | 9 | ||
| Strongly disagree | 1 | 2 | 4 | 0 | 3 | 4 | 0 | 3 | 4 | ||
The number of people in agreement with several other statements also increased after the pandemic compared with before, including: “many of my patients may be at risk for food safety” (109 before versus 155 after); “it is important to ensure that patients receive food safety education” (398 before versus 595 after); “food safety education is a part of the duties of doctors and nurses” (109 before versus 155 after); “I want to understand the risks of food safety for my patients” (123 before versus 174 after); “my patients are more interested in understanding and being educated about food safety than before the COVID-19 epidemic” (100 before versus 130 after); “educating patients on food safety will reduce foodborne illness” (190 before versus 279 after); “my patients are better able to follow the food safety advice I provide on preventing foodborne illness now than they were before the COVID-19 pandemic” (89 before versus 127 after).
Attitudes of Medical Professionals Towards Food Safety
Differences in the attitude towards food safety between the three periods (before, during and after the COVID-19 pandemic) were all significantly different (P<0.001) (Table 3). Medical professionals were more satisfied with the general knowledge of food safety education after the pandemic compared with before. Compared with before the COVID-19 outbreak, there was an increased willingness to provide advice on food safety; an increased number of medical professionals agreed that patients consider medical professionals a valuable resource for food safety education; more respondents agreed that a complete management system and traceability system must be established for food safety after the COVID-19 pandemic; a greater number agreed that a complete emergency response plan for food safety should be established after the COVID-19 pandemic; and more medical professionals reported that they were willing to have a short conversation (3 min) with patients to help them understand food safety concepts.
Table 3.
Comparison of Attitudes Towards Food Safety Before, After and During the COVID-19 Epidemic (p-valueA: Comparison Before and During the COVID-19 Epidemic, p-valueB: Comparison After the COVID-19 Epidemic)
| Before the COVID-19 Epidemic | During the COVID-19 Epidemic | After the COVID-19 Epidemic | p-valueA | p-valueB | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Passive Attention | Active Attention | Not Paying Attention | Passive Attention | Active Attention | Not Paying Attention | Passive Attention | Active Attention | Not Paying Attention | |||
| I am satisfied with the general knowledge of food safety education | |||||||||||
| Strongly agree | 32 | 62 | 20 | 19 | 85 | 10 | 20 | 86 | 8 | <0.001 (χ2 =22.7) | <0.001 (χ2 =18.6) |
| Agree | 323 | 422 | 211 | 255 | 586 | 115 | 209 | 632 | 115 | ||
| Neutral or no answer | 67 | 55 | 62 | 61 | 78 | 45 | 54 | 86 | 44 | ||
| Disagree | 69 | 68 | 35 | 63 | 92 | 17 | 55 | 96 | 21 | ||
| Strongly disagree | 0 | 3 | 2 | 0 | 3 | 2 | 0 | 3 | 2 | ||
| I am more willing to advise on food safety than before the COVID-19 outbreak | |||||||||||
| Strongly agree | 48 | 94 | 28 | 35 | 122 | 13 | 27 | 130 | 13 | <0.001 (χ2 =9.7) | <0.001 (χ2 =10.7) |
| Agree | 359 | 442 | 224 | 279 | 631 | 115 | 236 | 669 | 120 | ||
| Neutral or no answer | 63 | 57 | 62 | 64 | 68 | 50 | 57 | 81 | 44 | ||
| Disagree | 19 | 15 | 14 | 19 | 20 | 9 | 17 | 20 | 11 | ||
| Strongly disagree | 2 | 2 | 2 | 1 | 3 | 2 | 1 | 3 | 2 | ||
| My patients consider me as a valuable resource for food safety education | |||||||||||
| Strongly agree | 40 | 68 | 31 | 30 | 58 | 17 | 26 | 94 | 19 | <0.001 (χ2 =18.7) | <0.001 (χ2 =22.7) |
| Agree | 320 | 400 | 193 | 246 | 1 | 102 | 204 | 603 | 106 | ||
| Neutral or no answer | 92 | 98 | 73 | 81 | 92 | 54 | 74 | 140 | 49 | ||
| Disagree | 37 | 44 | 30 | 39 | 565 | 14 | 32 | 65 | 14 | ||
| Strongly disagree | 2 | 0 | 3 | 2 | 128 | 2 | 2 | 1 | 2 | ||
| A complete management system must be established for food safety in the post-COVID-19 era | |||||||||||
| Strongly agree | 154 | 235 | 96 | 112 | 328 | 45 | 98 | 343 | 44 | <0.001 (χ2 =14.7) | <0.001 (χ2 =11.9) |
| Agree | 312 | 354 | 196 | 258 | 492 | 112 | 216 | 529 | 117 | ||
| Neutral or no answer | 23 | 19 | 36 | 26 | 22 | 30 | 22 | 29 | 27 | ||
| Disagree | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| Strongly disagree | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | ||
| Food safety must establish a complete emergency response plan in the post-COVID-19 era | |||||||||||
| Strongly agree | 169 | 238 | 98 | 124 | 334 | 47 | 110 | 350 | 45 | <0.001 (χ2 =18.0) | <0.001 (χ2 =20.4) |
| Agree | 300 | 355 | 196 | 250 | 492 | 109 | 207 | 528 | 116 | ||
| Neutral or no answer | 18 | 15 | 34 | 21 | 17 | 29 | 17 | 23 | 27 | ||
| Disagree | 3 | 2 | 1 | 3 | 1 | 2 | 4 | 1 | 1 | ||
| Strongly disagree | 1 | 0 | 1 | 0 | 0 | 2 | 0 | 1 | 1 | ||
| Food safety must establish a complete traceability system in the post-COVID-19 era | |||||||||||
| Strongly agree | 194 | 257 | 109 | 144 | 361 | 55 | 125 | 379 | 56 | <0.001 (χ2 =18.7) | <0.001 (χ2 =14.7) |
| Agree | 283 | 336 | 184 | 239 | 464 | 100 | 202 | 497 | 104 | ||
| Neutral or no answer | 12 | 12 | 34 | 14 | 14 | 30 | 11 | 20 | 27 | ||
| Disagree | 1 | 4 | 1 | 0 | 4 | 2 | 0 | 5 | 1 | ||
| Strongly disagree | 0 | 1 | 2 | 1 | 1 | 2 | 0 | 2 | 2 | ||
| I am willing to have a short conversation (three minutes) with my patients to understand food safety | |||||||||||
| Strongly agree | 44 | 95 | 31 | 32 | 121 | 17 | 27 | 127 | 16 | <0.001 (χ2 =9.7) | <0.001 (χ2 =15.4) |
| Agree | 378 | 441 | 228 | 288 | 639 | 120 | 243 | 684 | 120 | ||
| Neutral or no answer | 56 | 55 | 53 | 63 | 63 | 38 | 53 | 71 | 40 | ||
| Disagree | 130 | 19 | 16 | 15 | 21 | 12 | 15 | 21 | 12 | ||
| Strongly disagree | 0 | 0 | 2 | 0 | 0 | 2 | 0 | 0 | 2 | ||
Discussion
The COVID-19 pandemic has changed people’s perceptions of food safety. For example, Iran’s health experts have recommended solutions to attenuate and prevent the spread of COVID-19.18 As the main disseminators of food safety, the food safety knowledge, attitudes, and self-reported behaviors of medical professionals may substantially affect public knowledge and attitudes towards food safety. Therefore, we conducted this study to better understand food safety knowledge, attitude, and self-reported behaviors of medical professionals before, during and after the pandemic.
In this study, statistically significant differences were found in both knowledge of and attitudes toward food safety among medical professionals before, during, and after the epidemic (P<0.001). In the wake of COVID-19, medical professionals are increasingly focused on food safety knowledge, which is a clinically important change: these professionals are an important source of food safety knowledge for the general public, and active concern about food safety may lead to more active promotion of food safety knowledge in their work, thus improving public understanding of food safety, and protecting the health of the population.
Food safety has long been the subject of research worldwide,19,20 and it is acknowledged to be an important national security issue.21 During the COVID-19 era, a large number of studies have shown that virulence, individual susceptibility, and immunity are key determinants of susceptibility to disease following exposure to the COVID-19 virus.22 Good personal nutrition may reduce the risk of infection and improve disease prognosis.23 The Chinese Nutrition Society and Chinese Medical Association have published a series of dietary nutrition recommendations and guidelines for the prevention and treatment of COVID-19,24,25 which are intended to guide the public to eat healthily, thereby bringing food safety, nutrition, and healthy lifestyle into the public consciousness.26 Our questionnaire demonstrates that increasing numbers of medical professionals agree that it is important to ensure patients receive food safety education. According to our medical professionals, their patients are more interested in understanding and receiving food safety education after the pandemic compared with before the pandemic; in addition, more medical professionals agreed that food safety education can reduce food-borne illnesses and that their patients are better able to follow food safety recommendations to prevent food-borne illnesses after compared with before the COVID-19 epidemic. This also fits well with the guidelines and recommendations.24,25
One study in the USA showed that the incidence of foodborne disease is at a high level.27 The severity of these diseases in high-risk groups implies that food safety education is an important part of prevention. Doctors with high-risk patients are therefore particularly important as food safety educators. Our results showed that a greater number of medical professionals agreed that food safety is a serious problem for patients with weakened immune functions (including confirmed COVID-19) after compared with before the COVID-19 pandemic, and that many patients may face risks associated with food safety. Patients are more likely to listen to suggestions from medical professionals regarding their diet and food ingredients when they have recently been exposed to disease, or believe that they are in danger. In one study, patients were shown to believe that the main reason why doctors might not provide nutritional advice is because the risk is low;28 however, at the same time, they regard doctors as the main source of food safety information. Compared with before the COVID-19 pandemic, more medical professionals reported that they were willing to have a short conversation with patients to help them understand food safety concepts in this study. One important obstacle that may prevent medical professionals from providing patients with education on their diet is a lack of appropriate health information. This includes interest in and expectations of dietary changes, noncompliance with recommendations, lack of nutritional knowledge, lack of available time, lack of impact on patients, lack of interest in the impact of diet on health, and lack of recommendations, treatments, or preventative measures for nutrition-related diseases.28–30
The results of targeted food safety education activities in a foreign country (countries outside the mainland) indicate that food safety education should be targeted to patients with the highest risks of serious consequences from foodborne diseases, increasing the role of doctors as food safety educators and verifying the role of doctors. Food safety educators value patients and increase their comfort by providing food safety information to their patients.31 In response to the COVID-19 pandemic, food safety services may also adopt phone-based screening and classification in the primary healthcare system to reduce unnecessary contact and spread.32 The COVID-19 pandemic has focused greater attention on food safety.33 In addition, in the post-COVID-19 era in China, understanding the risks of food safety hazards is essential to avoid potential negative health consequences of the food supply chain.34 The results of this study show that increasing numbers of medical professionals agree that they are satisfied with the general knowledge of food safety education compared with before the pandemic; in addition, a greater number agreed that they were willing to provide food safety advice. According to an increasing number of medical professionals, patients consider them to be a valuable source of food safety education. Increasing numbers of health professionals agree that complete management and traceability systems and a complete emergency response plan for food safety must be established after the COVID-19 epidemic. Domestic research in China also shows that food safety education is also very important.35 Overall, the global COVID-19 pandemic has made Chinese people pay more attention to food safety,36 a finding that is supported by our study; in response to the ongoing COVID-19 pandemic, greater global attention should therefore be paid food safety.
Conclusion
Medical professionals are important sources of food safety information, particularly during the global COVID-19 pandemic, providing direct support to patients. This creates opportunities to spread information and advice on food safety in the general population; our study indicates that more medical professionals agree with and are willing to take responsibility for food safety education in this context.
Acknowledgments
We would like to express our sincere gratitude to the medical staff all over the world who are fighting on the front lines against COVID-19. The work was supported by the Key medical disciplines of Hangzhou.
Funding Statement
This study was supported by Hangzhou Science and Technology Bureau fund (No. 20150733Q24; No. 20191203B96; No. 20191203B105; No. 20171334M01); Youth Fund of Zhejiang Academy of Medical Sciences (No. 2019Y009); Medical and Technology Project of Zhejiang Province (No. 2020362651, No. 2021KY890); Clinical Research Fund of Zhejiang Medical Association (No. 2020ZYC-A13); Hangzhou Health and Family Planning Technology Plan Key Projects (No.2017ZD02). Zhejiang Traditional Chinese Medicine Scientific Research Fund Project (No.2022ZB280).
Data Sharing Statement
All the data and materials mentioned in the manuscript are available.
Ethics Approval and Consent to Participate
Information about the purpose of the study, nature of voluntary participation, and risks associated with participation are presented in the information section of the survey. This study was approved by the ethics committee of Affiliated Hospital of Hangzhou Normal University. Informed consent was obtained from all participants. Throughout the study, the information was kept confidential, and anonymous data were recorded. This study was carried out according to the Declaration of Helsinki.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Phelan AL, Katz R, Gostin LO. The novel coronavirus originating in Wuhan, China: challenges for global health governance. JAMA. 2020;323(8):709–710. doi: 10.1001/jama.2020.1097 [DOI] [PubMed] [Google Scholar]
- 2.Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ji W, Wang W, Zhao X, et al. Cross-species transmission of the newly identified coronavirus 2019-nCoV. J Med Virol. 2020;92(4):433–440. doi: 10.1002/jmv.25682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singla R, Mishra A, Joshi R, et al. Human animal interface of SARS-CoV-2 (COVID-19) transmission: a critical appraisal of scientific evidence. Vet Res Commun. 2020;44(3–4):119–130. doi: 10.1007/s11259-020-09781-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Limon MR. Food safety practices of food handlers at home engaged in online food businesses during COVID-19 pandemic in the Philippines. Curr Res Food Sci. 2021;4:63–73. doi: 10.1016/j.crfs.2021.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iftekhar A, Cui X. Blockchain-based traceability system that ensures food safety measures to protect consumer safety and COVID-19 free supply chains. Foods. 2021;10(6):1289. doi: 10.3390/foods10061289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feng ZH, Cheng YR, Chen J, et al. Chinese medical personnel against the 2019-nCoV. J Infect. 2020;80(5):578–606. doi: 10.1016/j.jinf.2020.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang K, Wong ELY, Ho KF, et al. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine. 2020;38(45):7049–7056. doi: 10.1016/j.vaccine.2020.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma NL, Peng W, Soon CF, et al. Covid-19 pandemic in the lens of food safety and security. Environ Res. 2021;193:110405. doi: 10.1016/j.envres.2020.110405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azizi MR, Atlasi R, Ziapour A, et al. Innovative human resource management strategies during the COVID-19 pandemic: a systematic narrative review approach. Heliyon. 2021;7:e07233. doi: 10.1016/j.heliyon.2021.e07233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martindale R, Patel JJ, Taylor B, et al. Nutrition therapy in critically Ill patients with coronavirus disease 2019. JPEN J Parenter Enteral Nutr. 2020;44(7):1174–1184. doi: 10.1002/jpen.1930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.VanWeel C. Nutritional guidance in general practice—a conceptual framework. Eur J Clin Nutr. 1999;53(Suppl 2):S108–11. doi: 10.1038/sj.ejcn.1600813 [DOI] [PubMed] [Google Scholar]
- 14.Dantas KB, Tomé MABG, Aires JDS, et al. Nurses’ knowledge about regional foods, food & nutritional safety. Rev Bras Enferm. 2020;73(5):e20190044. doi: 10.1590/0034-7167-2019-0044 [DOI] [PubMed] [Google Scholar]
- 15.Buccheri C, Casuccio A, Giammanco S, et al. Food safety in hospital: knowledge, attitudes and practices of nursing staff of two hospitals in Sicily, Italy. BMC Health Serv Res. 2007;7:45. doi: 10.1186/1472-6963-7-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Su Z, McDonnell D, Wen J, et al. Mental health consequences of COVID-19 media coverage: the need for effective crisis communication practices. Global Health. 2021;17:4. doi: 10.1186/s12992-020-00654-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abbas J, Wang D, Su Z, et al. The role of social media in the advent of COVID-19 pandemic: crisis management, mental health challenges and implications. Risk Manag Healthc Policy. 2021;14:1917–1932. doi: 10.2147/RMHP.S284313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoosefi Lebni J, Abbas J, Moradi F, et al. How the COVID-19 pandemic effected economic, social, political, and cultural factors: a lesson from Iran. Int J Soc Psychiatry. 2021;67:298–300. doi: 10.1177/0020764020939984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alrobaish WS, Vlerick P, Luning PA, et al. Food safety governance in Saudi Arabia: challenges in control of imported food. J Food Sci. 2021;86(1):16–30. doi: 10.1111/1750-3841.15552 [DOI] [PubMed] [Google Scholar]
- 20.He S, Shi X. Microbial food safety in China: past, present, and future. Foodborne Pathog Dis. 2021;18:510–518. doi: 10.1089/fpd.2021.0009 [DOI] [PubMed] [Google Scholar]
- 21.Li N. Implementation and application of food safety risk assessment system in China. J Food Sci Technol. 2017;35(1):1–5. [Google Scholar]
- 22.Zhou Y, Han T, Chen J, et al. Clinical and autoimmune characteristics of severe and critical cases of COVID-19. Clin Transl Sci. 2020;13(6):1077–1086. doi: 10.1111/cts.12805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krawinkel MB. Interaction of nutrition and infections globally: an overview. Ann Nutr Metab. 2012;61:39–45. doi: 10.1159/000345162 [DOI] [PubMed] [Google Scholar]
- 24.Chinese Nutrition Society, Chinese Medical Doctor Association, Chinese Medical Association of Parenteral and Enteral Nutrition. Nutritional diet guidance for prevention and treatment of pneumonia caused by new coronavirus infection; 2020. Available from: http://www.gov.cn/fuwu/2020-02/08/content_5476196.htm. Accessed November 24, 2021.
- 25.Chinese Nutrition Society. Nutrition and Diet Guidance During Period of Anti COVID-19. 1st ed. Tsinghua University Press; 2020. [Google Scholar]
- 26.Clinical Nutrition Branch of Chinese Society of Nutrition. Nutritional suggestions for prevention and therapy of novel coronavirus pneumonia; 2020. Available from: http://food.china.com.cn/2020-02/03/content_75668384.htm. Accessed November 24, 2021.
- 27.Mead PS, Slutsker L, Dietz V, et al. Food-related illness and death in the United States. Emerg Infect Dis. 1999;5(5):607–625. doi: 10.3201/eid0505.990502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hiddink GJ, Hautvast JG, van Woerkum CM, et al. Nutrition guidance by primary-care physicians: LISREL analysis improves understanding. Prev Med. 1997;26(1):29–36. doi: 10.1006/pmed.1996.9996 [DOI] [PubMed] [Google Scholar]
- 29.Worsley A. How to improve the impact of nutrition guidance by general physicians: public health versus individual patient? Eur J Clin Nutr. 1999;53(Suppl 2):S101–7. doi: 10.1038/sj.ejcn.1600812 [DOI] [PubMed] [Google Scholar]
- 30.Kottke TE, Foels JK, Hill C, et al. Nutrition counseling in private practice: attitudes and activities of family physicians. Prev Med. 1984;13:219–225. doi: 10.1016/0091-7435(84)90053-7 [DOI] [PubMed] [Google Scholar]
- 31.Isoni Auad L, Cortez Ginani V, Stedefeldt E, et al. Food safety knowledge, attitudes, and practices of brazilian food truck food handlers. Nutrients. 2019;11(8):1784. doi: 10.3390/nu11081784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.NeJhaddadgar N, Ziapour A, Zakkipour G, et al. Effectiveness of telephone-based screening and triage during COVID-19 outbreak in the promoted primary healthcare system: a case study in Ardabil province, Iran. Z Gesundh Wiss. 2020:1–6. doi: 10.1007/s10389-020-01407-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Desai AN, Aronoff DM. Food safety and COVID-19. JAMA. 2020;323(19):1982. doi: 10.1001/jama.2020.5877 [DOI] [PubMed] [Google Scholar]
- 34.Zhang W, He H, Zhu L, et al. Food safety in Post-COVID-19 pandemic: challenges and countermeasures. Biosensors. 2021;11(3):71. doi: 10.3390/bios11030071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ma L, Chen H, Yan H, et al. Food safety knowledge, attitudes, and behavior of street food vendors and consumers in Handan, a third tier city in China. BMC Public Health. 2019;19(1):1128. doi: 10.1186/s12889-019-7475-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luo Y, Chen L, Xu F, et al. Investigationon knowledge, attitudes and practices about food safety and nutrition in the China during the epidemic of Corona virus disease 2019. Public Health Nutr. 2021;24(2):267–274. doi: 10.1017/S1368980020002797 [DOI] [PMC free article] [PubMed] [Google Scholar]